Abstract
Purpose
First-line catheter ablation of ventricular tachycardia/ventricular fibrillation (VT/VF) in patients with ischemic cardiomyopathy (ICM) has been associated with improved outcomes; however, most benefit seems to be in patients with moderately depressed left ventricular ejection fraction (LVEF). Herein, outcomes were stratified based on LVEF.
Methods
A meta-analysis of randomized controlled trials (RCTs) evaluating first-line ablation versus medical therapy in patients with VT and ICM was performed. Risk estimates and 95% confidence intervals (CI) were measured.
Results
Four RCTs with a total of 505 patients (mean age 66 ± 9 years, 89% male, 80% with previous revascularization) were included. Mean LVEF was 35 ± 8%. At a mean follow-up of 24 ± 9 months, a significant benefit in survival-free from appropriate implantable cardioverter-defibrillator (ICD) therapies was observed in all patients undergoing first-line catheter ablation compared with medical management (RR 0.70, 95% CI 0.56–0.86). In patients with moderately depressed LVEF (> 30–50%), first-line VT ablation was associated with a statistically significant reduction in the composite endpoint of survival free from VT/VF and appropriate ICD therapies (HR 0.52, 95% CI 0.36–0.76), whereas there was no difference in patients with severely depressed LVEF (≤30%) (HR 0.56, 95% CI 0.24–1.32). Funnel plots did not show asymmetry suggesting lack of bias.
Conclusions
Patients with ICM and VT undergoing first-line ablation have a significantly lower rate of appropriate ICD therapies without a mortality difference compared with patients receiving an initial approach based on medical therapy. The beneficial effect of a first-line ablation approach was only observed in patients with moderately depressed LVEF (> 30–50%).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
In patients with ischemic cardiomyopathy (ICM), ventricular tachycardia and ventricular fibrillation (VT/VF) typically originate from a relatively discrete portion of the myocardium, within or bordering the infarct zone that is amenable to catheter ablation [1]. However, the mainstay of treatment for these patients is typically based on medical therapy and implantable cardioverter defibrillators (ICDs) [2]. Use of anti-arrhythmic drugs (AAD) is typically the first approach as an adjunctive therapy to reduce ICD interventions; yet, success is limited and may be associated with significant drug-related adverse events [3]. Conversely, catheter ablation has emerged as an important therapeutic strategy for VT/VF with the advent of improved mapping technologies and ablation strategies, particularly the success seen with substrate based approaches [4]. As such, randomized controlled trials (RCTs) have shown improved outcomes in patients undergoing first-line catheter ablation for VT in patients with ICM [5, 6]. However, increased early mortality has been reported in patients with severely depressed left ventricular ejection fraction (LVEF), whereas outcomes in moderately depressed LVEF seem different [7]. Herein, we characterized outcomes based on LVEF of patients with ICM presenting with VT undergoing first-line VT ablation compared with an initial approach based on medical therapy.
2 Methods
2.1 Search strategy
We searched PubMed, Embase, and Cochrane Central Register of Clinical Trials (Cochrane Library, Issue 5, 2020) to identify studies evaluating the outcomes of patients with prior myocardial infarction that presented with VT were randomized to first-line therapy with catheter ablation or medical therapy. We used the terms (“ventricular tachycardia” OR “VT” OR “ventricular fibrillation” OR “VF” OR “ventricular tachyarrhythmia”) AND (“ischemic cardiomyopathy” OR “ICM” OR “myocardial infarction” OR “MI”) AND (“catheter ablation” OR “CA” OR “radiofrequency ablation”). Our search was restricted to human studies, published in peer-reviewed journals up to May 2020. No language restriction was applied. The reference lists of identified articles were also reviewed. We also searched clinicaltrials.gov to identify ongoing and unpublished trials.
2.2 Selection criteria
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting systematic reviews and meta-analyses was applied to the methods of this study. Studies with the following characteristics were considered eligible for this analysis: (a) had a randomized controlled design, (b) included patients with prior myocardial infarction and VT, (c) reported outcomes stratified by LVEF, (d) included patients that were randomized to first-line VT ablation or a control group based on medical therapy as an initial therapy, (e) patients were followed for an average duration of at least 12 months, and (f) reported survival-free from VT/VF and/or rates of appropriate ICD therapies as their endpoints.
