Abstract
Trans-Resveratrol (RV) is a natural polyphenol characterized by interesting pleiotropic potentials and health benefits, but its administration is hampered by a unsatisfactory pharmacokinetics. Various approaches have been identified to circumvent it: among them, 2-hydroxypropyl-β-cyclodextrins (HPβCD) are valuable strategy. Here, we compare the employment of HPβCD based formulation with a resveratrol nanosupension (obtained by diluting a RV ethanol solution with PBS, added of 0.05 % hydroxyethylcellulose) to improve RV bioavailability after oral administration to mice. The inclusion of RV in HPβCD was confirmed by differential scanning calorimetry, Fourier transformed infrared spectroscopy, and phase solubility study. The two formulations were orally administered to BALB-c mice. RV concentrations in plasma and tissues were detected at different time (0–120 min) by HPLC method. HPβCD complexation mediate a approximately fourfold increment in plasma RV Cmax and approximately twofold augment of RV AUC0-120 in comparison with RV nanosuspension. Similar increased concentrations were observed in heart, liver, kidney and gut. In particular, HPβCD mediated a 5.5-folds increase of resveratrol concentration in the intestine, in comparison to the nanosuspension. In conclusion, based on our results, HPβCD complexation is a promising approach to increase the oral bioavailability of RV. Moreover, the achievement of high concentrations in gut suggested a potential employment of oral RV-HPβCD as anti-inflammatory/chemopreventive agent in this tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A great number of natural molecules were identified and characterized for their utilization in human disorders. Although they displayed strong in vitro activities, the unfavorable physical/chemical properties frequently limited their clinical utilization [1]. Among others, trans-resveratrol (RV, 3,5,4′-trihydroxy-trans-stilbene) is one of the most studied natural polyphenols. It is a phytoalexin synthesized by various plants in response to stress and microbial attack. Moreover, it shows interesting in vitro pleiotropic effects, including anti-oxidant, anti-aging, anti-inflammatory, and anti-cancer actions as well as neuro- and cardiovascular protection [2, 3]. However, the systemic administration of RV is hampered by its low water solubility, low stability (mainly linked to inactivation by trans-to-cis isomerization in solution) and rapid extensive in vivo metabolism [4], which together impair the achievement and the maintenance of bioefficacious concentrations in the blood and target tissues [5, 6]. Thus, the limited amount of intact RV existed in the systemic circulation could not guarantee therapeutic concentration, producing uncertain in vivo results, as already reviewed by Carter et al. [7].
Various approaches have been identified to circumvent these problems, some of which are nowadays in clinical experimentation [8–10]. Among them, cyclodextrins (CDs) have displayed a considerable ability to include and protect natural compounds [11, 12]. CDs are a family of cyclic oligosaccharides made up of variable glucose residues linked by glycosidic bonds; furthermore, they consist of a truncated cone structure with a hydrophobic cavity, which could form inclusion complexes with a wide range of guest molecules, modifying their physical and chemical properties. In particular, 2-hydroxypropyl-β-CD (HPβCD), a semisynthetic CD, demonstrated to possess high molecular recognition and inclusion ability as well as to improve water-solubility of natural molecules, including RV [13]. In this context, the complexation with HPβCD has been already employed to reduce the trans-to-cis isomerization rate of resveratrol, thus enhancing its molecular stability [14].
The aim of our study was to investigate improvements that HPβCD complexation should induce to RV pharmacokinetics. In particular, in a mouse model we evaluated and compared RV bioavailability and concentration in different tissues after the oral administration of a single dose of RV, which was formulated as complex in HPβCD (RV-HPβCD) or as aqueous nanosuspension in water (RV-ns).
Materials and methods
Materials
Trans-resveratrol (RV) was purchased from Cayman Chemical (Ann Arbor, MI, USA); HPβCD (KLEPTOSE® HPB ORAL GRADE MEDIUM MS, DS 4.5, average MW 1399.35) was kindly gifted by Roquette (Lestrem, France). Hydroxyethylcellulose was from A.C.E.F. (Piacenza, Italy); HPLC grade acetonitrile was from VWR International PBI (Milan, Italy); HPLC grade water was produced with Milli DI system coupled with a Synergy 185 system by Millipore (Milan, Italy); HPLC grade methanol and acetic acid were from Sigma-Aldrich (St. Louis, MO, USA), as well as all the other analytical grade reagents.
HPLC determination of trans-resveratrol
For HPLC determination of trans-resveratrol a Lachrom7000 HPLC (Merck–Hitachi, Merck KGaA, Darmstadt, Germany) equipped with a C18 analytical column 250 × 4.6 mm, 5 μm (Alltech Italia S.r.l., Milano, Italy) preceded by a guard column (C18 SecurityGuard Cartridges 4.0 × 3.0, Phenomenex, Castel Maggiore, Italy) was used. The mobile phase consisted of a gradient of 0.5 % acetic acid, methanol, and acetonitrile (0–5 min: 52:48:0, v/v/v; 6–19 min: 52:10:38, v/v/v; 20–21 min: 52:48:0, v/v/v) at the constant flow rate of 1 ml/min at 30° C. Sample elution was monitored at the 303 nm wavelength.
