Abstract
Previous reviews explored weight loss-induced metabolic changes in overweight and obese adults with type 2 diabetes (T2D) but did not report on the impact on patient-reported outcomes (PROs). This systematic review investigated the effect of weight loss interventions on weight loss and PROs in overweight and obese adults with T2D. We searched three electronic databases from inception to March 2018 for randomised controlled trials (RCTs) of weight loss interventions in overweight and obese (according to BMI) adults aged ≥ 18 years reporting changes in PROs from baseline to at least one follow-up assessment during or post-intervention. One reviewer screened abstracts, performed data extraction, and conducted the narrative synthesis, with 25% cross-checking by a second reviewer. We extracted data relating to sample characteristics, intervention and comparison conditions, weight loss, and change in PROs. We identified 540 papers of which 23 met eligibility reporting on 19 RCTs. Four types of interventions (diet, surgery, pharmacological, and multi-component lifestyle interventions) significantly reduced weight. Weight loss was consistently associated with improvements in sexual and physical function across all intervention types, with diet and multi-component lifestyle interventions producing more substantial improvements than surgical or pharmacological interventions. Findings for other PROs, such as HRQOL and depressive symptoms, were inconsistent across studies and intervention types. The four weight loss interventions can be prescribed to engender weight loss in overweight and obese adults with T2D, with multi-component lifestyle interventions generating substantial improvements in physical and sexual function, perhaps due to the potency of exercise in improving PROs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Obesity is a complex, chronic disease which has reached epidemic proportions, particularly in Western countries (Hruby & Hu, 2015). The body mass index (BMI) scale is used to determine whether an individual is underweight, of normal weight, overweight, or obese (Dey et al., 2013). The World Health Organisation estimates that the global prevalence of obesity (BMI ≥ 30 kg/m2) almost tripled between 1975 and 2016 (Organisation WH, 2019). Obesity is associated with a number of comorbid conditions, one of which is type 2 diabetes (T2D) (Oguma et al., 2005). Indeed, the risk of developing T2D is three and seven times higher in overweight and obese individuals, respectively, than individuals of normal weight (Abdullah et al., 2010). Moreover, up to 90% of adults with T2D are either overweight or obese (Organisation WH, 2019; Gatineau et al., 2014). Patients with both obesity and T2D experience additional complications over and above those of an obese person without T2D, including more metabolic problems, greater use of medication, increased prevalence of comorbidities, and reduced health-related quality of life (HRQOL) (Berk et al., 2018; Slagter et al., 2015).
Obesity and T2D are both associated with poorer psychological outcomes relative to the general population, such as higher depression (Mezuk et al., 2013; Luppino et al., 2010) and emotional distress (Perrin et al., 2017), and lower HRQOL (Abdullah et al., 2010; Kolotkin et al., 2003; Giuli et al., 2014). Sustained weight loss is the primary goal to restore and maintain physical and psychological health in overweight and obese adults with T2D (Samuel 2004; Billington et al., 2000). Common weight loss interventions include diet and/or exercise plans, pharmacological methods, and surgery (Cannon & Kumar, 2009). Several reviews investigated the impact of weight loss interventions on biological outcomes in overweight and obese adults with T2D (Franz et al., 2015; Norris et al., 2004). Results from these reviews suggest that achieving moderate weight loss (> 5%) is difficult, but such weight loss is needed to generate improvements in metabolic outcomes, such as blood pressure, lipid profiles, and HbA1c (Franz et al., 2015; Norris et al., 2004).
These reviews, however, did not assess the impact of changes in weight on patient-reported outcomes (PROs). A PRO is any health-related outcome that is assessed via self-report rather than via a medical practitioner, clinician, or researcher (U.S. Department of Health and Human Services Food and Drug Administration 2019). PROs offer valuable insight into a patient’s perception of the impact of a disease and treatment on their life, and are a hallmark of patient-centred care (Wu et al., 2013). As such, PROs represent an important class of clinical outcome in intervention design (FDA-NIH Biomarker Working Group, 2016). Several PROs are clinically relevant to our population of interest of overweight and obese adults with T2D. Psychological outcomes, such as depressive symptoms and anxiety, provide useful insight into the mental health of patients. Physiological outcomes, such as physical function and erectile function, are also extremely relevant to overweight and obese adults with T2D who might be hindered by weight or diabetes-related complications. Impaired functioning can negatively affect overall HRQOL (both generic and disease-specific). The present systematic review was exploratory, aiming to describe the effect of weight loss interventions on PROs in overweight and obese adults with T2D. Further, to provide a context in which to interpret PRO results, we also documented their effect on weight loss.
Methods
Search methods
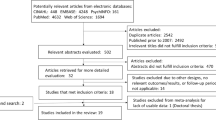
We searched three electronic databases for randomised controlled trials (RCTs) published from database inception to the time of our search: MEDLINE (1946–March 2018), Embase (1947–March 2018), and CENTRAL (1996–March 2018). The search comprised terms relating to weight (e.g., overweight and obese), diabetes, PROs (e.g., HRQOL, depression, and body image), weight change outcomes (e.g., weight loss), study design (e.g., clinical trial), and exclusions (e.g., adolescent, animal, and case study; see “Appendix 1”). The search was limited to peer-reviewed papers published in English. Lead authors of conference abstracts were searched to find full text articles. If the relevant full text was found, and it met the eligibility criteria, it was included in the review. Our systematic review of RCTs was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance.
Eligibility criteria
Studies were included if: (a) the trial design was a phase II, II, or IV RCT; (b) the sample was defined as overweight and/or obese adults (assessed using the BMI scale) with T2D; (c) weight loss was a study outcome; (d) longitudinal PRO data was reported, including baseline assessment and at least one assessment during or post-intervention; and (e) PROs were collected using a standardised and validated PRO instrument. Literature reviews, theoretical articles, and position papers were excluded. Studies were also excluded if weight loss or PRO data for the overweight and/or obese adult T2D sample was combined with data for other BMI groups (e.g., normal weight) (Chapman et al., 2005; Ma et al., 2008) or comorbid conditions (e.g., obstructive sleep apnoea or ischemic heart disease) (Shechter et al., 2014; Chung et al., 2011) without presenting subgroup results.
One reviewer (JM) screened titles and abstracts against the eligibility criteria. Full texts were obtained for papers considered relevant or where inclusion was uncertain. A second reviewer (CR) screened 25% of excluded papers, selected at random, and all obtained full texts. Both reviewers (JM and CR) reviewed the full texts of included articles against eligibility criteria. Queries regarding eligibility were resolved through discussion with a third reviewer (MK).
