Abstract
Tamoxifen (TMX), a class II antiestrogen drug consistent with the biopharmaceutical classification system, shows low plasma levels leading to therapeutic failure as a result of poor aqueous solubility. Complexation with multifunctional excipients cyclodextrins (CDs) is an effective technique to increase the bioavailability of low water-soluble drugs in oral dosage forms. In this study, solid complexes were obtained with three cyclodextrins (methyl-beta-cyclodextrin (M-β-CD), hydroxypropyl-beta-cyclodextrin (HP-β-CD) and sulfobutyl ether β-cyclodextrin (SBE7-β-CD)) using co-lyophilization or kneading methods. Physicochemical characterization of solid complexes were performed by differential scanning calorimetry and Fourier transform infrared spectroscopy. The obtained results demonstrated that co-lyophilization method comprises stable inclusion complexes between TMX and cyclodextrins. Dissolution study exhibited that aqueous solubility of TMX was significantly enhanced by complexation with methyl-beta-CD. Consequently, tablet formulation using co-lyophilized complex of TMX and M-β-CD (1:1) with drug dose equivalent to 10 mg was prepared by direct compression method. 99% drug was released from the formulation at the end of 30 min. From the comparative results of dissolution study, it was found that the prepared formulation showed better release properties than commercial TMX tablets. Animal studies were performed with tablet formulation of TMX:M-β-CD and commercial tablet formulation administered to Sprague–Dawley rats by oral gavage. Peak concentration (Cmax) of tablet formulation containing TMX/M-β-CD inclusion complex in mice was efficaciously enhanced twofold over commercial tablet. In conclusion, complexation of TMX with M-β-CD gives a more effective tablet formulation with improved dissolution and enhanced oral bioavailability which can be promising for the formulation of tamoxifen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiestrogen tamoxifen is applied in clinics for first-line hormone treatment as well as adjuvant therapy in early/metastatic breast cancers in postmenopausal females. Also, this drug is approved to prevent breast cancer for high-risk women [1, 2]. The commercial tablet formulation of tamoxifen citrate has several limitations to its bioavailability such as precipitation in gastric environment after oral administration, first-pass metabolism, multidrug resistance (MDR) transporters efflux in potential organs (intestine and liver) that hinders systemic exposure and causes drug-induced hepatotoxicity and poor systemic bioavailability [3,4,5,6,7]. In addition, tamoxifen is considered the cause of significant adverse effects including endometrial carcinoma, vein thrombosis, pulmonary embolism and ocular effects that are related to be dose- and concentration-dependent [8]. Thus, there is need to develop a new formulation for TMX to diminish these important side effects and to improve bioavailability upon oral administration.
Tamoxifen is classified as class 2 compound, which has low solubility and favorable permeability characteristics in biopharmaceutics classification system (BCS) suggesting that it shows low oral bioavailability [9,10,11]. For class 2 drugs, drug dissolution is the rate-limiting step of drug absorption. Thus, when administered as oral dosage forms, the pharmaceutical formulation, in particular the use of excipients and innovative technologies, play an important role in drug absorption from gastrointestinal tract [12].
Potential bioavailability difficulties are common in hydrophobic drugs characterized with low water solubility or uncomplete absorption from gastrointestinal area [13]. In addition, TMX’s very poor water solubility lead to formulation problems and limits its therapeutic use [14]. Up to now, different formulation approaches like salt formation, particle size reduction, solid dispersions, prodrugs and complexation have applied to increase the drug solubility in the gastrointestinal area and their oral bioavailability [15,16,17]. Jena et al. developed TMX:phospholipid complex and found its positive effect on solubility and bioavailability of TMX due to increased hydrophilicity [11]. Dehghani et al. prepared a TMX loaded microemulsion system as an oral administered drug. The in vivo results showed that a new formulation could be a useful candidate in terms of a significant reduction in tumor growth [18]. In another study, hot melt extrusion (HME) technique were used to ensure co-delivery of tamoxifen and resveratrol that is effective for ER-positive breast cancer. Dissolution studies confirmed that HME extrudates were able to release drug more rapidly than drug suspension. Also, pharmacokinetic studies in rats demonstrated that extrusion significantly increased the tamoxifen oral bioavailability [19].
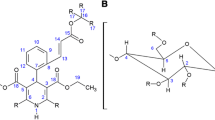
Among these techniques, a popular approach is the utilization of cyclodextrin-based formulations in which the drug enters the nonpolar cavity of CDs and the resulting complex of drug:CD enhances the solubility while retaining the original chemical composition thus maintaining stability [20]. Host–guest complexation studies take place in the literature to overcome drawbacks like low bioavailability. In a study, Shukla and colleagues prepared and characterized a water-soluble complex of TMX-2HP-beta-CD to increase TMX solubility. The results showed that TMX-2HP-β-CD complex penetrated the tissue because of the enhanced permeability and retention characteristic of tumor tissue resulting remarkable antitumor effect in the ovarian cancer cell line [21]. Shangguan et al. used pillar[6]arene to increase the solubility and stability of TMX by host–guest complexation. These drug complex showed increased water solubility and higher anticancer efficiency than free drug [22].
