Abstract
Cardiac patients who have social support generally have better prognosis than patients who lack social support. Several theoretical mechanisms have been proposed to explain this protective effect, including the capacity of social support to buffer the negative effects of stress. We tested this buffering effect in a study of patients hospitalized for acute coronary syndrome (ACS) in Spain. Several days after the cardiac event patients answered a questionnaire measuring stressful events during their lifetime, perceived social support around the time of the cardiac event, and depression symptoms in the past week. Results showed that stressful life events were related to depressive symptoms and worse renal function post-ACS only among patients with low perceived social support. Among patients who reported enough social support, lifetime stress was not related to depressive symptoms. No similar effects were observed on other prognostic indicators such as troponin levels or the number of obstructed arteries. These results suggest that social support can buffer the negative effects of stress on the mental and physical well-being of cardiac patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
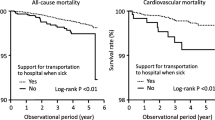
A meta-analytic review of 148 studies concluded that social support is related to a 50% reduction in the likelihood of dying from all-causes—an effect size comparable to that of several well-established risk factors such as smoking or lack of physical activity (Holt-Lunstad et al., 2010). More specifically, social support plays an important role in the onset and recovery from cardiovascular disease (CVD) (Lett et al., 2005). People with limited social support are at a greater risk to develop CVD and are more likely to die once they develop it (Barth et al., 2010). Low social support also predicts more extensive CVD progression measured by the extent of atherosclerosis (Wang et al., 2005).
The mechanisms explaining the effect of social support on cardiovascular health are likely multiple (Uchino et al., 2012; Wills & Ainette, 2012). Research suggests that social support can have an indirect effect on cardiovascular outcomes through several biological, cognitive, and behavioural pathways. For instance, high social support is related to better immune-system functioning, less cardiac reactivity, lower blood pressure, and lower inflammation (e.g., IL-6 and C-reactive protein) (Tomfohr et al., 2015; Uchino et al., 2012; Wills & Ainette, 2012). In addition, low social support often coexists with depression and it can contribute to the emergence and increase of depression symptoms (Lett et al., 2005). Cross-sectional and longitudinal studies in cardiac patients show that low social support increases the chances of suffering depression following a cardiac event (Frasure-Smith et al., 2000; Leifheit-Limson et al., 2012). Depression, in turn, is a risk factor associated with a two-fold increase in the risk of negative cardiovascular outcomes (e.g., mortality) (Van Melle et al., 2004).
Stress is another psychological factor found to contribute significantly to cardiovascular disease (Greenwood et al., 1996). Social support can be beneficial to cardiac patients because it can attenuate harmful cardiovascular changes during stressful events. This benefit is predicted by the buffering model, which posits that social support becomes crucial when individuals undergo stressful events (Cohen & Wills, 1985). This means that the negative effect of stressful events would be stronger or only observed in individuals who lack social support, whereas individuals high on social support would be protected from the negative effects of stress. For instance, a recent study found that social support buffered the negative effects of post-discharge stress on depressive symptoms a month after cardiac hospitalization (León-Pérez et al., 2016). Whereas the positive effects of social support on mental health are easily replicable, the evidence of the stress-buffering effects of social support on health is more inconsistent (Lakey & Orehek, 2011). Studies testing the buffering effect of social support in cardiovascular patients are relatively scarce (Cohen & Wills, 1985; Fontana et al., 1989; Greenwood et al., 1996; León-Pérez et al., 2016) and after many years of research there is no convincing body of evidence to support the model. In addition, studies have also often measured different types of social support including structural, received, or perceived, which may have contributed to the generation of mixed results (Barth et al., 2010; Gallant, 2013). Among these, perceived social support has most consistently been related to health outcomes (Uchino, 2009). Researchers have also called for more sophisticated statistical methods to test for the proposed theoretical pathways (Uchino et al., 2012).
To address these issues, in the current research we tested the buffering model in cardiac patients. We hypothesized that perceived social support would buffer the negative effect of stress on health, such that stressful events will have a negative relationship with health mainly among individuals with low social support.
We examined the proposed mechanisms in a retrospective study of patients hospitalized for an acute coronary syndrome (ACS). In particular, we investigated the relationship between stressful life events and perceived social support with mental and physical health outcomes, including depressive symptoms and disease severity. Suffering depression after ACS is a recognized predictor of new cardiovascular events, cardiac mortality, and all-cause mortality in ACS patients (Van Melle et al., 2004). Measures of disease severity included the subtype of disease (ACS with or without ST-segment elevation), cardiac enzymes (troponin), and the number of obstructed arteries. These indicators are recognized predictors of patient prognosis and are routinely used in practice for diagnostic and prognostic purposes (Hamm et al., 2011; Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology (ESC) et al., 2012). We also considered indicators of renal function, which is another recognized predictor of mortality and morbidity of patients with ACS (Al Suwaidi et al., 2002). Even mild renal impairment was found to be a predictor of increased risk of death and cardiovascular impairment in ACS patients (Anavekar et al., 2004).
The current study builds on previous research conducted mainly in the United States or North-Europe (Wills & Ainette, 2012). Given that social support can act differently across diverse cultures (Rodrigues et al., 2014), the current research adds valuable cross-cultural evidence.
