Abstract
Purpose
The combination of left atrial appendage (LAA) occlusion with pulmonary vein isolation (PVI) potentially represents a comprehensive treatment for atrial fibrillation (AF), controlling symptoms while at the same time reducing the risk of stroke and the need for chronic anticoagulation. The aim of this randomized clinical trial was to assess the impact of LAA closure added to PVI in patients with high-risk AF.
Methods
Patients with a history of symptomatic paroxysmal or persistent AF refractory to ≥2 antiarrhythmic drugs, CHA2DS2-VASc score ≥2, and HAS-BLED score ≥3 were randomized to PVI-only (n = 44) or PVI with LAA closure (n = 45).
Results
Six patients in PVI + LAA closure group crossed over to PVI-only group due to failure of LAA closure device implantation. On-treatment comparisons at the 24 month follow-up revealed that 33 (66 %) of the 50 PVI group and 23 (59 %) of the 39 PVI with LAA closure group were AF-free on no antiarrhythmic drugs (p = 0.34). The PVI + LAA closure treatment was significantly associated with a higher AF burden during the blanking period: 9.7 ± 10.8 vs 4.2 ± 4.1 % (p = 0.004). At the end follow-up, there were no serious complications and no strokes or thromboembolic events in either group.
Conclusions
The combination of LAA closure device implantation with PVI was safe but was not observed to influence the success of PVI in patients with symptomatic refractory AF. Early AF after ablation, however, is increased by LAA closure.
Clinical Trial Registration
URL: http://www.clinicaltrials.gov. Unique identifier: NCT01695824.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cerebral stroke is one of the major complications of atrial fibrillation (AF) because of formation of atrial thrombi. The left atrial appendage (LAA) is the source of thrombi in more than 90 % of patients with non-valvular AF, [1] and thus percutaneous catheter-based devices have been developed to close and thereby effectively exclude the LAA from the systemic circulation. Pilot studies have shown acceptable risk-to-benefit ratios for these non-pharmacological alternatives to chronic warfarin therapy [2].
Catheter ablation using pulmonary vein isolation (PVI) has been shown to be an effective therapy for the treatment of drug-refractory AF. However, several studies have shown that together with the PVs, many extra-PV areas may be the source of initiation and maintenance of AF [3, 4]. Indeed, the LAA has been reported to be a potential trigger for AF, and electrical isolation of the LAA may enhance the success of ablative treatment of AF [3, 4].
The combination of LAA occlusion with catheter ablation might be a comprehensive way to ameliorate the symptoms of AF while at the same time reducing the risk of stroke and abolishing the need for vitamin K antagonists (VKA) or other anticoagulants. In a recent study in patients with non-valvular AF with a moderate to severe risk of stroke or contraindication for VKA, it was demonstrated that the combination of PVI with LAA closure device implantation could be safely performed [5]. It was also reported that LAA closure produced acute reductions in LAA unipolar and bipolar voltages, suggestive of LAA ischemic necrosis. If these changes were a marker of long-term electrical LAA isolation, there is the potential to improve the efficacy of PVI [6].
We hypothesized that LAA closure implantation could have a salutary effect on AF patterns by reduction of the electrical activity in the LAA, recognizing the possibility that AF could worsen by a mechanical irritant effect. The aim of this prospective randomized open label study was to assess the impact of LAA closure implantation added to PVI in patients with a history of AF.
2 Methods
The study protocol was approved by the local ethics committee and conducted in compliance with the protocol and in accordance with standard institutional operating procedures and the Declaration of Helsinki. All patients enrolled in the study provided written informed consent.
2.1 Patient eligibility
Patients with a history of symptomatic paroxysmal (P) AF and/or persistent (Pers) AF and CHA2DS2-VASc score ≥2 and HAS-BLED score ≥3 were eligible for this study.
Inclusion criteria are as follows:
-
1.
Symptomatic drug-refractory non-valvular AF (with history of failure of ≥2 class I or III antiarrhythmic drugs) in patients referred for catheter ablation of AF
-
2.
PAF with ≥1 monthly episodes or PersAF in patients who had already undergone ≥3 electrical cardioversions: PAF was defined as episodes lasting less than 7 days with spontaneous termination. PersAF was defined as lasting more than 7 days before being terminated pharmacologically or by electrical cardioversion
-
3.
