Abstract
Purpose
Jacobsen syndrome (JS) is a rare form of genetic disorder that was recently classified as a syndromic immunodeficiency. Available detailed immunological data from JS patients are limited.
Methods
Clinical and immunological presentation of twelve pediatric patients with JS by means of revision of clinical records, flow cytometry, real-time PCR, and lymphocyte functional testing were collected.
Results
Recurrent infections were registered in 6/12 patients (50%), while bleeding episodes in 2/12 (16.7%). White blood cell and absolute lymphocyte counts were reduced in 8/12 (66.7%) and 7/12 (58.3%) patients, respectively. Absolute numbers of CD3+ and CD4+ T cells were reduced in 8/12 (66.7%) and 7/12 (58.3%), respectively. Of note, recent thymic emigrants (RTE) were reduced in all tested patients (9/9), with T-cell receptor excision circle analysis (TRECs) showing a similar trend in 8/9 patients; naïve CD4+ T cells were low only in 5/11 patients (45.4%). Interestingly, B-cell counts, IgM memory B cells, and IgM serum levels were reduced in 10/12 (83.3%) patients. Natural killer (NK) cell counts were mostly normal but the percentages of CD16+CD56low/− cells were expanded in 7/7 patients tested. The observed immunological alterations did not correlate with patients’ age. Finally, responses to proliferative stimuli were normal at presentation for all patients, although they may deteriorate over time.
Conclusions
Our data suggest that patients affected with JS may display important numeric and maturational alterations in the T-, B-, and NK-cell compartments. These findings suggest that JS patients should be regularly monitored from an immunological point of view.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Jacobsen syndrome (JS) is a rare syndromic condition caused by partial deletions of the 11q chromosome. It was first described by Jacobsen in 1973 [1] and appears more frequently among males (male:female ratio = 2:1) [2]. The estimated prevalence of this disorder is 1/100,000 births. The length and position of the chromosomal deletion define the diagnosis of complete (11q23del; 5 to 20 MB) or partial JS (less than 5 MB) [2,3,4]. Rarely, partial JS can be due to single nucleotide variants or small indels in critical genes in this region, such as ETS1 or FLI1 [5, 6].
Clinical presentation of JS is variable and may include growth and neurodevelopmental delay, facial dysmorphisms, and behavioral disorders, together with possible endocrine, auditory, and ocular burdens [2,3,4, 7, 8]. Affected patients may present malformations in various organs such as kidneys, gastrointestinal, urinary, and genital tract [2,3,4]. Central nervous system involvement has also been reported [2,3,4]. Hematological findings include macrothrombocytopenia with platelet dysfunction, known as Paris-Trousseau anomaly, variably associated with a reduction in the other cell lines and progressively resolving with age [8].
In 2019, the latest International Union of Immunological Societies (IUIS) classification recognized JS as a syndromic form of primary immunodeficiency [9]. Altered immunological parameters included variable hypogammaglobulinemia, lymphopenia, and reduction of switched memory B cells suggesting a defective germinal center function [2,3,4, 10]. Affected patients have been reported to frequently suffer from recurrent respiratory infections both of the upper and the lower tract, as well as from warts [2,3,4, 7,8,9].
To date, available data on immune alterations in JS are limited and derive mostly from small cohorts or single case reports.
We report on a detailed immunological evaluation from twelve pediatric patients with JS at onset. We also performed a longitudinal 7-year immunological follow-up of a female patient currently in adolescence. Collectively, our data show novel and important phenotypic and numeric alterations in the T-cell compartment of affected patients with progressive functional impairment over time. In addition, affected patients’ NK cells show impaired maturational profile, a finding that has not been reported yet. Finally, the humoral compartment also resulted affected, in line with previously published data. Our data suggest that clinicians following patients with JS should consider periodic immunological evaluation during follow-up.
Materials and Methods
Patients
Retrospective clinical data of twelve JS patients from five centers in Italy (Brescia, Monza, Firenze, Bologna, Padova) were collected. All patients were diagnosed with JS based on genetic analysis showing deletions of the long arm of chr 11. Informed consent was collected from all patients or their legal guardians. The study was approved from the local hospital Ethical Committee and was conducted in accordance with the 1964 Helsinki Declaration.
