Abstract
We tested the effectiveness of Brief Behavioral Activation Treatment for Depression-Revised (BATD-R), and its impact on secondary outcomes: anxiety, dysfunctional attitudes, and mindfulness. It was expected that individuals who completed BATD-R would exhibit decreased depression, anxiety, and dysfunctional attitudes, as well as increased mindfulness. A sample of adults with depression (n = 42) was recruited to complete the 10-week treatment. A healthy control group (n = 38) was included for comparison. Outcomes (depression, anxiety, dysfunctional attitudes, and mindfulness) were assessed at pre-treatment, post-treatment or 10 weeks for the healthy control group, and three-month follow-up. At pre-treatment, the clinical group reported greater depression, anxiety, and dysfunctional attitudes, and less mindfulness than the healthy control group. At post-treatment, the clinical group reported decreased depressive symptoms, trait anxiety, and dysfunctional attitudes, and increased mindfulness, compared to pre-treatment. The control group did not exhibit changes across the 10 weeks. Clinical and healthy control group post-treatment scores did not differ. At three-month follow-up, the clinical group reported a slight increase in depressive symptoms from post-treatment, but still maintained lower depressive symptoms than pre-treatment. The clinical group maintained treatment gains in dysfunctional attitudes, and mindfulness. Results support the effectiveness of BATD-R and suggest BATD-R may influence dysfunctional attitudes and mindfulness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Randomized control trials (RCTs) have demonstrated that Brief Behavioral Activation Treatment for Depression (BATD; Lejuez et al., 2001) is an efficacious therapy for depression (e.g., Hopko et al., 2003, 2011). However, these RCTs have primarily focused on specific populations, such as adult inpatients and breast cancer patients. As such, evidence for the effectiveness of BATD in the general population is scant, with only one study to date having demonstrated effectiveness of this treatment in a small sample of Swedish individuals (N = 8; Freij & Masri, 2008). Additionally, relatively little is known about the broader effects of BATD on psychological functioning. Some research suggests that BATD may reduce anxiety (Hopko et al., 2004, 2006, 2016), though findings are inconsistent (Hopko et al., 2005). Considerable empirical work has identified dysfunctional attitudes and mindfulness as risk and protective factors for depression (e.g., Abela, 2001; Ford & Shook, 2019), and both may be linked to BATD. One study found that behavioral activation decreased dysfunctional attitudes (Jacobson et al., 1996), and conceptually BATD may encourage mindfulness. However, these associations have yet to fully tested.. Thus, the purpose of the current study was to build upon the existing empirical evidence for BATD by testing the effectiveness of a 10-week version of BATD (i.e., BATD-Revised; Lejuez et al., 2011) among a non-specific community population and to determine the effects of BATD-R on anxiety, dysfunctional attitudes, and mindfulness.
Brief Behavioral Activation Treatment for Depression
BATD (Lejuez et al., 2001) and BATD-Revised (BATD-R; Lejuez et al., 2011) are relatively short (12 and 10 sessions, respectively), manualized, evidence-based behavioral treatments for depression. Both treatments use the conceptualization of depression derived from functional contextualism and Herrnstein’s Matching Law (1970). Specifically, depression is thought to arise from the individual receiving greater reinforcement for depressive behaviors (e.g., avoiding social activities) and less reinforcement for non-depressive behaviors (e.g., engaging in social activities). BATD is designed to systematically change the ratio of reinforcement for depressive to non-depressive behaviors. Individuals schedule and engage in values-based activities, increasing opportunity for reinforcement of non-depressed behavior (Kanter et al., 2010). Research supports the efficacy of BATD in treating depressive symptoms among inpatients and cancer patients (Hopko et al., 2005, 2013; Ryba et al., 2014; Snarski et al., 2011).
BATD-R reflects a streamlined treatment protocol with an increased emphasis on the treatment rationale, simplified treatment forms, and enhanced procedural details for providers (Lejuez et al., 2011). Sessions 1–3 discuss the behavioral conceptualization of depression and treatment rationale, introduce self-monitoring of daily activities, and begin identifying activities that align with the individual’s values. In Session 4, the individual works with the therapist to schedule a few easily achievable activities. Activity scheduling is completed each week following Session 4, with activities increasing in frequency and difficulty as treatment progresses. In Sessions 5 and 6, the individual creates behavioral contracts with significant people in their lives for support in treatment. During Sessions 7 and 8, the life areas, values, and activities are reviewed and edited. Behavioral contracts are reviewed and edited in Session 9. In Session 10, completed daily self-monitoring forms are reviewed in order to examine the individual’s progress and suggestions are made about what to do in case symptoms return.
To date, only two studies have assessed the efficacy of BATD-R, with one being a pilot study (Collado et al., 2014) that informed the other (Collado et al., 2016). These researchers found that BATD-R significantly reduced depression in clinically depressed Spanish-speaking Latinx community members, and in both studies, clinical gains were sustained from the conclusion of treatment to the one-month follow-up. Of note, adaptations of BATD-R have resulted in significantly reduced depression in inner-city illicit drug users (Daughters et al., 2008) and smokers (MacPherson et al., 2010). Although findings from these RCTs are promising, more work is needed to demonstrate the robustness of these effects and the utility of BATD-R in non-specific populations. Understanding the effectiveness of BATD-R among a broader community sample would extend the external validity of the treatment (Rothwell, 2005), providing clinicians with greater means to make informed clinical judgments regarding treatment of depression among diverse patient populations. Furthermore, as depression can be both an acute and chronic condition (Monroe & Harkness, 2011), it also becomes important to examine whether BATD-R contributes to the maintenance of clinical gains beyond a one-month follow-up.
BATD and Anxiety
Beyond reducing depression, there is some evidence that BATD may also reduce anxiety (Armento & Hopko, 2009; Hopko et al., 2004). Behavioral activation encourages individuals to increase their engagement in reinforcing behaviors and activities while simultaneously extinguishing avoidant behaviors (Judah et al., 2020). Given that avoidance behavior is a central feature of anxiety (e.g., Barlow, 2002), increasing engagement might have important implications for anxiety (Judah et al., 2020). As such, it is reasonable to expect that BATD would reduce symptoms of anxiety and depression. However, the research on the relation between BATD and anxiety is limited in its generalizability (Armento & Hopko, 2009; Gawrysiak et al., 2009; Hopko et al., 2004; Tull et al., 2018). Moreover, some of the findings indicate that BATD may not affect anxiety (Hopko et al., 2005; McIndoo et al., 2016; Tull et al., 2019). Only one study to date has examined the effects of BATD-R on anxiety (Hopko et al., 2016), finding reductions in anxiety among a sample of breast cancer patients. Thus, the literature examining the effect of BATD on anxiety is inconsistent, and very little is known about the effects of BATD-R on anxiety.