CHA2DS2-VASc (acronym for congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, and prior stroke or transient ischemic attack, vascular disease, age 65–74 years, sex) risk score ≥2
-
4.
HAS-BLED (acronym for hypertension, abnormal renal-liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly 65 years, drugs or alcohol concomitantly) risk score ≥3
Exclusion criteria include the following:
-
Comorbidities other than AF that required chronic warfarin use
-
Congestive heart failure with NYHA II–IV symptoms
-
Left ventricular ejection fraction <35 %
-
Transverse left atrial diameter >60 mm on transthoracic echocardiography
-
Previous AF ablation procedure
-
Treatment with amiodarone
-
Type 1 diabetes mellitus
Patients were randomized to PVI only (n = 48) or PVI with percutaneous implantation of the LAA closure device (n = 48) using a coded envelope system opened on the day of the procedure. All patients were followed for at least 24 months to assess maintenance of sinus rhythm by means of an implanted cardiac monitor (Fig. 1).
The primary endpoint of the study was time to first recurrence of >30 s of atrial tachyarrhythmia, including AF and left atrial flutter/tachycardia, after a single ablation procedure on no antiarrhythmic drug over 24 months of follow-up. The blanking period (the first 3 months after ablation) was excluded from endpoint analysis [7]. The secondary endpoints were safety data at 3, 6, 9, 12, 18, and 24 months after procedure, AF burden during the blanking period, and AF burden during the 24 months follow-up based on implantable loop recorder (ILR) findings.
2.2 Pulmonary vein isolation
The ablation procedure has been defined in detail previously [8]. At the beginning of the procedure, patients could have either sinus rhythm or AF. All procedures were performed under conscious or moderate sedation.
The left atrium and PVs were explored through a transseptal approach. Real-time 3D LA maps were reconstructed by using a nonfluoroscopic navigation system (CARTO, Biosense-Webster Inc.). The ipsilateral left and right PVs were encircled in one lesion line by circumferential PVI. Radiofrequency energy was delivered at 43 °C, 35 W, and 0.5 cm away from the PV ostia at the anterior wall and was reduced to 43 °C, 30 W, and 1 cm away from the PV ostia at the posterior wall, with a saline irrigation speed of 17 mL/min. RF was delivered continuously at each site until the local potential amplitude decreased by >80 % or RF energy delivery exceeded 40 s. We did not perform either complex fractionated atrial electrogram ablation or LAA isolation. Patients with PAF and PersAF were ablated using the same lesion sets.
The endpoint of ablation was complete PVI; this was confirmed when Lasso catheter mapping showed the disappearance of all PV potentials or the dissociation of PV potentials from LA activity. We performed monitoring for PV reconduction at 20 min following the last ablation. We did not use isoproterenol or adenosine to assess for dormant PV conduction.
The protocol included burst pacing (25 impulses with stepwise reduction of pacing cycle length from 300 ms down to 200 ms). Sustained rhythms were defined as those lasting greater than 2 min. For patients with induced left atrial flutter, additional RF ablation lines were created by connecting the left inferior PV to the mitral annulus (mitral isthmus) and the roof of the LA between the two superior PVs, depending on mechanism of induced flutter. No empiric lesions sets were created in the LA. In the case of registration or induction of typical atrial flutter, the cavo-tricuspid isthmus was ablated. Bidirectional conduction block across the lines was assessed in all patients by differential pacing. If still in AF at the end of the procedure, patients were converted to sinus rhythm electrically.
2.3 LAA closure procedure
The design, structure, and method of deploying the Watchman device (Boston-Scientific, MapleGrove, MN) have been described previously [9, 10]. Briefly, the device consists of a self-expanding nitinol frame with fixation barbs and a permeable, polyester fabric covering. The Watchman implantation was performed immediately after the ablation procedure by using fluoroscopy and transesophageal echocardiographic guidance. All measurements of the LAA were performed after ablation. A device size approximately 20 % larger than the largest diameter of the LAA body (as measured by angiography and TEE) was chosen to have sufficient compression for stable positioning. An appropriately sized Watchman device (21–33 mm in diameter) was advanced to the ostium of the LAA through a 12-F sheath. Proper positioning and stability were verified by transesophageal echocardiography and angiography before device release.
