Abstract
Using a targeted controlled infusion of remifentanil during total intravenous anesthesia, we investigated the effect-site concentrations of remifentanil that correlate with different values of the Pupillary Pain Index and which concentrations were necessary for achieving a Pupillary Pain Index ≤ 4 and its usefulness in titrating opioids. The Pupillary Pain Index was measured in 54 patients prior to surgery under different remifentanil effect-site concentrations and subsequently modeled. One hundred and twenty-eight measurements were taken at different remifentanil concentrations while titrating propofol for a similar depth of hypnosis using a BIS monitor. Our modeled Hill equation revealed a remifentanil of 2.96 ng/mL for a PPI of 4, and the probability model a Ce of 3.22 ng/mL for the probability of 50% of patients achieving a PPI score ≤ 4. For the probability of 80% of patients achieving a PPI score ≤ 4 the Ce of remifentanil was 4.39 ng/mL. We conclude that concentrations of remifentanil that have been shown to suppress movement in response to noxious stimulation correspond to a Pupillary Pain Index ≤ 4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
During total intravenous anesthesia, concentrations of remifentanil of between 3.0 and 3.5 ng/mL will obliterate hemodynamic responses to tracheal intubation and LMA insertion [1, 2] as well as bodily movements secondary to skin incision [3]. This is valuable information because it provides the practitioner with a range of concentrations that prevents excessive doses of remifentanil. However, target controlled effect-site concentrations anesthetics are not always available. Furthermore, intravenous anesthetics are sometimes conducted with opioids other than remifentanil, or with a combination of opioids that may or may not include remifentanil. Some patients are tolerant to opioids and then effect site concentrations might be misleading.
In the present study we evaluate a technique to measure the nociception/antinociception balance based upon measurement of the pupil. The Pupillary Pain Index (PPI) is quantified by steadily increasing intensity of electric current delivered to the forearm. The technique is designed to prevent excessive stimulations that would result in movement or a stress response. Electrical stimulation at 100 Hz begins at 10 milliamps and is increased every second until pupillary dilation exceeds 13% of basal pupil size. PPI values range from 1 to 9 based upon the current required to dilate the pupil.
Optimal values of PPI to blunt nociceptive reflexes without using excessive opioids have been proposed by the manufacturer (PPI ≤ 4), but have not been validated. Our study aims to examine this question. We will model remifentanil effect-site concentrations with various PPI values. Our hypothesis is that a PPI of 4 will correlate with the minimum remifentanil concentrations (CeRemi) that have been shown by other studies to block nociception responses following tracheal intubation and skin incision.
Considering innovative possible applications of the pupillary reflex dilation, we conducted a clinical study with the main objective of investigating, in surgical patients under general anesthesia, the effect of different CeRemi on the Pupillary Pain Index, testing two hypothesis: the first was that the Pupillary Reflex Dilation (PRD) could be used to model the pharmacodynamics of remifentanil due to the effect that increasing concentrations of remifentanil have on the dilation response to noxious stimuli; the second was the identification of remifentanil’s concentrations compatible with a PPI score of 4 or less, considered adequate for anti-nociception.
2 Methods
This was a prospective observational study with institutional review board and ethics committee approval from Centro Hospitalar Universitário do Porto, Porto, Portugal. All participating patients gave informed consent.
A total of 54 neurosurgical patients scheduled for elective craniotomies (biopsies, tumor resections and external ventricular drainage) or lumbar spinal surgeries (laminectomies, decompressions and fusions) were included.
Anesthesia consisted exclusively of Total Intravenous Anesthesia (TIVA) with propofol and remifentanil. The study was limited to the time-period between anesthesia induction and tracheal intubation. No premedication was given. Patients with ocular diseases other than refractive errors were excluded, as well as patients with upper limb sensitive deficits due to the underlying neurosurgical pathology.
In the operating room, after placement of standard monitors and of an intravenous line in the dorsum of the hand, an infusion of a balanced electrolytic solution was started at 6 mL/kg/h. The anesthesiologist would then start a target control infusion (TCI) of remifentanil (Minto PKPD model [4, 5]) using a Fresenius Base Primea docking station (Fresenius-Kabi, Bad Homburg, Germany), at the effect-site concentration (Ce) deemed to be adequate both for the individual patient and the procedure. Afterwards, an intravenous infusion of 1% propofol was started at 3.3 mL/kg/h until loss of responsiveness was attained. This was defined as loss of eye opening to name calling and tapping on the forehead. A bolus of rocuronium was then given and the propofol infusion titrated to maintain BIS between 40 and 60 (BIS Vista™ monitor - Medtronic, Ireland). Before proceeding to intubation, the PPI was measured, and the CeRemi and BIS value noted. Based on the PPI measurement and on the clinical information available, the anesthesiologist could choose to increase or decrease the remifentanil Ce. If this was the case, after reaching pseudo-equilibrium, another PPI measurement was taken. This could be repeated several times for a same patient until the anesthesiologist deemed the CeRemi adequate to proceed to laryngoscopy. The study was terminated just before tracheal intubation.
