Abstract
Research into nonsuicidal self-injury (NSSI) has primarily focussed on the experience and regulation of emotion. Recently, NSSI-specific cognitions, including self-efficacy to resist self-injury, have been explored to further understand the behaviour. However, within these studies self-efficacy to resist NSSI has been assessed broadly using an adapted measure of self-efficacy to avoid suicide. There is a need for a NSSI-specific measure of self-efficacy, which considers specific contexts that may influence confidence in the ability to resist self-injuring. This paper reports the development of such a measure. An initial item pool (125 items) was generated from interviews with people with lived experience of NSSI and experts in the field of self-injury. These items were then administered to 650 participants aged 18–40 years (M = 21.14, SD = 2.32, 45.69% with a history of NSSI). Analyses revealed a three-factor structure representing: contexts in which it would be difficult to resist NSSI (risk contexts); contexts which make it easier to resist NSSI (protective contexts); and contexts in which people are reminded of self-injury (reminders of NSSI). To reduce the number of items, eight items with the highest loadings on each factor were retained. The final 24 item (three subscales) scale fit the data well and demonstrated invariance across individuals with and without a history of self-injury. Correlations with related but distinct constructs (e.g., self-esteem, locus of control) supported convergent and discriminative validity. This measure could be used to further theoretical understanding of NSSI and may be useful in clinical settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nonsuicidal self-injury (NSSI; also referred to as self-injury within this paper) is the direct and deliberate damage to one’s own body tissue, without suicidal intent (e.g., cutting, burning, biting the skin; International Society for the Study of Self-Injury, 2018). Self-injury is commonly engaged in to regulate unwanted emotional experiences (Taylor et al., 2018) and is prevalent in clinical (Hauber et al., 2019) and non-clinical populations (Swannell et al., 2014). A history of engaging in NSSI is associated with diagnosis of mental illness and an increased risk of suicidal thoughts and behaviours (Kiekens et al., 2018a, b). Due to these associations, it is important to understand emotional and cognitive factors that may facilitate the onset, maintenance, and cessation of self-injurious behaviours.
Bandura (1986, 1997) proposed that our beliefs in our abilities to successfully complete activities (self-efficacy) influence which behaviours we engage in. Although related, these beliefs are distinct from self-esteem which refers to beliefs about self-worth, and separate concepts from locus of control (whether one’s own actions affect outcomes; Bandura, 1997). According to Social Cognitive Theory (Bandura, 1997), the more confidence we have in our ability to successfully complete a task, the more likely we are to engage in the behaviour. This theory has been reflected in the results of cross-sectional (e.g., Dawkins et al., 2018, 2019; Oei et al., 2007) and longitudinal studies (e.g., Chavarria et al., 2012; Tatnell et al., 2014) and further supported in reviews (e.g. Kadden & Litt, 2011) and meta-analyses (e.g. Gwaltney et al., 2009). Having little confidence in your overall ability to be successful and overcome obstacles (general self-efficacy) is associated with engagement in health risk behaviours such as risky drinking (Oei et al., 2007), disordered eating (Glasofer et al., 2013), and NSSI (Tatnell et al., 2014). However, behaviour-specific self-efficacy is a better predictor of whether a particular behaviour is engaged in (Bandura, 1997; Hasking et al., 2018). Similarly, having confidence in our ability to resist specific behaviours (e.g., drinking, smoking, substance use, self-injury) is related to a reduced likelihood of future engagement in that behaviour (Chavarria et al., 2012; Dawkins et al., 2018, 2019; Gwaltney et al., 2009; Kadden & Litt, 2011). Our self-efficacy beliefs also vary depending on the context we are in (Bandura, 1997). For example, we may believe that it would be easy to resist consuming alcohol in the morning on the way to work but anticipate that we would find it difficult to resist drinking alcohol at a party on a Friday night with friends (Oei et al., 2005). As such, it is important to know which contexts are believed to make it easier or more difficult to resist or engage in a behaviour if we want to predict behaviour across contexts.
Recently, within the Cognitive-Emotional Model of NSSI, Hasking et al. (2017) included a role for self-efficacy to resist NSSI in the onset, maintenance, and cessation of self-injury. Supporting this, recent studies exploring this relationship have found that people who have recently self-injured (in the past 12 months) have less belief in their ability to resist self-injury than people who have never self-injured, and people who have a history of self-injury but have not self-injured in the past 12 months (Dawkins et al., 2018, 2019; Hasking & Rose, 2016). This suggests that self-efficacy to resist NSSI may play a role in facilitating and/or limiting engagement in NSSI.
To date, studies exploring self-efficacy to resist NSSI have used an adapted version of Czyz et al. (2014)’s Self-Efficacy to Avoid Suicide Action scale to measure participants’ general belief in their ability to resist NSSI (Dawkins et al., 2018, 2019; Hasking, 2017; Hasking & Boyes, 2017; Hasking & Rose, 2016). This single dimension scale was developed in consideration of contexts which may make it difficult to avoid suicide. However, Bandura (1997, 2006) highlighted the necessity to develop measures specific to individual behaviours as the best, and most nuanced, way to identify an individual’s self-efficacy beliefs. Most important is the inclusion of items spanning differing contexts so that context-dependant changes in self-efficacy can be identified (Bandura, 2006).
This paper outlines the development and preliminary validation of a measure of self-efficacy to resist NSSI across a variety of contexts identified as particularly relevant to the behaviour. Phase One includes the generation of an initial item pool in consultation with experts in the field of NSSI and people with lived experience of self-injury. It also outlines a hypothesized scale structure. Phase Two includes 1) assessment of the factor structure and reduction of items; 2) assessment of convergent and discriminant validity; 3) assessment of measurement invariance among people with and without a history of self-injury.
Phase One: Item Generation
Method
Participants
Participants included people with lived experience of NSSI (n = 10) and people considered clinical and/or research experts (n = 9) in NSSI. Participants with lived experience of NSSI were Australian university students who self-identified as having a history of self-injury. They were recruited through an online portal where studies are advertised to undergraduate psychology students for course credit. Ten students, 6 females and 4 males, aged 19–23 (M = 21.5, SD = 1.65) participated in the study. Participants reported age of NSSI onset ranged from 8 to 20 years old (M = 14.20, SD = 4.10). Cutting was the most frequently reported main form of self-injury (n = 4), followed by pinching (n = 2), scratching (n = 2), biting (n = 1) and self-battery (n = 1). Participants reported having engaged in self-injury between 20 and 675 times in their lives (M = 145, SD = 211.14) and four reported that the last time they had engaged in self-injury was within the past 12 months.
Seventeen people considered experts in the research and/or treatment of NSSI were invited to participate in the study. Of these 9 (6 female and 3 male) accepted the invitation to participate. Experts were three clinicians, four academic researchers, and two people who worked in both research and clinical settings. Participants had an average of 17 years’ experience.Footnote 1
Materials
Demographics
Participants with a history of NSSI completed a demographic questionnaire asking their name, age, gender, year at university, and country of birth in an open response format.
History of Nonsuicidal Self-Injury
Participants with lived experience of NSSI were asked to complete the Inventory of Statements About Self-Injury (ISAS; Klonsky & Glenn, 2009). It asks participants to indicate how many times they had self-injured in the past 12 months and their lifetime frequency of 13 methods of self-injury (e.g., cutting, burning, self-battery). They are also asked to indicate their main form of self-injury if they have one. The ISAS has demonstrated test–retest reliability (Glenn & Klonsky, 2011) and is correlated with mental illness diagnoses such as depression, anxiety, and borderline personality disorder (Glenn & Klonsky, 2011; Klonsky & Olino, 2008).
