Abstract
Somatosensory evoked potentials (SEPs) have been linked to noxious activation and stimulus intensity. In this exploratory study we investigated the impact of anaesthetic drugs on SEPs and pain ratings, to assess their applicability as an objective measure of the nociception/anti-nociception balance. Following institutional approval and written informed consent, 10 healthy adult volunteers were enrolled (29.5 ± 9.1 years, 63.0 ± 8.9 kg and 171.4 ± 7.2). Median nerve electrical stimulation was adjusted according to volunteers’ sensitive, motor and painful thresholds (PT). Baseline SEPs were registered, and remifentanil and propofol administered using a stair scheme TCI. For each drug combination a 1.3×PT stimulus was administered, and volunteers evaluated pain intensity in a numerical rating scale (0–10). SEPs’ amplitudes and latencies were normalized by the baseline values, reducing volunteers’ intervariability. Stimulation currents varied between 6–52 mA (1.3×PT) and pain ratings between 0 and 9. Cortical SEPs latencies were decreased for higher stimulus intensities (P < 0.01), accompanied by increased pain ratings (P < 0.01). An individually adjusted/normalized ratio based on cortical SEPs amplitude and interpeak latency is proposed(\(R_{Norm}\)): \(R_{Norm}\) and NSR were significantly correlated in three out of nine subjects, and \(R_{Norm}\) and remifentanil Ce were significantly correlated in two (low number of evaluation points). \(R_{Norm}\) was shown to decrease with increasing doses of propofol and remifentanil (P < 0.05). The proposed metric was depressed by anaesthetics and reflected pain evaluations. Further research is necessary to increase the number of volunteers and drugs’ combination, to assess its applicability during surgically adequate anesthetic leves.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Establishment of objective methods for pain assessment, comparable between individuals, is still an open research question. Pain is a multifaceted experience that depends on several factors such as stimulus characteristics [11, 14, 23], patient’s experience [18], or attention [19], activating different coding and interpreting brain areas [6, 11, 23]. Understanding pain perception and pathways from sensing organs to higher processing in the brain, is of paramount importance when developing a tool to assess nociception. Most of the research done in the search for a tool to translate the nociception/anti-nociception balance (Noc/ANoc) is focused on the use of physiological variables, such as heart rate and blood pressure, basing the translation of the patients’ state on passive variables linked to nociception [3, 12, 13, 22, 26]. This hampers definition of the adequate Noc/ANoc state, because indirect signals related to pain activation are used to translate the patient’s state, rather than direct measures of the sensing process. The concept of evoked potentials may configure a solution for this issue, since it is based on the register of an electrical potential from the nervous system, in response to a known stimulus, and it may be measured anywhere along the anatomical pathways [15, 27]. The use of evoked potentials has been of great importance in understanding the sensing and brain mechanisms in response to outer stimuli both in human and animal subjects [21, 25]. In anaesthesia, evoked potentials have been explored mostly using auditory and somatosensory evoked potentials (SEPs), to evaluate hypnosis state and sensory impairment of the patient [4, 9]. Application of evoked potentials during anaesthesia, technical aspects, and the influence of drugs used in the perioperative period on the measured responses were reviewed [15, 27], demonstrating that different factors interfere with waves collection and characteristics, particularly drugs. It has been shown that propofol and remifentanil increase SEPs latency and decrease amplitude in a dose-dependent manner [9, 15], leading to the assumption that SEPs may contain information on the sensing process and drug attenuation. We decided to investigate, in healthy adult volunteers, the use of SEPs for different stimuli intensities, and inspect anaesthetic drugs’ impact on the evoked responses and pain evaluations reported by the volunteer.
2 Methods
Clinical protocol and experiments were approved by the Ethics Committee and Administration Council of Santo António’s Hospital, Centro Hospitalar do Porto. Written informed consent was obtained from all subjects.
2.1 Subjects
Healthy volunteers without pre-medication filled the study requirements. Ten healthy adult volunteers, five men, age \(29.5\pm 9.1\) years old, weight \(63.0 \pm 8.9\,\hbox {kg}\) and height \(171.4 \pm 7.2\,\hbox {cm}\), were enrolled in the study, providing written informed consent after being informed about the experimental procedure. The volunteers did not receive any kind of monetary compensation. For each volunteer a folder, referenced by a code number, was created to store study files collected during the experiment.