Data extraction and analysis
Standardised data items were extracted from each article, including: (a) RCT identification information; (b) sample characteristics; (c) intervention and comparison group description; (d) weight loss findings; (e) PROs assessed including which PRO instruments were used; (f) PRO findings; and (g) study limitations. Data extraction was performed by one reviewer (JM) and cross-checked against the original paper on a separate occasion. Meta-analysis was not feasible given the heterogeneity in weight loss interventions, time intervals between baseline and follow-up assessments, and PRO instruments across included studies. Instead, we used narrative synthesis to describe results for weight loss and change in PROs.
Quality assessment
The quality of included studies was appraised using the 2010 CONSORT checklist (37 items assessing the design and general reporting of RCTs) (Schulz et al., 2010) and the 2013 CONSORT-PRO Extension (14 items assessing the quality of PRO reporting of RCTs) (Calvert et al., 2013). Each quality item was scored by one reviewer (JM) as fully met (1), partially met (.5), or not met (0). We did not use study quality as a criterion for inclusion in this review.
Results
Of 540 papers identified, 23 reported on 19 RCTs and were included in this review (Fig. 1). Five papers reported data from the Look AHEAD trial (Foy et al., 2011; Rejeski et al., 2015; Stewart et al., 2011; Williamson et al., 2009; Wing et al., 2010). The 19 RCTs included 9271 overweight and obese adults with T2D, of which 58% were female. Sixteen trials (84.2%) were conducted in Western or European countries, two (10.5%) were based in Asian countries (China and India) (Woo et al., 2007; Palikhe et al., 2014), and one (5.3%) was conducted in multiple countries (Davies et al., 2015). Nine trials (47.4%) were multi-centre. Table 1 summarises the 23 papers that included overweight and/or obese adults with T2D; “Appendix 2” provides further detail of the PRO(s) assessed and full names of the abbreviated PRO measures used. Of the interventions in the 19 RCTs, five (26.3%) used dietary modification alone to elicit weight loss, four (21.1%) used surgical procedures, three (15.8%) used pharmacological agents, and seven (36.8%) used multi-component lifestyle interventions (six of them included a physical activity component), sometimes in combination with diet modification, pharmacological agents, and/or counselling.
Quality appraisal
Figures 2 and 3 show the percentage of studies meeting (either fully or partially) and not meeting each quality criterion for general RCT reporting and PRO-specific reporting, respectively. Overall, the quality of general RCT reporting was good. However, less than 50% of the included studies identified their study as a RCT in the title and failed to provide thorough descriptions of results for all primary and secondary outcomes, including lack of reporting of effect sizes and confidence intervals. Studies often did not explicitly document important aspects of the randomisation process, including how random allocation was generated and implemented. The quality of PRO reporting was suboptimal. Authors generally failed to: identify whether the PRO was a primary or secondary outcome in the abstract, provide a priori hypotheses for PRO instruments, and provide PRO-specific limitations and implications for clinical practice in the discussion. There was little association within studies between the quality of general RCT reporting (total scores ranged from 49 to 86%) and PRO-specific reporting (total scores ranged from 18 to 82%) (Spearman correlation coefficient = .05; scatterplot shown in Fig. 4).
Scatterplot showing the general RCT reporting and PRO-specific reporting scores for each article (number indicates citation number of the article in the manuscript and Table 1 for cross-reference)
Dietary interventions
Five studies comprising 1120 participants used diet to induce weight loss (Davis et al., 2012; Lean et al., 2017; Brinkworth et al., 2016; Khoo et al., 2011; Holland-Carter et al., 2017). Two of these were high quality and reported greater weight loss with dietary interventions compared to a non-active control of standard diabetes care at 12 months; Lean et al. (2017) used an evidence-based weight management programme (Counterweight-Plus) [37 (n = 306)], while Holland-Carter et al. (2017) used a modified weight watchers program [40 (n = 563)]. Both studies used generic HRQOL instruments. Lean et al. (2017) reported better HRQOL (EQ-5D instrument) with the Counterweight-Plus nutrition programme compared to standard diabetes care at 12 months (Lean et al., 2017). In contrast, Holland-Carter et al. (2017) found no significant differences in HRQOL (SF-36 instrument) between a modified weight watchers diet and standard diabetes care at 12 months (Holland-Carter et al., 2017), but they did find some differences with disease-specific PROs. Their results from the Impact of Weight on Quality of Life-Lite (IWQOL-Lite) (Holland-Carter et al., 2017) instrument indicated better obesity-specific HRQOL, specifically physical function, sex life, and work domains, with the modified weight watchers program compared to standard diabetes care at 12 months (Holland-Carter et al., 2017), but no differences between groups for the self-esteem and public distress domains of the IWQOL-Lite (Holland-Carter et al., 2017). They also found greater reductions in diabetes-related emotional distress with the modified weight watchers diet compared to standard diabetes care at 6 and 12 months, as measured by the Diabetes Distress Scale total score and all four subscales (emotional burden, physician-related stress, regimen-related distress, and interpersonal distress) (Holland-Carter et al., 2017). However, they found no significant differences in depressive symptoms (Patient Health Questionnaire-9) between groups at 6 and 12 months (Holland-Carter et al., 2017).
Two moderate quality studies found similar weight loss between low-carbohydrate and high-carbohydrate diets at 12 months [36 (n = 105), 38 (n = 115)]. Both assessed disease-specific HRQOL using the Diabetes-39 instrument and found no significant differences in all five dimensions of the Diabetes-39 (anxiety and worry, diabetes control, energy and mobility, social burden, and sexual functioning) between low-carbohydrate and high-carbohydrate diets at 12 months (Davis et al., 2012; Brinkworth et al., 2016). Brinkworth et al. (2016) also assessed emotional distress (Problem Areas in Diabetes instrument), depressive symptoms (Beck Depression Inventory-II), anxiety (Spielberger State Anxiety Inventory), and global mood (Profile of Mood States instrument), but found no significant differences in these PROs between low-carbohydrate and high-carbohydrate diets at 6 and 12 months (Brinkworth et al., 2016).
The fifth dietary intervention study of moderate quality found that a meal replacement-based low-calorie diet produced greater weight loss than a high-protein diet at 8 weeks [39 (n = 31)]. The only PRO assessed in this study was erectile function using an abridged International Index of Erectile Function-5 questionnaire; no significant differences were found between low-calorie and high-protein diets at 8 weeks (Khoo et al., 2011).