2.4 Implantable loop recorder
The ILR (Reveal XT, Medtronic, Inc., Minneapolis, MN) was implanted on the day of the ablation procedure. The ILR protocol has been defined in detail previously [8]. The device stores the amount of AF per day (daily AF burden, hours of AF in 1 day) and the AF burden of the overall follow-up period, defined as the percentage of time spent in AF (AF%). In addition, the ECG is stored for the visual confirmation of AF episodes. AF was visually verified by investigators through the analysis of the stored ECGs. By accumulating data from multiple follow-up sessions, it was possible to discern the trend in the AF burden over prolonged periods.
2.5 Follow-up
In both groups, patients received warfarin at least 1 month before ablation (with international normalized ratio (INR) maintained between 2 and 3). On the day of the ablation procedure, patients did not receive warfarin. Patients were fully heparinized with a target ACT >300 s immediately after transseptal access in both groups. The use of warfarin just after procedure was based on the INR value.
All patients were treated with antiarrhythmic drugs (propafenone or flecainide) for 6 weeks after PVI; these drugs were subsequently withdrawn, regardless of the cardiac rhythm, in order to prevent their influence after the blanking period.
In PVI + LAA closure group, patients were treated with warfarin for 45 days to facilitate device endothelialization. TEE imaging was done at 45 days, 6 months, and 12 months to assess residual peri-device flow and device stability and position. The TEE interpretation at the time of the procedure as well as TEE during follow-up was performed by the same echocardiographer. Patients discontinued warfarin therapy if the 45-day TEE showed either complete closure of the LAA or if there was limited residual peri-device flow (jet <5 mm in width). After stopping of warfarin, daily clopidogrel 75 mg and aspirin (81–325 mg) were prescribed until the 6-month follow-up visit, at which time clopidogrel was discontinued and aspirin alone was continued indefinitely.
Patients in the PVI only group received warfarin for the duration of the study (target INR between 2 to 3). Monitoring of the INR was done by the patient’s treating physician at least every 2 weeks for 6 months and at least once a month thereafter.
Weekly ECGs were obtained for the first month, and 24-h Holter recordings were performed at 3, 6, 9, 12, 18, and 24 months. Patients were instructed to report symptoms suggestive of AF and to undergo prompt ECG recording. Patients were provided with the patient assistant, a tool that allows each patient to store the ECG through the implanted device during symptoms, in order to analyze heart rhythm during symptomatic events. Holter, ECG, and ILR interpretation was by consensus of two physicians blinded to the phase of the study (i.e., baseline or follow-up) and assigned study treatment.
2.6 Statistical analysis
The primary endpoint of the study was time to the first recurrence of any atrial tachyarrhythmia >30 s after a single ablation procedure when the first 3 months following ablation had elapsed. A secondary endpoint was AF burden, the duration of AF divided by the total time in study in percentages.
Results are presented as mean values ± standard deviation (SD) or as absolute values and percentages, as appropriate. Continuous variables were compared by Student’s t test or the Mann–Whitney U test when the nature of the data did not assume normal distribution. The analysis for categorical variables was conducted using the chi-square test.
For the primary endpoint, Kaplan-Meier analysis was performed to determine the probability of success and estimated as the percentage of patients with first recurrence of any atrial tachyarrhythmia. Differences in arrhythmia-free survival, i.e., time to the first AF onset, were assessed by using the log-rank test. Linear and Cox regression analyses were used to evaluate independent predictors of AF burden and AF recurrences, respectively. The baseline characteristics, presented in Table 1, were included in the regression models. The results are presented as hazard ratio (HR) and 95 % confidence interval (CI) for the Cox regression and treatment difference and 95 % CI.
The comparison of outcomes in study groups followed the intention-to-treat principle. In addition, because several patients were unable to have successful LAA closure performed, we have also provided on-treatment endpoint analysis.
All reported p values were based on two-sided tests, and p values less than 0.05 were considered significant. All statistical calculations were performed by using the SPSS version 13.0 software (SPSS Inc, Chicago, IL, USA).
3 Results
3.1 Study Patients
We enrolled 96 patients (48 randomized to PVI only and 48 to PVI with LAA closure device), all of whom were followed for 24 months after ablation. Four patients (8 %) of the 48 in the PVI only group and 3 patients (6 %) of the 48 in the PVI with LAA closure device implantation group were lost to follow-up without outcome data and were excluded from analysis (Fig. 1). The remaining 89 patients and their outcomes are presented. Table 1 shows the baseline characteristics of the patient population; the clinical characteristics of patients in the two groups did not differ significantly.
