Abstract
Purpose
Point-by-point radiofrequency (RF) ablation has been the cornerstone of pulmonary vein isolation (PVI) for patients with atrial fibrillation (AF); however, it remains a complex and time-consuming procedure. Many novel AF catheter ablation (CA) techniques have been introduced, but whether they represent valuable alternatives remains controversial. Thus, we conducted a network meta-analysis to comprehensively evaluate the efficacy and safety of different CA interventions.
Methods
We systematically searched several databases (Embase, PubMed, the Cochrane Library, and ClinicalTrials.gov) from inception to March, 2020. The primary outcomes of interest were freedom from atrial tachyarrhythmia (AT) and procedure-related complications; secondary outcomes included procedure time and fluoroscopy time.
Results
Finally, 33 randomized controlled trials (RCTs) with a total of 4801 patients were enrolled. No significant differences were found among the different interventions in terms of primary efficacy or safety outcomes. PVAC was most likely to have the shortest procedure time (Prbest = 61.5%) and nMARQ the shortest fluoroscopy time (Prbest = 60.6%); compared with conventional irrigated RF (IRF) ablation, cryoballoon ablation (CBA) showed comparable clinical efficacy and safety; CBA with second-generation CB (CB2) had a significantly shorter procedure time than IRF with contact force technology (CF-IRF) (WMD = − 20.75; p = 0.00).
Conclusion
There is insufficient evidence to suggest that one CA technique is superior to another. However, PVAC may be associated with a shorter procedural duration, and the CB2 catheters also seemed to reduce the procedure time compared with that of CF-IRF. Further large-scale studies are warranted to compare the available CA techniques and provide an up-to-date optimum recommendation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
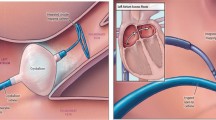
Atrial fibrillation (AF) is the most common cardiac arrhythmia and is independently associated with an increased risk of stroke, heart failure, and cardiovascular morbidity [1]. Catheter ablation (CA) has been recommended for patients with symptomatic AF refractory to antiarrhythmic drugs, with pulmonary vein isolation (PVI) being the cornerstone of ablation procedures [2]. Point-by-point radiofrequency (RF) ablation has been applied to achieve PVI since 1998, and the success rate has approximately been 70% for patients with paroxysmal AF (PAF) after the first procedure [3]. Although point-by-point RF has been the cornerstone of CA and is widely used, it still remains a complex and time-consuming procedure and is highly operator dependent.
In recent years, several novel AF ablation techniques, mainly “single-shot-systems,” have emerged, including the balloon-based techniques such as cryoablation ablation (CBA), hot balloon ablation (HBA), and laser balloon ablation (LBA); non-balloon multielectrode RF techniques such as nMARQ, mesh ablator (MA), and pulmonary vein ablation catheter (PVAC); and the high-power short-duration ablation technique. All of the alternative techniques intend to simplify the PVI procedure and reduce radiation exposure.
Although a number of studies have been performed to evaluate their efficacy and safety of these techniques, whether they represent valuable alternatives to the conventional irrigated RF (IRF) ablation remains controversial. Thus, we performed this network meta-analysis to assess the efficacy and safety of different CA intervention techniques based on the evidence from randomized controlled trials (RCTs).
2 Materials and methods
2.1 Search strategy and selection criteria
PubMed, Embase, the Cochrane Library, and ClinicalTrials.gov were systematically searched from their date of inception to March, 2020. The following terms and variants thereof were used: “atrial fibrillation,” “cryoablation,” “radiofrequency,” “multi-electrode,” “laser balloon,” “hot balloon,” and “high-power ablation.” The references of the selected articles and relevant reviews were further reviewed for potentially relevant studies. To be included in our research, the studies were required to meet the following criteria: (1) RCTs, (2) published as a full-text article in English, (3) comparison between different CA interventions for AF patients, and (4) the outcomes of interest were reported.
2.2 Data collection and quality assessment
Data extraction and a quality assessment were performed independently by two investigators, and discrepancies were resolved by discussion and consensus. The following data were extracted: patients number, type of AF, participant characteristics, interventional strategy, duration of follow-up, and outcomes of interest. The quality of the included studies was assessed using the Cochrane Collaboration tool [4].
2.3 Primary and secondary outcomes
The primary efficacy outcome of interest was freedom from atrial tachyarrhythmia (AT) and without the administration of antiarrhythmic drugs (AADs) during follow-up. The primary safety outcome of interest was procedure-related complications. Secondary outcomes included procedure time and fluoroscopy time.
2.4 Statistical analysis
Continuous variables were described as median and standard deviation (SD) and categorical variables as n (%). For a conventional pairwise meta-analysis, STATA version 12.0 (STATA Corporation, TX, USA) was applied. The odds ratio (OR) and weighted mean difference (WMD) were calculated to demonstrate the overall result. The chi-square test was applied to estimate the heterogeneity across studies, and I2 > 50% was considered indicative of significant heterogeneity. If there was significant heterogeneity, the possible causes were investigated and a random effects model was applied; otherwise, a fixed effects model was used. The publication bias for the pairwise meta-analysis was analyzed graphically with funnel plots and statistically using Egger’s and Begg’s tests.