Surgical interventions
Four studies reporting on 233 participants that underwent surgical weight loss procedures found that most weight loss occurred within the first 3 months post-surgery (Palikhe et al., 2014; Ding et al., 2015; Halperin et al., 2014; Murphy et al., 2018). Three of these studies compared surgery with medical management (Palikhe et al., 2014; Ding et al., 2015; Halperin et al., 2014). Palikhe et al. (2014) reported greater weight loss with laparoscopic sleeve gastrectomy (a procedure which uses a stapling device to reduce the size of the stomach and therefore the amount of food needed to reach satiety) compared to intensive medical treatment consisting of diet intervention, exenatide, and metformin supplementation, at 6 and 12 months [34 (n = 31)]. They reported significant within-group improvements in six domains of the SF-36 instrument (physical functioning, physical role functioning, emotional role functioning, vitality, social functioning, and general health) with laparoscopic sleeve gastrectomy at 6 months, but failed to report between-group differences with the non-surgical medical management control group (Palikhe et al., 2014). This study was low quality. In a comparative effectiveness trial, Halperin et al. (2014) reported no significant differences in weight loss and worse HRQOL (SF-36 instrument) at 3 months but greater weight loss at 12 months with Roux-en-Y gastric bypass surgery (a procedure which separates the stomach into dual portions and connects the upper portion to the small intestine, reducing nutrient absorption) compared to a 12-week ‘Why WAIT’ medical management program, consisting of a hypocaloric diet, 300 min of weekly exercise, weekly medication adjustments, cognitive-behavioural therapy, and group education [42 (n = 43); moderate quality study]. The EQ-5D instrument indicated comparable HRQOL at 3 months between groups (Halperin et al., 2014). Similarly, Ding et al. (2015) reported greater weight loss with laparoscopic adjustable gastric band surgery (a procedure which places an inflatable band around the upper portion of the stomach, which can be adjusted to change the size of the stomach) compared to the 12-week ‘Why WAIT’ medical management program at 12 months [41 (n = 45)] but found no significant differences in generic HRQOL (SF-36 and EQ-5D instrument) between groups at 3 months (Ding et al., 2015). Both studies reported no significant differences in generic HRQOL between surgery and medical management at 12 months (Ding et al., 2015; Halperin et al., 2014). Obesity-specific HRQOL (IWQOL-Lite instrument total score) did not differ between surgical intervention and medical management at 3 months; however, results at 12 months were inconsistent between the studies (Ding et al., 2015; Halperin et al., 2014). Halperin et al. (2014) reported better obesity-related HRQOL with Roux-en-Y gastric bypass surgery relative to medical management at 12 months (Halperin et al., 2014), while Ding et al. (2015) found no significant differences in obesity-related HRQOL between laparoscopic adjustable gastric band surgery and medical management at 12 months (Ding et al., 2015). Both studies found no significant differences in diabetes-specific emotional distress (Problem Areas in Diabetes instrument) between surgery and medical management at 3 and 12 months (Ding et al., 2015; Halperin et al., 2014). Perceived barriers to being physically active (Barriers to Being Physically Active instrument) were also comparable between surgery and medical management at 3 months in both studies but differed at 12 months (Ding et al., 2015; Halperin et al., 2014). Halperin et al. (2014) found that physical activity barriers were lower following Roux-en-Y gastric bypass surgery compared with medical management (Halperin et al., 2014), while Ding et al. (2015) found no significant differences in physical activity barriers between laparoscopic adjustable gastric band surgery and medical management (Ding et al., 2015).
In a recent high quality comparative effectiveness trial, Murphy et al. (2018) compared two surgical weight loss procedures and reported greater weight loss with silastic-ring laparoscopic Roux-en-Y gastric bypass surgery (similar to standard Roux-en-Y gastric bypass surgery with the addition of a silastic ring) compared to laparoscopic sleeve gastrectomy surgery at 12 months [43 (n = 114)]. However, this difference in weight loss did not translate into improvements in PROs as generic HRQOL (SF-36 instrument total and domain scores), and anxiety and depression (Hospital Anxiety and Depression Scale) were comparable between the two surgical procedures at 12 months (Murphy et al., 2018).
Pharmacological interventions
Three studies comprising 1705 participants used pharmacological methods to elicit weight loss (Davies et al., 2015; Kipnes et al., 2010; Kaukua et al., 2004). One of these studies reported greater weight loss with 15 mg sibutramine daily compared to a relatively non-active placebo control at 12 months [45 (n = 236); moderate quality study]. However, no significant differences were found across eight HRQOL domains (SF-36 instrument: physical functioning, physical role functioning, emotional role functioning, vitality, mental health, social functioning, bodily pain, and general health) between sibutramine and placebo at 3, 6, 9, and 12 months (Kaukua et al., 2004).
Kipnes et al. (2010) reported more weight loss with 0.5 mg, 1 mg, and 2 mg taranabant daily compared to a relatively non-active placebo control at 9 and 12 months [44 (n = 623)]. No significant differences in global mood (Profile of Mood States Brief Form instrument) were found between the three doses of taranabant (0.5 mg, 1 mg, and 2 mg daily) and placebo at 12 months; however, the anger-hostility and depression-dejection scales of the Profile of Mood States Brief Form instrument deteriorated with 2 mg taranabant daily compared to placebo at 12 months (Kipnes et al., 2010). Further, 0.5 mg and 1 mg taranabant daily, but not 2 mg taranabant daily, produced higher confusion-bewilderment scores compared to placebo at 12 months (Kipnes et al., 2010). Although Kipnes et al. (2010) reported assessing generic HRQOL (SF-36 instrument) and obesity-specific HRQOL (IWQOL-Lite instrument) in the methods, corresponding results were not reported in-text and the overall PRO reporting quality was low (Kipnes et al., 2010).
Davies et al. (2015) reported more frequent weight loss (> 5% or > 10% body weight) with 1.8 mg and 3.0 mg liraglutide daily compared to a relatively non-active placebo control at 56 weeks [35 (n = 846); high quality study]. Additional pairwise comparisons indicated that 3.0 mg liraglutide daily produced significantly more > 5% and > 10% weight loss than 1.8 mg liraglutide daily (Davies et al., 2015). Satisfaction with diabetes treatment (Diabetes Treatment Satisfaction Questionnaire) and obesity-specific HRQOL (IWQOL-Lite total and physical function domain scores) was greater in 3.0 mg liraglutide daily, but not 1.8 mg liraglutide daily, group compared to placebo at 56 weeks (Davies et al., 2015). There were no significant differences between either of the liraglutide doses and placebo for the self-esteem, sexual life, public distress, or work domains at 56 weeks (Davies et al., 2015).