Method
We conducted a cross-sectional observational study of patients with acute coronary syndrome (ACS). We measured stressful life events, perceived social support, depressive symptoms, and several disease severity and prognostic indicators. We also recorded information on classical CVD risk factors which we used as control variables.
This study was part of the project “PySCA: Study on the impact of psychological factors in acute coronary syndrome” developed in collaboration between the University Hospital Virgen de las Nieves and the University of Granada in Spain. The project consists of a series of studies investigating the relationship of diverse psychological factors to clinical outcomes in ACS patients. The sample used in this study forms part of a larger study investigating the relationship between Type D personality and cardiac outcomes, the results of which are reported elsewhere (Garcia-Retamero et al., 2016). The social support and depression measures reported here were added to the existing questionnaire (which already included the stress measure) to test the hypothesis of the current study.
Participants
Participants were admitted with ACS to the hospital Virgen de las Nieves in Granada (Spain) between June 2012 and June 2013 and were recruited on average 4 days after the cardiac episode. Recruitment took plays on days when both a research assistant and a cardiologist were available. The inclusion criteria for the study were having elevated cardiac markers (i.e., Troponin-I) and clinical and electrocardiographic signs of ischaemia. These criteria aimed to identify patients with high-risk coronary syndromes as opposed to other causes of thoracic pain. The exclusion criteria were having an inflammatory disease and/or having neurological problems, as these could influence the values of diverse tests and/or patients’ ability to participate in the research. A cardiologist screened the day’s admission charts for clinically stable eligible patients. Eligible patients were addressed by a psychologist who described the purpose of the study and answered questions when required. The study was described as a study about the role of psychological factors in heart disease which involved the completion of a questionnaire (the information sheet provided can be found in “Appendix 1”). In an effort to minimize exclusion due to illiteracy or other obstacles (e.g., decreased vision), the researcher offered help with questionnaire completion to all patients. Patients who were not feeling well at that moment or were otherwise occupied but were willing to participate were approached again on the next day. Patients received a brief description of the study in written form and signed an informed consent.
During the study period, a total of 301 patients with ACS were admitted to the cardiology department. Of these, 152 were screened when research personnel was available, qualified for participation according to the criteria, and were approached. Ninety-nine (65%) agreed to participate and constituted the sample for this study. Common reasons to decline participation were not feeling well at the moment, not having time, and not being interested in the research. All participants who agreed to participate formed part of the final sample.
Post-hoc sensitivity analysis with G*power (http://gpower.hhu.de/) showed that, given an alpha level of .05, power of .80, 5 control variables, and 3 predictors of interest (social support, stress, and their interaction), with the current sample (N = 99) a medium-sized effect (R2 = .10) could be detected. We considered a medium-effect size to be of potential clinical significance.Footnote 1
Measures
Participants completed the questionnaires described below and several other questionnaires included in the larger study described elsewhere (Garcia-Retamero et al., 2016). Experienced practicing cardiologists extracted information regarding classical risk factors and biomarkers of ACS severity from patients’ medical records.
Psychological constructs
Holmes and Rahe’s stress scale (Holmes & Rahe, 1967)
The scale includes a list of 45 stressful life events (e.g., a death of a spouse, promotion at work, retirement, pregnancy, etc.). Patients indicate if they have experienced each event during their lifetime. Each experienced event is then assigned a “life change” score in accordance with how traumatic the event was rated. These scores are summed up with final scores ranging from 0 to 1467, where a score > 300 indicates a high risk of developing a stress-related illness. The scale is validated for use in a Spanish population and has demonstrated significant associations with health variables (Blasco-Fontecilla et al., 2012; Motrico et al., 2017). The internal consistency of the scale in the current sample was Cronbach’s α = .82.
ENRICHD Social Support Instrument (ESSI) (Vaglio et al., 2004)
This instrument measures patients’ current situation with regard to perceived social support. Items 1–6 assess perceived emotional and instrumental support (e.g., having someone who listens, who gives advice or helps with everyday tasks) on scales ranging from 1 (never) to 5 (always). The last item is a dichotomous question (whether the patient is married or living with a partner; 0 = no, 1 = yes). The final score is a sum of all items and ranges from 6 to 31, where higher scores indicate more perceived social support. We could not locate a validated Spanish version of the scale, so we translated it from English (translation available in “Appendix 2”). We did not consider any items to need cultural adaptation and no difficulties with any particular item emerged during data collection. The internal consistency of the scale in the current sample (Cronbach’s α = .82) and the pronounced positive skew of the distribution corresponded to those of the original version (Mitchell et al., 2003), demonstrating the suitability of the translation.
Beck’s Depression Inventory (BDI) (Beck et al., 1996)
This questionnaire includes 20 items that evaluate the presence of depressive symptoms in the week preceding the study. Answers were coded from 0 (absence) to 3 (permanent or insistent presence). A final score is obtained by summing the corresponding items (range 0–60). There is evidence from diverse populations demonstrating the validity and reliability of the instrument, which has been translated into Spanish and validated for use (Sanz et al., 2005). The internal consistency of the scale in the current sample was Cronbach’s α = .87.