BATD and Dysfunctional Attitudes
Cognitive behavioral theories of depression assert that depressed individuals possess dysfunctional attitudes, or maladaptive rules and expectations concerning one’s self-worth, which play a substantial role in the etiology and maintenance of depression (Abramson et al., 1989; Beck, 2008). Accordingly, individuals prone to depression develop negative self-schemata, which in turn result in automatic, negative thoughts about the self, the world, and the future. There is a sizable literature of prospective studies demonstrating that higher levels of dysfunctional attitudes predict subsequent depression (e.g., Abela, 2001; Dykman & Johll, 1998; Just & Alloy, 1997).
BATD may affect dysfunctional attitudes by addressing the context and function of negative cognitions (Jacobson et al., 2001). Contrary to traditional cognitive therapy which focuses on challenging the content of negative attitudes, BATD helps individuals understand how behavior, attitudes, and emotion affect one another while also teaching how values-based activities can improve mood. Over the course of treatment, individuals might come to understand how negative attitudes about oneself reduce engagement in values-based activities and perpetuate depression. Engaging in values-based activities may also prompt individuals to adopt positive attitudes that counter dysfunctional attitudes. In fact, Jacobson et al. (1996) found that a general behavioral activation treatment condition was as effective as cognitive therapy at altering dysfunctional attributional style, and that changes in dysfunctional attitudes were more likely to be followed by decreased depression in behavioral activation therapy than in cognitive therapy. Taken together, BATD-R may reduce dysfunctional attitudes despite a lack of formal cognitive training. However, no studies have tested whether BATD-R reduces dysfunctional attitudes, conceptually replicating prior findings (Jacobson et al., 1996).
BATD and Mindfulness
Mindfulness is a sustained, receptive attention to and awareness of internal and external experiences as they occur (Brown & Ryan, 2003). Mindfulness is conceptualized as both a state of consciousness, as well as a dispositional trait. State mindfulness can be cultivated through practice, and with time and repetition, one’s ability and propensity to be mindful on a regular basis increases (i.e., trait mindfulness; Garland et al., 2010). Considerable research has linked trait mindfulness with lower levels of depression (e.g., Ford & Shook, 2019; Kiken & Shook, 2011, 2012), and mindfulness-based interventions generally reduce depression (e.g., Hofmann et al., 2010).
Components of BATD may encourage mindfulness. Indeed, researchers draw parallels between behavioral activation and mindfulness, positing that behavioral activation counters depressive, experiential avoidance behaviors by encouraging focus on present activities (Kanter et al., 2006; Martell & Kanter, 2011). The emphasis on values and engagement in daily activities may increase awareness of the present moment (Jacobson et al., 2001). As individuals track activities, learn and clarify values (i.e., through the life areas, values, and activities inventory), and schedule values-based important and enjoyable activities, mindfulness may be increased through daily attention to the present moment across 10 weeks. Therefore, it is possible that BATD-R increases mindfulness without providing specific training in mindfulness skills. To date, no studies have tested whether BATD-R increases mindfulness.
Present Study
The goals of the present study were to replicate and extend the empirical basis for BATD among a non-specific community sample by: (1) providing more robust evidence for the effectiveness of BATD-R in reducing depression; and (2) testing the broader effects of BATD-R on psychological well-being. Specifically, we tested whether BATD-R affected depression, anxiety, dysfunctional attitudes, and mindfulness in a group of community adults with major depressive disorder or dysthymic disorder, compared to a healthy control group who did not receive treatment. A healthy control group was included to assess the stability of depression, anxiety, dysfunctional attitudes, and mindfulness. The healthy control group was also necessary to obtain indices reflecting the extent to which a non-clinical sample from the same community as the clinical group would endorse depressive symptoms to allow for investigation of clinically meaningful change. We predicted that the clinical group would report less depression, less anxiety, less dysfunctional attitudes, and greater mindfulness at post-treatment and three-month follow up relative to pre-treatment. We expected no significant changes in depression, anxiety, dysfunctional attitudes, or mindfulness across the three time points in the healthy control group.
Method
Participants
Sample size was determined by a power analysis with a medium to large effect size and α = 0.05 (Cohen, 1992), and a total of 99 individuals were recruited from a small-medium sized city in the south-Atlantic region of the U.S. To participate, individuals had to be 18 years or older and fluent in English. Participants were recruited through flyers and online advertisements. Participants in the clinical group were also recruited through referrals from psychological service centers at a large public university. All participants were assessed with an electronic version of the Structured Clinical Interview for the DSM-IV (netSCID; First et al., 1997) to confirm their eligibility to participate. Clinical group participants met criteria for major depressive disorder (MDD) or dysthymic disorder and were not currently receiving other forms of psychotherapy.Footnote 1 Exclusion criteria for the clinical group were psychosis, substance dependence, active mania, and suicidal thoughts. For the healthy control group, exclusion criteria were any current diagnoses of depression or other psychological disorders, developmental disorders, or cognitive impairment.
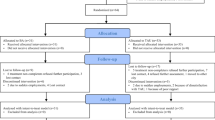
A total of 80 participants met inclusion/exclusion criteria and completed the pre-treatment assessment (see Fig. 1 for a Consort Diagram). There were 42 in the clinical group (54.8% female; Mage = 27.1, SD = 11.7; 83.3% White; Mdneducation = Some college (but no degree); Mdnincome = $20,000—$39,999), and 38 in the healthy control group (50.0% female; Mage = 29.8, SD = 14.9; 89.5% White; Mdneducation = Associate’s degree or equivalent; Mdnincome = $60,000—$79,999; see Supplemental Material for more detailed demographic information). Fifty-two participants completed the post-treatment assessment (35% attrition rate). Twenty-one participants were in the clinical group (52.4% female; Mage = 26.6, SD = 12.0; 76.2% White; Mdneducation = Some college (but no degree); Mdnincome = $20,000—$39,999), and 31 were in the healthy control group (45.2% female; Mage = 31.6, SD = 16.0; 90.3% White; Mdneducation = Associate’s degree or equivalent; Mdnincome = $60,000—$79,999). Thirty-six participants completed a 3-month follow-up assessment (30.9% attrition rate). Fourteen participants were in the clinical group (35.7% female; Mage = 26.9, SD = 11.8; 71.4% White; Mdneducation = Associate's degree or equivalent; Mdnincome = between $20,000—$39,999 and $40,000—$59,999), and 22 were in the healthy control group (50% female; Mage = 29.7, SD = 14.8; 90.9% White; Mdneducation = Some college (but no degree); Mdnincome = $60,000—$79,999).
Demographic characteristics did not differ between the clinical and healthy control groups at pre-treatment, post-treatment, or 3-month follow-up (ps > 0.10). Attrition rates from pre-treatment to post-treatment assessments significantly differed between the two groups, χ2(1, N = 80) = 7.61, p = 0.01. There was greater attrition in the clinical group (50%) than the healthy control group (18.4%). Attrition rates from post-treatment to three-month follow-up assessments did not significantly differ between the two groups, χ2(1, N = 52) = 0.11, p = 0.74.