2.2 Electrical stimulation
For the assessment of patterned responses to electrical stimulation, skin contact electrodes were positioned on volunteers’ wrist, for median nerve stimulation. Rectangular (0.5 ms) electrical stimuli were initiated and increased in 0.1 mA steps. The volunteers were instructed to state when the stimulus was perceived (sensitive threshold, ST), when it produced involuntary movement (motor threshold, MT), and when it was perceived as painful (painful threshold, PT). Electrical stimuli thresholds were assessed at the beginning of the experiment, and a supra-painful stimulus was defined (1.3-fold painful threshold, 1.3×PT) for SEPs acquisition.
2.3 Somatosensory evoked potentials
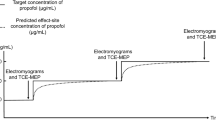
Volunteers were maintained in a comfortable position, in a silent environment during the experiment. EEG needle electrodes were placed according to the monitoring standards (international 10–20 system), and two EEG channels were collected: scalp contralateral to the stimulation site (C3′ or C4′, 2 cm posterior to C3 and C4, respectively), scalp (Cz); and neck (C5S or C2S, cervival on the spinous processes C5 or C2), scalp (Cz). Monitor Endeavor™ CR (Nicolet-Vyasis) was used to collect SEPs data, with a stimulation rate of 3.1Hz (180 stimulus/min). Before drugs’ administration, all baseline values were registered for the PT and 1.3×PT. SEPs’ latencies and amplitudes were extracted as follows: for the cortical SEPs, the amplitude was determined as the difference between the positive and negative peaks, and the latency the difference between the latencies of the positive and negative peaks (interpeak latency); for the cervical SEPs amplitude and latency of the single peak were used (Fig. 1).
2.4 Anesthesia
Volunteers presented themselves in the operating room with fasting superior to 6 hours. Standard monitoring was used including ECG, SpO2, non-invasive arterial blood pressure, and Bispectral Index (BIS). A hand vein was catheterized with a venous catheter G20, saline infusion started at 400 ml/h to maintain steady drugs’ infusion throughout the procedure, and nasal oxygen at 3 l/min. Anaesthetics’ administration was conducted using a target controlled infusion (TCI) system and data synchronization software RugloopII© Waves. Propofol and remifentanil were administered by effect-site concentration (Ce) steering using Schnider [24] and Minto [20] pharmacokinetic models, respectively. All stimuli and important events were registered in a text file. Collected data were later exported to data-sheet files using Labgrab2.03©.
2.5 Experimental protocol
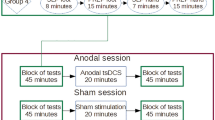
The experimental design is presented in Fig. 2. At the beginning of the experiment sensing thresholds were identified, followed by acquisition of correspondent baseline SEPs (Baseline). Drugs’ TCI was initiated following three different administration schemes: remifentanil 0.5/1.0 ng/ml increasing steps only (scheme 1); fixed remifentanil (1.0 ng/ml) and propofol (0.5 μg/ml) increasing steps (scheme 2); and finally, fixed propofol (1.2 μg/ml) and increasing remifentanil 0.5/1.0 ng/ml steps (scheme 3). For each drug change, when effect-site and plasmatic concentrations reached equilibrium, infusion was maintained for two minutes to assure drugs’ steady-state, and only then electrical stimulation was initiated (1.3×PT). For each stimulus, volunteers were instructed to rate pain intensity in a numerical rating scale (NRS), varying from 0 (no pain) to 10 (worst possible pain). Each administration scheme was interrupted if arterial pressure or heart rate decreased 20% from baseline values, the volunteer lost response to verbal stimulus, maintaining response to mechanical stimulation (score 2 in the Observer Assessment of Awareness and Sedation Score [8], OAAS/S = 2), or by clinical recommendation. Following the procedure described above, volunteers rested for a period of one hour in the recovery room, receiving express indication not to drive a car, operate machinery or precision mechanisms during that day.
Study experimental protocol timeline. Baseline: period without drug administration to acquire sensing thresholds. scheme 1: remifentanil 0.5/1.0 ng/ml increasing steps only. scheme 2: fixed remifentanil (1.0 ng/ml) and propofol (0.5 μg/ml) increasing steps. scheme 3: fixed propofol (1.2 μg/ml) and increasing remifentanil 0.5/1.0 ng/ml steps
2.6 Statistical analysis
Data were compiled in Microsoft Office Excel 2010, and analysed using Matlab R2007B. To assess relations between stimulus intensity, SEPs’ wave characteristics, pain evaluations in the NRS and drug doses, non-parametric Spearman rank correlation coefficient, paired sample Wilcoxon rank sign test, and Kruskal-Wallis test were used. \(P<0.05\) was considered statistically significant.