Flow Cytometry
All analyses were performed from fresh blood samples drawn in the previous 24 h and conserved at room temperature. Appropriate mixtures of monoclonal antibodies (MoAb) were used to design multicolor panels and stain blood cells according to the manufacturer’s protocols in order to screen circulating main lymphocyte populations as well as T- and B-cell subsets.
A TBNK panel, including CD45, CD3, CD4, CD8, HLA-DR, CD19, CD16, and CD56, was used to analyze the main lymphocyte populations and T-cell activation (HLA-DR).
T-cell differentiation was assessed by using CD3, CD4, CD8, CD45RA, CCR7, CD31, and TCRγδ MoAb, which allow to recognize T CD4 and CD8 naïve (CD45RA+CCR7+), central memory (CM) (CD45RA−CCR7+), effector memory (EM) (CD45RA−CCR7−), and terminal differentiated cells (TD) (CD45RA+CCR7−), as well as recent thymic emigrants (RTEs) (CD45RA+CCR7+ CD31+), and TCRγδ expressing cells.
Analyses of B-cell subpopulations were assessed by using CD10, CD19, CD20, IgM, IgD, CD38, CD27, and CD21 MoAb. It enables the differentiation of recent bone marrow emigrants (RBEs) (CD38++CD10+), naïve (IgD+IgM+CD27−), switched memory (Sw. Mem.) (IgD−IgM−CD27+), IgM memory (IgM Mem.) (IgD+IgM+CD27+), terminal differentiated (CD38++CD27+CD20−), and CD21lowCD38low cells.
Multicolor tubes were acquired on FACSCanto II (BD Biosciences) flow cytometers. Data were analyzed with FACSDiva (BD Biosciences).
Quantification of TRECs
The number of TRECs was quantified by multiplex quantitative real-time PCR, using DNA obtained from peripheral blood mononuclear cells (PBMC), isolated by density gradient centrifugation from fresh blood samples as previously reported [11]. Their quantities, as well as that of the T-cell receptor alpha chain constant (TRAC) region, which is used as a reference gene, have been extrapolated from a standard curve obtained by tenfold serial dilutions of a plasmid DNA which contains an insert of TREC and TRAC fragments. The number of TRECs is given per milliliter of blood, equal to (TRECs/PBMC) × (lymphocyte + monocyte count in 1 mL of blood).
Alternatively, TREC assays were measured in dried blood spot [12]. Calibration curves were generated by means of tenfold serial dilution of plasmids that contain TREC and ß-actin sequences. The forward, reverse primers and probes for TRECs were designed using Primer Express software version 3.0 (Applied Biosystems). TREC levels were normalized per microliter of blood, assuming that the sample contains approximately 9 μL of whole blood (3 punch, 3 μL of whole blood/punch). Finally, TREC values were converted to numbers per milliliter.
Reference values previously generated using the first protocol were validated also in groups of age-matched healthy controls tested with the alternative protocol.
T-cell Proliferation Assay
PBMCs were isolated by density gradient centrifugation from fresh blood samples and labelled with Carboxyfluorescein Succinimidyl Ester (CFSE) (1.6 × 106 cells resuspended in 1 mL of PBS) according to the manufacturer’s protocol (BD Biosciences). CFSE-labelled PBMCs were placed in 96-well culture plates and stimulated with phytohemagglutinin (PHA) (6.25 μg/mL) (Sigma Aldrich), or anti-CD3 MoAb (5 μg/mL) (Beckman Coulter) with or without interleukin 2 (IL2) (600 U/mL) (Peprotech). After 4 days of incubation under standard culture conditions, cells were stained with anti-CD3 PerCP-Cy5.5, anti-CD4 APC, and anti-CD8 APC-H7 MoAb according to the manufacturer’s protocol (BD Biosciences). Samples were acquired on FACSCanto II flow cytometer and T-cell proliferation was quantified using FlowJo (Tree Star) software.