Measures
Beck Depression Inventory-II (BDI-II; Beck et al., 1996)
The BDI-II is a 21-item measure of depressive symptoms. Participants select the statement that best describes the way they have felt during the past two weeks. For example, one item asks participants to describe how much they have felt sadness. Participants choose either 0 (I do not feel sad), 1 (I feel sad much of the time), 2 (I am sad all of the time), or 3 (I am so sad or unhappy that I can’t stand it). Scores are summed to create a total score (range = 0–63). Higher scores indicate greater depressive symptoms (αs = 0.81 – 0.95).
Clinical significance was assessed by calculating a cutoff point and reliable change index (RCI; Seggar et al., 2002). The cutoff point determines whether changes in scores are large enough to move subjects out of one sample’s (i.e., clinical group) distribution and into another sample’s (i.e., healthy control group) distribution. The RCI assesses whether the magnitude of change is statistically reliable (Jacobson & Truax, 1992). If the RCI is greater than 1.96, then the change is considered to be reliable and unlikely to be due to measurement error. Of note, for change after treatment to be considered clinically significant, post-treatment (or follow-up) scores must be below the cutoff point and have an RCI greater than 1.96.
Dysfunctional Attitude Scale (DAS; Weissman & Beck, 1978)
The DAS is a 64-item measure of pervasive negative attitudes toward the self, outside world, and future. Participants rate how well each statement describes how they think (e.g., If others dislike you, you cannot be happy) on a scale from 1 (Totally agree) to 7 (Totally disagree). Responses are reverse-scored and averaged. Higher scores indicate greater dysfunctional attitudes (αs = 0.93 – 0.96).
Mindful Attention Awareness Scale (MAAS; Brown & Ryan, 2003)
The MAAS is a 15-item measure of trait mindfulness. We used an abbreviated, 11-item version (Shook et al., 2017). Participants rate their present-moment orientated attention to and awareness of everyday experiences (e.g., I rush through activities without being really attentive to them) on a scale from 1 (Almost always) to 6 (Almost never). Scores are summed (range = 11–66), such that higher scores indicate higher levels of trait mindfulness (αs = 0.69 – 0.88).
Beck Anxiety Inventory (BAI; Beck et al., 1988)
The BAI is a 21-item measure of somatic anxiety symptoms (Julian, 2011). Participants rate the extent to which they have been bothered by symptoms of anxiety during the past week (e.g., Numbness or tingling) on a scale from 0 (Not at all) to 3 (Severely; I could barely stand it). Scores are summed (range = 0–63). Higher scores indicate greater anxiety symptoms (αs = 0.77 – 0.98).
State-Trait Anxiety Inventory (STAI; Spielberger, 1983)
The STAI consists of 20 items that assess trait anxiety and 20 items that assess state anxiety. Given our interests in the effects of BATD-R on trait anxiety, only the STAI-Trait scale was examined. Participants rate the extent to which each item (e.g., I worry too much over something that really doesn’t matter) describes themselves in general on a scale from 1 (Not at All) to 4 (Very Much So). Scores are averaged, such that higher scores are indicative of greater trait anxiety (αs = 0.86 – 0.91).
Procedure
Study procedures were approved by the last author’s Institutional Review Board, and data were collected between 2013 and 2016. Individuals interested in the study completed a brief screening via phone or email to check inclusion/exclusion criteria. For those who met the initial screening, an in-person clinical screening was scheduled. Participants met a researcher (trained clinical psychology graduate students under the supervision of a licensed psychologist) at a psychological service center located at a large public university. Participants were seated in a private room and provided informed consent. The netSCID (First et al., 1997) was administered to ensure that individuals met inclusion/exclusion criteria for their respective group (i.e., clinical or healthy control). Eligible individuals were invited to complete the pre-treatment assessment, which consisted of a computer task and several self-report measures on a laptop computer. After completing the pre-treatment measures, all participants were paid $20.
Within a week of completing the pre-treatment, participants in the clinical group began the manualized treatment for depression free of charge with a clinical doctoral student other than the pre-assessment researcher. Each treatment session was held at the psychological service center and video recorded with participants’ consent. Therapists delivered 10 weekly one-hour treatment sessions in accordance with the BATD-R manual (Lejuez et al., 2011). A treatment integrity checklist was used by the therapists.
Upon completion of the last treatment session, the clinical group immediately completed the post-treatment assessment, which included the same pre-treatment assessment measures. The healthy control group returned to the psychological service center approximately 10 weeks after the pre-treatment session to complete the assessment measures a second time. After completing the post-treatment measures, all participants were paid $20. Three months later, all participants returned to the psychological service center to complete the assessment measures for a third time. Participants were paid $30 for the 3-month follow-up. The healthy control group completed measures on the same timeline as the clinical group to ensure that any changes in scores were due to treatment and not an artifact of repeated exposure to the measures.
Treatment Fidelity
Treatment fidelity was assessed based on established recommendations for study design, training of interventionists, treatment delivery, treatment receipt, and utilization of treatment skills (Bellg et al., 2004). Interventionists were clinical psychology doctoral students with at least one year of clinical experience. Interventionists received training on BATD-R and shadowed an experienced staff member in providing live BATD-R treatment. Weekly supervision was provided by a licensed clinical psychologist. To assess treatment integrity post hoc, an independent clinician, who was not previously involved in the study, randomly selected and reviewed 10 videotapes (i.e., one for each of the 10 BATD-R sessions). Twenty percent of these videotapes were independently reviewed by the study’s licensed clinical psychologist; no substantial differences were noted between these reviews. Across the 10 reviewed sessions, 89.2% of key elements were covered in sessions, with six of the sessions reflecting 100% adherence. Only one session was below 75% adherence due to issues in the patient’s functioning that necessitated clinical intervention. Homework assignment adherence by patients averaged 66.7% across the 10 sessions, with four of the sessions at 100% adherence. The BATD-R treatment sessions were also evaluated to determine whether components of CBT or mindfulness were incorporated into any sessions. We wanted to ensure that treatment sessions were differentiated from CBT and mindfulness. None of the sessions involved content that overlapped with these other approaches. Overall, treatment integrity was verified and determined to be consistent with recommendations (Bellg et al., 2004).