2.3 Study outcomes
2.3.1 Primary outcome
The primary outcomes were (1) all-cause mortality, (2) appropriate ICD therapies, and (3) adverse events in all the patients included.
2.3.2 Secondary outcomes
The secondary outcomes were (1) composite of survival-free from VT/VF and appropriate ICD therapies in patients with moderately depressed LVEF (> 30–50%) and (2) composite of survival-free from VT/VF and appropriate ICD therapies in patients with severely depressed LVEF (≤30%).
2.4 Sensitivity analysis
Sensitivity analyses were performed for the secondary endpoints, considering the composite nature of the outcomes, using the leave-one-study-out method in order to address the influence of each study by testing whether deleting each individually would significantly change the pooled results of the meta-analysis. Additionally, chronological cumulative analyses were used to test whether the effect size and precision would shift based on technical advancement of mapping technology and ablation strategies.
2.5 Data extraction and quality assessment
Two investigators (D.F.B and J.R) independently screened all titles and abstracts and manually searched the full text versions of all pertinent studies that fulfilled the inclusion criteria. References of the relevant studies were independently reviewed for potential identification of further studies. Two investigators (D.F.B and J.R) independently assessed the quality items. Disagreements were resolved by consensus. Quality assessment of all included studies was done by using the 6 domains of the Cochrane tool for assessing risk for bias of RCTs.
2.6 Statistical analysis
Hazard ratios (HR) or Mantel–Haenszel (MH) risk ratio (RR) models and 95% confidence intervals (CI) were used to summarize data across treatment arms. The Cochran Q-test and the Higgins I-squared (I2) statistic were used for heterogeneity testing; in cases of heterogeneity (defined as I2 > 25%), random effects models of DerSimonian and Laird were used; otherwise (I2 < 25%) fixed effects models were used. To address publication bias, we used the funnel plots. If any bias was observed, further bias quantification was measured using the Begg-Mazumdar test, Egger test, and the Duval and Tweedie’s trim and fill test.
Descriptive statistics are presented as means and standard deviations (SD) for continuous variables or number of cases (n) and percentages (%) for dichotomous and categorical variables. Number needed to treat (NNT) was calculated. Statistical analysis was performed in line with recommendations from the Cochrane Collaboration and the PRISMA guidelines, using Review Manager (RevMan) (Computer program) Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014, and the Comprehensive Meta-Analysis Software version 2.0 (Biostat, Inc).
3 Results
3.1 Qualitative analysis
3.1.1 Study selection
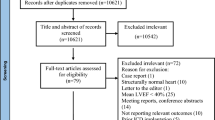
We screened 455 abstracts, out of which 12 full-text articles were retrieved and reviewed for possible inclusion based on inclusion criteria. Ultimately, four studies fulfilled the inclusion criteria and were analyzed. Flow chart of the literature review is illustrated in Fig. 1.
3.1.2 Baseline characteristics
The baseline characteristics of the patients included in this meta-analysis are reported in Table 1. A total of 505 patients (mean age 66 ± 9 years, 89% males) were analyzed. The mean duration of follow-up was 24 ± 9 months. The use of AADs was similar in both groups during the first 12 months of follow-up (mean AAD use was 21% in the first-line ablation group vs. 20% in controls). All the studies evaluated an endocardial-only ablation approach. Previous revascularization with percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass grafting (CABG) was performed in 80% of patients. Mean duration since last MI was 10 ± 9 years. Mean LVEF was 35 ± 8%, and 84% of patients were on beta-blockers. Table 2 illustrates a summary of the included studies.
3.2 Quantitative analysis
3.2.1 Primary endpoints
A significant benefit was observed with first-line catheter ablation compared with medical management in survival-free from appropriate ICD therapies, with a 30% relative risk reduction and 14% absolute risk reduction when compared with the medical treatment group (RR 0.70, 95% CI 0.56–0.86) (Fig. 2). There was no difference in all-cause mortality (RR 0.98, 95% CI 0.52–1.82) and in adverse events between both treatment strategies (RR 1.51, 95% CI 0.89–2.54) (Supplemental Fig. 1).
