Abstract
With the publication of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, the American Psychiatric Association published several disorder-specific severity measures to support a dimensional approach to disorder classification. The Severity Measure for Specific Phobia – Adult (SMSP; Craske et al., 2013) was designed to provide a dimensional assessment of specific phobia symptoms, but limited psychometric data is currently available for this tool. This study assessed the construct and criterion validity of the SMSP in a sample of adults (n = 67) who self-reported specific phobia symptoms. The SMSP demonstrated excellent internal consistency (Cronbach’s α = 0.93) and statistically significant positive correlations were observed between the SMSP and an associated measure of specific phobia and distress. Statistically significant group differences were observed based on the outcome of a telephone-administered psychodiagnostic interview, such that SMSP scores were higher for participants who met diagnostic criteria for specific phobia than participants who did not (p < .001, d = 1.30). Regression models based on the outcome of the telephone interview indicated that scores on the SMSP uniquely predicted the presence or absence of specific phobia (p < .001) compared to scores from a hypothesized discriminant measure of depression (p = .67). Results provide support for the psychometric utility of the SMSP, though further evaluation of the construct validity of this measure in larger and more diverse samples is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Investigating the Psychometric Properties of the Severity Measure for Specific Phobia
Specific phobia is classified as an anxiety disorder characterized by fear and avoidance towards specific objects or situations according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5; American Psychiatric Association, 2013). The DSM-5 describes specific phobia as consisting of five broad subtypes: Animal Type (e.g., snakes, rodents, and spiders); Natural Environment Type (e.g., heights, water, and storms); Blood-Injection-Injury Type (e.g., needles and seeing blood); Situational Type (e.g., flying, driving, and enclosed spaces); and Other Type (e.g., vomiting, choking, and stimuli not accounted for by another subtype). Diagnostic data indicate that specific phobia is a prevalent condition estimated to affect between 7% and 13% of North Americans during their lifetime (Eaton et al., 2018). Importantly, it has been reported that over 60% of individuals with specific phobia will experience an additional mental health disorder over the course of their life, with the highest rates of comorbidity occurring with other mood and anxiety disorders (Wardenaar et al., 2017). Specific phobia is also debilitating, as evidenced by issues of role impairment and compromised functioning in domains such as employment that can worsen without treatment (Wardenaar et al., 2017; Witthauer et al., 2016). The condition responds well to exposure therapy, which is widely regarded as the gold standard for specific phobia treatment (Eaton et al., 2018; Grös & Antony, 2006; Wolitzky-Taylor et al., 2008).
Despite the high prevalence and considerable burden of illness associated with specific phobia, the condition is largely under-detected and under-treated (Bandelow & Michaelis, 2015; Eaton et al., 2018). Several self-report measures have been developed to assess single phobias (i.e., fear of spiders, flying, and the dentist, among others; Szymanski & O’Donohue 1995; Haug et al., 1987; Stouthard et al., 1993). However, these measures cannot be used to assess the severity of specific phobia symptoms across all subtypes of the disorder. The Fear Survey Schedule (FSS-II; Geer 1965) and Phobic Stimuli Response Scales (PSRS; Cutshall & Watson 2004) are existing self-report measures used to assess a range of specific phobia subtypes. Although the FSS-II has been a popular measure of fear in research and clinical practice (McCabe & Antony, 2002), studies have not been able to agree upon a factor structure for the FSS-II and the measure has been reported to not reliably distinguish between individuals with and without specific phobia (Beck et al., 1998; Cutshall & Watson, 2004). The psychometric properties of the PSRS, on the other hand, have not been validated in a clinical population (Hood & Antony, 2012). Furthermore, neither the FSS-II or PSRS are aligned with the DSM-5 criteria for specific phobia, and do not evaluate key components of the disorder, such as avoidance (Hood & Antony, 2012). Both measures also include several items that are unrelated to specific phobia and may be explained by another anxiety disorder (e.g., fear of angry people, worry about life after death, and fears of being criticized by others; Grös & Antony 2006; Hood & Antony, 2012).
To support the broad range of DSM-5 specific phobia subtypes, the American Psychiatric Association published the Severity Measure for Specific Phobia – Adult (SMSP; Craske et al., 2013), which is a 10-item self-report questionnaire that assesses the severity of specific phobia symptoms. Unlike self-report tools used to measure single specific phobias, the SMSP assesses symptoms across all specific phobia subtypes in the DSM-5. Further, the SMSP assesses specific phobia symptoms in accordance with DSM-5 criteria for the disorder, distinguishing the measure from tools such as the FSS-II and PSRS. An initial study of the DSM-5 severity measures indicated that the SMSP had good internal consistency (Cronbach’s α = . 96), and scores on the SMSP were significantly higher for individuals determined to have a specific phobia compared to individuals without this condition. However, the effect size of this difference was lower for the SMSP (d = 0.72) compared to the other dimensional severity measures examined (d = 0.81 − 1.5), which led to calls for further psychometric studies of the SMSP (Lebeau et al., 2012).
