Abstract
To date, the utility of behavioral activation (BA) as a treatment for depression has been primarily demonstrated in an individual therapy format, with few empirical investigations exploring group-based delivery. In addition, little is known about the utility of such interventions within veterans, a population known to have increased rates of depression. To this end, the purpose of the proposed study was to examine the potential therapeutic benefits of BA delivered in a group-based format to an outpatient sample of veterans with a primary depressive diagnosis. The sample consisted of 32 veterans presenting for psychological services within a general mental health clinic at a large, Southeastern Veterans Affairs (VA) hospital. Depression and quality of life symptoms were measured pre- and post- delivery of the Brief Behavioral Activation Treatment for Depression-Revised (BATD-R; Lejuez et al. Behavior Modification, 35(2), 111–161, 2011), a 10-session manualized protocol designed to address depressive symptoms by increasing patient contact with reinforcing environmental contingencies. Consistent with prediction, engagement in BATD-R led to reductions in depression symptoms and increases in overall life satisfaction from pre- to post-treatment. The present study provides preliminary support for the effectiveness of BATD-R delivered in a group-based format among an outpatient sample of veterans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Depressive disorders, characterized by the presence of sad, empty, or irritable mood, along with somatic and cognitive changes, are a prevalent yet pernicious category of mental illnesses (American Psychiatric Association 2013). With a lifetime prevalence rate of 21% (Kessler et al. 2005), depressive disorders have been identified as a leading cause of global disease burden and a significant contributor to suicide (Ferrari et al. 2013). Depressive disorders are often associated with decreased physical, social, and occupational functioning (American Psychiatric Association 2013). In addition, when direct (e.g., medical and suicide related mortality) and indirect (e.g., decreased work productivity) costs are considered, the economic burden of depression is estimated at 83 billion dollars annually (Greenberg et al. 2003). As such, the need to identify and understand risk and prognostic factors that contribute to the onset and maintenance of depressive disorders is salient.
Exposure to extremely traumatic or stressful life events is one of the most well-known and recognizable risk factors for depression (Kendler et al. 1999). Unsurprisingly, exposure to combat has been found to be a persistent and powerful predictor of depressive disorders (Grieger et al. 2006). Indeed, prevalence rates of depression among combat veterans may be comparable to, or even higher than, rates of posttraumatic stress disorder (PTSD). For example, depressive disorders (45%) were the second most common mental health diagnosis following PTSD (55%) found among newly returning veterans evaluated within the Department of Veterans Affairs (VA) from 2002 to 2015 (Epidemiology Program 2015). Moreover, in a large outpatient sample of veterans drawn from the VA (N = 2160), researchers found screening rates were 31% for depression and 20% for PTSD (Hankin, Spiro, Avron, Miller, & Kazis, 1999). Considering the risk for increased healthcare utilization and mortality among depressed patients (Trivedi et al. 2015), the treatment of such disorders has become a top priority within the VA.
Fortunately, there are a number of effective treatments for depressive disorders including biological (e.g., selective serotonin reuptake inhibitors) and psychological (e.g., interpersonal psychotherapy) interventions (Gelenberg 2010). One psychological intervention that has received increasing empirical support is Behavioral Activation (BA). BA is defined as a therapeutic process in which patients engage in personally meaningful activities that are congruent with their values and goals to increase contact with reinforcing elements of their environment (Lejuez et al. 2011). BA treatments evolved from both behavioral theories of depression and research demonstrating that depressed individuals engage in few pleasurable activities, leading to a decrease in positive reinforcement and subsequent depressive affect (Lewinsohn 1974). Jacobson et al. (1996) were the first to find evidence for the efficacy of a BA intervention in the acute treatment of depression. Since that time, support for BA has been found across a wide range of populations relative to wait-list and active control conditions (for review and meta-analysis see, Mazzucchelli et al. 2009). For example, using 26 randomized controlled trials (N = 1524), Ekers et al. (2014) conducted a meta-analysis of BA for depression. The authors found BA to be superior to various control conditions (including waitlist, placebos, and usual care) and antidepressant medications with between group effect sizes in the large (Hedges g = −0.74) to moderate (Hedges g = −0.42) range, respectively. Notably, despite variability in delivery mode across studies (i.e., individual, group, and self-help formats), there was no evidence that the number of sessions was associated with effect size.