Results
Clinical Presentation at First Immunological Evaluation
All patients in our cohort presented typical dysmorphic features of JS. Nearly all showed neurodevelopmental delay (11/12, 91.7%), while 6/12 (50%) patients displayed growth retardation. Interestingly, congenital heart disease was observed in 7/12 (58.3%) patients (Table 1).
Susceptibility to Infectious Diseases
The patients with JS in our cohort presented an increased susceptibility to infections: three out of twelve patients (25%) suffered from recurrent herpes simplex mucocutaneous infections, while another four out of twelve (33.3%) presented recurrent respiratory infections. One of these four patients (Pt5) suffered from severe Aspergillus fumigatus pneumonia and developed bronchiectasis at the age of 4 years, based on lung CT scan. Due to the recurrence and/or severity of the infectious episodes, 5/12 (41.7%) patients receive antimicrobial prophylaxis and 2/12 (16.7%) immunoglobulin substitution (Table 1).
Bleeding Diathesis
Two out of twelve patients (16.7%) had a positive clinical history for bleeding-related complications and they both experienced brain hemorrhage during the perinatal period. More in detail, multiple cerebral cysts containing hemorrhagic material were identified by ultrasound and magnetic resonance imaging (MRI) at birth in Pt1, resulting in secondary epilepsy and contributing to an important neurodevelopmental delay. Pt8 presented with intraventricular and parenchymal hemorrhage in the first days of life, as documented by brain computed tomography and MRI. These bleeding manifestations were associated with a very severely reduced platelet count (10 × 103/μL at birth for Pt1 and 4 × 103/μL at birth for Pt8).
During our evaluation, two out of twelve patients (16.7%) developed a mild thrombocytopenia (platelet count between 100 and 150 × 103/μL), two patients (16.7%) had a moderate thrombocytopenia (platelet count between 50 and 100 × 103/μL), while the remaining ones (8/12; 66.7%) presented normal platelet counts (Table 2).
Immunological Evaluation
The immunological work-up during the first evaluation showed altered values for several parameters (Table 2). More in detail, white blood cell (WBCs) and absolute lymphocyte counts were reduced in 8/12 (66.7%) and 7/12 (58.3%) patients, respectively (Table 2 and Supplementary Table 1), independently of their age. Absolute neutrophil and platelet counts were reduced in 1/12 (8.3%) and 4/12 (33.3%) patients, respectively.
Immunoglobulin serum values determination showed reduced IgM levels in 10/12 (83.3%) patients while IgG and IgA levels were reduced in 4/12 (33.3%) and 5/12 (41.7%), respectively.
Peripheral distribution of T-cell subsets at first evaluation revealed alterations in CD3+, CD4+, and CD8+ cell percentages in 5/12 (41.7%), 3/12 (25%), and 6/12 (50%), respectively. Of note, absolute lymphocyte counts of these subsets displayed a common trend, with total CD3+ and CD4+ T cells reduced in 8/12 (66.7%) and 7/12 (58.3%) patients, respectively, while only four out of twelve (33.3%) patients showed a reduction in the CD8+ T-cell counts (Table 2 and Supplementary Table 1).
Lymphocyte alterations were observed also in B and NK compartments. Percentages of CD19+ and CD3−CD16/CD56+ cells were reduced in 5/12 (41.6%) and increased in 2/12 (16.7%), respectively. On the other hand, absolute numbers of the same subsets were reduced in 10/12 (83.3%) and 3/12 (25%), respectively (Table 2 and Supplementary Table 1).
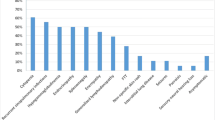
These evident immunological abnormalities in the lymphocyte compartments prompted us to proceed with a more detailed immunophenotyping (Table 3, Fig. 1, and Supplementary Table 1).
