Abstract
To investigate in vitro cellular cytokine expression in relation to commercially pure titanium discs, comparing a native surface to a fluorinated oxide nanotube surface. Control samples pure titanium discs with a homogenous wave of the margins and grooves and an often smeared-out surface structure. Test samples pure titanium discs with a fluorinated titanium oxide chemistry and surface morphology with nanopore/tube geometry characterized by ordered structures of nanotubes with a diameter of ≈120 nm, a spacing of ≈30 nm, and a wall thickness of ≈10 nm. Cross-section view showed vertically aligned nanotubes with similar lengths of ≈700 nm. Peripheral blood mononuclear leucocytes were cultured for 1, 3, and 6 days according to standard procedures. BioPlex Pro™ assays were used for analysis and detection of cytokines. Selected inflammatory cytokines are reported. A pronounced difference in production of the inflammatogenic cytokines was observed. Leucocytes exposed to control coins produced significantly more TNF-α, IL-1ß, and IL-6 than the test nanotube coins. The effect on the TH2 cytokine IL-4 was less pronounced at day 6 compared to days 1 and 3, and slightly higher expressed on the control coins. The morphology and surface chemistry of the titanium surface have a profound impact on basic cytokine production in vitro. Within the limitations of the present study, it seems that the fluorinated oxide nanotube surface results in a lower inflammatory response compared to a rather flat surface that seems to favour inflammation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Healing around implants is a complex process which is affected by the biomaterial used, including the macro-, micro-, and nano-design of the device. Oral implants have a long success record, and there is rising demand to treat more complicated and less healthy bone tissue. Hence, there is extensive ongoing research on biomaterial-related factors. Current biomaterials research focuses on factors such as the implant surface roughness, its morphometric characteristics, and its chemical and physical properties [1].
The surgical trauma and the insertion of an implant into the bone bed means that the implant surface is immediately exposed to tissue fluids with all their complex components. The proteins that primarily cover the implant surface will interact with various cell types, and the cells themselves may react differently. Leucocytes will migrate from the blood stream into the tissue, and thus macrophages will be activated and become involved in the inflammatory response [2]. The presence of different cell types varies depending on the stage: immediately post-surgery, acute inflammation, or chronic inflammation. Several growth factors are involved in skeletal repair, specifically of importance is TGF-b, including BMPs, FGFs and IGFs, as well as the PDGFs [3]. There are numerous excellent papers related to fracture healing and molecules involved. For the readers interested, please refer to Marsell et al. [4] and Tsiridis et al. [5].
The biomaterial itself may influence the inflammatory reaction, and given the wide array of novel “beyond state-of-the-art” implant surfaces ranging from the micrometre to the nanometre level and involving complex structures (including chemistry), it is not easy to precisely understand the possibilities of enhanced osseointegration today. However, it might be the case that, depending on what tissue type should be treated, this knowledge of complex structures will enable a future production of on-demand tailor-made implants.
In a number of in vivo rabbit studies, we have investigated how different surface treatments of titanium implants affect osseointegration of the implants. We have seen that the surface oxide chemistry of titanium implants gives rise to an enhanced osseointegration compared to implants with native oxide surfaces [6]. Hence it is clear that osseointegration is governed by the surface morphometric parameters as well as the chemical treatment of the implants [7]. Although what happens in vitro does not necessarily also happen in vivo, the necessity of screening implant surfaces using in vitro methods including various cell types may be even more interesting for our basic understanding of complex implant morphology [8].
An ordinary processed titanium surface such as the old Brånemark implant (turned/machined) will have an oxide film of about 4–15 nm thickness. Modifications of the titanium oxide layer by, for example, oxidation processes including incorporation of trace elements in the oxide film, has rendered an enhanced osseointegration compared to implants with native oxide formation in several in vivo animal studies [6, 7]. Advanced surface technology refers to fabrication of nanostructured implant surfaces with, for example, nanopores both with and without additional incorporation of trace elements [9, 10].
Neacsu et al. reported that TiO2 nanotubes (NT) with 78 nm diameter significantly decreased inflammatory activity of macrophages with respect to cytokine and chemokine gene expression/protein secretion, induction of foreign body giant cells (FBGCs), and nitric oxide (NO) release [11]. Furthermore, Park et al. reported that the surface diameter of titanium oxide NT from 15 to 100 nm critically influenced cell adhesion, spreading, growth, and differentiation [9]. Ainslie et al. reported effects of inflammatory cytokines (IL-1a and b, IL-6, IL-10, IFN-a and g, TNF-a, IL-12, MIP-1 and b) and reactive oxygen species production on nanostructured surfaces, compared to flat surfaces of the same material [12].