3.2 Procedural results
Complete disconnection of the PVs from the LA was successfully achieved in all 89 patients. Cavo-tricuspid isthmus ablation was successfully performed in all 37 patients with a history of atrial flutter, 20 in the PVI only group, and 17 in the PVI with LAA closure group. Three patients (two in the PVI only group and one in the PVI with LAA closure device implantation group) with induced LA flutter during the procedure had additional mitral isthmus and/or roof line created.
The LAA closure device was successfully implanted after PVI in 39 (87 %) of the 45 patients assigned to this intervention. Six patients in PVI + LAA closure group were crossed over to PVI only group due to failure of LAA closure device implantation (Fig. 1).
The mean total duration of the procedure was 151 ± 24 min for PVI-only group compared to 189 ± 29 min for PVI with LAA closure group (including 36 ± 7 min for LAA closure device implantation) (p = 0.16).
Eighty-seven patients (98 %) agreed to receive ILR implantation, 42 patients (95 %) in the PVI only group and 45 patients (100 %) in the PVI with LAA closure device implantation group. The other two patients refused ILR implantation.
3.3 Time to the first recurrence of any atrial tachyarrhythmia (primary endpoint)
By intention-to-treat, at the 24-month follow-up examination, 29 (66 %) of the 44 PVI-only group and 27 (60 %) of the 45 PVI with LAA closure group were AF/AT-free on no antiarrhythmic drugs (p = 0.49, log-rank test) (Fig. 2a).
Six patients in the PVI with LAA closure device implantation group were effectively in the PVI-only group after failure of LAA closure device deployment. The on-treatment comparisons at the 24-month follow-up indicated that 33 (66 %) of the 50 PVI only patients and 23 (59 %) of the 39 PVI with LAA closure patients were AF/AT-free on no antiarrhythmic drugs (p = 0.34, log-rank test) (Fig. 2b).
Six patients (12 %) in the PVI only group and four patients (10 %) in the PVI with LAA closure with recurrent AF underwent re-ablation (p = 0.79) due to sustained episodes of AF recurrences associated with antiarrhythmic drug failure.
3.4 AF burden
During the 3-month blanking period, 38 patients (43 %) were AF-free. Of these, 23 patients (46 %) were in the PVI-only group, and 15 patients (38 %) were in the PVI with LAA closure group (p = 0.48).
Based on ILR data at the first month follow-up, AF% was significantly higher in the PVI with LAA closure group than PVI-only group, 9.7 ± 10.8 and 4.2 ± 4.1 %, respectively (p = 0.004) (Fig. 3). At the end of the blanking period, the AF% dramatically decreased in both groups, and AF% was similar in the PVI with LAA closure (2.8 ± 2.6 %) and PVI-only groups (2.2 ± 2.7 %) (p = 0.31).
After the blanking period, the AF% during the next 21-month follow-up was similar in both groups (Fig. 3).
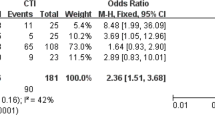
3.5 Predictors of AF burden and recurrences
On multivariate linear regression analysis, higher AF burden was associated with the type of the treatment and was significantly higher in the PVI + LAA closure treatment group compared to the PVI only during the blanking period. The regression slope for interaction between the time and treatment was highly significant 2.46 (95 % CI 1.35–3.58, p < 0.0001). Similar analysis of AF burden during the follow-up did not show significant interaction between type of treatment in both groups and time after the procedure, −0.02 (95 % CI −0.1 to 0.06, p = 0.58; Table 2).
Cox regression, adjusted to prespecified baseline characteristics (AF type, hypertension, age, CHA2DS2-VASc score), did not identify an association between AF recurrence and the type of treatment either during the blanking period or during follow-up with HR 0.89 [95 % CI 0.51–1.55; p = 0.69] and HR 0.76 [95 % CI 0.37–1.55; p = 0.45], respectively (Table 3).
3.6 Safety data
There were no procedure-related complications either to LAA closure device implantation or PVI procedure in PVI + LAA closure group. In one patient who was assigned to PVI-only group, cardiac tamponade occurred (p = 0.38). The patient recovered uneventfully after immediate pericardiocentesis. One patient (2 %) in the PVI-only group and two patients (5 %) PVI with LAA closure device implantation group developed a groin hematoma (p = 0.42).