Cyclodextrins are cyclic crystalline, nonhygroscopic oligomers of glucose that are connected to each other by α-(1,4) glycosidic bonds. Alpha (α-CD), beta (β-CD) and gamma-cyclodextrins (γ-CD) are the pharmaceutically relevant natural CDs with number of α-d-glucopyranose units that are 6, 7 and 8, respectively [20, 23, 24]. Cyclodextrins has a torus shape with a hydrophilic surface and a relatively hydrophobic inner cavity. This lets inclusion complex formation between cyclodextrin as a host molecule and hydrophobic guest molecules. This property could give to widespread usage of cyclodextrins in pharmaceutical formulations in an effort to enhance solubility of low-water soluble drugs [1, 9]. Also, cyclodextrins have an ability to overcome drawbacks of anticancer drugs. The lack of treatment efficacy has created the need to develop new strategies based on combination of cyclodextrin complexation and nanotechnology in an attempt to achieve more efficient therapy [25]. In the literature, many anticancer drugs have been reported to complex with natural cyclodextrins and their derivatives to improve physicochemical characteristics like solubility, stability, dissolution and oral bioavailability. Complexation of oridonin with 2-HP-β-CD led to significant improvement in dissolution and permeability. As a result of this, nanosuspensions prepared from drug:CD complex significantly increased the oral bioavailability of anticancer drug oridonin [26]. Similarly, complexation of myricetin with HP-β-CD led to an approximately tenfold increase in oral bioavailability in comparison with free drug [27]. For tamoxifen, inclusion complexes were prepared with β-cyclodextrin and 2,3-di-O-hexanoyl-β-cyclodextrin resulting in high anticancer efficacy for free drug [28].
In the light of the present status of the literature in the field, the purpose of this study was to increase dissolution rate and oral bioavailability of the class II drug Tamoxifen through a tablet formulation based on cyclodextrin complexation. Different cyclodextrin types and preparation techniques were evaluated for the optimal tamoxifen formulation and in vivo bioavailability of the novel formulation was compared to commercial product in animal model pharmacokinetic study.
Materials and methods
Materials
Tamoxifen citrate (TMX, molecular weight (MW): 371.51 g/mol) was kind gifts from TEVA Pharmaceuticals (Plantex Netanya), Israel. Methyl-β-cyclodextrin (M-β-CD, MW: 1310 g/mol, solubility in water at 25 °C: 800 g/L) and hydroxypropyl-β-cyclodextrin (HP-β-CD, MW: 1541.547 g/mol, solubility in water at 25 °C: 2300 g/L) were supplied as Cavasol® W7 M and Cavasol® W7HP respectively, as kind gifts of Wacker Chemie, Germany. Sulfobutyl ether β-cyclodextrin (SBE7-β-CD, MW: 1134.987 g/mol, solubility in water at 25 °C: 700 g/L) was supplied as Captisol®, as kind gift of Cydex Inc. (Lenexa, KS). Octane-1-sulfonic acid sodium salt was purchased from Merck (Germany). Methanol (HPLC grade) was purchased from Sigma-Aldrich (Germany). Ultrapure water was obtained using Millipore Simplicity 185, France. Sodium starch glycolate, magnesium stearate and Avicel® pH 102 were obtained from Eczacıbaşı (Turkey). All other reagents were of reagent grade and were used without purification.
Methods
Preparation of TMX:CD inclusion complexes
Kneading method
Weighed accurately the specified quantity of TMX and CDs (totally 1 g) were mixed 1:1 molar ratio in a glass mortar for 5 min. Small amount of water was added drop by drop until the mixture became slurry and this slurry mixture was kneaded for 30 min. The paste was dried in an incubator at 40 °C for 48 h.
Physical mixtures (PM) of the drug and the cyclodextrins that were also characterized were prepared by homogeneous mixing of formerly weighed amounts of TMX and CD (1:1 molar ratio) in a mortar with a spatula for 15 min.
Co-lyophilization method
TMX and cyclodextrins were accurately weighed (1:1 molar ratio). Saturated solutions were prepared with cyclodextrins and water. Following, TMX was dissolved in ethanol and slowly put into CD aqueous solution. Then, suspension was stirred at 25 °C for 24 h in dark. Ethanol was evaporated with rotavapor (IK RV 10 basic, Germany) at 40 °C and obtained mass were freeze-dried for 24 h to get white fluffy powder (Heto PowerDry PL 3000, Denmark).
Physicochemical characterization of TMX-CD inclusion complexes
Inclusion complexes and physical mixtures of TMX with different CDs and different preparation techniques were evaluated using spectroscopic, thermal and microscopy techniques. These studies are described and carried out as follows:
FT-IR analysis
FT-IR spectra of free TMX, M-β-CD, HP-β-CD, SBE-β-CD, PMs and inclusion complexes were collected on the FT-IR spectrophotometer (Perkin-Elmer BX, USA). The spectral range was between 800 and 4000 cm−1.
Differential scanning calorimetry (DSC)
DSC curves of TMX, M-β-CD, HP-β-CD, SBE-β-CD, PMs and inclusion complexes were performed using a DuPont DSC 910 Instrument (DuPont, USA). Each sample (3–5 mg) was pierced in aluminum pans which were heated over temperature range of 20–270 °C with a rate of 10 °C/min, in a nitrogen atmosphere. To observe the possible crystalline conversion to amorphous form during lyophilization, free drug was also subject to the same procedures of the co-lyophilization technique without the presence of CDs.