2.1 Measurement of Pupillary Reflex Dilation
A portable infrared pupillometer (AlgiScan, IDMed, France) was used to provide an objective measure of pupil size and pupillary reflex dilation. A light-emitting diode of infrared light is directed toward the eye, a sensor detects the reflected infrared light from the iris and calculates the area and the diameter of the pupil. Application of a noxious stimulus elicits the PRD [6].
To assess the PRD, we used a stimulation mode available in Algiscan, the Pupillary Pain Index. It continuously measures the pupillary diameter (67 Hz) and applies continuously increasing electric stimulus discharge from 10 to 60 mA through skin electrodes. The response to this stimulus is assessed every 1 s interval and increased to the next intensity if the pupillary dilation is inferior to 13%. Then it classifies the response from 9 (pupillary dilation rises above 13% with just 10 mA) to 1 (when pupillary dilation is < 5% despite 3 s of 60 mA tetanic stimulation) [7, 8]. If the pupil dilates more than 20% at any point, the PPI is increased 1 point.
Using PPI instead of fixed tetanic stimulus of 60 mA avoids unnecessary high stimulation by standardizing the stimulation threshold. In our study the electrodes were placed on the volar surface of the forearm after a skin prep gel was used to lower impedance. During the measurement period there was no concurrent stimulation. A rubbed cup was used around the measured eye, while the contralateral eye was closed to exclude ambient light.
2.2 Statistical analysis
Data were compiled and analyzed using SPSS Statistics (version 25.0, IBM, USA) and Matlab® (version 2018a, Mathworks, Inc., USA).
A multivariate linear regression was used to assess the relations between the PPI and the other variables (age, gender, CeRemi and BIS). For the comparison between groups of patients ANOVA tests were performed. A p value lower than 0.01 was considered statistically significant. Data are presented as mean ± standard-deviation and median (interquartile range). For some analyses, we categorized CeRemi into intervals: [0, 1], [1, 2], [2, 3], [3, 4], [4, 5], and [5, 6] ng/mL.
Data were analyzed using a continuous probabilistic model for binary data with the probit link function, and considering as a positive event a PPI score ≤ 4 [9]. This is the suggested target range based on the manufacturer recommendations, and based on our clinical experience, the ideal target for laryngoscopy. This PPI interval means that patients tolerate at least 50 mA without a significant pupil dilation (< 13% from baseline). This analysis produces a curve of remifentanil Ce versus probability of event, allowing to estimate the Ce in which at least 50% of the observed patients reached the recommended PPI target range.
Because PPI is an ordinal variable we considered it as a continuous monotonic variable and applied a generalized sigmoid model based on the general Hill equation [10]. This model was used to describe the relation between remifentanil Ce and the observed PPI values in the total dataset using a four parameters Hill equation, and a non-linear least-square estimation (Eq. 1):
where E is the observed effect (PPI), Ce is the remifentanil effect-site concentration, E0 is the effect at CeRemi of 0, Emax is the maximum effect, and EC50 is the CeRemi for which 50% of maximum effect is obtained.
3 Results
The PPI score was evaluated in 54 patients, with an average of 56.8 ± 13.7 years of age, of which 63% were female. Mean weight and height were 67.4 ± 9.9 kg and 164.8 ± 7.7 cm, respectively. Mean Body Mass Index was 25.1 ± 3.6. There were 8 ASA I, 43, ASA II and 3 ASA III. A total of 128 measurements under different remifentanil Ce were obtained (Fig. 1). The lowest PPI score obtained was 1 and the highest was 9. For remifentanil, the lowest Ce was zero and the highest was 6.0 ng/mL. There was a wide interpatient variability for the same Ce interval that can be observed in the boxplots of Fig. 1.
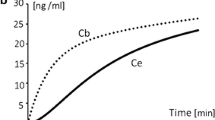
Average BIS at the moment of each of the 128 measurements was 47.0 ± 9.1. BIS values did not differ (p = 0.655) across CeRemi intervals (Fig. 2).
Age, gender and BIS did not statistically influence the PPI score (p = 0.074; p = 0.128; p = 0.884 respectively).
Figure 3 presents the probability of achieving PPI ≤ 4 considering the remifentanil Ce. The remifentanil Ce at which 50% of samples were estimated to have a PPI ≤ 4 was 2.96 (95% CI 2.54–3.44) ng/mL and for 80% it was 4.39 (95% CI 3.84–5.40) ng/mL.