Indeed, novel surface technology renders very complex implant morphologies. There is thus a need for in vitro screening tests of implant surface modifications, using adequate cells and specific assays. The results obtained from such studies will give information about inflammatory driven response that can be related to specific implant topography.
The aim of this study was to investigate if differences in surface structure and oxide chemistry of commercially pure titanium disc/coin shaped implants (i.e. a native oxide surface as control vs. a fluorinated nanotube oxide surface as test) would influence cytokine production of human mononuclear leucocytes in vitro. If so, we also aimed to ask whether it would be possible to draw any conclusions with regard to in vivo osseointegration.
2 Materials and methods
2.1 Commercially pure titanium samples
Disc-shaped titanium samples (ASTM grade 4, 10 × 2 mm) were prepared and ground with 800-grit SiC wet grinding paper during water-cooling. Half of the samples underwent further preparation by potentiostatic anodization in 1 M H3PO4 (ACS reagent, Sigma-Aldrich) + 0.4 wt% HF (48 % aqueous solution, Sigma-Aldrich), resulting in fluorinated titanium oxide nanotubes (NT) on the surfaces. The surface preparation technique is fully described elsewhere [10]. All samples were individually cleaned in 100 % ethanol, dried in an oven at 60 °C for 1 day, and then sterilized in an autoclave at 120 °C for 90 min.
The morphology of the samples was observed by scanning electron microscopy (LV-SEM, JSM-6380LV, JEOL) and a FE-SEM (Hitachi FE-SEM S4800). The surface chemistry was investigated with X-ray photoelectron spectroscopy (XPS). Surface roughness was measured using an optical profilometer (MicroXAM™, Phase Shift, Arizona). The roughness parameters measured were Sa (arithmetic average height deviation, um) and Sdr (the ratio of the increment of the interfacial area of a surface over the sampling area, %).
2.2 Cell culture
Buffy coats were obtained from ten healthy volunteer blood donors at the Sahlgrenska University Hospital in Gothenburg, Sweden. Peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll-Paque (Amersham Pharmacia Biotech AB, Uppsala, Sweden) density gradient centrifugation and resuspended in Dulbecco’s modified Eagle’s medium+GlutaMAX-1™ (Gibco) supplemented with 5 % heat inactivated human serum type AB (Sigma-Aldrich), penicillin (100 U/mL), and streptomycin (100 μg/mL) (Sigma-Aldrich). Cells were seeded at 2 × 106 cells per well in 24-well plates and cultured at 37 °C in a humidified atmosphere with 5 % CO2 in the presence or absence of control titanium discs or test NT discs. Supernatants were collected after 24 h, 3 days, and 6 days of incubation and kept at −80 °C until further use.
2.3 Cytokine analysis
For cytokine analysis of culture supernatants, the commercially available cytokine panels 21plex Group II and 27plex Group I (Bio-Plex Pro™ Human Cytokine Assay, Bio-Rad Laboratories, Hemel Hempstead, UK) were used in accordance with the manufacturer’s instructions, thus allowing multiple cytokines in one sample to be quantified simultaneously. In brief, supernatants were incubated with sets of colour-coded beads, each conjugated with antibodies directed against a specific cytokine. A biotinylated detection antibody was added and subsequently allowed to bind to streptavidin–phycoerythrin. To remove unbound protein, thorough washing series were performed between each step. Finally, the samples were analysed using a BioPlex 200 instrument equipped with BioManager analysis software (BioRad), measuring the cytokine concentrations by comparing the bead colour and mean fluorescence intensity from each set of beads against an automatically optimized and manually verified standard curve.
2.4 Qlucore
Qlucore Omics Explorer bioinformatics software (Qlucore, Lund, Sweden, http://www.qlucore.com/) was used to create a heatmap of expression of selected cytokines after cell exposure to control and test coins. The program is an interactive 3D application that produces 2D plots using principal component analysis. Direct, immediate visualization helps the user to find structures and patterns in the data set.
