Abstract
Introduction
Chronic granulomatous disease (CGD) is an inherited mutational defect in any of the NADPH oxidase complex, CYBB (gp91-phox), NCF1 (p47-phox), CYBA (p22-phox), NCF2 (p67-phox), or NCF4 (p40-phox) leading to inability of phagocytes to perform effective respiratory burst and thus diminished killing of bacteria and fungi. The identification of defective proteins aids in establishing a diagnosis prior to genetic analysis, which is rather labor-intensive, expensive, and time-consuming.
Aim
The present study aims at assessing the NADPH proteins by performing the intracellular staining with specific monoclonal antibodies and their assessment on flow cytometry. The use of flow cytometry is less laborious and faster to perform than western blot. It also confirms the diagnosis of CGD and detects the affected components allowing proper management of patients.
Materials and Methods
Twenty-eight patients from 25 different kindred, clinically suspected as CGD were recruited in Egypt. Dihydrorhodamine test was performed to confirm the diagnosis of the patients. Intracellular staining of NADPH components using specific monoclonal antibodies was performed followed by flow cytometric analysis.
Results
The present study revealed that the most common defective protein in our cohort is p22-phox, found in 13 patients (46.4 % of cases) followed by p47-phox in 8 patients (28.6 %), gp91-phox in 5 patients (17.9 %), and finally p67-phox in 2 patients (7.1 %).
Conclusion
In countries with limited resources and yet large number of CGD patients, the analysis of the defective proteins by flow cytometry is an optimum solution for confirming the diagnosis and is a step for targeted sequencing in families seeking prenatal diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic granulomatous disease (CGD) [OMIM No. 306400] is an inherited mutational defect in the NADPH oxidase complex leading to inability of phagocytes to perform effective respiratory burst and thus diminished killing of bacteria, yeasts, and fungi [1, 2].
CGD patients suffer from two categories of clinical manifestations: recurrent, life-threatening infections with catalase positive organisms and excessive inflammatory reactions leading to granulomatous lesions [3].
Mutations in any of the genes of NADPH oxidase components will lead to CGD, including X-CGD due to defects in CYBB (encoding gp91-phox) and AR-CGD due to defects in NCF1 (for p47-phox), CYBA (for p22-phox), or NCF2 (for p67-phox) or NCF4 (for p40-phox) [4].
Diagnosis of CGD is concluded by demonstrating absent or markedly reduced oxidase activity in stimulated neutrophils. Screening for CGD is accomplished by nitro blue tetrazolium test (NBT) or by flow cytometry dihydrorhodamine (DHR) 123 assay [5].
NBT is a yellow dye which is reduced to blue formazan by the production of superoxide resulting from the respiratory burst and is interpreted manually. Whereas the DHR depends on stimulating neutrophils with phorbol 12-myristate 13-acetate (PMA) to produce reactive oxygen intermediates (ROIs) that react with a non-fluorescent probe such as DHR turning it into fluorescent rhodamine, detected by the flow cytometer [6].
The identification of defective proteins prior to genetic analysis—which is often labor-intensive, expensive, and time-consuming—aids in establishing the diagnosis. Here, we aimed to perform intracellular staining of the NADPH proteins by specific monoclonal antibodies followed by their assessment by flow cytometry presuming an easier and faster technique to detect the defective proteins.
Material and Methods
Subjects
Patients clinically suspected as CGD were recruited from the Primary Immunodeficiency Unit, at the Pediatric Department of Cairo University Children Hospital, Egypt, between the years 2014 and 2015. The clinical diagnosis was based on the European Society for Immunodeficiencies (ESID) criteria for diagnosis including deep-seated infection due to bacteria and/or fungi (abscesses, osteomyelitis, lymphadenitis), recurrent pneumonia, lymphadenopathy and/or hepatomegaly and/or splenomegaly, obstructing/diffuse granulomata (gastrointestinal or urogenital tract), chronic inflammatory manifestations (colitis, liver abscess, and fistula formation), failure to thrive, and having affected family member. Diagnosis was confirmed by abnormal DHR assay results (Fig. 1). In accordance with the Helsinki Declaration, an informed consent was obtained from the patient’s guardians prior to enrolment.