The DSM-5 severity measures have since been adapted for German-, Dutch-, Portuguese-, and Spanish-speaking populations, however researchers have pointed out the need for further evaluation of the SMSP in its original form (Craske et al., 2013; DeSousa et al., 2017; LeBeau et al., 2012, 2015; Vidal-Arenas et al., 2021). Furthermore, data from preliminary psychometric evaluation of modified versions of the SMSP have been inconclusive. For example, adequate criterion validity has been observed for the Dutch and German versions of the SMSP (Beesdo-Baum et al., 2012; Knappe et al., 2013; Möller & Bögels, 2016), but estimates of clinical utility have varied. One study found that the German SMSP possessed adequate predictive utility (AUC = 0.72; Beesdo‐Baum et al., 2012), while a subsequent publication found the measure to have low predictive utility (AUC = 0.53; Knappe et al., 2014). Good convergent validity has been reported for German and Dutch versions of the SMSP when compared to other phobia measures (i.e., Fear Questionnaire, Fear Survey schedule, and Screen for Child Anxiety Related Disorders – Adult: Specific Phobia Subscale), however convergent measures utilized in previous studies have lacked the scope to assess all DSM-5 subtypes of specific phobia and criteria such as interference and avoidance (Beesdo‐Baum et al., 2012; Knappe et al., 2014; Möller & Bögels, 2016). Therefore, the construct validity (i.e., ability of a test to demonstrate expected correlations with other measures of related constructs) and criterion validity (i.e., degree to which a measure is correlated with the presence or absence of a specific criterion) of the SMSP is in particular need of further examination with a wider selection of validity measures (Knappe et al., 2014).
Study Aims
Given the need for further psychometric data for the standard adult version of the SMSP, the objective of this study was to evaluate the construct and criterion validity of the SMSP in a sample of Canadian adults from the general population. The primary aim of this study was to provide psychometric support for the SMSP by comparing its performance to other measures of specific phobia, while also examining its performance relative to measures of distress, anxiety, and depression. As such, our primary hypotheses were that: (1) the SMSP would demonstrate high internal consistency, (2) scores on the SMSP would demonstrate statistically significant positive correlations with existing measures of specific phobia and a general measure of distress [convergent validity], and (3) scores on the SMSP would demonstrate comparatively smaller positive correlations with a presumed divergent measure of anxiety and depression [divergent validity].
A secondary aim of the study was to examine the SMSP when compared to the results of a semistructured telephone interview designed to assess the presence of specific phobia according to DSM-5 criteria. Secondary hypotheses for this study were that: (1) average scores on the SMSP would be higher for individuals determined to meet diagnostic criteria for specific phobia during the telephone interview compared to individuals who did not [criterion validity], and (2) scores on the SMSP would be statistically predictive of the outcome of the telephone interview compared to a proposed discriminant measure of depression [predictive validity].
An exploratory aim for this study was to assess the curve of a Receiver Operating Characteristics (ROC) analysis for the SMSP. This was done to estimate the diagnostic accuracy of SMSP scores for the presence or absence of a specific phobia according to the results of the telephone interview. For this analysis, no hypotheses were generated due to the limited conclusive psychometric data for the SMSP published to date.
Methods
Participants
Data were collected from a sample of adults (n = 67) recruited online through social media, classified websites, phobia forums, and other online communities. Recruitment began in January 2021, and data collection concluded in February 2021. Study procedures were approved by the research ethics board at the institution involved and informed consent was obtained from all individuals who chose to participate in the study. Participants were included in the study if they resided in Canada, were between 18 and 65 years of age, and self-reported as having specific phobia symptoms. The mean age of participants was 31.3 years (SD = 10.6), with the majority of participants being female (67.2%), employed full- or part-time (59.7%), university educated (70.1%), and of White European (49.3%) or Asian (31.3%) ethnocultural background. A summary of the demographic characteristics of the sample is provided in Table 1.
Measures
Diagnostic Assessment and Research Tool (DART; McCabe et al., 2017)
The DART is a semistructured open-access interview tool developed at St. Joseph's Healthcare Hamilton and McMaster University. The DART was designed to assess a broad range of diagnostic criteria associated with several DSM-5 disorders and is modular in design, such that several distinct modules are available for administration either together or separately for clinical or research purposes. Each module follows a semistructured question format, including mandatory questions appraising DSM-5 diagnostic criteria for a given disorder and optional follow-up questions for further clarification. Interviewers indicate their diagnostic impression at the end of each module by selecting one of three response options (i.e., absent, present, or subthreshold). The DART has demonstrated excellent psychometric properties in a clinical sample (Schneider et al., 2021). For the purposes of this study, only the specific phobia module of the DART was administered to participants.