Survival-free from VT/VF and from appropriate ICD therapies in patients with ICM presenting with VT undergoing first-line catheter ablation compared with medical management. a Survival-free from appropriate ICD therapies in all patients. b Survival-free from VT/VF in patients with moderately depressed LVEF (> 30–50%). ICD implantable-cardioverter defibrillator, ICM ischemic cardiomyopathy, VF ventricular fibrillation, VT ventricular tachycardia
3.2.2 Secondary endpoints
In patients with moderately depressed LVEF (> 30–50%), survival-free from VT/VF in patients who underwent first-line catheter ablation was 56% vs. 45% in those receiving conservative treatment. A significant benefit of survival-free from VT/VF was observed with first-line catheter ablation, with a 44% relative risk reduction and 11% absolute risk reduction when compared with the medical treatment group (HR 0.56, 95% CI 0.38–0.83) (Fig. 2).
First-line VT ablation was associated with a statistically significant reduction in the composite endpoint of survival-free VT/VF and appropriate ICD therapies in patients with moderately reduced LVEF (HR 0.52, 95% CI 0.36–0.76) (Fig. 3). In patients with severely depressed LVEF (≤30%), first-line VT ablation was not associated with a reduction in the composite endpoint of survival-free VT/VF and appropriate ICD therapies (HR 0.56, 95% CI 0.24–1.32) (Fig. 3).
Forest plot reporting the hazard ratio illustrating the composite endpoint of survival-free VT/VF and appropriate ICD therapies in patients with ICM presenting with VT undergoing first-line catheter ablation compared with conservative treatment. a Patients with moderately depressed LVEF (> 30–50%). b Patients with severely depressed LVEF (≤30%). Diamond indicates overall summary estimates for the analysis: width of the diamond represents 95% CI; width of the shaded square represents the size of the population (fixed effects model was used in the analysis). CI confidence interval, ICM ischemic cardiomyopathy, VF ventricular fibrillation, VT ventricular tachycardia
3.3 Sensitivity analysis
Sensitivity analysis for the secondary endpoints involving the removal of each of the studies sequentially demonstrated that if some of the studies were removed from the analysis, the summary risk estimates for the composite survival-free VT/VF and appropriate ICD therapies was not influenced making the overall results significant (Fig. 4). The chronologic cumulative analysis for each outcome before inclusion of all studies in the final effect summary did not have a significant impact in the overall final effect (oldest RCT from 2007 and most recent in 2020) (Fig. 4).
Forest plots reporting the sensitivity analysis for the secondary endpoint: a leave-one-study-out method for moderately depressed LVEF; b leave-one-study-out method for severely depressed LVEF; c chronological cumulative analysis for moderately depressed LVEF; d chronological cumulative analysis for severely depressed LVEF. Diamond indicates overall summary estimate for the analysis (width of the diamond represents the 95% CI); width of the shaded square, size of the population. CI confidence interval, ICD implantable-cardioverter defibrillator, ICM ischemic cardiomyopathy, LVEF left ventricular ejection fraction, VF ventricular fibrillation, VT ventricular tachycardia
3.4 Number needed to treat
The absolute difference in event rates yielded an NNT of 10 patients in order to improve survival-free from VT/VF in those with moderately depressed LVEF.
3.5 Quality assessment and publication bias
Funnel plots did not show asymmetry, suggesting lack of bias for any outcome (Supplemental Fig. 2). A graph and summary of the tools recommended by the Cochrane Collaboration for the risk of bias (selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias) identified in each individual RCT is shown in Fig. 5.
4 Discussion
In patients with ICM, VT/VF is a major cause of morbidity and mortality. Thus, strategies to minimize arrhythmia burden in these patients is essential. Our study, which included 505 patients enrolled in RCTs, with a mean follow-up duration of 24 ± 9 months, showed that patients with ICM presenting with VT/VF, first-line catheter ablation have a significantly lower rate of recurrent appropriate ICD therapies compared with patients receiving an initial approach based on medical therapy (RR 0.70, 95% CI 0.56–0.86). However, this benefit was only significant in the subgroup of patients with moderately depressed LVEF (> 30–50%) (HR 0.52, 95% CI 0.36–0.76) compared with patients with severely depressed LVEF (≤30%) (HR 0.56, 95% CI 0.24–1.32). Only RCTs were included in this meta-analysis to minimize bias considering the nature of the research question involving the evaluation of 2 specific interventions in a specific sub-group of patients.
