Abstract
Pulse pressure variation (PPV) and stroke volume variation (SVV) during mechanical ventilation have been shown to be effective parameters to predict preload responsiveness. Although induced hypertension decreases PPV and SVV, the influences of different vasopressors on PPV and SVV are unknown. 94 patients undergoing elective otologic surgery were randomly divided into three groups: Group P (patients were given phenylephrine), Group D (patients were given dopamine), Group E (patients were given ephedrine). When surgery was ongoing and the circulation state was stable, patients were given the vasopressor to increase the systolic arterial pressure (SAP) to the pre-calculated levels: low level, 10 % < ΔSAP ≤ 20 %; medium level, 20 % < ΔSAP ≤ 30 %; high level, 30 % < ΔSAP ≤ 40 %. When invasive arterial pressure reached the target value, PPV, SVV and other parameters were recorded. Dopamine decreased the PPV and SVV more significantly than ephedrine, but less significantly than phenylephrine. The influences of phenylephrine, dopamine and ephedrine on SVV and PPV are different due to their different pharmacological mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Fluid therapy during the perioperative period is very important mostly due to the preoperative fasting, vascular dilatation and intraoperative blood loss. Many clinical studies have proven that pulse pressure variation (PPV) and stroke volume variation (SVV) are effective volume monitoring parameters to guide fluid therapy. There are other studies which have shown that central venous pressure (CVP), left ventricular end-diastolic area and pulmonary artery occlusion pressure (PAOP) as static indicators of cardiac preload have low value and are inconvenient [1, 12]. For example, Dunki-Jacobs et al. [2] demonstrated that SVV as a predictor of fluid status had more advantages than CVP by avoiding central venous catheter insertion and complications, and CVP could be safely replaced with SVV. Kramer et al. [3] concluded that PPV and SVV were superior to CVP and POAP in predicting fluid responsiveness.
PPV and SVV are greatly influenced by various factors such as the tidal volume [4–6], intravascular volume status [7], intra-abdominal pressure, [8] position [9, 10], and vasoactive drugs [11, 12]. Hadian et al. [11] found that volume challenge decreased both PPV and SVV, vasodilator therapy increased PPV and SVV, whereas increasing inotropes or vasoconstrictors did not alter PPV or SVV. Wajima et al. [12] proved that induced hypertension decreased SVV, while induced hypotension and induced hypotensive anesthesia increased SVV. Phenylephrine, dopamine and ephedrine are clinically commonly used vasopressors. Phenylephrine is an α1 receptor agonist which can elicit reflex inhibition of heart rate (HR). Dopamine and ephedrine can excite β1 and α1 receptors, and the pharmacological action of dopamine has a close relationship with its concentration. Since there must be some differences in changes of arterial pressure and HR, the decrease in PPV and SVV may vary among the three drugs.
According to the above facts, we hypothesized that PPV and SVV values were decreased differently by phenylephrine, dopamine and ephedrine. The aim of this prospective study was to find the differences in the decrease of PPV and SVV caused by phenylephrine, dopamine and ephedrine and to analyze the possible reasons by exploring whether or not the differences in changes of HR play an important role in this process.
2 Materials and methods
2.1 Subjects
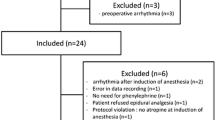
94 patients aged 18–60 years who underwent elective otologic surgery were included in this study. Such patients were selected because they have the following advantages: circulation stability that made adequate analgesia easy to achieve, less bleeding, and better physical condition. The reason for choosing patients, whose American Society of Anesthesiologists (ASA) physical status was one or two, was to tolerate blood pressure fluctuations better. And their body mass index (BMI) ranged from 18 to 26. None of the patients had known diabetes mellitus, hypertension, cardiovascular, pulmonary, endocrinological, neurological diseases, or diseases that influenced intravascular fluid volume or balance. Exclusion criteria were persistent arrhythmias and intraoperative application of vasoactive drugs except phenylephrine, dopamine and ephedrine. The study was approved by the Institutional Review Board of People’s Liberation Army General Hospital (reference number: S2014-006-02) and written informed consent was obtained from all subjects.
