Abstract
In this study we applied a smart biomaterial formed from a self-assembling, multi-functional synthetic peptide amphiphile (PA) to coat substrates with various surface chemistries. The combination of PA coating and alignment-inducing functionalised substrates provided a template to instruct human corneal stromal fibroblasts to adhere, become aligned and then bio-fabricate a highly-ordered, multi-layered, three-dimensional tissue by depositing an aligned, native-like extracellular matrix. The newly-formed corneal tissue equivalent was subsequently able to eliminate the adhesive properties of the template and govern its own complete release via the action of endogenous proteases. Tissues recovered through this method were structurally stable, easily handled, and carrier-free. Furthermore, topographical and mechanical analysis by atomic force microscopy showed that tissue equivalents formed on the alignment-inducing PA template had highly-ordered, compact collagen deposition, with a two-fold higher elastic modulus compared to the less compact tissues produced on the non-alignment template, the PA-coated glass. We suggest that this technology represents a new paradigm in tissue engineering and regenerative medicine, whereby all processes for the bio-fabrication and subsequent self-release of natural, bio-prosthetic human tissues depend solely on simple template-tissue feedback interactions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
In recent years there has been an increasing change of focus within the fields of tissue engineering and regenerative medicine towards the development of new bottom-up strategies for the bio-fabrication of complex tissues (i.e., using cells to synthesise native-like tissues and organs in vitro). These strategies benefit from the increased understanding of the biochemical and biomechanical conditions required to induce differentiation, maintain viability and direct the function of cells in vivo. Furthermore, there have been considerable efforts to apply these principles to the development of new biomaterials that reproduce said conditions [1].
Some of the most innovative applications are based on hydrogel biomaterials capable of promoting cell adhesion, proliferation, and/or differentiation, and subsequently induce cell detachment by changing their characteristics in response to external physical (temperature, magnetic field), chemical (ionic strength, pH), or biological (anabolic or catabolic) stimuli (reviewed in [2–4]). For example, thermo-responsive polymers with different chemistries have been successfully used to create contiguous intact constructs using numerous cell types, including corneal [5], skin [6], oral [7], and nasal epithelial cells [8], cardiomyocytes [9], muscle myoblasts [10], and mesenchymal stem cells [11]. This is evidently an attractive bottom-up strategy, as it not only provides cells with a template to produce native-like tissues but also ensures that, by the end of the bio-fabrication process, the tissue is dissociated from the template. This approach avoids having the final bio-product associated with artificial or exogenous biomaterials, scaffolds, or carriers. However, these techniques have been used mainly to create cell sheets [12], with limited control on the three-dimensional structure and hierarchical organization of the tissue [13].
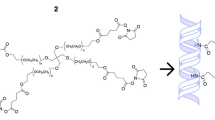
In this study we explored the potential of peptide amphiphile (PA) molecules as templates to bio-fabricate scaffold-free corneal stromal tissues with native-type structure and composition, and to subsequently release such tissues under fully-defined physiological conditions. PA molecules have been used for their ability to self-assemble in aqueous media at physiological pH into highly-structured nanostructures presenting specific peptide motifs that interact with cells and regulate cell phenotype and extracellular matrix (ECM) production [14, 15]. More recently, we developed a novel fully-synthetic, multi-functional PA comprising a mix of two different self-assembling molecules, a bio-functional one that contained an MMP1 cleavage site contiguous to the RGDS cell adhesion motif (MMP/RGDS) and a second molecule used as diluent (ETTES) [16]. This binary system PA was tested as a coating template to create corneal tissue with native-like structure and organisation, using human corneal stromal fibroblasts (hCSFs) as sole source for bio-synthesis [17]. The potential application of PAs in corneal tissue engineering has recently been reviewed [18].