Preparation of the resveratrol formulations
To prepare the HPβCD complex, RV was finely suspended in a water solution containing an equimolar amount of HPβCD and the suspension was stirred at room temperature in the dark until the equilibrium was reached (24 h) [14]. After centrifugation, the supernatant was freeze-dried. To determine the RV percentage in the complex, a weighted amount of obtained freeze-dried inclusion complex (RV-HPβCD) was dissolved in methanol. After sonication, the sample was diluted with methanol and analyzed by HPLC for a quantitative determination of RV. As stock solution, freeze-dried RV-HPβCD complex was dissolved at the concentration equivalent to 7 mM RV in PBS, pH 7.4.
To prepare the nanosuspension a two-step process was employed. Firstly, an ethanolic solution of RV was prepared at the concentration of 200 mM. Then, the RV nanosuspension (RV-ns) was obtained, diluting with PBS the ethanolic solution, to reach the same final molar concentration of RV-HPβCD complex. As the dilution causes a rapid precipitation of RV, the nanosuspension was stabilized by the addition of hydroxyethylcellulose (0.05 % w/w).
Phase solubility studies
Phase solubility studies were carried out according to the Higuchi-Connors method [15]. An excess of RV (5 mg) was added to a series of aqueous solutions (5 ml) containing increasing concentrations of HPβCD from 0 to 5 mg/ml (3.24 mM). The samples were shaken in the dark at room temperature for 24 h. After equilibration, suspensions were centrifuged and quantitative determination of RV in the supernatant was carried out by HPLC method. The phase diagram was constructed by plotting the total molar concentration of RV in solution against the molar concentration of HPβCD.
Stability constants (Kst) from the phase solubility diagram was calculated according to the formula #1 (F1):
where S0 represents the intrinsic solubility of RV in absence of HPβCD. The slope was determined from the initial straight-line portion of the plot of concentration of RV against the concentration of CDs.
The complexation efficiency (CE), defined as the concentration ratio between cyclodextrin in a complex and free cyclodextrin, is calculated from the phase-solubility diagrams, with the formula #2 (F2):
In vitro solubility studies
In vitro experiments were conducted by dialysis bag technique to evaluate the solubility kinetics of the RV-ns. The analysis was carried out at 37 °C. A cellulose membrane (Spectrapore, cut-off 12000 Da) separates the donor compartment containing 15 mg/ml of RV-ns from the receiving compartment filled with filtered water and 0.05 % sodium dodecyl sulfate (SDS) as dissolution medium, to maintain sink conditions. The receiving phases were withdrawn at regular intervals and replaced with the same amount of fresh receiving medium; quantitative determination of RV was carried out by HPLC method. Data were expressed as percentage of RV dissolved over time.
Characterization of the resveratrol formulations
The analysis of RV-ns particle size was performed by photoncorrelation spectroscopy using a 90 Plus instrument (Brookhaven, NY, USA), at a scattering angle of 90° and a temperature of 25 °C, after an opportune dilution of the nanosuspension with deionized water.
Differential scanning calorimetry analysis (DSC) was carried out using a DSC/7 differential scanning calorimeter (Perkin-Elmer, Branford, CT, USA) equipped with a TAC 7/DX instrument controller. The instrument was calibrated with indium for melting point and heat of fusion before analyses took place. A heating rate of 10 °C per minute was used in the 25–290 °C temperature range. The thermal behavior was studied by heating about 3 mg of RV and freeze-dried RV-ns and RV-HPβCD in standard aluminum sample pans (Perkin-Elmer); an empty aluminum pan was used as the reference standard. Analyses were carried out under nitrogen purge; analyses were performed in triplicate for each sample.
RV, HPβCD, and RV-HPβCD underwent to Fourier transformed infrared spectroscopy (FTIR) studies by potassium bromide disc method using Perkin Elmer system 2000 FTIR Spectrophotometer in the region of 4000–450 cm−1.
In vivo pharmacokinetics assessment
Pharmacokinetics profile was evaluated on 75 two-month old BALB-c mice from the animal facility of Molecular Biotechnology Center (University of Turin). Animals were fed ad libitum, but starved the night before the experiment.