Characterization of CD4+ T cells in patients with Jacobsen syndrome. (A) Representative flow cytometry plots of cell subset distribution for Pt 9 (right) and an age-matched healthy control (HC) (left). Cell subsets were measured as percentages of CD4+ cells and are presented as follows: CD45RA+ CCR7+ naïve cells (red), among which CD31+ recent thymic emigrants (RTEs) are highlighted in yellow, CD45−CCR7+ central memory (orange), CD45RA−CCR7− effector memory (light orange), and CD45RA+CCR7− terminally differentiated cells (pink). (B) Graphic representation of CD4+ naïve cells, RTEs, and TRECs in patients with Jacobsen syndrome. Patients’ percentages of naïve cells, RTEs, and number of TRECs are indicated with black dots and plotted on X axis according to patients’ age group; gray boxes and lines represent interquartile ranges and 2.5–97.5 percentile ranges, respectively, of age-matched healthy control values derived from our laboratory database
As seen in Fig. 1A, patients’ T cell showed important alterations in the early stages of CD4+ T cell maturation. Of note, while the percentages and absolute counts of naïve CD4+ T cell subsets were decreased only in 5/11 (45.4%) and 6/11 (54.5%) patients, respectively (Table 3, Fig. 1B, and Supplementary Table 1), RTEs were significantly reduced in all patients analyzed both as absolute counts and as percentages. TRECs showed a similar trend, with 8/9 (89.9%) patients displaying values below or at the lower end of the normal range for age (Fig. 1C).
Analysis of peripheral B-cell distribution showed several alterations (Fig. 2, Table 3, and Supplementary Table 1), mostly involving the memory compartment, as shown in Fig. 2A. More in detail, the early stages of B cell maturation (i.e., RBEs) were normal in almost all patients, while naïve B cells were increased in 3/12 (25%) patients suggesting a perturbance at early stage of both CD4+ and CD19+ cells in this syndrome. In parallel with the reduction of IgM serum levels, five out of twelve patients (41.7%) (10/12 in terms of absolute counts) showed a reduction in IgM memory B cells. Switched memory B cell percentages were reduced only in one patient (8.3%), but 7/12 showed a reduction in terms of absolute counts (Table 3, Fig. 2B, and Supplementary Table 1). Of note, the CD21lowCD38low population showed a relative expansion in 4/12 (33.3%) patients in the absence of autoimmune manifestations. Finally, the terminal stages of peripheral B-cell maturation (terminally differentiated cells) were below normal range in 1/9 (11.1%) patients (Table 3 and Supplementary Table 1).
Flow cytometry characterization of B-cell subsets in patients with Jacobsen syndrome. (A) Representative plots of B-cell subsets distribution for Pt8 (right) and an age-matched healthy control (HC) (left). Cell subsets were measured as percentages of total CD19+ B cells and, after gating on CD19+CD20+ cells, are presented as follows: IgD+IgM+CD27−, naïve cells (light blue), among which CD38++CD10+ recent bone marrow emigrants (RBEs) are highlighted in yellow, sIgD+sIgM+CD27+ IgM memory (green), and sIgD−sIgM−CD27+ switched memory cells (light green). (B) Graphic representation of switched and IgM memory B cells in patients with Jacobsen syndrome. Black dots indicate patients’ percentages of switched (left panel) and IgM memory B cells (right panel) at first immunological evaluation and are plotted on X axis according to patients’ age group; gray boxes and lines represent interquartile ranges and 2.5–97.5 percentile ranges, respectively, of age-matched healthy control values derived from our laboratory database
Analysis of NK cells, based on CD16 and CD56 expression on CD3 negative cells, revealed a marked reduction of the percentage of the main NK subset, constituted by CD16+CD56dim cells, in all tested patients (7/7), independently of patients’ age (Supplementary Table 1 and Supplementary Fig. 1). On the opposite, all of these patients displayed a number of CD16+CD56low/− cells that exceeded their normal age range (Supplementary Table 1 and Supplementary Fig. 1).
Based on the T-cell alterations in our cohort, responses to proliferative stimuli were evaluated and resulted normal in all tested subjects at first evaluation (Table 3 and Supplementary Table 1).
Data on long-term immunological follow-up in patients affected with JS are not available. However, one of the affected patients from our cohort has been in regular follow-up for 7 years starting from the age of 6 (Pt8). As shown in Supplementary Fig. 2, during follow-up, her neutrophil and platelet counts remained at the lower end of the normal range for age (data not shown), while her absolute lymphocyte counts were constantly below the lower limit for age (Supplementary Fig. 2). Within lymphocyte subsets, both CD4+ and CD8+ naïve T cells remained constantly below the normal range for age. RTEs followed the same pattern (Supplementary Fig. 2).