Dihydrorhodamine assay on flow cytometry in a normal control (1) and a CGD patient (2) showing a gating on the neutrophils by their characteristic forward and side scatter, b fluorescence after incubation of neutrophil with the dihydrorhodamine, and c fluorescence after incubation with phorbol myristate acetate that result in reduction of dihydrorhodamine into fluorescent rhodamine. The (W) represent the residual enzyme activity which is calculated as the percentage of cells after the PMA stimulation that showed fluorescence shift from the unstimulated cells (37.6 % in this patient); however, the amount of fluorescence per cell is markedly reduced as indicated by the MFI (3.2). Stimulation index was calculated by dividing mean fluorescence intensity (MFI) in stimulated cells over MFI of unstimulated cells
Dihydrorhodamine Assay
One hundred microliters of patient’s blood was diluted 1:9 with phosphate-buffered saline (PBS) and incubated with DHR (Sigma-Aldrich) for 15 min; stimulation with PMA (Abcam) for 30 min was done; then, blood was washed, and red blood cells (RBCs) were lysed for 10 min (Versalyse, Beckman Coulter). A stimulation index (SI) was calculated for gated neutrophils by dividing the mean fluorescent intensity (MFI) of stimulated cells by the MFI of unstimulated cells. SI of 70 was considered the cutoff in our laboratory based on testing 100 normal healthy individuals [7]. Residual NADPH activity of neutrophils was also estimated for each patient as percent of cells shifted after PMA stimulation compared to unstimulated cells as previously described [8] (Fig. 1).
Intracellular Staining of Neutrophil NADPH Components
Staining for NADPH components was done on either whole blood samples or on neutrophils collected by dilution of blood 1:1 with PBS and density separation using Ficoll hypaque, followed by RBCs lysis from the sediment at the bottom of tubes.
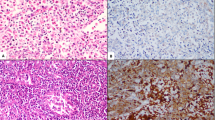
For each of NADPH components, 50 μl of either whole EDTA blood or separated neutrophil was added in a flow cytometry tube; blood was fixed and permeabilized with Beckman Coulter IntraPrepTM permeabilization kit (PNIM2389) according to the manufacturer’s instructions. In each tube, 5 μl of monoclonal antibody diluted 1:20, specific either to rabbit monoclonal [EPR5065] to NOXA2/p67-phox (ab109523), rabbit monoclonal [ERP13134] to NCF1/p47 (ab179457), mouse monoclonal [CS9] to cytochrome b245 light chain antibody/p22 (ab87736), or rabbit polyclonal to NOX2/gp91-phox antibody (ab80508), was added, and the mixture was incubated at 4 °C in the dark for 1 h. Cells were washed with PBS; then, secondary antibody Alexa Fluor® 647-conjugated goat anti-rabbit polyclonal antibody (ab181474) diluted 1:200 was added in all tubes except for p22-phox where a secondary FITC-conjugated goat anti-mouse IgG/IgM antibody (BD #555988) was added for 15 min. Stained cells were analyzed by flow cytometry Beckman Coulter FC500, gating on neutrophils based on forward and side scatter properties. Analysis of data was done using CXP Software version 2.2. Relevant isotypic control was used for each stained tube to evaluate for the non-specific antibody binding (Fig. 2). Residual protein expression was recorded for each patient.
Analysis of different components of NADPH enzyme by flow cytometry. Overlay of different NADPH components versus isotypic control. The neutrophil characterization was done by using forward and side scatter properties present in whole blood sample except in p67-phox-deficient patient, neutrophils were separated using Ficoll hypaque
Targeted Sanger Sequencing
Based on the flow cytometry results, targeted Sanger sequencing was performed for the candidate genes as described before [9] to confirm the results and detect the mutations.