3 Material
The equipment used were hemodynamic multifunctional monitor (Philips InteHivue MP50, Philips, Holland), anesthesia machine (Datex-Ohmeda S/5 Aspire200, Datex. Ohmeda, Inc, Finland), bispectral index monitor (BIS XP Platform A-2000, Aspect Medical Systems, Inc, America), multifunctional injection pump (Graseby 3500, Graseby Medical Limited, UK) and vigileo stroke volume monitor (Vigileo, Edward Life-science LLC, America). Philips InteHivue MP50 could calculate the PPV value according to the arterial waveform. Cardiac output (CO), SVV, cardiac output index (CI), stroke volume (SV) and stroke volume index (SVI) were monitored continuously with the FloTrac/Vigileo system (software version 01.14).
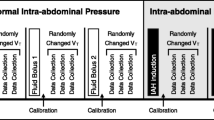
3.1 Measurement protocol
94 patients were successively numbered according to the operation time, then randomly divided into three groups: phenylephrine group (Group P), dopamine group (Group D), ephedrine group (Group E). Before arriving at the operating theatre, all patients were pre-medicated with 0.5 mg of atropine in order to reduce respiratory secretions. After the routine hemodynamic monitoring equipment was placed, all patients received an intravenous infusion of midazolam (0.05 mg/kg), propofol (1–2 mg/kg), fentanyl (3 μg/kg), and rocuronium (0.8 mg/kg) to induce anesthesia. After successful induction of anesthesia, the left radial artery catheter was inserted. Mechanical ventilation was applied with a Vt of 8 mL/kg, an inspiratory:expiratory ratio of 1:2, an inspired oxygen concentration of 50 % and an end-expiratory pressure of 0 cm H2O. Respiratory rate was adjusted to keep the arterial CO2 pressure between 30 and 40 mmHg. Anesthesia was maintained by a continuous infusion of remifentanil (0.3–0.8 μg/kg/min) and target controlled infusion of propofol (2–4 μg/mL) to keep the bispectral index between 40 and 50 and circulatory variables stable. Before the stop drug delivery, all patients received constant infusion of acetate Ringer’s solution (8 mL/kg/hr).
While the surgery was performed, the circulatory variables were stable, i.e., the SAP had a fluctuation within 10 mmHg in no <3 min. SAP, diastolic arterial pressure (DAP), mean arterial pressure (MAP), PPV, CO, CI, SV, SVI and SVV (T1) were recorded every 30 s. Target SAP values were calculated according to the following variation ranges: low (L) level, 10 % < ΔSAP ≤ 20 %; medium (M) level, 20 % < ΔSAP ≤ 30 %; high (H) level, 30 % < ΔSAP ≤ 40 % [12]. Important note: If the calculated SAP value of any level was more than 140 mmHg, this level would be abandoned. After calculation, the patient received vasopressor to increase the SAP to the pre-calculated value. In order to increase the SAP smoothly from L to H level, phenylephrine (0.1–0.5 µg/kg/min) and dopamine (5–12 µg/kg/min) were given using a Graseby 5300 pump, while ephedrine 2 mg was given intravenously each time. When the parameters were recorded, the delivery speed was adjusted to make the SAP appropriate. The research was single blind, all patients did not know what the vasopressor was given.
3.2 Statistical analysis
Values are expressed as mean ± standard deviation (SD). In every study group, comparisons of HR, SAP, DAP, MAP, PPV, CO, CI, SV, SVV and SVI were performed using Student–Newman–Keuls (SNK) test to determine if there were significance differences. A P value < 0.05 was required to reject the null hypothesis. All analyses were performed using SPSS 15.0 software (SPSS Inc., Chicago, IL, USA).
4 Results
4.1 Demographic data
Patient characteristics are shown in Table 1. Although most of the patients had data of three levels, there were few patients whose SAP could be increased to only two levels, and even one level.