Lived Experience Interviews
A semi-structured interview guide was developed which included questions pertaining to details of participants’ experience of engaging in NSSI including onset, whether they believed they had ceased engaging in NSSI, and contexts in which they had engaged in NSSI. Questions explored participant’s views on contexts which may make it difficult or easier to resist engaging in NSSI. In consultation with experts and people with lived experience we considered the appropriate language when asking participants about their experience of self-injury.
Expert Interviews
A semi-structured interview guide was developed which included open-ended questions about participants’ professional experience with NSSI and covered contexts in which participants thought people found it difficult or easy to resist an urge to self-injure. They were also asked what they believed would be important to include in a measure of self-efficacy to resist NSSI.
Procedure
Prior to commencing interviews with people with lived experience of NSSI and experts, participants were asked to read the participant information sheet and were given an opportunity to ask any questions about the research and their participation. If they agreed to participate, they were asked to sign the consent form. All interviews were audio recorded. At completion of the interviews participants with a history of engaging in self-injury were debriefed and provided information about NSSI and support services.
Analysis
Thematic analysis was used to explore contexts surrounding self-injury using Braun and Clarke’s (2006) procedure. Beginning with the initial transcription of the interviews verbatim the first and second authors familiarised themselves with the transcripts and generated initial topic codes which described the content of the transcripts. These codes were further explored to discover themes which represented patterns within the data. These possible themes were reviewed among the researchers and further refined. These themes were named and described in line with the overarching research aim. Possible questionnaire items were generated from themes, codes, and quotes which represented contexts which may impact on an individual’s belief in their ability to resist an urge to self-injure.
Findings
Thematic Analysis
Analysis of interview transcripts revealed similar themes across participants with lived experience and participants considered experts in the field of NSSI. Therefore, findings from all participants are presented together. The contexts surrounding self-injury as reported by participants, reflects the literature with regards to self-injury and the functions of self-injury. Eight themes, reflecting a variety of contexts which may make it difficult or easy to resist an urge to self-injure, were identified: emotional contexts; interpersonal relationships; cognitions and cognitive processes; physical contexts; alcohol and other drugs; reminders of NSSI; thoughts of NSSI; and alternative regulation strategies. For most themes there were times when it may be easier to resist an urge to self-injure (e.g., when feeling connected to other people) or more difficult to resist that urge (e.g., after an argument with a family member or friend).
Unsurprisingly, given the existing literature on the functions of NSSI as a method of emotion regulation in response to distress (Taylor et al., 2018), participants overwhelmingly noted the emotional contexts surrounding self-injury. Participants reported that NSSI was often engaged in the context of unpleasant emotional experiences “… that could be extreme anxiety, sadness, emptiness, anger, and it’s reached a threshold at which they feel they can’t resist the urge to engage in behaviours to hurt themselves.” (expert). The emotion regulation function of NSSI was also highlighted “…during that time I felt anxiety was like the highest I ever felt, and I didn’t know what else I could do to manage it.” (lived experience). It was apparent that unpleasant and unwanted emotional experiences were salient as an important context in which NSSI was engaged.
Interpersonal relationships and interactions were seen as potentially increasing the risk of engaging in NSSI or possibly encouraging resistance from acting on an urge to self-injure. Having an argument or disagreement with a loved one was noted as making it difficult to resist an urge to self-injure “So, what we often see, is they er, have troubles with their peers, or their boy er, or girlfriends, or with family members, so er, there’s also a sort of conflict in an interpersonal situation…” (expert). The importance of interpersonal relationships was also highlighted when it came to resisting NSSI. Participants noted that strong relationships and thinking of loved ones could make it easier to resist self-injury “I think now I have more community support the chance [of engaging in self-injury] is much lower than what it has been, what it would have been.” (lived experience).
Cognitions and cognitive processes were also seen to be related to engaging in NSSI. Participants noted the role of persistent worry and rumination or found it difficult to resist the urge to self-injure when they had specific negative thoughts about themselves. Often there was a combination of the two:
“It was just like, it was mostly overthinking, stress, panic, it would go from worrying about, like, certain situations, worrying about grades, to worrying about just thinking about how I’m presenting myself, thinking I’m worthless, or like, I’m useless or I don’t deserve what I have. Like not deserving was like quite big for me, constantly stressing over how you were gonna lose friends, or like anything because you just didn’t deserve it, so you shouldn’t have had it in the first place.” (lived experience).
Participants expressed that NSSI was often associated with negative self-thoughts and beliefs, including self-hatred and thoughts of deserving to be punished “…a form of self-punishment, sort of a heightened emotional state combined with self-criticism and a desire to self-punish themselves.” (expert). Thoughts of suicide were also associated with engaging in NSSI, as self-injury was perceived as an alternative to suicide. These negative thoughts and thought processes were often reported to be experienced in the lead up to engaging in self-injury.
Physical contexts surrounding self-injury could be seen to make it easier or more difficult to resist an urge to self-injure. Participants described self-injury being engaged in when they were alone and in a private space: “when it was in XX it was like my family home um so it kind of, I guess to me it felt, I felt, more safer or um it was more private like in my own room or in the bathroom” (lived experience). It was perceived to be easier to resist engaging in self-injury when out in a social context “… if you are amidst your friends and surrounded by people, or in class, or on a date, chances are you’re going to be able to resist, because the context is not conducive to something as alarming and provocative as self-injury.” (expert). Participants spoke about how leaving a particular physical environment could help them resist engaging in self-injury but also reported times they left where they were to find a “safe” environment where they could self-injure.
Some participants highlighted that being under the influence of drugs and/or alcohol had increased the likelihood of engaging in self-injury, “Honestly, I was just really drunk when I did and I kind of just, couldn’t stop myself. Which was new to me at the time so now that I know that I don’t think I am gonna do that again.” (lived experience). Similarly, participants acknowledged that avoiding drugs and alcohol made it easier to resist an urge to self-injure “Umm, maybe just avoiding umm, things like, things that alter you, your control of yourself so like alcohol and drugs. I think it is super important to avoid those sorts of things.” (lived experience). As such, being under the influence of drugs and/or alcohol was considered to make engaging in NSSI more likely. However, there was another experience expressed in that substance use could replace NSSI as a coping strategy and as such, reduced the likelihood of engaging in NSSI.
“there are groups of individuals who stop engaging in more direct forms of self-injury like cutting and burning, but as they get into college and beyond, they might engage in other types of behaviours that serve that same kind of self-punishing function, so we see when they transition into college, they may engage in substance misuse and less direct forms of self-harm, but a lot of emotional cognitive pieces remain the same.” (expert).
Participants noted that being reminded of NSSI either by seeing their own or other people’s scars or engaging in conversations with people about self-injury were seen to be related to subsequent NSSI engagement “I think I had also started noticing scars on like friends and things like that.” (lived experience). Participants also reported that reminders of self-injury may be sought out “they tell me when they are in a bad period of self-injury that unconsciously or consciously, I don’t know, they look at videos or sad songs about self-injury and then it’s very difficult [to resist an urge to self-injure]” (expert).
Participants often reported having thoughts specifically about self-injury in the lead up to engaging in self-injury.
“it’s usually, the thoughts usually, how can I do this without people knowing, and yeah just thinking how I will do it and how I will hide it, and yeah, yeah thinking about doing it rather than thinking about sort of, what’s going on, cause I guess that’s the reason I do it, like to distract myself from whatever the issue is, cause now that’s the thing I’m thinking of, or that’s the issue in my head now, how am I going to self-harm, not what lead me to want to self-harm in the first place.” (lived experience).
Participants also stated that changing positive beliefs about self-injury decreased the frequency of engaging in NSSI “Cause like I said, I used to think it [self-injury] helped me, like for the better, but then it kind of hit one day that it doesn’t at all.” (lived experience). Participants also said that the intensity of urges to self-injure made it difficult to resist NSSI “… sort of intensity of urge was associated with greater likelihood of self-injury happening…” (expert). These thoughts about NSSI appeared separate from the negative self-thoughts and cognitive patterns which were seen to be associated with NSSI.