Depression Anxiety Stress Scales 21-item Version (DASS-21; Lovibond & Lovibond 1995)
The DASS-21 is a self-report questionnaire containing three subscales designed to measure emotional states of depression, anxiety, and stress. Each item assesses the extent to which the statement applied to the respondent over the past seven days and is rated on a 4-point scale ranging from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). A total score (ranging from 0 to 63) may be calculated by summing all items in the measure, or individual depression, anxiety, and stress scores can be derived by summing the appropriate items for each of the three corresponding subscales. The DASS-21 has excellent psychometric properties (Cronbach’s α = 0.88-0.94 across subscales; Antony et al., 1998; Lovibond & Lovibond, 1995). Cronbach’s α for the Depression, Anxiety, and Stress subscales of the DASS-21 in the current sample were 0.93, 0.87, and 0.88, respectively.
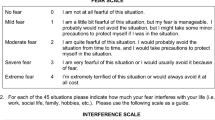
Fear Survey Schedule (FSS-II; Geer 1965)
The FSS-II is a 51-item self-report questionnaire that lists a range of objects and situations considered to be commonly feared by the authors (e.g., injury, social interaction, and animals). The measure requires respondents to rate the amount of fear they experience in response to each item on a 7-point scale that ranges from 1 (no fear) to 7 (terror). Scores of each of the 51 items are summed to calculate a total score, which may range from 51 to 357. Initial validation of the FSS-II demonstrated high internal consistency (r = .94; Geer 1965). Cronbach’s α in the current sample was 0.96.
Illness Intrusiveness Ratings Scale (IIRS; devins 2010)
The IIRS is a 13-item self-report questionnaire that measures the extent to which illness, or the treatment of illness, interferes with quality of life. Respondents rate the extent of the interference they experience in the 13 domains of life on a 7-point Likert scale that ranges from 1 (not very much) to 7 (very much). All items on the measure may be summed to give a total score ranging from 13 to 91. The IIRS has high validity, test-retest reliability, and internal consistency (Cronbach’s α = 0.78-0.95; Devins 2010). Cronbach’s α for the IIRS in the current sample was 0.88.
Phobic Stimuli Response Scales (PSRS; Cutshall & Watson 2004)
The PSRS is a self-report questionnaire that was designed to measure a range of fears related to social and specific phobia as described in the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (American Psychiatric Association, 2000). The measure contains 46 items that evaluate emotions and thoughts related to fears in several domains (i.e., social, animal, physical-confinement, bodily harm, and blood-injection situations). Each item is rated on a 4-point Likert scale that ranges from 1 (strongly disagree) to 4 (strongly agree). All items may be summed to give a total score, which ranges from 46 to 184, or scores may be calculated for each of the five subscales. The PSRS has good internal consistency (Cronbach’s α = 0.73-0.88 across subscales; Cutshall & Watson 2004). Cronbach’s α in the current sample were 0.88, 0.87, 0.92, 0.81, and 0.92 for the social, animal, physical confinement, bodily harm, and blood-injection subscales of the PSRS, respectively.
Severity measure for specific phobia – adult (SMSP; Craske et al., 2013)
The SMSP is a self-report questionnaire that contains 10 items that assess the severity of specific phobia symptoms across five specific phobia groups: driving, flying, tunnels, bridges, or enclosed spaces; animals or insects; heights, storms, or water; blood, needles, or injections; and choking or vomiting. Like all anxiety severity measures published in the DSM-5, the SMSP requires respondents to rate the degree to which each item applies to them over the past 7 days on a 5-point scale that ranges from 0 (Never) to 4 (All of the time). The scores of each of the 10 items are summed to give a raw total score which ranges from 0 to 40 points. An average total score may also be calculated by dividing the raw total score by the number of items in the measure. The SMSP is one of the American Psychiatric Association’s emerging dimensional measures of anxiety disorders, and further evaluation of the tool’s psychometric properties is needed (LeBeau et al., 2012, 2015). Cronbach’s α for the SMSP in the current sample was 0.93.