4.2 Data of parameters except PPV and SVV
Values except PPV and SVV of three groups are shown on Table 2. HR, SAP, DAP, MAP, CO, CI, SV and SVI between any two levels had significant differences (P < 0.05 for all) in Group P and Group E. But in Group D, the HR had no significant differences (P > 0.05), other parameters between any two levels had significant differences (P < 0.05 for all).
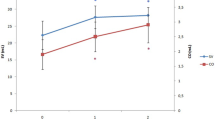
4.3 Data of PPV and ∆PPV
PPV and ∆PPV value were shown on Table 3. PPV of three levels and ∆PPV had significant differences (P < 0.05 for all) between every two of the three groups.
4.4 Data of SVV and ∆SVV
SVV and ∆SVV value were shown on Table 4. SVV of three levels and ∆SVV had significant differences (P < 0.05 for all) between every two of the three groups.
5 Discussion
The primary finding of the present study are that phenylephrine, dopamine and ephedrine influenced the PPV and SVV differently because of their different pharmacological actions. Phenylephrine decreased PPV and SVV most significantly, while ephedrine decreased PPV and SVV least. Wajima proven that induced hypertension decreased SVV, whereas induced hypotension increased SVV [12]. Therefore, we believe that PPV and SVV values may be misinterpreted due to the use of vasoactive drugs. The decrease in PPV and SVV caused by increased blood pressure due to vasopressor use may not demonstrate that the patient is hypervolemic [11, 12].
During positive pressure breathing, the SV of the left ventricle and pulse pressure vary periodically with the variation of pleural pressure, reaching the maximum during inspiration and the minimum during expiration [1, 11, 13–15] Michard has given the schematic representation of the Frank-Starling relation between ventricular preload and SV [1]. For patients with normal cardiac function, the more the ventricular preload, the less the change in SV during mechanical ventilation, that is to say, the PPV and SVV decrease with the increase of the ventricular preload [1]. Any factor that affects the preload can influence the SVV as well as PPV.
The pharmacological action of dopamine has a close relationship with its concentration, and it excites D1 receptor at 1–2 µg/kg/min, β1 receptor at 2–10 µg/kg/min and α1 receptor at >10 µg/kg/min. In this study, the concentration of dopamine was 5–12 µg/kg/min, which made the SAP values increase and the HR rise a little or remain unchanged. For the patients treated with dopamine, the HRs among the three levels did not differ significantly (P > 0.05). Therefore, it can be surmised that although dopamine could increase the SAP from the low to high level, it had no significant impact on the HR. Since dopamine can make the blood vessel contractive, the patients treated with dopamine are relatively hypervolemic, and thus the mean circulation filling pressure rises so as to increase the volume returned to the left atrium without influencing the ventricular filling time. As a result, the values of PPV and SVV decrease. The SV remained increasing because the SAP of high level was no more than 140 mmHg and dopamine improved the ability of cardiac contraction (β1 receptor excited), and the afterload might not obstruct cardiac ejection. The more the SAP increase from the low to high level, the more the PPV and SVV decrease.
Phenylephrine is an α1-adrenergic receptor agonist. When phenylephrine is administered, the HR decreases significantly as a result of its reflex inhibition of the HR. For phenylephrine, there are two reasons which can explain the improvement of the venous return: one is the recruitment of unstressed volume because of venous vessel constriction [16, 17], and the other is the increase of the ventricular filling time due to the HR decrease and diastolic extension. Since dopamine lacks the effect of diastolic prolongation (the HR did not differ significantly among the three levels), phenylephrine might increase the preload more than dopamine. When dopamine or phenylephrine is given to a patient for increasing the SAP to the same level, the PPV and SVV values changed by dopamine must be greater than those by phenylephrine, that is to say, phenylephrine decreases the PPV and SVV more than dopamine. Thiel et al. stated that “in both animal and human studies, the effect of α1-agonists on global CO depends on dosing as well as the complex interplay between the arterial and venous vasculature of both the pulmonary and systemic systems. α1-agonists have the potential to both increase and decrease CO, the former via venoconstriction and conversion of unstressed to stressed volume (thus increasing preload), the latter by restriction of venous return (thus decreasing preload)” [16]. They also stated that α1-agonists decreased venous compliance and increased venous return although their influence on CO was controversial [17–21] In this study, the venoconstriction and conversion were superior to restriction of venous return, because the SAP of high level was no more than 140 mmHg and homometric regulation improved myocardial contractility, and the afterload might not obstruct cardiac ejection. Therefore, the CO was increasing.