The availability of alternative regulation strategies was also seen as an important factor that could influence whether someone believed they could resist the urge to self-injure. This was premised with the knowledge that the alternative strategies often were not as effective as NSSI at regulating emotions “So they found that there were gradients of effectiveness. So, like, people reported trying to sort of distract themselves, like spending time with friends, or watch TV, but that wasn’t as effective as exercising, or removing the means to self-harm.” (expert). It was noted by participants that, with practice, these strategies would become more and more effective “But as I got more, more, used to it I found that I could distract myself, I could like, do other things, it would eventually go away.” (lived experience).
Item Generation
Following thematic analysis, 100 items were developed which reflected the identified themes within the data. Items for each theme reflected contexts which were perceived to be difficult (e.g., When I feel anxious) and easier (e.g., When I feel relaxed) to resist an urge to engage in NSSI. The scale format was informed by Bandura’s (2006) “Guide for constructing self-efficacy scales” in that participants were asked what they believed they could do rather than what they believe they would do. Participants were instructed to rate on a scale of 1 (not confident at all) to 4 (extremely confident) how confident they are that they could resist the urge to self-injure given a variety of situations (e.g., “When I feel lonely”, “When I know no one will find out”, “Before social situations”).
Review of Items
The 100 items resulting from the item generation phase were reviewed by attendees of an international academic conference focussed on clinical work and research related to NSSI. Attendees included researchers, clinicians, students, and people with lived experience of NSSI. Items were provided to all attendees as part of their information pack, and they were given the opportunity to provide anonymous feedback on the content or format of the questionnaire and items. Feedback was provided by seven attendees, which included suggestions for additional items and item format (e.g., consistency in item stems). Once the feedback was incorporated into the item pool the total number of items was 125. Items reflected the eight themes extracted from interview transcripts: emotional contexts (25 items, e.g. When I feel hopeless); interpersonal contexts (27 items, e.g., When someone I love is angry at me); cognitions and cognitive processes (14 items, e.g. When I think I am not loveable); physical contexts (19 items, e.g. When I am in my bedroom); alcohol and other drugs (4 items, When I have been drinking); reminders of self-injury (9 items, e.g. When I see an image of self-injury); thoughts about self-injury (11 items, e.g. When I am motivated to resist self-injury); other regulation strategies (12 items, e.g. When I have other coping strategies).
Discussion
The aim of Phase One was to develop an initial item pool for a measure of self-efficacy to resist NSSI. This was done through semi-structured interviews exploring contexts surrounding self-injury. Eight themes were identified from the transcripts which represented contexts which could make it easier or more difficult to resist an urge to self-injure.
As NSSI is commonly used to regulate intense and unwanted emotional distress (Taylor et al., 2018) it is unsurprising that emotional experiences were considered to impact whether someone believed they could resist an urge to self-injure. Participants noted that feelings of loneliness, anxiety, anger, and sadness precipitate engagement in NSSI and were perceived to make it more difficult to resist and urge to self-injure. The perceived influence of interpersonal situations reflects interpersonal functions of NSSI (Taylor et al., 2018). NSSI is sometimes engaged to communicate pain to other people (Taylor et al., 2018) and is less likely to be engaged in when people consider that they feel connected to other people (Assavedo & Anestis, 2016), as was expressed by participants.
The often-solitary nature of NSSI engagement (Victor & Klonsky, 2018) was reflected in the physical contexts in which people perceived it would be difficult or easier to engage in NSSI. People reported being alone when they self-injured and usually in a perceivably safe and private location (e.g. bathroom, bedroom). Likewise, participants found it easier to resist NSSI when in public or around other people. Participants noted that seeing other people’s self-injury scars or engaging with media (e.g., images, songs) which depicted or reminded people of self-injury could make it difficult to resist an urge to self-injure. In previous studies, participants with a history of self-injury have reported that viewing images online can act as a replacement to engaging in self-injury but can also trigger urges to engage in NSSI (Lewis & Seko, 2016).
Phase Two: Item Reduction and Psychometric Evaluation
The 125 items developed in Phase One reflect contexts in which self-efficacy to resist NSSI may vary. The aim of Phase Two was to reduce the item pool and test the internal structure of the scale. Additionally, convergent and discriminant validity were assessed using similar but distinct constructs, such as self-esteem and locus of control (Chen et al., 2004; Joo et al., 2013; Tatnell et al., 2014), as well as general self-efficacy (Hasking et al., 2018), emotion regulatory self-efficacy (Hasking et al., 2017, 2018), and the adapted measure previously used to assess self-efficacy to resist NSSI (Czyz et al., 2014). Measurement invariance across people with and without a history of self-injury was also assessed.
Method
Participants
Participants were 650 Australian university students recruited from 42 Australian universities. They were aged between 17–40 years (M = 21.14, SD = 2.32) and the majority (n = 486, 74.8%) were female; 147 (22.6%) were male and 15 (2.3%) identified as “another gender”. Two participants (0.3%) preferred not to disclose their gender. Thirteen (2.0%) participants identified as Aboriginal or Torres Strait Islander. Most participants (94.6%) were enrolled in undergraduate studies.
Materials
Self-Efficacy to Resist NSSI Scale
The 125 items developed in Phase One were administered to participants.
Nonsuicidal Self-Injury
As in Phase One, the Inventory of Statements About Self-Injury (ISAS; Klonsky & Glenn, 2009) was used to assess participants’ engagement in self-injurious behaviours.
Adapted Self-Efficacy to Avoid Suicide Action Scale
Czyz et al.’s (2014) measure has previously been adapted to measure self-efficacy to resist NSSI (Dawkins et al., 2018, 2019; Hasking, 2017; Hasking & Boyes, 2017; Hasking & Rose, 2016). The six-item scale asks participants to indicate, on a scale of 1 (very uncertain) to 6 (very certain), how certain they are that they could resist the urge to self-injure in the future (e.g. How certain are you that you could resist the urge to self-injure if you lost an important relationship?). A total score is calculated with higher scores indicating stronger self-efficacy to resist NSSI. Czyz et al.’s original measure has strong convergent validity being correlated with suicidal ideation (r = -0.59; p < 0.001) and evidencing strong internal consistency α = 0.96. The adapted NSSI version also has demonstrated strong internal consistency previously α = 0.92 (Hasking & Rose, 2016) and in the current study \(\alpha\) = 0.94.
General Self-Efficacy
Participants’ level of general self-efficacy was measured using Schwarzer and Jerusalem’s (1995) General Self-Efficacy Scale. This 10-item scale asks participants to indicate, on a four-point Likert scale from 1 (not at all true) to 4 (exactly true), their perceived ability to cope with daily stressors and adapt after stressful events (e.g., I am confident that I could deal efficiently with unexpected events). A total score is calculated with a higher score indicating stronger general self-efficacy. Internal consistency in the current sample was high \(\alpha\) = 0.90. General self-efficacy is associated with NSSI (Tatnell et al., 2014) and self-efficacy to resist NSSI (Hasking et al., 2017, 2018).