For indirect and mixed comparisons, a Bayesian network meta-analysis was performed using R version 3.6.2 with R2WINBUGS and GeMTC packages computing OR or MD and their 95% credible intervals (CrIs). Markov chain Monte Carlo (MCMC) simulations were applied to estimate posterior probabilities with Gibbs sampling from at least 100,000 iterations. The probability of being the best treatment (Prbest) was estimated and ranked for each intervention. The node-splitting method was applied to assess network inconsistency.
3 Results
3.1 Eligible studies and characteristics
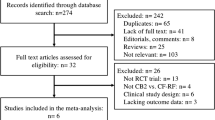
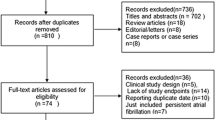
Thirty-three RCTs with a total of 4801 patients were finally included in this meta-analysis (Fig. 1). Six CA intervention strategies were evaluated, including conventional IRF, two kinds of balloon-based ablation strategies (CBA and LBA), two nonballoon multielectrode technologies (PVAC and nMARQ) and one basket-based technology (MA). There were no studies that meet the inclusion criteria for other CA strategies, such as hot balloon ablation or high-power ablation.
The baseline characteristics of the included studies are outlined in Table 1. Briefly, across the trials,15 studies compared CBA with IRF [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]; 2 studies compared CBA with MA [20, 21]; one study compared CBA with PVAC [22]; 7 studies compared PVAC with IRF [23,24,25,26,27,28,29]; 2 studies compared nMARQ with PVAC [30, 31]; one study compared nMARQ with IRF [32]; 3 studies compared LBA with IRF [33,34,35]; and 2 studies compared three interventions, including CBA, IRF, and LBA [36, 37]. The mean age of the patients ranged from to 52 to 67.5 years. Eight studies included both patients with paroxysmal AF (PAF) and persistent AF (PerAF) [8, 12, 18, 22, 27, 28, 30, 34], and the rest included only patients with PAF.
According to the Cochrane Collaboration tool [4], none of the included trials were thought to have a definite high risk of bias, and the study quality was adequate in most cases (Supplement Table 1). No significant publication bias was found with the funnel plot (Supplement Fig. 1) or revealed by the Begg’s and Egger’s tests based on the primary efficacy outcome of freedom from AT (Begg’s test: p = 0.556, Egger’s test: p = 0.062).
3.2 Primary endpoints
A pairwise meta-analysis was first performed, and results demonstrated that there were no significant differences among different interventions in terms of freedom from AT (comparisons including CBA vs. IRF, CBA vs. PVAC, CBA vs. MA, PVAC vs. IRF, nMARQ vs. PVAC, LBA vs. IRF, LBA vs. CBA, p > 0.05 for all). However, significant heterogeneity was detected for the comparison between CBA and IRF (I2 = 74.7%) (Fig. 2). Another pairwise meta-analysis was also conducted in terms of procedure-related complications; no significant difference was found among interventions, and no significant heterogeneity was detected (Fig. 3).
Further sensitivity analyses were conducted for the comparison for CBA vs. IRF depending on the type of cryoballoon/IFA catheter (first or second generation cryoballoon/with or without contact force technology) and type of AF patient (PAF or PerAF). The results showed that there were also no significant differences between CBA and IRF in terms of freedom from AT and complications when only patients with PAF were enrolled and analyzed (Supplement Fig. 2). There were also no significant differences between the second-generation cryoballoon (CB2) and contact force IRF (CF-IRF) or the first-generation cryoballoon (CB1) and no contact force IRF (nCF-IRF) regarding the primary endpoints (Supplement Fig. 3).
We then conducted a network meta-analysis to compare the six interventions (Fig. 4). The results indicated that LBA was most likely to be the best treatment for achieving the freedom from AT (Prbest = 36.7%), and nMARQ was most likely associated with the fewest procedure-related complications (Prbest = 76.1%). Both LBA and CBA had significantly more complications than both nMARQ (OR = 7.5 (95% CrCls, 1.0–72); OR = 7.2 (95% CrCls, 1.1–54); p < 0.05, respectively) and PVAC (OR = 3.9 (95% CrCls, 1.1–18); OR = 3.7 (95% CrCls, 1.3–12); p < 0.05, respectively (Tables 2 and 3). Consistency of the network analyses was satisfactory as the results from consistent and inconsistent Bayesian models were similar.
Network of comparisons included in the analyses. The size of every circle is proportional to the number of randomly assigned patients and indicates the sample size. The thickness of the line corresponds to the number of trials. LBA, laser balloon ablation; nMARQ, nMARQ ablation; CBA, cryoballoon ablation; PVAC, pulmonary vein ablation catheter; IRF, irrigated radiofrequency ablation; MA, mesh ablator
3.3 Secondary endpoints
The pairwise meta-analysis showed that there were no significant differences between CBA and IRF concerning procedure or fluoroscopy time (WMD = − 8.55 min, p = 0.131; WMD = 2.51 min, p = 0.259, respectively), whereas significant heterogeneities were detected (I2 = 93.5 and 94.5%, respectively). Further analysis found that CBA with CB2 had a significantly shorter procedure time than CF-IRF (WMD = − 20.75 (95% CI, − 25.44 to − 16.06); p = 0.00), whereas no such difference was seen between CB1 and nCF-IRF (p = 0.95).