Estimated remifentanil effect-site concentration and the PPI ≤ 4 probability response curve. The effect-site concentrations at which 50% and 80% of the sample were estimated to have a PPI score ≤ 4 were 2.96 and 4.39 ng/mL respectively. Circles represent patients with a PPI > 4, squares represent patients with PPI ≤ 4 and the plus sign represents the proportion of patients for each concentration. Diamonds represent the point where model estimated 50% and 80% of patients achieve a PPI ≤ 4
Regarding the dynamic effect modeling, PPI scores in relation to CeRemi in individual patients is shown in Fig. 4; a Hill model was adjusted to the total dataset, resulting in a mean square error of 5.6. Estimated parameters in Eq. 1 were E0 8.08, Emax 7.30, α 2.06 and EC50 2.87. The determined CeRemi for a PPI score of 4 was 3.22 ng/mL.
4 Discussion
We confirmed our hypothesis that a mean PPI value of 4 is recorded at average CeRemi that have been shown to suppress nociceptive responses to manipulation of the airway and to a subsequent surgical stimulus. We also observed that a PPI ≤ 4 was correlated with a wide range of CeRemi. This is consistent with other studies indicating that opioid effects are highly variable between subjects [11, 12]. Having determined this dose-dependent effect of remifentanil in the PPI might be useful to estimate the equipotent concentration of other opioids that do not have a PKPD model, and help to improve the titration of the analgesic component. This could also be useful when more than one opioid was used in the same patient.
Hypnotic monitors are in common use today, but they do not evaluate the level of antinociception during anesthesia. Pharmacokinetic-Pharmacodynamic models are useful in adjusting opioid infusion rates, but even in a normal population such as the one we have studied here, there are differences in responses to these agents. These differences would be magnified in opioid tolerant patients and those with significant co-morbidities. Several attempts are underway to address this issue as a means to tailor the delivery of analgesic agents in a precise manner for each individual patient. Pupillometry is one technique to address the nociception–antinociception balance during general anesthesia but it is only one of many such monitors [13]. Pupillometry is unique because it does not rely on hemodynamic parameters that can be altered in patients taking anti-hypertensive medications.
We propose that PPI measurements are taken at the beginning of each case, after loss of consciousness is attained, in order to appreciate the individual suppression of nociception by opioids under general anesthesia. This can be particularly useful to determine the individual opioid concentration necessary for laryngoscopy, intubation and skin incision, as these are usually the first nociceptive stimuli surgical patients receive. During the surgical procedure, the surgical dissection provides the noxious stimulus and PPI measurements then would be less useful. Sabourdin et al. [14] have demonstrated that maintaining pupil diameter during the surgical procedure within 30% of its preincision pupil size will reduce the total opioid administered, control nociceptive responses and result in a more favorable recovery.
We elected to use BIS values to control the hypnotic effect of propofol instead of measuring effect site concentrations, as propofol also has a wide interpatient variability [15]. The rate of propofol infusion was continuously adjusted according to the BIS values. Although it has been reported that low BIS values (below 30) can depress pupillary dilation following tetanic electrical stimulation [16], we were careful to avoid deep hypnosis for all of our subjects and thus avoid this potentially confounding factor. Our analysis could not detect an effect of differing CeRemi on hypnosis as evaluated by the BIS scores. One limitation of this approach in that even though we get a more personalized approach to the hypnotic effect, we cannot assess the pharmacodynamic interactions between remifentanil and propofol.
The decrease of PPI with opioid was previously demonstrated by [17] using a standard bolus of 10µk/kg of alfentanil. Here, we show this decrease using remifentanil Ce, which even under equipotent doses of opioid changes differently across patients, emphasizing the interindividual sensitivity to opioids and the need to measure the analgesic effect.
We did not correlate PPI values to hemodynamic responses following airway manipulation or to movement following the skin incision and this is a shortcoming of our study. Instead we correlated PPI values to CeRemi that have been reported by others to suppress nociception. Other investigators have observed that the magnitude of pupillary reflex dilation is predictive of movement in response to a standardized noxious stimulus over a wide range of CeRemi [3, 18]. We therefore suggest, but cannot prove, that a PPI ≤ 4 would be sufficiently antinociceptive as a preliminary value to obtain prior to the skin incision or airway manipulation. Another limitation is that the concentrations of remifentanil used for the analysis were not measured but predicted via pharmacokinetic parameters from the Minto model.
To address some of the limitations of this study, a subsequent study is needed where randomized concentrations of remifentanil and propofol are targeted and plasma concentrations are measured at pseudo-equilibration.
5 Conclusion
We confirmed that a PPI value ≤ 4 is correlated with CeRemi that have been shown to block nociceptive responses to clinical nociceptive stimuli. We propose that PPI is a measure of opioid induced suppression of nociceptive transmission in the central nervous system and can provide a guide to opioid therapy that is more precisely tailored for each individual patient.