3 Results
Following data collection, one subject was excluded from the analysis since SEPs evaluation for the PT stimulus was not available. Drugs’ administration was interrupted every time the volunteer was unable to respond to verbal command, while being capable of responding to mechanical stimulation (OAAS/S = 2), and this was achieved in all volunteers. Brief periods of apnoea occurred, all spontaneously reversed requiring only neck extension and drugs’ administration interruption. BIS minimum values reached during the experiment were \(52.3 \pm 8.6\). Pain ratings in the NRS varied from 0 to 9, and 1.3×PT stimulation currents varied between 6 and 52 mA.
3.1 Stimulus intensity and baseline cortical somatosensory evoked responses
Individually adjusted stimulus currents for ST were \(2.9 \pm 1.3\), for MT \(8.0 \pm 2.8\), for PT \(20.3 \pm 9.6\) and for 1.3×PT \(26.5 \pm 12.4\,\hbox {mA}\). Increasing variability in stimulation currents from the sensitive threshold to the painful threshold was observed. Volunteers presented different painful thresholds, meaning different sensitivities to electrical stimulation; also, SEPs’ wave characteristics varied among volunteers, in spite of stimulation with the individually adjusted painful stimulus, or supra-painful as shown in Fig. 3.
a Pain evaluation in the numerical rating scale (NRS, 0–10), and b baseline amplitudes and interpeak latencies of cortical SEPs, in response to painful (PT) and 1.3-fold painful (1.3×PT) stimuli. Pain NRS evaluations were significantly higher for the 1.3×PT than for the PT, and SEPs latency lower (**\(P< 0.01\))
Volunteers evaluated pain in a NRS both when the PT was achieved, and for every 1.3×PT stimulus applied subsequently. We observed that as soon as the stimulus was intense enough to produce pain the NRS evaluations were superior or equal to 5 in almost all volunteers. Figure 3 presents the pain evaluations for the PT and 1.3×PT stimuli at baseline. From the PT to the 1.3×PT stimuli, the evaluations in the NRS were either maintained or increased (\(P<0.01\)). Cortical interpeak latency was significantly decreased within the same subject (\(P<0.01\)) when comparing SEPs for the PT and 1.3×PT at baseline (Fig. 3).
3.2 Pain evaluations and anaesthetics’ concentrations
Remifentanil administration, at increasing concentrations, resulted in a reduction of reported pain in the NRS (\(P<0.01\)). The same occurred when propofol was administered. Figure 4 presents the NRS evaluations for the maximum drugs combinations achieved in each administration scheme. Although a decrease in the NRS evaluations was observed for all administration schemes, in schemes 2 and 3 the volunteers either evaluated pain with lower values in the NRS, or were unable to evaluate pain due to becoming unresponsive (lack of verbal response, OAAS/S = 2).
Pain evaluations in the numerical rating scale (NRS, 0–10) for the maximum combination on each administration scheme (a), and corresponding normalized ratio (\(R_{Norm}\)) of cortical SEPs’ amplitude and interpeak latency (b) (\(\circ\) data outliers). Significant difference was found between baseline and scheme 1 NRS pain evaluation, and between \(R_{Norm}\) at baseline and scheme 3 (*\(P<0.05\), **\(P<0.01\))
3.3 Normalized cortical somatosensory evoked responses’ ratio
The interindividual variability in current stimuli, and corresponding SEPs’ amplitudes (Fig. 3), led us to normalize SEP’s amplitude in response to the 1.3×PT stimulus, by the observed SEP’s amplitude at baseline for the PT stimulus individually adjusted, as follows:
where \(SEPAmp\) is the observed SEP’s amplitude in response to the 1.3×PT stimulus, and \(SEPAmp_{0}\) is the SEP’s amplitude for the PT stimulus baseline.
Since increased latencies and decreased amplitudes are related to drug SEPs attenuation [9, 15], the ratio \(R_{Norm}\) was also obtained as follows:
where \(SEPLat_{Norm}\) is the normalized latency by the observed latency to the PT baseline (\(SEPLat_{0}\)) as given by
This way, a normalized and dimensionless metric \(R_{Norm}\) is proposed.
