Abstract
The relation of posttraumatic stress disorder (PTSD) to other forms of psychopathology is complex as diagnostic criteria include symptoms of both mood- and anxiety-related conditions. Drawing from Watson’s (2009) quadripartite model of comorbidity, the current study examined (a) the association of PTSD symptom dimensions with indices of generalized distress, (b) the specificity of PTSD symptom dimensions for core aspects of anxiety and depression, and (c) the unique associations of symptom dimensions with markers of positive emotionality, somatic arousal, generalized distress, and cumulative trauma history. Confirmatory analyses were used to model symptom dimensions in help-seeking survivors of intimate partner violence (N = 238; 51.7% White/Non-Hispanic). Latent markers of positive emotionality, somatic arousal, and generalized distress were also estimated. A 3-factor version of the Simms et al. (2002) Dysphoria model was identified as a preferred solution, with Intrusion and Avoidance criteria collapsed on a common dimension. Analyses revealed moderate correlations of generalized distress with Intrusion-Avoidance, Dysphoria, and Hyperarousal dimensions (r = .30–.38). Intrusion-Avoidance and Hyperarousal factors evidenced specificity for the core aspects of anxiety while Dysphoria demonstrated an association with the characteristic features of depression when controlling for nonspecific distress. Hyperarousal was the only symptom dimension holding a unique association with cumulative trauma controlling for somatic arousal, positive emotionality, and generalized distress. Results offer preliminary support for the specificity of core dimensions of PTSD above and beyond the influence of nonspecific distress.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
The diagnosis of posttraumatic stress disorder (PTSD) has been controversial since its introduction in DSM-III (APA 1980). Concerns with the nosology of this condition involve the nature of its relation to other forms of psychopathology and the extent to which symptoms hold unique associations with life threatening or traumatic events (e.g., Rosen and Lilienfeld 2008; Spitzer et al. 2007). From an empirical standpoint, the high degree of comorbidity with other conditions questions the validity of PTSD as a diagnostic construct. Several authors have suggested that PTSD may be best conceptualized as a syndrome of nonspecific distress given its overlap with generalized features of anxiety and depression (e.g., Bodkin et al. 2007; Watson 2005). From a clinical perspective, a lack of clarity on what symptoms best capture a unique pathological response to threatened death, serious injury, and/or violation of physical integrity continues to limit the assessment of trauma-related disorders (Rosen et al. 2010; Watson 2009). Conceptualizations giving greater weight to symptoms most characteristic of exposure to traumatic or life-threatening events could enhance the sensitivity and specificity of diagnosis. Despite a proliferation of research over the past four decades, the question of what makes PTSD PTSD remains a matter of continued debate (Rasmussen et al. 2019).
Specificity and General Distress: A Quadripartite Model
Comorbidity models are one approach to conceptualizing overlap noted in the larger clinical literature. In a review of this research, Watson (2009) proposes a novel framework intended to capitalize on the strengths of existing models of comorbidity. Whereas previous efforts to account for the interrelation of mood- and anxiety-focused conditions include systems exploring overlap at both the symptom (e.g., Barlow et al. 1996; Clark and Watson 1991) and the diagnostic (e.g., Brown and Barlow 1992; Mineka et al. 1998) level, Watson’s (2009) quadripartite model offers a compromise, calling instead for analyses to target individual symptom dimensions of relevant conditions. This approach maintains DSM nosology as an organizing framework while simultaneously addressing the heterogeneity of symptom content within a given disorder.
From a quadripartite perspective, symptom dimensions of a target condition are examined with respect to two primary characteristics: specificity and general distress variance. Specificity involves the extent to which symptom dimensions are more closely related to the unique features of anxiety or depression. This component of the model borrows from early, symptom-based theories identifying somatic arousal (e.g., dizziness, shaking) as characteristic of pathological anxiety, and low levels of positive emotionality (e.g., low interest, low optimism) as unique to depression (e.g., Barlow et al. 1996; Clark and Watson 1991). General distress variance, by contrast, refers to the overlap of symptom dimensions with markers of nonspecific distress (e.g., sadness, worry). As with disorder-based models of comorbidity (e.g., Brown and Barlow 1992; Mineka et al. 1998), distress variance in Watson’s framework is conceptualized as a nonspecific component of negative affectivity, believed to account for the high comorbidity of mood- and anxiety-related conditions.
The combination of specificity and general distress variance yields a framework in which symptom dimensions of a given disorder are placed in one of four quadrants: (I) those marked by high distress [i.e., identified by strong associations with negative affectivity] and high specificity [i.e., identified through differential associations with the cardinal features of anxiety (somatic arousal) or depression (low positive emotion)], (II) those marked by low distress and high specificity, (III) those marked by high distress and low specificity, and (IV) those marked by low distress and low specificity (see Fig. 1). Symptoms demonstrating high specificity for anxiety- or depression-related concerns (quadrants I & II) are viewed as critical indicators of diagnosis. Suicidality and positive affect are given as examples of symptoms with high specificity for depression (i.e., stronger correlations with low positive emotion vs. somatic arousal) but differing in their relation to generalized distress (Watson 2009). By contrast, symptoms characterized by low specificity (i.e., similar correlations with markers of both anxiety and depression) and high distress (i.e., strong correlations with negative affectivity; quadrant III) are viewed as nonspecific indicators of pathology, capturing the shared features of mood- and anxiety-related conditions. Symptoms in the final quadrant – those characterized by low specificity and low distress (e.g., appetite disturbance in depression) – are seen as contributing minimally to the identification of disorder and are recommended for possible removal from diagnostic algorithms.
Graphical representation of Watson’s (2009) Quadripartite Model. General distress involves the strength of the association of symptom dimensions with measures of nonspecific distress. Specificity involves the degree to which symptom dimensions are more strongly correlated with core aspects of anxiety (somatic arousal) versus depression (positive emotionality) or vice versa
Characterizing PTSD in the Quadripartite Model
Conclusions regarding the specificity and general distress variance of PTSD were provided in Watson’s (2009) initial presentation of the quadripartite model. Given that symptom dimensions serve as the fundamental unit of analysis for this framework, a pair of structural models with wide empirical support (e.g., Elhai and Palmieri 2011; Marshall et al. 2013; Yufik and Simms 2010) were selected as the basis for the 2009 review. The first model - forwarded by King et al. (1998) - identifies correlated dimensions of Reexperiencing, Avoidance, Numbing, and Hyperarousal. From a quadripartite perspective, Reexperiencing, Avoidance, and Hyperarousal dimensions are expected to demonstrate greater specificity for the core aspects of anxiety whereas Numbing is seen as more closely related to depression (Watson 2009).