In terms of fluoroscopy time, there were no significant differences between CB2 and CF-IRF or CB1 and nCF-IRF (p > 0.05) (Supplement Fig. 3). PVAC had significantly both shorter procedure and fluoroscopy times compared with IRF (WMD = − 58.59 (95% CI, − 75.16 to − 42.02); p = 0.00 and WMD = − 9.58 (95% CI, − 16.82 to −2.34); p = 0.01, respectively).
In the comparison between different multielectrode technologies, nMARQ had shorter procedure and fluoroscopy times than PVAC (WMD = − 13.86 (95% CI, − 23.16 to − 4.57); p = 0.003; WMD = − 7.81 (95% CI, − 12.33 to − 3.30); p = 0.001, respectively). In addition, IRF was found to have shorter procedure and fluoroscopy times than LBA (WMD = 24.42 (95% CI, 1.42–47.43); p = 0.037 and WMD = 9.17 (95% CI, 0.09–18.26); p = 0.048, respectively). CBA was also found to have a shorter procedure time than LBA (WMD = 20.0 (95% CI, 4.75–35.25); p = 0.01), as well as a shorter fluoroscopy time than PVAC (WMD = − 15.0 (95% CI, − 21.17 to − 8.83); p = 0.00) (Figs. 5 and 6). Similar results were found when only patients with PAF were analyzed (Supplement Fig. 2).
Additional network analyses for the secondary endpoints were conducted and indicated that PVAC was most likely to have the shortest procedure time (Prbest = 61.5%) and that nMARQ may have the shortest fluoroscopy time (Prbest = 60.6%). The consistency of the network analyses for secondary outcomes was also satisfactory (Tables 4 and 5).
4 Discussion
4.1 Principal findings
To the best of our knowledge, this may be the first study to simultaneously compare 6 different CA techniques using a network meta-analysis based on evidence from RCTs. The main findings are as follows: (1) no significant differences were found among the different interventions in terms of freedom from AT or procedure-related complications; (2) PVAC seemed to be associated with a shorter procedure time than that of other techniques; and (3) compared with IRF, CBA had comparable efficacy and safety, while CB2 had a significantly shorter procedure time than CF-IRF.
4.2 Efficacy
A number of previous studies have evaluated efficacy of the “single-shot” approaches in comparison with a “point-by-point” technique such as IRF for PVI, but no consensus has been reached so far. These “single-shot” technologies have advantages of simplifying the PVI procedure by placing the ablation catheter at the antrum/ostium of the PV instead of continuous repositioning.
Based on evidence from both conventional meta-analyses and network analyses, we found no significant differences in terms of the freedom from AT among various interventions, which is consistent with a previous study showing that endocardial PVI has similar outcomes regardless of the technique used [38].
Among these approaches, CBA and LBA are both balloon-based techniques. The visually guided LBA has been commercially available in Europe since 2009 and has been demonstrated to be noninferior compared with IRF for paroxysmal AF in large-scale RCTs [35]. In addition, the lesions created with laser energy were all found to be circumferential and transmural, which may lead to a low reconnection rate after PVI [33].
Regarding CBA, it is currently the most common alternative intervention for IRF, and the second-generation cryoballoon has also been introduced to address issues with abnormal PV anatomy. Both the pairwise and network meta-analyses demonstrated that cryoballoons have comparable efficacy with IRF, regardless of the type of CB (CB1 or CB2) or type of IRF (CF or nCF). These results are consistent with recently published meta-analyses and the largescale Fire and ICE trial [13]. However, significant heterogeneity was detected in the comparison between CBA and IRF for the efficacy outcome, and further sensitive analyses showed similar outcomes, whereas a comparison between CB2 and IRF was not available due to the lack of data.
Compared with IRF, CBA has a relatively high risk of phrenic nerve palsy, but it may also reduce the risk of cardiac tamponade and represents a valuable alternative for PVI.
PVAC and nMARQ are both circular, multielectrode catheters. PVAC is based on the nonirrigated duty-cycled ablation phased RF technology, and nMARQ is an irrigated, multielectrode electroanatomically guided catheter; despite their supposed clinical effectiveness both in our study and previous studies, the issue of safety remains a major concern [39, 40]. It should be noted that the nMARQ catheter was recalled from clinical use and a redesigned prototype is under evaluation [41]. Meanwhile, the recently introduced PVAC-GOLD catheter is also being re-evaluated, which may subsequently alter the risk-benefit profile [41].
The basket-based MA catheter was found to have the lowest Prbest ratio (2.2%), which has been shown in other studies in comparison with LBA. The MACPAF study revealed that complete PVI was not achieved in any of the MA groups, compared with 75% in the LBA group [21], and other studies showed that only 18–36% of all MA patients could maintain sinus rhythm at 6–12 months follow-up; thus, this approach may not be recommended due to the insufficient efficacy [42].