Forty-eight mice received oral administration of either RV-ns or RV-HPβCD (n = 24 each group) by orogastric tube. After administration, each mouse had received a single dose equivalent to 15 mg/kg RV. Three mice per group were bled and then euthanized at 1, 2, 5, 10, 15, 30, 60 and 120 min. Blood samples were collected and immediately centrifuged at 3000 rpm, 4 °C for 10 min to obtain plasma. Brain, heart, liver, kidney, and gut were explanted, rinsed in saline, and frozen in liquid nitrogen for further HPLC analysis.
To calculate and compare bioavailability of RV formulations, 27 mice were administered with RV-ns (equivalent to 15 mg/kg RV) by tail vein injection; 3 mice were bled immediately after the RV injection or at 1, 2, 5, 10, 15, 30, 60 and 120 min. All blood samples were processed as above described.
Bioavailability (F) was evaluated in collected bloods through the employment of the formula #3 (F3):
where AUC (Area Under Curve) represents the concentration–time profile, and D represents the administered dose for both per os (po) and intravenous (iv) administrations.
All procedures for the animal care and treatment were in accordance with the Institutional and National Animal Care Committees.
Resveratrol extraction
Plasma samples were supplemented with 1.5-folds of extraction solution (methanol/2.5 % acetic acid solution 90:10 v/v containing 0.05 % of ascorbic acid), containing 2 μg/ml flavon (as internal standard, IS). Samples were centrifuged at 2000 rpm at 4 °C for 3 min and supernatants were collected. Tissues were processed as follows: 100 mg of each organ were homogenized in 3 ml of extraction solution for 3 min by means of an ULTRA TURRAX (T25, IKA, Germany), added of 2 μg/g IS and processed as described above. Obtained pellets were re-extracted with the same procedure. The two corresponding supernatants were unified and freeze-dried. For each passage, samples were kept on ice and protected from light.
Blank tissues added with different RV concentrations were processed as described above in order to obtain calibration curves for each organ in the subsequent analyses.
Resveratrol quantification
Dried samples were reconstituted with 300 μl of the starting composition of the mobile phase (0.5 % acetic acid/methanol 52:48 v/v) and centrifuged. Fifty microliters of each supernatant was collected and analysed by means of a Lachrom7000 HPLC (Merck–Hitachi, Merck KGaA, Darmstadt, Germany) as described above.
Statistical analysis
The calibration curves for HPLC analyses were constructed by plotting the peak-height ratios of RV to IS versus the nominal concentrations in the standard biological samples using linear regression analysis.
RV concentrations were represented as mean ± standard error of the mean (SEM).
The maximum reached concentration (Cmax), the time needed to reach the Cmax (Tmax), and concentration–time profile (AUC) were calculated with PKSolver v2.0.
Results
Phase solubility studies
The RV solubility increased as a function of HPβCD concentration as reported in Fig. 1a. An “A-type” diagram was obtained, according to the Higuchi and Connors classification [15], where the guest solubility increased linearly with HPβCD concentration. The calculated stability constant (Kst) was 6960 M−1. The slope of the curve was lower than one, thus it was assumed that the gain in solubility observed was due to the formation of a 1:1 complex. In fact, the calculated complexation efficiency (CE) was 1.11.
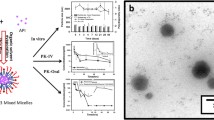
Characterization of RV-HPβCD inclusion complex. Solubility of RV improves at the increasing concentration of HPβCD (a); Differential Scanning Calorimetry (DSC) thermograms of RV, RV-ns and RV-HPβCD (b); and FTIR spectra of RV and RV-HPβCD (c); In vitro solubility kinetics of 15 mg/ml RV nanosuspension (d)
Characterization of resveratrol formulations
As demonstrated by photon-correlation spectroscopy, the average diameter of RV nanoparticle in the RV-ns was about 800 nm. Furthermore, both RV-ns and RV-HPβCD formulations induced alteration in the thermogram of RV (Fig. 1b). In fact, a shift of the 267 °C melting endothermic peak of RV toward cooler temperatures accompanied by a reduction in endothermic energy was observed in RV-ns, due to the stabilization induced by the hydroxyethylcellulose. Meanwhile in RV-HPβCD, the endothermic peak was absent, indicating the interaction between RV and HPβCD and the formation of inclusion complexes. In this context, RV is molecularly dispersed in the cyclodextrin cavity without the possibility to crystallize. In addition, the characteristic infrared absorption of C–C aromatic double bond stretching founding in the spectrum of RV in the range of 1700–450 cm−1 was altered in RV-HPβCD (Fig. 1c). The shifted spectral features of guest molecule in RV-HPβCD complex confirmed the inclusion of RV in the HPβCD cavity. Finally, RV-ns required 6 h to be dissolved quite completely (about 95 %) in water. Figure 1d reports the in vitro solubility kinetics of RV from RV nanosuspension.
