Abstract
High levels of stress during pregnancy can have lasting effects on maternal and offspring health, which disproportionately impacts families facing financial strain, systemic racism, and other forms of social oppression. Developing ways to monitor daily life stress during pregnancy is important for reducing stress-related health disparities. We evaluated the feasibility and acceptability of using mobile health (mHealth) technology (i.e., wearable biosensors, smartphone-based ecological momentary assessment) to measure prenatal stress in daily life. Fifty pregnant women (67% receiving public assistance; 70% Black, 6% Multiracial, 24% White) completed 10 days of ambulatory assessment, in which they answered smartphone-based surveys six times a day and wore a chest-band device (movisens EcgMove4) to monitor their heart rate, heart rate variability, and activity level. Feasibility and acceptability were evaluated using behavioral meta-data and participant feedback. Findings supported the feasibility and acceptability of mHealth methods: Participants answered approximately 75% of the surveys per day and wore the device for approximately 10 hours per day. Perceived burden was low. Notably, participants with higher reported stressors and financial strain reported lower burden associated with the protocol than participants with fewer life stressors, highlighting the feasibility of mHealth technology for monitoring prenatal stress among pregnant populations living with higher levels of contextual stressors. Findings support the use of mHealth technology to measure prenatal stress in real-world, daily life settings, which shows promise for informing scalable, technology-assisted interventions that may help to reduce health disparities by enabling more accessible and comprehensive care during pregnancy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Exposure to life stressors and stress-related mental health problems during pregnancy are known risk factors for a wide range of negative offspring outcomes, ranging from adverse birth outcomes to risk for child psychopathology (Gelaye & Koenen, 2018; Glover, 2011; Tung et al., 2023). These factors disproportionately impact pregnant people of color and families living in under-resourced communities (Alhusen et al., 2016; Bloom et al., 2013; Robinson et al., 2016; Thayer & Kuzawa, 2015), who often experience unique stressors related to their experiences of marginalization (e.g., discrimination, structural challenges to accessing support and healthcare; Almeida, 2005; Bloom et al., 2013; Rosenthal et al., 2015). Exposure and response to daily psychosocial stressors during pregnancy may be a key pathway through which stress-related health disparities are perpetuated across generations (Entringer et al., 2015; Lefmann & Combs-Orme, 2014; Lu & Halfon, 2003). Indeed, life stress during pregnancy has been linked to heightened maternal symptoms of emotional distress and alterations in stress physiology (e.g., autonomic/neuroendocrine regulation; Dunkel Schetter, 2011; Latendresse, 2009; Sandman et al., 2012). These emotional and physiological health indicators during pregnancy, in turn, have direct implications for fetal development and birth outcomes (Glover, 2015; Kim et al., 2015). From a prevention science perspective, the pregnancy period represents a unique window of opportunity to address health inequities by identifying ways to buffer prenatal stress and interrupt the transmission of stress to the next generation (Gelaye & Koenen, 2018). To this end, there is a critical need to develop ways to accurately monitor prenatal stress in naturalistic settings, particularly for individuals facing daily, systemically rooted stressors during pregnancy.
To date, most prenatal stress studies have been conducted in the laboratory setting and have relied on retrospective questionnaires of life stress and/or single-assessment lab-based measures of stress physiology. Although experimental stress paradigms have many strengths, single responses evoked from a mild-moderate stressor (e.g., speech task) in a controlled setting may not represent patterns of stress regulation in daily life. In other words, it is unclear how well these measures generalize to the way pregnant people experience stress and emotions in the real-world context. Accumulating evidence shows that emotional distress and stress physiology vary significantly day-to-day depending on both stressful and positive experiences (Bernstein et al., 2018; Sliwinski et al., 2009; Zawadzki et al., 2019). For example, one study of pregnant women collected salivary cortisol samples across four days and then compared them to single timepoint measures collected in the lab; higher salivary cortisol collected in the real-world context predicted shorter offspring gestational age, whereas cortisol measured at a single timepoint in the lab setting was unrelated to offspring outcomes (Entringer et al., 2011). These preliminary data support the utility of investigating prenatal stress regulation in the context of daily real-world stressors. Furthermore, studies using intensive sampling methods in the real-world context are needed to better understand the impact of daily life experiences on day-to-day changes in emotional health and stress physiology during pregnancy.
Recent advances in mobile health (mHealth) technology, including smartphone applications (apps) and wearable biosensors, provide an opportunity to measure real-world changes in stress in near real-time. These cutting-edge methods are making significant advances in other fields of mental health (Lecomte et al., 2020; Luxton et al., 2011; Melia et al., 2020), yet relatively few studies have applied this technology to the study of prenatal stress (Collins et al., 2023; Gyselaers et al., 2019; Omowale et al., 2021). The ability to monitor prenatal stress in a more continuous fashion and with high ecological validity offers significant advantages to traditional lab-based approaches. For example, smartphone-based ecological momentary assessment (EMA) protocols often include multiple data collection points per day, reducing retrospective bias and improving the accuracy of measuring prenatal stress experiences in daily life (Smyth et al., 2017). The intensive longitudinal data collected from these methods also enable statistical modeling of more complex dynamic associations between day-to-day variability in social experiences and stress during pregnancy, which is important given the central role of social and environmental factors on pregnancy health (Runkle et al., 2019). Similarly, many wearable biosensing devices can now be synced to smartphone-based EMA apps to characterize the dynamic associations between psychosocial experiences and stress physiology during pregnancy, including changes in sympathetic and parasympathetic regulation of stress responses. Despite the promise of these methods, however, it is not yet clear how feasible it is to use these devices to monitor or investigate daily prenatal stress, particularly for pregnant individuals already facing high levels of contextual stressors.
