Abstract
Purpose
The relation between dyslipidemia and atrial fibrillation (AF) development remains controversial. We conducted a prospective study to investigate the association of lipids with the risk of recurrence of AF after radiofrequency catheter ablation (RFCA).
Methods
This study enrolled 287 consecutive patients who underwent initial circumferential pulmonary vein ablation (CPVA). Fasting levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG) were measured at baseline before ablation. Patients were classified according to lipid quartiles. AF recurrence was confirmed by 48-h electrocardiograms at follow-up visits.
Results
A total of 71 patients (24.7%) experienced AF recurrence during 3 to 12 months after ablation. By univariate Cox regression survival analysis, TC (HR, 0.63; 95%CI, 0.48–0.82), LDL-C (HR, 0.61; 95%CI, 0.44–0.84), non-paroxysmal AF type (HR, 2.56; 95%CI, 1.52–4.21), and left atrial diameter (HR, 2.18; 95%CI, 1.46–3.24) were significantly associated with AF recurrence. By multivariate Cox regression survival analysis, lower quartiles of TC (HR, 3.66; 95%CI, 1.56–8.56) and LDL-C (HR, 2.28; 95%CI 1.09–4.77) were associated with higher risk of AF recurrence compared with the highest quartiles. After adjustment by sex, lower TC (HR, 11.70; 95%CI, 2.79–49.13) and LDL-C (HR, 11.00; 95%CI, 2.77–43.72) levels were associated with the recurrence of AF in women, but not in men. HDL-C and TG levels showed no association with AF recurrence in both genders.
Conclusions
TC and LDL-C levels were negatively correlated with AF recurrence after RFCA in women. HDL-C and TG were not independently associated with AF recurrence in both genders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Dyslipidemia is considered to be an independent risk factor for cardiovascular disease, but the relationship between dyslipidemia and atrial fibrillation (AF) remains controversial. A recent review [1] systematically examined 84 reports from 32 independent cohorts for the effect of cardiovascular risk factors on AF incidence. The authors found that serum cholesterol is associated with AF incidence in the opposite direction compared to the known associations of cholesterol with coronary artery disease and stroke. Previous studies [2,3,4] have shown that there is a cholesterol paradox in the relationship between cholesterol and AF, that is, low levels of cholesterol are associated with a higher risk of AF occurrence. And some recent prospective cohort studies suggest that total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) levels are inversely associated with the incidence of AF [5, 6]. Many studies showed that dyslipidemia have a paradoxical association with AF incidence, which has aroused our interest.
Since Haissaguerre et al. [7] used pulmonary vein isolation to treat paroxysmal AF; radiofrequency catheter ablation (RFCA) has made significant progress in AF treatment. However, the high AF recurrence rate after RFCA and the prognostic factors related to AF recurrence have attracted much attention [8]. Therefore, identifying the risk factors of AF recurrence after RFCA allows physicians to better select patients with higher success rates and may provide insight into developing novel preventive therapies. Although studies have shown that the metabolic syndrome is associated with recurrence of AF [9, 10], there are no specific studies to explore whether blood lipid levels affect AF recurrence after RFCA, and the impact of lipid levels on AF ablation is still unknown. Therefore, this prospective study aimed to investigate the associations of lipids with the risk of AF recurrence after RFCA.
2 Methods
2.1 Study participants
In this prospective and observational study, we enrolled 287 consecutive patients who underwent initial circumferential pulmonary vein ablation (CPVA) from January 2015 to December 2016. Patients with left atrial thrombosis, severe mitral stenosis, New York Heart Association functional classes III and IV, percutaneous coronary intervention within the 6 months before the ablation, malignancies, autoimmune or inflammatory diseases, and severe hepatic and renal dysfunction were excluded from the study. Clinical, echocardiographic, and laboratory evaluations were carried out prior to the ablation. All patients gave written informed consent, and the study was approved by the institutional review board.
2.2 Data collection
Baseline characteristics were collected upon admission, including age, sex, smoking and drinking history, body mass index (BMI), AF type, history of hypertension, diabetes, coronary heart disease, and drug use (for example, use of angiotensin-converting enzyme inhibitors/angiotensin receptor antagonists [ACEI/ARB], β-receptor blockers, antilipidemic drugs, and lipid-lowering drugs). Persistent and long-standing persistent AF were collectively defined as non-paroxysmal AF (non-PAF).