Emotion Regulation Self-Efficacy
Caprara et al.’s (2008) Regulatory Emotional Self-Efficacy (RESE) scale was used to measure participants’ belief in their ability to regulate their emotional experience. The 12-item scale asks participants to indicate, on a Likert scale of 1 (not well at all) to 5 (very well), their perceived capability to express positive emotions (positive: 4 items, e.g. How well can you express joy when good things happen to you?), manage feelings of despondency (despondency: 4 items, e.g. How well can you keep from getting discouraged in the face of difficulties?), and manage feelings of anger (anger: 4 items, e.g. How well can you avoid flying off the handle when you get angry?). Items are totalled for each subscale with higher scores indicating a stronger belief in the ability to express positive emotion, manage distress, and manage anger. The three subscales have previously demonstrated adequate internal consistency: positive \(\alpha\) = 0.64-0.85; despondency \(\alpha\) = 0.72-0.82; anger \(\alpha\) = 0.68-0.73 (Caprara et al., 2008). In the current sample Cronbach’s alphas were: positive = 0.88; despondency = 0.87; and anger = 0.81. Given emotion regulation is a common function of NSSI, it is unsurprising that emotion regulatory self-efficacy is associated with engagement in NSSI and self-efficacy to resist NSSI (Hasking et al., 2017, 2018). It would be expected that these constructs are correlated but distinct from one another.
Locus of Control
The Locus of Control of Behaviour Scale (Craig et al., 1984) was used to measure participants’ perception of their perceived control over their behaviours. Participants respond on a 6-point Likert scale, from 1 (strongly disagree) to 6 (strongly agree), how much they agree with 17 statements about their “personal beliefs” which indicated their perceived control over their lives (e.g., My life is controlled by outside actions and events; Everyone knows that luck or chance determine one’s future). Seven items are reverse coded, and the total score indicates the level of external locus of control an individual has, with higher scores indicating more external locus of control and lower scores indicating more internal locus of control. Internal consistency in the current sample was \(\alpha\) = 0.80.
Self-efficacy and locus of control are both expectancies but are distinct in that one is an assessment of capability (self-efficacy) while the other is assessment of control over outcomes (locus of control). Although it has not been evaluated in relation to NSSI, locus of control and self-efficacy are generally related in terms of predicting learning outcomes (Joo et al., 2013) and play related but distinct roles in abstaining from alcohol use (Soravia et al., 2015).
Self-Esteem
The Rosenberg self-esteem scale was used to measure participants’ overall self-esteem (Rosenberg, 1965). The 10-item scale asks participants to indicate, on a scale of 1 (strongly disagree) to 4 (strongly agree), how much they agree with each statement (e.g., On the whole, I am satisfied with myself; I certainly feel useless at times). Four items are reverse scored, and a total score calculated with higher scores indicating higher self-esteem. Internal consistency in the current sample was \(\alpha\) = 0.92.
Self-esteem and self-efficacy are considered under an umbrella of self-evaluations but are distinct constructs in that one is an evaluation of capability (self-efficacy) while the other is an evaluation of self-worth (self-esteem; Chen et al., 2004). Having lower self-esteem and weaker self-efficacy are associated with engagement in NSSI (Tatnell et al., 2014).
Procedure
This study was part of a larger study exploring cognitive and emotional constructs related to NSSI. Participants were recruited through an online portal where studies available for participation are advertised to students for course credit. The study was also advertised on social media (e.g., Facebook, Reddit) for the chance to win an iPad. Any student interested in participating was directed to an information sheet via Qualtrics. Information regarding the aims, participation requirements, confidentiality, and data storage was provided before students who wished to participate could provide informed consent. Participants were able to complete the study in a time and place of their choosing. The survey took approximately 45 min to complete. Once completed participants were able to download information about NSSI, stress reduction, and support services available.
Results
Preliminary Results
Missing values analysis revealed less than 5% missing data across variables. Data was not missing completely at random, \(\chi\) 2 (12,027) = 15,777.43, p < 0.001, however, all variables had less than 1% missing data. Considering the small percentage of missing data, Expectation Maximisation was used to impute these data (Tabachnick & Fidell, 2013). Of the full sample 297 (45.69%) reported a lifetime history of NSSI. Cutting (51.2%) was the most frequently reported main form of self-injury, followed by self-battery 11.6%), and severe scratching (10.9%). The mean age of NSSI onset was 13 years old (SD = 2.97). Gender (binary male/female)Footnote 2 was related to NSSI \(\chi\) 2(1, N = 629) = 45.90, p < 0.001, with females (52.4%) more likely to report a history of self-injury than males (20.5%). Age was not significantly related to history of self-injury t(634) = 1.41, p = 0.161.
Participants with a history of NSSI reported having engaged in self-injury between 1 and 22,337 times in their lives (M = 659, SD = 2516.67) and 195 reported that the last time they had engaged in self-injury was within the past 12 months with 95 having engaged more than five times in the past 12 months.
Factor Structure
Confirmatory Factor Analysis
Confirmatory Factor Analysis (CFA) was conducted using MPlus version 8 (Muthén & Muthén, 2017). As expected, items were negatively skewed (-0.197−-2.341) so Maximum Likelihood with Robust Standard Errors was used as the estimator. Items were hypothesised to load onto the 8 factors they were developed to represent, as outlined in Phase 1. Model fit was assessed using the following fit indices: Comparative fit indices (CFI) above 0.90; and Root Mean Square Error of Approximation (RMSEA), and Standardized Root Mean Square Residual (SRMR) close to or below 0.08. Items were developed to tap into these themes and theorised to correlate as factor scores. Testing this model revealed poor model fit \({\chi }^{2}(7617)\) = 27,990, p < 0.001; RMSEA = 0.064; CFI = 0.714; SRMR = 0.091.
Exploratory Factor Analysis
Given poor fit of the hypothesised model, the data were randomly divided, with one half used to conduct Exploratory Factor Analysis, and the other half used to confirm these factors using another Confirmatory Factor Analysis. Parallel analysis and principal axis factoring (PAF) with Promax (oblique) rotation was used, as the factors were assumed to be correlated. Factors with eigenvalues above 1 and visual inspection of the inflection point on the scree plot were used to determine the number of factors. Items were only included if they loaded on a single factor at above 0.30, did not cross-load, had high communalities, and were conceptually coherent (Costello & Osborne, 2005).
Principal axis revealed seven factors with eigenvalues exceeding 1. After inspection of the scree plot and the items loadings on the factors, it appeared the three factors with eigenvalues exceeding two made the most conceptual sense and accounted for 72.5% of the variance in the questionnaire. A three-factor solution was requested, and cross-loading items were removed leaving 103 items. Parallel analysis confirmed the three-factor solution. As the third factor had 8 items, we chose the eight highest loading, theoretically relevant, items for each of the other factors. The first factor reflected contexts in which it may be difficult to resist self-injury (Risk contexts, e.g., When I think I am a burden to someone else), the second reflects contexts in which it may be perceived as easier to resist engaging in self-injury (protective contexts, e.g., When I feel in control of my situation), and the third reflected times at which there were reminders of self-injury (Contexts which remind individuals of NSSI; e.g. When I see my own scars). A final PAF of the final 24 items was conducted in which the factors accounted for 77.78% of the variance in the data (Table 1). All subscales demonstrated internal consistency (Table 1).
Confirmatory Factor Analysis of Reduced Items
CFA, using Maximum Likelihood with Robust Standard Errors as the estimator, was conducted on the reduced item pool. Residuals were allowed to correlate within (but not across) factors. We found the model fit the data well, \(\chi\) 2 = 313.271, df = 171, p < 0.001; CFI = 0.971 RMSEA = 0.050; SRMR = 0.043. See Table 2 for factor loadings. Although factors correlated (Table 2), these were stronger for people with no history of self-injury p < 0.001.
Scale Validation
All subscales were positively correlated with Czyz et al.’s (2014) measure, general self-efficacy, and two of the emotion regulatory self-efficacy subscales (i.e., positive, anger; Table 3). Risk contexts and reminders of NSSI were positively correlated with the third (i.e., despondency subscale. All subscales were positively correlated with self-esteem and more self-efficacy on each subscale was related to internal locus of control.