2.5 Statistics
All statistical analysis was performed using GraphPad Prism 6 software (GraphPad Software Inc., San Diego, CA, USA). The Wilcoxon matched-pairs signed-ranks test was used to compare paired data, and a P-value of <0.05 was considered to indicate statistical significance. In addition to the statistical graphs, illustrative figures of the cytokine profiles were prepared with the Prism 6.0e program but without statistical comparisons.
3 Results
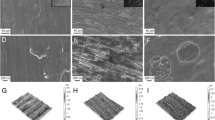
The scanning electron microscopy images (Fig. 1a, c) revealed dissimilar morphologies of the control and test sample surfaces. The control samples showed a homogenous wave of the margins and grooves and an often smeared-out surface structure, while the test surfaces demonstrated a structure of vertically aligned nanotubes. The nanopore geometry of the test coins was characterized by highly ordered structures of nanotubes with a diameter of ≈120 nm, a spacing of ≈30 nm, and a wall thickness of ≈10 nm. The cross-section view showed vertically aligned nanotubes with similar lengths of ≈700 nm in all samples.
Scanning electron microscopy images of the coin-surface structures used in this in vitro study: a pure titanium sample ground with 800 grit paper (control), b fluorinated titanium oxide with nanotube surface morphology with a diameter of ≈120 nm, a spacing of ≈30 nm, and a wall thickness of ≈10 nm (test surface), and c cross-section view showing vertically aligned nanotubes with similar lengths of ≈700 nm
The surface chemistry based on XPS showed similar peak intensities of the Ti 2p and O 1s spectra as appeared at the similar binding energy of 458.8 eV and 530.1 eV, respectively, for both control and test samples. However, the test samples showed fluorinated titanium oxide chemistry. A full description is given elsewhere [10]. The surface roughness parameters were 0.87 (±0.09) and 0.61 (±0.09) in Sa (um), and 46.1 (±9.7) and 16.0 (±0.7) in Sdr (%) for the control and test samples, respectively.
3.1 Cytokines
In order to compare the cytokine profile elicited by the two investigated Ti surfaces, PBMCs were cultured in the presence or absence of test or control coins for 1, 3, or 6 days after which cytokine concentrations in the supernatants were determined by multiplex cytokine array. A heatmap based on median values of selected cytokines from 8 to 10 blood donors was prepared, illustrating surface-dependent cytokine expression (Fig. 2). The cytokine kinetics were very similar between the two surfaces, with most cytokines showing more pronounced expression at early time points and declining with time. However, the expression of GROa, IL-8, MIG, MCP-1, IL-13, and TNFβ was highest after 6 days of incubation for the control coin compared to test coins, as well as in comparison to the other time points. With the exception of TNFβ, significant differences were observed between control and test coins after 6 days. The concentration of IL-6 seemed to be highest at 3 days for control coins, although the difference between test and control was larger at day 6.
Secretion profile of selected cytokines from PBMCs cultured in the presence or absence of control or test coin for 1, 3 or 6 days. The heat map plot represents median values of cytokine concentrations in supernatants from PBMCs purified from 8 to 10 blood donors and cultured with or without the different Ti surfaces at different time points. For each cytokine, values were normalised and transformed into colour codes representing higher (red), intermediate (black) or lower (green) concentration. Graphics were made using the Qlucore Omics Explorer bioinformatics software program. Cell control = PBMCs unexposed to coins, control coin = PBMCs cultured in the presence of ground titanium sample, test coin = PBMCs cultured in the presence of titanium with nanotube surface morphology
For VEGF, IL-12p70, G-CSF, and IL-1β, the concentration was highest after 3 days of culture together with the control coin. Notably, the IL-10 expression, which is related to anti-inflammatory cytokines, had a median value about 50 % higher for the control coins after 1 and 3 days, while after 6 days the test coins demonstrated a somewhat higher expression compared to control coins. Overall, a higher cytokine/chemokine response was generated by PBMCs cultured in the presence of control surface compared to the test samples, thus demonstrating the impact of Ti nanostructure as well as an altered surface chemistry on cytokine production.