Results
BATD-R Effectiveness
To test the effectiveness of BATD-R, a 3 (Time: pre-treatment, post-treatment, and follow-up) × 2 (Group: control or clinical) mixed-factorial ANOVA was conducted on depression scores.Footnote 2 Time was a within-subjects variable, and group was a between-subjects variable. There was a significant main effect of time on depressive symptoms (F(2,68) = 10.83, p < 0.001, ηp2 = 0.24). Post hoc comparisons revealed that participants exhibited the highest levels of depression at pre-treatment compared to post-treatment and follow-up (ps < 0.01), and depression scores did not differ between post-treatment and follow-up (p = 0.14). There was a significant main effect of group on depressive symptoms (F(1,34) = 24.16, p < 0.001, ηp2 = 0.42). Participants in the clinical group reported higher levels of depression than those in the healthy control group. Finally, there was a significant Time x Group interaction (see Table 1). Simple main effects analyses indicated that participants in the clinical group reported lower levels of depression at post-treatment and follow-up as compared to their pre-treatment scores (ps < 0.01). Participants in the clinical group exhibited a slight increase in depressive symptoms from post-treatment to follow-up (p = 0.03). Participants in the control group did not exhibit any change in depression levels across time (ps > 0.20). Of note, the clinical group exhibited greater depressive symptoms than the healthy control group at pre-treatment (p < 0.001), but the two groups did not significantly differ in depressive symptoms at post-treatment (p = 0.45). At 3-month follow-up, the clinical group reported more depressive symptoms than the healthy control group (p = 0.02).
Clinical significance was assessed by calculating a cutoff point and RCIs (Seggar et al., 2002). For change after treatment to be considered clinically significant, post-treatment (or follow-up) scores must be below the cutoff point and have an RCI greater than 1.96. The clinical cutoff point was calculated to be 11.71 based on the means and standard deviations of the clinical group and healthy control group. The RCI for the change in scores from pre-treatment to post-treatment was 3.02. Given that the clinical group had a mean score of 8.79 at post-treatment and an RCI greater than 1.96, change is considered to be clinically significant. From pre-treatment to follow-up, the RCI for the change in scores was 2.08, which is also greater than 1.96. However, given that the clinical group had a mean score of 13.79 at follow-up, it can only be concluded that they reliably improved from pre-treatment to follow-up.
Intent-to-Treat Analyses
Given participant attrition over the three assessment points, intent-to-treat analyses were conducted.Footnote 3 Pre-treatment scores for participants who prematurely terminated treatment or failed to complete post-treatment measures were carried forward and used as post-treatment and 3-month follow-up scores. Post-treatment scores for participants who failed to attend the 3-month follow-up were carried forward and used as follow-up scores. Patterns of results regarding main effects were similar to those of the original analysis (ps < 0.01; see Supplemental Material). There was also a significant interaction effect between time and group (F(1.83,142.80) = 15.83, p < 0.001, ηp2 = 0.17), which largely replicated that of the original analysis (see Table 2). There were only two exceptions to this finding, namely, post-treatment effects for the clinical group were maintained through follow-up (p = 0.07), and the clinical group exhibited greater depressive symptoms than the control group across all assessments (ps < 0.001).
Broader Effects of BATD-R
To determine whether BATD-R led to changes in anxiety, dysfunctional attitudes, or mindfulness, a series of 3 (Time: pre-treatment, post-treatment, and follow-up) × 2 (Group: control or clinical) mixed-factorial ANOVAs were conducted. There was a significant main effect of time on STAI-Trait scores (F(2,68) = 9.42, p < 0.001, ηp2 = 0.22) and dysfunctional attitudes (F(2,68) = 12.08, p < 0.001, ηp2 = 0.26). Post hoc comparisons revealed that participants exhibited the poorest psychological functioning at pre-treatment compared to post-treatment and follow-up (ps < 0.01), and psychological functioning did not differ between post-treatment and follow-up (ps > 0.13). The main effect of time was not significant for mindfulness (F(1.84,62.68) = 3.21, p = 0.05, ηp2 = 0.09) or BAI scores (F(1.13,38.30) = 0.64, p = 0.45, ηp2 = 0.02). There was a significant main effect of group on BAI (F(1,34) = 12.20, p = 0.001, ηp2 = 0.26), STAI-Trait (F(1,34) = 12.09, p = 0.001, ηp2 = 0.26), and dysfunctional attitudes (F(1,34) = 12.33, p = 0.001, ηp2 = 0.27). Post hoc comparisons indicated that the clinical group reported poorer psychological functioning than the healthy control group (ps ≤ 0.001). The main effect of group on mindfulness was not significant (F(1,34) = 0.44, p = 0.51, ηp2 = 0.01).
Many of these main effects were qualified by significant Time x Group interactions (see Table 1). Specifically, significant interactions were found for STAI-Trait, dysfunctional attitudes, and mindfulness. Each interaction was decomposed, and simple main effects analyses indicated that participants in the clinical group reported more positive psychological functioning at post-treatment and follow-up as compared to their pre-treatment scores (ps < 0.01). Participants in the clinical group did not exhibit any significant change in STAI-Trait scores, dysfunctional attitudes, and mindfulness from post-treatment to follow-up (ps > 0.20). Participants in the healthy control group did not exhibit any change in psychological functioning across time (ps > 0.08). Of note, the two groups differed in psychological functioning at pre-treatment, such that the clinical group exhibited greater STAI-Trait levels and dysfunctional attitudes, as well as less mindfulness than the healthy control group (ps < 0.05). At post-treatment, the two groups did not significantly differ in STAI-Trait, dysfunctional attitudes, or mindfulness (ps > 0.13). STAI-Trait and mindfulness did not differ between groups at follow-up (ps > 0.06), but the clinical group did report more dysfunctional attitudes than the healthy control group at follow-up (ps < 0.05).
Given the comorbidity between anxiety and depression (Brown et al., 1998), we reran the 3 (Time: pre-treatment, post-treatment, and follow-up) × 2 (Group: control or clinical) ANOVAs with both anxiety measures as outcomes, controlling for depressive symptoms. When BAI was the outcome, the main effects of time (F(1.12,37.01) = 0.06, p = 0.84, ηp2 = 0.002) and group (F(1,33) = 0.44, p = 0.51, ηp2 = 0.01), as well as the Time x Group interaction (F(1.12,37.01) = 0.29, p = 0.62, ηp2 = 0.01), were not significant. Similarly, when STAI-Trait was the outcome, the main effects of time (F(2,66) = 1.03, p = 0.36, ηp2 = 0.03) and group (F(1,33) = 0.003, p = 0.96, ηp2 = 0.00), as well as the Time x Group interaction (F(2,66) = 2.32, p = 0.11, ηp2 = 0.07), were not significant.
Intent-to-Treat Analyses
Given participant attrition over the three assessment points, intent-to-treat analyses were conducted, carrying forward previous scores. Patterns of results regarding main effects replicated those of the original analyses (ps ≤ 0.02; see Supplemental Material). Patterns of results regarding interaction effects for the intent-to-treat analyses generally paralleled those of the original findings (see Table 2). There were four exceptions. First, a significant Time x Group interaction emerged for BAI scores (F(1.39,108.28) = 3.65, p = 0.028, ηp2 = 0.05). Pre-treatment BAI scores for the clinical group were higher than post-treatment scores (p < 0.001), but their pre-treatment scores did not differ from follow-up scores (p = 0.30). Post-treatment BAI effects for the clinical group were maintained through follow-up (p = 0.19). Second, the healthy control group exhibited a significant decrease in mindfulness from pre-treatment to post-treatment (p = 0.02). Third, at pre-treatment, the clinical group exhibited greater anxiety as measured by the BAI than the healthy control group (p < 0.001). Fourth, the healthy control group demonstrated more positive psychological functioning than the clinical group at post-treatment (ps < 0.01) and follow-up (ps < 0.01) across all variables, except mindfulness (ps = 0.41 & 0.34, respectively).