Measurement Invariance
Measurement invariance of the final scale was assessed across people with (n = 297) and without (n = 353) a history of NSSI using MPlus version 8 (Muthén & Muthén, 2017). Multiple Group Confirmatory Factor Analysis was used to test measurement invariance and model fit was assessed using Maximum Likelihood Estimation with Robust Standard Errors. Measurement invariance was supported if the configural model had adequate fit, and the subsequent models had changes in CFI of < 0.01, RMSEA of < 0.015, and SRMR of < 0.030 (for metric invariance) or < 0.015 (for scalar or residual invariance; Chen, 2005). Scores on the self-efficacy to resist NSSI subscales were then compared between people with and without a history of NSSI.
The baseline model fit well for both groups of participants (Table 4). The configural, full metric, full scalar, and partial residual error invariance was supported. Full residual error invariance was not supported as indicated by change in CFI (Table 4). The residual error variances were larger in the group reporting NSSI compared to the group not reporting NSSI for items “When I feel connected to my body” (Residual Variance (no NSSI) = 0.110 vs. Residual Variance (NSSI) = 0.303), “When I know I can talk to a friend about my problem” (Residual Variance (no NSSI) = 0.127 vs. Residual Variance (NSSI) = 0.289), “When I am out with friends” (Residual Variance (no NSSI) = 0.080 vs. Residual Variance (NSSI) = 0.236), “When I am motivated to resist self-injury” (Residual Variance (no NSSI) = 0.74 vs. Residual Variance (NSSI) = 1.01), “It is difficult for me to reveal my innermost feelings, even to my close friends’ (Residual Variance (no NSSI) = 0.098 vs. Residual Variance (NSSI) = 0.379), and “When I see my own injuries” (Residual Variance (no NSSI) = 0.045 vs. Residual Variance (NSSI) = 0.242). The residual error variance was larger in the group not reporting NSSI compared to the group reporting NSSI for the item “When I don’t want to live” (Residual Variance (no NSSI) = 0.715 vs. Residual Variance (NSSI) = 0.393).
Group Differences
To assess whether self-efficacy to resist NSSI varied between groups and within groups a 2 (Group: History of NSSI; no history of NSSI) \(\times\) 3 (Self-efficacy to resist NSSI: risk contexts; protective contexts; NSSI reminders) mixed model ANOVA was conducted. Due to the assumption of sphericity being violated Huynh–Feldt correction was applied. Overall, participants with a history of self-injury (M = 23.15, 95% CI = 22.49–23.81) had significantly weaker self-efficacy to resist NSSI than people who had never engaged in NSSI (M = 27.99, 95% CI = 27.38–28.6), F(1, 643) = 112.69, p < 0.001, \(\eta\) 2 = 0.15.
There was significant variation in self-efficacy to resist NSSI across contexts, F(1.90, 1220.17) = 554.73, p < 0.001, \(\eta\) 2 = 0.46, with participants holding weaker self-efficacy to resist NSSI when in risk contexts (M = 21.92, 95% CI = 21.37–22.49) compared to protective contexts (M = 28.79, 95% CI = 28.19–29.19), p < 0.001, and reminders of NSSI (M = 25.99, 95% CI = 25.45–26.53), p < 0.001. Self-efficacy to resist NSSI when reminded of NSSI was significantly weaker than when in risk contexts, p < 0.001.
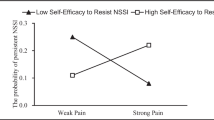
There was also a significant interaction between history of NSSI and self-efficacy to resist NSSI in different contexts, F(1.90, 643) = 133.52, p < 0.001, \(\eta\) 2 = 0.17 (Table 5). Pairwise comparisons revealed significant differences for both groups with self-efficacy to resist NSSI when in risk contexts weakest, followed by reminders of NSSI, with self-efficacy to resist NSSI when in protective contexts being strongest. Inspection of group means indicated that these differences are larger for people who had a history of engaging in NSSI.
Predicting NSSI History
An exploratory binary logistic regression was conducted to investigate whether the subscales developed accounted for unique variance above and beyond the amended self-efficacy to avoid suicide action scale when predicting history of NSSI. The assumption of multicollinearity was met (VIF = 1.82 – 3.49). The full model differentiating people who had engaged in NSSI from those who had not was statistically significant, χ2(8, N = 645) = 249.78, p < 0.001, predicting between 32.1% (Cox & Snell R2) and 42.9% (Nagelkerke R2) of the variance. A history of NSSI engagement was associated with weaker self-efficacy to resist NSSI as measured by the “risk contexts” subscale and the amended self-efficacy to avoid suicide action scale (Table 6).
NSSI Frequency and Recency
To explore the relationship between self-efficacy to resist NSSI and the frequency and recency of engagement in NSSI among people with a history of NSSI, we considered the relationships between lifetime frequency of NSSI and 12-month frequency of NSSI with self-efficacy to resist NSSI. Bivariate correlations indicated that lifetime frequency of NSSI was significantly negatively correlated with both the risk context subscale and the reminder of NSSI subscale (Table 3). However, there was no significant relationship between self-efficacy to resist NSSI in protective contexts and lifetime frequency of NSSI.
To further assess the relationship between the frequency and recency of NSSI with self-efficacy to resist NSSI, we created 3 groups: people who had not self-injured in the past 12 months; people who had self-injured 1–4 times in the past 12 months; and people who had self-injured 5 or more times in the past 12 months. To assess whether self-efficacy to resist NSSI varied between groups and within groups a 3 (12-month engagement: no self-injury; 1–4 incidents of self-injury; 5 + incidents of self-injury) \(\times\) 3 (Self-efficacy to resist NSSI: risk contexts; protective contexts; NSSI reminders) mixed model ANOVA was conducted.
Overall, participants level of self-efficacy was significantly associated with how many times they had self-injured in the past 12 months, F(1, 272) = 28.07, p < 0.001, \(\eta\) 2 = 0.17. Pairwise comparisons revealed that people who had not self-injured in the past 12 months (M = 25.62, 95% CI = 24.60 – 26.63) reported significantly stronger self-efficacy that people who had self-injured in the past 12 months between 1 and 4 times (M = 23.12, 95% CI = 21.96 – 24.27) and those who had self-injured more than 5 times in the past 12 months (M = 20.04, 95% CI = 18.98 – 21.10).
There was significant variation in self-efficacy to resist NSSI across contexts, F(2, 272) = 28.07, p < 0.001, \(\eta\) 2 = 0.17, with participants holding weaker self-efficacy to resist NSSI when in risk contexts (M = 17.46, 95% CI = 16.69–18.23) compared to protective contexts (M = 27.88, 95% CI = 27.28–28.48), p < 0.001, and reminders of NSSI (M = 23.43, 95% CI = 22.59–24.27), p < 0.001. Self-efficacy to resist NSSI when reminded of NSSI was significantly weaker than when in risk contexts, p < 0.001.
There was also a significant interaction between the recency of engagement in NSSI and self-efficacy to resist NSSI in different contexts, F(4, 544) = 18.10, p < 0.001, \(\eta\) 2 = 0.12. Pairwise comparisons revealed that self-efficacy to resist NSSI in risk contexts was significantly stronger for people had self-injured 5 or more times in the past 12 months when compared to people who had self-injured 1–4 times and those who had not self-injured in the past 12 months (Table 7). People who had self-injured 1–4 times had significantly stronger self-efficacy than people who had self-injured 5 or more times.
When considering protective contexts, there was no difference in self-efficacy when comparing people who had self-injured 1–4 times and people who had not self-injured in the past 12 months (Table 7). People who had self-injured 5 or more times had significantly weaker self-efficacy to resist NSSI when in protective contexts than people who had not self-injured in the past 12 months and those who had self-injured less than 5 times.