Finally, while the IgG serum levels resulted within normal range for age, both IgA and IgM remained constantly below normal limits, indicating a parallelism with the poor amount of switched and IgM memory B cells, whose percentages on total B cells were constantly at the lower end of the normal range for age (Supplementary Fig. 2).
Considering the important lymphopenia associated with profound T-cell alterations, responses to proliferative stimuli were repeated over time and revealed a progressive impairment upon in vitro PHA stimulation at the age of 11 years (Supplementary Fig. 2), while the responses to the other stimuli (i.e., anti-CD3 MoAb, anti-CD3 MoAb + IL2) resulted impaired starting from the age of 12 (Supplementary Fig. 2).
Discussion
The recent IUIS classification included JS (11q23del) as a syndromic form of primary immunodeficiency [9]. The limited number of patients that have been evaluated from an immunological point of view presented mainly with humoral alterations such as low immunoglobulin serum levels and reduced switched memory B cells [9]. A minority of reported patients showed reduced T- and NK-cell counts, in the context of reduced lymphocytes count [9, 10, 13]. We report on the first detailed immunological evaluation of twelve pediatric patients affected with JS and show that all the main lymphocyte compartments presented with some alterations in cell differentiation.
From a clinical point of view, our study confirms the previously reported increased incidence of respiratory infections among patients with JS, independently of age. Both the upper and the lower respiratory tract were affected, with only one patient presenting with bronchiectasis and opportunistic lung infections (fungal). Based on clinical complications and/or immunological alterations, 5/12 patients were put on antimicrobial prophylaxis and 2/12 on immunoglobulin replacement treatment.
Patients with JS have been reported to show an increased bleeding risk due both to reduced platelet number and altered platelet function [2, 3]. Brain hemorrhages are a rare manifestation of JS but have been reported exclusively beyond the perinatal period [14]. Here we report that cerebral bleeding can occur in utero or in the immediate post-natal period, most likely resulting in a worsening of the neurological status. The relatively high prevalence of perinatal brain hemorrhages in our cohort suggests that this might be an under-estimated feature of JS.
Lymphopenia resulted a rather common finding, being present in 58.3% of patients, independently of age, and can be severe in some cases. In fact, Pt1 has an important reduction of CD3+ T cells, reduced TREC and profound hypogammaglobulinemia requiring immunoglobulin substitution since the first months of life, similar to what observed in Severe Combined Immune Deficiency. Reduction of immunoglobulin serum levels has previously been reported in JS and is considered a hallmark of JS in the recent IUIS classification. In our cohort, all of the patients displayed abnormal immunoglobulin serum levels in at least one subclass. Specifically, 10/12 patients had low IgM serum levels, while IgG and IgA levels were reduced in 4/12 and 5/12 patients, respectively. Peripheral B-cell evaluation showed a profound reduction in IgM memory cell counts in all patients with low IgM serum levels (10/10). Five of them also presented with an associated reduction in IgG serum levels with a parallel reduction in switched memory B cell counts. Overall, these data suggest that, at least in this cohort of JS patients, humoral alteration associated with reduction in one or more immunoglobulin isotypes may reflect a B-lymphocyte maturation impairment that appears more evident in later stages of cell differentiation.
Defective immunoglobulin secretion and B-cell maturation are both observed in JS patients from an early age to adulthood, and there are no signs of amelioration of immunoglobulin serum levels nor enlargement of memory B-cell compartment during follow-up in Pt8.
The T-cell compartment has been reported to be numerically altered in a minority of JS patients, together with reduced NK cells [10]. In our cohort, evaluation of peripheral T-cell distribution showed variable alterations. More in detail, patients’ T-cell compartment showed an important defect in the early stages of CD4+ T-cell maturation with a significant reduction in RTEs in all patients analyzed and a concomitant reduction of TRECs in the majority of cases. Of note, naïve CD4+ T cells followed the same trend only in a small number of subjects. The later stages of peripheral T cell differentiation were not significantly altered. Our data clearly suggest that patients with JS may present important T-cell alterations, in slight contrast with previously published data [10], with evident clinical implications. Although T cells were phenotypically and numerically significantly altered in our cohort, initial functional evaluation of these cells by means of responses to proliferative stimuli was normal. Nonetheless, during follow-up, the functional performance of T cells in Pt8 appears to decline, further suggesting that periodic detailed immunological evaluation in affected patients is warranted.