Recently, researchers also have found evidence for the utility of BA among veterans (Gros and Haren 2011; Luxton et al. 2016). For example, Mulick and Naugle (2004) investigated the utility of BA to treat a 37-year-old military veteran presenting with comorbid PTSD and depression. Using both self-report and observer-rated data, the authors found that the client no longer met diagnostic criteria for either disorder at post-treatment. Notably, these gains were maintained throughout a brief one-month follow-up period. Extending upon this research, Jakupcak et al. (2010) examined treatment satisfaction and potential therapeutic benefits of BA in a primary care-based setting using a small sample of Iraq and Afghanistan war veterans. Despite the diagnostic complexity of patients (i.e., comorbid PTSD and depression), BA was associated with high patient satisfaction and meaningful decreases in depression that were maintained throughout a three-month follow-up period. More recently, Egede et al. (2015) examined the effectiveness of BA delivered either in-person or via telemental health into the home using a large sample of older veterans. Treatment response did not differ significantly between groups with both tolerating and clinically benefiting from the treatment.
Although there is strong evidence for the use of BA, many veterans receive treatment after years of impairment or no treatment at all (Hoge et al. 2004; Wang et al. 2005). According to a VA audit, the largest barrier to care is an acute shortage of mental health care providers (US Department of Veterans Affairs 2014). One practical and cost-effective solution to solving this access issue is to increase use of group-based empirically supported treatments. However, there is limited research on group-based BA treatments for depression and even less within veteran samples. For example, Kellett et al. (2017) recently conducted an implementation pilot study of group-based BA within community clients receiving care at family practice (n = 25) and students presenting to a university counseling center (n = 46). The authors found BA was acceptable and effective (d’s = .73 to .74) with 20% of patients meeting criteria for reliable recovery. To our knowledge, only one study to date has examined the effectiveness of such an intervention among veterans. Hershenberg et al. (2017) examined the acceptability, feasibility, and utility of a 12-week group-based BA protocol among veterans presenting to a specialty PTSD clinic at a large VA medical facility. Among the 64 veterans who attended Session 1, 54 (84%) completed treatment, attending an average of 10 sessions (SD = 1.66). In terms of clinical outcomes, the authors found statistically significant improvements in depression (d = 1.19) and PTSD (d = .69) from pre- to post-treatment. Though promising, further studies are needed to test the utility of this potentially cost-effective intervention in veteran samples, particularly among those with primary depressive disorders.
To this end, the primary purpose of the current investigation was to assess the potential therapeutic benefits of the Brief Behavioral Activation Treatment for Depression- Revised (BATD-R; Lejuez et al. 2011) delivered in a group-based format to an outpatient sample of veterans with a primary depressive diagnosis. Consistent with previous research, it was hypothesized that engagement in the BATD-R would lead to reductions in depression symptoms. Further, in line with previous investigations, it was hypothesized that BATD-R would lead to increases in overall life satisfaction from pre- to post-treatment. To our knowledge, this is only the second study to date to examine a group-based BA protocol among veterans, despite increased rates of depression in such samples (Epidemiology Program 2015).
Method
Participants
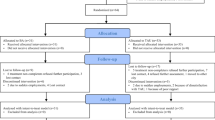
All data was collected as part of routine clinical care among 32 veterans presenting for psychological services within a general mental health clinic at a large VA facility in the Southeastern United States. Veterans were primarily male (87.5%) with a mean age of 56.97 years (SD = 14.79). The racial/ethnic breakdown was as follows: 68.8% African-American; 28.1% Caucasian; and 3.1% Asian/Pacific Islander. Regarding marital status, 43.8% of the sample was divorced, 28.1% married, 21.9% never married, 3.1% separated, and 3.1% widowed. In terms of military characteristics, most of the sample served in the Army (37.5%), followed by Marine Corps (18.8%), Navy (15.6%), and Air Force (15.6%), with 12.5% serving in some other capacity (i.e., Coast Guard or National Guard). Further, the majority of individuals served in combat operations in Vietnam (37.5%), followed by Desert Storm (12.5%), Iraq and Afghanistan (9.4%), Korea (3.1%), and other (3.1%; e.g., peace keeping missions), with 3.1% serving in multiple war zones, 25.0% never having served in a war zone, and 6.3% failing to respond.