In patients implanted with secondary prevention ICDs, shocks have been reported in up to ~ 39% of patients within the first year of implantation [3]. Recurrent ICD shocks may cause deterioration of heart failure, increase hospitalization rates, and have been associated with increased mortality [8]. The SCD-HeFT trial noted that a single appropriate ICD shock increased patient mortality-risk up to five-fold [8]. Shocks with their potential to worsen HF also tend to alter mode of mortality in the direction of non-arrhythmic death, thereby, offsetting the arrhythmic mortality advantage offered by ICDs [9]. Moreover, they do not alter the underlying pathological substrate and do not prevent VT. Therefore, it is important to adopt a strategy that reduces the absolute incidence of VT/VF, and as such, subsequent ICD shocks. Utilization of AADs and ICD reprogramming has been employed with moderate degrees of success [3]. Accordingly, the VANISH trial demonstrated that there was a significantly lower rate of the composite primary outcome of death, VT storm, or appropriate ICD shock among patients undergoing catheter ablation than among those receiving an escalation in AAD (HR 0.72, 95% CI 0.53 to 0.98; p = 0.04) [10].
In patients with ICM, VT usually arises from a fairly distinct region of the myocardium, within or neighboring the scar tissue. This scar tissue is comprised of non-excitable fibrous material, with islands of surviving myocytes composing the substrate for VT. A general physiology seems to be common in patients with ICM and sustained monomorphic VT, characterized by larger endocardial lower voltage zones, more frequent fractionated, very late voltage potentials as compared with patients with a similar profile without VT [11]. Nonetheless, scars are not homogenous considering tissue characteristics can be variable in each patient depending largely on the infarct type (i.e., size, location, revascularization time) posing a challenge for the treatment of VT/VF. Therefore, is not surprising that ablation studies have shown variable results reflecting conservative guideline recommendations. Guidelines recommend VT ablation as a Class I indication in patients with prior MI, only with recurrent episodes of symptomatic sustained VT, or VT storm, and have failed or are intolerant to AADs [2]. However, this recommendation may not apply to every patient, as there seems to be a significant benefit in different subgroups of patients including those undergoing early ablation and preserved LVEF [12]. In general, a lower threshold to consider catheter ablation of VT (whether it is determined by failure of 1 AAD or immediately after a VT episode) could be associated with a favorable outcome [12]. Furthermore, data from the International VT Ablation Center Collaborative Group reported higher rates of both VT recurrence and mortality in patients with lower EF and higher NYHA status [13]. In contrast, ICM and higher EF (> 30%) were associated with lower probability of VT recurrence that was reflected in improved transplant-free survival compared with those with VT recurrence (93% vs. 89%, adjusted HR 3.190 (1.517–6.707); p = 0.002) [13].