3.3.1 Cortical somatosensory evoked responses’ ratio and pain evaluations
A decrease in cortical SEPs’ amplitude with decreasing pain evaluations in the NRS was observed. After normalization volunteers’ intervariability was reduced, and the associations maintained. All volunteers exhibited the same direction of relation, confirmed by the Spearman rank correlation coefficients (Table 1): in all volunteers the correlation coefficients were positive, but significant in only three subjects (larger number of evaluation points). Since \(R_{Norm}\) is dimensionless and comparable between subjects, data from all volunteers were combined to obtain a group correlation coefficient. The correlation coefficient between \(R_{Norm}\) and the evaluations in the NRS exhibited a positive relation (\(\rho =0.17\), P = 0.05 and 137 data points).
3.3.2 Cortical somatosensory evoked responses’ ratio and anaesthetics’ concentrations
In general, a decrease in \(R_{Norm}\) with increasing drug doses is observed, although the relation is not always evident (reduced number of evaluation points for each volunteer). Spearman rank correlation coefficients between \(R_{Norm}\) and the remifentanil Ce were obtained for each volunteer (Table 1). Almost all volunteers exhibited the same association direction, however statistical significance was achieved in only one volunteer. A decrease tendency of \(R_{Norm}\) in each drug scheme was observed, although not statistically significant (scheme 1 \(\rho =-0.18\), 96 data points; scheme 2 \(\rho =-0.13\), 46 data points; scheme 3, \(\rho =-0.02\), 32 data points).
3.3.3 Cortical somatosensory evoked responses’ ratio of maximum drug doses analysis
\(R_{Norm}\) values for the maximum drug doses achieved in each volunteer, for each administration scheme, were analyzed (Fig. 3b), this way we are able to compare SEPs for the same state in all volunteers (loss of response, cardiovascular depression, or apnoea), regardless of their intervariability in terms of necessary Ce to induce these changes. There was a decrease in \(R_{Norm}\) for every administration scheme in comparison to baseline, accompanied by a decrease in pain evaluations (Fig. 3a). This difference was significant between the values observed at Baseline (no drugs) and the values observed at scheme 3 (increasing remifentanil Ce with fixed propofol, \(P<0.05\)). Although we may observe a tendency of decreasing \(R_{Norm}\) for the maximum drug doses achieved in schemes 1 and 2, more data would be necessary; the incidence of outliers still has an important effect since we are analyzing isolated measurements of SEPs, in non-paralyzed conscious volunteers, with a limited number of samples.
3.4 Cervical somatosensory evoked potentials
Data was collected both from cervical and cortical sites to compare evoked potentials pre and post central sensory processing. The ratio between cervical SEPs’ amplitude and latency were analyzed with original and normalized values. No relation between cervical SEPs’ ratio and corresponding NRS ratings, or anaesthetics’ Ce was observed. Correlation coefficients between NRS evaluations and the SEPs ratio obtained for each volunteer presented different directions, with average value of \(0.13 \pm 0.25\). The same happened for the SEPs ratio versus remifentanil Ce (\(-0.09 \pm 0.40\)).
4 Discussion
In this study a new method, combining both amplitude and interpeak latency of cortical SEPs, is proposed as an objective indicator of the Noc/ANoc balance. Propofol and remifentanil increasing doses led to cortical SEPs wave depression with amplitude reduction, increased interpeak latency, and simultaneously to decreased NRS pain evaluations. Our observations corroborate results presented in previous studies [9, 15], indicating a depression in wave amplitude, and increase in latency, with increasing doses of propofol and remifentanil. Information contained on SEPs’ wave morphology was analyzed, in collaborating volunteers, in response to different stimulus intensities, and in response to hypnotic and analgesic drugs, allowing for a more complete analysis of SEPs applicability in the assessment of Noc/ANoc balance, since volunteers’ pain evaluations were obtained for each drug combination.
Sensory evoked potentials wave characteristics are affected by several factors [1, 2, 15, 19, 27], including genetic predisposition [10], leading to wide interindividual variability in sensing thresholds and amplitude responses. We observed interindividual variability both on the individually adjusted stimulus thresholds, especially in the PT, and in the evoked responses, confirming that pain mechanisms vary between subjects. Any tool capable of objectively assessing the Noc/ANoc balance must take this into account. To overcome this limitation we decided to normalize the SEPs wave characteristics by the PT response at baseline, producing measures comparable between subjects. Cortical SEP’s interpeak latency and amplitude were combined into a single index (\(R_{Norm}\)), taking advantage of the information contained in both parameters and their inverse proportionality in response to anaesthetics [15], and providing a dimensionless measure, comparable between subjects. We observed that this information is complementary, and the relation between pain evaluations in the NRS, drug doses, and the ratio are maintained.