Again, we reran the ANOVAs with anxiety as the outcome controlling for depressive symptoms. When examining anxiety as measured by the BAI, results replicated the original results (i.e., the main effects and interaction were not significant; ps > 0.16). When examining STAI-Trait as the outcome, results differed from the main analyses in that a significant Time x Group interaction emerged (F(1.47,112.83) = 6.27, p = 0.01, ηp2 = 0.08). Simple main effects analyses indicated that participants in the clinical group reported less STAI-Trait at post-treatment and follow-up as compared to pre-treatment (ps < 0.01). Participants in the clinical group did not exhibit any significant change in STAI-Trait from post-treatment to follow-up (p = 0.15). Participants in healthy control group did not exhibit any change in STAI-Trait across time (ps > 0.25). Of note, the clinical group exhibited greater STAI-Trait levels than the healthy control group at pre-treatment (p = 0.03). At post-treatment and follow-up, the two groups did not significantly differ in STAI-Trait scores (ps > 0.26).
Discussion
The primary goals of the present research were to test the effectiveness of BATD-R and to examine the effects of BATD-R across a broad range of psychological outcomes in a community sample. Results demonstrated that BATD-R was associated with a reduction in depressive symptoms across data analytic techniques, even when controlling for anxiety. From pre-treatment to post-treatment, the clinical group exhibited a clinically significant reduction in depressive symptoms, as evidenced by levels of depressive symptoms that were comparable to those of the healthy control group. There was some mixed evidence regarding the effect of BATD-R on anxiety, but the notion that BATD-R might reduce anxiety independent of changes in depression was generally not supported. BATD-R was also associated with decreased dysfunctional attitudes and increased trait mindfulness.
With regard to depression, results consistently showed that BATD-R was associated with a reduction in depression for both per-protocol and intent-to-treat analyses, with large effect sizes. BATD-R was associated with reduced depression, even when controlling for pre-treatment anxiety. These findings are consistent with previous BATD efficacy studies (e.g., Snarski et al., 2011), as well as previous studies that utilized the BATD-R protocol (e.g., Collado et al., 2016). However, the present research expands on the previous work in three important ways. First, this is the first study to examine the effect of BATD-R on depression, while controlling for pre-treatment anxiety symptoms. Our results suggest that the treatment appears to uniquely target depression. Second, the present study builds upon previous BATD-R studies that targeted specific populations (e.g., Spanish-speaking Latinx). By demonstrating that BATD-R is associated with clinically significant reductions (at post-treatment) in depressive symptoms in a sample of community members who meet criteria for depression, the present findings provide evidence for the generalizability of BATD-R in the treatment of depression. Third, our findings provide additional support for the reliable clinical gains that BATD-R confers after conclusion of treatment. Previous studies of BATD-R have only examined clinical gains up to one month after the conclusion of treatment (Collado et al., 2016). Our findings demonstrate that BATD-R has positive effects on depression that are statistically reliable up to three months post-treatment.
Although the effect of BATD-R on depression was fairly robust, the evidence regarding the effects of BATD-R on anxiety was mixed, depending on the assessment measure examined. Generally, BATD-R was associated with reductions in symptoms of anxiety as measured by the STAI, but not the BAI. Potentially, this suggests that BATD-R may be more helpful in reducing aspects of anxiety that manifest as feelings of apprehension, worry, or nervousness, as opposed to somatic symptoms. However, it should be noted that some researchers have found that the STAI is limited in its ability to discriminate anxiety from depression (Endler et al., 1992; Julian, 2011). Indeed, there was much less evidence that BATD-R influenced anxiety symptoms after controlling for pre-treatment depression. This pattern of findings suggests BATD-R likely does not directly treat anxiety symptoms, but rather reduces anxiety symptoms due to the covariance between anxiety and depression. There are important clinical considerations based on these findings. BATD-R does not appear to be an appropriate intervention for anxiety symptoms when depression is not present. Conversely, BATD-R is an effective treatment for depression, even when comorbid anxiety is present. When delivering BATD-R to treat depression with comorbid anxiety, clinicians should re-assess anxiety symptoms at the completion of treatment and should employ a separate intervention if significant anxiety symptoms persist.
BATD-R was also associated with lower levels of dysfunctional attitudes, with large effect sizes. In the clinical group, dysfunctional attitudes decreased from pre-treatment to post-treatment and those reductions were maintained at the 3-month follow-up. No such changes over time were observed in the healthy control group. Although the intervention does not directly teach cognitive coping skills, BATD-R influenced dysfunctional attitudes. This finding is consistent with Jacobson et al.’s (1996) results, which showed that BATD decreased negative thinking and negative attributional style as much as cognitive therapy techniques. BATD-R may alter the context and functioning of negative thoughts through mechanisms aside from challenging overly negative thoughts, which is characteristic of traditional cognitive therapy. By increasing opportunities of reinforcement for non-depressed behavior, BATD-R may indirectly teach patients how negative thoughts can decrease likelihood of engagement in valued activity. It is also possible that engaging in valued activity may lead to positive thoughts that counter dysfunctional attitudes.
The clinical group’s decrease in dysfunctional attitudes has important implications for depression relapse. There is substantial support for the role of dysfunctional attitudes in predicting later depression (e.g., Abela, 2001; Just & Alloy, 1997). If BATD-R reduces a cognitive pattern that increases subsequent risk of depression, BATD-R might be effective in reducing the long-term risk of relapse. However, the mechanisms underlying the long-term clinical gains of BATD-R are still not well understood. In the current study, reductions in depression and dysfunctional attitudes were mostly sustained at three months after the conclusion of the intervention. The combination of decreased dysfunctional attitudes and findings that treatment gains are generally sustained for months following the conclusion of treatment suggests that BATD-R not only treats depression, but also decreases long-term risk. However, future research with longer follow-up assessment periods are warranted.
This is the first study to examine the extent to which behavioral activation may influence mindfulness. Participants who underwent BATD-R reported increases in trait mindfulness from pre-treatment to post-treatment, and those gains were maintained at the 3-month follow-up, with medium to large effect sizes. Trait mindfulness did not differ across assessment points in the healthy control group, demonstrating the general reliability of this construct without intervention. Although BATD-R does not explicitly have a mindfulness component, the sustained practice of monitoring one’s own engagement with activities, appraisal of the enjoyment and importance of activities, and mood may have increased tendencies toward present moment awareness. By repeatedly monitoring one’s mood and behavior, mindful attention may be fostered. Mindfulness is typically conceptualized as a multi-dimensional construct consisting of at least two factors: attention to present moment experiences and a perspective of nonjudgment (e.g., Bishop et al., 2004; Kabat-Zinn, 2003). The MAAS, which was used in the present study, is a unidimensional assessment of mindfulness that assesses attention to present moment experience. It remains unclear whether BATD-R helps to cultivate a non-judgmental orientation to experiences. Future studies should employ multi-dimensional measures of mindfulness to clarify this potential distinction.