Disease severity indicators and classical risk factors
Based on guidelines of the European Society of Cardiology regarding management of ACSs (Hamm et al., 2011) and cardiovascular disease prevention (Perk et al., 2012), we recorded several relevant indicators of severity of ACS and classical cardiovascular risk factors. First, we recorded if patients suffered a STEMI (i.e., an ST-elevation myocardial infarction) or a non-STEMI. STEMI refers to a more severe ACS characterized by ST-segment elevation on an electrocardiogram test, whereas non-STEMI refers to a less severe ACS, characterized by absence of ST-elevation; STEMI is generally characterized by worse prognosis (Park et al., 2013). We also recorded peak levels of the cardiac enzyme troponin-I which is released in response to damage of the myocardium. Higher peak values of troponin-I reflect more damage to the myocardium. Troponin-I is currently the biomarker with the best diagnostic and prognostic value (Thygesen et al., 2012).Footnote 2 We also recorded the number of obstructed arteries. An artery was defined as obstructed when the stenosis reached more than 50% in a main branch. In case a percutaneous coronary intervention was performed on the patient, we recorded the number of coronary stents that the patient had implanted. Finally, we measured renal function expressed as the concentration of blood urea nitrogen (BUN) (mg/dl) and creatinine (mg/dl). Elevated levels of these waste products in the blood imply an impaired renal function, which is strongly predictive of subsequent disease prognosis (e.g., mortality) (Al Suwaidi et al., 2002). Of the two measures, creatinine concentration is considered a better indicator of renal function (Orvin et al., 2015).
We recorded if patients had any of the following classical risk factors: hypertension, diabetes, and smoking. Patients were classified as hypertensive if they had more than 140 MmHg of systolic blood pressure and more than 90 MmHg of diastolic pressure, had previous history of hypertension, or were taking antihypertensive drugs. Patients were classified as diabetics if they had (a) fasting blood glucose of > 126 mg/dL, (b) they had previous history of diabetes mellitus, or (c) they were taking insulin or oral hypoglycemic. If patients smoked daily, they were classified as smokers. Otherwise, they were classified as non-smokers [see Garcia-Retamero et al. (2016) for similar procedures]. Finally, we also considered age and gender (Hamm et al., 2011; Perk et al., 2012).
Analyses
Patients’ profiles were analysed using descriptive statistics. We assessed the reliability of the scales and addressed assumptions for the use of statistical analyses when required. To investigate the relationship between the psychological constructs and biomarkers we first computed Pearson correlations (Spearman Rho for troponin-I which was skewed). We next tested the hypothesized buffering model (i.e., an interaction between stress and social support indicating moderation) using the PROCESS Add-on for SPSS (Preacher & Hayes, 2008). We also divided patients into two social support groups based on a median split that due to the skewed distribution created two meaningful categories: high (enough) social support (49%, score ≥ 27, e.g., indicating that social support is “always” available on most or all question) and low (lacking) social support (51%, score, e.g., < 27 indicating some lack of support on several or most questions). We conducted analyses using both the continuous score and the group variable. Below we report the results using the group variable and discuss the differences found between these results and the results with the continuous variable.
Results
Participants were 84 males and 15 females with an average age of 61 years (min = 31, median = 62, max = 80). Out of the 99 participants, 33 were smokers, 42 had diabetes, 56 had hypertension, and 37 had a STEMI. Table 1 shows detailed descriptive statistics of the continuous variables. Correlations between the psychological constructs and biomarkers are reported in Table 2. There were no significant correlations between stress or social support and STEMI, troponin-I, the number of obstructed arteries, or the number of stents; however, there were significant correlations between both social support and depressive symptoms with the indicators of renal function (BUN and creatinine). In addition, higher social support was not related to stress but it was related to fewer depressive symptoms.
In sum, social support was related to depressive symptoms and to worse renal function. In addition, depressive symptoms were also related to renal function, suggesting that there could be a relationship from depressive symptoms to renal function. Following these correlation results, we tested the buffering effect on the two indicators of renal function, also integrating the possibility of a relationship between depressive symptoms and renal function. Thus, we tested for an extended moderated mediation model consistent with our initial hypothesis, such that stress was related to worse health (more depressive symptoms and worse renal function), and this negative cascade was only found in individuals low on social support (see Fig. 1 for an illustration).
The PROCESS macro offers methods suitable for small samples and estimates a moderated mediation index (MMI) testing for moderated mediation consistent with the model displayed in Fig. 1 (Preacher & Hayes, 2008). In addition to estimating the coefficients of the model using ordinary least squares regression, the macro estimates conditional indirect effects in moderated mediation models. In particular, first the proposed mediator (depressive symptoms) is regressed on the independent variable (stress), the proposed moderator (social support), their interaction, and control variables. Second, each of the proposed outcome variables is regressed on the mediator, the independent variable, and control variables. Moderated mediation indices (MMI), unstandardized mediated effects (UME), and associated 95% confidence intervals (CIs) are obtained using a bias-corrected bootstrap procedure based on 5000 samples. An effect is considered significant if the CIs exclude 0. The MMI indicates whether the indirect effect is conditional, i.e., differs significantly as a function of the moderator (Hayes, 2015). The UME estimates the indirect effects at pre-specified levels of the moderator. In the context of this research, a significant MMI would indicate that the effect of stress on outcomes through depressive symptoms is different for patients high and low on social support. Estimating the UMEs separately in patients with high and low social support will tell us how this effect is different. To estimate the effect sizes of the UMEs, we used Preacher and Kelley’s (Preacher & Kelley, 2011) Kappa2 coefficient (.01 for small, .09 for medium, and .25 for large). We also used the completely standardized indirect effect (CSIE), which reflects by how many standard deviations the outcome variable changes for one unit change in the independent variable (due to the indirect effect only). Both of these effect size measures are available only in models without control variables.