A second model - proposed by Simms et al. (2002) - draws on early theories of comorbidity to account for the overlap of PTSD and co-occurring conditions. Whereas Reexperiencing and Avoidance dimensions in the Simms model are identical to those proposed by King et al. (1998), Simms restricts the specification of Hyperarousal to symptoms of hypervigilance and exaggerated startle, indicators believed to be more closely related to anxiety- versus depression-related concerns. All other criteria are collapsed on a nonspecific Dysphoria dimension intended to capture variability attributable to generalized distress.
Two conclusions were drawn from Watson’s (2009) initial review of studies exploring the relation of PTSD symptom clusters with general measures of anxiety and depression. First, all dimensions in the King et al. (1998) Numbing and Simms et al. (2002) Dysphoria models were characterized by high distress variance given strong correlations with external measures of negative affectivity. Second, symptom clusters in both models were found to demonstrate limited specificity as indicated by similar correlations with measures of anxiety and depression. Dysphoria was identified as a possible exception, with some research suggesting stronger associations of Dysphoria with depression as compared to correlations with generalized anxiety (Grant et al. 2008; Simms et al. 2002). Results of the preliminary review, however, failed to support the hypothesized specificity of Reexperiencing, Avoidance, and Hyperarousal for anxiety- versus depression-related concerns.
Although Watson’s (2009) initial review provides a critical assessment of data available during development of the quadripartite model, methodological aspects of studies included in the summary limit strong conclusions regarding the specificity of PTSD. First, specificity estimates were drawn exclusively from research exploring correlations between observed scores for PTSD, anxiety, and depression (Elklit and Shevlin 2007; Simms et al. 2002; Witteveen et al. 2006). More recent studies exploring the relation of latent factor dimensions with external criteria offer preliminary evidence for the hypothesized specificity of Reexperiencing, Avoidance, and Hyperarousal for anxiety- versus depression-related concerns (e.g., Elhai et al. 2013; Forbes et al. 2012, 2015; Miller et al. 2010; Wang et al. 2011a, b). Second, research included in Watson’s (2009) review targeted correlations of symptom dimensions with broad clinical measures as opposed to scales capturing the unique aspects of anxiety and depression. Analyses exploring differential associations with indices of positive affectivity and somatic arousal are expected to provide stronger tests of hypothesized specificity. Finally, the extent to which PTSD symptom dimensions hold unique associations with the frequency/severity of reported trauma warrants further attention. Trauma-related disorders are unique among psychological conditions in that diagnosis is formally tied to an external stressor (McNally 2003; Rosen and Lilienfeld 2008). Although not a specific component of Watson’s (2009) larger model, evidence of differential associations with global trauma history could help determine what symptom dimensions best characterize pathological response to actual or threatened death, injury, and sexual violence. Meta-analyses provide support of reliable correlations between individual symptom dimensions and the severity of past exposure (Gootzeit and Markon 2011). However, unique associations controlling for somatic arousal, positive emotionality, and non-specific distress remain unexplored.
The Current Study
Aims of the current study were to examine the specificity and general distress variance of DSM-IV symptom dimensions in help-seeking survivors of intimate partner violence (IPV). For this research, King et al. (1998) Numbing and Simms et al. (2002) Dysphoria models were chosen as the primary basis of analysis given [a] extensive empirical support for the structural validity of these solutions (e.g., Elhai and Palmieri 2011; Marshall et al. 2013; Yufik and Simms 2010), [b] efforts to maximize comparability to the results of Watson’s (2009) initial review, and [c] the direct influence of these models and associated research on the conceptualization of PTSD in DSM-5 (APA 2013; Rasmussen et al. 2019). The evaluation of symptom dimensions specified in the previous edition of DSM is intended to provide context to the larger structural literature and to offer a methodological framework for continued research exploring the specificity and general distress variance of symptom dimensions in novel models of PTSD.
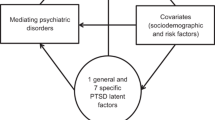
For this research, scores from the Clinician-Administered PTSD Scale (CAPS; Blake et al. 1990) were used to assess symptom dimensions outlined in the Numbing and Dysphoria models. Sub-models combining symptoms of intrusion and avoidance on a common dimension were also estimated given evidence of potential collinearity in CAPS ratings for these scales (e.g., Forbes et al. 2015). Viable structural models were then combined with an independent measurement model specifying latent dimensions of generalized distress, positive emotionality, and somatic arousal. Factor correlations in the joint measurement model were used to test hypotheses regarding the specificity and general distress variance of PTSD symptom dimensions as described in the quadripartite framework. Finally, joint measurement models were respecified to regress symptom dimensions onto external covariates including reported trauma history. Path coefficients were used to determine partial specificity, defined in this study as the unique relation of symptom dimensions with characteristic elements of anxiety, depression, and cumulative trauma, controlling for variability attributable to nonspecific distress.
A number of hypotheses were proposed. First, fit indices and factor correlations were expected to provide the strongest support for the 4-factor Dysphoria model based on evidence from the larger literature (Yufik and Simms 2010). Second, all symptom dimensions were expected to show moderate to large associations with generalized distress (Hypothesis 2: Distress Variance). Third, Intrusion, Avoidance, and Hyperarousal dimensions characterized by anxiety-focused difficulties were expected to evidence stronger correlations with somatic arousal as compared to positive emotionality. An opposite pattern was expected for Numbing and Dysphoria dimensions (Hypothesis 3: Specificity). Finally, path analyses were expected to provide evidence for unique associations of somatic arousal and trauma history with Intrusion, Avoidance, and Hyperarousal dimensions, controlling for positive emotionality and nonspecific distress (Hypothesis 4: Partial Specificity). Unique effects of positive emotionality on Numbing and Dysphoria dimensions were also expected given the overlap of these factors with characteristic features of depression.