Multi-component lifestyle interventions (including a physical activity component)
Six trials (10 papers) reporting on 6055 participants used a combination of weight loss intervention methods to elicit weight loss, often in the form of lifestyle interventions. In the Look AHEAD trial (n = 5145), participants assigned to intensive lifestyle intervention (a combination of moderate-intensity physical activity, diet modification via replacing meals with liquid shakes and meal bars, weight loss medication, and individual and group counselling) lost more weight than those assigned to general diabetes support and education (standard diabetes education sessions focused on exercise, nutrition, and social support) at 12 (Foy et al., 2011; Stewart et al., 2011; Williamson et al., 2009; Wing et al., 2010) and 96 months (Rejeski et al., 2015), based on moderate to high quality evidence. Williamson et al. (2009) reported greater improvement in physical function (SF-36 instrument) with intensive lifestyle intervention compared to diabetes support and education at 12 months [31 (n = 5145)]. Physical function (SF-36 instrument) was also higher with intensive lifestyle intervention compared to diabetes support and education at 12 and 96 months; an effect which was more pronounced in older participants [29 (n = 4998)]. In contrast, there were no significant group differences in the mental component summary of the SF-36 instrument at 12 months (Williamson et al., 2009). Williamson et al. (2009) also reported larger reductions in depressive symptoms (Beck Depression Inventory-II) with intensive lifestyle intervention compared to diabetes support and education at 12 months (Williamson et al., 2009). Stewart et al. (2011) found that perceived current body size, but not perceived ideal body size (Body Morph Assessment Version 2.0) was greater in the intensive lifestyle intervention compared to diabetes support and education at 12 months [30 (n = 157); moderate quality study]. Perceptions of acceptable body size were higher in the diabetes support and education group compared to the intensive lifestyle intervention group at 12 months among both men and women (Stewart et al., 2011). Wing et al. (2010) reported better erectile function (International Index of Erectile Function-5) with intensive lifestyle intervention compared to diabetes support and education at 12 months among older men [32 (n = 372); moderate quality study]. In a subset of the Look AHEAD sample with knee pain, Foy et al. (2011) reported reduced pain and improved physical function related to knee pain and discomfort (modified Western Ontario and McMaster Universities Osteoarthritis Index) with intensive lifestyle intervention compared to diabetes support and education at 12 months [28 (n = 2203); high quality study]. Self-reported knee stiffness did not differ between the groups at 12 months (Foy et al., 2011).
Two studies used exercise as a primary component of a 16-week multi-component weight loss program (Mensberg et al., 2017; Wycherley et al., 2014). Wycherley et al. (2014) reported greater weight loss with an energy-restricted diet plus resistance training exercise program compared to an energy-restricted diet alone at 16 weeks [47 (n = 106); moderate quality study]. However, there were no significant group differences in diabetes-specific HRQOL (Diabetes-39 instrument total score, energy and mobility, diabetes control, anxiety and worry, social burden, and sexual functioning domain scores) or diabetes-related emotional distress (Problem Areas in Diabetes instrument total score) at 16 weeks (Wycherley et al., 2014). The Mensberg et al. (2017) study found no significant differences in weight loss or generic HRQOL (SF-36 instrument total score) between exercise (spin classes and resistance training) plus liraglutide relative to exercise alone at 16 weeks [46 (n = 34); low quality study].
Moncrieft et al. (2016) reported no significant differences in weight loss between lifestyle intervention (17 structured sessions focusing on exercise and diet modification, combined with cognitive-behavioural and social learning treatment approaches) and standard diabetes care (received a short educational booklet on diabetes management) at 12 months in patients with significant depressive symptoms (Beck Depression Inventory-II total score ≥ 11) [48 (n = 111); high quality study]. Despite the absence of group differences in weight loss, depressive symptoms reduced more with intensive lifestyle intervention compared to standard diabetes care at 12 months (Moncrieft et al., 2016).
Two studies used a combination of pharmacological agents and lifestyle intervention to elicit weight loss (Woo et al., 2007; O’Neil et al., 2012). In Woo et al. (2007) participants received 360 mg Orlistat daily for 6 months and were then randomised to 6 months of lifestyle intervention (eucaloric meal plan, exercise program, and peer group support) or a relatively non-active control [33 (n = 55)]. In this low quality study, participants assigned to the lifestyle intervention group lost significantly more weight and had better generic HRQOL (SF-36 instrument total score, Chinese Version) than participants assigned to the non-intervention control group at 12 months (Woo et al., 2007). However, there were no significant group differences in obesity-related HRQOL (Obesity-Related Well-Being 97) at 12 months (Woo et al., 2007). O’Neil et al. (2012) reported greater weight loss with lorcaserin (10 mg or 20 mg daily) plus lifestyle intervention (specific advice about exercise, calorie restriction, food choices, and behaviour modification techniques) relative to lifestyle intervention alone at 12 months [49 (n = 604)]. This moderate quality study found better obesity-related HRQOL (IWQOL-Lite instrument total score) with 10 mg lorcaserin daily, but not 20 mg lorcaserin daily, plus lifestyle intervention compared to lifestyle intervention alone at 12 months (O’Neil et al., 2012). There were no significant differences in depressive symptoms (Beck Depression Inventory-II) between the two doses of lorcaserin (10 mg and 20 mg daily) plus lifestyle intervention and lifestyle intervention alone at 1, 6, or 12 months (O’Neil et al., 2012).
Multi-component lifestyle interventions (no physical activity component)
Berk et al. (2018) reported similar weight loss with standard diabetes care (semi-annual consultations with a diabetes nurse) plus 17 group cognitive-behavioural therapy sessions compared to standard diabetes care alone at 24 months [7 (n = 158)]. However, participants in this moderate quality study who received standard diabetes care plus group cognitive-behavioural therapy reported better HRQOL (EQ-5D instrument) at 24 months than those who received diabetes care alone (Berk et al., 2018). There were no significant group differences in other PROs, including anxiety and depression (Hospital Anxiety and Depression Scale), self-esteem (Rosenberg Self-Esteem Scale), fatigue (Checklist Individual Strength instrument), eating concern, weight concern, and shape concern (Eating Disorder Examination Questionnaire) at 24 months (Berk et al., 2018).
Discussion
Synthesis of results and clinical implications
This systematic review investigated PROs associated with weight loss interventions in overweight and obese adults with T2D, and to provide a context within which to interpret PRO results, it also documented the effectiveness of such interventions in terms of weight loss. Weight loss in overweight and obese T2D has many benefits including improved insulin sensitivity, cardiac function, and cholesterol. However, weight loss does not consistently improve HRQOL and physical and psychosocial function. It may be that weight loss is just one component of treatment for overweight and obese adults with T2D.
Evidence from 23 RCTs revealed that multicomponent interventions tend to improve physical function but not psychological/emotional function unless a psychosocial component was included. Changes in PROs were reported in the absence of weight loss following multi-component interventions focused on diet and exercise combined with cognitive-behavioural and social learning techniques, suggesting improvements in PROs are more likely if an intervention targets symptomology and functioning. Combined exercise and diet interventions led to greater weight loss than diet alone, but did not consistently translate to improved diabetes-specific HRQOL or emotional distress. These interventions targeted weight loss and not HRQOL impairment due to having a chronic condition like T2D. As is becoming increasingly common in clinical practice, a holistic approach to the treatment and management of obesity and T2D is needed.