We ran two moderated mediation analyses: one for BUN and one for creatinine. We conducted all analyses controlling for basic demographics and risk factors (age, gender, smoking, hypertension, and diabetes). Results including standardized coefficients (β) are depicted in Fig. 1. Below we report unstandardized coefficients B.
Depressive symptoms
In the multiple regression model with depressive symptoms as dependent variable, higher stress was related to more depressive symptoms post-ACS, B = .01, CI [.004, .02], p = .021. Social support was not related to depressive symptoms, B = 6.07, CI [− 2.31, 14.46], p = .232. However, there was a significant interaction between stress and social support, B = − .02, CI [− .03, − .003], p = .048, indicating that social support moderated the relationship between stress and depression symptoms. To understand this interaction effect, we divided the sample in two groups − low social support and high social support—using the median split variable and conducted multiple regressions including stress and the control variables as predictors. This revealed that high stress was related to more depressive symptoms among patients with low social support, β = .37, p = .026, but not among patients with high social support, β = − .06, p = .734. None of the control variables were significantly related to depressive symptoms (p > .05).
BUN
In the multiple regression model with BUN as dependent variable, depressive symptoms were the only significant predictor of BUN, B = .81, CI [.43, 1.19], p < .001, suggesting the presence of a mediation effect of stress via depressive symptoms on BUN (see Fig. 1). There was also a significant moderated mediation index MMI = − .012, CI [− .037, − .001], showing that social support moderated this mediation effect. Among patients with low social support, there was significant mediation, UME = .012, CI [.002, .032], with a medium-to-large effect size, Kappa2 = .18, CI [.03, .39], CSME = .17, CI [.03, .37]. However, among patients with high social support depressive symptoms did not mediate the relationship between stress and BUN, UME = − .001, CI [− .008, .009].
Creatinine
In the multiple regression model with creatinine as dependent variable, depressive symptoms were the only significant predictor of creatinine, B = .05, CI [.03, .07], p < .001, also suggesting the presence of a mediation effect of stress via depressive symptoms on creatinine (see Fig. 1). The moderated mediation index MMI = − .001, CI [− .003, .000], suggested that social support moderated this mediation effect (although note that the lower 95% CI bound is 0). In particular, among patients with low social support, there were indications of mediation, UME = .001, CI [.0000, .002], with a medium-to-large effect size, Kappa2 = .17, CI [.02, .36], CSME = .16, CI [.00, .36]. However, among patients with high social support depressive symptoms did not mediate the relationship between stress and creatinine, UME = 0, CI [− .0007, .0004].
The mediation results with social support as a continuous variable were in a similar direction, showing positive mediation effects for values of social support at or lower than the 50th percentile (UMEs from .003 to .010 for BUN and from .0002 to .0007 for creatinine) and zero or no mediation effects for values of social support higher than the 50th percentile (UMEs from − .0002 to − .001 for BUN and from .000 to − .0001 for creatinine). However, the interaction between stress and social support on depressive symptoms was not significant (p > .05) and the 95% CIs for the moderated mediation indexes included 0 with MMI = − .001, CI [− .004, .0001] for BUN, and MMI = − .0001, CI [− .0003, .000] for creatinine, showing that the effect did not proportionally decrease at higher values of social support. We discuss the implication of this finding in the discussion. Figure 2 illustrates the moderation effect of social support based on the analysis with the continuous variable, showing that the effect of stress is only observed for values below the cut-off used for the median split.
Discussion
More stressful life events were related to more depressive symptoms post-ACS, which were in turn related to more impaired renal function. Consistent with the buffering model, this negative cascade was observed only among patients with low perceived social support. In contrast, stressful life events were not related to depressive symptoms in patients with high social support (see Fig. 2).
These results demonstrate that the availability of social support can help buffer the negative effects of accumulated stressful events on individuals’ responses to acute life stressors such as a life-threatening cardiac event. Previous research has often focused on studying different types of stress separately (e.g., adverse life events, acute stress or chronic strains) and establishing which type is most influential; however, different stressors rarely occur in isolation. Instead, stressors most likely interact and exert joint effects on health (Sandín, 2003). For example, a primary stressor (e.g., divorce) can indirectly lead to a secondary stressor (e.g., chronic stress and daily hassles) that has an effect on health. Thus, the experience of previous stressors can result in cumulative adversity and condition how individuals will respond to new stressors (Sandín, 2003). However, the extent to which individuals will be affected by accumulated life stressors depends on the resilience they develop to adverse circumstances (Seery et al., 2010). Social support is one of the factors proposed to help build such resilience (Sandín, 2003). In line with this proposition, in the current study participants who had experienced more stressful life events were more affected by a new stressor (i.e.,. had worse mental health and renal function after a cardiac event) but only if they perceived that they lacked social support. This demonstrates how the availability of social support can make vulnerable individuals more resilient to new acute stressors.