Establishing the feasibility and acceptability of mHealth technology for measuring prenatal stress also has important clinical translational implications for reducing prenatal health disparities. The ability to monitor experiences of stress in real-time may help to inform the development of person-centered and technology-assisted interventions that can target specific daily experiences and behaviors to improve prenatal stress regulation. Indeed, national surveys indicate that 96% of young adults in the United States own a smartphone (Pew Research Center, 2021). Wearable biosensing technology is also rapidly becoming a common tool for personalized health management, with positive perceptions of its usefulness particularly when combined with smartphones or other mHealth tools (Materia & Smyth, 2021). Thus, mobile technology utilized to investigate prenatal stress regulation is also one of the most scalable and translatable platforms for the development of technology-assisted prenatal interventions delivered in daily life.
A few studies have surveyed pregnant patients and healthcare providers about their perceptions of mHealth technology. These studies suggest that the use of smartphone and wearable sensors to monitor health during pregnancy is desirable by pregnant individuals and their physicians (Runkle et al., 2019). One population-based study surveyed 507 women in the U.S. and found that 91% of women expecting to become pregnant in the next 5 years found wearable electrocardiogram (ECG) devices to be an acceptable way to increase monitoring of maternal and fetal health (Wakefield et al., 2023). Although this survey study did not directly assess the feasibility and acceptability of these mHealth tools, the results emphasize that there are generally positive attitudes towards the use and benefits of mHealth tools during pregnancy. Similarly, another survey study found that both clinicians and pregnant patients expressed openness in using wearables and health monitoring devices during pregnancy, particularly if the data are being monitored by a clinician and lead to tailored information (Li et al., 2021).
However, emerging research has also highlighted important considerations when using mHealth tools to monitor prenatal stress. A systematic review by Sakamoto et al. (2022) found mixed evidence on the effectiveness of mHealth interventions for improving psychosocial health outcomes like anxiety, stress, and depression among pregnant women. Other studies surveying clinicians and pregnant patients report that both groups expressed concerns about the convenience of using these tools, highlighting the importance of gathering data on the acceptability of using wearable biosensors in daily life settings (Li et al., 2021), including the amount of perceived burden that mHealth tools may add for participants already experiencing high levels of life stress. Additional factors such as technical issues, digital literacy, and cultural beliefs and norms may also influence engagement with mHealth tools (Tumuhimbise et al., 2020). Taken together, these findings emphasize the need to carefully consider contextual factors when implementing mHealth tools to measure prenatal stress, especially among families living in under-resourced communities who often face more frequent and persistent contextual stressors in daily life.
The Present Study
The goal of this study was to evaluate the feasibility and acceptability of using smartphone-based EMA and a wearable heart rate sensor to measure prenatal stress in daily life for a predominantly low-income sample of pregnant individuals recruited from an urban community. First, we hypothesized that the ambulatory protocol would demonstrate strong feasibility as evidenced by high levels of participant adherence and engagement (i.e., completing > 70% of EMA prompts and wearing the heart rate sensor for > 70% of the assessment days). Second, we hypothesized that the ambulatory protocol would be perceived as acceptable to participants as evidenced by quantitative ratings and qualitative feedback during an exit interview. Finally, we hypothesized that these methods would be suitable for assessing daily life experiences during pregnancy as evidenced by high perceived representativeness of the assessment period relative to participants’ daily lives during pregnancy. In addition, we explored potential predictors of these outcomes, including demographic factors (e.g., age, socioeconomic status), contextual factors (e.g., number of life stressors, work status), and pregnancy-related factors (e.g., trimester, pain and fatigue related to pregnancy). Given the lack of studies that have examined these factors in relation to the acceptability and feasibility of ambulatory assessment methods, we did not make any directional hypotheses for this final research aim.
Method
Participants
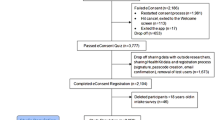
Data were drawn from the first 50 participants from an ongoing sub-study of pregnant individuals who were recruited from a larger longitudinal study of prenatal health and child development (ECHO-Pittsburgh Girls Study). Inclusion criteria included: ability to read English, willingness to answer surveys on a study smartphone multiple times a day for 10 days, and willingness to wear a biosensing device to monitor their heart rate during a 10-day ambulatory assessment period.
All study procedures were approved by the university’s institutional review board. We approached participants with a flyer about the sub-study during their first prenatal lab visit as part of the larger longitudinal study of prenatal health and child neurodevelopment (ECHO-Pittsburgh Girls Study), which included 3 total prenatal visits (approximately one per trimester). Those who were interested in participating in the new sub-study (74% of the original N = 68 approached) completed a phone screener for eligibility; all interested participants were eligible to participate. Interested and eligible participants completed written informed consent to participate in the sub-study during their second ECHO prenatal lab visit scheduled as part of the larger study. Due to the spacing of the visits for the larger longitudinal study, participants were all in their second or third trimester by the time they enrolled in the current sub-study. Participants who declined to participate did not differ from participants who enrolled on any demographic characteristics (i.e., age, race, income, public assistance status, marital status, number of children; all p’s > 0.05), with the exception that participants who declined to participate in the new sub-study were more likely to report that they were not currently working (χ2(1) = 4.77, p = .03).