HPLC method results
The specificity of HPLC method was determined by comparing the chromatograms of blank plasma/tissue with the corresponding spiked plasma/tissue. RV and IS were eluted approximately at 6.4 and 19.0 min, respectively (Fig. 2). Data from calibration curves were reported in Table 1.
Quantitation of resveratrol in plasma after single oral administration
The concentration of RV in plasma was determined by HPLC. The mean plasma concentration–time profiles after single administration of RV-ns (per os and intravenous) and RV-HPβCD (per os) are shown in Table 2, whereas the corresponding pharmacokinetic parameters are reported in Table 3.
Cmax of RV-HPβCD was 3.94-folds than RV-ns, while the AUC0-120 was 2.04 folds greater. Consequently, oral bioavailability of the two RV formulations was 52.5 and 25.8 %, respectively. Curve profiles of oral administered formulations showed peaks of concentration at 5 and 30 min for HPβCD and RV respectively. After intravenous administration the RV plasmatic concentration reached about 100 g/ml and tended to zero after 30 min, with a T1/2 of ~10.34 min.
Tissue distribution of resveratrol
The detection of RV concentrations in brain, heart, liver, kidney, and gut was performed as previously described for plasma samples. The tissue concentration–time profiles of orally administered RV-ns and RV-HPβCD are shown in Fig. 3a. Similarly to what occurs in plasma, the complexation in HPβCD significantly improved the RV Cmax and AUC1-120 in all considered organs, at exclusion of brain where RV was detected in concentrations ten-fold smaller than other tissues (Fig. 3b, c). Interestingly, a great amount of RV was detected in gut where HPβCD was able to mediate a 5.5-fold increase of AUC1-120. This is due to the presence of a great peak of concentration at 30 min from the administration that is not detectable in RV-ns profile.
Discussion
Researchers’ trays are full of unfulfilled dreams: in particular, those of chemists and pharmacologists contain a large number of molecules, often of natural origin, which are characterized by interesting beneficial effects, but not clinically employable due to poor pharmacokinetics (poor water solubility, rapid metabolism, etc.).
Resveratrol was discovered in 1940 [16], but its first beneficial effect was detected in 1992 [17] when RV has been postulated to explain some of the cardio-protective effects of red wine. From then, RV has been extensively studied and, though the exact molecular mechanisms are currently still unclear, a broad-spectrum of beneficial health properties has been shown, such as anti-infective (anti-bacterial, anti-fungal, anti-malarial, and anti-viral), anti-oxidant, anti-inflammatory, anti-allergic (immune regulation), and anti-diabetic (it enhances insulin sensitivity) actions [18, 19]. Moreover, Jang and colleagues [20] firstly reported in 1997 the RV-mediated chemoprevention through the inhibition of cyclooxygenase activities. Likewise, other anticancer related mechanisms were soon revealed, and RV-mediated inhibition of ribonucleotide reductase [21], DNA polymerase [22], cell cycle progression [23] as well as the targeting of ornithine decarboxylase [24], PTEN/Akt [25], NFkB [26], and STAT3 [27] have been reported.
The main obstacle to the clinical RV employment resides in its poor aqueous solubility and bioavailability, which greatly hampers its efficacy after oral administration [28]. In deep, based on the urinary excretion data in humans, the absorption of RV appears to be at least 70 % [6, 29]. Also in rats, after oral administration, RV intestinal absorption was elevated (about 77–80 %) [30]. However, due to rapid and extensive metabolism, RV has a very short initial half-life that was approximately calculated in 8–14 min [31]. Consequently, circulating RV is rapidly inactivated and removed from the body [32], resulting in only trace amounts of unchanged molecules in the systemic circulation. Hence, circulating RV is unlikely able to achieve 1.14 mg/L (5 µM) in plasma, which is postulated as a minimum effective chemoprevention concentration to guarantee its therapeutic activities [29].
Beyond these important shortcomings, several research groups threw light on the complex RV metabolic pattern identifying precursors to be employed as pro-drugs [5] and several different metabolites (e.g. sulfated and glucuronide), some of which still retain the RV activities [29, 33]. On these bases and to improve kinetics and biological efficacy, several RV analogues were thus synthetized, allowing to the findings that poly-hydroxylated RV derivatives showed high rate of COX inhibition, free radical scavenging activity and ribonucleotide reductase inhibition.
Another strategy to circumvent the poor pharmacokinetics of RV and achieve therapeutic doses after oral administration is the possibility to formulate RV to protect it from metabolism and elimination. Focusing the attention on CDs, they have been shown to enhance drug bioavailability through stabilization of drug molecules that have low aqueous solubility but show good membrane permeability [34], such as resveratrol. Furthermore, hydrophilic CDs, e.g. HPβCD, are able to increase permeation of lipophilic drugs. In this context, we already reported that the complexation of RV in HPβCD was able to mediate a chemo-preventive action in an in vivo model of chemically induced oral squamous cell carcinoma, even though after topic application on buccal mucosae [35]. In addition, RV complexation with either HPβCD or random-methyl-βCD improved the water solubility of RV, though data about oral administration were limited only to random-methyl-βCD [36, 37].
