Abstract
The purpose of the current study was to extend research on the Personality Disorder (PD) Spectra scales developed for the Minnesota Multiphasic Personality Inventory-2-Restructured Form (MMPI-2-RF). We evaluated the scales against measures of both the DSM-5 Section II (traditional model) and Section III (Alternative Model of Personality Disorders; AMPD) PD diagnostic criteria. The participants were 474 undergraduate students from the University of Otago who were administered a range of measures for both DSM-5 PD models. The MMPI-2-RF PD Spectra scales showed significant moderate to large correlations with traditional PD measures, with the exception of Histrionic PD, as well as evidenced incremental validity over the MMPI-2-RF Personality Psychopathology-5 (PSY-5) – the only current formal measurement of personality pathology on the MMPI-2-RF- in accounting for scores on traditional PD measures. The MMPI-2-RF PD Spectra scales also showed moderate to high correlations with most hypothesized AMPD personality trait and impairment scales used to assess DSM-5 AMPD diagnostic criteria. The findings indicated that the scales align well with both paradigms for PD assessment, situating the MMPI-2-RF in a unique position as a bridging measure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Accurate and valid assessment of Personality Disorders (PDs) is an issue of significant import for clinicians. PDs are chronic, pervasive mental health disorders, with an estimated prevalence of almost 15% in the United States alone (e.g., Grant et al., 2004). PDs often result in significant impairments for individuals and are also associated with many major public health problems. For example, Antisocial PD is highly associated with non-violent and violent criminal activities (Fridell et al., 2006) and individuals with Borderline PD are at high risk for suicidal behaviors (Hooley et al., 2012). Accurate assessment, diagnosis, and treatment of PDs is therefore essential to minimize their negative impact for both individuals and wider society. Furthermore, clinicians are busy and often do not have time to include a large number of diagnosis-specific measures in their armamentarium; therefore, the recent inclusion of PD spectra scales (Sellbom et al., 2018) on the Minnesota Multiphasic Personality Inventory 2-Restructured Form (MMPI-2-RF; Ben-Porath and Tellegen 2008/2011a), given the widespread use of the MMPI-2-RF in clinical practice, could facilitate such diagnosis. However, these scales require further validation before widespread use, and the current study was designed to begin to fill this gap.
The Diagnostic and Statistical Manual of Mental Disorders (5th ed. [DSM-5]; American Psychiatric Association, 2013) currently includes two different classification systems for PDs. Section II: Diagnostic Criteria and Codes holds the traditional categorical system for PD diagnosis, which classifies PDs as the manifestation of inflexible and maladaptive personality traits, which cause an individual significant functional impairment or distress. The validity and utility of the current categorical model in the DSM-5 has been widely debated throughout the literature, with a substantial body of research indicating a dimensional model is a more appropriate conceptualization of PDs (e.g., Hopwood et al., 2018; Skodol, 2012).
The Alternate Model of Personality Disorders (AMPD) was proposed as the formal model during the development of the DSM-5 but was ultimately placed in Section III: Emerging Measures and Models. In direct contrast to the current categorical model, the AMPD conceptualizes PDs dimensionally, recognizing that while all individuals have personality traits, extremely low or high levels of these traits are not always adaptive to everyday life (Skodol, 2012). New general criteria for PDs were introduced under the AMPD, requiring moderate or severe impairment in personality functioning, in addition to trait dysfunction (Skodol et al., 2011). The trait dysfunction is captured through five broad domains, encompassing Negative Affectivity, Detachment, Antagonism, Disinhibition and Psychoticism. Four PD diagnoses were also removed for the AMPD: Paranoid, Schizoid, Histrionic and Dependent PDs. A recent meta-analysis has revealed substantial overlap between the personality trait criteria of the AMPD and traditional PD diagnosis in a manner that aligns relatively well, albeit imperfectly, with the DSM-5 AMPD proposed configurations (Watters et al., 2019).
The inclusion of both the traditional model and AMPD in the DSM-5 provides clinicians two different models through which they can conceptualize and diagnose PDs. The majority of clinicians are likely to continue to use the traditional model for diagnosis because it is the official system of diagnosis, it is emphasized in current psychology training paradigms, and due to general clinical familiarity; however, the scientific PD literature provides far more support for the AMPD and related dimensional paradigms (Krueger & Markon, 2014). Therefore, there is a necessity for an assessment modality that is capable of not only catering to clinicians’ current needs (i.e., the traditional model), but is also in line with the current scientific progress (i.e., the AMPD). A modality that incorporates both the traditional model and the AMPD would facilitate the transition between the two models as the field progresses, by providing a ‘traditional’ operationalization of the AMPD diagnoses. Furthermore, incorporating such measure into an instrument already widely used by clinicians, such as the MMPI-2-RF, would provide particular utility as clinicians would not be required to learn the administration and interpretation of a new measure.
The MMPI-2-RF was designed to cover a more clinically relevant and contemporary range of psychopathology and maladaptive personality constructs than earlier MMPI versions (Ben-Porath, 2012). Previous iterations of the MMPI- instruments have included PD scales- modeled heavily on the DSM. Morey et al., (1985) developed a set of PD scales for the original MMPI, modelled after the DSM-III (American Psychiatric Association 1987) PD diagnostic criteria. These scales were updated by Levitt and Gotts (1995) to reflect the DSM-III-R PD diagnostic criteria. Somwaru and Ben-Porath (1995) developed their own PD scales to reflect the DSM-IV (American Psychiatric Association 1994) diagnostic criteria, based on the MMPI-2 items. None of these scale sets were formally included in the MMPI/MMPI-2 scoring, and none of them were converted for the MMPI-2-RF.
Sellbom et al. (2018) recently developed a set of scales for the MMPI-2-RF for the assessment of PDs. Specifically, these scales were to be a dimensional assessment of the traditional PD criteria, through what they termed “spectra scales”. The spectra terminology was used deliberately, as a representation of the perspective that PDs exist dimensionally, encompassing multiple facets of traits, symptoms and characteristics (Millon & Strack, 2015) bridging traditional DSM constructs with dimensional personality assessment. Moreover, Sellbom et al. (2018) argued for the clinical utility of having scales available for a psychometric evaluation popular with clinicians, to aid the diagnostic process, while assessing these constructs influenced by a dimensional trait perspective, making them palatable to PD scientists as well.