2.3 Measurement of lipid levels
Blood samples were collected on the first morning of hospitalization and were taken as fasting blood samples to measure a panel of biochemistry markers, including lipid parameters. TC, LDL-C, high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG) were all measured using the enzymatic colorimetric method (Roche Diagnostics GmbH, Germany). The laboratory reference ranges of TC were 3.14–5.86 mmol/L, of LDL-C 1.31–3.29 mmol/L, of HDL-C 0.88–2.04 mmol/L, and of TG 0.30–1.70 mmol/L. According to the distribution of blood lipid levels in the cohort, quartiles of TC were determined as: Q1 < 3.54 mmol/L, Q2 3.54–4.14 mmol/L, Q3 4.14–4.73 mmol/L, Q4 > 4.73 mmol/L; quartiles of LDL-C were determined as: Q1 < 1.87 mmol/L, Q2 1.87–2.46 mmol/L, Q3 2.46–2.90 mmol/L, Q4 > 2.90 mmol/L; quartiles of HDL-C were determined as: Q1 < 0.92 mmol/L, Q2 0.92–1.12 mmol/L, Q3 1.12–1.34 mmol/L, Q4 > 1.34 mmol/L; and quartiles of TG were determined as: Q1 < 0.9 mmol/L, Q2 0.90–1.26 mmol/L, Q3 1.26–1.78 mmol/L, Q4 > 1.78 mmol/L.
2.4 Electrophysiological study and ablation procedure
Transthoracic echocardiography, performed by a dedicated sonographer, was recorded by a commercially available echocardiographic system (VIVID E9; General Electric Company, Milwaukee, WI, USA). Left atrial anterior-posterior diameter (LAD) was measured from the parasternal long-axis view, orthogonal from the aortic root at the left ventricular (LV) end-systole phase. Procedural details regarding CPVA have been previously described in an expert consensus statement [11]. The RF-based circumferential isolation of pulmonary veins was performed using an irrigated radiofrequency ablation catheter (Thermocool, Biosense Webster, Diamond Bar, CA, USA), with the aid of electroanatomical mapping (Carto 3, Biosense Webster, Diamond Bar, CA, USA) (target temperature 43 °C, maximum power 30 W). Successful ablation was defined as complete elimination of all fragmented signals at pulmonary vein ostium, as well as verified exit and entrance block.
2.5 Post-procedural follow-up
Follow-up visits were performed every 3 months, or earlier if patients developed symptoms consistent with recurrent AF. All asymptomatic patients were followed with surface electrocardiogram (ECG) and 48-h Holter ECG. If the patient had palpitations, dizziness, and other discomfort during follow-up, a new ECG was obtained. AF recurrence was defined as the occurrence of confirmed atrial tachyarrhythmia (documented by ECG or Holter recordings) lasting longer than 30 s after ablation, excluding a 3-month blanking period. Antiarrhythmic therapy and anticoagulant was maintained for at least 3 months. If there was no atrial tachyarrhythmia recurrence after 3 months, the AADs were stopped. Dependent on CHA2DS2-VASc score, anticoagulant was discontinued or reduced.
2.6 Statistical analysis
Normal distributed data are presented as mean ± standard deviation and compared by single factor variance analysis. Abnormal distributed data are presented as median and interquartile range (IQR) and were compared by the Mann-Whitney U test. Categorical variables are shown as percentages and were compared by chi-square analysis.
Patients were categorized into quartiles based on lipid levels, and chi-square test was used to calculate the difference of AF recurrence between quartiles. Hazard ratios (HRs) and 95% confidence intervals (95%CI) were calculated using Cox proportional hazards models to estimate the relationship between lipid levels and the recurrence of AF. Adjusted Cox regression was done using two models. Model 1 adjusted for age and sex. Model 2 adjusted for sex, age, BMI, smoking, alcohol use, hypertension, diabetes mellitus (DM), cardiovascular disease, LAD, AF type, and medication use (ACEI/ARB, β-blockers, lipid-lowering drugs). The analyses were performed separately for men and women. A P value of < 0.05 was considered statistically significant. All analyses were performed using the SPSS software (version 23.00; SPSS, Inc., Chicago, IL, USA).