Dissolution of TMX from inclusion complexes
The dissolution profiles of free TMX and TMX:CD complexes prepared by either kneading or co-lyophilization methods were determined. The dissolution behavior of tablets was determined using the USP 29 method [29]. Dissolution experiments were performed with 6 times on lyophilized samples with a Sotax dissolution apparatus (USA). This study was carried out using Apparatus 2 in 0.02 N HCl at 37 °C and stirring speed of 100 rpm. Aliquots from lyophilized samples, equivalent to 10 mg of TMX, were added to 1000 mL 0.02 N HCl. At appropriate time, aliquot was withdrawn and replaced with the same volume of fresh medium. All samples were filtered by 0.45 μm filter. Filtrate was assayed by an HP Agilent 1100 HPLC system with a DAD detector. The column was Kromasil® reversed phase C18 (250 × 4.6 mm), a mobile phase of methanol:water (678:322 v/v) including 1.08 g octane-1-sulfonic acid sodium salt and 2 mL glacial acetic acid, injection volume: 20 µL and flow rate: 1 mL/min.
Formulation of TMX:M-β-CD tablets
A tablet formulation was prepared using the optimized TMX/M-β-CD co-lyophilized complex to compare commercial tablet from the point of dissolution as well as in vivo behavior. Since in vitro characterizations of the complexes and dissolution studies indicated M-β-CD and co-lyophilization technique giving optimal results, TMX/M-β-CD co-lyophilization complex was further used in the tablet formulation. The tablets were prepared using direct compression of formulation constituents shown in Table 1. The tablets were compressed using single punch direct compression machine.
The respective powders (TMX:M-β-CD inclusion complex, Avicel pH 102, sodium starch glycolate and magnesium stearate) mixed with a mortar and a pestle. The admixture were weighed and fed manually into an instrumented single-punch tablet press.
Dissolution profile of TMX from tablets
Dissolution test for TMX/M-β-CD tablets and commercial conventional tablets were performed at twelve times, via a Sotax dissolution test apparatus (USA). The dissolution study was carried out using Apparatus 1 in 0.02 N HCl at 37 °C and stirring speed of 100 rpm according to USP 29. Tablets were added to 1 L 0.02 N HCl. At predetermined time, aliquot replaced with the same volume of fresh medium. All samples were filtered by 0.45 μm filter. Filtrate was assayed by analytically validated HPLC method. f1 value (difference factor) and f2 value (similarity factor) were calculated to compare dissolution profiles.
In vivo bioavailability studies
Animal and dosing
A total of 16 female Balb-c mice (35–40 g, 6–8 weeks age) were purchased from Hacettepe University, Laboratory Animals Research and Application Center (Ankara, Turkey). The animals were maintained in cages at 22 ± 3 °C, 55% relative humidity of under a 12-h dark/light cycle. Mice were allowed free access to water but were fasted for 12 h before drug administration. This experiment was carried out according to the Turkish Law for the Protection of Animals. The local ethics committee of animal experimentations (Hacettepe University) approved this study. (Approval number 2013/40-14) For each test group, eight mice were used to investigate tamoxifen pharmacokinetics.
Mice were anesthetized for approximately intraperitoneal dose of chloral hydrate (400 mg/kg body weight). Group 1 and 2 received a single oral gavage of commercial tablet and tablet formulation preparing with tamoxifen citrate:M-β-CD complex dissolved in water (equivalent to 10 mg/kg of tamoxifen base), respectively.
Blood sampling
Blood samples were withdrawn via catheter inserted into the jugular vein of mice at 1, 2, 4, 8, 24, 48 and 72 h after dosing. Then, blood samples were collected into heparinized tubes and placed on wet ice until centrifugation. After that plasma was separated with centrifugation at 5000 rpm for 15 min. 200 µL acetonitrile was added in 100 µL plasma, to precipitate proteins. The samples were vortexed at 30 s and centrifugated at 13,500 rpm for 15 min. The supernatant were separated and analysed for drug content by validated LC–MS/MS method. Pharmacokinetic parameters were estimated with non-compartmental analysis using PKSolver.
LC–MS/MS analysis of tamoxifen in mice plasma
The analysis of tamoxifen in mice plasma was performed using LC–MS/MS method from Gjerde et al. with slight modifications [30]. LC–MS/MS system consists of a Shimadzu 8530 triple quadrupole mass spectrometer with an electrospray ionization source (ESI), pump and autosampler system. Separations were carried out using a C18 column (2.1 × 50 mm, 3 µm) at 40 °C with a flow rate of 300 µL/min. An isocratic elution was performed with mixture of mobile phase A (0.1% formic acid in water) and B (0.1% formic acid in acetonitrile) (55:45, v/v). The injection volume was 10 μL and the total run time was 6 min. The ESI–MS/MS conditions were as follows: interface voltage, 4.5 kV; Q1 pre-rod bias voltage, − 14 V; Q3 pre-rod bias voltage, − 21 V; collision energy, − 35 eV; nebulizer gas flow rate, 3 mL/min; drying gas flow rate, 15 L/min; desolvation line temperature, 250 °C; heat block temperature, 400 °C. Quantification was performed using multiple reaction monitoring (MRM) mode with m/z 372.3 [M+H]+ → 72.1 (product ion) for tamoxifen with 200 ms of the Dwell time.
Statistical analysis
All the results are given as mean ± standard deviation (SD). Data was analyzed using Student’s t test or one-way ANOVA (SPSS Statistics, US); p-values < 0.005 was considered as statistically significant.
Results and discussion
In order to develop an enhanced tablet formulation of BCS Class II drug TMX, drug inclusion complexes with three different CD derivatives (M-β-CD, HP-β-CD, SBE-β-CD) were prepared by two preparation techniques. Complexation capabilities and enhancement of dissolution and bioavailability were comparatively evaluated to obtain optimal TMX:CD complex to be further formulated into tablets.