When faced with reminders of NSSI, people who had not self-injured in the past 12 months had significantly stronger self-efficacy to resist self-injury compared to people who had self-injured 1–4 times and people who had engaged in NSSI 5 or more times (Table 7). People who had self-injured 1–4 times had significantly stronger self-efficacy to resist NSSI when compared to people who had self-injured 5 or more times in the past 12 months.
Variations in self-efficacy across contexts were significant within each group (Table 7). For each group, self-efficacy was reported to be stronger in protective contexts, followed by when reminded of NSSI, with the weakest self-efficacy reported for risk related context.
Discussion
Recently, self-efficacy to resist NSSI has become a concept of interest in understanding cognitive factors associated with self-injurious behaviours (Dawkins et al., 2018, 2019; Hasking et al., 2017, 2018). Initial evidence for the role of self-efficacy to resist NSSI provides a basis for future research into specific NSSI-related cognitions. Previous studies have used an adapted version of Czyz et al. (2014) single dimension Self-Efficacy to Avoid Suicide Action Scale to measure self-efficacy to resist NSSI. However, in measuring self-efficacy, it is important to consider the situations or contexts which may influence an individual’s confidence in their ability to engage in or avoid the specific behaviour (Bandura, 1997, 2006). We developed a behaviour-specific measure of self-efficacy to resist NSSI which assesses three contexts in which self-efficacy may vary: contexts which it may be difficult to resist NSSI (risk contexts); contexts where it may be easier to resist NSSI (protective contexts) and contexts where people are reminded of self-injury. We also conducted preliminary validation of the scale and assessed measurement invariance across people with and without a history of NSSI.
The resulting three-factor structure reflects different contexts in which self-efficacy to resist NSSI may vary (Bandura, 1997, 2006). Rather than representing specific “types” of contexts (e.g., emotional, physical) as identified in Phase One, two of the resulting factors represent collective contexts which appear to reflect the impact they have on self-efficacy rather than the context itself (i.e., risk and protective contexts). The final factor reflected the theme “reminders of self-injury” identified in Phase One suggesting that the presence of NSSI-related stimuli or reminders of self-injury are distinct from other contexts surrounding NSSI. Validity of the subscales was suggested through correlations with measures of general and emotion regulation self-efficacy. Weak correlations with related but distinct constructs of self-esteem and locus of control provide some initial indication of discriminant validity. Additionally, the subscales discriminated between people with and without a history of self-injury, providing further evidence of discriminant validity.
The Risk Contexts subscale reflects contexts in which people believe it would be more difficult to resist the urge to self-injure such as feelings of depression and anxiety, negative thoughts or thought patterns, thoughts of wanting to die, and strong urges to self-injure. This subscale mirrored the previously used adapted version of the self-efficacy to resist suicide action scale (Czyz et al., 2014) as its items also reflect situations which may be considered risk factors for suicide/NSSI. In line with previous studies (Dawkins et al., 2018, 2019; Hasking, 2017; Hasking & Rose, 2016), people who had self-injured held weaker beliefs in their ability to resist NSSI than people who had never self-injured when faced with distressing thoughts, feelings, and/or situations. When exploring self-efficacy among people with a history of self-injury, more recent and frequent self-injury was related to having weaker self-efficacy to resist NSSI.
Self-efficacy to resist NSSI when in protective contexts relates to the belief people have in their ability to resist NSSI when they are with other people, when they feel supported, and when they are motivated to resist self-injury. When considering protective contexts, people with a history of self-injury had less confidence in their ability to resist NSSI than people who had never self-injured. However, they had more confidence that they could resist self-injury in protective contexts than when in risk contexts or when reminded of self-injury. Among people with a history of self-injury, people with the most recent and frequent engagement held weaker belief in their ability to resist NSSI in protective contexts than people with less recent or frequent engagement in NSSI. Self-efficacy beliefs have been found to be a significant predictor of future behaviour when treating substance abuse (Chavarria et al., 2012; Kadden & Litt, 2011). If individuals are trying to reduce their engagement in NSSI, it is possible that there will be an increase in confidence to resist NSSI in protective contexts before they believe they can resist NSSI in more difficult situations. In a clinical setting this could indicate a future change in behaviour and may be used to identify protective situations that could help reduce an urge to engage in self-injury.
Having strong self-efficacy to resist NSSI when in protective contexts was associated with participants believing they could express positive emotions and manage feelings of anger but was not associated with confidence to manage feelings of depression. People who self-injure tend to report less positive emotion generally (Boyes et al., 2019) and experience less physiological response to positively valanced stimuli than people who have not self-injured (Tatnell et al., 2017). Perhaps if an individual does not believe they can express positive emotions, then situations which are perceivably positive may not be experienced as intensely, and not be perceived as protective.
The final subscale reflects contexts in which people were reminded of self-injury. Items included seeing images of self-injury, seeing other people’s injuries, and seeing your own injuries. While accounting for only a small proportion of variance (4.69%), this subscale was differentiated from risk contexts indicating that exposure to NSSI stimuli is a salient context when considering an individual’s belief in their ability to resist NSSI. Both people with, and without, a history of NSSI perceived that it would be more difficult to resist self-injury when reminded of self-injury than when they were in protective contexts, but less difficult than when they were in risk contexts. This may indicate that avoiding or reducing exposure to NSSI stimuli when trying to resist NSSI may be helpful. Previous studies have identified that engagement with self-injury content online may maintain self-injury or trigger an urge to self-injure (Jacob et al., 2017; Lewis & Seko, 2016). People with a history of self-injury have reported experiencing a physical reaction to images online, which work to trigger or intensify an urge to engage in self-injury (Jacob et al., 2017). However, there is also evidence that for some people engaging with NSSI-related content can have positive outcomes such as receiving encouragement in their recovery and finding that images of self-injury diminish an urge to self-injure (Lewis & Seko, 2016). The relationship between engaging with NSSI related content and engagement in NSSI may also change over time as previously seen when NSSI is associated with aversive stimuli (Franklin et al., 2016). It is possible that interpretation of this measure at an individual level could be useful to identify how people are engaging with NSSI-related content and how this may play a role in maintaining or ceasing NSSI.
Implications
The development of this measure has the potential to further theoretical understanding of NSSI. Findings are consistent with Bandura’s (1997) proposal that self-efficacy will vary in relation to the same behaviour across contexts and confirms the need to develop behaviour-specific measures of self-efficacy. The ability to measure self-efficacy to resist NSSI in varying contexts will allow predictions of the Cognitive Emotion Model of NSSI (Hasking et al., 2017, 2018) to be tested. Specifically, it will allow testing of how self-efficacy to resist NSSI in different contexts may work with NSSI-related outcome expectancies, emotional experiences, and emotion regulation in predicting NSSI. Measuring these concepts in longitudinal studies through onset, maintenance, cessation, and recovery from NSSI will allow us to see how these thoughts and beliefs change and work together over time. Ecological momentary assessment would also provide insight into the salience of these beliefs in different contexts and in the lead up to and following when NSSI is engaged. Changes in cognitions may indicate individuals at risk of future engagement of self-injury providing opportunity for early intervention.
The scale may also be useful in clinical practice. Behaviour change, including in treatment of NSSI, is often characterised by ambivalence which treatment protocols often try to address (Andover et al., 2015). Within motivational interviewing, the goals are to increase motivation and encourage commitment to change (Rollnick & Miller, 1995). Within this context this measure could be useful in identifying cognitive changes that suggest a future change in behaviour before it can be seen. If self-efficacy to resist NSSI is found to predict future behaviour, as has been found with measures of self-efficacy to avoid substance use (Chavarria et al., 2012; Kadden & Litt, 2011), this measure could be used as an indicator of change. The measure may also be useful in clinical settings to assess (at an item level) when it is more difficult to resist self-injury, identifying treatment targets. It can be used to identify contexts which may limit the likelihood of engaging in NSSI for clients who would like to stop injuring themselves.