Procedure
Veterans were referred to the BA group after completing an initial intake evaluation with a provider (i.e., psychiatrists, psychologists, and social workers) in the general mental health clinic. To be referred, veterans had to meet diagnostic criteria for a primary depressive disorder (i.e., Persistent Depressive Disorder, Major Depressive Disorder). All diagnoses were made using unstructured or semi-structured interviews depending on provider preference. While formal inclusion or exclusion criteria were not used, veterans are generally not referred for group psychotherapy in this outpatient clinic if they are actively psychotic, suffer from uncontrolled bipolar disorder, or display evidence of serious suicidal intent that would require immediate hospitalization. Given the routine nature of data collection, no other inclusion or exclusion criteria were used; further, diagnostic status was not confirmed.
Upon receipt of a referral, veterans were contacted via telephone by the group leaders. Veterans were informed of the purpose and duration of the group as well as the start date and time. Treatment consisted of 10 group-sessions, delivered once weekly, lasting approximately one hour in duration. Veterans were treated in one of five groups from August 2016 to August 2017. The groups ranged in size from five to eight veterans, with an average group size of 6.40 (SD = 1.14). All groups were led by the first author (who at the time was a clinical psychology post-doctoral fellow) and the second author (who at the time was a clinical psychology intern) and supervised by two licensed clinical psychologists (authors four and five) as part of a general mental health rotation. The first author was trained to deliver BATD-R by one of the developers of the treatment protocol (Carl Lejuez, Ph.D.) and had previous experience delivering this treatment in an individual format. Veterans completed a brief battery of self-report questionnaires pre- and post-treatment to assess symptom change. Upon completion of the group, veterans were referred back to the referral source for further treatment planning as clinically indicated. Given that the data was collected as part of routine clinical care, informed consent was not obtained. Nevertheless, the VA Institutional Review Board approved the use of this data for research purposes.
Measures
Patient Health Questionnaire (PHQ-9)
The PHQ-9 is a nine-item self-report questionnaire designed to assess depression diagnostic criteria and other leading major depressive symptoms (Kroenke et al. 2001). Veterans were asked to rate how often they have been bothered by a list of depressive symptoms within the past two weeks using a four-point Likert-type scale ranging from zero to three. The PHQ-9 has been found to have strong psychometric properties (Kroenke et al. 2001). In the current study, the PHQ-9 demonstrated good internal consistency pre- and post-treatment (α = 0.84 and α = 0.90, respectively).
Quality of Life Inventory (QOLI)
The QOLI is a 32-item self-report questionnaire designed to assess overall life satisfaction and dissatisfaction in 16 areas of life (e.g., love, work, and health; Frisch et al. 1992). Veterans were asked to rate each area in terms of importance to their overall happiness and in terms of their satisfaction with the area. Weighted satisfaction ratings range from −6 to 6 and are the product of satisfaction ratings (scale of −3 to 3) multiplied by importance ratings (scale of 0 to 2). A raw score is then created by averaging the weighted satisfaction ratings. QOLI raw scores are then converted to T scores, which have a mean of 50 and standard deviation of 10. The QOLI has been found to have strong psychometric properties including test-retest reliability, internal consistency, convergent, and discriminant validity (Frisch 1994).