Methods
Participants
Data were collected through a university-based research clinic specializing in the assessment and treatment of PTSD following IPV (e.g., Beck et al. 2014; Cody et al. 2017; Dodson and Beck 2017). Referral sources included health care professionals, legal advisors, newspaper advertisements, faith communities, and public service announcements. Individuals presenting for assessment received a comprehensive psychosocial interview including administration of the CAPS and the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; DiNardo et al. 1994). Participants also were given a battery of self-report measures to return in a subsequent feedback session. All procedures received Institutional Review Board approval.
Of the 375 individuals completing the diagnostic interview, 28 were excluded given experiences failing to meet Criterion-A for PTSD (APA 1994). Eight women were removed due to evidence of cognitive impairment based on scores from the Montreal Cognitive Assessment (Nasreddine et al. 2005). Eleven were excluded given evidence of severe psychopathology (e.g., symptoms of psychosis). Nine participants were dropped in response to concerns with the reliability of reported symptoms. Eighty-one failed to return self-report questionnaires necessary for inclusion. Participants with incomplete data were younger (p = .038; d = .27), more likely to identify as an ethnic minority (p = .028; ϕ = .12), and indicated lower levels of education (p = .021; ϕ = .22) than those in the final sample (N = 238; see Table 1).
Measures
PTSD
Trauma-related symptoms were assessed using the CAPS. The CAPS is a clinician-rated instrument widely considered to be the gold-standard assessment of DSM-IV PTSD (Weathers et al. 2001). Items correspond to cardinal symptoms of PTSD, with interviewers rating the frequency and severity of symptoms experienced over the past 30 days on a 0–4 Likert scale. For this study, symptom scores were calculated as the sum of corresponding frequency and severity ratings (range 0–8).
Interviews were administered by trained doctoral students supervised by the fourth author. Assessments were presented in weekly staffing meetings attended by all clinicians. Interviews were recorded with approximately 30% of cases (n = 74) selected at random for independent review. Reliability estimates for individual symptom scores (one-way random effects, single measure) ranged from good to excellent (ICC = .66 to .95; Cicchetti 1994). Loss of interest was an exception, falling in the “fair” range (ICC = .58). Estimates for this item were found to be attenuated by a handful of cases in which loss of interest was attributed to symptoms of comorbid depression by the reliability clinician. Consensus ratings were established by the research team for all discrepancies.
External Factors: Generalized Distress, Positive Emotionality, Somatic Arousal
Consistent with previous research (Marshall et al. 2010), indicators of generalized distress, positive emotionality, and somatic arousal were selected from measures demonstrating conceptual similarity to items from General Distress, Anhedonic Depression, and Anxious Arousal subscales of Watson and Clark’s (1991) Mood and Anxiety Symptom Questionnaire (MASQ). Candidate indicators for the current study were operationalized as those similar in content to MASQ items demonstrating strong loadings on their intended factor (λ ≥ .50) and weak loadings on all others (λ ≤ .34) as reported in development research for the MASQ (Watson et al. 1995a). Correlations between MASQ General Distress, Anhedonic Depression, and Anxious Arousal scales in the original development study were rGD.AD = .69, rGD.AA = .75, and rAA.AD = .49, respectively (Watson et al. 1995b).
Generalized Distress
Generalized distress was modeled using four items from the Beck Depression Inventory-II (BDI-II; Beck et al. 1996) and the Beck Anxiety Inventory (BAI; Beck et al. 1988).Footnote 1 For this study, two indicators corresponding to MASQ General Distress: Mixed Symptom items (“Trouble making decisions” ➔ BDI-II #13: Indecisive; “Felt irritable” ➔ BDI-II #17: Irritability) and single indicators corresponding to MASQ General Distress: Depressive Symptom (“Felt sad” ➔ BDI-II #1: Sadness) and MASQ General Distress: Anxious Symptom (“Felt afraid” ➔ BAI #17: Scared) items were selected as markers of nonspecific distress. The internal consistency of items selected as markers of generalized distress was acceptable (α = .70).Footnote 2
Positive Emotionality
Four items from the Internalized Shame Scale (ISS: Cook 1994) were used as markers of positive emotionality. Indicators consistent with MASQ items for “Felt successful” (ISS #4: All in all, I’m inclined to feel that I am a success); “Was proud of myself” (ISS #9: I feel I have much to be proud of); “Felt good about myself” (ISS #18: On the whole, I am satisfied with myself); and “Felt confident” (ISS #28: I take a positive attitude towards myself) were selected based on evidence that indicators of positive emotional experience more strongly reflect the unique aspects of depression than negatively valenced items (Watson et al. 1995a). Coefficient alpha was excellent for markers on the current scale (α = .92).
Somatic Arousal
Somatic arousal was identified using four items from the BAI. Items corresponding to MASQ indicators for “Felt numbness or tingling” (BAI #1: Numbness or tingling), “Felt dizzy, lightheaded” (BAI #6: Dizzy or lightheaded), “Shaky hands” (BAI #13: Shaky), and “Felt faint” (BAI #19: Faint) were chosen as markers for the current study. The internal consistency of selected indicators was acceptable (α = .72).
Cumulative Trauma History
History of probable trauma was assessed using a screener adapted from the Life Events Checklist (Blake et al. 1990). Participants were instructed to indicate whether they had directly experienced, witnessed, or learned about any of 18 potentially traumatic events. Respondents also were permitted to indicate exposure to other stressful or life-threatening events not included on the measure. Exposure severity was calculated as the number of events reported as directly experienced.
Analytic Approach
Data Screening
Indicators in this help-seeking sample evidenced moderate deviations from normality (skew ≤ |1.9|; kurtosis ≤ |2.2|) but remained within acceptable limits for multivariate analysis (Kline 2016; Tabachnick and Fidell 2013). Standardized scores indicated possible extreme values for flashbacks (z ≤ 3.41) and detachment (z ≤ 3.92); however, no corrective action was taken given acceptable item distributions and the expectation of boundary values in a large help-seeking sample. No concerns were noted with respect to linearity, collinearity, or multivariate outliers. Indicators of generalized distress and somatic arousal were multiplied by a factor of 2 to address ill-scaling of the variance-covariance matrix (Kline 2016).