Here, we further evaluate the different properties of the PA-directed bio-fabricated tissues containing an ECM comprised of either highly-oriented or randomly-deposited collagen fibres. This distinction in isotropy is important, as it is well known that the highly aligned spatial arrangement of the corneal stromal collagen is fundamental to the structural and functional role of the organ [19]. In order to achieve control of the orientation of deposited ECM, the binary MMP/RGDS:ETTES PA mixture was used to coat micro-rubbed PTFE on glass, an anisotropic substrate that induces the alignment of cells and ECM [20], or on borosilicate glass coverslips, previously shown suitable for the isotropic attachment of hCSFs in serum-free medium (SFM) [21]. The combination of PA coatings and different substrates thus allowed the production and subsequent self-release of corneal stromal tissue equivalents with distinct structural and mechanical properties (i.e., collagen fibre orientation, topography, stiffness). As such, these smart PA templates provide a promising platform for improved control of the bio-fabrication process by influencing the structural and mechanical properties of the engineered tissues.
2 Materials and methods
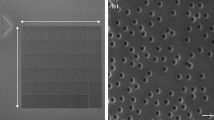
2.1 Preparation of peptide amphiphile (PA) coatings
Peptide amphiphiles (PAs) were custom-synthesized by CS Bio (Menlo Park, USA) as >95 % pure trifluoroacetic acid salts, and their molecular weight was confirmed by electrospray-mass spectrometry. Briefly, the lyophilized C16-TPGPQG↓IAGQRGDS (MMP/RGDS; ↓ indicates cleavage site for MMP1) and C16-ETTES (ETTES) were weighed separately and then dissolved as a 15:85 mol:mol binary component solution in ultrapure water from a Barnstead Nanopure system to obtain a 1 × 10−2 M solution. PAs were solubilised by 15 min sonication treatment at 55 °C, and then maintained at 4 °C overnight to ensure extensive and homogeneous self-assembly. PA solutions were kept refrigerated until further use. Specifically, dry PA film coatings were produced by using 500 µL aliquots of PA solutions at 1.25 × 10−3 M in ultrapure water to drop-spot glass slides coated with oriented stripes of polytetrafluoroethylene (PTFE) prepared as previously described [22], or untreated borosilicate glass coverslips (Gerhard Menzel No. 0, Thermo-Scientific), and left to dry overnight at room temperature inside an aseptic Class II cell culture cabinet (Fig. 1a). Resulting films (~5 cm2) were washed three times with sterile phosphate buffer saline (PBS) just prior to cell seeding.
Scheme representing tissue bio-fabrication and controlled self-release using the multifunctional MMP/RGDS:ETTES binary PA as a smart template. The diagram depicts a the application of PA in solution on PTFE-covered glass (to induce cell alignment; left panels) or glass coverslips (right panels) to minimise unspecific cell adhesion; b the formation of stable PA film coatings; c the seeding and adhesion of human corneal stromal fibroblasts (hCSFs) to the biomaterial template; d the culture of these cells during 90 days in serum-free, retinoic acid (RA)-supplemented conditions to allow the continuous deposition of corneal stroma-specific ECM components while abrogating the expression of endogenous MMPs; and e the controlled self-release of bio-fabricated tissues (black arrows) subsequent to the removal of RA from the culture medium and consequent increased expression of cellular matrix metalloproteases (MMPs; red arrows), MMP-specific cleavage of PA molecules, and degradation of the adhesive template (Color figure online)
2.2 Isolation and culture of human corneal stromal fibroblasts
Corneal tissues were obtained as by-products of grafting procedures, and kindly provided by Mr. Martin Leyland, MD, FRCOphth, following informed consent. All experiments were approved by the Royal Berkshire NHS Foundation Trust (RBFT) R&D Office and in accordance with RBFT and MHRA ethical guidelines. hCSFs were isolated from epithelia-depleted corneal rings and cultured as previously described [20]. Briefly, human corneal rings including the limbus region were dissected into quarters and remaining scleral tissue removed. Corneal tissue was shredded using a scalpel, transferred to 1:1 Dulbecco’s modified Eagle medium:Ham’s F12 (DMEM/F12) supplemented with 2 g L−1 of collagenase type-I (Life Technologies, USA) and 5 % FBS (Biosera, France), and incubated under rotation for 5 h at 37 °C, followed by incubation with 0.25 % Trypsin–EDTA in DMEM/F12 for 10 min. Isolated hCSFs were plated onto standard polystyrene culture plates (Nunc, Thermo Scientific, USA), and maintained in culture medium (DMEM/F12 supplemented with 5 % FBS, 1 × 10−3 M ascorbic acid, and 1 % penicillin/streptomycin) at 37 °C and 5 % CO2. Medium was replaced every 2–3 days. Upon reaching 70–80 % confluence, cells were enzyme-dissociated using TrypLE (Life Technologies) and passaged, or transferred to serum-free culture medium supplemented with all-trans retinoic acid (RA) at 1 × 10−5 M (SFM + RA) 3 days prior to subsequent experiments in order to inactivate hCSFs and inhibit MMP expression [21].