Treatment
The BATD-R is a 10-session manualized protocol designed to address depressive symptoms by increasing patient contact with reinforcing environmental contingencies. It has been noted that BA is particularly adaptable to group delivery due to its parsimonious nature (Kellett et al. 2017). In line with this notion, the protocol was not altered in any way for group-based delivery. Consistent with the individual protocol, treatment began with an overview and assessment of depressive symptoms followed by an introduction to the treatment rationale for BA. Because a primary focus of the treatment is to increase healthy behaviors, patients were taught early on to monitor already occurring daily activities. This information was then used to provide a baseline assessment of activity level and to generate ideas of behaviors to target during treatment. Following the monitoring phase, the emphasis of treatment shifted to identifying values within 10 life areas (i.e., family, social, intimate relationships, education, employment/career, hobbies/recreation, physical health, psychological health, spirituality, and daily activities) and translating these values into activities. An activity hierarchy was then created in which patients rank ordered each item from “easiest” to “most difficult” to accomplish. Using the daily monitoring forms, patients progressively moved through their hierarchy scheduling in new behavioral activation goals each week. Towards the end of treatment, patients were prepared for termination and relapse prevention was discussed. Of note, at the beginning of each session homework was examined and reviewed.
Data Analytic Plan
First, means, standard deviations, and zero-order correlations for all self-report measures were examined. Second, Chi-square test for independence and independent samples t-tests were used to compare pretreatment differences in basic demographic (i.e., age, race) and psychological variables (i.e., baseline PHQ-9 total) between those individuals who did and did not complete treatment. In the current study, treatment completion was defined as completing at least 60% of the treatment (i.e., six out of 10 ten sessions of BA). This benchmark was selected based on previous depression treatment research (Gortner et al. 1998; Jacobson et al. 1996). Third, paired-samples t-test were conducted to compare pre-post treatment effects on symptoms of depression (as measured by the PHQ-9 total score) and overall quality of life (as measured by the QOLI) for the entire intent-to-treat (ITT) sample using multiple imputation and for the treatment completers sub-sample.
Fourth and finally, to determine if reductions in depression were meaningful, reliable change index (RCI) scores and clinically significant change was calculated using the criteria set forth by Jacobson and Truax (1992). In the current study, clinically significant change was defined as a decrease of at least two standard deviations from the average pre-treatment PHQ-9 score following treatment (i.e., Jacobson and Truax 1992a criteria). Individuals were considered to be recovered if they began with a clinical level PHQ-9 score at pre-treatment and then crossed the a criteria threshold to subclinical levels at post-treatment. Additionally, the clinically significant change a criteria was supplemented by established cut scores delineating thresholds of the level of depression severity for the PHQ-9 (Kroenke et al. 2001) including: 1 to 4 (None-Minimal), 5 to 9 (Mild), 10 to 14 (Moderate), 15 to 19 (Moderately Severe), and 20 to 27 (Severe). The second approach to presenting indicators of meaningful change in depression was the RCI. The RCI is a test statistic that provides criteria for a decision to be made regarding whether the amount of change in individual symptom scores is sufficiently large to be considered a reliable change (i.e., more than would be expected by chance alone), with values larger than 1.96 indicating that a patient has improved (Evans et al. 1998; Jacobson and Truax 1992). Of note, improvement and recovery ratings were calculated only for those individuals who had pre and post-treatment data (n = 21).
Results
Preliminary Analyses
Zero-order correlations for all self-report measures can be found in Table 1. The mean pre-treatment PHQ-9 total score was in the moderately severe range (M = 17.14, SD = 5.68, Range 9–26). All constructs of interest were positively and moderately correlated at pre-treatment.
Twenty-one veterans (65.6%) met criteria as treatment completers. The mean number of sessions for treatment completers was 8.71 (SD = 1.39). Eleven individuals discontinued treatment (34%). The mean number of sessions for those who dropped was 2.64 (SD = 1.43). The mean number of sessions for the total sample was 6.63 (SD = 3.24). Results revealed that there were no significant differences in veteran age between those who did (M = 60.38, SD = 11.80) and did not complete treatment (M = 50.45, SD = 18.14), t (30), −1.87, p = .071, two-tailed. Similarly, there were no significant associations between veteran race χ2 (1, n = 32) = .11, p = .737, phi = .13, and completer status. Regarding psychological variables, there were also no significant differences in pre-treatment PHQ-9 total scores between those who did (M = 17.14, SD = 5.69) and did not (M = 15.90, SD = 7.05) complete treatment, t (29), −.53, p = .602, two-tailed.