We found that the psychological constructs were related to biomarkers of renal function but were not related to other markers of disease severity. Among individuals with low social support, the indirect effect of stress on renal function was of medium size, suggesting an important clinical difference. It is possible that renal function biomarkers offer more sensitive measurement than the other markers of disease severity or that there are small buffering effects that the current study was not powered enough to detect. Renal function might also have a more direct impact on the subjective well-being of patients. Fatigue and trouble sleeping are common symptoms of renal dysfunction that could be reflected in the depression symptoms score. In clinical practice of ACS care renal function is rarely monitored beyond the purpose of adjusting the medication dosage. We included it in the study protocol because of its documented prognostic value. Renal function is a recognized predictor of mortality, morbidity, and quality of life of CVD patients (e.g., it predicts death or subsequent MI at 30-day and 6-month follow-ups) (Al Suwaidi et al., 2002; Borghi et al., 2015). However, renal function in the context of ACS remains an under researched area, especially in relation to psychological factors. The current study suggests that its relationship to mental health in the context of ACS should be explored further. To our knowledge this is the first study to show that common psychological risk factors such as life stress and depressive symptoms are related to renal function post-ACS in some patients.
Potential bio-behavioural pathways that underlie the relationships between stress, social support, and renal function include dysregulation of the Hypothalamic–Pituitary–Adrenal (HPA) axis and inflammation (Cukor et al., 2006; Uchino, 2006). For example, prolonged stress responses may lead to overstimulation of the sympathetic nervous systems and an increase of adrenaline and cortisol, which could increase cardiovascular risk (O’Neil, 2013). In addition, kidneys are responsible for the metabolism of peptide and steroid hormones acting on the HPA axis, suggesting a potential relationship between the HPA axis and impaired renal function (Fallon, 2011). Finally, high social support of family and friends is related to decreased cortisol reactivity in stressful situations, which diminishes activity in the dorsal anterior cingulate cortex and Brodmann area 9—areas related to social distress and emotional regulation (Eisenberger et al., 2007).
Among different types of social support (Taylor, 2011) such as tangible (i.e., receiving instrumental assistance) or informational social support (i.e., receiving useful information), the support measured in our study reflects people’s perceptions of emotional social support (i.e., receiving affection from others, feeling that there is someone who would listen or help when needed). Such support may be especially effective when stressors are structural, i.e., cannot be changed by the individual (e.g., such as experiencing an ACS). For instance, precisely perceived emotional support from family and friends buffered the impact of the economic crisis (a structural stressor) on Spanish residents’ health-related quality of life (Fernandez et al., 2015).
In addition, it was the perception of having enough versus lacking social support expressed by the dichotomized variable that resulted in the hypothesized interaction between stress and social support. This procedure and result is consistent with a large number of previous studies that have contrasted high versus low social support and found statistically and clinically significant effects on outcomes (e.g., mortality, see Holt-Lunstad et al., 2010). In the current study, the model predicted important differences in mental health (i.e., about 2–3 points) between patients perceiving high versus low social support at high levels of stress (see Fig. 2). Although the interaction with the continuous social support variable was not significant, results were in a similar direction. On one hand, these results support the view of a threshold effect: the importance of perceiving enough support versus perceiving any lack of support as the determining factor (Wills & Ainette, 2012). On the other hand, although there is a theoretical justification for the dichotomization, it can produce spurious results. Thus, it is important that the current model is replicated, preferably in a larger sample, to see if the obtained results are robust and the effect sizes reliable.
Although the buffering model was proposed more than 30 years ago (Wills & Ainette, 2012), this is the first research to our knowledge to examine its validity in ACS patients in Spain. A crucial next step would be to find how perceptions of emotional social support are formed and how they can be enhanced, thereby generating health benefits. Unfortunately, successfully increasing social support does not guarantee observing more positive cardiovascular outcomes. For instance, the ENRICHD intervention using counselling sessions successfully increased perceived social support but this increase did not reduce risk of major adverse cardiac events (Berkman et al., 2003), suggesting that more research is needed. One theoretical model that could be helpful in studying how health-benefiting perceptions of social support are formed is Relational Regulation Theory (Lakey & Orehek, 2011). It proposes that, instead of talking about how to cope with stress, people learn to regulate their thoughts and emotions through daily social activities, and that social support is effective to the extent that there is a match between the support providers and recipients (Lakey & Orehek, 2011). This emphasis on regulation in daily interactions suggests that modern technologies like research apps that track daily activities and people’s perceptions of support can be cost-effective tools that can help design interventions (Hogan et al., 2002). To the best of our knowledge there are no published interventions yet aiming to increase social support and improve health specifically based on insights from Relational Regulation Theory. The theory predicts that such interventions will be more effective if they focus on relational influences and match recipients with providers, so that supportive relationships emerge (Lakey & Orehek, 2011). However, in most interventions participants are assigned providers that the researchers assume will be supportive (Hogan et al., 2002; Lakey & Orehek, 2011). Given the current results, another important aspect to consider in intervention design is whether an intervention would benefit all patients or only those who have experienced high stress.