As engaging with NSSI-related content online can reduce or increase the likelihood of engaging in NSSI (Lewis & Seko, 2016), having a measure that assesses whether being reminded of NSSI is seen to make it difficult or easier to resist an urge to self-injure could be helpful. It could open up discussion in a clinical setting about how reminders of NSSI affect the individual. Clients may be encouraged to avoid content which trigger urges to self-injure or promote stigma of NSSI while moving towards content, which encourages recovery or diminishes an urge to self-injure (Lewis & Seko, 2016).
Limitations and Directions for Future Research
Due to the scale being validated with university students, the measure will need to be validated in other populations in which self-injury is prevalent (e.g., adolescents, clinical settings). Compared to the amended version of the self-efficacy to avoid suicide action the current measure accounted for added variance when differentiating history of NSSI. However, this exploratory analysis needs replication to substantiate the performance of the new measure in accounting for variance in engagement in NSSI. The risk contexts subscale was the only subscale to differentiate participants by NSSI history when all were included in the binomial regression. The salience of this subscale is possibly due to it representing the contexts in which people are more likely to engage in self-injury and therefore more likely to differentiate them from people who have not self-injured. Additional exploration is needed to understand the influence that potential shared variance may play in the role of each subscale in differentiating history of self-injury.
Exploration of the utility of each subscale with regards to the structure of the measure and their contribution to understanding NSSI is also needed. Future studies could also explore the association between different aspects of self-efficacy to resist NSSI and the recency and frequency of NSSI among people who self-injury. Further exploration of the use of the measure in clinical settings will be needed to determine whether the measure is sensitive to change, and valid to use as an indicator of change across treatment. Considering the high correlations between factors, psychometric work is needed to confirm the factor structure of the measure. A total score has not been explored within this study. Merging subscales could provide a false sense of an individual’s self-efficacy as high self-efficacy in protective contexts would likely “cancel out” weaker self-efficacy in other contexts. As the sample was primarily female, future studies should examine measurement invariance across gender. Longitudinal data could look at both reliability and sensitivity to change to assess the utility of the measure in both research and clinical settings. We have not considered whether participants are motivated to resist an urge to engage in self-injury. It is likely that the measure will only be predictive of behaviour if someone wants to resist an urge. An individual could think that they could resist an urge to self-injure but have no intention of doing so. In clinical settings it will be imperative to ask people their intentions as well as assess their confidence that they could resist an urge to self-injure.
Conclusion
We developed a measure of self-efficacy to resist NSSI and validated it among university students. The underlying structure of the measure indicated three differing contexts in which an individual’s belief in their ability to resist NSSI may differ. The measure will further research into the role of self-efficacy in NSSI, and how it fits into the Cognitive-Emotional Model of NSSI. Future research validating the measure in clinical samples could provide evidence that this measure can be used as an indicator of change in clinical settings.
Availability of Data and Material
We do not have permission from participants to make the data publically available.
Notes
Demographic data for expert participants has not been presented to maintain confidentiality.
People who identified as “another gender” (n = 15) and people who preferred not to disclose their gender (n = 2) could not be included in the analysis due to the small group size.
References
Andover, M. S., Schatten, H. T., Morris, B. W., & Miller, I. W. (2015). Development of an intervention for nonsuicidal self-injury in young adults: An open pilot trial. Cognitive and Behavioral Practice, 22, 491–503. https://doi.org/10.1016/j.cbpra.2014.05.003
Assavedo, B. L., & Anestis, M. D. (2016). The relationship between non-suicidal self-injury and both perceived burdensomeness and thwarted belongingness. Journal of Psychopathology and Behavioral Assessment, 38, 251–257. https://doi.org/10.1007/s10862-015-9508-8
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Prentice Hall.
Bandura, A. (1997). Self-Efficacy: The exercise of control. W. H. Freeman & Co.
Bandura, A. (2006). Guide for constructing self-efficacy scales. In F. Pajares & T. Urdan (Eds.), Self-efficacy beliefs in adolescents (pp. 307–337). Information Age Publishing.
Boyes, M., Wilmot, A., & Hasking, P. (2019). Non-suicidal self-injury-related differences in the experience of negative and positive emotion. Suicide and Life Threatening Behaviour.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. https://doi.org/10.1191/1478088706qp063oa
Caprara, G. V., Di Giunta, L., Eisenberg, N., Gerbino, M., Pastorelli, C., & Tramontano, C. (2008). Assessing regulatory emotional self-efficacy in three countries. Psychological Assessment, 20, 227–237. https://doi.org/10.1037/1040-3590.20.3.227
Chavarria, J., Stevens, E. B., Jason, L. A., & Ferrari, J. R. (2012). The effects of self-regulation and self-efficacy on substance use abstinence. Alcohol Treatment Quarterly, 30, 422–432. https://doi.org/10.1080/07347324.2012.718960
Chen, F. F. (2005). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14, 464-504. https://doi.org/10.1080/10705510701301834
Chen, G., Gully, S. M., & Eden, D. (2004). General self-efficacy and self-esteem: Toward theoretical and empirical distinction between correlated self-evaluations. Journal of Organizational Behavior, 25, 375–395. https://doi.org/10.1002/job.251
Costello, A. B., & Osbourne, J. (2005). Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research, and Evaluation, 10, 1-9. https://doi.org/10.31234/osf.io/c8zk2
Craig, A. R., Franklin, J. A., & Andrew, G. (1984). A scale to measure locus of control of behaviour. British Journal of Medical Psychology, 57, 173–180. https://doi.org/10.1111/j.2044-8341.1984.tb01597.x
Czyz, E. K., Bohnert, A. S., King, C. A., Price, A. M., Kleinberg, F., & Ilgen, M. A. (2014). Self-efficacy to avoid suicide action: Factor structure and convergent validity among adults in substance use disorder treatment. Suicide and Life Threatening Behviour, 44, 698–709. https://doi.org/10.1111/sltb.12101
Dawkins, J., Hasking, P., & Boyes, M. (2019). Thoughts and beliefs about nonsuicidal self-injury: An application of Social Cognitive Theory. Journal of American College Health., 69(4), 428–434. https://doi.org/10.1080/07448481.2019.1679817
Dawkins, J., Hasking, P., Boyes, M., Greene, D., & Passchier, C. (2018). Applying a cognitive-emotional model to nonsuicidal self-injury. Stress & Health, 35, 39–48. https://doi.org/10.1002/smi.2837
Franklin, J. C., Fox, K. R., Franklin, C. R., Kleiman, E. M., Ribeiro, J. D., Jaroszewski, A. C., Hooley, J. M., & Nock, M. K. (2016). A brief mobile app reduces nonsuicidal and suicidal self-injury: Evidence from three randomized controlled trials. Journal of Consulting and Clinical Psychology, 84(6), 544–557. https://doi.org/10.1037/ccp0000093