2.3 Adhesion and proliferation of hCSFs on PA coating templates
Confluent hCSF monolayers maintained for 3 days in SFM + RA were washed twice and then triturated with sterile PBS for dissociation. Cells were seeded at a density of 2 × 10−4 hCSFs per cm2 of PA films coating PTFE-covered glass slides (alignment-inducing template) or borosilicate glass coverslips (non-aligned template) (Fig. 1c). The orientation of hCSFs grown on both templates was monitored using a Nikon Eclipse inverted microscope (Nikon, Japan) coupled with a Jenoptik CCD camera (Jenoptik AG, Germany). Cell proliferation was evaluated during tissue bio-fabrication (at day 3, 7, 30, 60, 90 of culture) and the 3 days immediately after tissue self-detachment (90 + 1, +2, and +3) using the AlamarBlue assay (Life Technologies) to quantify differences in the metabolic activity of viable cells between experimental groups. Briefly, cultures were incubated with resazurin reagent diluted 1:10 in SFM + RA for 4 h at 37 °C, with supernatants sampled (0.1 mL aliquots, in triplicate) for fluorescence emission at 590 nm, and then replaced with fresh SFM + RA. The process was repeated for each time point evaluated. Cell number was calculated by interpolation using a standard curve for the fluorescence values of 1, 5, 10, 20, 50, and 100 × 103 cells. All experiments were performed three times, independently (n = 3).
2.4 Bio-fabrication and controlled self-release of tissues
Corneal stromal tissue formed by hCSFs and corresponding ECM deposited during 90 days culture in SFM + RA (Fig. 1d) was released as previously described [17]. Briefly, the dense, multi-layered tissues attached to aligned or non-aligned biomaterial templates were washed thrice with sterile PBS and then maintained in serum-free culture medium without RA supplementation (SFM) for cells to resume MMP expression, and to allow specific cleavage of the cell-adhesive PA coating and tissue self-release (Fig. 1e). After 3 days, the free-floating self-released tissues were recovered and analysed, or fixed in 4 % paraformaldehyde in water for 20 min at room temperature, washed thrice in PBS, and then maintained in water for up to 18 months.
2.5 Nano-topography and mechanical properties of bio-fabricated tissues
Analysis of surface topography was performed for aligned and non-aligned bio-fabricated corneal tissues in the static force mode using a Nanosurf Easyscan 2-controlled atomic force microscope (AFM) equipped with commercial soft contact mode cantilevers (ContAI-G, BudgetSensors; resonant frequency 13 kHz, nominal spring constant 0.2 N/m). Briefly, the different tissue samples were mounted onto glass slides that were previously covered with a layer of plastic paraffin film (Parafilm M) to avoid having the very high rigidity of the glass influence the stiffness measurements, and minimise sample displacement and drift. Surface topography was analysed from three separate regions in each sample, with 512 × two-direction lines scanned at 10 µm s−1 at 10 nV, and with a P- and I-gain of 1. The mechanical properties of the tissue samples were evaluated by force-distance spectroscopy. The stiffness of the tissues was evaluated from 100 force-distance curves acquired at 2 µm s−1 from different positions across each sample, and using SPIP data analysis software (Image Metrology A/S, Denmark) for baseline and hysteresis correction, followed by elastic modulus calculation using the Sneddon model, applicable for soft biological materials [23]. Elastic modulus was represented in terms of frequency, in percentage of measured values, within 20 MPa bins. All experiments were performed three times, independently (n = 3).