Demographic characteristics of the final study sample are shown in Table 1. Participants ranged between 25 and 30 years of age and were in their second or third trimester of pregnancy at the time of assessment (range: 16–39 weeks pregnant). Most participants (70%) self-identified as Black or African American, with the remainder identifying as White or Multiracial. Regarding household composition, most participants had at least one child in the home (range between 0 and 4 children), and approximately half of the participants self-identified as single (vs. married or living with a partner). Most participants reported a total combined household income of less than $50,000 per year, including over half of the sample reporting less than $30,000 per year. Over half of the participants reported receiving some form of public assistance, including food stamps or support from the Supplemental Nutrition Assistance Program (SNAP), the Woman, Infants, and Children (WIC) Program, or cash assistance from government welfare. Most participants were full- or part-time employed; among those employed, over 20% reported currently working two jobs during their pregnancy. Types of occupation varied across industries, with about 61% reporting that they work in health care or social assistance. None of the participants reported that they were currently on leave (paid or unpaid).
Data collection procedures
Data collection included (1) a prenatal lab visit, (2) 10 days of ambulatory data collection using a study smartphone and heart rate sensor (described below), and (3) an exit interview. Participants received monetary compensation for completing each component of the study, as well as an additional monetary bonus for (1) responding to at least 70% of the surveys during the ambulatory assessment period and (2) wearing the charged sensor for more than half of the day for at least 7 out of the 10 days.
Lab visit: baseline measures and ambulatory assessment training
After providing consent during their lab visit, participants completed baseline questionnaires about demographic characteristics and pregnancy health as part of the larger longitudinal pregnancy study. The questionnaire included questions about age, race and ethnicity, income level, receipt of public assistance, number of children currently living in the home, marital status, work status, and type of employment. Participants also completed the Difficult Life Circumstances Scale (DLC; Barnard, 1988), a 28-item self-reported questionnaire developed to measure the number of current stressors in an individual’s life, with a focus on stressors that impact families living in under-resourced environments, such as financial problems, inadequate housing, exposure to violence, and interpersonal conflict. Each item is scored as 1 = Yes or 0 = No, and items are summed for a total score representing number of life stressors. Most participants (90%) were experiencing at least one life stressor, with 58% reporting two or more (range 0–10). Participants also completed questionnaires about their pregnancy status and health, including questions about the participant’s current gestational week, ratings of their current experiences of fatigue and pain on a 5-point Likert scale, and ratings on the impact of their pregnancy on everyday physical activities (e.g., walking, climbing stairs, carrying groceries). Most participants (75%) reported at least some diminishing of everyday physical activities from pregnancy, and participants typically reported experiencing mild-moderate fatigue and mild pain.
At the end of the baseline visit, participants completed a tutorial led by a research assistant on how to answer surveys on the study smartphone and how to wear and take care of the heart rate sensor. Prior research shows that participant training improves adherence in EMA studies (Wen et al., 2021). We also provided participants an information packet with the instructions to take home for reference. Participants were then asked to complete 10 days of ambulatory assessment, in which they answered surveys six times a day on a study smartphone and wore a chest band sensor for measuring heart rate, heart rate variability, and activity level (described below).
Ambulatory daily life assessment (10-days)
Ecological momentary assessment. Starting the day after the baseline lab visit, participants responded to EMA questions about their mood and daily life experiences through the movisensXS app (Movisens GmbH, Karlsruhe, Germany) on a study smartphone for 10 days. Participants received EMA prompts six times a day: (1) a “morning survey” after specified waketime (varying by weekday and weekends as indicated by participant), (2) four semi-random “mid-day surveys” approximately every 2–4 h apart, and (3) a “end-of-day survey” at a self-specified bedtime. Each EMA survey was estimated to take 3–5 min to complete and included items adapted from validated measures of perceived stress and mood (e.g., Perceived Stress Scale [Watson et al., 1988], Positive and Negative Affect Schedule [Cohen et al., 1983]) and daily stressful and positive events (e.g., Daily Inventory of Stressful Events [Almeida et al., 2002], Daily Uplifts Scale [Kanner et al., 1981], Pregnancy Experience Scale [DiPietro et al., 2008]). For all six surveys, participants were prompted by a scheduled “It’s time for your survey” notification from the movisensXS app. For the morning and end-of-day surveys, participants had the additional option to press a button in the app to initiate the survey before the specified wake or sleep time, which allowed participants to complete the morning and end-of-day surveys earlier than the programmed notification time (e.g., if waking up or planning to sleep earlier than usual). Upon receiving a notification from the movisensXS app that a survey was ready to complete, participants could either complete the survey immediately or press a button to “delay” the survey up to the end of the response window (see below). If the participant missed the notification, the movisensXS app would send a repeated alarm reminder after 90 s and another reminder after three minutes. Participants could delay the mid-day surveys up to 45 min after initial notification. The delay period allowed was longer for the morning and end-of-day surveys: up to 90 min for the morning survey and up to 5 h for the end-of-day survey, which allowed for additional flexibility in wake and sleep time.
Heart rate sensor. During the 10-day ambulatory assessment, participants were asked to wear a chest band device (movisens EcgMove4) during waking hours to collect data on their heart rate, heart rate variability, and activity level. The Movisens EcgMove4 is a research-grade wearable device that captures ECG using a fast sampling rate (1024 Hz) that is comparable to gold-standard ECG devices. The sensor is small (62.3 mm x 38.6 mm x 11.5 mm) and is used with an elastic dry electrode chest belt or two disposable adhesive electrodes. The device requires minimal charging (every 2–3 days) and holds up to two weeks of continuously collected ambulatory data. The device is connected to the movisensXS smartphone app via Bluetooth, which enables the heart rate data to be synced with the EMA data. Participants received automated alerts from the movisensXS app notifying them when the device is disconnected, low in battery, or having issues collecting valid HRV data, as well as troubleshooting tips to address these issues. The device uses Bluetooth to transmit the HRV data collection status every minute (“HrvIsLive”: 1 = collecting valid HRV data, 0 = no valid HRV data collected), allowing the investigative team to monitor HRV data collection quality in near real-time and to contact the participant to provide troubleshooting support as needed. The data collection status variable transmitted via Bluetooth from the device was used to quantify the number of hours and minutes per day that the participant wore the device while providing valid HRV data for the present feasibility and acceptability analyses.