Glasofer, D. R., Haaga, D. A. F., Hannallah, L., Field, S. E., Kozlosky, M., Reynolds, J., & Tanofsky-Kraff, M. (2013). Self-efficacy beliefs and eating behavior in adolescent girls at-risk for excess weight gain and binge eating disorder. International Journal of Eating Disorders, 46(7), 663–668. https://doi.org/10.1002/eat.22160
Glenn, C. R., & Klonsky, E. D. (2011). Prospective prediction of nonsuicidal self-injury: A 1-year longitudinal study in young adults. Behavior Therapy, 42, 751-762. https://doi.org/10.1016/j.beth.2011.04.005
Gwaltney, C. J., Metrik, J., Kahler, C. W., & Shiffman, S. (2009). Self-efficacy and smoking cessation: A meta-analysis. Psychology of Addictive Behaviors, 23, 56–66. https://doi.org/10.1037/a0013529
Hasking, P. (2017). Differentiating non-suicidal self-injury and risky drinking: A role for outcome expectancies and self-efficacy beliefs. Prevention Science., 18(6), 694–703. https://doi.org/10.1007/s11121-017-0755-7
Hasking, P., & Boyes, M. (2017). The nonsuicidal self-injury expectancy questionnaire (NEQ): Factor structure and initial validation. Clinical Psychologist. https://doi.org/10.1111/cp.12127
Hasking, P., Boyes, M., & Greves, S. (2018). Self-efficacy and emotionally dysregulated behaviour: An exploratory test of the role of emotion regulatory and behaviour-specific beliefs. Psychiatry Research, 270, 335–340. https://doi.org/10.1016/j.psychres.2018.09.045
Hasking, P., & Rose, A. (2016). A preliminary application of social cognitive theory to nonsuicidal self-injury. Journal of Youth and Adolescence, 45, 1560–1574. https://doi.org/10.1007/s10964-016-0449-7
Hasking, P., Whitlock, J., Voon, D., & Rose, A. (2017). A cognitive-emotional model of NSSI: Using emotion regulation and cognitive processes to explain why people self-injure. Cognition and Emotion, 31(8), 1543–1556. https://doi.org/10.1080/02699931.2016.1241219
Hauber, K., Boon, A., & Vereiren, R. (2019). Nonsuicidal self-injury in clinical practice. Frontiers in Psychology, 10, 1–8. https://doi.org/10.3389/fpsyg.2019.00502
International Society for the Study of Self-Injury. (2018). What is self-injury? Retrival date 28/02/2020. Retrieved from: https://itriples.org/about-self-injury/what-is-self-injury
Jacob, N., Evans, R., & Scourfield, J. (2017). The influence of online images on self-harm: A qualitative study of young people aged 16–24. Journal of Adolescence, 60, 140–147. https://doi.org/10.1016/j.adolescence.2017.08.001
Joo, Y. J., Lim, K. Y., & Kim, J. (2013). Locus of control, self-efficacy, and task value as predictors of learning outcome in an online university context. Computers & Education, 62, 149–158. https://doi.org/10.1016/j.compedu.2012.10.027
Kadden, R. M., & Litt, M. D. (2011). The role of self-efficacy in the treatment of substance use disorders. Addictive Behaviour, 36, 1120–1126. https://doi.org/10.1016/j.addbeh.2011.07.032
Kiekens, G., Hasking, P., Boyes, M., Claes, L., Mortier, P., Auerbach, R., & Bruffaerts, R. (2018a). The associations between non-suicidal self-injury and first onset suicidal thoughts and behaviours. Journal of Affective Disorders, 239, 171–179. https://doi.org/10.1016/j.jad.2018.06.033
Kiekens, G., Hasking, P., Claes, L., Mortier, P., Auerbach, R. P., Boyes, M., & Bruffaert, R. (2018b). The DSM-5 nonsuicidal self-injury disorder among incoming college students: Prevalence and association with 12-month mental disorders and suicidal thoughts and behaviors. Depression and Anxiety, 35, 629–637. https://doi.org/10.1002/da.22754
Klonsky, E. D., & Glenn, C. R. (2009). Assessing the functions of non-suicidal self-injury: Psychometric properties of the inventory of statements about self-injury (ISAS). Journal of Psychopathological Behaviour Assessment, 31, 215–219. https://doi.org/10.1007/s10862-008-9107-z
Klonsky, E. D., & Olino, T. M. (2008). Identifying clinically distinct subgroups of self-injurers among young adults: A latent class analysis. Journal of Consulting and Clinical Psychology, 76, 22–27. https://doi.org/10.1037/0022-006X.76.1.22
Lewis, S., & Seko, Y. (2016). A double –edged sword: A review of benefits and risks of online nonsuicidal self-injury activities. Journal of Clinical Psychology, 72, 249–262. https://doi.org/10.1002/jclp.22242
Muthén, L. K., & Muthén, B. O. (2017). Mplus User’s Guide (8th ed.). Muthén & Muthén.
Oei, T. P., Hasking, P., & Philips, L. (2007). A comparison of general self-efficacy and drinking refusal self-efficacy in predicting drinking behaviour. The American Journal of Drug and Alcohol Abuse, 33, 833–842. https://doi.org/10.1080/00952990701653818
Oei, T. P., Hasking, P., & Young, R. M. (2005). Drinking refusal self-efficacy questionnaire-revised (DRSEQ-R): A new factor structure with confirmatory factor analysis. Drug and Alcohol Dependence, 78, 297–307. https://doi.org/10.1016/j.drugalcdep.2004.11.010
Rollnick, S., & Miller, W. R. (1995). What is motivational interviewing? Behavioural and Cognitive Psychotherapy, 23, 325–334. https://doi.org/10.1017/S135246580001643X
Rosenberg, M. (1965). Society and the adolescent self-image. Prnceton University Press.
Schwarzer, R., & Jerusalem, M. (1995). Generalized Self-Efficacy scale. In J. Weinman, S. Wright, & M. Johnston (Eds.), Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: NFER-NELSON.
Soravia, L. M., Schlafli, K., Stutz, S., Rosner, S., & Moggi, F. (2015). Resistance to temptation: The interaction of external and internal control on alcohol use during residential treatment for alcohol use disorder. Alcoholism: Clinical and Experimental Research, 39, 2209–2214. https://doi.org/10.1111/accr.12880
Swannell, S. V., Martin, G. E., Page, A., Hasking, P., & St John, N. J. (2014). Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide and Life-Threatening Behaviour, 44, 273–303. https://doi.org/10.1111/sltb.12070
Tabachnick, B. G., & Fidell, L. S. (2013). Using Multivariate Statistics (6th ed.). Pearson.
Tatnell, R., Hasking, P., Lipp, O., Boyes, M., & Dawkins, J. (2017). Emotional responding in NSSI: Examinations of appraisals of positive and negative emotional stimuli, with and without acute stress. Cognition and Emotion, 32, 1304–1316. https://doi.org/10.1080/02699931.2017.1411785
Tatnell, R., Kelada, L., Hasking, P., & Martin, G. (2014). Longitudinal analysis of adolescent NSSI: The role of intrapersonal and interpersonal factors. Journal of Abnormal Child Psychology, 42, 885–896. https://doi.org/10.1007/s10802-013-9837-6
Taylor, P. J., Jomar, K., Dhingra, K., Forrester, K., Shahmalak, U., & Dickson, J. M. (2018). A meta-analysis of the prevalence of different functions of non-suicidal self-injury. Journal of Affective Disorders, 227, 759–769. https://doi.org/10.1016/j.jad.2017.11.073
Victor, S. E., & Klonsky, E. D. (2018). Understanding the social context of adolescent nonsuicidal self-injury. Journal of Clinical Psychology, 74, 2107–2116. https://doi.org/10.1002/jclp.22657
Funding
JD is supported by an Australian Government Research Training Program Scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The research protocol was approved by the Human Research Ethics Committee at XXX University.
Consent to Participate
All participants provided informed consent before participating in any part of the study.
Conflict of Interest
Jessica C. Dawkins, Penelope A. Hasking and Mark E. Boyes declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dawkins, J.C., Hasking, P.A. & Boyes, M.E. Development and Validation of a Measure of Self-Efficacy to Resist Nonsuicidal Self-Injury. J Psychopathol Behav Assess 44, 511–526 (2022). https://doi.org/10.1007/s10862-021-09935-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-021-09935-7