2.6 Statistical analysis
Error bars represent the standard deviation (SD) of the mean, analysed a priori for homogeneity of variance. Replicates from each independent experiment were confirmed to follow a Gaussian distribution, and differences between groups were determined using one- or two-way analysis of variance (ANOVA) followed by Bonferroni’s multiple comparison post hoc test. Significance between groups was established for P < 0.05, 0.01, and 0.001, with a 95 % confidence interval, and a R2 value in the proliferation assay at days 30, 60, 90, and 90 + 1 of 0.86, 0.83, 0.88, and 0.84, respectively. The average ± SD frequency distribution of elastic modulus of both aligned and non-aligned tissue samples was tested for correlation, and fit to Gaussian curves using a non-linear least-squares regression model, which were then analysed for independence using the χ2 test.
3 Results
In this work, we combined a multi-functional PA with micro-rubbed PTFE or glass surfaces to create smart templates able to control cell attachment and orientation, promote the deposition of natural ECM, and ultimately capable of degrading by the action of endogenous MMPs to release highly-structured native-like tissues comprising aligned or random-oriented collagen, respectively. As such, the usefulness of bioactive PAs as templates for tissue bio-fabrication was explored by adding its application as a coating to other functionalised substrates (Fig. 1).
The different PA-substrate templates (using PTFE or glass) influenced cell attachment and growth. The hCSFs cultured on the PTFE alignment-inducing template (Fig. 2, blue bars) proliferated up to day 60 and then maintained cell numbers up to day 90 in SFM + RA conditions. Cells grown on PA-coated glass also proliferated, albeit at a slower rate (Fig. 2, orange bars). After 2 months in culture, cells grew as part of the newly-formed tissue, and surrounded by large amounts of deposited ECM. In addition, cells on the alignment-inducing PA template showed significantly higher proliferation between days 30 and 90 compared to those grown on PA-coated glass (Fig. 2). Upon incubation with SFM without RA, hCSFs comprising the bio-fabricated tissues showed a marked decrease in numbers, particularly on the second and third days after RA removal from media (Fig. 2, +2 and +3). Percentage-wise, a similar loss was observed in tissues grown on aligned and non-aligned templates, with a corresponding reduction in cell numbers between day 90 and +3 of 21 ± 6 and 16 ± 4 %, respectively.
Proliferation of hCSFs grown on multifunctional PA templates during tissue bio-fabrication. Cells grown on PA-coated PTFE (aligned; blue bars) or glass coverslips (non-aligned; orange bars) were quantified while cultured in serum-free, RA-supplemented medium, from day 3 up to day 90, and during the subsequent 3 days when maintained in SFM without RA (+1, +2, and +3). Bars represent average ± SD; *, **, and *** correspond to P < 0.05, 0.01, and 0.001, respectively; n = 3 independent experiments (Color figure online)
After 3 days of RA deprivation, hCSFs comprising the newly-formed bio-fabricated tissues resumed MMP expression and elicited the cleavage and degradation of the adhesive PA template (Fig. 1e). Free-floating tissues, formed either on aligned or non-aligned templates, were visually transparent and maintained their structural integrity after lift-off (Fig. 3). These tissue equivalents were easily manipulated, transferrable, and able to retain their original shape and size even after extensive handling (Fig. 3a, b). Moreover, this structural stability was evident even in paraformaldehyde-fixed tissues maintained in water for 18 months (Fig. 3, right panels). However, tissues bio-fabricated on alignment-inducing templates were seen to be more robust and less friable than those produced on PA-coated glass.