4.3 Safety
The prevalence of major complications varies widely, from 0.8 to 16.3% according to the previous studies [2, 43,44,45]. In our study, comparable risk estimates for procedure-related major complications were found between different ablation techniques.
Previous studies have demonstrated the differences in the risk profiles of different ablation technologies [13]; for example, a high risk of pericardial injury for IRF, phrenic nerve palsy (PNP) for LBA, thromboembolic events and PV stenosis for PVAC, and esophageal-atrial fistula for nMARQ.
PVAC was reported to be associated with a 1.48 times higher risk of silent cerebral embolism compared with IRF and CBA [46, 47], and its unknown impact on long-term cognitive function still remains a concern. Recently, the redesigned PVAC GOLD was found to have a similar safety profile, but with lower complication rates [48]. However, one should note that the results may be overshadowed by a high background rate of silent cerebral events, which may not be catheter-specific, as previous studies have shown that asymptomatic cerebrovascular emboli is common, with an incidence of 11–14% [41, 49]. As was different from PVAC, the later continuous irrigated forms of multiple electrode catheters, such as nMARQ, were thought to help reduce the risk of thrombus formation and, consequently, the incidence of cerebral microembolism [50].
Although the network analysis revealed that nMARQ and PVAC may be associated with less absolute complication numbers, especially compared with LBA and CBA, their complications were more severe and life-threatening, which is also why nMARQ was recalled for further investigation after early studies [39, 51].
PNP is a common complication of CBA; however, it is usually transient, and persistent PNP is only seen in < 1% of patients [52]. The recently introduced second-generation CBA was reported to have greater PVI efficacy, but at the same time, a higher incidence of transient PNP, possibly due to the larger cooling surface area and deeper damaged foci [53,54,55,56].
From the present analysis, we did not detect any best technique in terms of safety, and as the definition of procedure-related complications mostly lacked in the designs, the outcomes were relatively heterogeneous among the included studies. Thus, the individual risk profile should be taken into account when selecting CA energy sources, as the procedure-related complications may to a large extent be related to individual characteristics, operator experiences, and other procedural factors.
4.4 Secondary endpoints
In the current report, we found that fluoroscopy times were comparable among techniques, and PVAC may be associated with a shorter procedure time according to the network analysis. This is not surprising, as the “one-shot” techniques may require less catheter manipulation than point-by-point CA strategies such as IRF. The shorter procedure duration could lead to a more cost-effective approach for hospitals, as well as for patients with impaired heart function. However, the results became controversial when the pairwise meta-analysis was conducted. For example, the conventional meta-analysis demonstrated that nMARQ had shorter procedure and fluoroscopy times than PVAC, and IRF was found to have shorter procedure and fluoroscopy times than LBA. Possible explanations may be the heterogeneities between studies and between different comparisons. In terms of the secondary endpoints, nMARQ performed better than PVAC and PVAC performed better than IRF. However, when compared with IRF, nMARQ displayed a trend towards a longer procedural and fluoroscopy times. Thus, the results of the network analysis may have been influenced and should be interpreted with caution. The small study numbers for the comparisons of nMARQ vs. PVAC and nMARQ vs. IRF should be taken into account.
Compared with LBA, CBA has become more promising and increasingly used over the last few years, and in this study, CBA and IRF were comparable concerning procedure and fluoroscopy times. Previous studies have shown that CBA is associated with shorter procedure and fluoroscopy times compared with IRF [57]. However, in this meta-analysis, patients with mixed AF were included, and several trials were randomized with significant heterogeneities. In the sensitive analysis, CBA with CB2 was found to have a significantly shorter procedure time compared with CF-IRF. This result was consistent with the study by Buiatti et al. [58] but was different from that by Jourda et al. [59], which found that the procedural duration was significantly shorter with CF-IRF in comparison with CB2 catheters.
Newly updated and developed technologies, such as CB2 and CF-IRF catheters, should greatly improve the outcomes and shorten the procedural duration. The structural improvements with CB2 could optimize the refrigerant flow and distribution, creating a more uniform freezing zone [60,61,62].
In addition, the procedure and fluoroscopy times may be shortened even more, as the recently advanced technologies, such as intracardiac echocardiography and high-power short-duration methods, should be utilized for IRF. The newly introduced hot balloon technique is also promising, although the evidence is limited. Thus, the comparison between CBA and IRF needs further investigation; and it is intuitive that differences may become less pronounced, as the efficacy is comparable, especially in centers with a high-volume and more experienced operators.
The results of this study also bring about clinical interests regarding whether the continuous improvement of the CA technologies could help to overcome both the inherent and common limitations, to make the procedure dependent on operator experience and shorten the learning curve for new operators.
5 Limitations
The present study was performed using both pairwise and network meta-analytic methods based on 33 RCTs with 4801 patients; however, there are several limitations.