The effect of the complexation of trans-resveratrol with HPβCD on its biological properties was largely investigated [38]. The antioxidant activity of RV in the absence and presence of increasing concentrations of HPβCD was determined by Lucas-Abellan et al. [39] showing that complexation led to an increase not only in its aqueous solubility but also in its antioxidant activity. On the contrary, other authors [13] reported that the differences in scavenging capacity between free and complexed RV are slight, suggesting that the inclusion process had little influence on the antioxidant activity. Moreover, Sapino et al. demonstrated that the inclusion phenomenon did not significatively interfere with the radical scavenging activity, the metal-chelating efficiency and the antilipoperoxidative potential of RV [14].
In the light of these premises, we evaluated the HPβCD complex as strategy for the oral administration of RV, inasmuch as orally administered HPβCD (up to 500 mg/kg/day [40]) is non-toxic likely due to their low absorption (2–4 %) along the gastrointestinal tract [41]. Moreover, also RV displays a good safety profile: in vivo study demonstrated that RV toxicity occurs at high dose, only. Indeed, as reviewed by Cottart et al. [42], RV is safe in the animal until the dose of 3 g/kg/day, which corresponds to 210 g/day in humans. At this concentration, 2 of 40 rats (5 %) died after being treated continuously for 4 weeks.
In this study, we confirmed that RV is able to interact with and to be included within HPβCD cavity to form an inclusion complex in the 1:1 ratio as evinced by the direct correlation between RV aqueous solubility and HPβCD concentration in the phase-solubility study, likewise what already reported by Das et al. [36] and Duarte et al. [37]. In fact, they both demonstrated “A-type” phase solubility diagrams characterized by the formation of 1:1 ratio moderately stable complexes with either HPβCD or random-methyl-βCD.
Obtained inclusion complexes are noteworthy able to mediate, in vitro, a higher and faster diffusion through membranes with respect to the free drug. Motivated by this result, we thus assessed the in vivo systemic pharmacokinetics of RV comparing the results of the nanosuspension with those of HPβCD complexes. To our best knowledge, this is the first work that investigated the tissue distribution of RV after oral administration of RV-HPβCD complex.
Results agree with those obtained in vitro and indicate a general improvement of RV in analyzed tissues, which is reflected in an improved oral bioavaislability and kinetics of RV-HPβCD when compared with unvehicled RV. The plasma pharmacokinetics is in agreement with previous findings. Das and coworkers [36] studied the pharmacokinetics of RV-HPβCD complex after the intravenous administration at different doses. The complexation with HPβCD did not marked affect the blood circulation time. Indeed, the dissociation of included molecule from the cyclodextrin complexes occurs after the blood dilution, determining a rapid release of the drug. Interestingly, in our study, HPβCD complexation enabled RV to reach the minimum chemoprevention concentration in plasma within the first ten minutes after oral administration of a single dose of RV-HPβCD complex. This effect may be likely owing to the increased stability, water solubility and permeation through membranes demonstrated by HPβCD complex [43]. Besides this initial response, a second peak was detected in plasma after 30 min from the administration. It is noteworthy that, in this case, high amounts of RV were also detectable concomitantly in the gut. This type of kinetics is consistent with the enterohepatic recirculation already reported by other Authors and likely due to glucuronated metabolites that are reconverted in RV by the intestinal flora [44]. The phenomenon, together with the in vitro enhancement of permeation through the membranes, can explain the great amount of RV detectable even after 1 h in kidney, which is the main elimination route of RV in the organisms [44]. HPβCD complexation was not able to allow RV to pass the hematoencephalic barrier: as a result, only trace of RV was found in brain.
Anyway, it has been demonstrated that changing the formulation employed to vehiculate the drug, its pharmacokinetics can consequently change: indeed, utilizing a similar approach, but exploiting lipophilic vectors (solid lipid nanoparticle), Jose and co-workers were able to specifically enhance the brain delivery of RV [45].
The development of new formulations can make an old drug suitable for a new medicinal product registration. The use of CDs as excipients allows the achievement of a formulation ready for clinical trials. HPβCD is an excipient admitted by Regulatory Authorities for oral and intravenous administration and its monography is reported in the European Pharmacopoeia. A number of medicinal products containing HPβCD are already on the market. Here, we demostrated in our knowledge for the first time that RV can be efficaciously delivered in vivo with non-expensive and safe carriers represented by cyclodextrins. In fact, we showed that RV-HPβCD complexes greatly enhanced the oral bioavailability of RV (more than twice with respect to RV aqueous nanosuspension). Despite we analyzed the pharmacokinetics after a single dose administration only, our formulation was able to reach bioactive concentrations in both plasma and gut. In particular, considering the time and concentration profile of RV detected in the latter, RV-HPβCD complexes could become a promising tool to address chronic inflammatory and/or precancerous lesion of gut, thus the efficacy of chronically administered RV-HPβCD complexes are under investigations.