Sellbom et al. (2018) conducted two studies. First, they reported on the development and initial criterion validation of the PD spectra scales, and second, a study to examine broader construct validity of the PD spectra scales. Sellbom et al. (2018) observed generally good convergent validity, with the exception of the Schizoid PD Spectra scale. Discriminant validity was also found to be generally acceptable, however Schizoid PD scores showed a relatively large (negative) inter-correlation with Histrionic PD and a large inter-correlation with the Avoidant PD Spectra scales, thought to be due to the shared social avoidance variance exhibited in these PDs. The Obsessive-Compulsive PD spectra scale was moderately correlated with Paranoid, Borderline, Avoidant and Dependent PDs Spectra scales, indicating poor discriminant validity for the Obsessive-Compulsive Spectra scale. In the examination of the AMPD trait associations, the median convergent correlations were moderate to large for all scales except the Obsessive-Compulsive PD Spectra scale. Sellbom et al. (2018) cautioned that further validation of their spectra scales must be conducted before they are made available for clinical use.
The current study aimed to replicate and extend validation of Sellbom et al.’s (2018) MMPI-2-RF PD Spectra scales, through an examination of the associations between the MMPI-2-RF PD Spectra scales in a non-clinical sample from New Zealand. The latter is not trivial. The MMPI-2-RF is available in New Zealand for clinical use, yet the majority of research conducted on the MMPI-2-RF has occurred in North America. New Zealand’s cultural make-up is highly varied from that of North America, largely due to the sizeable indigenous Māori (15%) and Pacifica (7%) populations. New Zealand is also influenced by U.K. cultural values and norms to a far greater degree than North America. Therefore, while it is not unreasonable to expect the North American research would generalize to a New Zealand population, further empirical research is needed to validate this assertation. Moreover, the current study considered a more extensive set of measures of both the traditional model and those relevant to the AMPD as external criteria for the PD Spectra scales. It is important these scales are able to encapsulate both the traditional and AMPD diagnostic criteria given the purpose the purport to serve. It was hypothesized that each PD Spectra Scale would be most highly correlated with the corresponding traditional measure of PD, and less strongly correlated with the other PDs (for example, the Paranoid PD Spectra Scale would be most highly correlated with another measure of Paranoid PD, and less so with other PD scales). However, it was expected that discriminant validity may not be exhibited, due to PD measures often showing high levels of inter-correlations (e.g., Morey et al., 2015). Furthermore, the 10 PD Spectra scales are expected to provide incremental utility over the existing PSY-5 scales in predicting PD criterion scale scores (Sellbom et al. 2018). Failure to do so would have significant implication for the added utility of such scales to the MMPI-2-RF.
Associations between the MMPI-2-RF Spectra scales with AMPD traits and personality impairment were also examined. The AMPD traits were operationalized through an emerging assessment model, the CAT-PD, which includes measurement of the 25 AMPD traits along with eight additional traits deemed important to PDs but not fully covered within the current AMPD model. Hypotheses were developed as to which AMPD personality traits would be most highly correlated with each PD Spectra scale by examining both the DSM-5 traditional and AMPD diagnostic criteria. For example, it was hypothesized the Paranoid PD Spectra scale would be positively correlated with the traits of Anger, Hostile Aggression, and Mistrust. These traits are the most conceptually relevant to Paranoid PD and those identified for Paranoid PD during a trait to disorder crosswalk (Hopwood et al., 2012). The full set of a priori hypotheses are displayed in Table 3 (bolded correlations). It was further hypothesized that all PD Spectra scales would be positively correlated with personality impairment, in both individual impairment domains, and overall impairment. Finally, it was hypothesized that both the conceptually relevant traits and impairment would account for unique variance within the PD Spectra scales. These exploratory analyses were untaken to better understand the nature of what underlies the PD scales. Due to the assertion in the DSM-5 traditional model and AMPD that PDs result in both personality dysfunction and functional impairment (American Psychiatric Association, 2013), it is expected measures of both personality traits and impairment would account for unique variance within each of the PD Spectra scales.
Method
Participants
A sample of 529 university students were recruited through the University of Otago undergraduate psychology participation program. There were 116 men, 412 women and one participant who identified as transgender. The mean age was 19.71 years (SD = 2.74), ranging from 17 to 50 years old. The largest ethnic groups were 71.1% NZ European/Pākehā, 13.6% Other European (e.g., Australian, English, Scottish), and 9.2% Māori. Relationship demographics were as follows: 69.8% of participants were single, 29.6% had a serious relationship/partner, and 0.4% were married.
The MMPI-2-RF Cannot Say-revised (CNS-r), Variable Response Inconsistency-revised (VRIN-r), True Response Inconsistency-revised (TRIN-r), Infrequent Responses-revised (F-r) and Infrequent Psychopathology Responses-revised (Fp-r) validity scales were used to exclude participants who had invalid MMPI-2-RF profiles due to unscoreable, random, fixed indiscriminant or extremely deviant responding, to reduce the impact of measurement error. Fifty-five participants were excluded, resulting in a total of 474 participants remaining for the analyses. There were no significant group differences for included vs. excluded profiles in age, gender, or relationship status (p < 0.05). However, excluded participants were less likely to be NZ European/ Pākehā (χ2 [1, N = 530] = 6.328, p < .001, Cramer’s V = 0.11), though the associated effect size was small.
Measures
Descriptive statistics and internal consistency reliability estimates were calculated for each scale score and are reported in Supplemental Table S1 in the online supplemental materials.
Minnesota Multiphasic Personality Inventory-2-Restructured Form (MMPI-2-RF)
The MMPI-2-RF (Ben-Porath and Tellegen 2008/2011b) is a 338-item self-report questionnaire designed to cover a range of contemporary psychopathology and personality symptoms and traits. The items on the MMPI-2-RF are grouped into nine validity scales and 42 scales that measure substantive clinical content. The scales have been extensively validated across a number of settings and contexts (Sellbom, 2019). The MMPI-2-RF PD Spectra scales (Sellbom et al., 2018) and PSY-5 scales were used in the current study. These scales were designed to assess the 10 traditional PD syndromes in a dimensional manner, but with an aim of also incorporating the dimensional trait definitions of these disorders, as described earlier. The 10 scales consist of non-overlapping item sets derived from the MMPI-2-RF item pool, ranging from 12 (Obsessive-Compulsive) to 35 (Borderline) items. Cronbach’s alpha ranged from .67 (Obsessive-Compulsive) to .86 (Borderline); see Table 1.