Latent Variable Models
Structural analyses of PTSD symptom dimensions included 4-factor King et al. (1998) Numbing and Simms et al. (2002) Dysphoria models. Given research by Forbes et al. (2015) indicating collinearity between CAPS Intrusion and Avoidance dimensions, 3-factor versions of the Numbing and Dysphoria models were also examined, collapsing Intrusion and Avoidance criteria along a single dimension.
Adequacy of a measurement model specifying factors for generalized distress, positive emotionality, and somatic arousal was examined following the evaluation of structural models for PTSD. Correlations between symptom dimensions and latent factors for generalized distress, positive emotionality, and somatic arousal were then examined in joint measurement models to test hypotheses regard specificity and general distress variance of PTSD.
In the final step of analyses, joint measurement models were respecified to regress PTSD symptom dimensions onto indices of generalized distress, somatic arousal, positive emotionality, and cumulative trauma history. Path coefficients were used to estimate the unique relation of external criterion with corresponding symptom dimensions.Footnote 3
Model Evaluation
Analyses were conducted in MPlus Version 8.2 (Muthén and Muthén 1998–2018) using maximum likelihood estimation with robust standard errors (MLR). Fit indices included the Bayesian information criterion (BIC); comparative fit index (CFI) and Tucker Lewis index (TLI); the root mean square error of approximation (RMSEA) with accompanying 90% confidence intervals; and the standardized root-mean-square residual (SRMR). BIC is a predictive index reflecting fit in hypothetical replications of randomly drawn samples. Values are used to compare non-nested models with lower scores indicating greater likelihood of replication (Kline 2016). Reductions in BIC values ranging from 0 to 2; 2 to 6; 6 to 10; and greater than 10 relative to a competing model serve as benchmarks for weak, positive, strong, and very strong evidence of superior replicability (Raftery 1995).
CFI and TLI, by contrast, are comparative indices, evaluating global fit relative to a hypothetical model specifying zero correlation between indicators (Kline 2016). Values exceeding .90 and .95 are interpreted as evidence of adequate and close fit, respectively (Bentler 1990; Hu and Bentler 1999). RMSEA is a parsimony-corrected, population-based estimator of global fit. Point estimates ≤ .05, ≤ .06, and ≤ .08 are interpreted as evidence of close, excellent, and adequate fit (Browne and Cudeck 1993; Hu and Bentler 1999). Finally, SRMR was examined as an indicator of the average discrepancy between observed and model-implied correlations. SRMR values < .10 and ≤ .08 are interpreted as evidence of acceptable and excellent fit, respectively (Hu and Bentler 1999; Kline 2016).
Quadripartite Assessment
Cohen’s (1988) benchmarks for small (r = .10), medium (r = .30), and large (r = .50) effects were used to qualify the magnitude of correlations between PTSD symptom dimensions and generalized distress (Hypothesis 2). The specificity of symptom dimensions for somatic arousal and positive emotionality was examined using Meng et al. (1992) procedures for comparing correlated correlation coefficients (Hypothesis 3). These analyses permit the formal comparison of dependent correlations with inferential tests utilizing a standard Z-distribution (Meng et al. 1992). Finally, R2 values of .01, .09, and .25 were used as benchmarks for small, medium, and large effects (Cohen 1988) in respecified structural models regressing PTSD symptom dimensions onto external covariates (Hypothesis 4).
Results
PTSD Symptom Dimensions
Indices of global fit are provided in Table 2. CFI, TLI, RMSEA, and SRMR values were consistent with benchmarks for adequate to excellent fit in the 4-factor Numbing and Dysphoria solutions. Coefficients indicated incremental improvement in fit for the 4-factor Dysphoria model whereas change in BIC (BICΔ = 20.8) indicated a clear preference relative to the corresponding Numbing solution. Indicators demonstrated salient loadings (λ ≥ .30; Brown 2006) on their respective factors in both models. Discriminant validity was a concern, however, given strong evidence of collinearity between Intrusion and Avoidance dimensions in the 4-factor Dysphoria (φ = .921) and the 4-factor Numbing (φ = .922) solutions.
Three-factor versions of these models (collapsing Intrusion and Avoidance on a common factor) produced improvements with respect to parsimony and overall fit. Fit indices for the 3-factor Numbing solution were similar to those in the parent model although collinearity between Intrusion-Avoidance and Hyperarousal factors remained problematic (φ = .913). Fit of the 3-factor Dysphoria solution was also similar to the corresponding 4-factor model but with improvements in the discriminant validity of latent factors. BIC values (BICΔ = 21.1) continued to indicate a relative preference for the 3-factor Dysphoria model as compared to the 3-factor Numbing solution.
Consistent with observed change in BIC, formal comparison of nested models (Satorra and Bentler 2010) provided little evidence for reductions in the fit of 3-factor Dysphoria (χ2Δ [3] = 1.64; p = .651) or 3-factor Numbing (χ2Δ [3] = 1.81; p = .612) models relative to parent 4-factor solutions. Based on these data, the 3-factor Dysphoria model was selected for further evaluation given evidence of parsimony, acceptable fit, adequate discriminant validity, and increased replicability as indicated by BIC. Item loadings for this model are presented in Table 3.Footnote 4
Quadripartite Assessment
Estimation of the measurement model containing general distress, somatic arousal, and positive emotionality factors provided clear evidence of close fit (χ251 = 85.0; CFI = .966; TLI = .957; RMSEA = .053, 90% CI [.032, .072]; SRMR = .048). All indicators demonstrated salient loadings on their corresponding dimensions (see Table 3).
Estimation of the joint 3-factor Dysphoria model provided further evidence of close fit (see Table 2). Factor loadings for indicators of PTSD symptom clusters and external covariates were similar to those in the component model (see Table 3).
Correlations between PTSD symptom dimensions and external factors in the joint 3-factor Dysphoria model were generally consistent with hypotheses (see Table 4). Intrusion-Avoidance, Dysphoria, and Hyperarousal dimensions all demonstrated moderate associations with generalized distress [Hypothesis 2: Distress Variance]. As predicted, both Intrusion-Avoidance (z = 2.77, p = .006) and Hyperarousal factors (z = 4.29, p < .001) were more strongly correlated with somatic arousal than with positive emotionality [Hypothesis 3: Specificity]. Dysphoria, by contrast, showed comparable correlations with both outcomes (z = 0.39; p = .694).