Specific Phobia Questionnaire (SPQ; Fairbrother & Antony 2012)
The SPQ is a 43-item self-report questionnaire that assesses both the severity of fear and the extent to which fear interferes in daily activities for a broad range of phobic stimuli corresponding to the five subtypes of specific phobia described in the DSM-5. Respondents rate the severity of the fear and interference they experience in response to the situations described in each item (e.g., high open places, driving on highways, getting minor surgery) on a 5-point scale that ranges from 0 (None) to 4 (Extreme). The sum of the fear and interference scores of all items may be used to derive a total score ranging from 0 to 344, or fear scores may be summed to calculate individual scores for each of the five subscales. Preliminary psychometric analysis of the SPQ demonstrated good test-retest reliability, construct validity, and internal consistency (Cronbach’s α = 0.64-0.92; Ovanessian et al., 2019). In the current sample, Cronbach’s α for the Animal, Blood-Injection-Injury, Natural Environment, Situational, and Other subscales of the SPQ were 0.94, 0.96, 0.92, 0.92, and 0.85, respectively.
Procedure
Interested participants (N = 157) were directed to complete an online survey hosted by the institution where the study was conducted. Survey responses were recorded using the Research Electronic Data Capture program (REDCap; Harris et al., 2009). Eligible participants who consented to participate in the study (n = 133) were directed to complete a battery of self-report questionnaires, which included items assessing demographic characteristics as well as measures assessing specific phobia, distress, anxiety, and depression symptoms. Participants who completed the battery of self-report questionnaires (n = 108) were contacted by the principal investigator and invited to complete a telephone interview consisting of the specific phobia module of the DART to further assess specific phobia symptoms. Of the 108 participants contacted, a total of 67 participants completed the subsequent telephone interview and thus their data was eligible for analysis. Data were excluded from analysis in cases where participants did not respond to the interview invitation (n = 34), did not attend their scheduled interview (n = 2), or where duplicate responses were observed (n = 5).
The specific phobia module of the DART interview was administered over the telephone to gain a better understanding of participants’ symptoms and to supplement their responses on the self-report questionnaires. Specifically, the results of the DART interview were used to distinguish between individuals in the sample who reported experiencing symptoms of specific phobia consistent with DSM-5 diagnostic criteria from individuals who did not. Telephone interviews were conducted by the principal investigator following an initial training period with an experienced doctoral-level registered psychologist (L.H.S.), which consisted of observing the administration of a minimum of three telephone interviews and completing a minimum of three telephone interviews under live supervision. Ongoing supervision was also provided, which consisted of individual supervision and a review of completed telephone interviews throughout data collection. Both the principal investigator and supervisor were blind to participant scores on the self-report measures prior to conducting the telephone interview.
Data Analysis
All data analyses were conducted using IBM SPSS (Version 27) predictive analytics software. Cronbach’s α was calculated for the SMSP to provide an estimate of internal consistency. Spearman’s rank-order correlation coefficients (Spearman’s Rho) were generated to examine relationships between the SMSP and hypothesized convergent (i.e., SPQ, PSRS, FSS-II, and IIRS) or divergent (i.e., DASS-21) measures. Spearman’s Rho was chosen because it a robust statistic that minimizes the effect of uneven data distribution that is often observed in small sample sizes (Akoglu, 2018). The criterion validity of the SMSP was examined by conducting an independent samples t-test which used the outcome of the telephone interview as a grouping variable (e.g., participants who did or did not meet the diagnostic criteria for specific phobia). Bootstrapping was used to overcome the shortcoming of uneven data distribution often observed in small sample sizes. Estimates of effect size (Cohen’s d) and associated 95% confidence intervals were also calculated for the independent samples t-test. Binary logistic regression models were used to compare the predictive validity of the SMSP to that of a hypothesized divergent measure (i.e., DASS-21: Depression Subscale) based on the outcome of the telephone interview. The area under the curve (AUC) was calculated for the SMSP based on the outcome of the telephone interview to estimate the diagnostic accuracy of SMSP scores for the presence or absence of a specific phobia. It is generally acknowledged that an AUC value of 0.5 represents a lack of discriminant validity, while a value of 0.7 to 0.8 suggests good discriminant validity, and 0.9 or above indicates excellent discriminant validity (Mandrekar, 2010). From this analysis, a cutoff score maximizing sensitivity for screening purposes in clinical settings was proposed.
Prior to recruitment, a power analysis was conducted using G*Power (Version 3.1) to determine the sample size required for this study. The analysis specified a large effect (Cohen’s d = 0.8) with 80% power for a test of mean differences between two independent groups. Results indicated that a total sample of 42 individuals (i.e., 21 individuals meting diagnostic criteria for specific phobia and 21 individuals not meeting diagnostic criteria for specific phobia, as determined by the DART) would be adequate for the purposes of this study. At the end of the data collection period, data was obtained from 33 individuals who met diagnostic criteria for specific phobia and 34 individuals who did not meet diagnostic criteria for specific phobia. Descriptive data for all administered measures are presented in Table 2.