Stability of self-released corneal bio-fabricated tissue. Photographs of free-floating corneal stromal tissue equivalents immediately after detachment from the smart PA template (left) and after 18 months in water (right panels) showed that bio-fabricates were able to maintain structural integrity over long periods of time. Tissues were highly transparent (a), easily recovered (b), and able to retain size and shape after manipulation (c). Although showing no evident differences in total thickness, tissue produced on the aligned template was found to be more robust and less friable during handling. Scale bars from right and left panels = 1 and 0.5 cm, respectively
In order to understand the ultrastructural basis for their different mechanical properties, tissues were imaged by atomic force microscopy immediately after self-release from either template. The analysis of surface topography showed that tissues produced on the alignment-inducing PA template consisted of a dense collagenous matrix, with highly-ordered collagen fibres deposited in compact bundles, and predominantly aligned throughout the tissue surface parallel to the axis of the micro-rubbed lines of PTFE used as the underlying substrate during tissue bio-fabrication (Fig. 4, left panel). Tissues formed on PA-coated glass, albeit presenting also a very dense collagenous matrix, had collagen fibres deposited more or less randomly, with occasional alignment only in restricted regions of the tissue surface (Fig. 4, right panel). In addition, the surface of aligned and non-aligned tissues also showed substantial differences in terms of roughness (Fig. 5). Specifically, false colour images demonstrated that aligned tissues had a much more uniform compact surface, with no distinctive topographical features (Fig. 5, upper panel). In contrast, non-aligned tissues showed a less compact, looser deposition of the randomly-oriented collagen fibres, and a rougher topography (as indicated by the wider colour range; Fig. 5, lower panel).
Alignment of collagens matrix of corneal stromal tissue equivalents. False colour images of forward deflection scans performed by atomic force microscopy (AFM) of self-released corneal bio-fabricates produced on PA-coated PTFE (aligned, left panel) or non-aligned biomaterial templates (right panel). The surface of tissues produced on the aligned template showed compact deposition of collagen fibres, predominantly oriented along the axis of PTFE indentations (arrowheads). In contrast, collagen fibres of corneal tissues produced on the non-aligned template were oriented more or less randomly. False colour scale, 500 nm. Scale bars, 500 nm
Topography of corneal stromal tissue equivalents. Three-dimensional map of surface topography produced by forward deflection AFM scans of corneal tissue bio-fabricated on PA-coated PTFE (aligned, upper panel) or non-aligned biomaterial templates (lower panel). Collagen fibres from tissue produced on the aligned template showed predominant orientation parallel to the axis of PTFE indentations (arrowheads), in contrast with the more random orientation of collagen from non-aligned tissue. False colour scale, 500 nm. Scale bars of x, y, and z axis = 1, 1, and 5 µm, respectively
Furthermore, the stiffness of both aligned and non-aligned tissues was evaluated by force-distance spectroscopy (Fig. 6). The analysis of frequency after repeated measurements showed a statistically significant difference (P = 0.003) in the distribution of the values for elastic modulus, with aligned tissues presenting an increased percentage of high-modulus measurements in a wide range of values (Fig. 6, blue bars), while non-aligned tissues had lower-elastic modulus values distributed through a shorter stiffness range (Fig. 6, orange bars). Moreover, non-linear regression analysis allowed the frequency histograms from aligned and non-aligned tissues to be well fitted (R2 = 0.74 and 0.81, respectively) to statistically independent Gaussian curves (χ2 test; P = 0.0001), and with corresponding elastic modulus of 69 ± 43 and 29 ± 24 MPa. Taken together, these results show that that multifunctional PAs can stably coat hydrophobic materials such as PTFE and borosilicate glass, and thus can be applicable to a wide array of tissue culture substrates. Moreover, the alignment-inducing PA template is capable of enhancing not only the adhesion and proliferation of hCSFs, but also the mechanical properties of tissues bio-fabricated de novo by these cells.