To further analyse the difference in inflammatory response between the control and test coins, the expression of four typical pro-inflammatory cytokines (TNF-α, IL-1ß, IL-6, IL-8), and the typical TH2 cytokine (IL-4) was selected for statistical analysis (Fig. 3). There was a significant increase in expression observed for IL-4 after 1 day of incubation with the control coin compared to the test coin and the same was observed for IL-8, IL-6, TNF-a and IL-1b after 6 days of culture. The kinetics of the selected cytokines is further illustrated in Fig. 4.
Increased pro-inflammatory response from leukocytes exposed to the titanium control compared to the test coin surface. Cytokine concentration was measured in supernatants from PBMCs cultured in the absence (cell control) or presence of control coin or test coin. Note 1 day for a and 6 days for b–e. Each line denotes cytokine production from one blood donor. Significant differences were often obtained for the control coins compared to the test NT coins. The P-values indicated in the figure demonstrate a significant difference between control and test coins. a IL-4, b IL-8, c IL-6, d TNF-a, e IL-1b
Illustrations of median expression of selected cytokines in supernatants from PBMCs incubated for 1, 3 and 6 days with test coin, control coin or unexposed to coins. Clear square cell control, clear circle control coin, black dot test coin. No statistical comparisons were made. Note the scale difference in Cytokine expression (pg/mL, log 10). a IL-4, b IL-8, c IL-6, d TNF-a, e IL-1b, f IL-10, g VEGF
Due to their importance in relation to osseointegration, we chose to study the kinetics and expression of growth factors VEGF, FGF, and PDGF in more detail. Although not significant, the expression of VEGF tended to increase in supernatants from the control group compared to the test group after 1–3 days, while the opposite was the case after 6 days of incubation (Fig. 4g). No difference was seen in FGF or PDGF expression between surfaces (data not shown).
4 Discussion
Several studies have demonstrated that different materials evoke different cytokine secretion. However, to date, the majority of published literature related to material-induced cytokine expression investigates particles of various clinically-relevant materials [13–15], while few references can be found related to surface morphology [16–18]. Some in vitro studies have investigated nanostructured titanium, revealing that the nano-architecture reduces the inflammatory response [12]. Park et al. investigated titanium nanotube surfaces, and reported that a lateral surface geometry of approximately 15 nm “will be preferentially recognized by many more if not all cell types” [19]. We have also shown that a smaller spacing (below 30 nm) significantly stimulated osteoclasts compared to smooth TiO2 surfaces [9]. Park et al. demonstrated less osteoclast differentiation (7 days) on surfaces with 100 nm sized nanotubes, and observed the greatest osteoclast activity on 15 nm sized nanotubes; they also demonstrated similar findings using a TRAP assay [19]. These studies used different cell types, different analytical methods, and different surface morphologies of the tested samples, and so no direct comparison between studies can be made.
The aim of the present study was to investigate in vitro cellular cytokine expression in relation to commercially pure titanium discs, comparing a native oxide surface (control) to a fluorinated titanium oxide NT surface (test). In order to obtain an overview of the general cytokine profile evoked by each surface, we also studied selected cytokines in greater detail, choosing those which have previously been shown to be important for inflammatory response as well as osseointegration, and thus are likely to affect the outcome of implant surgery [20].
The results of our study demonstrate large differences in cytokine secretion by mononuclear leukocytes exposed to the control surface compared to the test NT surface structure (Fig. 2). Cytokine profile is thus clearly related to the surface morphology and chemistry of the Ti disc. We also showed an increase of pro-inflammatory cytokines IL-1β, TNF-α, and IL-6 in supernatants from the control group compared to the test group (Fig. 3). The elevated levels in the control group are in accordance with a previous investigation of titanium particles in an injection model in mice, which showed that cells were stimulated by particles and released these cytokines [14]. However, it is unclear why the inflammatory response to the test NT surface was less pronounced. In addition to its pro-inflammatory properties, IL-1β is also involved in osteoclast activation; these factors considered, high levels of IL-1β may not be favourable in a transplant/implant situation. The clinical importance of the abovementioned pro-inflammatory cytokines is that they are related to osteoclast activation and subsequent bone resorption [14]. The anti-inflammatory cytokines, on the other hand, may be related to bone remodelling due to inflammation.