Statistical Methods
Data were statistically described in terms of mean/standard deviation (SD) or frequencies (number of cases) and percentages when appropriate. Independent sample t test was used to compare between groups and one-way analysis of variance (ANOVA) test with post hoc multiple two-group comparisons when comparing more than two groups. Kruskal-Wallis test was used for comparing groups with non-parametric data. p values less than 0.05 was considered statistically significant. All statistical calculations were done using computer program SPSS (Chicago, IL, USA) version 15 for Microsoft windows.
Results
Demographic and Clinical Data
Twenty-eight CGD patients from 25 different kindred were enrolled in this study: 15 were males (53.5 %) and 13 were females (46.5 %). Three families had two affected members each.
Five male patients (17.9 %) from five different kindred (four non-consanguineous, one consanguineous) were considered X-CGD based on their mother’s DHR assay showing X-CGD carrier status pattern (bimodal neutrophil populations) and exclusive male affection.
Twenty-three patients (82.1 %) (13 females and 10 males) from 20 kindred were suspected as AR-CGD. All the AR-CGD patients came from consanguineous families. The median age at onset of symptoms was 8 months (range from 0.1 to 72 months), and diagnosis was made at a median age of 36 months (range from 6 to 180 months). However, in X-CGD, the age of first presentation and the age at diagnosis were at a younger age than in AR-CGD: 2 months (range from 0.5 to 13 months) and 18 months (range from 3 to 60 months), respectively. There was no statistically significant difference obtained when comparing the age at diagnosis among different subgroups (p = 0.058), yet there was a trend having the p47-phox-deficient patients diagnosed at older age.
Before the second month of life, all patients received BCG vaccine containing a live attenuated form of Mycobacterium bovis. BCG-itis, a severe lymphadenopathy following tuberculosis vaccination, was the first symptom of CGD in four (14.2 %) of the patients of this cohort: two with AR-CGD and two with X-CGD. They all required antimycobacterial therapy.
Autoimmune manifestations (in the form of inflammatory bowel disease, autoimmune anemia, uveitis) appeared more commonly in AR-CGD (seven patients); Five of the seven (71 %) were p47-phox. Pneumonia was the most common presenting feature in AR-CGD followed by recurrent abscesses, while in X-CGD, the most common presentations were recurrent abscesses, anemia, and lymphadenopathy. No correlations between different manifestations and the deficient proteins were obtained. A statistically significant difference (p = 0.049) was detected when comparing age of survival among different subgroups, seeing better outcome in p47-phox-deficient patients (Table 1).
Laboratory Results
Although two methods were used for separation of neutrophils for intracellular staining of NADPH components, they both gave the same results (Fig. 2). Assessment of the affected protein components by flow cytometry revealed deficiency in p22-phox in 13 patients (46.4 %) followed by p47-phox in 8 patients (28.6 %), gp91-phox in 5 patients (17.9 %), and p67-phox in 2 patients (7.1 %)
The DHR was impaired in all CGD cases; however, the mean SI was 1.36 ± 0.4 in X-CGD versus 4.4 ± 3.5, 2.9 ± 2, and 2.2 ± 0.53 in p47-phox, p67-phox, and p22-phox AR-CGD, respectively (p = 0.055). The median residual NADPH activity was 1 % in X-CGD while 17.4, 2.2, and 2.0 % in p47-phox, p67-phox, and p22-phox AR-CGD, respectively (p value = 0.057). The residual protein expression was statistically significant among the four groups (p value = 0.006) with higher values of residual NADPH and residual protein expression among the p47-phox deficiency subgroup (Table 2).
Mothers of five of the male patients showed the bimodal X-linked carrier pattern in DHR pointing to gp91-phox deficiency.
The protein defects detected were confirmed by targeted Sanger sequencing based on the flow cytometry results at the Laboratory for Genetic Diagnosis for Infectious Diseases at Human Genetic of Infectious Disease, Imagine Institute, France, and genetic analysis for three X-CGD patients was done at the Molecular Genetics Laboratory, CKTCH Brno, Czech Republic. Mutations detected matched the flow cytometry results.