Mechanical properties of corneal stromal equivalents. The elastic modulus of tissue equivalents produced on PA-coated PTFE (aligned; blue bars) or glass coverslips (non-aligned; orange bars) was quantified by force-distance spectroscopy immediately after tissue detachment from the smart PA templates, calculated using the Sneddon model, and represented as percentage frequency of measured values. The frequency histograms of aligned and non-aligned tissues were used to calculate Gaussian curves by non-linear regression, with a fitness of 0.74 and 0.81, and an elastic modulus of 69 ± 43 (area in blue) and 29 ± 24 MPa (area in orange), respectively. Data is expressed as average ± SD of three independent experiments (n = 3) (Color figure online)
4 Discussion
The potential of the multifunctional MMP/RGDS:ETTES-PA to act as a template capable of inducing the formation of self-releasing tissues under physiological conditions was previously tested on low-attachment culture plates [17]. However, the present study now shows that the same PA can be applied to other functionalised substrates to further enhance the hierarchical organization of bio-fabricated tissues, or even to untreated borosilicate glass and still ensure complete tissue self-release.
By combining PA coatings with the cell alignment-inducing PTFE-rubbed surface we were able to produce a corneal stromal tissue equivalent that closely resembles its native counterpart [24, 25]. In particular, cells grown on PA-coated PTFE were directed to adhere, align, and proliferate along the axis of PTFE lines. This allowed the uniform orientation of hCSFs throughout the entire surface of the template, and consequently the formation of a more compact cell monolayer, with significantly higher number of cells compared to the template with randomly-oriented, but still highly-viable cells [17]. In addition, the aligned cells were constrained to deposit their ECM components, namely collagen fibres, along the same orientation axis. These results are in line with previous observations, where a single-function PA coating PTFE was able to enhance proliferation and stratification of hCSFs while still allowing cells to align and deposit highly-oriented collagen fibres [20].
Although not impairing the controlled self-release, the increased organisation of cells and ECM from the alignment-inducing template had an obvious effect on the overall robustness of the tissue. Aligned tissues were maintained intact even after extensive manipulation, very difficult to cut, and easily folded and unfolded. In contrast, and despite their stability and capacity to maintain the original shape and size even during long periods of storage in water and at room temperature, non-aligned tissues were, from the start, observed to be more difficult to handle (less robust) and easily friable.
The different structural properties at the macroscopic level were derived from the ultrastructural properties of the resolved tissues. The alignment of cells also resulted in the bio-fabrication of tissues with a more compact ECM, as observed by scanning surface topography using AFM. In addition, the aligned tissue presented a higher elastic modulus compared to non-aligned samples, previously shown to have collagen fibres densely deposited in lamellae-like layers 2.6 ± 1.6 µm thick [17]. The twofold increase of the average elastic modulus recorded for aligned over non-aligned corneal tissue was probably the result of higher collagen fibre alignment and compaction, density, or cross-linking. Recent studies have demonstrated that the stiffness of fibrillar materials is substantially increased due to anisotropy [26, 27]. In addition, similar differences were observed between plastic-compressed collagen gels subjected to different loads [28]. Overall, the values of 5–100 MPa recorded for our corneal stromal tissue equivalents were in line with other collagen-rich natural tissues such as cartilage (elastic modulus of 0.02–27 MPa; [29, 30]), skin (0.05–10 MPa; [31, 32]), and corneal stroma (1–3 MPa; [33]), but lower than those reported for isolated collagen fibrils (300–2000 MPa; [34]). The considerable range of values reported in the literature is due to the different measurement conditions and cantilever geometries and sizes used, as well as to the models applied for the calculation of the elastic modulus. In this context, a direct comparison between absolute values of elastic modulus would require the use of the same experimental setup.
In conclusion, the present results revealed that different PA-coated multifunctional templates are capable of instructing cells to fabricate tissues with different organisations and mechanical properties. Moreover, these bio-fabricated tissues were also formed by specific proteoglycans such as the keratocan, lumican, and decorin [20], ECM components with important structural and functional roles in the corneal stroma [19]. In the future, it will be interesting to perform further studies to characterise the proteoglycan composition and distribution in both aligned and non-aligned corneal tissues, and the influence of these molecules in the mechanical properties of bio-fabricated tissue equivalents.
References
Rice JJ, Martino MM, De Laporte L, Tortelli F, Briquez PS, Hubbell JA. Engineering the regenerative microenvironment with biomaterials. Advanced Healthc Mater. 2013;2:57–71.