Results
The SMSP demonstrated excellent internal consistency in the current sample (Cronbach’s α = 0.93). With respect to convergent validity, statistically significant correlations were observed between the SMSP and the hypothesized measure of distress (i.e., IIRS) as well as a measure of specific phobia (i.e., SPQ); however, correlations between the SMSP and other measures of phobia (i.e., FSS-II and PSRS) were not statistically significant. In terms of divergent validity, correlations between the SMSP and the DASS-21 depression, anxiety, and stress subscales were not statistically significant. See Table 3 for details.
In regard to criterion validity, total scores on the SMSP were higher for participants who met diagnostic criteria for specific phobia (M = 28.91; SD = 7.45) based on the outcome of the telephone interview compared to participants who did not meet criteria for specific phobia (M = 17.85; SD = 9.41). This difference was statistically significant (t(65) = 5.34; p < .001) and represented a large effect (d = 1.30). Bootstrap generated confidence intervals provided further support for a statistically meaningful group difference (95% CIs [6.50, 15.11]).
With respect to predictive validity, results of the binary logistic regression indicated that SMSP scores were a significant predictor of the presence or absence of specific phobia based on the outcome of the telephone interview. Compared to the SMSP, the proposed discriminant measure (i.e., DASS-21: Depression Subscale) did not confer any additional predictive utility for discriminating between individuals who did and did not meet diagnostic criteria for specific phobia (p = .67). See Table 4 for details.
The AUC of the SMSP was found to be a good predictor of the presence or absence of specific phobia (AUC = 0.82). Based on this analysis, a score of 22 would provide high sensitivity (88%) and adequate specificity (62%) and thus may be a useful cutoff score to be used in primary care and community settings.
Discussion
In this study, the construct and criterion validity of the SMSP were evaluated among a sample of Canadian adults from the general population. This was accomplished by examining the internal consistency of the SMSP and comparing scores on the SMSP to other measures of specific phobia, anxiety, depression, and distress while also examining the relationship between SMSP scores and the results of a semistructured telephone interview designed to assess the likely presence of specific phobia. Exploratory analyses were also conducted to examine the predictive utility of the SMSP.
As hypothesized, the internal consistency of the SMSP in the sample was excellent (Cronbach’s α = 0.93) and corresponds well with past literature assessing preliminary and translated versions of the measure (DeSousa et al., 2017; Lebeau et al., 2012; Möller & Bögels, 2016; Vidal-Arenas et al., 2021). Regarding convergent validity, statistically significant correlations were observed between the SMSP, SPQ and the IIRS as hypothesized. However, statistically significant correlations were not observed between the SMSP and either the FSS-II or PSRS; therefore, only partial support was provided for the convergent validity of the SMSP. Small and statistically non-significant correlations were observed between the SMSP and DASS-21, which provides support for the divergent validity of the SMSP.
There are several potential explanations for the statistically non-significant correlations observed between the SMSP and FSS-II and PSRS. For example, poor utility and validity have been reported for the FSS-II and PSRS as measures of specific phobia (Grös & Antony, 2006; McCabe & Antony, 2002). The FSS-II performs poorly when used to distinguish between individuals with or without specific phobia in clinical samples, and it has been suggested that the tool should be restructured to better correspond with related diagnostic criteria (Beck et al., 1998; Hood & Antony, 2012). Similarly, PSRS items are not well-aligned with DSM-5 specific phobia subtypes or diagnostic criteria (Hood & Antony, 2012). Additionally, the SMSP contains considerably fewer items (i.e., 10) than the other two measures (i.e., 46–51) and was developed to assess an individual’s cognitive and behavioural responses to one particular specific phobia. Conversely, the FSS-II and PSRS primarily measure the number of situations or objects that an individual may fear. The FSS-II and PSRS also do not have an indicated recall period, which may further account for the correlational values observed. Overall, while the aforementioned factors may have played a part in the correlational data observed in the present study, it is clear that further evaluation of the SMSP’s construct validity must be conducted in larger samples.
Regarding criterion validity, an independent samples t-test indicated that scores on the SMSP were significantly higher for participants who met diagnostic criteria for specific phobia during the telephone interview, compared to participants who did not. This observation corresponds well with previous evaluations of preliminary English and German versions of the SMSP, both of which determined that SMSP scores were significantly higher for respondents who met criteria for specific phobia as assessed by clinical assessment or other self-report tools (Knappe et al., 2013; Lebeau et al., 2012). A large, significant group difference in SMSP scores was reported in a previous study when compared to results of a diagnostic clinical interview assessing the presence of specific phobia conducted in a routine clinical setting (Schneider et al., 2021). Considering these previous data together with the large group differences observed in the current study, it appears that the SMSP possesses excellent criterion validity. A regression model based on the outcome of the telephone interview provided further evidence of the predictive utility of the SMSP, such that scores were found to be a significant predictor of whether participants met diagnostic criteria for specific phobia relative to scores on the proposed divergent measure (i.e., DASS-21 depression subscale). These results were also observed in a similar and recent study, which demonstrated strong predictive utility for the SMSP compared to the DASS-21: Depression Subscale based on results from a clinical interview (Schneider et al., 2021). Taken together, these results indicate that the SMSP is able to reliably differentiate between individuals with and without specific phobia, which provides support for the discriminant validity of the measure.