References
Chabner, B.A., Roberts Jr., T.G.: Timeline: chemotherapy and the war on cancer. Nat. Rev. Cancer 5(1), 65–72 (2005). doi:10.1038/nrc1529
Lettieri Barbato, D., Tatulli, G., Aquilano, K., Ciriolo, M.R.: Inhibition of Age-Related Cytokines Production by ATGL: a Mechanism Linked to the Anti-Inflammatory Effect of Resveratrol. Mediators Inflamm. 2014, 917698 (2014). doi:10.1155/2014/917698
Udenigwe, C.C., Ramprasath, V.R., Aluko, R.E., Jones, P.J.: Potential of resveratrol in anticancer and anti-inflammatory therapy. Nutr. Rev. 66(8), 445–454 (2008). doi:10.1111/j.1753-4887.2008.00076.x
Francioso, A., Mastromarino, P., Masci, A., d’Erme, M., Mosca, L.: Chemistry, stability and bioavailability of resveratrol. Med. Chem. 10(3), 237–245 (2014). doi:10.2174/15734064113096660053
Liang, L., Liu, X., Wang, Q., Cheng, S., Zhang, S., Zhang, M.: Pharmacokinetics, tissue distribution and excretion study of resveratrol and its prodrug 3, 5, 4′-tri-O-acetylresveratrol in rats. Phytomedicine 20(6), 558–563 (2013). doi:10.1016/j.phymed.2012.12.012
Walle, T., Hsieh, F., DeLegge, M.H., Oatis, J.E., Walle, U.K.: High absorption but very low bioavailability of oral resveratrol in humans. Drug Metab. Dispos. 32(12), 1377–1382 (2004). doi:10.1124/dmd.104.000885
Carter, L.G., D’Orazio, J.A., Pearson, K.J.: Resveratrol and cancer: focus on in vivo evidence. Endocr. Relat. Cancer 21(3), R209–R225 (2014). doi:10.1530/ERC-13-0171
Basavaraj, S., Betageri, G.V.: Improved oral delivery of resveratrol using proliposomal formulation: investigation of various factors contributing to prolonged absorption of unmetabolized resveratrol. Expert Opin. Drug Deliv. 11(4), 493–503 (2014). doi:10.1517/17425247.2014.878701
Bonechi, C., Martini, S., Ciani, L., Lamponi, S., Rebmann, H., Rossi, C., Ristori, S.: Using liposomes as carriers for polyphenolic compounds: the case of trans-resveratrol. PLoS ONE 7(8), e41438 (2012). doi:10.1371/journal.pone.0041438
Neves, A.R., Lúcio, M., Martins, S., Lima, J., Reis, S.: Novel resveratrol nanodelivery systems based on lipid nanoparticles to enhance its oral bioavailability. Int. J. Nanomed. 8, 177–187 (2012). doi:10.2147/IJN.S37840
Mangolim, C.S., Moriwaki, C., Nogueira, A.C., Sato, F., Baesso, M.L., Neto, A.M., Matioli, G.: Curcumin–β-cyclodextrin inclusion complex: stability, solubility, characterisation by FT-IR, FT-Raman, X-ray diffraction and photoacoustic spectroscopy, and food application. Food Chem. 153, 361–370 (2014). doi:10.1016/j.foodchem.2013.12.067
Zhang, Q.F., Nie, H.-C., Shangguang, X.-C., Yin, Z.-P., Zheng, G.-D., Chen, J.-G.: Aqueous solubility and stability enhancement of astilbin through complexation with cyclodextrins. J. Agric. Food Chem. 61(1), 151–156 (2012). doi:10.1021/jf304398v
Lu, Z., Cheng, B., Hu, Y., Zhang, Y., Zou, G.: Complexation of resveratrol with cyclodextrins: solubility and antioxidant activity. Food Chem. 113(1), 17–20 (2009). doi:10.1016/j.foodchem.2008.04.042
Sapino, S., Carlotti, M.E., Caron, G., Ugazio, E., Cavalli, R.: In silico design, photostability and biological properties of the complex resveratrol/hydroxypropyl-β-cyclodextrin. J. Incl. Phenom. Macrocycl. Chem. 63(1–2), 171–180 (2009). doi:10.1007/s10847-008-9504-7
Higuchi, T., Connors, K.A.: Phase-solubility techniques. Adv Anal Chem Instrum 4, 117–212 (1965)
Takaoka, M.J.: Of the phenolic substances of white hellebore (Veratrum grandiflorum Loes. Fil.). J. Faculty Sci. Hokkaido Imperial University 3:1–16 (1940)
Siemann, E.H., Creasy, L.L.: Concentration of the phytoalexin resveratrol in wine. Am J Eno Vitic 43, 49–52 (1992)