The Assessment of DSM-IV Personality Disorders (ADP-IV)
The Assessment of DSM-IV Personality Disorders (ADP-IV; Schotte & De Doncker, 1994) is a 94-item self-report questionnaire, designed to assess DSM-IV PD criteria. All items are assessed on a “trait” scale, and a “distress” scale, in concordance with the conceptualization of PDs as trait dysfunctions, which results in distress for the individual and/ or others (Schotte & De Doncker, 1996). The trait questions were designed to correspond to a DSM-IV diagnostic criterion, and are measured dimensionally on a seven-point scale, from “totally disagree” to “totally agree”. If an individual answers in the range from “rather agree” to “totally agree”, they are referred to the distress scale. The trait scores were used in the current study. Schotte et al., (1998) reported acceptable internal consistency estimates for the ADP-IV scales and concurrent validity analyses were established using the Wisconsin Personality Disorders Inventory (WISPI; Klein et al., 1993).
The Personality Diagnostic Questionnaire 4+ (PDQ4+)
The PDQ4+ (Hyler, 1994a) is a 99-item self-report questionnaire, developed to assess the 10 traditional DSM-IV PDs criteria. PDQ4+ items correspond to a single DSM-IV diagnostic criterion, and are measured categorically on a True/False scale (Hyler, 1994b) indicating presence vs. absence of PD symptoms. The PDQ4+ scales have been extensively validated, including against structured interviews (e.g., Fossati et al., 1998).
Comprehensive Assessment of Traits Relevant to Personality Disorder- Static Form (CAT-PD-SF)
The CAT-PD-SF (Simms et al., 2011) is a 216-item self-report questionnaire. The items are assessed on a 5-point scale, ranging from “very untrue of me” to “very true of me”. The CAT-PD items were designed to comprehensively assess the maladaptive traits that characterize PDs. Although the trait model was developed independently, the CAT-PD facets are similar to those represented in the AMPD, although it measures 33 as opposed to 25 traits in total. Yalch and Hopwood (2016) observed generally strong convergent and discriminant validity for the CAT-PD with the Personality Inventory for DSM-5 (PID-5; Krueger et al., 2012), the formal measure of the AMPD trait model, except for CAT-PD trait scales that are not represented in the DSM-5 AMPD trait model. However, the additional CAT-PD traits were found to augment the AMPD traits in predicting important criterion variables.
The Levels of Personality Functioning Scale- Self Report (LPFS-SR)
The Levels of Personality Functioning Scale- Self Report (LPFS-SR; Morey, 2017) is an 80-item self-report questionnaire, developed to measure the Levels of Personality Functioning Scale (LPFS-SR; Morey, 2017) of the DSM-5 AMPD: the formal impairment criterion. Each item is responded to on a four-point scale ranging from “totally false” to “very true”, which correspond to levels of “little or no impairment”, to “extreme impairment”. The items of the LPFS-SR are aggregated onto four scales: Identity, Self-Direction, Empathy and Intimacy, and the four scales can be summed for a total impairment score. Morey (2017) presented promising reliability and validity data against other established personality impairment measures.
Procedures
This research was approved by the University of Otago Human Ethics Committee (Health). All participants provided informed consent prior to starting the study. Participants were administered the measures in groups of up to 12 under supervision by a trained research assistant. All participants received course credit through the University of Otago undergraduate psychology participation program for completing the study.
Data Analyses
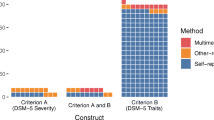
Due to their similarities and very large inter-correlations, the PDQ4+ and ADP-IV scale scores for each PD were combined to form overall aggregate PD scores.Footnote 1 First, correlation analyses were used to examine the associations between the MMPI-2-RF PD Spectra scales and aggregate PD scale scores, to examine criterion-related validity. Due to shared method variance artificially inflating correlations to an unknown degree, correlations were only interpreted as meaningful if they reached a medium or larger effect size magnitude (i.e., r > .30).
Second, hierarchical linear regression analyses were conducted to examine the incremental validity of each PD Spectra scale over the five MMPI-2-RF PSY-5 scales in predicting aggregate PD scale scores. To account for the non-normal distributions of the aggregate PD scores, bootstrapping with 10,000 replications was used to estimate standard errors associated individual coefficients. Third, zero-order correlation analyses were conducted to examine the association between the MMPI-2-RF PD Spectra scales and the CAT-PD trait scales, and the LPFS-SR scales to evaluate associations with dimensional personality traits and impairment criteria relevant to the AMPD. Again, only medium effect size magnitudes and larger were interpreted as meaningful. Finally, hierarchical linear regression analyses were conducted to examine the unique variance accounted for by each hypothesized CAT-PD scale in their corresponding PD Spectra scale, and whether the four LPFS-SR impairment scales augmented such predictions. This latter analysis would provide for a clearer indication of the nature of each PD Spectra scale from the perspective of the AMPD. Again, to account for the non-normal distributions of the aggregate PD scores, bootstrapping with 10,000 replications was used to estimate standard errors associated individual coefficients.
Results
Associations with Traditional PD Model
Correlation analyses were conducted to examine the associations between the PD Spectra scales, and aggregate PD scores, which are reported in Table 1. We also calculated Steiger’s t-tests for dependent correlations to determine if there was a significant difference in magnitude between the MMPI-2-RF PD Spectra scale’s correlation with the target aggregate PD score relative to the largest non-target PD score (see Table 1). The pattern of correlations was generally consistent with hypotheses, in that the PD Spectra scales showed the highest correlations with their corresponding aggregate PD scores. The sole exception was Histrionic PD, which was most highly (negatively) correlated with Avoidant PD and Schizoid PD aggregate scores. MMPI-2-RF Obsessive-Compulsive PD scores were equally correlated with Obsessive-Compulsive PD and Avoidant PD scale scores (t = 0.00, p = 1.00). The Dependent PD Spectra scale was most also highly correlated with the Dependent PD aggregate score, however this correlation was not significantly larger than that with Avoidant PD (t = 0.37, p > .05). Low levels of discriminant validity are common for PD measures in general, owing to the excess overlap of symptoms across PD diagnoses (Grant, et al., 2005; Zimmerman & Rothschild, 2005), but the overall criterion-related validity observed here was promising.