Four randomized controlled trials have assessed the impact of first-line VT catheter ablation in the setting of ICM [5, 6, 14, 15]. SMASH VT and VTACH trials showed improved outcomes with first-line VT ablation in patients with ICM presenting with VT [5, 6]. However, the SMS and the recently published BERLIN VT trial showed opposite results [14, 15]. As expected, all of these trials had methodological differences but the major approach studied is homogenous, considering the use of first-line VT ablation in each of them and a medication-based approach in the control groups. In terms of the control groups, AADs were used in 31% of patients in the VTACH study, 22% in SMS, and 28% in BERLIN VT at 1-year follow-up, while no AADs were used in SMASH VT [5, 6, 14, 15]. All control groups were medications based except in the BERLIN VT trial, where patients were randomized to receive ablation after the third appropriate ICD shock [15]. Ultimately, 10 patients (12%) received ablation in this group, which is perhaps one of the reasons the trial showed no benefit in the ablation group [15]. They showed that first-line VT ablation did not reduce the combined endpoint of mortality or hospitalization for arrhythmia or worsening heart failure during 1 year of follow-up when compared with the deferred ablation strategy (HR 1.09, 95% CI 0.62–1.92; p = 0.77) [15]. Perhaps the study power, patient cross-over, and endocardial-only ablation strategy were not enough to demonstrate a significant clinical benefit of ablation. VT circuits in ICM are generally thought to have a subendocardial location, easily accessible, and targeted with endocardial mapping and ablation [16]. However, 34–75% of ICM patients may exhibit epicardial substrate, as confirmed by magnetic resonance imaging in post-infarct animal models [17]. This may explain why a combined endocardial-epicardial ablation has been shown to be beneficial in ICM. We recently published a meta-analysis with 17 studies including 975 patients [18]. After a mean follow-up of 27 months, endocardial-epicardial ablation was associated with a 35% reduction in risk of VT recurrence compared with endocardial ablation alone (RR 0.65, 95% CI 0.55 to 0.78; p < 0.001). Sensitivity analysis showed lower risk of VT recurrence in ICM (RR 0.43, 95% CI 0.28 to 0.67; p = 0.0002) with a nonsignificant trend in NICM (RR 0.87, 95% CI 0.70 to 1.08; p = 0.20). More importantly, an endocardial-epicardial approach was associated with reduced all-cause mortality (RR 0.56, 95% CI 0.32 to 0.97; p = 0.04), particularly in patients with ICM [18]. As such, perhaps early ablation using an endocardial-epicardial strategy in patients with LVEF > 30–50% could be the most beneficial therapeutic strategy.
Despite the mixed results from the four RCTs evaluating this concept, our results substantiate the use of VT ablation as a first-line approach in this population to improve survival-free from VT/VF, which may also have a positive impact from a healthcare resource utilization standpoint [19]. Multiple clinical studies are currently underway aiming to address the best therapeutic approach of these patients: Does Timing of VT ablation Affect Prognosis in Patients with an ICD? (PARTITA) (NCT01547208), Pan-Asia United States PrEvention of Sudden Cardiac Death Catheter Ablation Trial (PAUSE-SCD) (NCT02848781), and The Antiarrhythmics or Ablation for Ventricular Tachycardia 2 (VANISH 2) Study (NCT02830360).
4.1 Limitations
Our meta-analysis has several limitations, which should be taken into account while interpreting the results. Only a small number of studies have assessed the impact of first-line VT ablation in patients with ICM, and the data available to stratify outcomes based on LVEF is limited; hence, the necessity to assess a composite endpoint. Also, techniques for VT mapping and ablation differed among the studies. Our results are applicable only to patients with ICM, and should not be generalized to NICM.
5 Conclusion
Patients with ICM presenting with VT undergoing first-line VT ablation have a significant lower rate of appropriate ICD therapies without a mortality difference compared with patients receiving an initial approach based on medical therapy. The beneficial effect of a first-line ablation approach in improved survival-free from VT/VF and appropriate ICD therapies was seen only in patients with moderately depressed LVEF. First-line VT ablation should be considered the therapeutic approach of choice in this selected group of patients to improve clinical outcomes.
Data availability
Available upon request.
References
de Bakker JM, van Capelle FJ, Janse MJ, Wilde AA, Coronel R, Becker AE, et al. Reentry as a cause of ventricular tachycardia in patients with chronic ischemic heart disease: electrophysiologic and anatomic correlation. Circulation. 1988;77:589–606.
Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Heart Rhythm. 2020;17:e2–e154.
Connolly SJ, Dorian P, Roberts RS, Gent M, Bailin S, Fain ES, et al. Comparison of beta-blockers, amiodarone plus beta-blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC study: a randomized trial. JAMA. 2006;295:165–71.
Briceno DF, Romero J, Villablanca PA, et al. Long-term outcomes of different ablation strategies for ventricular tachycardia in patients with structural heart disease: systematic review and meta-analysis. Europace. 2018;20:104–15.
Reddy VY, Reynolds MR, Neuzil P, Richardson AW, Taborsky M, Jongnarangsin K, et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007;357:2657–65.
Kuck KH, Schaumann A, Eckardt L, Willems S, Ventura R, Delacrétaz E, et al. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): a multicentre randomised controlled trial. Lancet. 2010;375:31–40.