In our cohort, 3/12 patients presented with reduced NK-cell counts. The separate evaluation of CD56 and CD16 expression on NK cells showed the presence of a not age-related abnormal cell subset distribution also in this lymphocyte compartment. Specifically, we observed an increased frequency of CD16+CD56low/− cells in all JS tested patients compared to age-matched healthy controls. Given the phenotypic characteristics of this cell subset, whose expansion can be observed in aging and in some chronic viral infections such as HIV [15, 16], it is tempting to speculate that JS patients may present an increased proportion of poor cytotoxic-terminally differentiated cells compared to normal individuals from an early age.
The chromosomal deletion responsible for JS involves genes such as FLI-1, ETS-1, and TIRAP that have been shown to variably affect the immune system in experimental settings [17,18,19,20,21,22]. Among these, ETS-1 and TIRAP have been shown to be involved in T- and B-cell activation and maturation [17,18,19]. Available experimental data on the role of FLI-1 suggest its involvement in the maturation and function of T, B, and NK cells [20,21,22]. Although the role of these genes in patients with JS has not been studied yet in detail, it is possible that they may play a role in the immunological alterations observed in our cohort of patients.
In conclusion, our data show for the first time important alterations in all the main lymphocyte subsets in pediatric JS patients, independently of age. Reduced absolute lymphocyte counts should be considered one of the first elements indicating the necessity of an immunological evaluation for affected patients, besides infectious history. Finally, our data suggest that, since the T-cell compartment tends to deteriorate over time, periodic detailed immunological evaluations for affected patients are warranted.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Jacobsen P, Hauge M, Henningsen K, Hobolth N, Mikkelsen M, Philip J. An (11;21) translocation in four generations with chromosome 11 abnormalities in the offspring. A clinical, cytogenetical, and gene marker study. Hum Hered. 1973;23:568–85. https://doi.org/10.1159/000152624.
Favier R, Akshoomoff N, Mattson S, Grossfeld P. Jacobsen syndrome: advances in our knowledge of phenotype and genotype. Am J Med Genet C Semin Med Genet. 2015;169(3):239–50. https://doi.org/10.1002/ajmg.c.31448.
Grossfeld PD, Mattina T, Lai Z, Favier R, Jones KL, Cotter F, et al. The 11q terminal deletion disorder: a prospective study of 110 cases. Am J Med Genet A. 2004;129A(1):51–61. https://doi.org/10.1002/ajmg.a.30090.
Penny LA, Dell’Aquila M, Jones MC, Bergoffen J, Cunniff C, Fryns JP, et al. Clinical and molecular characterization of patients with distal 11q deletions. Am J Hum Genet. 1995;56(3):676–83.
Tootleman E, Malamut B, Akshoomoff N, Mattson SN, Hoffman HM, Jones MC, et al. Partial Jacobsen syndrome phenotype in a patient with a de novo frameshift mutation in the ETS1 transcription factor. Cold Spring Harb Mol Case Stud. 2019;5(3):1–9. https://doi.org/10.1101/mcs.a004010.
Stevenson WS, Rabbolini DJ, Beutler L, Chen Q, Gabrielli S, Mackay JP, et al. Paris-Trousseau thrombocytopenia is phenocopied by the autosomal recessive inheritance of a DNA-binding domain mutation in FLI1. Blood. 2015;126(17):2027–30. https://doi.org/10.1182/blood-2015-06-650887.
Pivnick EK, Velagaleti GV, Wilroy RS, Smith ME, Rose SR, Tipton RE, et al. Jacobsen syndrome: report of a patient with severe eye anomalies, growth hormone deficiency, and hypothyroidism associated with deletion 11 (q23q25) and review of 52 cases. J Med Genet. 1996;33(9):772–8. https://doi.org/10.1136/jmg.33.9.772.