Surgery produced the fastest and most substantial weight loss, particularly in the first 3 months post-surgery, but did not reliably correspond to improvements in HRQOL, emotional distress or barriers to being physically active. This is not surprising given extensive surgery will likely impair functioning and HRQOL in the short-term during recovery from surgery. Diet interventions produced greater weight loss relative to non-active controls and improved HRQOL but not self-esteem and depression. No difference was found in weight loss and PROs between low- and high-carbohydrate diets, suggesting both are equally effective. Weight loss from medication did not translate to improved HRQOL or mood, and it appears that mood changes may be a possible side-effect of some pharmacological interventions. However, these findings came from low quality studies so should be interpreted with caution. Overall, diet, surgical or pharmacological interventions are effective for weight loss but do not consistently improve PROs. No study reported that participants who underwent dietary, surgical, pharmacological or multi-component lifestyle interventions gained weight from baseline to post-intervention.
Building upon findings from existing reviews examining weight-loss induced changes in biological outcomes in overweight and obese adults with T2D (Franz et al., 2015; Norris et al., 2004), we found that: (a) PROs were typically secondary or tertiary outcomes, and that the reporting quality of these outcomes was low and likely prone to publication bias (i.e., negative findings unlikely reported); and (b) several of the studies did not find any significant differences/improvements in PROs. These factors combined suggest that particularly dietary, surgical and pharmacological interventions have little impact on important PROs in this population. These interventions were designed for weight loss and do not target any underlying problems or reasons for weight gain (or maintaining weight loss) and therefore unlikely to directly affect PROs. The results from this review suggest that weight loss itself does not translate to improved PROs; rather, interventions targeting multiple components, for example, weight loss, lifestyle, and psychosocial well-being had the greatest impact on improving PROs. Interventions targeting a specific PRO such as psychological function may be most effective at improving that specific outcome. Exercise, a well-established intervention to improve self-reported physical and psychological health in diverse populations (Sweegers et al., 2018; Schuch et al., 2016; Cai et al., 2017; Jadczak et al., 2018) was included in most of the multi-component lifestyle interventions, which may partially explain the physical function benefits observed in these interventions. Considering the benefits of counselling for mental health outcomes in primary care patients (Bower et al., 2011), it is also plausible that counselling contributed to improvements in PROs from multi-component lifestyle interventions comprising counselling. While the exact causative pathway between obesity, weight loss, intervention type and PROs is inconclusive, interventions that target weight loss as well as symptomology and functioning have the greatest effect on improving PROs.
There were limited evidence that surgical and pharmacological interventions benefit PROs more than medical management or placebo control. Few PROs worsened from baseline to follow-up assessments post-intervention, indicating that a scheduled weight loss program should not produce harmful changes in patient HRQOL. However, as one study found worsened mood from specific doses of medication, clinicians should consider potential side-effects when recommending pharmacological interventions (Kipnes et al., 2010). Overall, the evidence indicates that clinicians should favour dietary and multi-component lifestyle intervention methods if the principal therapeutic aim is to maximise PROs, such as HRQOL.
Comment on reporting of PRO data
Overall, there was no association between general RCT reporting and PRO-specific reporting, and the reporting of PRO data across the included studies was relatively poor. There were several instances where authors mentioned a specific PRO measure in the methods section but failed to report data for that PRO measure in the results (e.g., self-image, SF-36 and IWQOL-Lite questionnaires) (Woo et al., 2007; Kipnes et al., 2010). Similarly, some authors listed a range of PRO assessment time-points but failed to report data for all time-points assessed (Berk et al., 2018; O’Neil et al., 2012). Other authors presented some PRO results through a general statement of significance but failed to report corresponding numerical data (e.g., means, standard deviations and confidence intervals), either in-text or tabular (Brinkworth et al., 2016; Kaukua et al., 2004; Mensberg et al., 2017). Without these statistics, such PRO findings cannot be included in future meta-analyses, increasing the risk of publication bias as most of these non-numerical results were not statistically significant.
Further, it was often ambiguous what stage of the clinical trial the authors collected baseline PROs. Some papers explicitly stated that baseline was pre-intervention (e.g., before randomisation or at randomisation) (Berk et al., 2018; Foy et al., 2011; Woo et al., 2007; Khoo et al., 2011; Murphy et al., 2018; Wycherley et al., 2014), although most failed to state baseline relative to the intervention. In one paper, the authors assessed weight loss-specific HRQOL at baseline and depression at randomisation without clarifying the temporal difference between them (O’Neil et al., 2012). Only one study reported minimal clinically important differences in PRO data (Davies et al., 2015). Future studies should also endeavour to report minimal clinically important differences in PRO data wherever possible (in addition to statistical significance) to facilitate translation of RCT results from research into clinical practice.
In instances where PRO data reporting was adequate, authors: (a) utilised tables showing mean PRO scores at baseline and at all subsequent PRO assessment time-points, with a measure of dispersion (e.g., confidence intervals) and effect size, and (b) provided mean differences and labelled p-values for both within- and between-group differences. Suboptimal reporting may be improved with adherence to reporting guidelines, such as CONSORT-PRO (Calvert et al., 2013). Transparency in study design, conduct, and reporting of results is needed to ensure scientific rigour and aid in interpretation of study results.
Limitations
Our review had several limitations. Firstly, our review was not pre-registered. Secondly, our search did not extend to grey literature or non-electronic databases, and we did not contact authors for unpublished PRO data from previous weight loss intervention trials. It is also possible that additional databases (e.g., PsycINFO) may have contained other relevant studies that were excluded from our review. Thirdly, there was large variation in the sample sizes of the included studies, ranging from 31 (Khoo et al., 2011) to 5045 (Look AHEAD trial) (Williamson et al., 2009). Rather than excluding studies with small sample sizes, we have explicitly stated sample sizes, noting that small studies may lack reliability and generalisability and may be more susceptible to outliers than larger studies with more participants (IntHout et al., 2015). Our narrative synthesis approach was necessary due to heterogeneity of the weight loss interventions and PRO assessment intervals. Although we organised weight loss interventions into subgroups (e.g., diet, surgery, multicomponent), we acknowledge that, within these groups, there are still differences in intervention dose and design. Finally, we used BMI as a criterion for study eligibility as few studies report excess adiposity. Several meta-analyses have demonstrated that the BMI scale has low-to-moderate sensitivity to detect excess adiposity in both adults and children (Javed et al., 2015; Okorodudu et al., 2010). As such, future reviews could assess body composition using alternative measures, such as abdominal adiposity or body fat percentage.