3 Results
3.1 Baseline characteristics
Details of baseline characteristics per TC quartile are given in Table 1. From the lowest to the highest TC quartile, the proportion of women gradually increased. Patients in Q1 had an increased LAD, higher prevalence of coronary artery disease (CAD), and used more medication (lipid-lowering drugs) (P < 0.05). Other risk factors did not differ significantly between the TC quartiles.
3.2 AF recurrence and blood lipids
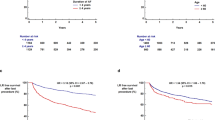
During a follow-up of 331 ± 163 days, 71 patients (24.7%) experienced AF recurrence within 3 to 12 months after RFCA. A trend of decreased recurrence rate of AF from the lowest TC and LDL-C quartiles to the highest quartiles is observed (Fig. 1). However, there were no significant differences in AF recurrence rates between HDL-C and TG quartiles. From the lowest TC quartile to the highest quartile, the AF recurrence rates were 35.2%, 26.8%, 26.8%, and 11.3%, respectively (P = 0.009). From the lowest LDL-C quartile to the highest quartile, the AF recurrence rates were 38.5%, 26.9%, 23.1%, and 11.5%, respectively (P = 0.040).
AF recurrence stratified by quartiles of blood lipids in total population. a AF recurrence by TC quartiles. b AF recurrence by LDL-C quartiles. c AF recurrence by HDL-C quartiles. d AF recurrence by TG quartiles. Abbreviations: TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; Q, quartile
After adjustment by sex, the relationship between lipid quartiles and the recurrence rate of AF was similar in women compared to the general population. There were significant inverse correlations between TC and LDL-C quartiles and AF recurrence rates in women (Fig. 2). From the lowest TC quartile to the highest quartile, the AF recurrence rates were 50.0%, 33.3%, 25.8%, and 11.3%, respectively (P = 0.004). From the lowest LDL-C quartile to the highest quartile, the recurrence rates were 50.0%, 26.9%, 21.4%, and 8.8%, respectively (P = 0.006). In contrast, chi-square test showed that there were no significant correlations between blood lipid quartiles and AF recurrence rates in men.
AF recurrence stratified by quartiles of blood lipids in women. a AF recurrence by TC quartiles in women. b AF recurrence by LDL-C quartiles in women. c AF recurrence by HDL-C quartile in women. d AF recurrence by TG quartile in women. Abbreviations: TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; Q, quartile
3.3 Univariate Cox regression analysis of risk factors and AF recurrence
By univariate Cox regression survival analysis (Table 2), TC (HR, 0.63; 95%CI, 0.48–0.82, P = 0.001), LDL-C (HR, 0.61; 95%CI, 0.44–0.84, P = 0.002), non-paroxysmal AF type (HR, 2.56; 95%CI, 1.52–4.21, P < 0.001), and LAD (HR, 2.18; 95%CI, 1.46–3.24, P < 0.001) were significantly associated with AF recurrence. There were no differences between AF recurrence rate and HDL-C, TG, free tetraiodothyronine (FT4), age, gender, BMI, smoking, alcohol use, medication use, and prevalence of diabetes, hypertension, CAD.
3.4 Blood lipid quartiles and AF recurrence
Considering blood lipid levels as category variates (Table 3), univariate Cox proportional hazard regression analysis showed an increased risk of AF recurrence in the lower quartiles of TC and in the lowest quartile of LDL-C compared with subjects in the highest quartiles. AF recurrence was not different between the HDL-C and TG quartiles. In the age- and sex-adjusted model (Model 1) and the multivariate model (Model 2), adjusted for sex, age, BMI, smoking, alcohol use, hypertension, DM, cardiovascular disease, LAD, AF type, and medication use (ACEI/ARB, β-blockers, lipid-lowering drugs), the inverse associations between TC, LDL-C, and risk of AF recurrence remained significant. The HRs and 95%CIs of the lowest quartile compared with the highest quartile of lipids adjusted by model 2 were as follows: TC (HR, 3.66; 95%CI, 1.56 = 8.56); LDL-C (HR, 2.28; 95%CI, 1.09–4.77).