We also observed a high variability between patients in the responses of the pupil at the same CeRemi. We conclude that anti nociceptive responses cannot always be accurately predicted only from PD-PK models.
References
Liu Z, Wang F, Wang W, Luo Y. Median effective concentration of remifentanil for the inhibition of laryngoscope-induced cardiovascular responses. Exp Ther Med. 2016;12(1):457–62.
Kim MK, Lee JW, Jang DJ, Shin OY, Nam SB. Effect-site concentration of remifentanil for laryngeal mask airway insertion during target-controlled infusion of propofol. Anaesthesia. 2009;64(2):136–40.
Guglielminotti J, Grillot N, Paule M, et al. Prediction of movement to surgical stimulation by the pupillary dilatation reflex amplitude evoked by a standardized noxious test. Anesthesiology. 2015;122(5):985–93.
Minto CF, Schnider TW, Egan TD, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil I. Model development. Anesthesiology. 1997;86(1):10–23.
Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil II. Model application. Anesthesiology. 1997;86(1):24–33.
Larson MD, Behrends M. Portable infrared pupillometry. Anesth Analg. 2015;120(6):1242–53.
Wildemeersch D, Peeters N, Saldien V, Vercauteren M, Hans G. Pain assessment by pupil dilation reflex in response to noxious stimulation in anaesthetized adults. Acta Anaesthesiol Scand. 2018;62(8):1050–56.
Vide S, Costa CM, Gambus PL, Amorim PP. Effects of ketamine on pupillary reflex dilation: a case report. A&A Pract. 2018;10(2):39–41.
Hannivoort LN, Vereecke HEM, Proost JH, et al. Probability to tolerate laryngoscopy and noxious stimulation response index as general indicators of the anaesthetic potency of sevoflurane, propofol, and remifentanil. Br J Anaesth. 2016;116(5):624–31.
Goutelle S, Maurin M, Rougier F, et al. The Hill equation: a review of its capabilities in pharmacological modelling. Fundam Clin Pharmacol. 2008;22(6):633–48.
Smith HS. Variations in opioid responsiveness. Pain Physician. 2008;11:237–48.
Searle R, Hopkins PM. Pharmacogenomic variability and anaesthesia. Br J Anaesth. 2009;103(1):14–25.
Cowen R, Stasiowska MK, Laycock H, Bantel C. Assessing pain objectively: the use of physiological markers. Anaesthesia. 2015;70(7):828–47.
Sabourdin N, Barrois J, Louvet N, et al. Pupillometry-guided intraoperative remifentanil administration versus standard practice influences opioid use: a randomized study. Anesthesiology. 2017;127(2):284–92.
Iohom G, Ni Chonghaile M, O’Brien JK, Cunningham AJ, Fitzgerald DF, Shields DC. An investigation of potential genetic determinants of propofol requirements and recovery from anaesthesia. Eur J Anaesthesiol. 2007;24(11):912–9.
Sabourdin N, Peretout JB, Khalil E, Guye ML, Louvet N, Constant I. Influence of depth of hypnosis on pupillary reactivity to a standardized tetanic stimulus in patients under propofol-remifentanil target-controlled infusion: a crossover randomized pilot study. Anesth Analg. 2018;126(1):70–7.
Sabourdin N, Diarra C, Wolk R, Piat V, Louvet N, Constant I. Pupillary Pain Index changes after a standardized bolus of Alfentanil under Sevoflurane Anesthesia. Anesth Analg. 2018;128(3):467–74.
Larson MD, Gambus PL, Agusti M, Pacheco A, Capsi P, Valencia JF. Pupil Size, Opioids, and Nociception: Does the Pupil Mirror Off Cell Activity During Anesthesia. In: Journal Symposium, ASA Annual Meeting October. 2017.
Author information
Authors and Affiliations
Contributions
SV: This author helped design and conduct the study; collect, analyze, and interpret the data; and write the manuscript. AC: This author helped analyze and interpret the data; and write the manuscript. PA: This author helped conduct the study; collect the data and write the manuscript. DL: This author helped interpret the data and write the manuscript. ML: This author helped analyze and interpret the data; and write the manuscript. PG: This author helped analyze and interpret the data; and write the manuscript. PA: This author helped design and conduct the study; collect, analyze, and interpret the data; and write the manuscript.
Corresponding author
Ethics declarations
Disclosures
Pedro Gambús is supported by a grant of COLCIENCIAS (Agency for Biomedical Research, Government of Colombia) [Registry nº 64083-807-2018].
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vide, S., Castro, A., Antunes, P. et al. Pharmacodynamic modelling of the effect of remifentanil using the Pupillary Pain Index. J Clin Monit Comput 34, 319–324 (2020). https://doi.org/10.1007/s10877-019-00323-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00323-x