Conclusion and future directions
Diet, surgery, pharmacological and multi-component lifestyle interventions are effective at reducing weight in overweight and obese adults with T2D. However, weight loss does not consistently improve PROs. When weight loss is the sole treatment objective, clinicians can prescribe individualised weight loss treatment programs suited to the patients’ preference to maximise adherence. When improvement in PROs is a principal therapeutic objective in addition to weight loss, clinicians should consider multi-component lifestyle interventions that target weight loss as well as symptomology and functioning. Few studies compared weight loss and PRO data between different intervention methods, limiting the scope for appraisal of one weight loss intervention relative to another in terms of benefits and harms to patients. Given the suboptimal reporting of PRO data across the included studies, future authors are encouraged to adhere to standardised reporting guidelines, such as CONSORT-PRO (Calvert et al., 2013).
References
Abdullah, A., Peeters, A., de Courten, M., & Stoelwinder, J. (2010). The magnitude of association between overweight and obesity and the risk of diabetes: A meta-analysis of prospective cohort studies. Diabetes Research and Clinical Practice, 89(3), 309–319.
Berk, K. A., Buijks, H. I. M., Verhoeven, A. J. M., Mulder, M. T., Ozcan, B., van’t Spijker, A., et al. (2018). Group cognitive behavioural therapy and weight regain after diet in type 2 diabetes: Results from the randomised controlled POWER trial. Diabetologia, 61(4), 790–799.
Billington, C., Epstein, L., Goodwin, N., Hill, J., Pi-Sunyer, F., Rolls, B., et al. (2000). Overweight, obesity, and health risk. Archives of Internal Medicine, 160(7), 898–904.
Bower, P., Knowles, S., Coventry, P. A., & Rowland, N. (2011). Counselling for mental health and psychosocial problems in primary care. Cochrane Database of Systematic Reviews, 9, Cd001025.
Brinkworth, G. D., Luscombe-Marsh, N. D., Thompson, C. H., Noakes, M., Buckley, J. D., Wittert, G., et al. (2016). Long-term effects of very low-carbohydrate and high-carbohydrate weight-loss diets on psychological health in obese adults with type 2 diabetes: Randomized controlled trial. Journal of Internal Medicine, 280(4), 388–397.
Cai, H., Li, G., Zhang, P., Xu, D., & Chen, L. (2017). Effect of exercise on the quality of life in type 2 diabetes mellitus: A systematic review. Quality of Life Research, 26(3), 515–530.
Calvert, M., Blazeby, J., Altman, D. G., Revicki, D. A., Moher, D., & Brundage, M. D. (2013). Reporting of patient-reported outcomes in randomized trials: The CONSORT PRO extension. JAMA, 309(8), 814–822.
Cannon, C. P., & Kumar, A. (2009). Treatment of overweight and obesity: Lifestyle, pharmacologic, and surgical options. Clinical Cornerstone, 9(4), 55–68.
Chapman, I., Parker, B., Doran, S., Feinle-Bisset, C., Wishart, J., Strobel, S., et al. (2005). Effect of pramlintide on satiety and food intake in obese subjects and subjects with type 2 diabetes. Diabetologia, 48(5), 838–848.
Chung, S. C., Hlatky, M. A., Stone, R. A., Rana, J. S., Escobedo, J., Rogers, W. J., et al. (2011). Body mass index and health status in the Bypass Angioplasty Revascularization Investigation 2 Diabetes Trial (BARI 2D). American Heart Journal, 162(1), 184–192.
Davies, M. J., Bergenstal, R., Bode, B., Kushner, R. F., Lewin, A., Skjoth, T. V., et al. (2015). Efficacy of liraglutide for weight loss among patients with type 2 diabetes: The SCALE diabetes randomized clinical trial. JAMA, 314(7), 687–699.
Davis, N. J., Tomuta, N., Isasi, C. R., Leung, V., & Wylie-Rosett, J. (2012). Diabetes-specific quality of life after a low-carbohydrate and low-fat dietary intervention. Diabetes Educator, 38(2), 250–255.
Dey, M., Gmel, G., & Mohler-Kuo, M. (2013). Body mass index and health-related quality of life among young Swiss men. BMC Public Health, 13, 1028.
Ding, S. A., Simonson, D. C., Wewalka, M., Halperin, F., Foster, K., Goebel-Fabbri, A., et al. (2015). Adjustable gastric band surgery or medical management in patients with type 2 diabetes: A randomized clinical trial. The Journal of Clinical Endocrinology and Metabolism, 100(7), 2546–2556.
FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and other Tools) Resource. Silver Spring, MD: Food and Drug Administration (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK326791/.
Foy, C. G., Lewis, C. E., Hairston, K. G., Miller, G. D., Lang, W., Jakicic, J. M., et al. (2011). Intensive lifestyle intervention improves physical function among obese adults with knee pain: Findings from the look AHEAD trial. Obesity, 19(1), 83–93.
Franz, M. J., Boucher, J. L., Rutten-Ramos, S., & VanWormer, J. J. (2015). Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: A systematic review and meta-analysis of randomized clinical trials. Journal of the Academy of Nutrition and Dietetics., 115(9), 1447–1463.
Gatineau, M., Hancock, C., Holman, N., Outhwaite, H., Oldridge, L., Christie, A., et al. (2014). Adult obesity and type 2 diabetes. Oxford: Public Health England.
Giuli, C., Papa, R., Bevilacqua, R., Felici, E., Gagliardi, C., Marcellini, F., et al. (2014). Correlates of perceived health related quality of life in obese, overweight and normal weight older adults: An observational study. BMC Public Health, 14(1), 35.
Halperin, F., Ding, S. A., Simonson, D. C., Panosian, J., Goebel-Fabbri, A., Wewalka, M., et al. (2014). Roux-en-Y gastric bypass surgery or lifestyle with intensive medical management in patients with type 2 diabetes: Feasibility and 1-year results of a randomized clinical trial. JAMA Surgery., 149(7), 716–726.
Holland-Carter, L., Tuerk, P. W., Wadden, T. A., Fujioka, K. N., Becker, L. E., Miller-Kovach, K., et al. (2017). Impact on psychosocial outcomes of a nationally available weight management program tailored for individuals with type 2 diabetes: Results of a randomized controlled trial. Journal of Diabetes and Its Complications, 31(5), 891–897.
Hruby, A., & Hu, F. (2015). The epidemiology of obesity: A big picture. Pharmacoeconomics, 33(7), 673–689.
IntHout, J., Ioannidis, J. P. A., Borm, G. F., & Goeman, J. J. (2015). Small studies are more heterogeneous than large ones: A meta-meta-analysis. Journal of Clinical Epidemiology, 68(8), 860–869.
Jadczak, A. D., Makwana, N., Luscombe-Marsh, N., Visvanathan, R., & Schultz, T. J. (2018). Effectiveness of exercise interventions on physical function in community-dwelling frail older people: An umbrella review of systematic reviews. JBI Database of Systematic Reviews and Implementation Reports, 16(3), 752–775.
Javed, A., Jumean, M., Murad, M. H., Okorodudu, D., Kumar, S., Somers, V. K., et al. (2015). Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: A systematic review and meta-analysis. Pediatric Obesity., 10(3), 234–244.