Phone check-ins. To maximize engagement during the 10-day ambulatory assessment period, a research assistant provided a check-in text or call after the first day of the ambulatory assessment protocol during a time and preferred mode of contact selected by the participant. A follow-up check-in text was provided every 2–3 days during a time selected by the participant until completion of the 10-day protocol. During the check-in texts, the research assistant asked about any issues the participant may be experiencing and provided instructional feedback when needed or requested. During the Day 5 check-in, the research assistant provided feedback on the participant’s survey completion progress so far, including whether the participant was currently on track for the monetary bonus (for completing at least 70% of the surveys and wearing the sensor for more than half of the day for at least 7 out of 10 days). In between the scheduled check-ins, the study staff were available to answer questions by text, phone call, or through the movisensXS app messaging system.
Exit interview
After the 10-day period, participants came back to the lab to return the study phone and sensor and complete an exit interview to provide feedback on their experience in the study. The exit interview included quantitative and qualitative questions regarding the participant’s experience during the ambulatory portion of the study, including perceived burden and suggestions for improvement. Specifically, participants rated three quantitative questions to evaluate the acceptability of the protocol, including a general question about quality of experience (“How was your experience completing the Daily Life Assessment for this study on a 0–10 scale, from 0 = Very Negative, 10 = Very Positive?”), two questions about burden of protocol (“How much of a burden was it to [answer the daily surveys/wear the heart rate sensor] over the past 10 days?”; both rated on a 0–10 scale from 0 = Not at all Burdensome to 10 = Extremely Burdensome). To assess the suitability of using data from a 10-day ambulatory assessment to generalize to experiences during pregnancy, participants answered “How much do you think the past 10 days represents your daily life experiences since becoming pregnant?” (from 0 = Not at all Representative to 10 = Extremely Representative). Participants also responded to open-ended questions, including: (1) What did you LIKE about the experience? (2) What did you NOT LIKE about the experience? Any suggestions for areas to improve? (3) Any other comments for our research team?
Data analysis plan
To evaluate the protocol, we examined descriptive statistics of the behavioral meta-data variables for feasibility (i.e., percentage of EMA surveys completed and number of days and hours per day the heart rate sensor was worn), acceptability (i.e., ratings about the quality of the experience and the burden of the surveys and sensor), and suitability (i.e., ratings about the perceived representativeness of the protocol relative to daily life during pregnancy). We examined bivariate correlations to explore potential demographic and pregnancy-related correlates of feasibility, acceptability, and suitability variables.
Results
Feasibility
Participants answered an average of 74.54% of the total number of surveys sent to them (SD = 18.15, Range: 26.67–98.33). Survey completion decreased across the 10 days (F(9) = 2.31, p = .02), from an average of 82% surveys completed on Day 1 to 69% completed on Day 10 (Fig. 1). On average, participants wore the heart rate sensor for nearly 9 out of the 10 days (M = 8.86 days; Mdn = 10 days; SD = 2.14; range = 0–10 days). On days that they wore the sensor, participants wore it for an average of 10.49 h (SD = 2.68, range = 4.85–17.17). The average number of hours per day of sensor wearing did not change significantly across the 10-day ambulatory period (F(9) = 1.54, p = .16) (Fig. 2).
Table 2 shows the bivariate correlations between study variables. Survey completion rates and number of hours the participant wore the sensor per day were unrelated to income, receipt of public assistance, employment status, or self-reported life stressors. Some differences by household composition were observed: Participants living with children wore the heart rate sensor for more hours per day, and participants living with a partner (e.g., married, domestic partner) completed a greater percentage of the EMA surveys. Participants reporting greater pregnancy-related difficulties with physical activity tended to wear the sensor for fewer number of hours per day; however, pregnancy-related fatigue and pain were unrelated to survey completion rates or sensor wearing patterns.
Acceptability
Participants generally liked the experience and rated it positively (8.18 out of 10). Examples of participant comments include: “It was easy to coordinate into my daily life” and “The surveys were like short and it didn’t take too long to complete them. And then I liked how they ask if we were like experiencing any stress throughout the day and stuff like that. That was really helpful because memory can change.” On average, participants perceived the EMA surveys to be low in burden (2.57 out of 10), and the sensor to be relatively low in burden (3.39 out of 10). As expected, positive experience ratings were inversely correlated with perceived burden of EMA and burden of sensor (Table 2).
Income and life stress were significantly correlated with the acceptability of the protocol (Table 2). Specifically, income was inversely related to the overall quality of experience and positively correlated with perceived burden of the surveys and heart rate sensor. That is, lower income was related to lower perceived burden. Consistent with this pattern, participants reporting more life stressors (i.e., difficult life circumstances) reported lower perceived burden of the heart rate sensor. Similarly, participants with children perceived both the surveys and heart rate sensor to be lower in burden than participants without children.