3.5 Blood lipid quartiles and AF recurrence by gender
Considering the gender-dependent differences in blood lipid levels (Tables 4 and 5), total subjects were divided by sex and in the age-adjusted model (Model 1) and the multivariate model (Model 2), lower quartiles of TC and LDL-C were associated with a higher risk of AF recurrence in women (Table 4), but not in men (Table 5), consistent with previous results. Also, no significant associations of AF recurrence with HDL-C and TG were observed in both genders. The HRs and 95%CIs for the different quartiles compared with the highest quartile of lipids in women are shown in Table 5. After adjustment by the multivariate model (Model 2), the HRs and 95%CIs of the lowest quartile compared with the highest quartile of lipids in women were as follows: TC (HR, 11.70; 95%CI, 2.79–49.13) and LDL-C (HR, 11.00; 95%CI, 2.77–43.72).
3.6 Continuous blood lipid levels and AF recurrence
Considering blood lipids level as continuous variates (Table 6), Cox analysis with multivariate adjustment (Model 2) revealed that higher TC and LDL-C levels were significantly associated with lower risk of AF recurrence (P = 0.001, P = 0.005, respectively). An increase in TC by 1.0 mmol/L was associated with a lower risk of new-onset AF of 41%, and a 1.0 mmol/L increase in LDL-C was associated with a 39% lower risk of new-onset AF. Neither HDL-C nor TG were associated with AF recurrence. Cox regression analyses were also performed by gender. An increase in TC and LDL-C were associated with a lower risk of AF recurrence after catheter ablation in women, but no association was found in men. The HRs and 95% CIs in women were as follows: TC (HR, 0.34; 95%CI, 0.18–0.62) and LDL-C (HR, 0.39; 95%CI 0.23–0.67).
4 Discussion
The main findings of this study are the following: (i) Lower levels of TC and LDL-C were associated with higher recurrence of AF independent of other risk factors, and this association was also significant in women, but not in men. The inverse associations also remained significant after adjustment for other standard AF risk factors. (ii) No relationship was observed between HDL-C and TG levels with AF recurrence in both genders. These findings suggest that lower levels of TC and LDL-C are an independent risk factor for AF recurrence.
Hyperlipidemia is a risk factor for cardiovascular disease, but the relationship between dyslipidemia and AF is controversial. As early as 1997, Psaty et al. [4] investigated risk factors of AF incidence in the elderly and found that the use of β-blockers, heavy drinking, and cholesterol were associated with a reduced risk of AF, and also stated that the inverse relationship between AF and cholesterol is unexpected and unexplained. After that, Annoura M et al. [2] proposed “cholesterol paradox” in PAF because they found low serum levels of TC and TG in patients with PAF. Recently, some studies [3, 5, 12] also showed significant inverse associations between cholesterol and AF incidence. Findings in the Atherosclerosis Risk in Communities study (ARIC) [12], and a prospective study among 23,738 women [3] and in the study based on the Swedish Primary Care Cardiovascular Database (SPCCD) [5] showed lower levels of LDL-C and TC were associated with an elevated risk for AF. However, in contrast to previous studies, a combined analysis from MESA-FHS cohorts [13] showed that HDL-C and triglycerides but not LDL-C or TC were associated with the risk of AF. Although the results are quite confusing, it seems that in general, “cholesterol paradox” does exist between lipid profiles and AF. In this study, lower TC and LDL-C levels were associated with high rate of AF recurrence in women, revealing a similar paradox, and it was reasonable to believe that low level of cholesterol would reduce the success rate of catheter ablation of AF. Although there are few other studies on the association of blood lipid levels and AF recurrence after ablation, a multicenter study suggests that the metabolic syndrome is associated with a high rate of AF recurrence, but components of the metabolic syndrome, such as hypertension, DM, obesity, and hyperlipidemia, were not independent factors associated with AF recurrence [10]. In contrast, one recent meta-analysis [14] included 36 studies to search for blood markers associated with AF recurrence after radiofrequency catheter ablation and found that the AF recurrence group had a higher LDL-C level. This finding is different from the results in this study; therefore, further study should be done to explore the correlation between blood lipids and the recurrence of AF.