First, this network meta-analysis intended to evaluate all the CA techniques based on RCTs data; however, some catheters in their first-generation phenotypes, such as nMARQ or PVAC, may not available now and data on their redesigned phenotypes are lacking. Furthermore, as MA and LBA were not commonly used, publication bias may exit, as newer technologies are usually favored over established technologies. Second, the quality of the included studies was adequate, but the blinding of patients and the operators was not possible, and the operator experience varied between the studies. Data were nonuniform in terms of endpoint definitions, follow-up duration, or arrhythmic recurrence monitoring protocols, all of which may cause possible bias, especially in the interpretation of the success rate. In addition, there were considerable heterogeneities, both in the pairwise meta-analysis and between the pairwise and network analyses due to multiple factors. Finally, an assessment of the newest CA technologies, such as hot balloon ablation and high-power ablation, was not available due to the lack of related studies or RCTs until now, and the question for the optimum technique remains open.
6 Conclusions
The efficacy and safety outcomes were comparable among various techniques, and there is insufficient evidence to suggest that one CA technique is superior to another. However, PVAC may be associated with a shorter procedural duration among the included techniques, and CB2 catheters seemed to reduce the procedure time compared with CF-IRF. Further large-scale studies are warranted to compare the available CA techniques and provide an up-to-date recommendation for the superior option.
Data availability
Available upon request to the corresponding author WeiMao (maoweilw@163.com).
References
Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham heart study: a cohort study. Lancet. 2015;386(9989):154–62.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016;18(11):1609–78.
Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(1):32–8.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019). Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
You L, Yao L, Zhou B, Jin L, Yin H, Wu J, et al. Effects of different ablation strategies on long-term left atrial function in patients with paroxysmal atrial fibrillation: a single-blind randomized controlled trial. Sci Rep. 2019;9(1):7695.
Giannopoulos G, Kossyvakis C, Vrachatis D, Aggeli C, Tsitsinakis G, Letsas K, et al. Effect of cryoballoon and radiofrequency ablation for pulmonary vein isolation on left atrial function in patients with nonvalvular paroxysmal atrial fibrillation: a prospective randomized study (Cryo-LAEF study). J Cardiovasc Electrophysiol. 2019;30(7):991–8.
Bin Waleed K, Yin X, Yang X, Dai B, Liu Y, Wang Z, et al. Short and long-term changes in platelet and inflammatory biomarkers after cryoballoon and radiofrequency ablation. Int J Cardiol. 2019;285:128–32.
Andrade JG, Champagne J, Dubuc M, Deyell MW, Verma A, Macle L, et al. Cryoballoon or radiofrequency ablation for atrial fibrillation assessed by continuous monitoring: a randomized clinical trial. Circulation. 2019;140(22):1779–88.
Watanabe R, Sairaku A, Yoshida Y, Nanasato M, Kamiya H, Suzuki H, et al. Head-to-head comparison of acute and chronic pulmonary vein stenosis for cryoballoon versus radiofrequency ablation. Pacing Clin Electrophysiol. 2018;41(4):376–82.
Gunawardene MA, Hoffmann BA, Schaeffer B, Chung DU, Moser J, Akbulak RO, et al. Influence of energy source on early atrial fibrillation recurrences: a comparison of cryoballoon vs. radiofrequency current energy ablation with the endpoint of unexcitability in pulmonary vein isolation. Europace. 2018;20(1):43–9.
Davtyan K, Shatakhtsyan V, Poghosyan H, Deev A, Tarasov A, Kharlap M, et al. Radiofrequency versus cryoballoon ablation of atrial fibrillation: an evaluation using ECG, Holter monitoring, and implantable loop recorders to monitor absolute and clinical effectiveness. Biomed Res Int. 2018;2018:3629384.
Buist TJ, Adiyaman A, Smit JJJ, Ramdat Misier AR, Elvan A. Arrhythmia-free survival and pulmonary vein reconnection patterns after second-generation cryoballoon and contact-force radiofrequency pulmonary vein isolation. Clin Res Cardiol. 2018;107(6):498–506.
Kuck KH, Brugada J, Furnkranz A, Metzner A, Ouyang F, Chun KR, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374(23):2235–45.
Luik A, Radzewitz A, Kieser M, Walter M, Bramlage P, Hormann P, et al. Cryoballoon versus open irrigated radiofrequency ablation in patients with paroxysmal atrial fibrillation: the prospective, randomized, controlled. Noninferiority FreezeAF Study Circulation. 2015;132(14):1311–9.
Hunter RJ, Baker V, Finlay MC, Duncan ER, Lovell MJ, Tayebjee MH, et al. Point-by-point radiofrequency ablation versus the cryoballoon or a novel combined approach: a randomized trial comparing 3 methods of pulmonary vein isolation for paroxysmal atrial fibrillation (the Cryo versus RF trial). J Cardiovasc Electrophysiol. 2015;26(12):1307–14.
Perez-Castellano N, Fernandez-Cavazos R, Moreno J, Canadas V, Conde A, Gonzalez-Ferrer JJ, et al. The COR trial: a randomized study with continuous rhythm monitoring to compare the efficacy of cryoenergy and radiofrequency for pulmonary vein isolation. Heart Rhythm. 2014;11(1):8–14.