Acceptability of the protocol was unrelated to participant age, week of pregnancy, or pregnancy-related fatigue and pain. However, participants who felt that pregnancy was restricting their normal physical activities reported higher perceived burden of wearing the heart rate sensor.
Representativeness
On average, participants felt that the 10 days of ambulatory assessment were relatively well representative of their daily life experiences since becoming pregnant (mean = 7.68 out of 10). The extent to which the sampling window was perceived as accurately capturing their daily life experiences since becoming pregnant was unrelated to age, week of pregnancy, household composition, income, employment status, or self-reported life stressors.
Discussion
Overall, findings from this study support the feasibility and acceptability of using smartphone-based EMA and wearable physiological monitors to measure daily prenatal stress responses in a predominantly low-income sample of pregnant individuals living in an urban setting. Consistent with hypotheses, the 10-day ambulatory protocol demonstrated strong feasibility as evidenced by high levels of participant engagement and adherence. Participants also perceived the protocol positively as evidenced by quantitative ratings and qualitative feedback during the exit interview, which supports the acceptability of using these methods to measure prenatal stress. Furthermore, these ambulatory methods appear suitable for measuring daily life experiences during pregnancy given that participants reported that their responses were thought to closely reflect their daily lives since becoming pregnant. Thus, our findings support the use of smartphone-based EMA and wearable physiological monitors to measure stress and health during pregnancy, particularly for pregnant individuals who are reporting high levels of contextual stress (e.g., financial strain, difficult life circumstances).
Notably, participants reporting more contextual stressors tended to rate the ambulatory protocol as less burdensome compared to participants with higher incomes and fewer difficult life circumstances. Similarly, participants who were caring for children in the home during pregnancy rated the protocol as less burdensome and wore the sensor for more hours per day compared to primiparous individuals. These findings were somewhat surprising: individuals who were living with multiple overlapping stressors appeared to perceive the study protocol as less invasive and burdensome on their life despite needing to balance the study protocol with a greater number of objective stressors in their daily life (e.g., childcare, multiple jobs, housing difficulties). It is possible that individuals who are experienced in managing multiple stressors perceive new responsibilities, such as completing an intensive 10-day ambulatory study protocol, as minimally arduous relative to the stress of their other life experiences, thus leading to lower ratings of perceived burden. Alternatively, perhaps individuals with more daily life stressors found the survey questions more relevant to their daily life experiences or experienced more benefits (e.g., increased insight about daily mood and stressors) from monitoring these experiences. More studies that examine predictors of perceived stress and burden may be needed to further elucidate this pattern of findings. Overall, these findings suggest that the use of mobile health technology and ambulatory sampling methods are not only feasible but perceived positively among communities that experience high levels of daily life stress. This is important to know when designing studies to investigate prenatal health disparities, as there may be assumptions that intensive longitudinal methods are too burdensome to use among lower-income and higher-stress samples, which can lead to the exclusion of these communities from such research.
Findings also suggest that data collected during the ambulatory sampling was relatively generalizable to daily life experiences during pregnancy, indicating that these methods are suitable for studying prenatal health. Participants generally rated their experiences during the 10-day assessment as well-representative of their experiences since becoming pregnant. The implications of these results are important given that most studies of prenatal stress rely on single timepoint measures of prenatal stress collected in the lab setting, which may have limited ecological validity. Indeed, there is emerging evidence that measures of prenatal stress (i.e., salivary cortisol) collected in the home using a daily life assessment protocol are better predictors of birth outcomes compared to measures collected during a single lab visit (Entringer et al., 2011). Building on the current findings, an important future direction is to evaluate the predictive utility of self-report and psychophysiological measures of prenatal stress collected using smartphone-based EMA and wearable biosensors.
Findings from the current study also have implications for the types of research questions that can be asked in studies of prenatal stress. Overall, there is a need to better understand how experiences such as stressors in daily life relate to physical and mental health during pregnancy. Use of EMA and mHealth devices expands the types of constructs that can be measured using single timepoint methods, improving the ability to measure fluctuations and changes in stressful experiences during pregnancy across days, weeks, and months. Survey studies indicate that pregnant people are interested in better understanding the impacts of these daily life experiences on pregnancy health, an area of research that is often undervalued by health care professionals despite the relevance of this work for psychosocial prenatal interventions (Runkle et al., 2019).
Establishing the feasibility and acceptability of mHealth tools for measuring experiences during pregnancy is an important step to informing person-centered and technology-assisted prenatal care. Advancing this knowledge is timely given that 96% of young adults now regularly use smartphones, and the number of health monitoring wearable devices are rapidly increasing (Pew Research Center, 2021). One of the strengths of mHealth technology is its potential to improve access to personalized prenatal care. For example, mHealth apps and wearables could help with promoting psychological and physical wellbeing during pregnancy by helping individuals gain insight into their daily stress and behavioral patterns and providing immediate feedback to clients that can supplement in-person visits to healthcare providers. For example in a survey study of 103 pregnant individuals from a rural health clinic, most participants (70%) indicated that they would be willing to change their health behaviors in response to personalized recommendations from a smartphone, which suggests that this technology is likely to be translatable to personalized interventions (Runkle et al., 2019). Of note, it was interesting that the smartphone-based EMA component of the study was seen as slightly less burdensome than the wearable biosensor, given that EMA requires more frequent activity (engaging in reporting) than the passive sensing of the device. It is possible these results are specific to the chest-band sensor device used in this study; follow up studies that use other types of wearables are needed to further assess the perceived burden of various biosensor devices for monitoring health and physiology during pregnancy.