Next, the aggregate PD scores were regressed onto the MMPI-2-RF PSY-5 and the PD Spectra scales, which were entered in separate steps of a hierarchical model, to examine the incremental validity of the PD Spectra scales in predicting their corresponding aggregate PD scores (e.g., Paranoid PD Spectra scale predicting Paranoid PD aggregate scores; see Table 2). All PD Spectra scales evinced statistically significant (p < .001) incremental validity over the PSY-5 scales in predicting scores on their corresponding aggregate PD scores, with effect sizes mostly in the moderate range (ΔR2 = .020–.149; median = .067).
Associations with AMPD Traits and Impairment
Next, we calculated correlations between the MMPI-2-RF PD Spectra scales and the CAT-PD trait scales (see Table 3). Support was generally provided for the hypothesized CAT-PD and PD Spectra scale correlations (using the r ≥ .30 threshold). For example, the BPD Spectra scale was strongly correlated with hypothesized CAT-PD scales such as Affective Lability, Anhedonia, and Relationship Insecurity, whereas the Avoidant PD Spectra scale exhibited medium to strong correlations with CAT-PD Anhedonia, Anxiousness, Depressiveness, Relationship Insecurity, Social Withdrawal and Submissiveness. The following exceptions were observed: Paranoid PD and Unusual Beliefs, Schizotypal PD and Emotional Detachment, Antisocial PD and Anger, Emotional Detachment and Irresponsibility, Borderline PD and Irresponsibility, Non-Planfulness and Risk-Taking, Narcissistic PD and Fantasy Proneness, and Obsessive-Compulsive PD with Perfectionism and Workaholism. Additionally, the Histrionic PD Spectra scale was not meaningfully correlated with Domineering and was also negatively correlated with Anhedonia. A substantial number of correlations were observed between the non-hypothesized CAT-PD traits and the PD Spectra scales, however many of the correlations were not meaningful (i.e., rs < .30). Unexpectedly, large correlations were also observed between the following PD Spectra scale and CAT-PD traits: Schizotypal PD, Borderline PD and Cognitive problems, Dependent PD and Affective Liability and Social Withdrawal, and Obsessive-Compulsive PD and Relationship Insecurity.
Median convergent and divergent correlations were calculated to allow for an examination of the differences in the overall hypothesized versus non-hypothesized sets of CAT-PD correlations for each PD Spectra scale (see Table 3). A one-tailed Fisher’s z-test was then calculated to determine if these magnitude differences were statistically significant. All PD Spectra scales showed statistically significant differences in median convergent and divergent correlations (ZDIFF = 2.574–7.583), with the exception of the Antisocial PD Spectra scale (ZDIFF = 0.545).
Furthermore, the majority of the MMPI-2-RF PD Spectra scales exhibited significant positive correlations with the LPFS-SR scales (see Table 3), although the following correlations were not meaningful: Schizoid PD with Identity and Self-Direction, and Antisocial PD with Intimacy. In addition, the Narcissistic PD Spectra scale showed no significant correlations with any LPFS-SR scales, and the Histrionic PD Spectra scale showed significant negative correlations with all LPFS-SR scales except for Empathy, although none were meaningful.
Contributions of Traits and Impairment to MMPI-2-RF PD Spectra Scales
Finally, regression analyses (full table can be located in the online supplemental materials; Table S2) examined the extent to which the a priori hypothesized CAT-PD scales contributed uniquely in predicting their respective MMPI-2-RF PD Spectra scales, as well as whether the four LPFS-SR impairment scales augmented such predictions. These analyses were conducted to further our understanding of the nature of what these PD Spectra scales are actually measuring from the AMPD perspective. Table 4 summarizes the supported and non-supported findings for each PD Spectra scale. The majority of hypothesized sets of CAT-PD traits contributed uniquely to the prediction (p < .01) of the respective PD Spectra scales, although there were notable exceptions. For example, CAT-PD Anxiousness, Rigidity and Social Withdrawal were all found to uniquely predict scores on the Obsessive-Compulsive PD Spectra scale, whereas CAT-PD Perfectionism and Workaholism did not.
The LPFS-SR scales evidenced incremental predictive utility for eight of 10 MMPI-2-RF PD Spectra scales (Δ R2 = .043–.101; ps < .001). More specifically, Identity augmented the prediction of Paranoid (β = .301; p < .001), Schizoid (β = −.181; p < .001), Schizotypal (β = .169; p = .001), Antisocial (β = .146; p = .008) Borderline (β = .271; p < .001), Narcissistic (β = −.057; p < .001) and Obsessive-Compulsive (β = .212; p = .001) PDs; Self-Direction augmented the prediction of Dependent (β = .256; p < .001) and Obsessive-Compulsive (β = .167; p = .002) PDs, and Empathy augmented the prediction of Paranoid (β = .187; p < .001) and Schizotypal PD (β = .152; p = .001). Intimacy did not contribute uniquely to any predictions above and beyond traits and other impairment criteria (all ps > .01).
Discussion
The current study aimed to replicate and extend the validity evidence for the Sellbom et al. (2018) MMPI-2-RF PD Spectra scales by examining associations between the scales and measures of both the traditional and AMPD PD diagnostic criteria. Overall, the results indicated that these scales have promising criterion, construct, and incremental validity with respect to in assessing both the traditional and AMPD models for PD assessment. As such, these scales are likely to be useful in assessing core PD-related psychopathology in both research and clinical settings.
