Abstract
A previous study reported primary macroreentrant atrial tachycardia (AT) in the left atrium (LA), including the epicardial circuit on a left atrial anterior wall (LAAW) scar, without any prior cardiac intervention (Miyazawa et al. in J Cardiovasc Electrophysiol 2019; 30: 263-264). However, determining the target for terminating macroreentrant ATs is challenging. The mapping revealed a centrifugal pattern but did not fully elucidate the AT circuit. The reentrant mechanism of these ATs was confirmed using entrainment pacing. The earliest excitation site (EES) was traditionally selected as the ablation site, typically located in healthy tissue. However, our two cases provide new insights into AT termination, including the epicardial bridge across the endocardial LAAW scar, using minimum ablation points, without the need to ablate the healthy EES.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Case presentation
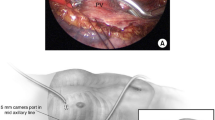
Case 1 involved an 86-year-old woman with a history of pulmonary vein isolation (PVI) admitted for the AT ablation procedure with a tachycardia cycle length (TCL) of 260 ms (Supplementary Fig. 1). The electroanatomical mapping system used was EnSite™ X EP System (Abbott, St Paul, MN, USA). The voltage map of the LA showed an endocardial scar at the center of the LAAW (Fig. 1A). The activation map showed a centrifugal pattern originating from the anterior base of the left atrial appendage (LAA) (Fig. 1B, site A) and propagated in a clockwise manner around the LAAW scar. However, we could only confirm the AT circuit at 190 ms on the endocardial map (supplementary video 1). The EES voltage was 1.4 mV, indicating healthy myocardium. Entrainment pacing from the opposite side of the EES, across the endocardial scar (Fig. 1B, site B), showed the match a postpacing interval and the TCL and the orthodromic capture of coronary sinus and right atrial septum (Fig. 1C). This finding indicated the presence of a reentrant mechanism and existence of an epicardial circuit, presumed to be located on the epicardial side of the endocardial scar. Ablation of the endocardial scar, with no potential detected, resulted in AT termination within 4 s. 3D mapping and all ablations were performed using a HD grid and a TactiCath Contact Force Ablation Catheter, Sensor Enabled (Abbott, St Paul, MN, USA), respectively. All radiofrequency (RF) energy applications were set to a maximum power of 35 W, and the target contact force (CF) was set to at least 10 g.
In case 2, a 72-year-old woman with a history of PVI and posterior wall isolation using RF catheter ablation for persistent atrial fibrillation (AF) was admitted for AT recurrence with a TCL of 225 ms (Supplementary Fig. 2). The AT in case 2 was similar to that of case 1 and was identified as an epicardial circuit (Fig. 2B, C, supplementary video 2). However, we could only confirm the AT circuit at 110 ms using an endocardial map. The EES had a voltage of 1.6 mV, indicating healthy myocardium (Fig. 2A). We assumed that the estimated epicardial circuit passed over the scar using entrainment pacing, similar to case 1. The AT terminated within 4 s after the first RF energy application targeting the endocardial scar without ablating the “healthy” EES. 3D mapping and all ablations were performed using the PentaRay multipolar mapping catheter and the Navistar Thermocool SmartTouch Surround Flow Ablation Catheter (Biosense Webster, Inc.), respectively. All RF energy applications were set to a maximum power of 35 W under the guidance of the ablation index, aiming at 550–600. The target CF value was set to at least 10 g.
In both cases, no antiarrhythmic was used at baseline since their prior PVI and recurrent AT. After AT termination, we added four or five extra ablation within scar, and no other AT was induced after the termination of AT. AT recurrence was not diagnosed in either case even though more than 6 months had been passed after ablation.
2 Discussion
Determining the target for terminating macroreentrant ATs in the LA, including the epicardial circuit on a LAAW scar, is controversial. Although Baskovski et al. reported that the strategy of endocardial EES targeting for ablation in epicardial ATs offers reliable termination with good long-term success, termination rates are not so high (63%) [1].
Yamabe et al. estimated the entrance of the circuit on the axis of the slow conduction area using the entrainment method in verapamil-sensitive AT. They reported that it could be eliminated by delivering RF energy at the estimated entrance site of the slow conduction zone [2]. Moreover, they reported that RF ablation targeting the entrance sites was superior to targeting the exit sites in reducing the number of RF deliveries and the occurrence of different ATs in verapamil-sensitive AT [3]. This suggests that the connection from the epicardial circuit to the endocardium spreads over a certain area. Moreover, epicardial fibers were confirmed using three-dimensional submillimeter diffusion tensor magnetic resonance imaging, which revealed that the epicardial fibers ran around and branched off the lateral side of the LA wall, resembling a fin [4]. In both cases, AT was immediately terminated with ablation from the assumed epicardial circuit on the epicardial side of the endocardial scar without targeting the EES.