Ephedrine can excite β1 and α1 receptors, thereby increasing the SAP and HR. The stressed volume makes the venous return improve, this impact will be weakened by decreasing the filling time due to the HR increase and diastolic shortening. Similarly, when ephedrine or dopamine is given to a patient for increasing the SAP to the same level, the PPV and SVV values changed by dopamine must be smaller than those by ephedrine, that is to say, ephedrine decreases the PPV and SVV less than dopamine which does not have the effect of HR decrease to make the diastole shorten. With small influence on restriction of venous return and afterload, the improvement of myocardial contractility and the increase of HR resulted in the increase in SV and CO.
Taken together, the change of HR plays an important role in the differences in the decrease of PPV and SVV caused by phenylephrine, dopamine and ephedrine. The extent the vasopressors reduce the PPV and SVV values depends on the receptor(s) the drug agonizes. There are some other clinically used vasopressors such as adrenaline, noradrenaline and metaraminol. We can distinguish the changes of PPV and SVV according to the changes of HR and SAP.
Besides, the differences might be due to the systematic errors in the monitor. Artifact of the increased arterial dP/dt or differential changes in arteriolar and arterial tone made the lesser decrease in PPV and SVV with dopamine and ephedrine. Presumably arterial pressure was monitored using a radial artery catheter which would accentuate such artifact.
6 Limitations of the study
This study had several limitations. First, the experiments were implemented when the surgery was started, which may have brought about many uncertainties. To overcome this problem, a control group in which the experiments were performed before surgery should be included. Second, monitoring data which could confirm effective and sufficient analgesia were lacking, and non-effective or insufficient analgesia could result in the much more release of catecholamine. In this study, monitoring the SAP and HR only was not enough to demonstrate sufficient analgesia. Third, some data were not recorded, such as the dosage of the three drugs, especially dopamine, and the volumes of urine, bleeding and transfusion, although it seemed that the patients’ volume was unchanged during our study.
7 Conclusion
The influences of phenylephrine, dopamine and ephedrine on SVV and PPV were different due to their different pharmacological actions. Phenylephrine influenced the SVV and PPV most significantly, and ephedrine influenced least. During administration of these drugs, PPV and SVV failed to reflect the volume. We believe that PPV and SVV can still guide fluid therapy when using vasoconstrictors and the changes of PPV and SVV have more significance than the PPV and SVV themselves.
References
Michard F. Changes in arterial pressure during mechanical ventilation. Anesthesiology. 2005;103:419–28.
Dunki-Jacobs EM, Philips P, Scoqqins CR, McMasters KM, Martin RC 2nd. Stroke volume variation in hepatic resection: a replacement for standard central venous pressure monitoring. Ann Surg Oncol. 2014;21:473–8.
Kramer A, Zygun D, Hawes H, Easton P, Ferland A. Pulse pressure variation predicts fluid responsiveness following coronary artery bypass surgery. Chest. 2004;126:1563–8.
Renner J, Cavus E, Meybohm P, Tonner P, Steinfath M, Scholz J, Lutter G, Bein B. Stroke volume variation during hemorrhage and after fluid loading: impact of different tidal volumes. Acta Anaesthesiol Scand. 2007;51(5):538–44.
Kim HK, Pinsky MR. Effect of tidal volume, sampling duration, and cardiac contractility on pulse pressure and stroke volume variation during positive-pressure ventilation. Crit Care Med. 2008;36(10):2858–62.