Results of the ROC analysis indicated that the AUC of the SMSP was a good predictor of whether participants met diagnostic criteria for specific phobia during the telephone interview. This is important, given that it has been recommended to establish clinical cutoff scores for the DSM-5 severity measures (Lebeau, 2015). In the current study, a SMSP score of 22 was generated as a potential cutoff score that could be used to screen respondents for a possible diagnosis of specific phobia. The specificity of this score is not optimal (62%), but the score has a high sensitivity (88%) and could be used to minimize the number of false negative results, which would be preferable when used in clinical settings for screening purposes (Akobeng, 2007).
This study had several strengths. Limited data is presently available regarding the psychometric properties of the SMSP, and even less research has been conducted to evaluate this scale individually and in samples where specific phobia is well-represented. To the authors’ knowledge, this study is the first to be conducted with the aim of evaluating the content and criterion validity of the English version of the SMSP and, as such, makes a valuable contribution to the literature. Further, the evaluation of the SMSP alongside a wider range of phobia measures and other measures of depression, anxiety, and distress has been called for in previous literature (Lebeau, 2015). The current study helps address this need by presenting novel correlations between the SMSP and the DASS-21, the IIRS, and the recently developed SPQ.
This study had several limitations. First, telephone interviews conducted for this study were administered by a psychology undergraduate student rather than a registered mental health professional. To mitigate this limitation, substantial training was provided by a registered doctoral-level psychologist who also provided ongoing support and supervision throughout the study. Further, the DART module utilized in the telephone interview was developed to be used by trainees as well as professionals. Still, future researchers may want to replicate these results with interviews conducted by a diverse range of registered mental health professionals (e.g., psychologists, social workers). Secondly, the eligibility of each participant in the sample could not be directly verified due to the online nature of the study. To maintain data integrity, survey entries were monitored for abnormal responses (i.e., duplicate entries and contradictory data) to demographic items throughout data collection. Third, participants were not assessed for the potential presence of additional mental disorders during the telephone interview and therefore symptoms reported by participants may have been better accounted for by another mental disorder. Fourth, the version of the SMSP as published in the DSM-5 relies on the respondent having encountered their phobic object or situation in the last seven days, which may have impacted estimates of criterion and construct validity in the current study (e.g., some participants may have scored lower on the SMSP than participants who had a recent exposure to their phobic stimulus). Outside of the context of this study however, the seven-day recall period may not pose a problem for the use of the SMSP in clinical settings, given that the tool was designed to monitor specific phobia severity over the course of treatment. Fifth, the majority of participants in the sample were women, university-educated, and of White European or Asian ethnocultural background. Additional research should be conducted in more diverse samples to provide more generalizable data regarding the psychometric properties and clinical utility of the SMSP. Finally, additional studies are required to confirm the utility of the average total score as a predictor of the severity of specific phobia symptoms and examine cut off scores for the SMSP in clinical, treatment-seeking samples. In addition, there is a need for further examination of the test-retest reliability and factor structure of the SMSP, as stated in previous literature (Knappe et al., 2014; Lebeau et al., 2012; Vidal-Arenas et al., 2021).