General Findings
The majority of the PD Spectra scales exhibited meaningful correlations with their corresponding aggregate PD scales, with the sole exception being the Histrionic PD Spectra scale; this finding was inconsistent with Sellbom et al. (2018). Moreover, in terms of discriminant validity, a large number of correlations were observed between the MMPI-2-RF Spectra scales and nearly all aggregate PD scores. However, with the exception of the Obsessive-Compulsive PD Spectra scale the correlations between the PD Spectra scales and their respective aggregate PD scores tended to be much larger than all other correlations. The overlap was not unexpected, however, due to the extensive literature illustrating the high co-morbidity rates and significant overlap of symptoms within PDs in general (e.g., Grant, et al., 2005; Morey et al. 2015; Zimmerman & Rothschild, 2005). Similar levels of discriminant validity were also observed in Sellbom et al. (2018).
In terms of incremental validity, all PD Spectra scales showed significant incremental utility over the MMPI-2-RF PSY-5 scales in predicting aggregate PD scores. Sellbom et al. (2018) observed similar findings, with nine of ten PD Spectra scales incrementing the PSY-5 scales in such predictions (with the exception of predicting Schizoid PD). The PSY-5 scales represent well-validated measures of dimensional personality psychopathology (Harkness et al. 2012); however, the unique variances accounted for by the PD Spectra scales in these predictions indicate they are assessing something pertaining to PDs above and beyond the PSY-5 scales. Thus, the PD Spectra scales would potentially provide additional benefit within the overall MMPI-2-RF scoring, particularly as the MMPI-2-RF is frequently administered within mental health settings, where PDs are prevalent. Although the PSY-5 scales provide a broad and well-validated operationalization of dimensional personality domains, the PD Spectra scales provide unique information in characterizing the traditional syndromal constructs that clinicians continue to use albeit in a more dimensional manner.
With respect to broader construct validity, most of the hypotheses were supported (see bolded correlations of Table 3), and the Schizoid, Avoidant and Dependent PDs Spectra scales exhibited significant moderate to large correlations with all hypothesized traits. Some of the hypothesized traits which failed to reach meaningful correlations can be argued to be the least conceptually relevant traits within the AMPD criteria (e.g., Emotional Detachment with Schizoid PD and Unusual Beliefs with Paranoid PD). Overall, the PD Spectra scales appear to be providing satisfactory assessment of the trait variance of PDs as described in the AMPD (Watters et al., 2019). It is important that the PD Spectra scales are assessing conceptually relevant traits to their respective diagnoses under the AMPD if they are to be used to assist dimensional PD diagnosis.
In terms of personality impairment, the PD Spectra scales showed meaningful correlations with nearly all the LPFS-SR scales. The exceptions were the Histrionic PD Spectra scale, which showed significant negative correlations with all scales except Empathy, and the Narcissistic PD Spectra scale, which showed no significant correlations with any of the LPFS-SR scales. It is likely that individuals with these disorders would indicate experiencing little or no functional impairment in self-report measures due to their symptomatology of unrealistic avowals of levels of functioning. Overall, the mostly meaningful correlations between the MMPI-2-RF PD Spectra scales and the LPFS-SR grant some confidence in their capacity to capture impairment, which is a diagnostic criterion of the AMPD.
Furthermore, the LPFS-SR scales did account for unique variance over the AMPD traits in predictions of all MMPI-2-RF PD Spectra scales, except for the Histrionic or Avoidant PD Spectra scales. Of particular interest is the LPFS Identity scale, which accounted for unique variance in seven of the PD Spectra scale scores, including the three PDs which can be considered part of the “psychotic spectrum”. Psychotic spectrum disorders have been shown throughout the literature to be associated with identity disturbances or anomalous self-experience (e.g., Parnas & Handest, 2003), so it is interesting to see that Paranoid, Schizoid and Schizotypal PD Spectra scales appear to be capturing some of this personality dysfunction. Further, it would appear that Identity impairments may be the most significant predictor of general functional impairment in the AMPD, at least as assess through the MMPI-2-RF Spectra scales, followed by Empathy and Self-Direction, which each predicted unique variance on three of the PD Spectra scales. These results indicate that the MMPI-2-RF PD Spectra scales may have utility for assessment of not only maladaptive personality traits, but also for general functional impairment that should come with such traits. Assessing functional impairment is likely to be critical for researchers and clinicians who are attempting to characterize the self and interpersonal dysfunction associated with PDs.
Specific PD Spectra Scale Considerations
Some PD Spectra scales displayed more conflicting evidence with regard to their ability to assess both traditional and AMPD constructs. First, the Narcissistic PD Spectra scale exhibited good convergent and discriminant validity with the CAT-PD traits, but only moderate levels of criterion-related validity with the aggregate PD scales. Sellbom et al. (2018) observed relatively similar results for the Narcissistic PD Spectra scale, finding more modest criterion-related validity, but good convergent and discriminant validity with respect to AMPD traits. The Narcissistic PD Spectra scale may, therefore, map better onto the AMPD criteria rather than the traditional model criteria.
Second, the Antisocial PD Spectra scale exhibited questionable construct validity in relation to AMPD traits. Correlations with the hypothesized CAT-PD traits and LPFS-SR scales were moderate at best. On the whole, it appears that the Antisocial PD Spectra scale is assessing traits emphasized in the traditional model’s diagnostic criteria more so than those emphasized by the AMPD. A possible explanation for these results is that the Antisocial PD operationalization in the AMPD appears to more broadly assess psychopathic personality traits than the traditional model criteria (Wygant et al., 2016). However, the results of the current results vastly contrasted those of Sellbom et al. (2018), who found the Antisocial PD Spectra scale to have good convergent and discriminant validity in relation to AMPD traits as assessed via the Personality Inventory for DSM-5 (Krueger et al., 2012). More research in other samples (e.g., forensic, correctional) will be necessary to further elucidate the construct validity associated with the Antisocial PD Spectra scale scores.
Furthermore, good criterion-related validity of the Antisocial PD Spectra scale was observed in the current study, whereas Sellbom et al. (2018) found relatively weak criterion-related validity for this scale. The discrepancies in the criterion-related validity results between these two studies may be the result of the different criterion measures used. The current study used the ADP-IV and the PDQ4+ which place more emphasis on the adult symptoms of Antisocial PD, whereas Sellbom et al. (2018) used the SCID-II-PQ, which is technically a screening measure that places more emphasis on the early Conduct Disorder symptoms. Thus, the MMPI-2-RF Antisocial PD Spectra scale is appropriately better aligned with adult than juvenile symptoms reflective of this disorder, which should be informative to clinicians seeking to use this scale in practice.