All AR-CGD patients had homozygous mutations. In all the patients with p47-phox deficiency, the common mutation p.Tyr26Hisfr*26 was detected, while in patients with p22-phox deficiency, 11 out of 13 patients had a previously described mutation p.Val99Profs*90 and two patients had previously undescribed mutations: one with p.Tyr54fsin and the other with p.Gly128Aspfs*81. The gp91-phox and the p67-phox-deficient patients had different mutations (Table 2).
Discussion
Early diagnosis of CGD is important for better patient survival and care. Clues for suspicion include a suggestive history, severity and recurrence of infections, tissue abscesses, and granulomas. However, routine diagnostics shows great variability, so it is advisable to have all CGD patients analyzed at specialized laboratories with high experience. Furthermore, two independent blood samples and at least two different methods should always be used to establish a definite diagnosis of CGD [3].
The present study clarifies the importance of utilizing flow cytometry in analyzing the defective proteins implicated in CGD as a method for confirming the diagnosis as well as detecting the defective component. The NBT and the DHR tests have been considered the main tests used for evaluation of neutrophil respiratory burst. In spite that the NBT is not costly, the test is time-consuming, labor-intensive, subjective, and requiring technical skills [10].
The DHR test has then widely replaced the NBT in the diagnosis of CGD. It can be performed quickly using small volumes of anticoagulated blood. The interpretation of the DHR test results is less subjective, and the test is able to differentiate between X-linked CGD patients and carriers. Although the DHR test has become the standard method for diagnosis of CGD, the test has some limitations. Important criticism for this method in routine diagnostics is its low sensitivity to in vitro artifacts and neutropenia besides the fact that the neutrophils may be unevenly damaged due to storage, handling, or mailing [11]. The relatively short lifespan of neutrophils implicates that samples must arrive in the laboratory on the same day of collection which could certainly comprise a challenge for laboratories acting as tertiary referral centers. In addition, patients with current infections as well as inflammatory states and severe sepsis causing exhaustion of neutrophils’ metabolism are negative indicators for using DHR assay for CGD screening [10, 12]. Among the limitations as well is the false positivity of the test in patients with myeloperoxidase deficiency [13]. Although uncommon, AR-recessive CGD patients can have substantial residual oxidative burst activity, leading to challenge of the diagnosis of AR-CGD [8].
Immunoblot and flow cytometry can be used to infer the specific genotype in CGD. There may be genotype/phenotype correlations that predict outcomes and might help in genetic counseling as well as in the consideration of bone marrow transplantation [12].
In the present study, the flow cytometry was used for the analysis the NADPH components in the diagnosed CGD patients, and the revealed results were confirmed by targeted Sanger sequencing.
We used two techniques for intracellular staining of NADPH components in the first ten cases as described previously in the “Material and Methods” section; however, both techniques gave similar results. Thus, the study was continued by the use of whole blood samples in immune-staining as it is less laborious and easier to perform.
Based on the consanguinity, DHR results, and testing the mothers of male patients, 5 (17.9 %) were diagnosed as X-linked CGD while 23 (82.1 %) were diagnosed as AR-CGD. The X-linked form of the disease is responsible for more than two thirds of the worldwide reported cases [14, 15], while the AR-recessive accounts for about one third. Although AR-CGD has been described in several studies among countries around Egypt before [14, 16, 17], the higher number of AR-CGD reported in the present study may be attributed to the high consanguinity (84 %) among the studied cohort families. In contrast to other studies reporting the AR-CGD which concluded that p47-phox deficiency is the commonest cause of AR-CGD [18], our study showed that p22-phox deficiency is the commonest form among Egyptian CGD patients (46.4 %). In Africa and Middle East, different CGD genotypes were reported. Köker et al. [17] published a study on 89 Turkish patients revealing quite high percentage of gp91-phox deficiency (38.2 %). Other studies conducted in Jordon, Tunisia, and Morocco showed that p47-phox deficiency accounts for most of the cases of AR-CGD with much fewer number of p22-phox deficiency reported cases [8, 14, 16]. The reason for this finding is not clear, and a reason like a founder effect as reported by Kim et al. in a Korean study [19] may be likely. Also, high consanguinity and inbreeding historically reported in Egyptian population may be an underlying cause.