Preparation of inclusion complexes
The method of complexation may play a role in drug solubilization [31]. Among the methods used in order to prepare complexes with cyclodextrin, the most efficient one proved to be the kneading method, as it was carried out with relatively high complexation yields compared with the co-lyophilization method, where complexation yields were low. In addition to this, kneading method is the easier, faster and cost effective method of complexation [32]. On the other hand, each preparation method may not be suitable for every active ingredient. In fact, the yields of the processes were approximately 93% for kneading, and 70% for co-liyophilization method in our experiments. However, co-liyophilization method was chosen that give the best results in terms of characterization and dissolution studies. Yield was calculated using the equation:
where, a is the mass of the inclusion complex, b is the mass of TMX taken for inclusion complex preparation, and c is the mass of cyclodextrin taken for inclusion complex preparation.
Characterization of inclusion complexes
Differential scanning calorimetry (DSC) analysis
DSC analysis gave further information about the thermal properties of drug-cyclodextrin complexes. Tamoxifen citrate has a well defined characteristic endotherm at 140–144 °C, corresponding to the melting point temperature and this finding is compatible with literature [33]. Disappearance of TMX’s characteristic endothermic peak between at 142–146 °C shows the absence of free crystalline TMX. DSC thermograms of TMX, different CDs, physical mixtures and different TMX:CD complexes are given in Fig. 1.
As shown in Fig. 1, the endothermic peak of TMX completely disappeared in all formulations with co-lyophilization method for all three cyclodextrin derivatives which indicated that drug was incorporated into cyclodextrin cavity and later formed amorphous complex through co-lyophilization method. For kneading method, a small and wider DSC peak was observed that indicates the presence of free TMX crystals and incomplexation. This suggested that the complexes prepared with co-lyophilization are more stable than the complexes prepared by kneading method. Otherwise, the endothermic peak of TMX is seen in physical mixture. Hence, the presence of TMX peak in physical mixture could evidence that no true inclusion complex has formed in this system as can be expected. These results were accordance with FT-IR results which are represented in Fig. 2.
FT-IR analysis
Figure 2 shows a comparison of FTIR spectra of TMX, physical mixtures and complexes. Spectra of all inclusion complexes can’t exhibit new peaks suggesting that no chemical bonds were obtained in formed compounds. However, it can be observed that the intensity of both bands is decreased in all inclusion complexes. FTIR spectrum of TMX indicated sharp peaks at: 699 cm−1 related to tertiary amine aromatic peak, an intense peak at 1157 cm−1 due to alkyl-substituted ether, C–O stretching, 1660 cm−1 due to alkenyl C=C stretching, 2929 cm−1 due to C–H stretching.
In the case of inclusion complexes, a major change was seen in the fingerprint region 900–1400 cm−1 as an intensive peak due to O–H stretching special to the carbohydrates that is shifted to 3000 cm−1 in the complex, showing interaction of –OH groups of CDs with the secondary amide R–NH–C=O group of TMX.
Dissolution of TMX from inclusion complexes
To compare dissolution profiles of optimal CD complexes in powder form of TMX prepared with co-lyophilization method, 0.02 N HCl was used as dissolution medium because it is registered by USP 29 for TMX tablets dissolution. In the light of previous characterization data, complexes prepared with co-lyophilization method showed better complexing ability than kneading method. Therefore, co-lyophilized TMC:CD complexes were selected for dissolution studies. Dissolution profiles of free TMX powder and TMX:CD complexes in 0.02 N HCl were given in Fig. 3.
In 0.02 N HCl medium, the dissolution of free TMX was slower than the TMX in inclusion complexes and also incomplete even after 60 min. All inclusion complexes prepared with different cyclodextrins showed better dissolution properties than TMX powder (immediate and complete dissolution within 30 min). HP-B-CD and M-B-CD inclusion complexes actually demonstrated immediate release profiles with more than 90% dissolution in the first 15 min. There was an efficient and significant increase (p < 0.05) in the dissolution of tamoxifen from inclusion complexes. It was indicated that all complexes demonstrated a faster dissolution rate with respect to free TMX due to complexation. Cyclodextrins have played a critical role to formulate of low water-soluble drugs by decreasing the drug crystallinity and improving apparent solubility and dissolution [34].
Complexation enhanced TMX solubility with particle size reduction in molecular grade and provide optimal interaction between drug and gastrointestinal fluid leading quick dissolution. It can be clarified by higher aqueous solubility, wetting capability and complexation capability of CDs to solid drug. In addition, complex stability is the principal property influencing the dissolution rate due to free crystal TMX impact. Obtained results are in correlation with complex characterizations and free crystalline TMX in complexes.
The presence of methyl groups on cyclodextrin ring is a superiority for simple ionic drugs like tamoxifen [35]. Tamoxifen is cationic and basic drug. The methylated β-CDs significantly increased the solubility of these cationic compounds due to charge–charge repulsion [35]. In the literature, many studies can be found that methyl-β-CD enhance the dissolution properties of many poorly soluble drugs [36,37,38,39].
On the other hand, many studies have reported about the superiorities of ionic CDs such as SBE-β-CD in complexation of drugs with the opposite charge [40]. The SBE-β-CD-formulated, FDA-approved, commercial drugs (amiodarone, aripiprazole, maropitant, voriconazol etc.) are all cationic molecules. The electrostatic interaction between the positive charge of the guest and the negative charge of the sulfonate groups in the SBE-β-CD host increase the effect of host–guest complexation, for example, the solubilization. Cationic molecules like tamoxifen interact with negatively charged SBE-β-CD that exhibit a high binding capacity as their neutral counterpart, due to charge-charge attraction. Only, this lower than expected increase in the complexation yield could be observed due to changes in the location of drug molecule within cyclodextrin cavity. That is, when the cyclodextrin and drug molecules have opposite charges, the drug molecule has to arrange itself within the cavity to allow for the ionic interactions, but at the same time the forces between the drug molecule and the cyclodextrin molecule within the cavity will be reduced. For example, in some cases the hydrophobic moiety of a drug molecule, which under normal conditions would be located well inside the cavity, will partly be located outside the cavity to allow for ionic interactions between the drug and the cyclodextrin molecules [41].