No relation was found between cervical SEPs and both NRS ratings and drug doses. This may be due to the fact that the cervical potential is collected prior to superior processing and therefore, is only representative of the stimulus conduction to higher processing, resulting in similar wave characteristics (same intensity stimulus and no attenuation provided by the drugs) [28], nonetheless the number of volunteers is low, and further studies would be necessary to evaluate these relations.
The hypnotic drug had an impact on the cortical SEPs wave, as well as the analgesic drug. Although one may think that the analgesic drug should be the only blocking the stimulus, the addition of propofol resulted in SEPs depression accompanied by a decrease in pain evaluations, both reversed with propofol withdrawal. Some studies have addressed the issue of propofol analgesic effects [5, 7, 16] and it is described that propofol also has the ability to inhibit the response to noxious stimuli [7]. A recent study also reported this relation with evoked potentials, demonstrating that SEPs were depressed by propofol, sevoflurane and ketamine in subanesthetic doses, although without significant suppression of cortical activity, leading to the conclusion that the observed effects seem to be specific to the analgesia [29].
It should be noted that the number of data points to determine the correlation coefficients individually is in many cases low and therefore with limited meaning. To strengthen the results presented in this study the number of volunteers should be increased. Also, SEPs curve extraction is very conditioned by noise, and since these are very low amplitude signals, this may hinder the results. More robust filtering techniques in the extraction of the SEPs should be studied, as well as the stimulus modality that only elicits noxious responses, such as thermal stimulation. This was an exploratory study, and although significant correlation between \(R_{Norm}\) and NRS evaluations was only observed in 3 of the 9 volunteers, we believe these are encouraging results to further explore SEPs as an indicator of the Noc/ANoc balance during anesthesia. Future studies should increase of the number of volunteers, drugs’ combinations, and the evaluation of the indicator for deeper levels of anesthesia.
5 Conclusion
In our study we analyzed the influence of an analgesic and a hypnotic drug on SEPs wave characteristics and corresponding pain as evaluated by the subject, demonstrating that cortical SEPs wave characteristics contain information on pain perceived intensity, and on the anti-nociception provided by the anaesthetic drugs. We propose a new method combining cortical SEPs wave amplitude and interpeak latency, which may be used as a dimensionless indicator, comparable between subjects, of the Noc/ANoc balance. Such an indicator would be valuable to translate the nociceptive/drug attenuation balance not only in conscious subjects, but most importantly in individuals not capable of communicating verbally or in other ways, due to disease, altered mental or conscious state, or young age. This is a new way of looking at nociception assessment that is gaining great interest in distinguishing the effects of anesthetics and analgesics during the intraoperative management [17, 29].
References
Arendt-Nielsen L, Bjerring P. Reaction times to painless and painful CO2 and argon laser stimulation. Eur J Appl Physiol. 1988a;58(3):266–73.
Arendt-Nielsen L, Bjerring P. Sensory and pain threshold characteristics to laser stimuli. J Neurol Neurosurg Psychiatry. 1988b;51(1):35–42.
Barvais L, Engelman E, Eba JM, Coussaert E, Cantraine F, Kenny GN. Effect site concentrations of remifentanil and pupil response to noxious stimulation. Br J Anaesth. 2003;91(3):347–52.
Bonhomme V, Llabres V, Dewandre PY, Brichant JF, Hans P. Combined use of bispectral indextm and a-linetm autorregressive indextm to assess anti-nociceptive component of balanced anaesthesia during lumbar arthodesis. Br J Anaesth. 2006;96(3):353–60.
Borgeat A, Wilder-Smith OH, Suter PM. The nonhypnotic therapeutic applications of propofol. Anesthesiology. 1994;80(3):642–56.
Bornhövd K, Quante M, Glauche V, Bromm B, Weiller C, Bchel C. Painful stimuli evoke different stimulus-response functions in the amygdala, prefrontal, insula and somatosensory cortex: a single-trial fmri study. Brain. 2002;125(6):1326–36.
Brunton L, Parker K, Blumenthal D, Buxton I (eds). Goodman and gilman’s manual of pharmacology and therapeutics, 12th edn. McGraw Hill; 2008.
Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, Schwam EM, Siegel JL. Validity and reliability of the observer’s: Assessment of alertness/sedation scale: Study with intravenous midazolam. J Clin Psychopharmacol. 1990;10(4).
Crabb I, Thornton C, Konieczko KM, Chan A, Aquilina R, Frazer N, Dor CJ, Newton DE. Remifentanil reduces auditory and somatosensory evoked responses during isoflurane anaesthesia in a dose-dependent manner. Br J Anaesth. 1996;76(6):795–801.