Primary Analyses
ITT Analyses
Results revealed a statistically significant decrease in PHQ-9 scores for the ITT sample from pre- (M = 16.74, SE = 1.06) to post-treatment (M = 11.06, SE = 1.05), t (2138), 4.91, p < .001, two-tailed. The mean decrease was 5.69 with a 95% confidence interval ranging from 3.41 to 7.96. Further, there was a statistically significant increase in overall life satisfaction from pre- (M = 29.32, SE = 2.69) to post-treatment (M = 36.05, SE = 2.47), t (1191), −2.49, p = .013, two-tailed. The mean increase was 6.73 with a 95% confidence interval ranging from −12.02 to −1.43.
Treatment Completer Analyses
Consistent with findings for the ITT sample, results revealed a statistically significant decrease in PHQ-9 scores from pre- (M = 17.14, SD = 5.68) to post-treatment (M = 10.95, SD = 6.90), t (20) = 4.90, p < .001, two-tailed, among completers. The mean decrease was 6.19 with a 95% confidence interval ranging from 3.56 to 8.82. There was also a marginally significant increase in overall life satisfaction from pre- (M = 27.76, SD = 16.27) to post-treatment (M = 34.58, SD = 17.61), t (16) = −2.01, p = .062, two-tailed. The mean increase was 6.82 with a 95% confidence interval ranging from −14.02 to .37.
Reliable and Clinically Significant Change
Improvement, recovery, and reliable change ratings are summarized in Table 2. The mean PHQ-9 score decreased from pre- (M = 17.14, SD = 5.68) to post-treatment (M = 10.95, SD = 6.90) resulting in an average RCI of 2.37 (SD = 2.21) for the 21 treatment completers. A total of 12 veterans (57%) were considered reliably improved following treatment. With regard to clinically significant change, four veterans (19%) were considered recovered and eight were considered improved (38%), while nine (43%) were neither improved nor recovered. Based on PHQ-9 thresholds of depression severity, there was a downward trend in patient classification severity from pre- to post-treatment including: severe (5 to 2), moderately severe (6 to 1), moderate (4 to 5), mild (2 to 6), and none-minimal (0 to 3).
Discussion
To date, the utility of BA has been primarily demonstrated in an individual therapy format, with few empirical investigations exploring group-based delivery. As such, the primary purpose of the current investigation was to assess the potential therapeutic benefits of BATD-R delivered in a group-based format to an outpatient sample of veterans with a primary depressive diagnosis. Consistent with prediction, engagement in BATD-R led to reductions in depression symptoms and increases in overall life satisfaction from pre- to post-treatment. These findings are consistent with the larger BA literature base (Cuijpers et al. 2007; Hopko et al. 2003b) and provide support for the effectiveness of BA in a group-based format (Hershenberg et al. 2017; Kellett et al. 2017).
Although there was clear indication that veterans benefitted from the treatment, there is reason to believe that the number of individuals identified as recovered would be higher with a larger sample. Indeed, clinically significant change is based on the level of sample variation. As such, the inclusion of additional subjects would likely decrease the amount of symptom decline necessary to cross the threshold for recovery. Further, under the conditions in the current study, the a criteria would be considered a conservative estimate to indicate patient recovery, and the use of the b (two standard deviations from the normative sample mean for PHQ-9) or c (the halfway point between the clinical and normative sample means) criteria would likely yield additional recovery. To this end, one veteran had a PHQ-9 score that decreased from 21 to 9, equating to a reduction of 57%, but was not considered recovered. However, when consulting the cutoffs established by Kroenke et al. (2001), this veteran moved from the severe depression level pre-treatment to the mild depression level post-treatment. As a whole, the movement in depression level categories from pre- to post-treatment indicated a clear trend towards decreased depression symptoms across the sample.