Baur, J.A., Sinclair, D.A.: Therapeutic potential of resveratrol: the in vivo evidence. Nat. Rev. Drug Discovery 5(6), 493–506 (2006). doi:10.1038/nrd2060
Pervaiz, S., Holme, A.L.: Resveratrol: its biologic targets and functional activity. Antioxid. Redox Signal. 11(11), 2851–2897 (2009). doi:10.1089/ARS.2008.2412
Jang, M., Cai, L., Udeani, G.O., Slowing, K.V., Thomas, C.F., Beecher, C.W., Fong, H.H., Farnsworth, N.R., Kinghorn, A.D., Mehta, R.G., Moon, R.C., Pezzuto, J.M.: Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science 275(5297), 218–220 (1997). doi:10.1126/science.275.5297.218
Fontecave, M., Lepoivre, M., Elleingand, E., Gerez, C., Guittet, O.: Resveratrol, a remarkable inhibitor of ribonucleotide reductase. FEBS Lett. 421(3), 277–279 (1998). doi:10.1016/S0014-5793(97)01572-X
Sun, N.J., Woo, S.H., Cassady, J.M., Snapka, R.M.: DNA polymerase and topoisomerase II inhibitors from Psoralea corylifolia. J. Nat. Prod. 61(3), 362–366 (1998). doi:10.1021/np970488q
Ragione, F.D., Cucciolla, V., Borriello, A., Pietra, V.D., Racioppi, L., Soldati, G., Manna, C., Galletti, P., Zappia, V.: Resveratrol arrests the cell division cycle at S/G2 phase transition. Biochem. Biophys. Res. commun. 250(1), 53–58 (1998). doi:10.1006/bbrc.1998.9263
Schneider, Y., Vincent, F., Duranton, B., Badolo, L., Gosse, F., Bergmann, C., Seiler, N., Raul, F.: Anti-proliferative effect of resveratrol, a natural component of grapes and wine, on human colonic cancer cells. Cancer Lett. 158(1), 85–91 (2000). doi:10.1016/S0304-3835(00)00511-5
Sheth, S., Jajoo, S., Kaur, T., Mukherjea, D., Sheehan, K., Rybak, L.P., Ramkumar, V.: Resveratrol reduces prostate cancer growth and metastasis by inhibiting the Akt/MicroRNA-21 pathway. PLoS One 7(12), e51655 (2012). doi:10.1371/journal.pone.0051655
Manna, S.K., Mukhopadhyay, A., Aggarwal, B.B.: Resveratrol suppresses TNF-induced activation of nuclear transcription factors NF-kappa B, activator protein-1, and apoptosis: potential role of reactive oxygen intermediates and lipid peroxidation. J Immun 164(12), 6509–6519 (2000). doi:10.4049/jimmunol.164.12.6509
Li, T., Wang, W., Chen, H., Li, T., Ye, L.: Evaluation of anti-leukemia effect of resveratrol by modulating STAT3 signaling. Int. Immunopharmacol. 10(1), 18–25 (2010). doi:10.1016/j.intimp.2009.09.009
Amri, A., Chaumeil, J.C., Sfar, S., Charrueau, C.: Administration of resveratrol: what formulation solutions to bioavailability limitations? J Control Release 158(2), 182–193 (2012). doi:10.1016/j.jconrel.2011.09.083
Boocock, D.J., Faust, G.E., Patel, K.R., Schinas, A.M., Brown, V.A., Ducharme, M.P., Booth, T.D., Crowell, J.A., Perloff, M., Gescher, A.J.: Phase I dose escalation pharmacokinetic study in healthy volunteers of resveratrol, a potential cancer chemopreventive agent. Cancer Epidemiol. Biomark. Prev. 16(6), 1246–1252 (2007). doi:10.1158/1055-9965.EPI-07-0022
Soleas, G.J., Angelini, M., Grass, L., Diamandis, E.P., Goldberg, D.M.: Absorption of trans-resveratrol in rats. Methods Enzymol. 335, 145–154 (2001). doi:10.1016/S0076-6879(01)35239-4
Athar, M., Back, J.H., Tang, X., Kim, K.H., Kopelovich, L., Bickers, D.R., Kim, A.L.: Resveratrol: a review of preclinical studies for human cancer prevention. Toxicol. Appl. Pharmacol. 224(3), 274–283 (2007). doi:10.1016/j.taap.2006.12.025
Walle, T.: Bioavailability of resveratrol. Ann. N. Y. Acad. Sci. USA 1215(1), 9–15 (2011). doi:10.1111/j.1749-6632.2010.05842.x