Fu ES, Zhang Y, Li Q, Morris RW, Levitt RC. Baseline differences in mechanical nociception: Genetic regulation. Anesthesiology p A505; 2010.
Gannong WF (ed). Review of Medical Physiology, 22nd edn. Lange Medical Books/McGraw-Hill; 2005.
Greenwald SD, Rosow C. Bis and emg variability increase before somatic responses during surgery. Anesthesiology. 2006;105:1027.
Gruenewald M, Meybohm P, Ilies C, Hcker J, Hanss R, Scholz J, Bein B. Influence of different remifentanil concentrations on the performance of the surgical stress index to detect a standardized painful stimulus during sevoflurane anaesthesia. Br J Anaesth. 2009;103(4):586–93.
Kruger L (ed). Methods in pain research. CRC Press; 2001.
Kumar A, Bhattacharya A, Makhija N. Evoked potential monitoring in anaesthesia and analgesia. Anaesthesia. 2000;55(3):225–41.
ller EAM, Spangsberg N, Arendt-Nielsen L, Schultz P, Kristensen MS, Bjerring P. Subhypnotic doses of thiopentone and propofol cause analgesia to experimentally induced acute pain. Br J Anaesth. 1991;66(2):185–8.
Mashour GA. Neurophysiology and intraoperative nociception: new potentials? Anesthesiology. 2013;118:239–40.
Melzack R, Torgerson WS. On the language of pain. Anesthesiology. 1971;34(1):50–9.
Miltner W, Jr, RJ, Braun C, Larbig W, Somatosensory event-related potentials to painful and non-painful stimuli: effects of attention. Pain. 1989;38(3):303–12.
Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. ii. model application. Anesthesiology. 1997;86:24–33.
Ohara S, Crone NE, Weiss N, Treede RD, Lenz FA. Amplitudes of laser evoked potential recorded from primary somatosensory, parasylvian and medial frontal cortex are graded with stimulus intensity. Pain. 2004;110(1–2):318–28.
Rantanen M, Yli-Hankala A, Gils MV, Yppril-Wolters H, Takala P, Huiku M, Kymlinen M, Seitsonen E, Korhonen I. Novel multiparameter approach for measurement of nociception at skin incision during general anaesthesia. Br J Anaesth. 2006;96(3):367–76.
Rhoades RA, Bell DR (eds). Medical physiology principles for clinical medicine, 3rd edn. Lippincott Williams and Wilkins, 2009.
Schnider TW, Minto CF, Gambus PL, Andresen C, Goodale DB, Shafer SL, Youngs EJ. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–82.
Shaw FZ, Chen RF, Tsao HW, Yen CT. Comparison of touch- and laser heat-evoked cortical field potentials in conscious rats. Brain Res. 1999;824(2):183–96.
Storm H. Changes in skin conductance as a tool to monitor nociceptive simulation and pain. Curr Opin Anaesthesiol. 2008;21(6):796–804.
Thornton C, Sharpe RM. Evoked responses in anaesthesia. Br J Anaesth. 1998;81(5):771–81.
Thornton C, Creagh-Barry P, Jordan C, Luff NP, Dor CJ, Henley M, Newton DE. Somatosensory and auditory evoked responses recorded simultaneously: differential effects of nitrous oxide and isoflurane. Br J Anaesth. 1992;68(5):508–14.
Untergehrer G, Jordan D, Eyl S, Schneider G. Effects of propofol, sevoflurane, remifentanil, and (s)-ketamine in subanesthetic concentrations on visceral and somatosensory painevoked potentials. Anesthesiology. 2013;118:308–17.
Acknowledgments
The authors would like to thank the participation of all volunteers and clinical investigators in this study, especially Dr. Francisco Lobo, Dr. Liliana Pinto, Dr. Diana Afonso, Dr. Germano Cardoso, Dr. Helena and Dr. Luís Silva (Neurinbloc). The first author was supported by a scholarship from the Portuguese Foundation for Science and Technology (FCT - SFRH/BD/35879/2007). The authors would also like to acknowledge the UISPA-IDMEC Porto.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Castro, A., Amorim, P., Nunes, C.S. et al. Effect of propofol and remifentanil on a somatosensory evoked potential indicator of pain perception intensity in volunteers. J Clin Monit Comput 29, 561–567 (2015). https://doi.org/10.1007/s10877-014-9632-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9632-0