When our findings are examined, enhanced dissolution was found to be consistent with ionic different cyclodextrins described above in the order of M-β-CD (cationic) > SBE-β-CD (anionic). Taking into account all of these results, presence of charge on the cyclodextrin structure provides an additional site of interaction compared to neutral cyclodextrins [40].
Dissolution profile of TMX from tablets
To compare the results and assess the influence of tablet formulation on TMX dissolution performance, dissolution tests were done under the same experimental conditions previously used. In fact, for the tablet formulation M-B-CD complexed with TMX was selected for further studies after the in vitro characterization data in especially dissolution from powder form. Dissolution profiles of TMX:M-β-CD tablets and commercial tablets were shown in Fig. 4.
Each data point defines a mean of twelve measurements for each product. The dissolution of TMX from commercial tablets was incomplete after 60 min in 0.02 N HCl. On the other hand, TMX:M-β-CD tablets show a 100% dissolution profile in 0.02 N HCl in 45 min, which may be significant property for industrial large-scale production. This situation proved low cost and the ordinary process that include less time and equipment. f1 and f2 values were calculated as 25.7 and 35.9 for 0.02 N HCl media, hence TMX:M-β-CD tablets and conventional Tamoxifen TEVA® dissolution were therefore demonstrated to be significantly different from each other (p < 0.05).
As can be seen, TMX:M-β-CD tablets showed significantly better drug dissolution performance than the commercial tablet formulation. Moreover, similar results were seen in dissolution rate for the corresponding inclusion complex powders (Fig. 3). In fact, TMX:M-β-CD tablets displayed analogous dissolution parameters, both allowing an increase of more than two times of drug dissolution efficiency at 60 min, in accordance with free TMX. These findings indicated that the superior performance of inclusion complex retained after its incorporation into tablet formulation. Based on these results, these new tablet formulation containing tamoxifen was chosen for oral bioavailability studies proposed to evaluate its therapeutic efficacy in comparison with commercial tablet formulation.
Due to inclusion complex-forming ability of cyclodextrins, CDs can be used as excipients in tablet formulations. It should be highlighted that cyclodextrin basic application is to increase the dissolution and bioavailability of low water-soluble drugs especially class II and class IV drugs [42]. The function of cyclodextrins in oral delivery system is as an excipient to transfer drugs across an aqueous phase to lipophilic surface in the gastrointestinal region by forming inclusion complexes which help in enhancing the dissolution rate of low aqueous soluble drugs [43].
When we look at the commercial tablets containing CDs, α-CD, β-CD and HP-β-CD were drawn attention for pharmaceutical applications [42]. β-CD, γ-CD, HP-β-CD and SBE-β-CD are included in EMA guideline for oral products. SBE-β-CD and HP-β-CD are cited in the FDA’s list of inactive pharmaceutical ingredients. There are cyclodextrin monographs in several pharmacopoeias such as European Pharmacopoeia, United States Pharmacopoeia National Formulary and Japanese Pharmacopoeia. Considering CDs that can be used in tablet formulations for oral drug delivery, β-CD, HP-β-CD and SBE-β-CD are the most commonly reported in the literature. In the light of these information, these new tablet formulation prepared modified cyclodextrin derivatives may be a promising candidate in terms of producibility and commercialization.
In vivo bioavailability studies
TMX bioavailability from the conventional and the M-B-CD complexed formulations were evaluated using the parameters, total area under the plasma level–time curve (AUC0–inf), peak plasma concentration (Cmax), and time to reach peak plasma concentration (Tmax). A statistically significant difference was observed between the values of the tablet including drug–CD complexes and commercial tablet for the three parameters. Moreover, the 90% confidence interval for the ratio of the AUC0–∝ values of the M-β-cyclodextrin complex over those of TMX was estimated to be 781 ± 155, while that of Cmax was 36.6 ± 25.3 ng/mL as can be seen in Table 2. These findings indicated that drug-cyclodextrin complexes had a much higher rate and extent of bioavailability in comparison with commercial product.
The plasma concentration versus time are shown in Fig. 5. The pharmacokinetic outline of TMX/M-β-CD tablet demonstrated an apparent advantage on commercial tablet formulation. As expected, plasma concentration of the complex was much higher than that of tamoxifen in 72 h. The pharmacokinetic parameters of tamoxifen as an inclusion complex and as a commercial tablet are listed in Table 1. Cmax of the TMX complex group were significantly (p < 0.01) increased twofold compared to that of the reference. Tmax of tamoxifen was statistically accelerated (p < 0.01) from 2.00 ± 3.46 h for commercial product to 1.00 ± 0.577 h for TMX/M-β-CD inclusion complex. AUC0–72h after oral administration of TMX/M-β-CD inclusion complex was much higher. Moreover, the elimination half-life (t1/2) of the inclusion complex was prolonged from 33.7 to 47.8 h, providing more time for absorption than the reference tablet formulation.