In addition to being effective lipid-lowering agents, clinical and basic studies have shown that statins also have anti-inflammatory properties and may therefore have a protective effect on AF [15]. However, previous prospective studies [12, 16, 17], like the present study, failed to show any benefit of the use of these drugs for reducing the recurrence of AF after catheter ablation, which indirectly supports our finding. In this study, we did not exclude patients on lipid-lowering drugs. Consistent with the views of Mourtzinis G and others in SPCCD study, we think that excluding them may artificially reduce the number of patients with the most severe dyslipidemia and distort the association with AF recurrence, and we think that there are many factors affecting blood lipids, such as diet structure, lifestyle intervention, and drug intervention; lipid-lowering drugs are only one of them. Our current study is concerned with the relationship between preoperative baseline levels of blood lipid and risk of AF recurrence. In our future study, we will further explore whether the recurrence risk of iatrogenic low cholesterol differs from that of intrinsic low cholesterol.
There is no exact mechanism to explain our findings. Several mechanisms may be responsible, as shown in recent studies. Firstly, there is a thyroid hormone–related mechanism. An increasing number of studies have shown that high FT4 levels are associated with AF recurrence, and hyperthyroidism can reduce levels of cholesterol [18, 19]. However, in our study, there was no difference in FT4 level between the TC quartiles, and there was no significant correlation between FT4 level and AF recurrence, thereby not supporting this assumption. Blood lipids can impact the composition of cell membranes and properties of cell electrophysiology [20], which is a major determinant of cell excitability. Membrane lipid content equilibrium can prevent the formation of arrhythmic potentials. Some reports suggest that lipoproteins have anti-inflammation effects and Kim et al. [21] found that the lipoprotein properties of patients with AF were severely impaired, resulting in increased oxidation and inflammation, and inflammation is a risk factor for the recurrence of AF [22]. Therefore, low levels of TC and LDL-C may increase the risk of AF recurrence by increasing inflammation. However, whether these mechanisms explain the observed association is hypothetical and requires further research.
AF is a heterogeneous disease with complex mechanisms, and the incidence of AF varies by age and sex. There are gender differences in blood lipid profiles and the electrophysiological properties of the atria are also different between men and women [23, 24]. Therefore, there may be gender differences in the association of blood lipids and the risk of AF recurrence. In this study, lower TC and LDL-C levels were associated with a higher risk of AF recurrence after catheter ablation in women, but not men. Similar to our results, the Niigata Preventive Medicine study [25] found that cholesterol levels were inversely associated with the incidence of AF, and the association of lipid levels with AF was significant in women, but there was a weak association in men. And their study suggested that changes in lipid levels after menopause may result in a stronger effect of lipid levels on the susceptibility to AF in women, so a large sample size of pre- and post-menopausal female is required to verify that hypothesis. As previously reported, increasing inflammation is associated with AF, while one report demonstrated that the LDL-C level was inversely related to CRP level only in women [26], so low levels of lipoproteins may increase the risk of AF recurrence by increasing inflammation in women.
Determining the risk factors for AF recurrence after catheter ablation allows physicians to better select patients with higher success rates and can provide insights into the development of new preventive treatments. We presently disclosed that lower cholesterol was not beneficial for the reduction of AF recurrence, but rather increases the risk of AF recurrence in women, this suggests that the use of statins or other lipid-lowering therapies in women undergoing RFCA requires comprehensive and careful consideration of a variety of factors. Moreover, how to prevent the recurrence of AF after catheter ablation in patients with low cholesterol in clinical practice needs to be further explored.
4.1 Study limitations
In our study, TC and LDL-C showed an inverse association with AF recurrence, and after dividing the total population by sex, this relationship was only significant in women. However, the sample size of women in this study was not large and underpowered for this analysis. A larger sample size is needed to further explore the correlation between blood lipids and the recurrence of AF in different genders. Furthermore, blood lipid levels of the population were measured at baseline before ablation and further study should include blood lipid levels at follow-up, especially with AF recurrence. Another limitation is that the diagnosis of AF recurrence was based on symptoms, ECG, and Holter-ECG findings. The mechanism of higher AF recurrence rates after catheter ablation in patients with a low level of blood lipids remains to be investigated.