A host of study specific factors including the type of population, measures and levels of depression at baseline, and treatment intensity make it difficult to directly compare outcomes across BA trials. All things considered, it is still useful to evaluate the efficacy of the current study in light of the trials that predate it. To facilitate comparisons between studies, d-type effect sizes (wherein the post-treatment score was subtracted from the pre-treatment score and divided by the pooled standard deviation) were calculated for the current and previous trials. Effects for depression in the current study were large with a d of 1.09. This level of change is comparable to other BA trails where large effects (d’s range from 1.17–1.56) were also observed (Gros and Haren 2011; Hopko et al. 2003a; Jakupcak et al. 2010). In addition, rates of dropout in the current study (i.e., 44%) were similar to those found in previous research (i.e., 40%; Gros and Haren 2011). Unlike the previous interventions, the current study utilized a group-based delivery format allowing for multiple patients to be seen during the same therapy hour. Given that one of the largest VA barriers to care is an acute shortage of mental health providers (US Department of Veterans Affairs 2014), group-based protocols may be a cost effective and efficient solution to solving access issues. In addition, such protocols are likely to be more attractive to clinicians than time intensive individual therapies and thus easier to implement and “roll out.” Although more research is needed, this is particularly salient as the VA has invested heavily in the dissemination of other evidence-based treatments for depression (e.g., Interpersonal Psychotherapy [IPT] and CBT-D).
It is also useful to compare findings from the current investigation to those found in the only other study to date to examine a group-based BA protocol among veterans. As previously noted, Hershenberg et al. (2017) evaluated a 12-week group BA treatment among veterans (N = 64) seeking services within a PTSD specialty clinic at a large, urban VA medical center. Consistent with findings from the current investigation, the authors found statistically significant reductions in depression and improvements in overall quality of life from pre- to post-treatment with large effect sizes (d’s = 1.19 and .95, respectively). In addition, when examining treatment response, over half of all veterans were considered recovered or improved (58%). Results in the current study were comparable with 57% of patients classified as recovered or improved. This is noteworthy given the equivalence of pre-treatment PHQ-9 means across studies (M = 17.14; SD = 5.68 compared to M = 18.70; SD = 4.30). Importantly, the treatment provided in the current study was briefer (i.e., 10 sessions vs. 12 sessions and 60 min vs. 90 min, respectively) and the sample size was considerably smaller; thus, rendering the equivalency in findings across the protocols even more notable.
Like any study, the current investigation has several limitations worth noting. First and foremost, all data were collected as part of routine clinical care. As such, the study lacked a comparison or control group. Although we observed overall reductions in depression symptoms and increases in life satisfaction, we cannot conclusively rule out that veterans merely improved due to the passage of time. Subsequent investigations should utilize wait-list and/or control groups to further investigate the effectiveness of this intervention and in particular mechanisms of change among veterans. Second, given the routine nature of data collection, the reliability of depression diagnoses is unclear as it was not validated upon receipt of referral. Similarly, information on comorbid diagnoses and/or medication at the time of referral was not recorded. Future research should seek to utilize standardized diagnostic tools to improve the validity of patient diagnoses in addition to gathering information on other variables that may influence treatment response (e.g., co-morbid diagnoses). Third, measures of treatment fidelity were not utilized. Measures of provider adherence are critical to evaluating the reliability and validity of the intervention and should be used in future investigations.
Fourth, the sample was somewhat small and comprised primarily of male veterans. Whereas men comprise 85% of our armed forces, the number of female military personnel has increased in recent years (Patten and Parker 2011). Thus, future investigations should seek to replicate these findings in larger, more diverse samples to assess generalizability. Fifth, all constructs of interest were measured using self-report. Despite use of well-validated assessment instruments, future research would benefit from multi-method approaches including gold standard diagnostic interviews to confirm symptom remission. Sixth and finally, given the naturalistic treatment setting, follow-up data was not collected. Consequently, it is unknown if gains were maintained beyond the initial treatment period. A much larger sample followed over longer intervals will be needed to examine the effects on factors like depression diagnoses.
Despite these limitations, the present study provides preliminary support for the effectiveness of BATD-R delivered in a group-based format among an outpatient sample of veterans. Consistent with prediction, results revealed significant reductions in depression and increases in overall life satisfaction from pre- to post-treatment. To our knowledge, this is only the second study to date to examine a group-based BA protocol among veterans, despite increased rates of depression in such samples. Although findings were promising, future research is needed to test the efficacy of this intervention compared to wait-list and/or control groups.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: American Psychiatric Publishing.