Linear ablation and complex fractionated atrial electrogram (CFAE) ablation are well-known strategies for patients with AF requiring substrate modification in addition to PVI. In contrast, linear and CFAE ablations have been reported to be associated with a higher incidence of organized and gap-related AT [5, 6]. Wang et al. reported that about one-third of iatrogenic scar-related LAAW reentrant ATs were based on LAAW epicardial connection in LA or bi-atrial ATs [7]. These results highlight the importance of preventing unnecessary ablation of normal lesions in the atrium.
3 Conclusion
The clinical implication of our cases is that it is possible to disconnect the epicardial circuit without targeting the breakthrough point in the endocardium, thus avoiding making an iatrogenic substrate. This finding may be helpful in the ablation of AT, including the epicardial bridge across the endocardial scar on the LAAW, with the least number of RF energy application points.
References
Baskovski E, Altin AT, Akyurek O, Kuru B, Korkmaz K, Ersoy İ, Kozluca V, Akbulut IM, Tutar E. Electrophysiological characteristics of epicardial atrial tachycardias and endocardial breakthrough site targeting for ablation: a single center experience. J Interv Card Electrophysiol. 2023. https://doi.org/10.1007/s10840-023-01513-z.
Yamabe H, Okumura K, Morihisa K, Koyama J, Kanazawa H, Hoshiyama T, Ogawa H. Demonstration of anatomical reentrant tachycardia circuit in verapamil-sensitive atrial tachycardia originating from the vicinity of the atrioventricular node. Heart Rhythm. 2012;9:1475–83.
Yamabe H, Kajiyama K, Soejima T, Fukami Y, Haraguchi K, Okonogi T, Hirai K, Fukuoka R, Orita Y, Umeji K, Koga H, Kawasaki T. Comparison of the catheter ablation outcome in patients between targeting the entrance and exit of the reentry circuit in verapamil-sensitive atrial tachycardia originating from the atrioventricular-node vicinity. Heart Vessel. 2021;36:1201–11.
Pashakhanloo F, Herzka DA, Ashikaga H, Mori S, Gai N, Bluemke DA, Trayanova NA, McVeigh ER. Myofiber architecture of the human atria as revealed by submillimeter diffusion tensor imaging. Circ Arrhythm Electrophysiol. 2016;9:e004133.
Sawhney N, Anousheh R, Chen W, Feld GK. Circumferential pulmonary vein ablation with additional linear ablation results in an increased incidence of left atrial flutter compared with segmental pulmonary vein isolation as an initial approach to ablation of paroxysmal atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3:243–8.
Wong KC, Paisey JR, Sopher M, Balasubramaniam R, Jones M, Qureshi N, Hayes CR, Ginks MR, Rajappan K, Bashir Y, Betts TR. No benefit of complex fractionated atrial electrogram ablation in addition to circumferential pulmonary vein ablation and linear ablation: benefit of complex ablation study. Circ Arrhythm Electrophysiol. 2015;8:1316–24.
Wang H, Xi S, Chen J, Gan T, Huang W, He B, Zhao L. Left atrial anterior wall scar-related atrial tachycardia in patients after catheter ablation or cardiac surgery: electrophysiological characteristics and ablation strategy. J Cardiovasc Dev Dis. 2022;9:249.
Author information
Authors and Affiliations
Contributions
Shota Tamura: drafting the article,
Kenji Shimeno: the conception and design of the study,
Yusuke Hayashi: revising it critically for important intellectual content,
Takahiko Naruko: revising it critically for important intellectual content,
Daiju Fukuda: final approval of the version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective article of case reports is not subject to informed consent by the participants..
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Activation map with a Sparkle map in case 1 (MP4 2357 kb)
Activation map with a Ripple map in case 2 (MP4 4358 kb)

Supplementary Figure 1
Electrocardiogram before second procedure in case 1 (PNG 707 kb)

Supplementary Figure 2
Electrocardiogram before second procedure in case 2 (PNG 689 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tamura, S., Shimeno, K., Hayashi, Y. et al. Effective ablation of atrial tachycardia with an epicardial circuit—insights from endocardial scars sites: a case study. J Interv Card Electrophysiol 67, 1–3 (2024). https://doi.org/10.1007/s10840-023-01687-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-023-01687-6