Third, the Obsessive-Compulsive PD Spectra scale exhibited poor discriminant validity, and was highly correlated with many non-hypothesized traits (e.g., Affective Lability, Anhedonia, Depressiveness and Mistrust). It appears the scale may be assessing negative emotionality more broadly, rather than core traits of Obsessive-Compulsive PD (such as Rigid Perfectionism and Workaholism), which may provide an explanation for the high rates of inter-correlations exhibited with the other MMPI-2-RF PD Spectra scales. However, the Obsessive-Compulsive PD Spectra scale did show incremental utility of the PSY-5 scale, and exhibited significant moderate to large correlations with all LPFS-SR scales. These findings were very similar to those of Sellbom et al. (2018), who found the Obsessive-Compulsive PD Spectra scale had questionable discriminate validity, and was also highly correlated to traits of negative affectivity. As such, it is unlikely that this scale will be of critical utility in the assessment of core Obsessive-Compulsive PD characteristics, and clinicians and researchers alike should be aware of its limited convergent and discriminant validity, but further research in clinical samples is needed prior to an ultimate conclusion in this regard.
Finally, the Histrionic PD Spectra scale was not meaningfully correlated with the Histrionic PD aggregate score, failed to show hypothesized correlations with two of the five CAT-PD scales, and exhibited negative correlations with the LPFS-SR scales. Although the overall findings for the Histrionic PD Spectra scale were suboptimal, the implications of these findings might be minor for actual assessment, as there has been much debate throughout the literature about the existence of Histrionic PD as it is currently conceptualized (e.g., Blashfield et al. 2014). Therefore, the poor performance of the Histrionic PD Spectra scale is perhaps less reflective of the scale itself, but more a reflection of the poor conceptualization of Histrionic PD. However, it is noteworthy that the current findings were quite inconsistent with those of Sellbom et al. (2018) who observed good criterion-related, convergent and discriminant validity for this scale. A potential explanation for the discrepancy may be cultural differences. New Zealanders have been found to exhibit a culture of ‘tall poppy syndrome’ where individuals who think to highly of themselves and their achievements are ‘cut down’ (Kennedy, 2007), meaning exhibitionistic and attention seeking traits are often seen as undesirable in New Zealand culture. Therefore, it may be that New Zealand participants are unlikely to endorse the types of items contained within the Histrionic PD Spectra scale in the same manner that U.S. individuals would. This hypothesis would of course require empirical testing in a measurement invariance framework.
General Implications
The MMPI-2-RF PD Spectra scales can, once implemented, provide clinicians some continuity between the traditional method of PD diagnosis and dimensional trait perspectives, while bringing the diagnostic process more in line with the current state of the literature (e.g., Hopwood et al., 2018). As the field moves towards conceptualizing PDs through a dimensional scope (as seen through the ICD-11’s adoption of a purely dimensional PD diagnostic approach) it is important to consider ease of transition for the clinicians who are likely to use such measures. Providing scales which align the traditional and dimensional approaches to PD diagnoses, and, additionally, through a commonly used measure such as the MMPI-2-RF is likely to aid clinicians in their uptake of a dimensional approach to diagnosis. The MMPI-2-RF PD Spectra scales will also allow for an even broader scope for the assessment of psychopathology within the MMPI-2-RF. Therefore, it appears the MMPI-2-RF PD Spectra scales are well positioned to provide clinicians with an assessment tool of both traditional and AMPD PD diagnostic criteria. The results of this study were also largely similar to the North American study conducted by Sellbom et al. (2018), providing confidence in the generalizability of the previous research to a New Zealand population, which is important for their clinical use in New Zealand. However, as only one previous study has been conducted to validate the MMPI-2-RF PD Spectra scales (Sellbom et al. 2018) further validation needs to be undertaken, especially in clinical samples, before the scales can be considered for applied use.
Finally, although we believe scores on the MMPI-2-RF PD Spectra scales can assist clinical interpretation with respect to formulating about personality psychopathology, significant caution should also be undertaken with the interpretation of these scales, as they are not diagnostic in nature. The MMPI-2-RF is not a diagnostic tool per se, rather it is a psychological test that can facilitate the clinical diagnostic and formulation process in the context of other sources of information.
Limitations and Future Directions
The current study is not without limitations upon which future work in this area can build. First, the use of a student population limits the generalizability of the results. The student population was largely NZ European/ Pākehā, middle class and between the ages of 18–24, providing a constrained demographic and age-range. Māori represented less than 10% of the population in the current study, and Pacifica were even less represented, and while consistent with the demographics of both the University of Otago student population and with those of New Zealand’s South Island more broadly, it limits the current study’s generalizability to New Zealand’s wider cultural makeup. Moreover, it is also unlikely there is a high prevalence of PDs within the student population. Furthermore, the use of a university student population resulted in a high proportion of women within the sample and the generalizability of the results is limited by this gender disparity. Further research should therefore aim to examine both clinical populations and the broader community population. Such research should also directly consider potential cultural differences within New Zealand with a direct comparison between NZ European/ Pākehā and Māori/Pacifica individuals, particularly as the latter have not been well-represented in MMPI-2-RF research more generally.
Second, the measures used for assessment of the traditional model and AMPD PDs are all self-report measures. The correlations between scale scores will therefore have been influenced by artificial inflation due to shared method variance. Such inflations were partially accounted for throughout the study by only interpreting correlations above a medium effect size threshold (r > .30) as meaningful. Further research should extend the validity research on the MMPI-2-RF PD Spectra scales by using structured clinical interviews and other hetero-method criterion measures.
Finally, although used as a proxy for AMPD trait measurement, the CAT-PD trait scales do not map perfectly onto the AMPD traits. If strictly adhering to the 25 traits in the DSM-5 AMPD model, the incongruence with of the CAT-PD scales the AMPD traits may restrict our confidence in the ability of the MMPI-2-RF PD Spectra Scales to assess AMPD-operationalized pathology. However, the literature has not suggested the specific AMPD trait model is set in stone in optimally capturing PDs from a dimensional perspective. The CAT-PD was developed concurrently to the AMPD, and includes a further eight traits to the AMPD. The seven additional trait scales may provide usual information about the nature of PDs not encapsulated by the AMPD. Further research would be required to assess whether the CAT-PD trait model provides better conceptualization for a dimensional model of PDs.