The biological significance of an observed effect in vitro is of course a question that always arises when in vitro studies are conducted. It is only possible to speculate, but considering the complexity of the immune system even a very small change in the concentration of a cytokine may have biological significance in vivo. Inflammation is an adequate response of the immune system in a situation where the agent causing the inflammation is not endless and thus vanishes by time, for example a viral infection. In a situation where the inflammatory causing agent is permanently present, such as a titanium implant or the auto-antigen in an autoimmune disease, inflammation leads to tissue destruction. In patients with rheumatoid arthritis treatment with TNF blockade inhibits progressive joint damage very efficiently, thus illustrating the importance of this cytokine in the destruction of bone in joints [21]. All of the inflammatory promoting cytokines we have studied have more or less deleterious effects on bone and connective tissue [22].
For the angiogenic cytokine VEGF, the control coin surface demonstrated higher values at 1 and 3 days, whereas at 6 days the test NT coin surface demonstrated higher value compared to controls (Fig. 4g). The reason for this may be that a surface with a NT structure has the ability to attract/“fill” the nanotubes with proteins directly at injury. Such a surface morphology may be a good alternative to a smooth surface within tissue engineering and drug delivery tasks. This matter was also discussed by Ainslie et al., who used 79 nm wide nanotubes to conclude that the NT surface structure was minimally inflammatory [12]. Brammer et al. demonstrated an enhanced endothelization to TiO2 NT samples in vitro, using NT dimensions similar to those in the present study, and reported that the NT structured samples increased the functionality of the cells in comparison to a flat titanium surface: “the nanotubes also up-regulated the antithrombic cellular state for maintaining vascular tone”. The authors suggested that such a NT surface could be useful as a vascular stent [23].
A study by von Wilmowsky et al. investigated bone implant healing in a pig skull model, showing that implants with TiO2 nanotubes with a pore diameter of 30 nm enhanced the osteoblast function [24]. Other in vivo animal studies have shown an enhanced integration of implants with additional HF treatment, with the HF rendering nano-features of size approximately 100 nm on the surface. The latter enhanced the osseointegration significantly when tested biomechanically [25]. Chen et al. used polymer implants with various topographies for in vitro tests of 6–48 h to show a reduction of pro-inflammatory (TNF-a) and pro-wound healing (VEGF) cytokines, suggesting that inflammation-related process may be reduced using a certain topography [26].
It is thus clear that surface morphology and chemistry both play a role in cytokine expression irrespective of surface structure. In general, the test NT surface structure demonstrated reduced pro-inflammatory cytokine exposure compared to the smoother control surface. With increasing time of cellular exposure to test NT surfaces, the anti-inflammatory cytokine IL-10 was greater compared to the control surfaces (Figs. 3f, 4f). Similar observations were made when investigating the VEGF expression; the test NT surface demonstrated higher values with increasing time, and after 6 days the test NT surface demonstrated about 50 % greater expression compared to control surfaces (Fig. 4g).
The original osseointegration protocol related to oral implants involves unloading of inserted implants for periods of 3–6 months. It is likely that this regime could be shortened using tailor-made implants, leading to an enhanced quality of life for the patient. To enhance and eventually predict the bone-remodelling pattern around bone-anchored implants, both pro- and anti-inflammatory cytokines are of importance. For patients with poor bone beds, one could select implants with a NT surface structure that may result in a shorter healing time and an enhanced and faster integration in bone. Of course, this potential clinical benefit is still only speculation, as what happens in vitro does not necessarily happen in vivo. However, implant surfaces with NT morphology similar to that used in the present in vitro study have been tested in an in vivo rabbit model, resulting in statistically significantly greater integration of the implants over 6 weeks [10].
In a rat study with implants inserted in cortical bone for 1, 3 and 6 days, gene expression analyses were performed using qPCR technique [27]. Their control implants were of similar surface morphology as the coin shaped sample surfaces used in the present in vitro study. The data from the in vivo study by Omar et al. demonstrated a higher expression of the inflammation promoting cytokine TNF-a after 1 day on the machined control surface compared to the rougher titanium surface [27]. Furthermore, the inflammatory marker IL-1b demonstrated a higher expression after 1 and 6 days on the control surface [27]. In the present in vitro study, the control titanium surface resulted in a higher expression of TNF-a and IL-1b after 3 and 6 days compared to the test NT surface. However, direct extrapolations between in vitro and in vivo data cannot and should not be performed, yet it is interesting to note that a similar surface morphology renders results in a similar direction.