Cuijpers, P., van Straten, A., & Warmerdam, L. (2007). Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review, 27(3), 318–326. https://doi.org/10.1016/j.cpr.2006.11.001.
Egede, L. E., Acierno, R., Knapp, R. G., Lejuez, C., Hernandez-Tejada, M., Payne, E. H., & Frueh, B. C. (2015). Psychotherapy for depression in older veterans via telemedicine: A randomised, open-label, non-inferiority trial. The Lancet Psychiatry, 2(8), 693–701.
Ekers, D., Webster, L., Van Straten, A., Cuijpers, P., Richards, D., & Gilbody, S. (2014). Behavioural activation for depression; an update of meta-analysis of effectiveness and sub group analysis. PLoS One, 9(6), e100100.
Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration, Department of Veterans Affairs. (2015). Analysis of VA health care utilization among operation enduring freedom, operation Iraqi freedom, and operation new Dawn veterans, from 1st Qtr FY2002 through 1st Qtr FY 2015. Retrieved from Washington, DC: https://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2015-qtr1.pdf
Evans, C., Margison, F., & Barkham, M. (1998). The contribution of reliable and clinically significant change methods to evidence-based mental health. Evidence-Based Mental Health, 1(3), 70–72.
Ferrari, A. J., Charlson, F. J., Norman, R. E., Patten, S. B., Freedman, G., Murray, C. J., Vos, T., & Whiteford, H. A. (2013). Burden of depressive disorders by country, sex, age, and year: Findings from the global burden of disease study 2010. PLoS Medicine, 10(11), e1001547.
Frisch, M. B. (1994). QOLI: Quality of life inventory: Manual and treatment guide: National Computer Systems.
Frisch, M. B., Cornell, J., Villanueva, M., & Retzlaff, P. J. (1992). Clinical validation of the quality of life inventory. A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment, 4(1), 92.
Gelenberg, A. J. (2010). A review of the current guidelines for depression treatment. The Journal of Clinical Psychiatry, 71(7), e15.
Gortner, E. T., Gollan, J. K., Dobson, K. S., & Jacobson, N. S. (1998). Cognitive–behavioral treatment for depression: Relapse prevention. Journal of Consulting and Clinical Psychology, 66(2), 377–384.
Greenberg, P. E., Kessler, R. C., Birnbaum, H. G., Leong, S. A., Lowe, S. W., Berglund, P. A., & Corey-Lisle, P. K. (2003). The economic burden of depression in the United States: How did it change between 1990 and 2000? Journal of Clinical Psychiatry, 64(12), 1465–1475.
Grieger, T. A., Cozza, S. J., Ursano, R. J., Hoge, C., Martinez, P. E., Engel, C. C., & Wain, H. J. (2006). Posttraumatic stress disorder and depression in battle-injured soldiers. American Journal of Psychiatry, 163(10), 1777–1783.
Gros, D. F., & Haren, W. B. (2011). Open trial of brief behavioral activation psychotherapy for depression in an integrated veterans affairs primary care setting. The primary care companion to CNS disorders, 13(4).
Hankin, C. S., Spiro III, A., Miller, D. R., & Kazis, L. (1999). Mental disorders and mental health treatment among US Department of Veterans Affairs outpatients: the Veterans Health Study. American Journal of Psychiatry, 156(12), 1924–1930.
Hershenberg, R., Smith, R. V., Goodson, J. T., & Thase, M. E. (2017). Activating veterans toward sources of reward: A pilot report on development, feasibility, and clinical outcomes of a 12-week behavioral activation group treatment. Cognitive and Behavioral Practice, 25(1), 57–69.
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22.
Hopko, D., Lejuez, C. W., Lepage, J. P., Hopko, S., & McNeil, D. W. (2003a). A brief behavioral activation treatment for depression: A randomized pilot trial within an inpatient psychiatric hospital. Behavior Modification, 27(4), 458–469. https://doi.org/10.1177/0145445503255489.