More generally, it will be important for future research to examine the MMPI-2-RF PD Spectra scales in ways that have clinical import. For instance, PDs affect therapeutic alliance, course, and treatment response (Tyrer et al., 2015), and it will be important to the determine the degree to which these scales moderate treatment outcomes. PDs are also important in forensic psychological practice, an area in which the MMPI instruments are frequently used (Neal & Grisso, 2014), and these scales’ role in risk assessment paradigms and risk formulation will also be important. The predictive validity of these scales for important outcomes, such as hospitalizations, suicide attempts, healthcare utilization, criminal justice involvement, will also be critical target areas for future research.
Notes
The pattern of correlations for the individual PDQ4+ and ADP-IV PD scales with MMPI-2-RF PD scales were highly similar. Indeed, intra-class correlations (two-way random, absolute agreement) for each measure’s set of correlations with MMPI-2-RF PD Spectra scales ranged from .93–.99 with the exception of the Histrionic PD scales, which was .61.
References
American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders, (3rd ed., rev.). Washington, DC: Author.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC. American Psychiatric Publishing.
Ben-Porath, Y. (2012). Interpreting the MMPI-2-RF. Minneapolis: University of Minnesota Press.
Ben-Porath, Y., & Tellegen, A. (2008/2011a). MMPI-2-RF, Minnesota multiphasic personality Inventory-2 restructured form. Minneapolis: University of Minnesota Press.
Ben-Porath, Y. S., & Tellegen, A. (2008/2011b). MMPI-2-RF (Minnesota multiphasic personality Inventory-2 restructured form): Manual for administration, scoring, and interpretation. Minneapolis: University of Minnesota Press.
Blashfield, R. K., Reynolds, S. M., & Stennett, B. (2014). The death of histrionic personality disorder. In T. A. Widiger (Ed.), The Oxford Handbook of Personality Disorder (pp. 603–627). New York: Oxford University Press.
Fossati, A., Maffei, C., Bagnato, M., Donati, D., Donati, M., Fiorilli, M., et al. (1998). Brief communication: Criterion validity of the personality diagnostic questionnaire-4+ (PDQ-4+) in a mixed psychiatric sample. Journal of Personality Disorders, 12, 172–178. https://doi.org/10.1521/pedi.1998.12.2.172.
Fridell, M., Hesse, M., & Johnson, E. (2006). High prognostic specificity of antisocial personality disorder in patients with drug dependence: Results from a five-year follow-up. American Journal on Addictions, 15, 227–232. https://doi.org/10.1080/10550490600626440.
Grant, B. F., Hasin, D. S., Stinson, F. S., Dawson, D. A., Chou, S. P., Ruan, W., & Pickering, R. P. (2004). Prevalence, correlates, and disability of personality disorders in the United States: Results from the National Epidemiologic Survey on alcohol and related conditions. The Journal of Clinical Psychiatry, 65, 948–958. https://doi.org/10.4088/JCP.v65n0711.
Grant, B. F., Stinson, F. S., Dawson, D. A., Chou, S. P., & Ruan, W. J. (2005). Co-occurrence of DSM-IV personality disorders in the United States: Results from the national epidemiological survey on alcohol and related conditions. Comprehensive Psychiatry, 46, 1–5. https://doi.org/10.1016/j.comppsych.2004.07.019.
Harkness, A. R., Finn, J. A., McNulty, J. L., & Shields, S. M. (2012). The Personality Psychopathology—Five (PSY–5): Recent constructive replication and assessment literature review. Psychological Assessment, 24(2), 432–443.
Hooley, J. M., Cole, S. H., & Gironde, S. (2012). Borderline personality disorder. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders. New York: Oxford University Press.
Hopwood, C. J., Kotov, R., Krueger, R. F., Watson, D., Widiger, T. A., Althoff, R. R., Ansell, E. B., Bach, B., Michael Bagby, R., Blais, M. A., Bornovalova, M. A., Chmielewski, M., Cicero, D. C., Conway, C., de Clercq, B., de Fruyt, F., Docherty, A. R., Eaton, N. R., Edens, J. F., Forbes, M. K., Forbush, K. T., Hengartner, M. P., Ivanova, M. Y., Leising, D., John Livesley, W., Lukowitsky, M. R., Lynam, D. R., Markon, K. E., Miller, J. D., Morey, L. C., Mullins-Sweatt, S. N., Hans Ormel, J., Patrick, C. J., Pincus, A. L., Ruggero, C., Samuel, D. B., Sellbom, M., Slade, T., Tackett, J. L., Thomas, K. M., Trull, T. J., Vachon, D. D., Waldman, I. D., Waszczuk, M. A., Waugh, M. H., Wright, A. G. C., Yalch, M. M., Zald, D. H., & Zimmermann, J. (2018). The time has come for dimensional personality disorder diagnosis. Personality and Mental Health, 12, 82–86. https://doi.org/10.1002/pmh.1408.
Hopwood, C. J., Thomas, K. M., Markon, K. E., Wright, A. J., & Krueger, R. F. (2012). DSM-5 personality traits and DSM-IV personality disorders. Journal of Abnormal Psychology, 121(2), 424–432. https://doi.org/10.1037/a0026656.
Hyler, S. E. (1994a). The personality diagnostic questionnaire 4+. New York: New York State Psychiatric Institute.
Hyler, S. E. (1994b). PDQ-4 and PDQ-4+ instructions for use. New York: New York State Psychiatric Institute.
Kennedy, J. C. (2007). Leadership and culture in New Zealand. Culture and Leadership Across the World: The GLOBE Book of In-Depth Studies of 25 Societies, 397-432.
Klein, M. H., Benjamin, L. S., Rosenfeld, R., Treece, C., Husted, J., & Greist, J. H. (1993). The Wisconsin personality disorders inventory: Development, reliability and validity. Journal of Personality Disorders, 7, 285–303.