Among the X-linked CGD patients reported in the present study, the gp91-phox deficiency was associated with p22-phox deficiency as well. Similar to our data, Baba et al. [8] detected no gp91-phox and p22-phox in X-linked CGD patients, as expected because the expression of p22-phox is dependent on the presence of gp91-phox.
Kuhns et al. [20] concluded that CGD patients with nonsense, frameshift, and splicing affecting mutations in gp91-phox generally exhibit no expression of gp91-phox, while p22-phox expression was reduced by >95 % but still detectable. On the other hand, missense mutations in gp91-phox exhibited variable expression of gp91-phox with proportionally preserved expression of p22-phox.
Among the patients with p22-phox deficiency reported hereby, 53 % of the patients showed normal expression of gp91-phox. This is in contrast to Köker study 2013 [17] who found that all the patients with CYBA mutations had no expression of either gp91-phox or p22-phox protein in the leukocytes.
Also, in a study by Kannengiesser et al. [21] that included CGD patients from 80 kindred, they did not detect gp91-phox in p22-phox-deficient patients, although using polyclonal antibody against C terminus of gp91 with similar specificity to the one used in the present study.
Nevertheless, Porter et al. [22] clarified the presence of a 65-kD high-mannose glycoprotein precursor of gp9l even in the absence of p22-phox expression consistent with the synthesis, posttranslational modification, and transport of gp91-phox as far as the endoplasmic reticulum but with no subsequent modification in the Golgi. The completion of the posttranslational modification process of the β subunit of cytochrome b-245 is apparently dependent on the presence of the α subunit.
Also, in agreement with our finding, Teimourian et al. [23] found residual gp91-phox expression by western blot in three out of the eight p22-phox-deficient patients reported in his study from Iran.
Worth to be mentioned is that Köker et al. [24] reported some preserved NADPH oxidase activity in neutrophils from three patients despite the apparently complete absence of gp91-phox and p22-phox expression by western blot. However, authors explained their finding by the possibility of the presence of some mutated p22-phox protein that allowed some stabilization of the gp91-phox but yet not detectable by the monoclonal antibody they used.
Kim et al. [19] reported results in 12 CGD patients on Jeju Island showing in contrast to all previous reports a normal level of gp91-phox protein expression in patients with p22-phox deficiency. They claimed that the co-expression of gp91-phox and p22-phox was required to support the generation of oxygen radicals in a cell-free NADPH oxidase assay, implying that the association is essential for regulation of electron transfer in the redox cycle, but p22-phox may not be necessary for the expression of gp91-phox protein. Further studies are required to understand the expression of gp91-phox in p22-phox-deficient cases. However, all patients in their study had an identical homozygous single-base substitution of C to T in exon 1 (c.7C>T) of the CYBA gene which may not affect the p22-phox function regarding gp91-phox expression.
The expression of gp91-phox in few of the p22-phox-deficient patients using the flow cytometry may point to a more sensitive detection of the proteins using this technique in comparison with western blot or a role of certain environmental factors affecting gp91-phox expression.
Interestingly, all the patients with defects in NCF1 gene had the same mutation (p.Tyr26Hisfs*26) and originated from eastern parts of Egypt, while 11/13 patients with defects in CYBA gene had the same mutation (p.Val99Pro fs*90) and originated from western parts of Egypt. This may point to a founder effect of these mutations (Supplemental 1). In spite that all the p47-phox patients had the same mutation, variations in the residual NADPH activity and protein expression among those patients were observed. This variation in the residual activity was also reported by other studies and may reflect the variability in the protein expression that is under control of many factors [20, 25, 26].
Conclusion
As the BMT is the only curative treatment of CGD, a pressing need arises for a rapid, reliable, and cost-effective test for definitive diagnosis of the disease. In countries with limited resources and yet large number of CGD patients, the analysis of the defective proteins by flow cytometry provides an optimum solution for confirming the diagnosis, especially in laboratories that carry the DHR test and are already equipped with flow cytometry. This can help in targeted sequencing as a main step in prenatal diagnosis.