Like most research, this study has some limitations. The data are cross-sectional and no causal inferences can be made regarding the direction of the relationship between stress, depression symptoms, and health outcomes. On one hand, the large cross-cultural INTERHEART study showed that psychosocial stress is associated with an increased risk of acute myocardial infarction (Rosengren et al., 2004) and a more recent study even demonstrated that activity in the amygdala (a brain region involved in stress) predicts cardiovascular events via increased bone marrow activity and arterial inflammation (Tawakol et al., 2017). In addition, there is evidence showing that post-discharge stress in cardiac patients affects subsequent depressive symptoms, supporting the model proposed in the current study (León-Pérez et al., 2016). On the other hand, intuition and longitudinal evidence speak in favour of bidirectional relationships between perceived stress, mental distress, and cardiac symptoms [e.g., perceived stress exacerbates cardiac symptoms and cardiac symptoms in turn increase perceived stress (Fontana et al., 1989)]. Whatever the specific direction of the relationship between stress, depression, and health outcomes, the current studies show that consistent with the buffering model, it is stronger among patients who lack social support.
Notes
To detect a small effect size (R2 = .05) under the same conditions, 212 participants would have been necessary.
Per protocol we also extracted peak myoglobin values (another cardiac biomarker similar to troponin). However, recently the hospital stopped using this biomarker for diagnostic or prognostic purposes because of the superiority of new generation high-sensitivity troponin tests. For this reason, we eventually do not report results using myoglobin (which also showed no significant relationships of interest).
References
Al Suwaidi, J., Reddan, D. N., Williams, K., Pieper, K. S., Harrington, R. A., Califf, R. M., et al. (2002). Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation, 106, 974–980.
Anavekar, N. S., McMurray, J. J., Velazquez, E. J., Solomon, S. D., Kober, L., Rouleau, J. L., et al. (2004). Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. New England Journal of Medicine, 351, 1285–1295.
Barth, J., Schneider, S., & von Kanel, R. (2010). Lack of social support in the etiology and the prognosis of coronary heart disease: A systematic review and meta-analysis. Psychosomatic Medicine, 72, 229–238.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory-II. San Antonio, 78, 490–498.
Berkman, L. F., Blumenthal, J., Burg, M., Carney, R. M., Catellier, D., Cowan, M. J., et al. (2003). Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. JAMA, the Journal of the American Medical Association, 289, 3106–3116.
Blasco-Fontecilla, H., Delgado-Gomez, D., Legido-Gil, T., De Leon, J., Perez-Rodriguez, M. M., & Baca-Garcia, E. (2012). Can the Holmes–Rahe social readjustment rating scale (SRRS) be used as a suicide risk scale? An exploratory study. Archives of Suicide Research, 16, 13–28.
Borghi, C., Rosei, E. A., Bardin, T., Dawson, J., Dominiczak, A., Kielstein, J. T., et al. (2015). Serum uric acid and the risk of cardiovascular and renal disease. Journal of Hypertension, 33, 1729–1741.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357.
Cukor, D., Peterson, R. A., Cohen, S. D., & Kimmel, P. L. (2006). Depression in end-stage renal disease hemodialysis patients. Nature Reviews Nephrology, 2, 678–687.
Eisenberger, N. I., Taylor, S. E., Gable, S. L., Hilmert, C. J., & Lieberman, M. D. (2007). Neural pathways link social support to attenuated neuroendocrine stress responses. NeuroImage, 35, 1601–1612.
Fallon, M. (2011). Depression in end-stage renal disease. Journal of Psychosocial Nursing and Mental Health Services, 49, 30–34.
Fernandez, A., Garcia-Alonso, J., Royo-Pastor, C., Garrell-Corbera, I., Rengel-Chica, J., Agudo-Ugena, J., et al. (2015). Effects of the economic crisis and social support on health-related quality of life: First wave of a longitudinal study in Spain. The British Journal of General Practice: The Journal of the Royal College of General Practitioners, 65, e198–e203.
Fontana, A. F., Kerns, R. D., Rosenberg, R. L., & Colonese, K. L. (1989). Support, stress, and recovery from coronary heart disease: A longitudinal causal model. Health Psychology, 8, 175–193.
Frasure-Smith, N., Lesperance, F., Gravel, G., Masson, A., Juneau, M., Talajic, M., et al. (2000). Social support, depression, and mortality during the first year after myocardial infarction. Circulation, 101, 1919–1924.
Gallant, M. P. (2013). Social networks, social support, and health-related behavior. In L. R. Martin & M. R. DiMatteo (Eds.), The Oxford handbook of health communication, behavior change, and treatment adherence (pp. 305–322). New York: Oxford University Press.
Garcia-Retamero, R., Petrova, D., Arrebola-Moreno, A., Catena, A., & Ramírez-Hernández, J. A. (2016). Type D personality is related to severity of acute coronary syndrome in patients with recurrent cardiovascular disease. British Journal of Health Psychology, 14, 111–119.
Greenwood, D. C., Muir, K. R., Packham, C. J., & Madeley, R. J. (1996). Coronary heart disease: A review of the role of psychosocial stress and social support. Journal of Public Health Medicine, 18, 221–231.
Hamm, C. W., Bassand, J. P., Agewall, S., Bax, J., Boersma, E., Bueno, H., et al. (2011). ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal, 32, 2999–3054.