Santangeli P, Frankel DS, Tung R, Vaseghi M, Sauer WH, Tzou WS, et al. Early mortality after catheter ablation of ventricular tachycardia in patients with structural heart disease. J Am Coll Cardiol. 2017;69:2105–15.
Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359:1009–17.
Hohnloser SH, Kuck KH, Dorian P, Roberts RS, Hampton JR, Hatala R, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med. 2004;351:2481–8.
Sapp JL, Wells GA, Parkash R, Stevenson WG, Blier L, Sarrazin JF, et al. Ventricular tachycardia ablation versus escalation of antiarrhythmic drugs. N Engl J Med. 2016;375:111–21.
Haqqani HM, Kalman JM, Roberts-Thomson KC, Balasubramaniam RN, Rosso R, Snowdon RL, et al. Fundamental differences in electrophysiologic and electroanatomic substrate between ischemic cardiomyopathy patients with and without clinical ventricular tachycardia. J Am Coll Cardiol. 2009;54:166–73.
Romero J, Di Biase L, Diaz JC, et al. Early versus late referral for catheter ablation of ventricular tachycardia in patients with structural heart disease: a systematic review and meta-analysis of clinical outcomes. JACC Clin Electrophysiol. 2018;4:374–82.
Tung R, Vaseghi M, Frankel DS, Vergara P, Di Biase L, Nagashima K, et al. Freedom from recurrent ventricular tachycardia after catheter ablation is associated with improved survival in patients with structural heart disease: an international VT ablation center collaborative group study. Heart Rhythm. 2015;12:1997–2007.
Kuck KH, Tilz RR, Deneke T, Hoffmann BA, Ventura R, Hansen PS, et al. Impact of substrate modification by catheter ablation on implantable cardioverter-defibrillator interventions in patients with unstable ventricular arrhythmias and coronary artery disease: results from the multicenter randomized controlled SMS (substrate modification study). Circ Arrhythm Electrophysiol. 2017;10:e004422. https://doi.org/10.1161/CIRCEP.116.004422.
Willems S, Tilz RR, Steven D, Kääb S, Wegscheider K, Gellér L, et al. Preventive or deferred ablation of ventricular tachycardia in patients with ischemic cardiomyopathy and implantable defibrillator (BERLIN VT): a multicenter randomized trial. Circulation. 2020;141:1057–67.
Tschabrunn CM, Roujol S, Nezafat R, Faulkner-Jones B, Buxton AE, Josephson ME, et al. A swine model of infarct-related reentrant ventricular tachycardia: electroanatomic, magnetic resonance, and histopathological characterization. Heart Rhythm. 2016;13:262–73.
Arenal A, Perez-David E, Avila P, et al. Noninvasive identification of epicardial ventricular tachycardia substrate by magnetic resonance-based signal intensity mapping. Heart Rhythm. 2014;11:1456–64.
Romero J, Cerrud-Rodriguez RC, Di Biase L, et al. Combined endocardial-epicardial versus endocardial catheter ablation alone for ventricular tachycardia in structural heart disease: a systematic review and meta-analysis. JACC Clin Electrophysiol. 2019;5:13–24.
Winterfield JR, Kent AR, Karst E, Dalal N, Mahapatra S, Bunch TJ, et al. Impact of ventricular tachycardia ablation on health care utilization. Heart Rhythm. 2018;15:355–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Di Biase is a consultant for Biosense Webster, Boston Scientific, and St. Jude Medical and has received speaker honoraria/travel from Medtronic, Atricure, EPiEP, and Biotronik. Dr. Natale is a consultant for Biosense Webster, Stereotaxis, and St. Jude Medical and has received speaker honoraria/travel from Medtronic, Atricure, EPiEP, Biotronik, and Janssen. The remaining authors report no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 7130 kb)
Rights and permissions
About this article
Cite this article
Briceño, D.F., Romero, J., Patel, K. et al. First-line ablation of ventricular tachycardia in ischemic cardiomyopathy: stratification of outcomes by left ventricular function. J Interv Card Electrophysiol 62, 391–400 (2021). https://doi.org/10.1007/s10840-020-00912-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00912-w