Jones RR, Hamley IW, Connon CJ. Chapter 4 the instructive role of biomaterials in cell-based therapy and tissue engineering. Hydrogels in cell-based therapies. Cambridge: The Royal Society of Chemistry; 2014. p. 73–94.
Liu JS, Gartner ZJ. Directing the assembly of spatially organized multicomponent tissues from the bottom up. Trends Cell Biol. 2012;22:683–91.
Samchenko Y, Ulberg Z, Korotych O. Multipurpose smart hydrogel systems. Adv Colloid Interface Sci. 2011;168:247–62.
Hayashida Y, Nishida K, Yamato M, Yang J, Sugiyama H, Watanabe K, et al. Transplantation of tissue-engineered epithelial cell sheets after excimer laser photoablation reduces postoperative corneal haze. Invest Ophthalmol Vis Sci. 2006;47:552–7.
Dworak A, Utrata-Wesolek A, Oleszko N, Walach W, Trzebicka B, Aniol J, et al. Poly(2-substituted-2-oxazoline) surfaces for dermal fibroblasts adhesion and detachment. J Mater Sci Mater Med. 2014;25:1149–63.
Takagi R, Murakami D, Kondo M, Ohki T, Sasaki R, Mizutani M, et al. Fabrication of human oral mucosal epithelial cell sheets for treatment of esophageal ulceration by endoscopic submucosal dissection. Gastrointest Endosc. 2010;72:1253–9.
Hama T, Yamamoto K, Yaguchi Y, Murakami D, Sasaki H, Yamato M, et al. Autologous human nasal epithelial cell sheet using temperature-responsive culture insert for transplantation after middle ear surgery. J Tissue Eng Regen Med. 2015. doi:10.1002/term.2012.
Sakaguchi K, Shimizu T, Okano T. Construction of three-dimensional vascularized cardiac tissue with cell sheet engineering. J Control Release. 2015;205:83–8.
Aranaz I, Martinez-Campos E, Nash ME, Tardajos MG, Reinecke H, Elvira C, et al. Pseudo-double network hydrogels with unique properties as supports for cell manipulation. J Mater Chem B. 2014;2:3839–48.
Hruschka V, Saeed A, Slezak P, Cheikh Al Ghanami R, Feichtinger GA, Alexander C, et al. Evaluation of a thermoresponsive polycaprolactone scaffold for in vitro three-dimensional stem cell differentiation. Tissue Eng Part A. 2015;21:310–9.
Sekiya S, Shimizu T, Okano T. Vascularization in 3D tissue using cell sheet technology. Regen Med. 2013;8:371–7.
Matsuura K, Utoh R, Nagase K, Okano T. Cell sheet approach for tissue engineering and regenerative medicine. J Control Release. 2014;190:228–39.
Boekhoven J, Stupp SI. 25th Anniversary article: supramolecular materials for regenerative medicine. Adv Mater. 2014;26:1642–59.
Hamley IW. Lipopeptides: from self-assembly to bioactivity. Chem Commun. 2015;51:8574–83.
Dehsorkhi A, Gouveia RM, Smith AM, Hamley IW, Castelletto V, Connon CJ, et al. Self-assembly of a dual functional bioactive peptide amphiphile incorporating both matrix metalloprotease substrate and cell adhesion motifs. Soft Matter. 2015;11:3115–24.
Gouveia RM, Castelletto V, Hamley IW, Connon CJ. New self-assembling multifunctional templates for the biofabrication and controlled self-release of cultured tissue. Tissue Eng Part A. 2015;21:1772–84.
Miotto M, Gouveia RM, Connon CJ. Peptide amphiphiles in corneal tissue engineering. J Funct Biomater. 2015;6:687–707.
Lewis PN, Pinali C, Young RD, Meek KM, Quantock AJ, Knupp C. Structural interactions between collagen and proteoglycans are elucidated by three-dimensional electron tomography of bovine cornea. Structure. 2010;18:239–45.