As pointed out by Mendoca et al., although it seems clear that nano-surface-structured modification of implants alters the in vitro and in vivo response, before this enters clinical practice both advantages and disadvantages must be evaluated in various long-term studies depending on the aim of the clinical device [28].
Our data so far demonstrate that the control smooth titanium surface renders an up-regulation of the pro-inflammatory cytokines, possibly indicating greater inflammatory response. Therefore our present in vitro results are of great interest. Our ongoing investigation of data from some 30 different cytokines expressed to these surfaces will possibly lead to in vivo studies including and involving various analytical methods.
5 Conclusion
The surface morphology and surface chemistry of the titanium samples have a profound impact on basic cytokine production in vitro. Within the limitations of the present study, it seems that the nanotube surface results in a lower inflammatory response compared to a rather flat surface that seems to favour inflammation. However, these in vitro results alone cannot be extrapolated to in vivo situations, and it should not be assumed that implants of fluorinated titanium oxide with a nano-structured surface morphology will result in a higher degree of osseointegration. Further in vitro tests with specific bone cells are ongoing, and the results may relate to our 6-week in vivo study in rabbit bone, which demonstrated an enhanced integration of screw-shaped implants with similar surface morphology and chemistry as used in this in vitro coin study.
References
Sul Y-T, Johansson CB, Petronis S, Krozer A, Jeong Y, Wennerberg A, Albrektsson T. Characteristics of the surface oxides on turned and electrochemically oxidized pure titanium implants up to dielectric breakdown: the oxide thickness, micropore configurations, surface roughness, crystal structure and chemical composition. Biomaterials. 2002;23:491–501.
Hunt JA, Abrams K, Williams DF. Modelling the pattern of cell distribution around implanted materials. Anal Chem Pathol. 1994;7:43–52.
Moucha CS, Einhorn TA. Enhancement of skeletal repair. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma. Philadelphia: WB Saunders; 2003. p. 639–59.
Marsell R, Einhorn TA. The biology of fracture healing. Injury. 2011;42(2011):551–5.
Tsiridis E, Upadhyay N, Giannoudis P. Molecular aspects of fracture healing: which are the important molecules? Injury. 2007;38:S11–25.
Sul YT, Johansson CB, Wennerberg A, Cho L-R, Jang B-S, Albrektsson T. Optimum surface properties of oxidized implants for reinforcement of osseointegration: surface chemistry, oxide thickness, porosity, roughness, and crystal structure. Int J Oral Maxillofacc Implant. 2005;20(3):349–59.
Sul YT, Kang BS, Johansson CB, Um HS, Park CJ, Albrektsson T. The roles of surface chemistry and topography in the strength and rate of osseointegration of titanium implants in bone. J Biomed Mater Res, Part A. 2009;89:942–50.
Rajyalakshmi A, Ercan B, Balasubramanian K, Webster T. Reduced adhesion of macrophages on anodized titanium with selected nanotube surface features. Int J Nanomed. 2011;6:1765–71.
Park J, Bauer S, von der Mark K, Schmuki P. Nanosize and vitality: TiO2 nanotube diameter directs cell fate. Nano Lett. 2007;7(6):1686–91.
Sul YT. Electrochemical growth behavior, surface properties, and enhanced in vivo bone response of TiO2 nanotubes on microstructured surfaces of blasted, screw-shaped titanium implants. Int J Nanomed. 2010;5:87–100.
Neacsu P, Mazare A, Cimpean A, Park J, Costache M, Schmuki P, Demetrescu I. Reduced inflammatory activity of RAW 264.7 macrophages on titania nanotube modified Ti surface. Int J Biochem Cell Biol C. 2014;55:187–95. doi:10.1016/j.biocel.2014.09.006.
Ainslie KM, Tao SL, Popat KC, Daniels H, Hardev V, Grinmes CA, Desai TA. In vitro inflammatory response of nanostructured titania, silicon oxid, and polycaprolaceton. J Biomed Mater Res, Part A. 2009;91:647–55. doi:10.1002/jbm.a.a32262.
Jacobsen SS, Larsen A, Stoltenberg M, Bruun JM, Soballe K. Effects of as-cast and wrought cobalt-chrome-molybdenum and titanium-aluminium-vanadium alloys on cytokine gene expression and protein secretion in J774A.1 macrophages. Eur Cells Mater. 2007;14:45–55.