Partial Specificity
The joint 3-factor Dysphoria model was respecified to regress PTSD symptom dimensions onto indices of generalized distress, positive emotionality, somatic arousal, and cumulative trauma history. Variance attributable to the combination of these indicators was consistent with large effects for Intrusion-Avoidance (R2 = .31, 95% CI [.138, .483]), Dysphoria (R2 = .29, 95% CI [.147, .426]), and Hyperarousal (R2 = .30, 95% CI [.126, .470]) dimensions. Path coefficients were generally consistent with hypotheses. Both somatic arousal (β = .63; b = 1.09, p = .006) and positive emotionality (β = −.27; b = −.503, p = .019) demonstrated unique associations with Intrusion-Avoidance, independent of generalized distress and prior trauma. Positive emotionality also evidenced a unique association with Dysphoria (β = −.34; b = −.48, p = .003). Somatic arousal (β = .59; b = 1.21, p = .003) and cumulative trauma history (β = .17; b = .14, p = .024) both demonstrated associations with Hyperarousal controlling for other factors.
Discussion
Concerns with the discriminant validity of PTSD have called into question whether symptoms represent a distinct clinical syndrome or whether post-trauma reactions are best conceptualized as nonspecific distress common across both mood- and anxiety-related disorders. Although symptom dimensions in the current sample did show moderate correlations with generalized distress, results also provide support for the specificity of multiple dimensions with the core features of anxiety. Confirmatory analyses identified a 3-factor version of the Simms et al. (2002) Dysphoria model as a preferred solution based on parsimony, incremental fit, the separation of latent factors, and information criteria denoting greater potential for replicability (Kline 2016; Raftery 1995). In this model, Intrusion-Avoidance evidenced moderate distress variance and high specificity for the core features of anxiety. Regression analyses offered further support for a unique association of Intrusion-Avoidance and somatic arousal when controlling for nonspecific distress. Results also identified a unique relation between Intrusion-Avoidance and positive emotionality although the magnitude of this association (βPE = −.27) was substantially smaller than the corresponding effect for somatic arousal (βSA = .63). Results may be interpreted as consistent with research identifying intrusive thoughts and corresponding avoidance as characteristic of anxiety-related difficulties (e.g., Forbes et al. 2015; Wang et al. 2011a, 2011b).
The characteristics of Dysphoria were also largely consistent with the conceptualization of this dimension as a marker of nonspecific distress (e.g., Gootzeit and Markon 2011; Simms et al. 2002) although conclusions regarding specific hypotheses were mixed. Contrary to trends noted in Watson’s (2009) review, the correlations of Dysphoria with positive emotionality and somatic arousal were similar, failing to provide evidence of specificity for the characteristic features of depression. Dysphoria did, however, demonstrate a unique relation with positive emotionality in subsequent regression analyses, controlling for associations with generalized distress and other external factors. Results suggest that Dysphoria may be interpreted as a dimension of low specificity and moderate to high distress as viewed from a quadripartite lens. The analysis of partial specificity provides some support for a unique association with the characteristic aspects of depression although strong conclusions await further replication.
Characteristics of the Simms et al. (2002) Hyperarousal dimension were relatively unambiguous given the results of these analyses. Hyperarousal evidenced a moderate association with generalized distress with stronger correlations for somatic arousal as compared to positive emotionality. Effects were replicated in subsequent regression analyses with somatic arousal demonstrating a unique relation with Hyperarousal, controlling for generalized distress and other external factors. From a quadripartite perspective, data suggest that Simms and colleagues’ conceptualization of hyperarousal is best qualified as a dimension marked by moderate distress variance and high specificity for the characteristic features of anxiety.
Simms’ Hyperarousal was also notable in that this was the only dimension found to hold a unique association with cumulative trauma. In these data, difficulties with hypervigilance and exaggerated startle became increasingly severe as a function of compounding exposure to lifetime trauma. The unique relation between Hyperarousal and trauma severity is particularly important for the conceptualization of PTSD in that diagnostic criteria presuppose exposure to some precipitating event (APA 1980, 1994, 2013; Rosen and Lilienfeld 2008). Whereas existing research provides support for a general dose-response relation with global symptom severity (e.g., Brewin et al. 2000; Ozer et al. 2003), data in this study point to a specific correspondence between cumulative trauma and the Simms et al. specification of Hyperarousal. Results are consistent with existing studies identifying Hyperarousal as a core feature of PTSD (e.g., Marshall et al. 2006; Schell et al. 2004). While associations between PTSD dimensions and global trauma severity have been previously documented (e.g., Gootzeit and Markon 2011), these data are the first to examine unique relations with cumulative trauma controlling for shared variance with positive emotionality, somatic arousal, and nonspecific distress.
Evidence supporting the combination of Intrusion and Avoidance symptoms also merits discussion. Despite precedent for the separation of Intrusion and Avoidance in the existing literature, collinearity in both 4-factor solutions (φ = .92) precluded reasonable interpretation of these dimensions as empirically distinct constructs (Brown 2006). Effects are consistent with structural analyses supporting the conceptualization of intrusion and avoidance as indicators of a common underlying factor (e.g., Charney and Keane 2007; Forbes et al. 2015; Gootzeit et al. 2015; Hunt et al. 2018). Results of these analyses and those of previous studies may be interpreted as reflecting the functional relation between unwanted memories and effortful avoidance hypothesized in prominent models of PTSD (e.g., Creamer et al. 1992; Foa and Rothbaum 1998). Avoidance is conceptualized as a direct reaction to memories of the traumatic event(s) and associated symptoms of intrusion. DSM avoidance criteria are similarly linked to behaviors resulting from trauma-related affect, memories, and cues (APA 1994, 2013). Although Intrusion and Avoidance dimensions in these analyses were not differentiable from an empirical standpoint, future research should consider carefully the functional relation of these symptoms.