Given that participants who underwent BATD-R exhibited a decrease in dysfunctional attitudes and an increase in trait mindfulness, it is possible that changes in dysfunctional attitudes and mindfulness may help to explain how BATD-R alleviates depressive symptoms. Negative cognitive styles mediate other cognitive-behavioral treatments for depression (e.g., Muñoz et al., 1995; Warmerdam et al., 2010). Furthermore, cognitive accounts of depression posit that negative cognitive styles maintain depressive symptoms (Abramson et al., 1989; Beck, 2008). It is possible that reductions in dysfunctional attitudes mediate the treatment effects of BATD-R on depression. Similarly, changes in mindfulness might also account for a portion of the improvements in depression following BATD-R. Trait mindfulness is associated with enhanced psychological health (e.g., Brown et al., 2007) and mediates treatment effects in cognitive behavioral interventions for social anxiety (Goldin et al., 2016; Kocovski et al., 2015). Thus, trait mindfulness may mediate treatment effects of BATD-R. Future studies are needed to assess dysfunctional attitudes, mindfulness, and depression over the course of treatment to explore whether changes in dysfunctional attitudes and mindfulness precede changes in depression.
Findings should be considered in the context of the study limitations. Participants with depression were not randomized into treatment or control conditions. A healthy control sample served as a basis for comparison, allowing us to estimate the clinical significance of treatment effects. As such, changes in the study variables cannot be causally attributed to BATD-R and could reflect regression to the mean. Depressive symptoms have been found to decrease 10–15% on average when untreated (Posternak & Miller, 2001). However, given that we observed a 64.5% decrease in depressive symptoms in our clinical group, it is unlikely that this change is solely an artifact of regression to the mean. Attrition rates in the study were about 35%, which is consistent with the attrition rates of existing BATD, BATD-R, and general behavioral activation treatment studies (range = 11% to 42%; e.g., Jacobson et al., 1996; Snarski et al., 2011). The variability in dropout rates for behavioral activation treatment studies falls within the range of previously reported psychotherapy dropout rates for depression treatment studies (i.e., range = 0 to 50%; Cooper & Conklin, 2015). Individuals in the treatment group were more likely to drop out of the study than individuals in the control group. Differential attrition is not uncommon in treatment studies, but it may confound accurate assessments of effects (Howard et al., 1986). Intent-to-treat procedures were utilized in an attempt to reduce potential biases introduced by the attrition rates. Although our community sample increased external validity of BATD-R, the sample was ethnically homogeneous and relatively young. Future studies should strive to recruit more diverse samples.
Conclusions
The present study provides significant support for the effectiveness of BATD-R in treating a community sample of adults with depression. Furthermore, BATD-R may have broader psychological effects—reducing dysfunctional attitudes and increasing mindfulness—by indirectly reducing negative thoughts about the self through reinforcement for values-based activities and encouraging present moment focus with behavioral monitoring. These findings may indicate potential mechanisms of action for BATD-R. In sum, BATD-R represents a valuable and accessible treatment that appears to impact psychological processes beyond behavioral activation to benefit individuals with depression.
Availability of Data and Material
Data and material available upon request.
Code availability
Code available upon request.
Notes
For individuals who indicated psychotropic medication usage, only those who were stabilized on their medication for six weeks were enrolled in the study.
As anxiety and depression are highly comorbid (Brown et al., 1998; Hranov, 2007), we ran analyses including each of the pre-treatment anxiety measures as a covariate. The pattern of results generally remained the same (see Supplemental Material).
The pattern of results remained the same when anxiety was included as a covariate (see Supplemental Material).
References
Abramson, L. Y., Metalsky, G. I., & Alloy, L. B. (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96, 358–372. https://doi.org/10.1037/0033-295X.96.2.358
Abela, J. R. (2001). The hopelessness theory of depression: A test of the diathesis–stress and causal mediation components in third and seventh grade children. Journal of Abnormal Child Psychology, 29, 241–254. https://doi.org/10.1023/A:1010333815728
Armento, M. E., & Hopko, D. R. (2009). Behavioral activation of a breast cancer patient with coexistent major depression and generalized anxiety disorder. Clinical Case Studies, 8, 25–37. https://doi.org/10.1177/1534650108327474
Barlow, D. H. (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.). Guilford Press.
Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. American Journal of Psychiatry, 165, 969–977. https://doi.org/10.1176/appi.ajp.2008.08050721
Beck, A. T., Epstein, N., Brown, G., & Steer, R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56, 893. https://doi.org/10.1037/0022-006X.56.6.893
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck Depression Inventory-II. Psychological Corporation.
Bellg, A. J., Borrelli, B., Resnick, B., Hecht, J., Minicucci, D. S., Ory, M., & Czajkowski, S. (2004). Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychology, 23, 443–451. https://doi.org/10.1037/0278-6133.23.5.443
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241. https://doi.org/10.1093/clipsy.bph077
Brown, T. A., Chorpita, B. F., & Barlow, D. H. (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107, 179–192. https://doi.org/10.1037/0021-843X.107.2.179
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822–848. https://doi.org/10.1037/0022-3514.84.4.822
Brown, K. W., Ryan, R. M., & Creswell, J. D. (2007). Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry, 18, 211–237. https://doi.org/10.1080/10478400701598298
Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159. https://doi.org/10.1037/0033-2909.112.1.155
Collado, A., Calderón, M., MacPherson, L., & Lejuez, C. (2016). The efficacy of behavioral activation treatment among depressed Spanish-speaking Latinos. Journal of Consulting and Clinical Psychology, 84, 651–657. https://doi.org/10.1037/ccp0000103
Collado, A., Castillo, S. D., Maero, F., Lejuez, C. W., & MacPherson, L. (2014). Pilot of the brief behavioral activation treatment for depression in Latinos with limited English proficiency: Preliminary evaluation of efficacy and acceptability. Behavior Therapy, 45, 102–115. https://doi.org/10.1016/j.beth.2013.10.001
Cooper, A. A., & Conklin, L. R. (2015). Dropout from individual psychotherapy for major depression: A meta-analysis of randomized clinical trials. Clinical Psychology Review, 40, 57–65. https://doi.org/10.1016/j.cpr.2015.05.001
Daughters, S. B., Braun, A. R., Sargeant, M. N., Reynolds, E. K., Hopko, D. R., Blanco, C., & Lejuez, C. W. (2008). Effectiveness of a brief behavioral treatment for inner-city illicit drug users with elevated depressive symptoms: The life enhancement treatment for substance use (LETS Act!). Journal of Clinical Psychiatry, 69, 122–129. https://doi.org/10.4088/jcp.v69n0116
Dykman, B. M., & Johll, M. (1998). Dysfunctional attitudes and vulnerability to depressive symptoms: A 14-week longitudinal study. Cognitive Therapy and Research, 22, 337–352. https://doi.org/10.1023/A:1018705112077
Endler, N. S., Cox, B. J., Parker, J. D., & Bagby, R. M. (1992). Self-reports of depression and state-trait anxiety: Evidence for differential assessment. Journal of Personality and Social Psychology, 63, 832–838. https://doi.org/10.1037//0022-3514.63.5.832
First, M. B., Gibbon, M., Spitzer, R. L., Benjamin, L. S., & Williams, J. B. (1997). Structured Clinical Interview for DSM-IV® Axis II Personality Disorders SCID-II. American Psychiatric Publishing.