Kaukua, J. K., Pekkarinen, T. A., & Rissanen, A. M. (2004). Health-related quality of life in a randomised placebo-controlled trial of sibutramine in obese patients with type II diabetes. International Journal of Obesity, 28(4), 600–605.
Khoo, J., Piantadosi, C., Duncan, R., Worthley, S. G., Jenkins, A., Noakes, M., et al. (2011). Comparing effects of a low-energy diet and a high-protein low-fat diet on sexual and endothelial function, urinary tract symptoms, and inflammation in obese diabetic men. Journal of Sexual Medicine., 8(10), 2868–2875.
Kipnes, M. S., Hollander, P., Fujioka, K., Gantz, I., Seck, T., Erondu, N., et al. (2010). A one-year study to assess the safety and efficacy of the CB1R inverse agonist taranabant in overweight and obese patients with type 2 diabetes. Diabetes, Obesity & Metabolism, 12(6), 517–531.
Kolotkin, R. L., Crosby, R. D., & Williams, G. R. (2003). Assessing weight-related quality of life in obese persons with type 2 diabetes. Diabetes Research and Clinical Practice, 61(2), 125–132.
Lean, M. E. J., Leslie, W. S., Barnes, A. C., Brosnahan, N., Thom, G., McCombie, L., et al. (2017). Primary care-led weight management for remission of type 2 diabetes (DiRECT): An open-label, cluster-randomised trial. Lancet, 391(10120), 541–555.
Luppino, F. S., de Wit, L. M., Bouvy, P. F., et al. (2010). Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry, 67(3), 220–229.
Ma, Y., Olendzki, B. C., Merriam, P. A., Chiriboga, D. E., Culver, A. L., Li, W., et al. (2008). A randomized clinical trial comparing low-glycemic index versus ADA dietary education among individuals with type 2 diabetes. Nutrition, 24(1), 45–56.
Mensberg, P., Nyby, S., Jorgensen, P. G., Storgaard, H., Jensen, M. T., Sivertsen, J., et al. (2017). Near-normalization of glycaemic control with glucagon-like peptide-1 receptor agonist treatment combined with exercise in patients with type 2 diabetes. Diabetes, Obesity & Metabolism, 19(2), 172–180.
Mezuk, B., Chaikiat, Å., Li, X., Sundquist, J., Kendler, K. S., & Sundquist, K. (2013). Depression, neighborhood deprivation and risk of type 2 diabetes. Health & Place, 23, 63–69.
Moncrieft, A. E., Llabre, M. M., McCalla, J. R., Gutt, M., Mendez, A. J., Gellman, M. D., et al. (2016). Effects of a multicomponent life-style intervention on weight, glycemic control, depressive symptoms, and renal function in low-income, minority patients with type 2 diabetes: Results of the community approach to lifestyle modification for diabetes randomized controlled trial. Psychosomatic Medicine, 78(7), 851–860.
Murphy, R., Clarke, M. G., Evennett, N. J., John Robinson, S., Lee Humphreys, M., Hammodat, H., et al. (2018). Laparoscopic sleeve gastrectomy versus banded roux-en-Y gastric bypass for diabetes and obesity: A prospective randomised double-blind trial. Obesity Surgery, 28(2), 293–302.
Norris, S. L., Zhang, X., Avenell, A., Gregg, E., Bowman, B., Serdula, M., et al. (2004). Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: A meta-analysis. American Journal of Medicine, 117(10), 762–774.
Oguma, Y., Sesso, H., Paffenbarger, R., & Lee, I.-M. (2005). Weight change and risk of developing type 2 diabetes. Obesity Research, 13(5), 945–951.
Okorodudu, D. O., Jumean, M. F., Montori, V. M., Romero-Corral, A., Somers, V. K., Erwin, P. J., et al. (2010). Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. International Journal of Obesity, 34(5), 791–799.
O’Neil, P. M., Smith, S. R., Weissman, N. J., Fidler, M. C., Sanchez, M., Zhang, J., et al. (2012). Randomized placebo-controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: The BLOOM-DM study. Obesity., 20(7), 1426–1436.
Organisation WH. Obesity and overweight: World Health Organisation. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Palikhe, G., Gupta, R., Behera, B. N., Sachdeva, N., Gangadhar, P., & Bhansali, A. (2014). Efficacy of laparoscopic sleeve gastrectomy and intensive medical management in obese patients with type 2 diabetes mellitus. Obesity Surgery, 24(4), 529–535.
Perrin, N. E., Davies, M. J., Robertson, N., Snoek, F. J., & Khunti, K. (2017). The prevalence of diabetes-specific emotional distress in people with type 2 diabetes: A systematic review and meta-analysis. Diabetic Medicine, 34(11), 1508–1520.
Rejeski, W. J., Bray, G. A., Chen, S. H., Clark, J. M., Evans, M., Hill, J. O., et al. (2015). Aging and physical function in type 2 diabetes: 8 years of an intensive lifestyle intervention. The Journals of Gerontology A: Biological Sciences and Medical Sciences, 70(3), 345–353.
Samuel, K. (2004). Advances in the long-term treatment of obesity. Obesity Research, 12(S12), 149S–150S.
Schuch, F. B., Vancampfort, D., Richards, J., Rosenbaum, S., Ward, P. B., & Stubbs, B. (2016). Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. Journal of Psychiatric Research, 77, 42–51.
Schulz, K. F., Altman, D. G., & Moher, D. (2010). CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ, 340, c332.
Shechter, A., St-Onge, M. P., Kuna, S. T., Zammit, G., RoyChoudhury, A., Newman, A. B., et al. (2014). Sleep architecture following a weight loss intervention in overweight and obese patients with obstructive sleep apnea and type 2 diabetes: Relationship to apnea-hypopnea index. Journal of Clinical Sleep Medicine, 10(11), 1205–1211.
Slagter, S. N., van Vliet-Ostaptchouk, J. V., van Beek, A. P., Keers, J. C., Lutgers, H. L., van der Klauw, M. M., et al. (2015). Health-related quality of life in relation to obesity grade, type 2 diabetes, metabolic syndrome and inflammation. PLoS ONE, 10(10), e0140599.
Stewart, T. M., Bachand, A. R., Han, H., Ryan, D. H., Bray, G. A., & Williamson, D. A. (2011). Body image changes associated with participation in an intensive lifestyle weight loss intervention. Obesity, 19(6), 1290–1295.
Sweegers, M. G., Altenburg, T. M., Chinapaw, M. J., Kalter, J., Verdonck-de Leeuw, I. M., Courneya, K. S., et al. (2018). Which exercise prescriptions improve quality of life and physical function in patients with cancer during and following treatment? A systematic review and meta-analysis of randomised controlled trials. British Journal of Sports Medicine, 52(8), 505–513.