Limitations and Future Directions
Interpretation of results should be made within the context of the study’s relative strengths and limitations. Data were collected from a racially and economically diverse sample of help-seeking women. Trauma symptoms were assessed using gold-standard interview methods with clinician ratings monitored through ongoing reliability checks. Analyses were organized to test specific assumptions outlined in Watson’s (2009) quadripartite model, including a priori hypotheses involving the relation of symptom dimensions with theory-based markers of positive emotionality, somatic arousal, and generalized distress.
Acknowledging these strengths, limitations of the study offer guidance for continued work in this area. First, data available for the current project were restricted to symptom criteria outlined in DSM-IV. Changes to diagnostic criteria in DSM-5 (APA 2013) – specifically the inclusion of indicators for negative expectations of the self, others, or the world (D2); blame of self or others (D3); persistent negative emotional state (D4); irritable/aggressive behavior (E1); and reckless/self-destructive behavior (E2) – could impact the distress variance and specificity profiles of revised Alteration in Cognition and Mood (Cluster D) and Alteration in Arousal and Reactivity (Cluster E) dimensions. However, symptom dimensions demonstrating the greatest degree of specificity for anxiety-related difficulties remain unaltered in DSM-5. Criteria for Intrusion and Avoidance dimensions are identical across DSM-IV and DSM-5 formulations. Symptoms of hypervigilance and exaggerated startle captured in Simms et al.’ (2002) specification of Hyperarousal are also unchanged. The consistency of symptom criteria across editions provide an opportunity for these data to 1.) inform conclusions drawn from the larger body of existing research and 2.) shape hypotheses regarding the specificity and general distress variance of Intrusion, Avoidance, and Simms et al. Hyperarousal dimensions in DSM-5. While the extent to which changes in DSM-5 impact the characteristics of revised Cognition-Mood and Arousal-Reactivity dimensions remains an open question, our hope is that these preliminary data help structure a system for ongoing study in this area.
Inferences are also necessarily limited to female survivors of IPV. Help-seeking women in this sample demonstrated elevated levels of overall psychopathology (76.9% with at least one mood, anxiety, or substance use disorder as determined by the CAPS and ADIS-IV; M = 1.9, SD = 1.6) with 52.5% of participants meeting criteria for full or partial PTSD (i.e., Intrusion criteria met with one missing symptom in Cluster C or Cluster D; Asmundson et al. 2004). Comorbidity in this sample is characteristic of difficulties observed in the help-seeking trauma populations and provides a demonstration of the radiating impact of intimate partner violence (Beck et al. 2014; Dutton 2009). That said, it is important to recognize that only a minority of women in this study (21.0%) reported symptoms meeting full diagnostic criteria for PTSD. It is possible that distinct patterns of specificity and general distress variance could emerge in participants selected based on PTSD diagnosis. It is also important to note that differential patterns of effects could be observed in other trauma populations. Veterans, for example, could fail to demonstrate unique associations between cumulative trauma and Hyperarousal symptoms given training experiences that reinforce persistent vigilance.5 Continued research with increasing diverse samples is needed to develop broad conclusions regarding the specificity and general distress variance of PTSD symptom dimensions.
Conclusions also would be strengthened through the incorporation of specific measures of positive emotionality, somatic arousal, and generalized distress. Given recent critiques of the existing literature (Elhai and Palmieri 2011; Marshall et al. 2013), research conducted over the past decade has begun to place a greater emphasis on evaluating links between proposed symptom dimensions and relevant external criteria. The concern from a quadripartite perspective is that studies differentiating associations with the core features of anxiety and depression from those with markers of generalized distress are limited (but see Miller et al. 2010). As noted in the Methods, indicators of positive affectivity, somatic arousal, and generalized distress in the current study evidenced clear overlap with corresponding MASQ items. Factor correlations were also comparable to observed associations between MASQ scales among help-seeking veterans in Watson et al.’s (1995b) initial study. Secondary analysis of scales in the current set provide a unique opportunity to examine the characteristics of posttrauma symptom dimensions from the perspective of Watson’s (2009) quadripartite model. However, replication using structured measures in continued research will provide increasingly precise estimates of these effects.
Finally, evaluation of the discriminant and convergent relations of PTSD symptom dimensions were limited to a subset of structural models receiving broad support in the literature (Elhai and Palmieri 2011; Marshall et al. 2013; Yufik and Simms 2010). Evaluation of Numbing and Dysphoria models served to maintain a focus on dimensions targeted in Watson’s (2009) initial summary. However, research evaluating the factor structure of PTSD is extensive, with studies providing arguments for increasingly nuanced models (e.g., Armour et al. 2015; Armour et al. 2016; Elhai et al. 2011; Liu et al. 2014). Although a comprehensive assessment of solutions having received support in the larger literature was beyond the scope of this study, we would note that the quadripartite model does offer a compelling framework from which to assess the convergent and discriminant validity of dimensions outlined in alternative models of PTSD. Trends in the recent literature indicate that such comparisons will be increasingly important for continued work in this area (Rasmussen et al. 2019).
Conclusions
The extent to which diagnostic constructs capture unique aspects of psychopathology is a matter of ongoing debate in the larger clinical literature. Evaluation of symptom data in the current study identified Intrusion-Avoidance and Simms et al. Hyperarousal as dimensions marked by moderate distress with high specificity for anxiety-related difficulties. Simms’ specification of Hyperarousal was the only symptom dimension to demonstrate a unique relation with cumulative trauma history after accounting for shared relations with positive emotionality, somatic arousal, and generalized distress. Continued assessment in increasingly diverse trauma samples promise to strengthen conclusions regarding the unique and nonspecific components of PTSD.
Notes
The number of items used to identify latent NA, PA, and SA factors was limited to manage the size of the joint measurement model. Efforts were taken to select indicators capturing various aspects of the target construct.
We thank an anonymous reviewer for their assistance with identification of this scale.
MPlus syntax for the final series of models are provided in a supplemental appendix.
Estimates of specificity and general distress variance for the 3-factor Numbing model are available from the first author upon request.
References
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3th ed.). Washington DC: Author.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington DC: Author.
Armour, C., Műllerová, J., & Elhai, J. D. (2016). A systematic literature review of PTSD's latent structure in the diagnostic and statistical manual of mental disorders: DSM-IV to DSM-5. Clinical Psychology Review, 44, 60–74.