Breton-Gorius J, Favier R, Guichard J, Cherif D, Berger R, Debili N, et al. A new congenital dysmegakaryopoietic thrombocytopenia (Paris-Trousseau) associated with giant platelet α-granules and chromosome 11 deletion at 11q23. Blood. 1995;85(7):1805–14. https://doi.org/10.1182/blood.v85.7.1805.bloodjournal8571805.
Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunningham-Rundles C, Etzioni A, et al. Human Inborn Errors of Immunity: 2019 Update on the Classification from the International Union of Immunological Societies Expert Committee. Epub 2020. Erratum in: J Clin Immunol. 2020 Feb 22. J Clin Immunol. 2020;40(1):24–64. https://doi.org/10.1007/s10875-019-00737-x.
Dalm VASH, Driessen GJA, Barendregt BH, van Hagen PM, van der Burg M. The 11q terminal deletion disorder Jacobsen syndrome is a syndromic primary immunodeficiency. J Clin Immunol. 2015;35(8):761–8. https://doi.org/10.1007/s10875-015-0211-z.
Sottini A, Ghidini C, Zanotti C, Chiarini M, Caimi L, Lanfranchi A, et al. Simultaneous quantification of recent thymic T-cell and bone marrow B-cell emigrants in patients with primary immunodeficiency undergone to stemcell transplantation. Clin Immunol. 2010;136:217–27. https://doi.org/10.1016/j.clim.2010.04.005.
Remaschi G, Ricci S, Cortimiglia M, De Vitis E, Iannuzzi L, Boni L, et al. TREC and KREC in very preterm infants: reference values and effects of maternal and neonatal factors. J Matern Fetal Neonatal Med. 2019;29:1–6. https://doi.org/10.1080/14767058.2019.1702951.
Seppänen M, Koillinen H, Mustjoki S, Tomi M, Sullivan KE. Terminal deletion of 11q with significant late-onset combined immune deficiency. J Clin Immunol. 2014;34(1):114–8. https://doi.org/10.1007/s10875-013-9966-2.
Grossfeld P. Brain hemorrhages in Jacobsen syndrome: a retrospective review of six cases and clinical recommendations. Am J of Med Genet A. 2017;173(3):667–70. https://doi.org/10.1002/ajmg.a.38032.
Muller-Durovic B, Grahlert J, Devine OP, Akbar AN, Hess C. CD56-negative NK cells with impaired effector function expand in CMV and EBV co-infected healthy donors with age. Aging. 2019;11:724–40. https://doi.org/10.18632/aging.101774.
Milush JM, Lopez-Verges S, York VA, Deeks SG, Martin JN, Hecht FM, et al. CD56negCD16(+) NK cells are activated mature NK cells with impaired effector function during HIV-1 infection. Retrovirology. 2013;10:158. https://doi.org/10.1186/1742-4690-10-158.
Weller S, Bonnet M, Delagreverie H, Israel L, Chrabieh M, Maródi L, et al. IgM+IgD+CD27+ B cells are markedly reduced in IRAK-4-, MyD88-, and TIRAP- but not UNC-93B-deficient patients. Blood. 2012;120(25):4992–5001. https://doi.org/10.1182/blood-2012-07-440776.
Nguyen HV, Mouly E, Chemin K, Luinaud R, Despres R, Fermand JP, et al. The Ets-1 transcription factor is required for Stat1-mediated T-bet expression and IgG2a class switching in mouse B cells. Blood. 2012;119(18):4174–81. https://doi.org/10.1182/blood-2011-09-378182.
Tsao HW, Tai TS, Tseng W, Chang HH, Grenningloh R, Miaw SC, et al. Ets-1 facilitates nuclear entry of NFAT proteins and their recruitment to the IL-2 promoter. Proc Natl Acad Sci U S A. 2013;110(39):15776–81. https://doi.org/10.1073/pnas.1304343110.
Smeets MF, Wiest DL, Izon DJ. Fli-1 regulates the DN2 to DN3 thymocyte transition and promotes gammadelta T-cell commitment by enhancing TCR signal strength. Eur J Immunol. 2014;44(9):2617–24. https://doi.org/10.1002/eji.201444442.