Pokushalov E, Romanov A, Artyomenko S, Baranova V, Losik D, Bairamova S, et al. Cryoballoon versus radiofrequency for pulmonary vein re-isolation after a failed initial ablation procedure in patients with paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24(3):274–9.
Herrera Siklody C, Arentz T, Minners J, Jesel L, Stratz C, Valina CM, et al. Cellular damage, platelet activation, and inflammatory response after pulmonary vein isolation: a randomized study comparing radiofrequency ablation with cryoablation. Heart Rhythm. 2012;9(2):189–96.
Tse HF, Kwong YL, Lau CP. Transvenous cryoablation reduces platelet activation during pulmonary vein ablation compared with radiofrequency energy in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2005;16(10):1064–70.
Schirdewan A, Herm J, Roser M, Landmesser U, Endres M, Koch L, et al. Loop recorder detected high rate of atrial fibrillation recurrence after a single balloon- or basket-based ablation of paroxysmal atrial fibrillation: results of the MACPAF study. Front Cardiovasc Med. 2017;4:4.
Koch L, Haeusler KG, Herm J, Safak E, Fischer R, Malzahn U, et al. Mesh ablator vs. cryoballoon pulmonary vein ablation of symptomatic paroxysmal atrial fibrillation: results of the MACPAF study. Europace. 2012;14(10):1441–9.
Malmborg H, Lonnerholm S, Blomstrom P, Blomstrom-Lundqvist C. Ablation of atrial fibrillation with cryoballoon or duty-cycled radiofrequency pulmonary vein ablation catheter: a randomized controlled study comparing the clinical outcome and safety; the AF-COR study. Europace. 2013;15(11):1567–73.
Kece F, Bruggemans EF, de Riva M, Alizadeh Dehnavi R, Wijnmaalen AP, Meulman TJ, et al. Incidence and clinical significance of cerebral embolism during atrial fibrillation ablation with duty-cycled phased-radiofrequency versus cooled-radiofrequency: a randomized controlled trial. JACC Clin Electrophysiol. 2019;5(3):318–26.
Boersma LV, van der Voort P, Debruyne P, Dekker L, Simmers T, Rossenbacker T, et al. Multielectrode pulmonary vein isolation versus single tip wide area catheter ablation for paroxysmal atrial fibrillation: a multinational multicenter randomized clinical trial. Circ Arrhythm Electrophysiol. 2016;9(4):e003151.
Podd SJ, Sulke AN, Sugihara C, Furniss SS. Phased multipolar radiofrequency pulmonary vein isolation is as effective and safe as conventional irrigated point-to-point ablation. A prospective randomised 1-year implantable cardiac monitoring device follow-up trial. J Interv Card Electrophysiol. 2015;44(3):257–64.
McCready J, Chow AW, Lowe MD, Segal OR, Ahsan S, de Bono J, et al. Safety and efficacy of multipolar pulmonary vein ablation catheter vs. irrigated radiofrequency ablation for paroxysmal atrial fibrillation: a randomized multicentre trial. Europace. 2014;16(8):1145–53.
Gal P, Aarntzen AE, Smit JJ, Adiyaman A, Misier AR, Delnoy PP, et al. Conventional radiofrequency catheter ablation compared to multi-electrode ablation for atrial fibrillation. Int J Cardiol. 2014;176(3):891–5.
Bittner A, Monnig G, Zellerhoff S, Pott C, Kobe J, Dechering D, et al. Randomized study comparing duty-cycled bipolar and unipolar radiofrequency with point-by-point ablation in pulmonary vein isolation. Heart Rhythm. 2011;8(9):1383–90.
Bulava A, Hanis J, Sitek D, Osmera O, Karpianus D, Snorek M, et al. Catheter ablation for paroxysmal atrial fibrillation: a randomized comparison between multielectrode catheter and point-by-point ablation. Pacing Clin Electrophysiol. 2010;33(9):1039–46.
Kozluk E, Piatkowska A, Rodkiewicz D, Peller M, Kochanowski J, Opolski G. Direct results of a prospective randomized study comparing ablation with the nMARQ catheter and the PVAC catheter used with and without a 3D system (MAPER 3D study). Arch Med Sci. 2019;15(1):78–85.
Sugihara C, Furniss S, Hyde J, Lewis M, Sulke N. Results of the first investigator-initiated randomized clinical trial of nMARQTM, PVACTM, and thoracoscopic ablation for paroxysmal atrial fibrillation. Europace. 2018;20(Fi_3):f384–f91.
Grimaldi M, Swarup V, DeVille B, Sussman J, Jais P, Gaita F, et al. Importance of anticoagulation and postablation silent cerebral lesions: subanalyses of REVOLUTION and reMARQable studies. Pacing Clin Electrophysiol. 2017;40(12):1432–9.
Ucer E, Janeczko Y, Seegers J, Fredersdorf S, Friemel S, Poschenrieder F, et al. A RAndomized trial to compare the acute reconnection after pulmonary vein ISolation with laser-BalloON versus radiofrequency ablation: RATISBONA trial. J Cardiovasc Electrophysiol. 2018;29(5):733–9.