5 Conclusions
In conclusion, TC and LDL-C were inversely associated with recurrence of AF after catheter ablation, and this association was significant in women, but not in men. HDL-C and TG were not independently associated with AF recurrence in both genders. Our study was the first to find that there is an inverse association between blood lipids and AF recurrence after RFCA. However, the sample size of women in this study was not large, and a larger sample size is needed to further explore the correlation between blood lipids and the recurrence of AF in different genders, and future studies are needed to disclose potential mechanisms of these associations.
References
Allan V, Honarbakhsh S, Casas J, Wallace J, Hunter R, Schilling R, et al. Are cardiovascular risk factors also associated with the incidence of atrial fibrillation? A systematic review and field synopsis of 23 factors in 32 population-based cohorts of 20 million participants. Thromb Haemost. 2017;117(5):837–50.
Annoura M, Ogawa M, Kumagai K, Zhang B, Saku K, Arakawa K. Cholesterol paradox in patients with paroxysmal atrial fibrillation. Cardiology. 1999;92(1):21–7.
Mora S, Akinkuolie A, Sandhu R, Conen D, Albert C. Paradoxical association of lipoprotein measures with incident atrial fibrillation. Circ Arrhythm Electrophysiol. 2014;7(4):612–9.
Psaty B, Manolio T, Kuller L, Kronmal R, Cushman M, Fried L, et al. Incidence of and risk factors for atrial fibrillation in older adults. Circulation. 1997;96(7):2455–61.
Mourtzinis G, Kahan T, Bengtsson Boström K, Schiöler L, Cedstrand Wallin L, Hjerpe P, et al. Relation between lipid profile and new-onset atrial fibrillation in patients with systemic hypertension (from the Swedish primary care cardiovascular database [SPCCD]). Am J Cardiol. 2018;122(1):102–7.
Li X, Gao L, Wang Z, Guan B, Guan X, Wang B, et al. Lipid profile and incidence of atrial fibrillation: a prospective cohort study in China. Clin Cardiol. 2018;41(3):314–20.
Haïssaguerre M, Gencel L, Fischer B, Le Métayer P, Poquet F, Marcus F, et al. Successful catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 1994;5(12):1045–52.
Cheema A, Vasamreddy CR, Dalal D, Marine JE, Dong J, Henrikson CA, et al. Long-term single procedure efficacy of catheter ablation of atrial fibrillation. J Interv Card Electrophysiol : an international journal of arrhythmias and pacing. 2006;15(3):145–55.
Chang S, Tuan T, Tai C, Lin Y, Lo L, Hu Y, et al. Comparison of outcome in catheter ablation of atrial fibrillation in patients with versus without the metabolic syndrome. Am J Cardiol. 2009;103(1):67–72.
Mohanty S, Mohanty P, Di Biase L, Bai R, Pump A, Santangeli P, et al. Impact of metabolic syndrome on procedural outcomes in patients with atrial fibrillation undergoing catheter ablation. J Am Coll Cardiol. 2012;59(14):1295–301.
Calkins H, Hindricks G, Cappato R, Kim Y, Saad E, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275–444.
Lopez F, Agarwal S, Maclehose R, Soliman E, Sharrett A, Huxley R, et al. Blood lipid levels, lipid-lowering medications, and the incidence of atrial fibrillation: the atherosclerosis risk in communities study. Circ Arrhythm Electrophysiol. 2012;5(1):155–62.
Alonso A, Yin X, Roetker N, Magnani J, Kronmal R, Ellinor P, et al. Blood lipids and the incidence of atrial fibrillation: the multi-ethnic study of atherosclerosis and the Framingham heart study. J Am Heart Assoc. 2014;3(5):e001211.
Jiang H, Wang W, Wang C, Xie X, Hou Y. Association of pre-ablation level of potential blood markers with atrial fibrillation recurrence after catheter ablation: a meta-analysis. Europace. 2017;19(3):392–400.