Gouveia RM, Castelletto V, Alcock SG, Hamley IW, Connon CJ. Bioactive films produced from self-assembling peptide amphiphiles as versatile substrates for tuning cell adhesion and tissue architecture in serum-free conditions. J Mater Chem B. 2013;1:6157–69.
Gouveia RM, Connon CJ. The effects of retinoic acid on human corneal stromal keratocytes cultured in vitro under serum-free conditions. Invest Ophthalmol Vis Sci. 2013;54:7483–91.
Wittmann JC, Smith P. Highly oriented thin-films of poly(tetrafluoroethylene) as a substrate for oriented growth of materials. Nature. 1991;352:414–7.
Lin DC, Horkay F. Nanomechanics of polymer gels and biological tissues: a critical review of analytical approaches in the Hertzian regime and beyond. Soft Matter. 2008;4:669–82.
Holmes DF, Gilpin CJ, Baldock C, Ziese U, Koster AJ, Kadler KE. Corneal collagen fibril structure in three dimensions: structural insights into fibril assembly, mechanical properties, and tissue organization. Proc Natl Acad Sci USA. 2001;98:7307–12.
Komai Y, Ushiki T. The three-dimensional organization of collagen fibrils in the human cornea and sclera. Invest Ophthalmol Vis Sci. 1991;32:2244–58.
Chen B, Jones RR, Mi SL, Foster J, Alcock SG, Hamley IW, et al. The mechanical properties of amniotic membrane influence its effect as a biomaterial for ocular surface repair. Soft Matter. 2012;8:8379–87.
Hamley IW, Castelletto V, Moulton CM, Rodriguez-Perez J, Squires AM, Eralp T, et al. Alignment of a model amyloid peptide fragment in bulk and at a solid surface. J Phys Chem B. 2010;114:8244–54.
Foster JW, Jones RR, Bippes CA, Gouveia RM, Connon CJ. Differential nuclear expression of Yap in basal epithelial cells across the cornea and substrates of differing stiffness. Exp Eye Res. 2014;127:37–41.
Loparic M, Wirz D, Daniels AU, Raiteri R, Vanlandingham MR, Guex G, et al. Micro- and nanomechanical analysis of articular cartilage by indentation-type atomic force microscopy: validation with a gel-microfiber composite. Biophys J. 2010;98:2731–40.
Stolz M, Raiteri R, Daniels AU, VanLandingham MR, Baschong W, Aebi U. Dynamic elastic modulus of porcine articular cartilage determined at two different levels of tissue organization by indentation-type atomic force microscopy. Biophys J. 2004;86:3269–83.
Achterberg VF, Buscemi L, Diekmann H, Smith-Clerc J, Schwengler H, Meister JJ, et al. The nano-scale mechanical properties of the extracellular matrix regulate dermal fibroblast function. J Invest Dermatol. 2014;134:1862–72.
Crichton ML, Donose BC, Chen X, Raphael AP, Huang H, Kendall MA. The viscoelastic, hyperelastic and scale dependent behaviour of freshly excised individual skin layers. Biomaterials. 2011;32:4670–81.
Lombardo M, Lombardo G, Carbone G, De Santo MP, Barberi R, Serrao S. Biomechanics of the anterior human corneal tissue investigated with atomic force microscopy. Invest Ophthalmol Vis Sci. 2012;53:1050–7.
Shen ZL, Kahn H, Ballarini R, Eppell SJ. Viscoelastic properties of isolated collagen fibrils. Biophys J. 2011;100:3008–15.
Acknowledgments
We thank Dr C. A. Bipes from Nanosurf AG, Switzerland for his expert technical support in atomic force microscopy. This work was funded by the Biotechnology and Biological Sciences Research Council (BBSRC Grant Reference BB/I008187/1).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gouveia, R.M., Hamley, I.W. & Connon, C.J. Bio-fabrication and physiological self-release of tissue equivalents using smart peptide amphiphile templates. J Mater Sci: Mater Med 26, 242 (2015). https://doi.org/10.1007/s10856-015-5581-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-015-5581-5