References
Suliaman F, Amra N, Sheikh S, Almuhsen S, Alsmadi O. Epidemiology of chronic granulomatous disease of childhood in Eastern Province, Saudi Arabia. Pediat asthma, Allergy immunol. 2009;22(1):21–6.
Roos D, De Boer M, Yavuz Koker M, Dekker J, Singh-Gupta V, Ahlin A, et al. Chronic granulomatous disease caused by mutations other than the common GT deletion in NCF1, the gene encoding the p47phox component of the phagocyte NADPH oxidase. Hum Mutat. 2006;27(12):1218–29.
Ben-Ari J, Wolach O, Gavrieli R, Wolach B. Chronic granulomatous disease: linking genetics to phenotypic expression. Expert Rev Anti Infect Ther. 2012;10(8):881–94.
Koker MY, Metin A, Özgür TT, De Boer M, Roos D. Prenatal diagnosis of chronic granulomatous disease in a male fetus. Iran J Allergy Asthma Immunol. 2009;8(1):57–61.
Rezvani Z, Mohammadzadeh I, Pourpak Z, Moin M, Teimourian S. CYBB gene mutation detection in an Iranian patient with chronic granulomatous disease. Iranian J aller, asthma Immunol. 2005;4(2):103–6.
Battersby AC, Cale CM, Goldblatt D, Gennery AR. Clinical manifestations of disease in X-linked carriers of chronic granulomatous disease. J Clin Immunol. 2013;33(8):1276–84.
Meshaal S, El Hawary R, Abd Elaziz D, Alkady R, Galal N, Boutros J, et al. Chronic granulomatous disease: review of a cohort of Egyptian patients. Allergol Immunopathol. 2015;43(3):279–85.
Yu G, Hong DK, Dionis KY, Rae J, Heyworth PG, Curnutte JT, et al. Focus on FOCIS: the continuing diagnostic challenge of autosomal recessive chronic granulomatous disease. Clin Immunol. 2008;128(2):117–26.
Baba LA, Ailal F, El Hafidi N, Hubeau M, Jabot-Hanin F, Benajiba N, et al. Chronic granulomatous disease in Morocco: genetic, immunological, and clinical features of 12 patients from 10 kindred. J Clin Immunol. 2014;34(4):452–8.
Dimitrova G, Bunkall C, Lim D, Kendrick C. Comparison of two methods for the diagnosis of chronic granulomatous disease – neutrophil oxidative burst measured by the nitro blue tetrazolium slide test versus the dihydrorhodamine 123 flow cytometric assay. N Z J Med Lab Sci. 2013;67:45–51.
Van Pelt LJ, Van Zwieten R, Weening RS, Roos D, Verhoeven J, Bolscher BG. Limitations on the use of dihydrorhodamine 123 for flow cytometric analysis of the neutrophil respiratory burst. J Immunol Methods. 1996;191(2):187–96.
Holland SM. Chronic Granulomatous Disease. Clinic Rev Allerg Immunol. 2010;38:3–10.
Mauch L, Lun A, O’Gorman MR, Harris JS, Schulze I, Zychlinsky A, et al. Chronic granulomatous disease (CGD) and complete myeloperoxidase deficiency both yield strongly reduced dihydrorhodamine 123 test signals but can be easily discerned in routine testing for CGD. Clin Chem. 2007;53:890–6.
Bakri FG, Martel C, Khuri-Bulos N, Mahafzah A, El-Khateeb MS, Al-Wahadneh AM, et al. First report of clinical, functional, and molecular investigation of chronic granulomatous disease in nine Jordanian families. J Clin Immunol. 2009;29:215–30.
Cross AR, Noak D, Rae J, Curnutte JT, PG H. Hematologically important mutations: the autosomal recessive forms of chronic granulomatous disease (first update). Blood Cells Mol Dis. 2000;26(5):561–5.
El Kares R, Barbouche MR, Elloumi-Zghal H, Bejaoui M, Chemli J, Mellouli F, et al. Genetics and mutational heterogeneity of autosomal recessive chronic granulomatous in Tunisia. J Hum Genet. 2006;51:887–95.