Quist-Paulsen P. Statins and inflammation: an update. Curr Opin Cardiol. 2010;25(4):399–405.
Suleiman M, Koestler C, Lerman A, Lopez-Jimenez F, Herges R, Hodge D, et al. Atorvastatin for prevention of atrial fibrillation recurrence following pulmonary vein isolation: a double-blind, placebo-controlled, randomized trial. Heart Rhythm. 2012;9(2):172–8.
Yang Q, Qi X, Dang Y, Song X, Hao X. Impact of statin therapy on recurrence of persistent atrial fibrillation after electrical cardioversion: a meta-analysis. Zhonghua Xin Xue Guan Bing Za Zhi. 2015;43(11):994–8.
Sousa P, Providência R, Albenque J, Khoueiry Z, Combes N, Combes S, et al. Impact of free thyroxine on the outcomes of left atrial ablation procedures. Am J Cardiol. 2015;116(12):1863–8.
Tang R, Liu D, Dong J, Liu X, Long D, Yu R, et al. High-normal thyroid function and risk of recurrence of atrial fibrillation after catheter ablation. Circ J. 2010;74(7):1316–21.
Dart C. Lipid microdomains and the regulation of ion channel function. J Physiol. 2010;588(Pt 17):3169–78.
Kim S, Kim J, Shin D, Kim J, Cho K. Relation of atrial fibrillation (AF) and change of lipoproteins: male patients with AF exhibited severe pro-inflammatory and pro-atherogenic properties in lipoproteins. Clin Biochem. 2014;47(10–11):869–75.
Kimura T, Takatsuki S, Inagawa K, Katsumata Y, Nishiyama T, Nishiyama N, et al. Serum inflammation markers predicting successful initial catheter ablation for atrial fibrillation. Heart Lung Circ. 2014;23(7):636–43.
Lew J, Sanghavi M, Ayers C, McGuire D, Omland T, Atzler D, et al. Sex-based differences in cardiometabolic biomarkers. Circulation. 2017;135(6):544–55.
Tse H, Oral H, Pelosi F, Knight B, Strickberger S, Morady F. Effect of gender on atrial electrophysiologic changes induced by rapid atrial pacing and elevation of atrial pressure. J Cardiovasc Electrophysiol. 2001;12(9):986–9.
Watanabe H, Tanabe N, Yagihara N, Watanabe T, Aizawa Y, Kodama M. Association between lipid profile and risk of atrial fibrillation. Circ J. 2011;75(12):2767–74.
Folsom AR, Pankow JS, Tracy RP, Arnett DK, Peacock JM, Hong Y, et al. Association of C-reactive protein with markers of prevalent atherosclerotic disease. Am J Cardiol. 2001;88(2):112–7.
Acknowledgements
We gratefully acknowledge all the participants in our study and we also thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Funding
This study was supported by the National Science Foundation for Young Scholars of China (Grant nos. 30900612 and 81800231), the Clinical Research Fund of Zhejiang Provincial Medical Association (2015ZYC-A16 and 2018ZYC-A11), the Grant of Medical Science Research Foundation of Zhejiang Province (Grant no. 2018ZD017), grants from the Zhejiang Provincial Natural Science Foundation (Grant no. LY15H020002 and Y17H020020), and a grant from the Department of Science and Technology, Zhejiang Province (Grant no. LGF19H020011), People’s Republic of China.
Author information
Authors and Affiliations
Contributions
Yunpeng Shang, Nan Chen, and Qiqi Wang conceived the idea for the research, wrote the framework, and drafted the manuscript as the principal author. Chengui Zhuo and Jianqiang Zhao were responsible for the data analysis and revision of the paper and made substantial contributions to the study conception and framework and design. Ning Lv and Yuan Huang performed the statistical analysis and made substantial contributions to the study conception and framework. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the First Affiliated Hospital of Zhejiang University.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Rights and permissions
About this article
Cite this article
Shang, Y., Chen, N., Wang, Q. et al. Blood lipid levels and recurrence of atrial fibrillation after radiofrequency catheter ablation: a prospective study. J Interv Card Electrophysiol 57, 221–231 (2020). https://doi.org/10.1007/s10840-019-00543-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00543-w