U.S. Department of Health and Human Services Food and Drug Administration. (2009). Guidance for industry patient-reported outcome measures: Use in medical product development to support labeling claims [43]. Available from: https://www.fda.gov/media/77832/download.
Williamson, D. A., Rejeski, J., Lang, W., Van Dorsten, B., Fabricatore, A. N., & Toledo, K. (2009). Impact of a weight management program on health-related quality of life in overweight adults with type 2 diabetes. Archives of Internal Medicine, 169(2), 163–171.
Wing, R. R., Rosen, R. C., Fava, J. L., Bahnson, J., Brancati, F., Gendrano, I. I. N. C., et al. (2010). Effects of weight loss intervention on erectile function in older men with type 2 diabetes in the Look AHEAD Trial. Journal of Sexual Medicine, 7(1), 156–165.
Woo, J., Sea, M. M. M., Tong, P., Ko, G. T. C., Lee, Z., Chan, J., et al. (2007). Effectiveness of a lifestyle modification programme in weight maintenance in obese subjects after cessation of treatment with Orlistat. Journal of Evaluation in Clinical Practice, 13(6), 853–859.
Wu, A. W., Kharrazi, H., Boulware, L. E., & Snyder, C. F. (2013). Measure once, cut twice—Adding patient-reported outcome measures to the electronic health record for comparative effectiveness research. Journal of Clinical Epidemiology, 66(8, Supplement), S12–S20.
Wycherley, T. P., Clifton, P. M., Noakes, M., & Brinkworth, G. D. (2014). Weight loss on a structured hypocaloric diet with or without exercise improves emotional distress and quality of life in overweight and obese patients with type 2 diabetes. Journal of Diabetes Investigation, 5(1), 94–98.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jordan Martenstyn, Madeleine King, and Claudia Rutherford state that she or he does not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Search strategy terms
Weight
-
1.
Obesity.ti,ab,mp
-
2.
Obese.ti,ab
-
3.
BMI.ti,ab
-
4.
(body mass index).ti,ab
-
5.
Overweight.ti,ab
-
6.
Or/1–5
Diabetes
-
7.
Diabetes.ti,ab,mp
-
8.
Diabetic.ti,ab
-
9.
Or/7–8
PROs
-
10.
(patient reported outcome* or PRO or PROM).ti,ab
-
11.
((quality adj1 life) or QOL or HRQOL or HRQL or HQL or HQOL).ti,ab
-
12.
pain.ti,ab
-
13.
sleep. ti,ab
-
14.
distress.ti,ab
-
15.
depression.ti,ab
-
16.
anxiety.ti,ab
-
17.
(physical function*).ti,ab
-
18.
Physical activit*.ti,ab
-
19.
Social activit*.ti,ab
-
20.
Daily activit*.ti,ab
-
21.
Social function*.ti,ab
-
22.
Isolation.ti,ab
-
23.
(body image).ti,ab
-
24.
sexual*.ab,ti
-
25.
(fatigue or tired*).ab,ti
-
26.
(appetite or satiety or satiate*).ab,ti
-
27.
or/10–26
Weight change outcomes
-
28.
(weight loss).ab,ti
-
29.
(weight reduction*).ab,ti
-
30.
(weight chang*).ab,ti
-
31.
(weight loss intervention*).ab,ti
-
32.
(weight loss program*).ab,ti
-
33.
Or/28–32
Trial design
-
34.
(clinical trial*).sh,ab,ti
-
35.
(randomi$ed controlled trial or controlled clinical trial).pt
-
36.
(randomi$ed or randomly).ab
-
37.
or/34–36
Exclusions terms
-
38.
p$ediatric.ti,ab
-
39.
(children or child or infant).ti,ab
-
40.
Childhood.ti,ab
-
41.
Youth.ti,ab
-
42.
Adolescent*.ti,ab
-
43.
animal*.mp,ti,ab
-
44.
(mouse or rat or mice).ti,ab
-
45.
(review adj3 (record* or image*)).ab
-
46.
incidence.ti,ab
-
47.
prevalence.ti,ab
-
48.
case study.ti,ab
-
49.
(qualitative or (patient interview*)).ti,ab
-
50.
(longitudinal cohort stud*).ab,ti
-
51.
(prospective cohort stud*).ab,ti
-
52.
(prospective stud*).ab,ti
-
53.
(prospective trial).ti,ab
-
54.
(cross-sectional stud*).ti,ab
-
55.
“in vivo”.mp
-
56.
“in vitro”.mp
-
57.
or/38–56
-
58.
6 and 9 and 27 and 33 and 37
-
59.
58 not 57
Appendix 2: PRO measure abbreviations presented in order of appearance in Table 1
PRO measure abbreviation | PRO measure full name | Construct assessed |
|---|---|---|
POMS | Profile of Mood States | Mood |
BDI-II | Beck Depression Inventory II | Depression |
STAI | State-Trait Anxiety Inventory | Anxiety |
D-39 | Diabetes-39 | Diabetes-specific quality of life |
PAID | Problem Areas in Diabetes | Diabetes-related distress |
SF-36 | 36-Item Short Form Survey | Health status and health-related quality of life |
IWQOL-Lite | Impact of Weight on Quality of Life-Lite | Obesity-specific quality of life |
DDS | Diabetes Distress Scale | Diabetes-related emotional distress |
PHQ-9 | Patient Health Questionnaire-9 | Depression |
IIEF-5 | International Index of Erectile Function-5 | Diagnostic tool for erectile dysfunction |
EQ-5D | EuroQol-5D | Health-related quality of life |
BBPA | Barriers to Being Physically Active | Barriers to engaging in regular exercise |
HADS | Hospital Anxiety and Depression Scale | Anxiety and depression |
DTSQ | Diabetes Treatment Satisfaction Questionnaire | Satisfaction with diabetes treatment regimens |
POMSb | Profile of Mood States Brief Form | Mood |
Modified WOMAC | Modified Western Ontario and McMaster Universities Osteoarthritis Index | Pain, stiffness and physical function of the knee and hip joints |
BMA 2.0 | Body Morph Assessment Version 2.0 | Body image |
RSES | Rosenberg Self-Esteem Scale | Self-esteem |
CIS | Checklist Individual Strength | Fatigue |
EDE-Q | Eating Disorder Examination Questionnaire | Range and severity of eating disorder features |
ORWELL 97 | Obesity-Related Well-Being 97 | Obesity-specific quality of life |
Rights and permissions
About this article
Cite this article
Martenstyn, J., King, M. & Rutherford, C. Impact of weight loss interventions on patient-reported outcomes in overweight and obese adults with type 2 diabetes: a systematic review. J Behav Med 43, 873–891 (2020). https://doi.org/10.1007/s10865-020-00140-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-020-00140-7