Schmidt B, Neuzil P, Luik A, Osca Asensi J, Schrickel JW, Deneke T, et al. Laser balloon or wide-area circumferential irrigated radiofrequency ablation for persistent atrial fibrillation: a multicenter prospective randomized study. Circ Arrhythm Electrophysiol. 2017;10(12).
Dukkipati SR, Cuoco F, Kutinsky I, Aryana A, Bahnson TD, Lakkireddy D, et al. Pulmonary vein isolation using the visually guided laser balloon: a prospective, multicenter, and randomized comparison to standard radiofrequency ablation. J Am Coll Cardiol. 2015;66(12):1350–60.
Casella M, Dello Russo A, Russo E, Al-Mohani G, Santangeli P, Riva S, et al. Biomarkers of myocardial injury with different energy sources for atrial fibrillation catheter ablation. Cardiol J. 2014;21(5):516–23.
Schmidt B, Gunawardene M, Krieg D, Bordignon S, Furnkranz A, Kulikoglu M, et al. A prospective randomized single-center study on the risk of asymptomatic cerebral lesions comparing irrigated radiofrequency current ablation with the cryoballoon and the laser balloon. J Cardiovasc Electrophysiol. 2013;24(8):869–74.
Vogler J, Willems S, Sultan A, Schreiber D, Luker J, Servatius H, et al. Pulmonary vein isolation versus defragmentation: the CHASE-AF clinical trial. J Am Coll Cardiol. 2015;66(24):2743–52.
Vurma M, Dang L, Brunner-La Rocca HP, Sutsch G, Attenhofer-Jost CH, Duru F, et al. Safety and efficacy of the nMARQ catheter for paroxysmal and persistent atrial fibrillation. Europace. 2016;18(8):1164–9.
Mahida S, Hooks DA, Nentwich K, Ng GA, Grimaldi M, Shin DI, et al. nMARQ ablation for atrial fibrillation: results from a multicenter study. J Cardiovasc Electrophysiol. 2015;26(7):724–9.
Laish-Farkash A, Suleiman M. Comparison of the efficacy of PVAC((R)) and nMARQ() for paroxysmal atrial fibrillation. J Atr Fibrillation. 2017;9(6):1550.
Maagh P, van Bracht M, Butz T, Trappe HJ, Meissner A. Eighteen months follow-up of the clinical efficacy of the high density mesh ablator (HDMA) in patients with atrial fibrillation after pulmonary vein isolation. J Interv Card Electrophysiol. 2010;29(1):43–52.
De Greef Y, Stroker E, Schwagten B, Kupics K, De Cocker J, Chierchia GB, et al. Complications of pulmonary vein isolation in atrial fibrillation: predictors and comparison between four different ablation techniques: results from the MIddelheim PVI-registry. Europace. 2018;20(8):1279–86.
Arbelo E, Brugada J, Blomstrom-Lundqvist C, Laroche C, Kautzner J, Pokushalov E, et al. Contemporary management of patients undergoing atrial fibrillation ablation: in-hospital and 1-year follow-up findings from the ESC-EHRA atrial fibrillation ablation long-term registry. Eur Heart J. 2017;38(17):1303–16.
Hoyt H, Bhonsale A, Chilukuri K, Alhumaid F, Needleman M, Edwards D, et al. Complications arising from catheter ablation of atrial fibrillation: temporal trends and predictors. Heart Rhythm. 2011;8(12):1869–74.
Herrera Siklody C, Deneke T, Hocini M, Lehrmann H, Shin DI, Miyazaki S, et al. Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. J Am Coll Cardiol. 2011;58(7):681–8.
Gaita F, Leclercq JF, Schumacher B, Scaglione M, Toso E, Halimi F, et al. Incidence of silent cerebral thromboembolic lesions after atrial fibrillation ablation may change according to technology used: comparison of irrigated radiofrequency, multipolar nonirrigated catheter and cryoballoon. J Cardiovasc Electrophysiol. 2011;22(9):961–8.
Leitz P, Guner F, Wasmer K, Foraita P, Pott C, Dechering DG, et al. Data on procedural handling and complications of pulmonary vein isolation using the pulmonary vein ablation catheter GOLD(R). Europace. 2016;18(5):696–701.
Neumann T, Kuniss M, Conradi G, Janin S, Berkowitsch A, Wojcik M, et al. MEDAFI-trial (micro-embolization during ablation of atrial fibrillation): comparison of pulmonary vein isolation using cryoballoon technique vs. radiofrequency energy. Europace. 2011;13(1):37–44.
Sauren LD, Vanb Y, Der L, Pison L, Lam M, van der Veen FH, et al. Transcranial measurement of cerebral microembolic signals during endocardial pulmonary vein isolation: comparison of three different ablation techniques. J Cardiovasc Electrophysiol. 2009;20(10):1102–7.
Deneke T, Schade A, Muller P, Schmitt R, Christopoulos G, Krug J, et al. Acute safety and efficacy of a novel multipolar irrigated radiofrequency ablation catheter for pulmonary vein isolation. J Cardiovasc Electrophysiol. 2014;25(4):339–45.