In this research, it seems that increased solubility and dissolution were featured parameters for higher Cmax and AUC following oral TMX/M-β-CD inclusion complex administration. In addition, extended elimination half-time may decrease Cl and render enough time to TMX absorption due to increased stability in gastrointestinal medium after complexation. Obtained results demonstrated that TMX absorption is extremely limited due to TMX solubility/dissolution properties (as can be seen in BCS Class II drugs) and solubility enhancing could be basic challenge. Hence, cyclodextrin complexation can be used as a promising tool for higher absorption with oral route.
In the literature, a few bioequivalance studies with TMX have drawn the attention. Tamoxifen and its active metabolite desmethyltamoxifen possess long elimination half-lives. According to Marzo et al., the case of tamoxifen and its active metabolite could be considered as a borderline situation between crossover and parallel group designs [44]. In 2004, same researchers found the usefulness of pilot trials on six volunteers with computer simulations in pharmaceutical development and in vitro-in vivo correlation studies [45]. Also, no clinical research studies with TMX:cyclodextrin complexes have taken part until today. In the light of data obtained oral bioavailability study, it can be indicated that these novel formulation significantly improve the permeability and absorption of TMX in vivo.
Cyclodextrins are being increasingly studied and are emerging as promising platforms for providing pharmacokinetic and formulation design efficiency, without a compromise on safety [46]. CDs are not toxic, because of the lack of absorption from the GI tract when administered orally [47, 48]. In EMA guideline, orally administered cyclodextrins at high doses (> 1000 mg/kg/day) may cause reversible diarrhea and cecal enlargement in animals. All parent cyclodextrins are accepted as food additives and are granted the excipient status “generally recognized as safe” (GRAS).
HP-β-cyclodextrin and SBE-β-cyclodextrin are considered non-toxic when administered as low doses by oral administration [49]. Also, methyl-β cyclodextrin are absorbed to a greater extent from gastrointestinal tract into the systemic circulation. Me-β-CD being known to enhance drug permeation through mucosal surface [50, 51]. Along, penetration enhancing effect of Me-β-CD, it was used to enhance the cytotoxic effect of tamoxifen by causing cell cycle arrest, induction of apoptosis and decreases tumor growth in vivo. Me-β-CD is a frequently used FDA approved cyclodextrin to disrupt lipid raft. These properties make Me-β-CD superior to other cyclodextrin derivatives [52].
Conclusion
In this study, TMX:CD inclusion complexes were succesfully prepared and characterized by DSC analysis, SEM and FT-IR studies. Then, a new oral tablet formulation was designed using TMX:M-β-CD inclusion complex and compared with tablets in the pharmaceutical market. In the light of data obtained in this study, the aqueous solubility and dissolution rate of TMX/M-β-CD inclusion complex were increased significantly compared to free TMX. Oral bioavailability of TMX were significantly enhanced with TMX/M-β-CD complex. Concisely, this study utilizes an efficient technique of complexation with CDs to come through the limited tamoxifen absorption and develop efficient oral dosage forms of TMX.
References
Buchanan, C.M., Buchanan, N.L., Edgar, K.J., Little, J.L., Malcolm, M.O., Ruble, K.M., et al.: Pharmacokinetics of tamoxifen after intravenous and oral dosing of tamoxifen-hydroxybutenyl-beta-cyclodextrin formulations. J. Pharm. Sci. 96(3), 644–660 (2007)
Park, W.C., Jordan, V.C.: Selective estrogen receptor modulators (SERMS) and their roles in breast cancer prevention. Trends Mol. Med. 8(2), 82–88 (2002)
Jain, S., Heeralal, B., Swami, R., Swarnakar, N.K., Kushwah, V.: Improved oral bioavailability, therapeutic efficacy, and reduced toxicity of tamoxifen-loaded liquid crystalline nanoparticles. AAPS PharmSciTech 19(1), 460–469 (2018)
Hard, G.C., Iatropoulos, M.J., Jordan, K., Radi, L., Kaltenberg, O.P., Imondi, A.R., et al.: Major difference in the hepatocarcinogenicity and DNA adduct forming ability between toremifene and tamoxifen in female Crl-Cd(Br) rats. Cancer Res. 53(19), 4534–4541 (1993)
McVie, J.G., Simonetti, G.P., Stevenson, D., Briggs, R.J., Guelen, P.J., de Vos, D.: The bioavailability of Tamoplex (tamoxifen). Part 1. A pilot study. Methods Find. Exp. Clin. Pharmacol. 8(8), 505–512 (1986)
Shin, S.C., Choi, J.S., Li, X.: Enhanced bioavailability of tamoxifen after oral administration of tamoxifen with quercetin in rats. Int. J. Pharm. 313(1–2), 144–149 (2006)