The implications of this research are particularly relevant for pregnant people of color, who often experience higher levels of psychosocial stress during pregnancy including racism-based stressors that impact prenatal health (Giurgescu et al., 2016). Racial disparities in stress exposure during pregnancy are further compounded by unique barriers that pregnant people of color face in accessing safe, respectful, and culturally sensitive care in hospitals and other primary healthcare settings (Mehra et al., 2020; Silva et al., 2022). In particular, in the United States, Black women receive the lowest rates of prenatal services in the first trimester of pregnancy (Silva et al., 2022) and experience the highest rates of adverse birth outcomes (e.g., low birthweight, preterm birth) compared to other racial-ethnic groups (Vilda et al., 2019). Establishing the utility of mHealth technology for monitoring prenatal health among Black women and other marginalized populations may help to inform the development of tools for relevant, tailored prenatal care that is also accessible to individuals facing barriers to high-quality care in primary healthcare settings.
There are several methodological limitations that should be considered when interpreting the current findings. First, data were drawn from a relatively small sample, which may have limited the ability to investigate predictors or moderators of variability in the findings. Although participants who enrolled in the study did not differ from participants who declined the study on almost all demographic factors, the recruitment pool consisted of participants who had already agreed to participate in a prior research study, which may have introduced selection bias regarding positive perception of research studies. In addition, participants were recruited from a single urban city in the United States, with most participants identifying as Black or African American. Thus, findings may not generalize to other racial-ethnic groups or populations in other geographic regions. For example, a study that interviewed 40 women living in rural communities about preferences surrounding use of smartphones for behavior change found that women perceived the potential annoyances with constant phone notifications as a disadvantage of using smartphones for health behavior change (Materia et al., 2018). Given that phone usage patterns and norms may differ between rural vs. urban and suburban populations, more research is needed to examine the extent to which these findings generalize to other geographic regions. Finally, the current study involved frequent contact with participants via phone check-ins to maximize data yield; studies that do not involve this level of participant contact may result in lower levels of participant engagement.
In conclusion, findings from this study provide support for the feasibility and acceptability of using smartphone-based EMA and wearable physiological monitors to measure prenatal stress in real-world, daily life settings, particularly for pregnant people living in under-resourced communities. This line of work has high relevance to social, health, and policy issues regarding disparities in prenatal stress transmission, with potential to inform scalable, technology-assisted interventions that can be delivered in real-time during the pregnancy period.
References
Alhusen, J. L., Bower, K. M., Epstein, E., & Sharps, P. (2016). Racial discrimination and adverse birth outcomes: An integrative review. Journal of Midwifery & Women’s Health, 61(6), 707–720. https://doi.org/10.1111/jmwh.12490.
Almeida, D. M. (2005). Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science, 14(2), 64–68. https://doi.org/10.1111/j.0963-7214.2005.00336.x.
Almeida, D. M., Wethington, E., & Kessler, R. C. (2002). The daily inventory of stressful events: An interview-based approach for measuring daily stressors. Assessment, 9(1), 41–55. https://doi.org/10.1177/1073191102091006.
Barnard, K. (1988). Difficult life circumstances scale. University of Washington.
Bernstein, M. J., Zawadzki, M. J., Juth, V., Benfield, J. A., & Smyth, J. M. (2018). Social interactions in daily life: Within-person associations between momentary social experiences and psychological and physical health indicators. Journal of Social and Personal Relationships, 35(3), 372–394. https://doi.org/10.1177/0265407517691366.
Bloom, T., Glass, N., Curry, A., Hernandez, M., R., & Houck, G. (2013). Maternal stress exposures, reactions, and priorities for stress reduction among low-income urban women. Journal of Midwifery & Women’s Health, 58(2), 167–174. https://doi.org/10.1111/j.1542-2011.2012.00197.x.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 385–396. https://doi.org/10.2307/2136404.
Collins, T. E., Akselrod, S., Altymysheva, A., Nga, P. T. Q., Banatvala, N., & Berlina, D. (2023). The promise of digital health technologies for integrated care for maternal and child health and non-communicable diseases. BMJ, 381. https://doi.org/10.1136/bmj-2022-071074.
da Silva, P. H. A., Aiquoc, K. M., Silva Nunes, A. D., da, Medeiros, W. R., de Souza, T. A., Jerez-Roig, J., & Barbosa, I. R. (2022). Prevalence of access to prenatal care in the first trimester of pregnancy among black women compared to other races/ethnicities: A systematic review and meta-analysis. Public Health Reviews, 43, 1604400. https://doi.org/10.3389/phrs.2022.1604400.
DiPietro, J. A., Christensen, A. L., & Costigan, K. A. (2008). The pregnancy experience scale–brief version. Journal of Psychosomatic Obstetrics & Gynecology, 29(4), 262–267. https://doi.org/10.1080/01674820802546220.
Dunkel Schetter, C. (2011). Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology, 62(1), 531–558. https://doi.org/10.1146/annurev.psych.031809.130727.
Entringer, S., Buss, C., Andersen, J., Chicz-DeMet, A., & Wadhwa, P. D. (2011). Ecological momentary assessment of maternal cortisol profiles over a multiple-day period predict the length of human gestation. Psychosomatic Medicine, 73(6), 469–474. https://doi.org/10.1097/PSY.0b013e31821fbf9a.
Entringer, S., Buss, C., & Wadhwa, P. D. (2015). Prenatal stress, development, health and disease risk: A psychobiological perspective—2015 Curt Richter Award Paper. Psychoneuroendocrinology, 62, 366–375. https://doi.org/10.1016/j.psyneuen.2015.08.019.