Krueger, R. F., Derringer, J., Markon, K. E., Watson, D., & Skodol, A. E. (2012). Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological Medicine, 42, 1879–1890. https://doi.org/10.1017/s0033291711002674.
Krueger, R. F., & Markon, K. E. (2014). The role of the DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. Annual Review of Clinical Psychology, 10, 477–501. https://doi.org/10.1146/annurev-clinpsy-032813-153732.
Levitt, E. E., & Gotts, E. E. (1995). The clinical application of MMPI special scales. London: Psychology Press.
Millon, T., & Strack, S. (2015). An integrating and comprehensive model of personality pathology based on evolutionary theory. In S. K. Huprich (Ed.), Personality disorders: Toward theoretical and empirical integration in diagnosis and assessment (pp. 367–393). Washington, DC: American Psychological Association.
Morey, L. C. (2017). Development and initial evaluation of a self-report form of the DSM-5 level of personality functioning scale. Psychological Assessment, 29, 1302–1308. https://doi.org/10.1037/pas0000450.
Morey, L. C., Benson, K. T., Busch, A. J., & Skodol, A. E. (2015). Personality disorders in DSM-5: Emerging research on the alternative model. Current Psychiatry Reports, 17, 1–9. https://doi.org/10.1007/s11920-015-0558-0.
Morey, L. C., Waugh, M. H., & Blashfield, R. K. (1985). MMPI scales for DSM-III personality disorders: Their derivation and correlates. Journal of Personality Assessment, 49, 245–251. https://doi.org/10.1207/s15327752jpa4903_5.
Neal, T. M. S., & Grisso, T. (2014). Assessment practices and expert judgment methods in forensic psychology and psychiatry: An international snapshot. Criminal Justice and Behaviour, 41(12), 1406–1421. https://doi.org/10.1177/0093854814548449.
Parnas, J., & Handest, P. (2003). Phenomenology of anomalous self-experience in early schizophrenia. Comprehensive Psychiatry, 44(2), 121–134.
Schotte, C., & De Doncker, D. (1994). ADP-IV Questionnaire. Antwerp: University Hospital Antwerp.
Schotte, C., & De Doncker, D. (1996). ADP-IV questionnaire : Manual and norms. Antwerp: University Hospital Antwerp.
Schotte, C. K. W., De Doncker, D., Vankerchkhoven, C., Vertommen, H., & Cosyns, P. (1998). Self-report assessment of the DSM-IV personality disorders. Measurement of trait and distress characteristics: The ADP-IV. Psychological Medicine, 28, 1179–1188. https://doi.org/10.1017/s0033291798007041.
Sellbom, M., Waugh, M. H., & Hopwood, C. J. (2018). Development and validation of personality disorder spectra scales for the MMPI-2-RF. Journal of Personality Assessment, 1–15. https://doi.org/10.1080/00223891.2017.1407327.
Sellbom, M. (2019). The MMPI-2-restructured-form (MMPI-2-RF): Assessment of personality and psychopathology in the twenty-first century. Annual Review of Clinical Psychology, 15, 8.1–8.29. https://doi.org/10.1146/annurev-clinpsy-050718-095701.
Simms, L. J., Goldberg, L. R., Roberts, J. E., Watson, D., Welte, J., & Rotterman, J. H. (2011). Computerized adaptive assessment of personality disorder: Introducing the CAT-PD project. Journal of Personality Assessment, 93, 380–389. https://doi.org/10.1080/00223891.2011.577475.
Skodol, A. E. (2012). Diagnosis and DSM-5: Work in Progress. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders. New York: Oxford University Press.
Skodol, A. E., Clark, L. A., Bender, D. S., Krueger, R. F., Morey, L. C., Verheul, R., et al. (2011). Proposed changes in personality and personality disorder assessment and diagnosis for DSM-5 part I: Description and rationale. Peronsality Disorders: Theory, Research and Treatment, 2, 4–22. https://doi.org/10.1037/a0021891.
Somwaru, D.P., & Ben-Porath, Y.S. (1995). Development and reliability of MMPI-2 based personality disorder scales. Paper presented at the 30th annual workshop and symposium on recent developments in use of the MMPI-2 and MMPI-A, St. Petersburg Beach, FL.
Tyrer, P., Reed, G. M., & Crawford, M. J. (2015). Classification, assessment, prevalence, and effect of personality disorder. Lancet, 385, 717–726.
Watters, C. A., Bagby, R. M., & Sellbom, M. (2019). Meta-analysis to derive an empirically-based set of personality facet criteria for the alternative DSM-5 model for personality disorders. Personality Disorders: Theory, Research, and Treatment, 10(2), 97–104. https://doi.org/10.1037/per0000307.
Wygant, D. B., Sellbom, M., Sleep, C. E., Wall, T. D., Applegate, K. C., Krueger, R. F., & Patrick, C. J. (2016). Examining the DSM-5 alternative personality disorder model operationalization of antisocial personality disorder and psychopathy in a male correctional sample. Personality Disorders: Theory, Research, and Treatment, 7, 229–239. https://doi.org/10.1037/per0000179.
Yalch, M. M., & Hopwood, C. J. (2016). Convergent, discriminant and criterion validity of DSM-5 traits. Personality Disorders: Theory, Research, and Treatment, 7, 394–404. https://doi.org/10.1037/per0000165.
Zimmerman, M., & Rothschild, L. (2005). The prevalence of DSM-IV personality disorders in psychiatric outpatients. American Journal of Psychiatry, 162, 1911–1998. https://doi.org/10.1176/appi.ajp.162.10.1911.
Funding
A grant awarded to Dr Sellbom from the University of Minnesota Press, publisher of the MMPI-2-RF, funded this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ms Brown declares that she has no conflict of interest. Dr Sellbom is a paid consultant to the University of Minnesota Press, publisher of the MMPI-2-RF. Dr Sellbom also teaches professional workshops and webinars for remuneration.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (University of Otago, Human Ethics Committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Experiment Participants
Research involved human participants.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 58 kb)
Rights and permissions
About this article
Cite this article
Brown, T.A., Sellbom, M. Further Validation of the MMPI-2-RF Personality Disorder Spectra Scales. J Psychopathol Behav Assess 42, 259–270 (2020). https://doi.org/10.1007/s10862-020-09789-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-020-09789-5