Elnaggar, Y.S., El-Massik, M.A., Abdallah, O.Y.: Self-nanoemulsifying drug delivery systems of tamoxifen citrate: design and optimization. Int. J. Pharm. 380(1–2), 133–141 (2009)
Layek, B., Mukherjee, B.: Tamoxifen citrate encapsulated sustained release liposomes: preparation and evaluation of physicochemical properties. Sci. Pharm. 78(3), 507–515 (2010)
Beig, A., Agbaria, R., Dahan, A.: Oral delivery of lipophilic drugs: the tradeoff between solubility increase and permeability decrease when using cyclodextrin-based formulations. PLoS ONE 8(7), e68237 (2013)
Shete, H.K., Selkar, N., Vanage, G.R., Patravale, V.B.: Tamoxifen nanostructured lipid carriers: enhanced in vivo antitumor efficacy with reduced adverse drug effects. Int. J. Pharm. 468(1–2), 1–14 (2014)
Jena, S.K., Singh, C., Dora, C.P., Suresh, S.: Development of tamoxifen-phospholipid complex: novel approach for improving solubility and bioavailability. Int. J. Pharm. 473(1–2), 1–9 (2014)
Kawabata, Y., Wada, K., Nakatani, M., Yamada, S., Onoue, S.: Formulation design for poorly water-soluble drugs based on biopharmaceutics classification system: basic approaches and practical applications. Int. J. Pharm. 420(1), 1–10 (2011)
Desai, S., Poddar, A., Sawant, K.: Formulation of cyclodextrin inclusion complex-based orally disintegrating tablet of eslicarbazepine acetate for improved oral bioavailability. Mater. Sci. Eng. C 58, 826–834 (2016)
Torne, S., Darandale, S., Vavia, P., Trotta, F., Cavalli, R.: Cyclodextrin-based nanosponges: effective nanocarrier for tamoxifen delivery. Pharm. Dev. Technol. 18(3), 619–625 (2013)
Piao, H., Yang, L., Piao, H., Wang, P., Shi, H., Fang, L., et al.: A pre-formulation study of a polymeric solid dispersion of paclitaxel prepared using a quasi-emulsion solvent diffusion method to improve the oral bioavailability in rats. Drug Dev. Ind. Pharm. 42(3), 353–363 (2016)
Rumondor, A.C., Dhareshwar, S.S., Kesisoglou, F.: Amorphous solid dispersions or prodrugs: complementary strategies to increase drug absorption. J. Pharm. Sci. 105(9), 2498–2508 (2016)
Junyaprasert, V.B., Morakul, B.: Nanocrystals for enhancement of oral bioavailability of poorly water-soluble drugs. Asian J. Pharm. Sci. 10(1), 13–23 (2015)
Dehghani, F., Farhadian, N., Golmohammadzadeh, S., Biriaee, A., Ebrahimi, M., Karimi, M.: Preparation, characterization and in vivo evaluation of microemulsions containing tamoxifen citrate anti-cancer drug. Eur. J. Pharm. Sci. 96, 479–489 (2017)
Chowdhury, N., Vhora, I., Patel, K., Bagde, A., Kutlehria, S., Singh, M.: Development of hot melt extruded solid dispersion of tamoxifen citrate and resveratrol for synergistic effects on breast cancer cells. AAPS PharmSciTech 19(2), 792–802 (2018)
Davis, M.E., Brewster, M.E.: Cyclodextrin-based pharmaceutics: past, present and future. Nat. Rev. Drug Discov. 3(12), 1023–1035 (2004)
Shukla, J., Sharma, U., Kar, R., Varma, I.K., Juyal, S., Jagannathan, N.R., et al.: Tamoxifen-2-hydroxylpropyl-beta-cyclodextrin-aggregated nanoassembly for nonbreast estrogen-receptor-positive cancer therapy. Nanomedicine 4(8), 895–902 (2009)
Shangguan, L.Q., Chen, Q., Shi, B.B., Huang, F.H.: Enhancing the solubility and bioactivity of anticancer drug tamoxifen by water-soluble pillar[6]arene-based host-guest complexation. Chem. Commun. 53(70), 9749–9752 (2017)
Loftsson, T., Jarho, P., Masson, M., Jarvinen, T.: Cyclodextrins in drug delivery. Expert Opin. Drug Deliv. 2(2), 335–351 (2005)
Singh, A., Worku, Z.A., Van den Mooter, G.: Oral formulation strategies to improve solubility of poorly water-soluble drugs. Expert Opin. Drug Deliv. 8(10), 1361–1378 (2011)
Gidwani, B., Vyas, A.: A comprehensive review on cyclodextrin-based carriers for delivery of chemotherapeutic cytotoxic anticancer drugs. Biomed. Res. Int. 2015, 198268 (2015)
Zhang, X., Zhang, T., Lan, Y., Wu, B., Shi, Z.: Nanosuspensions containing oridonin/HP-beta-cyclodextrin inclusion complexes for oral bioavailability enhancement via improved dissolution and permeability. AAPS PharmSciTech 17(2), 400–408 (2016)
Yao, Y., Xie, Y., Hong, C., Li, G., Shen, H., Ji, G.: Development of a myricetin/hydroxypropyl-beta-cyclodextrin inclusion complex: preparation, characterization, and evaluation. Carbohydr. Polym. 110, 329–337 (2014)
Bilensoy, E., Dogan, L., Sen, M., Hincal, A.: Complexation behavior of antiestrogen drug tamoxifen citrate with natural and modified beta-cyclodextrins. J. Incl. Phenom. Macrocycl. 57(1–4), 651–655 (2007)
Gjerde, J., Kisanga, E.R., Hauglid, M., Holm, P.I., Mellgren, G., Lien, E.A.: Identification and quantification of tamoxifen and four metabolites in serum by liquid chromatography-tandem mass spectrometry. J. Chromatogr. A 1082(1), 6–14 (2005)