Hayes, A. F. (2015). An index and test of linear moderated mediation. Multivariate Behavioral Research, 50, 1–22.
Hogan, B. E., Linden, W., & Najarian, B. (2002). Social support interventions: Do they work? Clinical Psychology Review, 22, 381–440.
Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of Psychosomatic Research, 11, 213–218.
Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS medicine, 7, e1000316.
Lakey, B., & Orehek, E. (2011). Relational regulation theory: A new approach to explain the link between perceived social support and mental health. Psychological Review, 118, 482–495.
Leifheit-Limson, E. C., Reid, K. J., Kasl, S. V., Lin, H., Buchanan, D. M., Jones, P. G., et al. (2012). Changes in social support within the early recovery period and outcomes after acute myocardial infarction. Journal of Psychosomatic Research, 73, 35–41.
León-Pérez, G., Wallston, K. A., Goggins, K. M., Poppendeck, H. M., & Kripalani, S. (2016). Effects of stress, health competence, and social support on depressive symptoms after cardiac hospitalization. Journal of Behavioral Medicine, 39, 441–452.
Lett, H. S., Blumenthal, J. A., Babyak, M. A., Strauman, T. J., Robins, C., & Sherwood, A. (2005). Social support and coronary heart disease: Epidemiologic evidence and implications for treatment. Psychosomatic Medicine, 67, 869–878.
Mitchell, P. H., Powell, L., Blumenthal, J., Norten, J., Ironson, G., Pitula, C. R., et al. (2003). A short social support measure for patients recovering from myocardial infarction: The ENRICHD social support inventory. Journal of Cardiopulmonary Rehabilitation and Prevention, 23, 398–403.
Motrico, E., Rodero-Cosano, M. L., Álvarez-Gálvez, J., Salinas-Pérez, J. A., & Moreno-Peral, P. (2017). Instrumentos de evaluación de los eventos vitales estresantes en población española adulta: Una revisión sistemática. Anales De Psicología, 33, 556–567.
O’Neil, A. (2013). The relationship between coronary heart disease (CHD) and major depressive disorder (MDD): Key mechanisms and the role of quality of life. Europe’s Journal of Psychology, 9, 163–184.
Orvin, K., Eisen, A., Goldenberg, I., Farkash, A., Shlomo, N., Gevrielov-Yusim, N., et al. (2015). The proxy of renal function that most accurately predicts short-and long-term outcome after acute coronary syndrome. American Heart Journal, 169, 702–712.
Park, H. W., Yoon, C. H., Kang, S. H., Choi, D. J., Kim, H. S., Cho, M. C., et al. (2013). Early-and late-term clinical outcome and their predictors in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction. International Journal of Cardiology, 169, 254–261.
Perk, J., De Backer, G., Gohlke, H., Graham, I., Reiner, Z., Verschuren, M., et al. (2012). European guidelines on cardiovascular disease prevention in clinical practice (version 2012). European Heart Journal, 33, 1635–1701.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891.
Preacher, K. J., & Kelley, K. (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16, 93–115.
Rodrigues, M. M. S., Gierveld, J. D. J., & Buz, J. (2014). Loneliness and the exchange of social support among older adults in Spain and the Netherlands. Ageing & Society, 34, 330–354.
Rosengren, A., Hawken, S., Ounpuu, S., Sliwa, K., Zubaid, M., Almahmeed, W. A., et al. (2004). Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): Case-control study. The Lancet, 364, 953–962.
Sandín, B. (2003). El estrés: Un análisis basado en el papel de los factores sociales [Stress: An analysis based on social factors]. International Journal of Clinical and Health Psychology, 3, 141–157.
Sanz, J., García-Vera, M. P., Espinosa, R., Fortún, M., & Vázquez, C. (2005). Adaptación española del inventario para la depresión de beck-II (BDI-II): 3. propiedades psicométricas en pacientes con trastornos psicológicos. Clínica y Salud, 16, 121–142.
Seery, M. D., Holman, E. A., & Silver, R. C. (2010). Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. Journal of Personality and Social Psychology, 99, 1025–1041.
Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology (ESC), Steg, P. G., James, S. K., Atar, D., Badano, L. P., Blömstrom-Lundqvist, C., et al. (2012). ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal, 33, 2569–2619.
Tawakol, A., Ishai, A., Takx, R. A., Figueroa, A. L., Ali, A., Kaiser, Y., et al. (2017). Relation between resting amygdalar activity and cardiovascular events: A longitudinal and cohort study. The Lancet, 389, 834–845.
Taylor, S. E. (2011). Social support: A review. In H. Friedman (Ed.), Oxford handbook of health psychology (pp. 189–214). New York: Oxford University Press.
Thygesen, K., Alpert, J. S., Jaffe, A. S., Simoons, M. L., Chaitman, B. R., White, H. D., et al. (2012). Third universal definition of myocardial infarction. Journal of the American College of Cardiology, 60, 1581–1598.
Tomfohr, L. M., Edwards, K. M., Madsen, J. W., & Mills, P. J. (2015). Social support moderates the relationship between sleep and inflammation in a population at high risk for developing cardiovascular disease. Psychophysiology, 52, 1689–1697.
Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29, 377–387.