Conclusions
The results presented in this study provide preliminary support for the psychometric properties of the SMSP. The SMSP demonstrated excellent internal consistency. Evidence of excellent criterion validity was also observed, such that SMSP scores were significantly higher for participants who met diagnostic criteria for specific phobia during the telephone interview compared to participants who did not. Furthermore, SMSP scores uniquely predicted the presence or absence of a specific phobia according to the results of the telephone interview. Good convergent and divergent validity was also found between the SMSP, a related measure of phobia, and measures of distress, anxiety, and depression. However, additional correlational data presented in this study warrant further research into the construct validity of the SMSP. Additional assessment of the SMSP should be conducted in larger and more diverse samples, and in clinical populations. Overall, results indicate that the SMSP is a useful and valid measure of the severity of specific phobia symptoms.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Akobeng, A. K. (2007). Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatrica, 96(5), 644–647. https://doi.org/10.1111/j.1651-2227.2006.00178.x
Akoglu, H. (2018). User’s guide to correlation coefficients. Turkish journal of emergency medicine, 18(3), 91–93. https://doi.org/10.1016/j.tjem.2018.08.001
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders. (4th ed.). https://dsm.psychiatryonline.org/doi/pdf/10.1176/appi.books.9780890420614.dsm-iv
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Antony, M. M., Bieling, P. J., Cox, B. J., Enns, M. W., & Swinson, R. P. (1998). Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment, 10(2), 176. https://doi.org/10.1037/1040-3590.10.2.176
Bandelow, B., & Michaelis, S. (2015). Epidemiology of anxiety disorders in the 21st century. Dialogues in clinical neuroscience, 17(3), 327. https://doi.org/10.31887/DCNS.2015.17.3/bbandelow
Beck, J. G., Carmin, C. N., & Henninger, N. J. (1998). The utility of the Fear Survey Schedule-III: An extended replication. Journal of Anxiety Disorders, 12(3), 177–182. https://doi.org/10.1016/S0887-6185(98)00007-3
Beesdo-Baum, K., Klotsche, J., Knappe, S., Craske, M. G., LeBeau, R. T., Hoyer, J. … Wittchen, H. U. (2012). Psychometric properties of the dimensional anxiety scales for DSM‐V in an unselected sample of German treatment seeking patients. Depression and Anxiety, 29(12), 1014–1024. https://doi.org/10.1002/da.21994
Craske, M., Wittchen, U., Bogels, S., Stein, M., Andrews, G., & Lebeu, R. (2013). Severity Measure for Specific Phobia Adult. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM5_Severity-Measure-For-Specific-Phobia-Adult.pdf
Cutshall, C., & Watson, D. (2004). The phobic stimuli response scales: A new self-report measure of fear. Behaviour Research and Therapy, 42(10), 1193–1201. https://doi.org/10.1016/j.brat.2003.08.003
DeSousa, D. A., Moreno, A. L., Osório, F. L., Crippa, J. A. S., LeBeau, R., Manfro, G. G. … Koller, S. H. (2017). Psychometric properties of the dimensional anxiety scales for DSM-5 in a Brazilian community sample. International Journal of Methods in Psychiatric Research, 26(3), e1531. https://doi.org/10.1002/mpr.1531
Devins, G. M. (2010). Using the illness intrusiveness ratings scale to understand health-related quality of life in chronic disease. Journal of Psychosomatic Research, 68(6), 591–602. https://doi.org/10.1016/j.jpsychores.2009.05.006
Eaton, W. W., Bienvenu, O. J., & Miloyan, B. (2018). Specific phobias. The Lancet Psychiatry, 5(8), 678–686. https://doi.org/10.1016/S2215-0366(18)30169-X
Fairbrother, N., & Antony, M. M. (2012). Specific Phobia Questionnaire. Unpublished scale
Geer, J. H. (1965). The development of a scale to measure fear. Behaviour Research and Therapy, 3(1), 45–53
Grös, D. F., & Antony, M. M. (2006). The assessment and treatment of specific phobias: a review. Current Psychiatry Reports, 8(4), 298–303. https://doi.org/10.1007/s11920-006-0066-3
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap): A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Haug, T., Berntzen, D., Götestam, K. G., Brenne, L., Johnsen, B. H., & Hugdahl, K. (1987). A three-systems
analysis of fear of flying: A comparison of a consonant vs a non-consonant treatment method.Behaviour Research and Therapy, 25(3),187–194. https://doi.org/10.1016/0005-7967(87)90045-3
Hood, H. K., & Antony, M. M. (2012). Evidence-based assessment and treatment of specific phobias in adults. In T. E. Davis III, T. H. Ollendick, & L. G. Öst (Eds.), Intensive one-session treatment of specific phobias (pp. 19–42). Springer. https://doi.org/10.1007/978-1-4614-3253-1_2