Armour, C., Tsai, J., Durham, T. A., Charak, R., Biehn, T. L., Elhai, J. D., & Pietrzak, R. H. (2015). Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid Anhedonia and externalizing behaviors model. Journal of Psychiatric Research, 61, 106–113.
Asmundson, G. J., Stapleton, J. A., & Taylor, S. (2004). Are avoidance and numbing distinct PTSD symptom clusters? Journal of Traumatic Stress, 17, 467–475.
Barlow, D. H., Chorpita, B. F., & Turovsky, J. (1996). Fear, panic, anxiety, and disorders of emotion. In D. A. Hope (Ed.), Nebraska symposium on motivation, 1995: Perspectives on anxiety, panic, and fear (pp. 251–328). Lincoln, NE, US: University of Nebraska Press.
Beck, A. T., Epstein, N., Brown, G., & Steer, R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56, 893–897.
Beck, A. T., Steer, R. A., & Brown, G. (1996). Manual for the Beck depression inventory II. (BDI-II). San Antonio: Psychological Corporation.
Beck, J. G., Clapp, J. D., Jacobs-Lentz, J., McNiff, J., Avery, M. L., & Olsen, S. A. (2014). The association of mental health conditions with employment, interpersonal, and subjective functioning after intimate partner violence. Violence Against Women, 20, 1321–1337.
Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246.
Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Klauminzer, G., Charney, D. S., et al. (1990). Clinician-administered PTSD scale (CAPS). Boston, MA: National Center for Post-traumatic Stress Disorder, Behavioral Science Division.
Bodkin, J. A., Pope, H. G., Detke, M. J., & Hudson, J. I. (2007). Is PTSD caused by traumatic stress? Journal of Anxiety Disorders, 21, 176–182.
Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748.
Brown, T. A. (2006). Confirmatory factor analysis for applied research. New York: Guilford Press.
Brown, T. A., & Barlow, D. H. (1992). Comorbidity among anxiety disorders: Implications for treatment and DSM-IV. Journal of Consulting and Clinical Psychology, 60, 835–844.
Browne, M. W., & Cudeck, R. (1993). Alternative ways of assessing model fit. In K. A. Bollen & J. S. Long (Eds.), Testing structural equation models. Newbury Park, CA: Sage Publications.
Charney, M. E., & Keane, T. M. (2007). Psychometric analyses of the clinician-administered PTSD scale (CAPS)--Bosnian translation. Cultural Diversity and Ethnic Minority Psychology, 13, 161–168.
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6, 284–290.
Clark, L. A., & Watson, D. (1991). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100, 316–336.
Cody, M. W., Jones, J. M., Woodward, M. J., Simmons, C. A., & Gayle Beck, J. (2017). Correspondence between self-report measures and clinician assessments of psychopathology in female intimate partner violence survivors. Journal of Interpersonal Violence, 32, 1501–1523.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates, Inc..
Cook, D. R. (1994, 2001). Internalized shame scale: Technical manual. North Tonawanda, NY: Multi-Health Systems, Inc.
Creamer, M., Burgess, P., & Pattison, P. (1992). Reaction to trauma: A cognitive processing model. Journal of Abnormal Psychology, 101, 452–459.
DiNardo, P. A., Barlow, D. H., & Brown, T. A. (1994). Anxiety disorders interview schedule for DSM-IV. Oxford University Press.
Dodson, T. S., & Beck, J. G. (2017). Posttraumatic stress disorder symptoms and attitudes about social support: Does shame matter?. Journal of Anxiety Disorders, 47, 106–113.
Dutton, M. A. (2009). Pathways linking intimate partner violence and posttraumatic disorder. Trauma, Violence, & Abuse, 10, 211–224.
Elhai, J. D., Biehn, T. L., Armour, C., Klopper, J. J., Frueh, B. C., & Palmieri, P. A. (2011). Evidence for a unique PTSD construct represented by PTSD's D1–D3 symptoms. Journal of Anxiety Disorders, 25, 340–345.
Elhai, J. D., Layne, C. M., Steinberg, A. M., Brymer, M. J., Briggs, E. C., Ostrowski, S. A., & Pynoos, R. S. (2013). Psychometric properties of the UCLA PTSD reaction index. Part II: investigating factor structure findings in a national clinic-referred youth sample. Journal of Traumatic Stress, 26, 10–18.
Elhai, J. D., & Palmieri, P. A. (2011). The factor structure of posttraumatic stress disorder: A literature update, critique of methodology, and agenda for future research. Journal of Anxiety Disorders, 25, 849–854.
Elklit, A., & Shevlin, M. (2007). The structure of PTSD symptoms: A test of alternative models using confirmatory factor analysis. British Journal of Clinical Psychology, 46, 299–313.
Foa, E. B., & Rothbaum, B. O. (1998). Treating the trauma of rape: Cognitive-behavioral therapy for PTSD. New York, NY, US: Guilford Press.
Forbes, D., Elhai, J. D., Lockwood, E., Creamer, M., Frueh, B. C., & Magruder, K. M. (2012). The structure of posttraumatic psychopathology in veterans attending primary care. Journal of Anxiety Disorders, 26, 95–101.
Forbes, D., Lockwood, E., Elhai, J. D., Creamer, M., Bryant, R., McFarlane, A., et al. (2015). An evaluation of the DSM-5 factor structure for posttraumatic stress disorder in survivors of traumatic injury. Journal of Anxiety Disorders, 29, 43–51.
Gootzeit, J., & Markon, K. (2011). Factors of PTSD: Differential specificity and external correlates. Clinical Psychology Review, 31, 993–1003.
Gootzeit, J., Markon, K., & Watson, D. (2015). Measuring dimensions of posttraumatic stress disorder: The Iowa traumatic response inventory. Assessment, 22, 152–166.
Grant, D. M., Beck, J. G., Marques, L., Palyo, S. A., & Clapp, J. D. (2008). The structure of distress following trauma: Posttraumatic stress disorder, major depressive disorder, and generalized anxiety disorder. Journal of Abnormal Psychology, 117, 662–672.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55.