Ford, C. G., & Shook, N. J. (2019). Negative cognitive bias and perceived stress: Independent mediators of the relation between mindfulness and emotional distress. Mindfulness, 10, 100–110. https://doi.org/10.1007/s12671-018-0955-7
Freij, K., & Masri, N. (2008). The brief behavioral activation treatment for depression. Nordic Psychology, 60, 129–140. https://doi.org/10.1027/1901-2276.60.2.129
Garland, E. L., Fredrickson, B., Kring, A. M., Johnson, D. P., Meyer, P. S., & Penn, D. L. (2010). Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30(7), 849–864. https://doi.org/10.1016/j.cpr.2010.03.002
Gawrysiak, M., Nicholas, C., & Hopko, D. R. (2009). Behavioral activation for moderately depressed university students: Randomized controlled trial. Journal of Counseling Psychology, 56, 468–475. https://doi.org/10.1037/a0016383
Goldin, P. R., Morrison, A., Jazaieri, H., Brozovich, F., Heimberg, R., & Gross, J. J. (2016). Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 84, 427–437. https://doi.org/10.1037/ccp0000092
Herrnstein, R. J. (1970). On the law of effect. Journal of the Experimental Analysis of Behavior, 13, 243–266. https://doi.org/10.1901/jeab.1970.13-243
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183. https://doi.org/10.1037/a0018555
Hopko, D. R., Armento, M. E., Robertson, S., Ryba, M. M., Carvalho, J. P., Colman, L. K., & Lejuez, C. W. (2011). Brief behavioral activation and problem-solving therapy for depressed breast cancer patients: Randomized trial. Journal of Consulting and Clinical Psychology, 79, 834–849. https://doi.org/10.1037/a0025450
Hopko, D. R., Bell, J. L., Armento, M. E. A., Hunt, M. K., & Lejuez, C. W. (2005). Behavior therapy for depressed cancer patients in primary care. Psychotherapy: Theory. Research, Practice, Training, 42, 236–243. https://doi.org/10.1037/0033-3204.42.2.236
Hopko, D. R., Funderburk, J. S., Shorey, R. C., McIndoo, C. C., Ryba, M. M., File, A. A., & Vitulano, M. (2013). Behavioral activation and problem-solving therapy for depressed breast cancer patients: Preliminary support for decreased suicidal ideation. Behavior Modification, 37, 747–767. https://doi.org/10.1177/0145445513501512
Hopko, D. R., Lejuez, C. W., & Hopko, S. D. (2004). Behavioral activation as an intervention for coexistent depressive and anxiety symptoms. Clinical Case Studies, 3, 37–48. https://doi.org/10.1177/1534650103258969
Hopko, D., Lejuez, C., LePage, J., Hopko, S., & McNeil, D. (2003). A brief behavioral activation treatment for depression: A randomized pilot trial within an inpatient psychiatric hospital. Behavior Modification, 27, 458–469. https://doi.org/10.1177/0145445503255489
Hopko, D. R., Lejuez, C. W., Ryba, M. M., Shorter, R. L., & Bell, J. L. (2016). Support for the efficacy of behavioural activation in treating anxiety in breast cancer patients. Clinical Psychologist, 20, 17–26. https://doi.org/10.1111/cp.12083
Hopko, D. R., Robertson, S., & Lejuez, C. W. (2006). Behavioral activation for anxiety disorders. The Behavior Analyst Today, 7, 212–232. https://doi.org/10.1037/h0100084
Howard, K. I., Krause, M. S., & Orlinsky, D. E. (1986). The attrition dilemma: Toward a new strategy for psychotherapy research. Journal of Consulting and Clinical Psychology, 54, 106–110. https://doi.org/10.1037//0022-006x.54.1.106
Hranov, L. G. (2007). Comorbid anxiety and depression: Illumination of a controversy. International Journal of Psychiatry in Clinical Practice, 11, 171–189. https://doi.org/10.1080/13651500601127180
Jacobson, N. S., Martell, C. R., & Dimidjian, S. (2001). Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice, 8, 255–270. https://doi.org/10.1093/clipsy.8.3.255
Jacobson, N. S., Dobson, K. S., Truax, P. A., Addis, M. E., Koerner, K., Gollan, J. K., & Prince, S. E. (1996). A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology, 64, 295–304. https://doi.org/10.1037/0022-006X.64.2.295
Jacobson, N. S., & Truax, P. (1992). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. https://doi.org/10.1037/10109-042
Judah, M. R., Dahne, J., Hershenberg, R., & Gros, D. F. (2020). Behavioral activation. In J. S. Abramowitz & S. M. Blakey (Eds.), Clinical handbook of fear and anxiety: Maintenance processes and treatment mechanisms (pp. 305–321). American Psychological Association. https://doi.org/10.1037/0000150-017
Julian, L. J. (2011). Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care & Research, 63, S467–S472. https://doi.org/10.1002/acr.20561
Just, N., & Alloy, L. B. (1997). The response styles theory of depression: Tests and an extension of the theory. Journal of Abnormal Psychology, 106, 221–229. https://doi.org/10.1037/0021-843X.106.2.221
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156. https://doi.org/10.1093/clipsy.bpg016
Kanter, J. W., Baruch, D. E., & Gaynor, S. T. (2006). Acceptance and commitment therapy and behavioral activation for the treatment of depression: Description and comparison. The Behavior Analyst, 29, 161–185. https://doi.org/10.1007/BF03392129
Kanter, J. W., Manos, R. C., Bowe, W. M., Baruch, D. E., Busch, A. M., & Rusch, L. C. (2010). What is behavioral activation?: A review of the empirical literature. Clinical Psychology Review, 30, 608–620. https://doi.org/10.1016/j.cpr.2010.04.001
Kiken, L. G., & Shook, N. J. (2011). Looking up: Mindfulness increases positive judgments and reduces negativity bias. Social Psychological and Personality Science, 2, 425–431. https://doi.org/10.1177/1948550610396585
Kiken, L. G., & Shook, N. J. (2012). Mindfulness and emotional distress: The role of negatively biased cognition. Personality and Individual Differences, 52, 329–333. https://doi.org/10.1016/j.paid.2011.10.031
Kocovski, N. L., Fleming, J. E., Hawley, L. L., Ho, M. H. R., & Antony, M. M. (2015). Mindfulness and acceptance-based group therapy and traditional cognitive behavioral group therapy for social anxiety disorder: Mechanisms of change. Behaviour Research and Therapy, 70, 11–22. https://doi.org/10.1016/j.brat.2015.04.005
Lejuez, C. W., Hopko, D. R., Acierno, R., Daughters, S. B., & Pagoto, S. L. (2011). Ten year revision of the brief behavioral activation treatment for depression: Revised treatment manual. Behavior Modification, 35, 111–161. https://doi.org/10.1177/0145445510390929
Lejuez, C. W., Hopko, D. R., & Hopko, S. D. (2001). A brief behavioral activation treatment for depression: Treatment manual. Behavior Modification, 25, 255–286. https://doi.org/10.1177/0145445501252005
MacPherson, L., Tull, M. T., Matusiewicz, A. K., Rodman, S., Strong, D. R., Kahler, C. W., & Lejuez, C. W. (2010). Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. Journal of Consulting and Clinical Psychology, 78, 55–61. https://doi.org/10.1037/a0017939
Martell, C. R., & Kanter, J. W. (2011). Behavioral activation in the context of “third wave” therapies. In J. D. Herbert & E. M. Forman (Eds.), Acceptance and mindfulness in cognitive behavior therapy: Understanding and applying the new therapies (pp. 193–209). John Wiley & Sons Inc.