Andrade JG, Dubuc M, Guerra PG, Macle L, Rivard L, Roy D, et al. Cryoballoon ablation for atrial fibrillation. Indian Pacing Electrophysiol J. 2012;12(2):39–53.
Cheng X, Hu Q, Zhou C, Liu LQ, Chen T, Liu Z, et al. The long-term efficacy of cryoballoon vs irrigated radiofrequency ablation for the treatment of atrial fibrillation: a meta-analysis. Int J Cardiol. 2015;181:297–302.
Straube F, Dorwarth U, Vogt J, Kuniss M, Heinz Kuck K, Tebbenjohanns J, et al. Differences of two cryoballoon generations: insights from the prospective multicentre, multinational FREEZE cohort substudy. Europace. 2014;16(10):1434–42.
Giovanni GD, Wauters K, Chierchia GB, Sieira J, Levinstein M, Conte G, et al. One-year follow-up after single procedure Cryoballoon ablation: a comparison between the first and second generation balloon. J Cardiovasc Electrophysiol. 2014;25(8):834–9.
Casado-Arroyo R, Chierchia GB, Conte G, Levinstein M, Sieira J, Rodriguez-Manero M, et al. Phrenic nerve paralysis during cryoballoon ablation for atrial fibrillation: a comparison between the first- and second-generation balloon. Heart Rhythm. 2013;10(9):1318–24.
Patel N, Patel K, Shenoy A, Baker WL, Makaryus AN, El-Sherif N. Cryoballoon ablation for the treatment of atrial fibrillation: a meta-analysis. Curr Cardiol Rev. 2019;15(3):230–8.
Buiatti A, von Olshausen G, Barthel P, Schneider S, Luik A, Kaess B, et al. Cryoballoon vs. radiofrequency ablation for paroxysmal atrial fibrillation: an updated meta-analysis of randomized and observational studies. Europace. 2017;19(3):378–84.
Jourda F, Providencia R, Marijon E, Bouzeman A, Hireche H, Khoueiry Z, et al. Contact-force guided radiofrequency vs. second-generation balloon cryotherapy for pulmonary vein isolation in patients with paroxysmal atrial fibrillation-a prospective evaluation. Europace. 2015;17(2):225–31.
Shao M, Shang L, Shi J, Zhao Y, Zhang W, Zhang L, et al. The safety and efficacy of second-generation cryoballoon ablation plus catheter ablation for persistent atrial fibrillation: a systematic review and meta-analysis. PLoS One. 2018;13(10):e0206362.
Ciconte G, Baltogiannis G, de Asmundis C, Sieira J, Conte G, Di Giovanni G, et al. Circumferential pulmonary vein isolation as index procedure for persistent atrial fibrillation: a comparison between radiofrequency catheter ablation and second-generation cryoballoon ablation. Europace. 2015;17(4):559–65.
Knecht S, Kuhne M, Osswald S, Sticherling C. Quantitative assessment of a second-generation cryoballoon ablation catheter with new cooling technology-a perspective on potential implications on outcome. J Interv Card Electrophysiol. 2014;40(1):17–21.
Funding
This work was supported by the Zhejiang Provincial Research Project of Public Welfare Technology (grant number LGF19H020003 to X.Z.). The funding sources had no role in study design, data collection and analysis, preparation of the article, or decision to publish.
Author information
Authors and Affiliations
Contributions
XZ and JD designed the research, performed the statistical analysis, and wrote the manuscript text. XX, YL, and ZL performed the literature search and data collation. ML prepared figures and tables. ZW and WM have jointly supervised the work and revised the article critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable as this is a meta-analysis of previously published papers.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Suppl. Fig. 1
Funnel plot for the studies included based on the outcome of freedom from AT (PNG 6965 kb)
Suppl. Fig. 2
Pairwise meta-analysis for the outcomes of paroxysmal atrial fibrillation patients. WMD = weighted mean difference, OR = Odds ratio, LBA = Laser Balloon Ablation, nMARQ = nMARQ ablation, CBA = Cryoballoon Ablation, PVAC = Pulmonary Vein Ablation Catheter, IRF = Irrigated Radiofrequency Ablation, MA = Mesh Ablator (PNG 95574 kb)
Suppl. Fig. 3
Pairwise meta-analysis for the outcomes according to different generations of CBA and IRF. WMD = weighted mean difference, OR = Odds ratio, LBA = Laser Balloon Ablation, nMARQ = nMARQ ablation, CBA = Cryoballoon Ablation, PVAC = Pulmonary Vein Ablation Catheter, IRF = Irrigated Radiofrequency Ablation, MA = Mesh Ablator, CB1 = the first generation cryoballoon, CB2 = the second generation cryoballoon, CF-IRF = contact force IRF, nCF-IRF = no contact force IRF, (PNG 104737 kb)
ESM 1
(DOCX 79 kb)
Rights and permissions
About this article
Cite this article
Zhou, X., Dai, J., Xu, X. et al. Comparative efficacy and safety of catheter ablation interventions for atrial fibrillation: comprehensive network meta-analysis of randomized controlled trials. J Interv Card Electrophysiol 62, 199–211 (2021). https://doi.org/10.1007/s10840-020-00878-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00878-9