Bradshaw S, Zheng WJ, Tsoi LC, Gilkeson G, Zhang XK. A role for Fli-1 in B cell proliferation: implications for SLE pathogenesis. Clin Immunol. 2008;129(1):19–30. https://doi.org/10.1016/j.clim.2008.05.010.
Masuya M, Moussa O, Abe T, Deguchi T, Higuchi T, Ebihara Y, et al. Dysregulation of granulocyte, erythrocyte, and NK cell lineages in Fli-1 gene-targeted mice. Blood. 2005;105(1):95–102. https://doi.org/10.1182/blood-2003-12-4345.
Acknowledgements
We would like to thank the patients, the patients’ families, and the nurses for their collaboration and efforts. Several of the authors are members of the European Reference Network for Rare Immunodeficiency, Autoinflammatory and Autoimmune Diseases (project identification no. 739543).
Funding
The research leading to these results has received funding from the European Community’s Seventh Framework Programme FP7/ 2007–2013 under grant agreement no 201549 (EURO-PADnet HEALTH- F2–2008–201549) and grant from the Italian Ministry of Research GR- 2010–2315762. The research leading to these results also received funding from the “Fondazione C. Golgi,” Brescia, Italy, and the Jeffrey Modell Foundation. We thank “Fondazione Città della Speranza ONLUS (https://cittadellasperanza.org/)” for their support to our scientific work.
Author information
Authors and Affiliations
Contributions
M.B., F.S., L.G., S.R., A.M., S.R., D.Z., A.P., D.M., V.L. designed the work and coordinated the project; M.B., F.S., L.G., S.R., A.M., S.R., D.M., B.P., C.C., L.L., M.C., A.S., L.I., C.G., L.R. R.B., A.P., D.M., V.L. contributed with clinical, immunological, and molecular data; M.B., L.G., S.R., A.M., S.R., A.P., D.M., V.L. analyzed the data and wrote the manuscript; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved from the local hospital Ethical Committee and was conducted in accordance with the 1964 Helsinki Declaration.
Consent to Participate
Informed consent was collected from all patients or their legal guardians.
Consent for Publication
Informed consent was collected from all patients or their legal guardians.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10875_2021_1169_MOESM1_ESM.pdf
Supplementary file1 (PDF 115 KB) Supplementary Table 1. Detailed hematologic and immunologic evaluation of twelve patients with Jacobsen Syndrome
10875_2021_1169_MOESM2_ESM.pdf
Supplementary file2 (PDF 84 KB) Supplementary Figure 1. Flow cytometry representation of natural killer cells distribution in Jacobsen Syndrome patients. Representative cytofluorimetric panels of CD3-CD16/CD56+ NK cells, in which it is highlighted the relative proportion of CD16+CD56dim (dark pink) and CD16+CD56low/- (pink) cells, are shown for Pt9 (right) compared to an age-matched heathy control (HC) (left)
10875_2021_1169_MOESM3_ESM.pdf
Supplementary file3 (PDF 158 KB) Supplementary Figure 2. Long term immunological follow-up of a single patient with Jacobsen Syndrome. Patient’s parameters over a 6-year follow up period: A) WBCs (absolute counts), B) lymphocytes (absolute counts), C) serum IgA, D) serum IgM, E) CD4 naïve (percentages) F) CD4 RTE (percentages), G) CD8 naïve (percentages) H) switched memory (percentages), I) IgM memory cells (percentages) compared to aged matched healthy controls’ range (grey full area). L) Mitogen proliferative response to anti-CD3 MoAb, anti-CD3 MoAb + IL2, PHA, over time. = reduced response compared to control
Rights and permissions
About this article
Cite this article
Baronio, M., Saettini, F., Gazzurelli, L. et al. Immunological Evaluation of Patients Affected with Jacobsen Syndrome Reveals Profound Not Age-Related Lymphocyte Alterations. J Clin Immunol 42, 365–374 (2022). https://doi.org/10.1007/s10875-021-01169-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-021-01169-2