Hunt, J. C., Chesney, S. A., Jorgensen, T. D., Schumann, N. R., & deRoon-Cassini, T. A. (2018). Exploring the gold-standard: Evidence for a two-factor model of the clinician administered PTSD scale for the DSM–5. Psychological Trauma: Theory, Research, Practice, and Policy, 10, 551.
King, D. W., Leskin, G. A., King, L. A., & Weathers, F. W. (1998). Confirmatory factor analysis of the clinician-administered PTSD scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment, 10, 90.
Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). New York: Guilford Press.
Liu, P., Wang, L., Cao, C., Wang, R., Zhang, J., Zhang, B., Wu, Q., Zhang, H., Zhao, Z., Fan, G., & Elhai, J. D. (2014). The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. Journal of Anxiety Disorders, 28, 345–351.
Marshall, G. N., Schell, T. L., Glynn, S. M., & Shetty, V. (2006). The role of hyperarousal in the manifestation of posttraumatic psychological distress following injury. Journal of Abnormal Psychology, 115, 624.
Marshall, G. N., Schell, T. L., & Miles, J. N. (2010). All PTSD symptoms are highly associated with general distress: Ramifications for the dysphoria symptom cluster. Journal of Abnormal Psychology, 119, 126–135.
Marshall, G. N., Schell, T. L., & Miles, J. N. (2013). A multi-sample confirmatory factor analysis of PTSD symptoms: What exactly is wrong with the DSM-IV structure? Clinical Psychology Review, 33, 54–66.
McNally, R. J. (2003). Progress and controversy in the study of posttraumatic stress disorder. Annual Review of Psychology, 54, 229–252.
Meng, X., Rosenthal, R., & Rubin, D. B. (1992). Comparing correlated correlation coefficients. Psychological Bulletin, 111, 172–175.
Miller, M. W., Wolf, E. J., Harrington, K. M., Brown, T. A., Kaloupek, D. G., & Keane, T. M. (2010). An evaluation of competing models for the structure of PTSD symptoms using external measures of comorbidity. Journal of Traumatic Stress, 5, 631–638.
Mineka, S., Watson, D., & Clark, L. A. (1998). Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology, 49, 377–412.
Muthén, L. K., & Muthén, B. O. (1998-2018). Mplus User's Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén.
Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., et al. (2005). The Montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatric Society, 53, 695–699.
Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52.
Raftery, A. E. (1995). Bayesian model selection in social research. Sociological Methodology, 25, 111–164.
Rasmussen, A., Verkuilen, J., Jayawickreme, N., Wu, Z., & McCluskey, S. T. (2019). When did posttraumatic stress disorder get so many factors? Confirmatory factor models since DSM–5. Clinical Psychological Science, 7, 234–248.
Rosen, G. M., & Lilienfeld, S. O. (2008). Posttraumatic stress disorder: An empirical evaluation of core assumptions. Clinical Psychology Review, 28, 837–868.
Rosen, G. M., Lilienfeld, S. O., Frueh, B. C., McHugh, P. R., & Spitzer, R. L. (2010). Reflections on PTSD’s future in DSM–V. The British Journal of Psychiatry, 197, 343–344.
Satorra, A., & Bentler, P. M. (2010). Ensuring positiveness of the scaled difference chi-square test statistic. Psychometrika, 75, 243–248.
Schell, T. L., Marshall, G. N., & Jaycox, L. H. (2004). All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology, 113, 189–197.
Simms, L. J., Watson, D., & Doebbelling, B. N. (2002). Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf war. Journal of Abnormal Psychology, 111, 637–647.
Spitzer, R. L., First, M. B., & Wakefield, J. C. (2007). Saving PTSD from itself in DSM-V. Journal of Anxiety Disorders, 21, 233–241.
Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics (6th ed.). Boston: Pearson.
Wang, L., Li, Z., Shi, Z., Zhang, J., Zhang, K., Liu, Z., & Elhai, J. D. (2011a). Testing the dimensionality of posttraumatic stress responses in young Chinese adult earthquake survivors: Further evidence for 'dysphoric arousal' as a unique PTSD construct. Depression and Anxiety, 28, 1097–1104.
Wang, L., Long, D., Li, Z., & Armour, C. (2011b). Posttraumatic stress disorder symptom structure in Chinese adolescents exposed to a deadly earthquake. Journal of Abnormal Child Psychology, 39, 749–758.
Watson, D. (2005). Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114, 522.
Watson, D. (2009). Differentiating the mood and anxiety disorders: A quadripartite model. Annual Review of Clinical Psychology, 5, 221–247.
Watson, D., & Clark, L. A. (1991). The mood and anxiety symptom questionnaire. University of Iowa, Department of Psychology, Iowa City: Unpublished manuscript.
Watson, D., Clark, L. A., Weber, K., Assenheimer, J. S., Strauss, M. E., & McCormick, R. A. (1995a). Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology, 104, 15–25.
Watson, D., Weber, K., Assenheimer, J. S., Clark, L. A., Strauss, M. E., & McCormick, R. A. (1995b). Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology, 104, 3–14.
Weathers, F. W., Keane, T. R., & Davidson, J. R. T. (2001). Clinician administered PTSD scale: A review of the first ten years of research. Depression and Anxiety, 13, 132–156.
Witteveen, A. B., Van der Ploeg, E., Bramsen, I., Huizink, A. C., Slottje, P., Smid, T., & Van der Ploeg, H. M. (2006). Dimensionality of the posttraumatic stress response among police officers and fire fighters: An evaluation of two self-report scales. Psychiatry Research, 141, 213–228.
Yufik, T., & Simms, L. J. (2010). A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. Journal of Abnormal Psychology, 119, 764–776.
Funding
This work was supported by funds provided through the University of Memphis Lillian and Morrie Moss Chair of Excellence, held by Dr. Beck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
Joshua Clapp, Joshua Kemp, Matthew Woodward, and J. Gayle Beck declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 21.4 kb)
Rights and permissions
About this article
Cite this article
Clapp, J.D., Kemp, J.J., Woodward, M.J. et al. Distress Variance and Specificity of Symptom Dimensions in Posttraumatic Stress Disorder: a Quadripartite Perspective. J Psychopathol Behav Assess 42, 328–339 (2020). https://doi.org/10.1007/s10862-019-09772-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-019-09772-9