Burkon, A., Somoza, V.: Quantification of free and protein-bound trans-resveratrol metabolites and identification of trans-resveratrol-C/O-conjugated diglucuronides—two novel resveratrol metabolites in human plasma. Mol. Nutr. Food Res. 52(5), 549–557 (2008). doi:10.1002/mnfr.200700290
Loftsson, T., Vogensen, S.B., Brewster, M.E., Konradsdottir, F.: Effects of cyclodextrins on drug delivery through biological membranes. J. Pharm. Sci. 96(10), 2532–2546 (2007). doi:10.1002/jps.20992
Berta, G.N., Salamone, P., Sprio, A.E., Di Scipio, F., Marinos, L.M., Sapino, S., Carlotti, M.E., Cavalli, R., Di Carlo, F.: Chemoprevention of 7,12-dimethylbenz[a]anthracene (DMBA)-induced oral carcinogenesis in hamster cheek pouch by topical application of resveratrol complexed with 2-hydroxypropyl-beta-cyclodextrin. Oral Oncol. 46(1), 42–48 (2010). doi:10.1016/j.oraloncology.2009.10.007
Das, S., Lin, H.S., Ho, P.C., Ng, K.Y.: The impact of aqueous solubility and dose on the pharmacokinetic profiles of resveratrol. Pharm. Res. 25(11), 2593–2600 (2008). doi:10.1007/s11095-008-9677-1
Duarte, A., Martinho, A., Luís, Â., Figueiras, A., Oleastro, M., Domingues, F.C., Silva, F.: Resveratrol encapsulation with methyl-β-cyclodextrin for antibacterial and antioxidant delivery applications. LWT Food Sci. Technol. 63(2), 1254–1260 (2015). doi:10.1016/j.lwt.2015.04.004
Lopez-Nicolas, J.M., Rodriguez-Bonilla, P., Garcia-Carmona, F.: Cyclodextrins and antioxidants. Crit. Rev. Food Sci. Nutr. 54(2), 251–276 (2014). doi:10.1080/10408398.2011.582544
Lucas-Abellan, C., Mercader-Ros, M.T., Zafrilla, M.P., Gabaldon, J.A., Nunez-Delicado, E.: Comparative study of different methods to measure antioxidant activity of resveratrol in the presence of cyclodextrins. Food Chem. Toxicol. 49(6), 1255–1260 (2011). doi:10.1016/j.fct.2011.03.004
Gould, S., Scott, R.C.: 2-Hydroxypropyl-beta-cyclodextrin (HP-beta-CD): a toxicology review. Food Chem. Toxicol. 43(10), 1451–1459 (2005). doi:10.1016/j.fct.2005.03.007
Del Valle, E.M.M.: Cyclodextrins and their uses: a review. Process Biochem. 39(9), 1033–1046 (2004). doi:10.1016/S0032-9592(03)00258-9
Cottart, C.H., Nivet-Antoine, V., Laguillier-Morizot, C., Beaudeux, J.L.: Resveratrol bioavailability and toxicity in humans. Mol. Nutr. Food Res. 54(1), 7–16 (2010). doi:10.1002/mnfr.200900437
Loftsson, T., Brewster, M.E.: Pharmaceutical applications of cyclodextrins: effects on drug permeation through biological membranes. J. Pharm. Pharmacol. 63(9), 1119–1135 (2011). doi:10.1111/j.2042-7158.2011.01279.x
Juan, M.E., Maijo, M., Planas, J.M.: Quantification of trans-resveratrol and its metabolites in rat plasma and tissues by HPLC. J. Pharm. Biomed. Anal. 51(2), 391–398 (2010). doi:10.1016/j.jpba.2009.03.026
Jose, S., Anju, S.S., Cinu, T.A., Aleykutty, N.A., Thomas, S., Souto, E.B.: In vivo pharmacokinetics and biodistribution of resveratrol-loaded solid lipid nanoparticles for brain delivery. Int. J. Pharm. 474(1–2), 6–13 (2014). doi:10.1016/j.ijpharm.2014.08.003
Acknowledgments
This work was supported by private grants generously funded by “Ordre International des Anysetiers, Commanderie du Piemont”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Roberta Cavalli and Giovanni N. Berta have contributed equally at this work.
Rights and permissions
About this article
Cite this article
Yang, Z., Argenziano, M., Salamone, P. et al. Preclinical pharmacokinetics comparison between resveratrol 2-hydroxypropyl-β-cyclodextrin complex and resveratrol suspension after oral administration. J Incl Phenom Macrocycl Chem 86, 263–271 (2016). https://doi.org/10.1007/s10847-016-0657-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10847-016-0657-5