Suehiro K, Okutani R. Influence of tidal volume for stroke volume variation to predict fluid responsiveness in patients undergoing one-lung ventilation. Jpn Soc Anesthesiol. 2011;25(5):777–80.
Biais M, Nouette-Gaulain K, Cottenceau V, Revel P, Sztark F. Uncalibrated pulse contour-derived stroke volume variation predicts fluid responsiveness in mechanically ventilated patients undergoing liver transplantation. Br J Anaesth. 2008;101:761–8.
Jacques D, Bendjelid K, Duperret S, Colling J, Piriou V, Viale JP. Pulse pressure variation and stroke volume variation during increased intra-abdominal pressure: an experimental study. Crit Care. 2011;15:R33.
Chin JH, Lee EH, Hwang GS, Choi WJ. Prediction of fluid responsiveness using dynamic preload indices in patients undergoing robot-assisted surgery with pneumoperitoneum in the Trendelenburg position. Anaesth Intensive Care. 2013;41(5):515–22.
Darlong V, Kunhabdulla NP, Pandey R, Chandralekha Puni J, Garq R, Kumar R. Hemodynamic changes during robotic radical prostatectomy. Saudi J Anaesth. 2012;6(3):213–8.
Hadian M, Severyn DA, Pinsky MR. The effects of vasoactive drugs on pulse pressure and stroke volume variation in postoperative ventilated patients. J Crit Care. 2011;26(3):328.e1–8.
Wajima Z, Shiga T, Imanaga K, Inoue T. Do induced hypertension and hypotension affect stroke volume variation in man. J Clin Anesth. 2012;24(3):207–11.
Pinsky MR. Instantaneous venous return curves in an intact canine preparation. J Appl Physiol. 1984;56:765–71.
Michard F, Chemla D, Richard C, et al. Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med. 1999;159:935–9.
Reuter DA, Bayerlein J, Goepfert MSG, et al. Influence of tidal volume on left ventricular stroke volume variation measured by pulse contour analysis in mechanically ventilated patients. Intensive Care Med. 2003;29:476–80.
Thiele RH, Nemergut EC, Lynch C 3rd. The physiologic implications of isolated alpha(1) adrenergic stimulation. Anesth Analg. 2011;113:284–96.
Thiele RH, Nemergut EC, Lynch C 3rd. The clinical implications of isolated alpha(1) adrenergic stimulation. Anesth Analg. 2011;113:297–304.
Butterworth J. Do alpha agonist increase venous return? Anesthesiology 2004; 101:1038. Author reply 1039.
Simon AC, Levenson JA, Levy BY, Bouthier JE, Peronneau PP, Safar ME. Effect of nitroglycerin on peripheral large arteries in hypertension. Br J Clin Pharmacol. 1982;14:241–6.
Toraman F, Karabulut H, Goksel O, Evrenkaya S, Tarcan S, Alhan C. Comparison of antihypertensives after coronary artery surgery. Asian Cardiovasc Thorac Ann. 2005;13:302–6.
Pinsky MR. The dynamic interface between hemodynamic variables and autonomic tone. Crit Care Med. 2005;33:2437–8.
Acknowledgments
First of all, I would like to extend my sincere gratitude to my supervisor, Wei-dong Mi, for his instructive advice and useful suggestions on my thesis. I am deeply grateful of his help in the completion of this thesis. High tribute shall be paid to Ms. Bin Zhao, whose profound knowledge of English triggers my love for this beautiful language and whose earnest attitude tells me how to learn English. I am also deeply indebted to all the other tutors and teachers in Department of Anesthesiology of People’s Liberation Army General Hospital for their direct and indirect help to me.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kong, R., Liu, Y., Mi, W. et al. Influences of different vasopressors on stroke volume variation and pulse pressure variation. J Clin Monit Comput 30, 81–86 (2016). https://doi.org/10.1007/s10877-015-9687-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9687-6