Patel, H.M., Suhagia, B.N., Shah, S.A., Rathod, I.S., Parmar, V.K.: Preparation and characterization of etoricoxib-beta-cyclodextrin complexes prepared by the kneading method. Acta Pharm. 57(3), 351–359 (2007)
Sapkal, N.P., Kilor, V.A., Bhusari, K.P., Daud, A.S.: Evaluation of some methods for preparing gliclazide beta-cyclodextrin inclusion complexes. Trop. J. Pharm. Res. 6(4), 833–840 (2007)
Shaker, D.S., Shaker, M.A., Hanafy, M.S.: Cellular uptake, cytotoxicity and in vivo evaluation of Tamoxifen citrate loaded niosomes. Int. J. Pharm. 493(1–2), 285–294 (2015)
Challa, R., Ahuja, A., Ali, J., Khar, R.K.: Cyclodextrins in drug delivery: an updated review. AAPS PharmSciTech 6(2), E329–E357 (2005)
Fenyvesi, E., Szeman, J., Csabai, K., Malanga, M., Szente, L.: Methyl-beta-cyclodextrins: the role of number and types of substituents in solubilizing power. J. Pharm. Sci. 103(5), 1443–1452 (2014)
Aloisio, C., Longhi, M.: Diloxanide furoate binary complexes with beta-, methyl-beta-, and hydroxypropyl-beta-cyclodextrins: inclusion mode, characterization in solution and in solid state and in vitro dissolution studies. Pharm. Dev. Technol. 23(7), 723–731 (2018)
de Freitas, M.R., Rolim, L.A., Soares, M.F.D., Rolim-Neto, P.J., de Albuquerque, M.M., Soares-Sobrinho, J.L.: Inclusion complex of methyl-beta-cyclodextrin and olanzapine as potential drug delivery system for schizophrenia. Carbohydr. Polym. 89(4), 1095–1100 (2012)
Rudrangi, S.R., Trivedi, V., Mitchell, J.C., Wicks, S.R., Alexander, B.D.: Preparation of olanzapine and methyl-beta-cyclodextrin complexes using a single-step, organic solvent-free supercritical fluid process: an approach to enhance the solubility and dissolution properties. Int. J. Pharm. 494(1), 408–416 (2015)
Rudrangi, S.R., Bhomia, R., Trivedi, V., Vine, G.J., Mitchell, J.C., Alexander, B.D., et al.: Influence of the preparation method on the physicochemical properties of indomethacin and methyl-beta-cyclodextrin complexes. Int. J. Pharm. 479(2), 381–390 (2015)
Zia, V., Rajewski, R.A., Stella, V.J.: Effect of cyclodextrin charge on complexation of neutral and charged substrates: comparison of (SBE)7 M-beta-CD to HP-beta-CD. Pharm. Res. 18(5), 667–673 (2001)
Másson, M., Loftsson, T., Jónsdóttir, S., Fridriksdóttir, H., Petersen, D.S.: Stabilisation of ionic drugs through complexation with non-ionic and ionic cyclodextrins. Int. J. Pharm. 164(1–2), 45–55 (1998)
Conceição, J., Adeoye, O., Cabral-Marques, H.M., Lobo, J.M.S.: Cyclodextrins as excipients in tablet formulations. Drug Discov. Today 23(6), 1274–1284 (2018)
Sharma, N., Baldi, A.: Exploring versatile applications of cyclodextrins: an overview. Drug Deliv. 23(3), 739–757 (2016)
Marzo, A.: Crossover design in tamoxifen bioequivalence: a borderline situation. J. Pharm. Pharmacol. 50(12), 1433–1434 (1998)
Marzo, A., Fibbioli, M., Marone, C., Cerutti, B.: The degree of predictivity in pilot studies on six subjects in bioequivalence trials. Pharmacol. Res. 49(3), 283–286 (2004)
Adeoye, O., Cabral-Marques, H.: Cyclodextrin nanosystems in oral drug delivery: a mini review. Int. J. Pharm. 531(2), 521–531 (2017)
Irie, T., Uekama, K.: Pharmaceutical applications of cyclodextrins. III. Toxicological issues and safety evaluation. J. Pharm. Sci. 86(2), 147–162 (1997)
Calleja, P., Huarte, J., Agueros, M., Ruiz-Gaton, L., Espuelas, S., Irache, J.M.: Molecular buckets: cyclodextrins for oral cancer therapy. Ther. Deliv. 3(1), 43–57 (2012)
Thompson, D.O.: Cyclodextrins—enabling excipients: their present and future use in pharmaceuticals. Crit. Rev. Ther. Drug Carrier Syst. 14(1), 1–104 (1997)
Sajeesh, S., Bouchemal, K., Marsaud, V., Vauthier, C., Sharma, C.P.: Cyclodextrin complexed insulin encapsulated hydrogel microparticles: an oral delivery system for insulin. J. Controll. Release 147(3), 377–384 (2010)
Boulmedarat, L., Piel, G., Bochot, A., Lesieur, S., Delattre, L., Fattal, E.: Cyclodextrin-mediated drug release from liposomes dispersed within a bioadhesive gel. Pharm. Res. 22(6), 962–971 (2005)
Mohammad, N., Malvi, P., Meena, A.S., Singh, S.V., Chaube, B., Vannuruswamy, G., et al.: Cholesterol depletion by methyl-beta-cyclodextrin augments tamoxifen induced cell death by enhancing its uptake in melanoma. Mol. Cancer 13, 204 (2014)
Acknowledgements
Alper B. Iskit has been supported by the Turkish Academy of Sciences, in the framework of the Young Scientist Award Program (EA-TUBA-GEBIP/2001-2-11).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Erdoğar, N., Nemutlu, E., İskit, A.B. et al. Improved oral bioavailability of anticancer drug tamoxifen through complexation with water soluble cyclodextrins: in vitro and in vivo evaluation. J Incl Phenom Macrocycl Chem 96, 81–91 (2020). https://doi.org/10.1007/s10847-019-00952-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10847-019-00952-4