Uchino, B. N. (2009). Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspectives on Psychological Science, 4, 236–255.
Uchino, B. N., Bowen, K., Carlisle, M., & Birmingham, W. (2012). Psychological pathways linking social support to health outcomes: A visit with the “ghosts” of research past, present, and future. Social Science and Medicine, 74, 949–957.
Vaglio, J., Conard, M., Poston, W. S., O’Keefe, J., Haddock, C. K., House, J., et al. (2004). Testing the performance of the ENRICHD social support instrument in cardiac patients. Health and Quality of Life Outcomes, 2, 24.
van Melle, J. P., de Jonge, P., Spijkerman, T. A., Tijssen, J. G., Ormel, J., van Veldhuisen, D. J., et al. (2004). Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis. Psychosomatic Medicine, 66, 814–822.
Wang, H., Mittleman, M. A., & Orth-Gomer, K. (2005). Influence of social support on progression of coronary artery disease in women. Social Science and Medicine, 60, 599–607.
Wills, T. A., & Ainette, M. G. (2012). Social networks and social support. In A. Baum, A. Revenson, & J. Singer (Eds.), Handbook of Health Psychology (pp. 465–492). New York: Psychology Press.
Funding
This research is part of the self-funded project “PySCA: Study on the impact of psychological factors in acute coronary syndrome” (Principal Investigator: JARH). Dafina Petrova is supported by a Juan de la Cierva Fellowship (FJCI-2016-28279) from the Spanish Ministry of Economy, Industry, and Competitiveness. Financial support was partially provided by the Ministerio de Economía y Competitividad (Spain) (PSI2011-22954 and PSI2014-51842-R).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Simona Wiesmaierova, Dafina Petrova, Antonio Arrebola Moreno, Andrés Catena, José Antonio Ramírez Hernández and Rocio Garcia-Retamero declare independence from the funding agencies and do not have conflicts of interest including financial interests, activities, relationships, and affiliations.
Ethical approval
The Ethics Committee of the University Hospital Virgen de las Nieves in Granada, Spain, provided approval for the study.
Human and animal rights and Informed consent
All procedures were in accordance with the ethical standards of the institutional research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Information given to participants about the objective of the study (translation from Spanish)
Dear patient:
Your doctor has raised the possibility of participating in the study “PYSCA: STUDY ON THE IMPACT OF PSYCHOLOGICAL FACTORS IN ACUTE CORONARY SYNDROME: INCIDENCE, PHYSIOPATHOLOGICAL MECHANISMS, AND INTERVENTION PROCEDURES.”
Atherosclerosis is the main and immediate cause of coronary heart disease and its clinical manifestation. We know a lot about how some factors such as smoking and diabetes affect the development of this disease, but it is also important to study the influence of psychological factors such as personality, stress, or depression.
The objective of this study is to determine how emotional and personality factors, evaluated by means of questionnaires, could influence coronary disease and/or the clinical outcomes after a coronary intervention. We also intend to determine how these psychological factors influence the development and progression of the disease. During your time in the hospital, we will evaluate your type of personality, lifestyle, and other relevant factors using standardized questionnaires. In addition to the usual analysis conducted, an additional 20 mL blood sample will be required for the analysis of inflammatory markers.
Appendix 2: Spanish version of the ENRICHD Social Support Instrument (Mitchell et al., 2003)
-
Por favor, lea las siguientes preguntas y marque la respuesta que mejor describa su situación en la actualidad.
-
1. ¿Hay alguna persona que esté dispuesta a escucharle cuando usted necesita hablar?
-
1: Nunca 2: Casi nunca 3: Algunas veces 4: La mayoría de las veces 5: Siempre
-
2. ¿Hay alguna persona que pueda darle un buen consejo sobre un problema cuando usted lo necesita?
-
1: Nunca 2: Casi nunca 3: Algunas veces 4: La mayoría de las veces 5: Siempre
-
3. ¿Hay alguna persona que le muestre amor y cariño?
-
1: Nunca 2: Casi nunca 3: Algunas veces 4: La mayoría de las veces 5: Siempre
-
4. ¿Hay alguna persona que le ayude con las tareas diarias?
-
1: Nunca 2: Casi nunca 3: Algunas veces 4: La mayoría de las veces 5: Siempre
-
5. ¿Hay alguien que pueda ofrecerle apoyo emocional (hablar sobre sus problemas o ayudarle a tomar una decisión difícil)?
-
1: Nunca 2: Casi nunca 3: Algunas veces 4: La mayoría de las veces 5: Siempre
-
6. Piense en una persona cercana, de la que pueda estar seguro(a) y en la que pueda confiar ¿Tiene con ella tanto contacto como desearía?
-
1: Nunca 2: Casi nunca 3: Algunas veces 4: La mayoría de las veces 5: Siempre
-
7. Actualmente, ¿está usted casado o vive con su pareja?
-
[ ] Si [ ] No
Rights and permissions
About this article
Cite this article
Wiesmaierova, S., Petrova, D., Arrebola Moreno, A. et al. Social support buffers the negative effects of stress in cardiac patients: a cross-sectional study with acute coronary syndrome patients. J Behav Med 42, 469–479 (2019). https://doi.org/10.1007/s10865-018-9998-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-018-9998-4