McIndoo, C. C., File, A. A., Preddy, T., Clark, C. G., & Hopko, D. R. (2016). Mindfulness-based therapy and behavioral activation: A randomized controlled trial with depressed college students. Behaviour Research and Therapy, 77, 118-128. https://doi.org/10.1016/j.brat.2015.12.012
Monroe, S. M., & Harkness, K. L. (2011). Recurrence in major depression: A conceptual analysis. Psychological Review, 118, 655–674. https://doi.org/10.1037/a0025190
Muñoz, R. F., Ying, Y. W., Bernal, G., Pérez-Stable, E. J., Sorensen, J. L., Hargreaves, W. A., & Miller, L. S. (1995). Prevention of depression with primary care patients: A randomized controlled trial. American Journal of Community Psychology, 23, 199–222. https://doi.org/10.1007/BF02506936
Posternak, M. A., & Miller, I. (2001). Untreated short-term course of major depression: A meta-analysis of outcomes from studies using wait-list control groups. Journal of Affective Disorders, 66, 139–146. https://doi.org/10.1016/S0165-0327(00)00304-9
Rothwell, P. M. (2005). External validity of randomised controlled trials: “To whom do the results of this trial apply?” The Lancet, 365, 82–93. https://doi.org/10.1016/S0140-6736(04)17670-8
Ryba, M. M., Lejuez, C. W., & Hopko, D. R. (2014). Behavioral activation for depressed breast cancer patients: The impact of therapeutic compliance and quantity of activities completed on symptom reduction. Journal of Consulting and Clinical Psychology, 82, 325. https://doi.org/10.1037/a0035363
Seggar, L. B., Lambert, M. J., & Hansen, N. B. (2002). Assessing clinical significance: application to the Beck Depression Inventory. Behavior Therapy, 33, 253–269. https://doi.org/10.1016/S0005-7894(02)80028-4
Shook, N. J., Ford, C., Strough, J., Delaney, R., & Barker, D. (2017). In the moment and feeling good: Age differences in mindfulness and positive affect. Translational Issues in Psychological Science, 3, 338–347. https://doi.org/10.1037/tps0000139
Snarski, M., Scogin, F., DiNapoli, E., Presnell, A., McAlpine, J., & Marcinak, J. (2011). The effects of behavioral activation therapy with inpatient geriatric psychiatry patients. Behavior Therapy, 42, 100–108. https://doi.org/10.1016/j.beth.2010.05.001
Spielberger, C. D. (1983). State-Trait Anxiety Inventory for adults. Mind Garden.
Tull, M. T., Berghoff, C. R., Bardeen, J. R., Schoenleber, M., & Konkle-Parker, D. J. (2018). An initial open trial of a brief behavioral activation treatment for depression and medication adherence in HIV-infected patients. Behavior Modification, 42, 196–209. https://doi.org/10.1177/0145445517723901
Tull, M. T., Rosenblatt, C. B., Berghoff, C. R., Dixon, L. J., Ciarloni, E., Montgomery, D. D., & Marshall, G. D. (2019). An uncontrolled open trial of a Brief Behavioural Activation Treatment for Depression in patients with chronic spontaneous urticaria. Behaviour Change, 36, 75–83. https://doi.org/10.1017/bec.2019.5
Warmerdam, L., van Straten, A., Jongsma, J., Twisk, J., & Cuijpers, P. (2010). Online cognitive behavioral therapy and problem-solving therapy for depressive symptoms: Exploring mechanisms of change. Journal of Behavior Therapy and Experimental Psychiatry, 41, 64–70. https://doi.org/10.1016/j.jbtep.2009.10.003
Weissman, A. N., & Beck, A. T. (1978). Development and validation of the Dysfunctional Attitude Scale. Chicago: Paper presented at the annual meeting of the Association for the Advancement of Behavior Therapy. Retrieved April 21, 2020, from https://files.eric.ed.gov/fulltext/ED167619.pdf
Funding
This work was supported by a NARSAD Young Investigator Award from the Brain and Behavior Foundation. The funding organization was not involved in designing the study, collecting and analyzing the data, or preparing the manuscript.
Author information
Authors and Affiliations
Contributions
Jerin Lee: Data Curation, Formal Analysis, Writing – Original Draft, Review & Editing. Cameron G. Ford: Investigation, Writing – Original Draft, Review & Editing. D. Lee McCluskey: Investigation, Writing – Review & Editing. Patricia D. Hopkins: Investigation, Writing – Review & Editing. Daniel W. McNeil: Investigation, Supervision, Writing – Review & Editing. Natalie J. Shook: Conceptualization, Methodology, Investigation, Resources, Writing – Original Draft, Review & Editing, Supervision, Project administration, Funding acquisition.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Institutional Review Board of West Virginia University (Protocol #1401167770) and conducted in line with the principles of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
Not applicable.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest
Jerin Lee, Cameron G. Ford, D. Lee McCluskey, Patricia D. Hopkins, Daniel W. McNeil and Natalie J. Shook have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, J., Ford, C.G., McCluskey, D.L. et al. Testing the Effectiveness of Brief Behavioral Activation Treatment for Depression—Revised: Changes in Depression, Anxiety, Dysfunctional Attitudes, and Mindfulness. J Psychopathol Behav Assess 44, 456–468 (2022). https://doi.org/10.1007/s10862-021-09938-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-021-09938-4