Gelaye, B., & Koenen, K. C. (2018). The intergenerational impact of prenatal stress: Time to focus on prevention? Biological Psychiatry, 83(2), 92–93. https://doi.org/10.1016/j.biopsych.2017.11.004.
Giurgescu, C., Engeland, C. G., Templin, T. N., Zenk, S. N., Koenig, M. D., & Garfield, L. (2016). Racial discrimination predicts greater systemic inflammation in pregnant African American women. Applied Nursing Research, 32, 98–103. https://doi.org/10.1016/j.apnr.2016.06.008.
Glover, V. (2011). Annual Research Review: Prenatal stress and the origins of psychopathology: An evolutionary perspective. Journal of Child Psychology and Psychiatry, 52(4), 356–367. https://doi.org/10.1111/j.1469-7610.2011.02371.x.
Glover, V. (2015). Prenatal stress and its effects on the fetus and the child: Possible underlying biological mechanisms. Perinatal Programming of Neurodevelopment (pp. 269–283). Springer. https://doi.org/10.1007/978-1-4939-1372-5_13.
Gyselaers, W., Lanssens, D., Perry, H., & Khalil, A. (2019). Mobile health applications for prenatal assessment and monitoring. Current Pharmaceutical Design, 25(5), 615–623.
Kanner, A. D., Coyne, J. C., Schaefer, C., & Lazarus, R. S. (1981). Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. Journal of Behavioral Medicine, 4, 1–39. https://doi.org/10.1007/bf00844845.
Kim, D. R., Bale, T. L., & Epperson, C. N. (2015). Prenatal programming of mental illness: Current understanding of relationship and mechanisms. Current Psychiatry Reports, 17(2), 5. https://doi.org/10.1007/s11920-014-0546-9.
Latendresse, G. (2009). The interaction between chronic stress and pregnancy: Preterm birth from a biobehavioral perspective. Journal of Midwifery & Women’s Health, 54(1), 8–17. https://doi.org/10.1016/j.jmwh.2008.08.001.
Lecomte, T., Potvin, S., Corbière, M., Guay, S., Samson, C., Cloutier, B., Francoeur, A., Pennou, A., & Khazaal, Y. (2020). Mobile apps for mental health issues: Meta-review of meta-analyses. JMIR mHealth and uHealth, 8(5), e17458. https://doi.org/10.2196/17458.
Lefmann, T., & Combs-Orme, T. (2014). Prenatal stress, poverty, and child outcomes. Child and Adolescent Social Work Journal, 31(6), 577–590. https://doi.org/10.1007/s10560-014-0340-x.
Li, J., Silvera-Tawil, D., Varnfield, M., Hussain, M. S., & Math, V. (2021). Users’ perceptions toward mHealth technologies for health and well-being monitoring in pregnancy care: Qualitative interview study. JMIR Formative Research, 5(12), e28628. https://doi.org/10.2196/28628.
Lu, M. C., & Halfon, N. (2003). Racial and ethnic disparities in birth outcomes: A life-course perspective. Maternal and Child Health Journal, 7(1), 13–30. https://doi.org/10.1023/A:1022537516969.
Luxton, D. D., McCann, R. A., Bush, N. E., Mishkind, M. C., & Reger, G. M. (2011). mHealth for mental health: Integrating smartphone technology in behavioral healthcare. Professional Psychology: Research and Practice, 42(6), 505–512. https://doi.org/10.1037/a0024485.
Materia, F. T., Smyth, J. M., Heron, K. E., Hillemeier, M., Feinberg, M. E., Fonzi, P., & Downs, S., D (2018). Preconceptional health behavior change in women with overweight and obesity: Prototype for SMART strong healthy women intervention. mHealth, 4, 24. https://doi.org/10.21037/mhealth.2018.06.06.
Materia, F. T., & Smyth, J. M. (2021). Acceptability of intervention design factors in mHealth intervention research: Experimental factorial study. JMIR mHealth and uHealth, 9(7), e23303.
Mehra, R., Boyd, L. M., Magriples, U., Kershaw, T. S., Ickovics, J. R., & Keene, D. E. (2020). Black pregnant women get the most judgment: A qualitative study of the experiences of black women at the intersection of race, gender, and pregnancy. Women’s Health Issues, 30(6), 484–492. https://doi.org/10.1016/j.whi.2020.08.001.
Melia, R., Francis, K., Hickey, E., Bogue, J., Duggan, J., O’Sullivan, M., & Young, K. (2020). Mobile health technology interventions for suicide prevention: Systematic review. JMIR mHealth and uHealth, 8(1), e12516. https://doi.org/10.2196/12516.
Omowale, S. S., Casas, A., Lai, Y. H., Sanders, S. A., Hill, A. V., Wallace, M. L., & Mendez, D. D. (2021). Trends in stress throughout pregnancy and postpartum period during the COVID-19 pandemic: Longitudinal study using ecological momentary assessment and data from the Postpartum Mothers Mobile Study. JMIR Mental Health, 8(9), e30422. https://doi.org/10.2196/30422.
Pew Research Center (2021). Mobile Fact Sheet. Pew Research Center: Internet, Science & Tech. https://www.pewresearch.org/internet/fact-sheet/mobile/.
Robinson, A. M., Benzies, K. M., Cairns, S. L., Fung, T., & Tough, S. C. (2016). Who is distressed? A comparison of psychosocial stress in pregnancy across seven ethnicities. BMC Pregnancy and Childbirth, 16(1), 215. https://doi.org/10.1186/s12884-016-1015-8.