Knappe, S., Klotsche, J., Heyde, F., Hiob, S., Siegert, J., Hoyer, J. … Wittchen, H. U. (2014). Test–retest reliability and sensitivity to change of the dimensional anxiety scales for DSM-5. CNS Spectrums, 19(3), 256–267. https://doi.org/10.1017/S1092852913000710
Knappe, S., Klotsche, J., Strobel, A., LeBeau, R., Craske, M., Wittchen, H. U., & Beesdo-Baum, K. (2013). Dimensional anxiety scales for DSM-5: sensitivity to clinical severity. European Psychiatry, 28(7), 448–456. https://doi.org/10.1016/j.eurpsy.2013.02.001
LeBeau, R., Bögels, S., Möller, E., & Craske, M. (2015). Integrating dimensional assessment and categorical diagnosis in DSM-5: The benefits and challenges of the paradigm shift for the anxiety disorders. Psychopathology Review, 2(1), 83–99. https://doi.org/10.5127/pr.036414
Lebeau, R. T., Glenn, D. E., Hanover, L. N., Beesdo-Baum, K., Wittchen, H. U., & Craske, M. G. (2012). A dimensional approach to measuring anxiety for DSM‐5. International Journal of Methods in Psychiatric Research, 21(4), 258–272. https://doi.org/10.1002/mprt.1369
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. https://doi.org/10.1016/0005-7967(94)00075-u
Mandrekar, J. N. (2010). Receiver operating characteristic curve in diagnostic test assessment
Journal of Thoracic Oncology, 5(9), 1315–1316. https://doi.org/10.1097/JTO.0b013e3181ec173d
Möller, E. L., & Bögels, S. M. (2016). The DSM-5 Dimensional Anxiety Scales in a Dutch non‐clinical sample: Psychometric properties including the adult separation anxiety disorder scale. International Journal of Methods in Psychiatric Research, 25(3), 232–239. https://doi.org/10.1002/mpr.1515
Stouthard, M. E. A., Mellenbergh, G. J., & Hoogstraten, J. (1993). Assessment of dental anxiety:
A facet approach.Anxiety, Stress and Coping, 6,89–105. https://doi.org/10.1080/10615809308248372
Szymanski, J., & O’Donohue, W. (1995). Fear of Spiders Questionnaire. Journal of Behavior Therapy and Experimental, & Psychiatry, 26(1),31–34. https://doi.org/10.1016/0005-7916(94)00072T
Vidal-Arenas, V., Ortet-Walker, J., Ibáñez, M. I., Ortet, G., & Mezquita, L. (2021). Self-reported DSM-5 Anxiety Severity Measures: Evidence of validity and reliability in Spanish youths. Psicothema, 33(2), 312–319. https://doi.org/10.7334/psicothema2020.398
Wardenaar, K. J., Lim, C. C., Al-Hamzawi, A. O., Alonso, J., Andrade, L. H., Benjet, C. … Florescu, S. E. (2017). The cross-national epidemiology of specific phobia in the World Mental Health Surveys. Psychological Medicine, 47(10), 1744. https://doi.org/10.1017/S0033291717000174
Witthauer, C., Ajdacic-Gross, V., Meyer, A. H., Vollenweider, P., Waeber, G., Preisig, M., & Lieb, R. (2016). Associations of specific phobia and its subtypes with physical diseases: an adult community study. BMC Psychiatry, 16(1), 155. https://doi.org/10.1186/s12888-016-0863-0
Wolitzky-Taylor, K. B., Horowitz, J. D., Powers, M. B., & Telch, M. J. (2008). Psychological approaches in the treatment of specific phobias: A meta-analysis. Clinical Psychology Review, 28(6), 1021–1037. https://doi.org/10.1016/j.cpr.2008.02.007
McCabe, R. E., Milosevic, I., Rowa, K., Shnaider, P., Pawluk, E. J., Antony, M. M., & the DART Working Group. (2017). Diagnostic Assessment Research Tool (DART). St. Joseph’s Healthcare/McMaster University.
McCabe, R. E. & Antony, M. M. (2002). Specific and social phobia. In M. M. Antony & D. H. Barlow (Eds.), Handbook of assessment and treatment planning for psychological disorders (1st ed., pp. 113–146). Guilford Press.
Ovanessian, M. M., Fairbrother, N., Vorstenbosch, V., McCabe, R. E., Rowa, K., & Antony, M. M. (2019). Psychometric properties and clinical utility of the Specific Phobia Questionnaire in an anxiety disorders sample. Journal of Psychopathology and Behavioral Assessment, 41(1), 36–52. https://doi.org/10.1007/s10862-018-9687-1.
Schneider, L. H., Pawluk, E. J., Milosevic, I., Shnaider, P., Rowa, K., Antony, M. M., Musielak, N., & McCabe, R. E. (2021). The diagnostic assessment research tool in action: A preliminary evaluation of a semistructured diagnostic interview for DSM-5 disorders. Psychological Assessment. https://doi.org/10.1037/pas0001059.
Funding
This work was supported by the Anxiety Treatment and Research Clinic, St. Joseph’s Healthcare, Hamilton.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Hamilton Integrated Research Ethics Board (Project #12,615).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
All participants provided informed consent regarding publishing the findings of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
MacLeod, S., Schneider, L.H. & McCabe, R.E. Investigating the Psychometric Properties of the Severity Measure for Specific Phobia. J Psychopathol Behav Assess 44, 826–835 (2022). https://doi.org/10.1007/s10862-022-09976-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-022-09976-6