StPierre CA, Chan M, Iwakura Y, Ayers DC, Kurt-Jaones EA, Finberg RW. Periprosthetic osteolysis: characterizing the innate immune response to titanium wear particles. J Orthop Res. 2010;28:1418–24.
Cachinho SCP, Pu F, Hunt JA. Cytokine secretion from human peripheral blood mononuclear cells cultured in vitro with metal particles. J Biomed Mater Res, Part A. 2013;101:1201–9.
Spyrou P, Papaioannou S, Hampson G, Brady K, Palmer EM, McDonald F. Cytokine release by osteoblast-like cells cultured on implant discs of varying alloy compositions. Clin Oral Implant Res. 2002;13:623–30.
Refai AK, Textor M, Brunette DM, Waterfield JD. Effect of titanium surface topography on macrophage activation and secretion of proinflammatroy cytokines and cehmokines. J Biomed Mater Res Part A. 2004;70:194–205. doi:10.1002/jbm.a.30075.
Schwartz-Filho HO, Morandini CF, Ramos-Junior ES, Jimbo R, Santos CF, Marcantonio E Jr, Wennerberg A, Marcantonio RAC. Titanium surfaces with nanotopography modulate cytokine production in cultured human gingival fibroblasts. J Biomed Mater Res, Part A. 2012;100:2629–36.
Park J, Bauer S, Schlegel KA, Neukam FW, von der Mark K, Schmuki P. TiO2 nanotube surface: 15 nm—an optimal length scale of surface topography for cell adhesion and differentiation. Small. 2009;5(6):666–71. doi:10.1002/small.200801476.
Chang PC, Lang NP, Giannobile WV. Review. Evaluation of functional dynamics during osseointegration and regeneration associated with oral implants Clin Oral Implant Res. 2010;21:1–12.
Ma X, Xu S. TNF inhibitor therapy for rheumatoid arthritis. Rev Biomed Rep. 2013;1(2):177–84. doi:10.4172/scientificreports.155.
Laveti D, Kumar M, Hemalatha R, Sistla R, Naidu VG, Talla V, Verma V, Kaur N, Nagpal R. Anti-inflammatory treatments for chronic diseases: a review. Inflamm Allergy Drug Targets. 2013;12(5):349–61.
Brammer KS, Oh S, Gallagher JO, Jin S. Enhanced cellular mobility guided by TiO2 nanotube surfaces. Nano Lett. 2008;8(3):786–93.
von Wilmowsky C, Bauer S, Lutz R, Meisel M, Neukam FW, Toyoshima T, Schmuki P, Nkenke E, Schlegel KA. In vivo evaluation of anodic TiO2 nanotubes: an experimental study in the pig. J Biomed Mater Res B. 2009;89(1):165–71. doi:10.1002/jbm.b.31201.
Johansson CB, Gretzer C, Jimbo R, Mattisson I, Ahlberg E. Enhanced implant integration with hierarchically structured implants: a pilot study in rabbits Clin. Oral Implant Res. 2012;23:943–53. doi:10.1111/j.1600-0501.2011.02233.x.
Chen S, Jones JA, Xu Y, Low H-Y, Anderson JM, Leong KW. Characterization of topographical effects on macrophage behavior in a foreign body response model. Biomaterials. 2010;31(13):3479–91. doi:10.1016/j.biomaterials.2010.01.074.
Omar O, Svensson S, Zoric N, Lennerås M, Suska F, Wigren S, Hall J, Nannmark U, Thomsen P. In vivo gene expression in response to anodically oxodozed versus machined titanium implants. J Biomed Mater Res A. 2010;92:1552–66.
Mendonca G, Mendonca DBS, Aragao FJL, Cooper LF. Advancing dental implant surface technology—from micron—to nanotopography. Biomaterials. 2008;29:3822–55.
Acknowledgments
We thank Wilhelm & Martina Lundgrens Science Fund and the TUA “Agreement concerning research and education of doctors”, 20140225TUAGBG-365041, Göteborg, Sweden for financial support.
Conflict of interest
No conflict of interests exists.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Östberg, AK., Dahlgren, U., Sul, YT. et al. Inflammatory cytokine release is affected by surface morphology and chemistry of titanium implants. J Mater Sci: Mater Med 26, 155 (2015). https://doi.org/10.1007/s10856-015-5486-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-015-5486-3