Hopko, D., Lejuez, C., Ruggiero, K. J., & Eifert, G. H. (2003b). Contemporary behavioral activation treatments for depression: Procedures, principles, and progress. Clinical Psychology Review, 23(5), 699–717.
Jacobson, N. S., & Truax, P. (1992). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research.
Jacobson, N. S., Dobson, K. S., Truax, P. A., Addis, M. E., Koerner, K., Gollan, J. K., Gortner, E., & Prince, S. E. (1996). A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology, 64(2), 295–304.
Jakupcak, M., Wagner, A., Paulson, A., Varra, A., & McFall, M. (2010). Behavioral activation as a primary care-based treatment for PTSD and depression among returning veterans. Journal of Traumatic Stress, 23(4), 491–495.
Kellett, S., Simmonds-Buckley, M., Bliss, P., & Waller, G. (2017). Effectiveness of group behavioural activation for depression: A pilot study. Behavioural and Cognitive Psychotherapy, 45(4), 401–418.
Kendler, K. S., Karkowski, L. M., & Prescott, C. A. (1999). Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry, 156(6), 837–841.
Kessler, R., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The Phq-9. Journal of General Internal Medicine, 16(9), 606–613.
Lejuez, C. W., Hopko, D., Acierno, R., Daughters, S. B., & Pagoto, S. L. (2011). Ten year revision of the brief behavioral activation treatment for depression: Revised treatment manual. Behavior Modification, 35(2), 111–161. https://doi.org/10.1177/0145445510390929.
Lewinsohn, P. M. (1974). A behavioral approach to depression. Essential Papers on Depression, 150–172.
Luxton, D. D., Pruitt, L. D., Wagner, A., Smolenski, D. J., Jenkins-Guarnieri, M. A., & Gahm, G. (2016). Home-based telebehavioral health for US military personnel and veterans with depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 84(11), 923–934.
Mazzucchelli, T., Kane, R., & Rees, C. (2009). Behavioral activation treatments for depression in adults: A meta-analysis and review. Clinical Psychology: Science and Practice, 16(4), 383–411. https://doi.org/10.1111/j.1468-2850.2009.01178.x.
Mulick, P. S., & Naugle, A. E. (2004). Behavioral activation for comorbid PTSD and major depression: A case study. Cognitive and Behavioral Practice, 11(4), 378–387.
Patten, E., & Parker, K. (2011). Women in the US military: Growing share, distinctive profile. Washington, DC: Pew Research Center.
Trivedi, R. B., Post, E. P., Sun, H., Pomerantz, A., Saxon, A. J., Piette, J. D., et al. (2015). Prevalence, comorbidity, and prognosis of mental health among US veterans. American Journal of Public Health, 105(12), 2564–2569.
US Department of Veterans Affairs. (2014). Access audit system-wide review of access: Results of access audit conducted May 12, 2014, through June 3, 2014. Washington, DC.
Wang, P. S., Berglund, P., Olfson, M., Pincus, H. A., Wells, K. B., & Kessler, R. C. (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 603–613.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Disclosures
The contents of this article do not represent the views of the Department of Veterans Affairs (VA) or the United States Government. This material is the result of work supported with resources and the use of facilities at the Southeast Louisiana Veterans Health Care System in New Orleans, LA.
Conflict of Interest
Amanda M. Raines, Elizabeth A. Thomas, Jamie L. Tock, Thomas M. Hallinan, Shannon Hartley, Holly MacKenna, Joseph I. Constans, and C. Laurel Franklin declare that they have no conflicts of interest.
Experiment Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Given that the data was collected as part of routine clinical care, informed consent was not obtained. Nevertheless, the VA Institutional Review Board approved the use of this data for research purposes.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raines, A.M., Thomas, E.A., Tock, J.L. et al. Examining the Effectiveness of a Group-Based Behavioral Activation Treatment for Depression among Veterans. J Psychopathol Behav Assess 42, 306–313 (2020). https://doi.org/10.1007/s10862-019-09778-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-019-09778-3