Koker MY, Camcioglu Y, Van Leeuwen K, Sebnem Kılıc S, Barlan I, Yılmaz M, et al. Clinical, functional, and genetic characterization of chronic granulomatous disease in 89 Turkish patients. J Allergy Clin Immunol. 2013;132(5):1156–63.
Kannengiesser C, Gérard B, El Benna J, Henri D, Kroviarski Y, Chollet-Martin S, et al. Molecular epidemiology of chronic granulomatous disease in a series of 80 kindreds: identification of 31 novel mutations. HUMAN MUTATION. 2008;29:E132–49.
Kim YM, Park JE, Kim JY, Lim HK, Nam JK, Cho M, et al. Genetic analysis of 10 unrelated Korean families with p22-phox-deficient chronic granulomatous disease: an unusually identical mutation of the CYBA gene on Jeju Island, Korea. J Korean Med Sci. 2009;24:1045–50.
Kuhns DB, Alvord WG, Heller T, Feld JJ, Pike KM, Marciano BE, et al. Residual NADPH oxidase and survival in chronic granulomatous disease. N Engl J Med. 2010;363:2600–10.
Kannengiesser C, Gérard B, El Benna J, Henri D, Kroviarski Y, Chollet-Martin S, Gougerot-Pocidalo M A, Elbim C and Grandchamp B. Molecular epidemiology of chronic granulomatous disease in a series of 80 kindreds: identification of 31 novel mutations. HUMAN MUTATION. 2008 #1019, 29:E132-E149.
Porter CD, Parkar MH, Verhoeven AJ, Levinsky RJ, Collins MK, Kinnon C. p22-phox-deficient chronic granulomatous disease: reconstitution by retrovirus-mediated expression and identification of a biosynthetic intermediate of gp91-phox. Blood. 1994;84:2767–75.
Teimourian S, Zomorodian E, Badalzadeh M, Pouya A, Kannengiesser C, Mansouri D, et al. Characterization of six novel mutations in CYBA: the gene causing autosomal recessive chronic granulomatous disease. Br J Haematol. 2008;141:848–51.
Koker MY, Van Leeuwen K, de Boer M, Elmeli FC, Metin A, Ozgur TT, et al. Six different CYBA mutations including three novel mutations in ten families from Turkey, resulting in autosomal recessive chronic granulomatous disease. Eur J Clin Invest. 2009;39(4):311–9.
Wolach B, Gavrieli R, de Boer M, Gottesman G, Ben-Ari J, Rottem M, et al. Chronic granulomatous disease in Israel: clinical, functional and molecular studies of 38 patients. Clin Immunol. 2008;129:103–14.
Manea S-A, Constantin A, Manda G, Sasson S, Manea A. Regulation of Nox enzymes expression in vascular pathophysiology: focusing on transcription factors and epigenetic mechanisms. Redox Biol. 2015;5:358–66.
Acknowledgments
This work is funded by Cairo University. We would like to thank the Molecular Genetics Laboratory, Centre for Cardiovascular Surgery and Transplantation, Brno, Czech Republic, for performing Sanger sequencing to detect the molecular mutations and The Laboratory of Human Genetics of Infectious Diseases which is supported by institutional grants from INSERM, University Paris Descartes, The Rockefeller University, and the St. Giles Foundation and grants from the French National Research Agency (ANR) under the “Investments for the Future” program (grant no. ANR-10-IAHU-01) and grant IFNGPHOX (no. ANR13-ISV3-0001-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors declare they have no conflict of interest.
Additional information
Rabab El Hawary and Safa Meshaal equally contributed to this work, Taghrid Gaafar and Aisha Elmarsafy share senior coauthorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(GIF 33 kb)
Rights and permissions
About this article
Cite this article
El Hawary, R., Meshaal, S., Deswarte, C. et al. Role of Flow Cytometry in the Diagnosis of Chronic Granulomatous Disease: the Egyptian Experience. J Clin Immunol 36, 610–618 (2016). https://doi.org/10.1007/s10875-016-0297-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-016-0297-y