Rosenthal, L., Earnshaw, V. A., Lewis, T. T., Reid, A. E., Lewis, J. B., Stasko, E. C., Tobin, J. N., & Ickovics, J. R. (2015). Changes in experiences with discrimination across pregnancy and postpartum: Age differences and consequences for mental health. American Journal of Public Health, 105(4), 686–693. https://doi.org/10.2105/AJPH.2014.301906.
Runkle, J., Sugg, M., Boase, D., Galvin, S. L., & Coulson, C., C (2019). Use of wearable sensors for pregnancy health and environmental monitoring: Descriptive findings from the perspective of patients and providers. Digital Health, 5, 2055207619828220. https://doi.org/10.1177/2055207619828220.
Sakamoto, J. L., Carandang, R. R., Kharel, M., Shibanuma, A., Yarotskaya, E., Basargina, M., & Jimba, M. (2022). Effects of mHealth on the psychosocial health of pregnant women and mothers: A systematic review. British Medical Journal Open, 12(2), e056807. https://doi.org/10.1136/bmjopen-2021-056807.
Sandman, C. A., Davis, E. P., Buss, C., & Glynn, L. M. (2012). Exposure to prenatal psychobiological stress exerts programming influences on the mother and her fetus. Neuroendocrinology, 95(1), 7–21. https://doi.org/10.1159/000327017.
Sliwinski, M. J., Almeida, D. M., Smyth, J., & Stawski, R. S. (2009). Intraindividual change and variability in daily stress processes: Findings from two measurement-burst diary studies. Psychology and Aging, 24(4), 828–840. https://doi.org/10.1037/a0017925.
Smyth, J. M., Juth, V., Ma, J., & Sliwinski, M. (2017). A slice of life: Ecologically valid methods for research on social relationships and health across the life span. Social and Personality Psychology Compass, 11(10), e12356. https://doi.org/10.1111/spc3.12356.
Thayer, Z. M., & Kuzawa, C. W. (2015). Ethnic discrimination predicts poor self-rated health and cortisol in pregnancy: Insights from New Zealand. Social Science & Medicine (1982), 128, 36–42. https://doi.org/10.1016/j.socscimed.2015.01.003.
Tumuhimbise, W., Atukunda, E. C., Ayebaza, S., Katusiime, J., Mugyenyi, G., Pinkwart, N., & Musiimenta, A. (2020). Maternal health-related barriers and the potentials of mobile health technologies: Qualitative findings from a pilot randomized controlled trial in rural Southwestern Uganda. Journal of Family Medicine and Primary Care, 9(7), 3657–3662. https://doi.org/10.4103/jfmpc.jfmpc_281_20.
Tung, I., Hipwell, A. E., Grosse, P., Battaglia, L., Cannova, E., English, G., Quick, A. D., Llamas, B., Taylor, M., & Foust, J. E. (2023). Prenatal stress and externalizing behaviors in childhood and adolescence: A systematic review and meta-analysis. Psychological Bulletin. https://doi.org/10.1037/bul0000407. Advanced online publication.
Vilda, D., Wallace, M., Dyer, L., Harville, E., & Theall, K. (2019). Income inequality and racial disparities in pregnancy-related mortality in the US. SSM - Population Health, 9, 100477. https://doi.org/10.1016/j.ssmph.2019.100477.
Wakefield, C., Yao, L., Self, S., & Frasch, M. G. (2023). Wearable technology for health monitoring during pregnancy: An observational cross-sectional survey study. Archives of Gynecology and Obstetrics, 308(1), 73–78. https://doi.org/10.1007/s00404-022-06705-y.
Watson, D., Clark, L. A., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063. https://doi.org/10.1037/0022-3514.54.6.1063.
Wen, C. K. F., Junghaenel, D. U., Newman, D. B., Schneider, S., Mendez, M., Goldstein, S. E., Velasco, S., Smyth, J. M., & Stone, A. A. (2021). The effect of training on participant adherence with a reporting time frame for momentary subjective experiences in ecological momentary assessment: Cognitive interview study. JMIR Formative Research, 5(5), e28007. https://doi.org/10.2196/28007.
Zawadzki, M. J., Scott, S. B., Almeida, D. M., Lanza, S. T., Conroy, D. E., Sliwinski, M. J., Kim, J., Marcusson-Clavertz, D., Stawski, R. S., Green, P. M., Sciamanna, C. N., Johnson, J. A., & Smyth, J. M. (2019). Understanding stress reports in daily life: A coordinated analysis of factors associated with the frequency of reporting stress. Journal of Behavioral Medicine, 42(3), 545–560. https://doi.org/10.1007/s10865-018-00008-x.
Acknowledgements
Special thanks to the participants of the Pittsburgh Girls Study for their participation in this research and to our dedicated research team for their continued efforts.
Funding
This research was supported by the National Institute of Mental Health (K01MH123505) and the National Institute of Health Environmental influences on Child Health Outcomes (ECHO) Program (UH3OD023244).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analyses were performed by I.T. and U.B. The first draft of the manuscript was written by I.T.; all authors provided feedback on previous versions of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The authors have no conflicts of interests to disclose. The study was approved by the Institutional Review Boards (IRB) of California State University, Dominguez Hills and the University of Pittsburgh. Written informed consent was obtained from all participants prior to data collection.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tung, I., Balaji, U., Hipwell, A.E. et al. Feasibility and acceptability of measuring prenatal stress in daily life using smartphone-based ecological momentary assessment and wearable physiological monitors. J Behav Med 47, 635–646 (2024). https://doi.org/10.1007/s10865-024-00484-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-024-00484-4