At the 45-day follow-up, 31 (79 %) of 39 patients with LAA closure device met TEE criteria and were able to stop taking warfarin. One (3 %) of the 39 patients had spontaneous contrast in the left atrium (device embolization), requiring continuation of VKA therapy. In the other seven patients, there was minimal residual flow. At 6 months, all of them demonstrated complete occlusion and the VKA was discontinued. None of the patients had dislocation of the LAA closure device.
At the end of follow-up, no thromboembolic events and no severe bleeding events had occurred in either group.
4 Discussion
To the best of our knowledge, this is a first prospective randomized study for assessment of the long-term outcome after PVI only vs PVI with LAA closure device implantation. The main findings of this study were as follows: (1) LAA closure device implantation did not have any impact on AF recurrences in refractory AF patients with CHA2DS2-VASc score ≥2 and HAS-BLED score ≥3 who also underwent PVI; (2) combination LAA closure device implantation with PVI was associated with an early higher AF burden during the blanking period; and (3) LAA closure implantation added to PVI in patients with AF was safe and did not alter the incidence of postoperative complications.
The results of PROTECT AF and PREVAIL trials have demonstrated that LAA occlusion with the Watchman device is noninferior to systemic treatment with warfarin in terms of thromboembolic event prevention and cardiovascular death even in long-term follow-up in patients with AF [2, 9, 10]. However, there is only one report from a nonrandomized prospective registry regarding feasibility of the LAA closure device implantation in combination with PVI [5].
Previously published studies have shown that the single-procedure ablation success rate in patients with PAF and PersAF varies from 20 to 70 % and dramatically decreased during long-term follow-up, especially in patients with non-PAF [11–13]. Theoretically, the implantation of the LAA closure device in combination with PVI could increase the efficacy of the ablation procedure, prevent thromboembolic events, and eliminate adverse effects of chronic warfarin. The increase of the ablation procedure efficacy could be achieved by elimination of non-PV LAA triggers, which can be responsible for initiation and maintenance of AF [14–17].
Di Biase et al. have suggested that the LAA is responsible for recurrence of AF/AT in at least 27 % of patients [3]. The optimal treatment was found to be complete circumferential LAA isolation. Because the Watchman device lies within the LAA itself, the combination of PVI isolation and LAA closure could lead to two possible, non-mutually exclusive, outcomes: (1) deterioration of results due to the irritating influence of the device or (2) salutary effect on AF patterns by reduction of the electrical activity in the LAA. Moreover, a high-risk patient group might especially benefit from LAA closure by reducing the risk of stroke and abolishing the need for chronic anticoagulant therapy.
There is a concern that LAA isolation via loss of LAA contractility could induce thrombus formation. However, it is still not clear regarding the influence of LAA electrical isolation and long-term thromboembolic events [4, 17].
Interestingly, PVI performed in combination with LAA closure device implantation resulted in higher AF burden in the blanking period, possibly from inflammation or mechanical irritation within the LAA with trigger activity due to lack of electrical isolation of the LAA. Nevertheless, the AF burden in both groups was comparably decreased at the end of follow-up. Epicardial LAA closure can potentially lead to electrical and mechanical isolation of LAA [18, 19].
It is important to emphasize as well that the combined procedure, i.e., when adding LAA closure to AF ablation, was completed in the vast majority of patients, was not associated with additional complications, and incremented procedure time by only a small amount. This paradigm will undoubtedly undergo further scrutiny in future investigations but is attractive for its potential as a combined antiarrhythmic and anti-embolic intervention in high-risk patients.
4.1 Limitations
In our study, the implantation of the LAA closure device did not improve long-term efficacy in terms of AF recurrences; however, we did not perform formal electrical isolation of the LAA nor test for it. Also, the results of our study with regard to periprocedural safety were in accordance with previous published data [5]. None of the patients in either group developed thromboembolic events during follow-up regardless of the presence or absence of the AF recurrences. These findings need to be studied in a larger patient cohort with long-term follow-up and focused on this critical outcome. This was the first randomized study of combined LAA closure implantation and AF ablation so that a limited number of patients were enrolled. Although the study was randomized, the results will require validation in additional and larger trials. As our data refers to a follow-up period of 24 months after the ablation procedure, we cannot extrapolate our results to the long-term maintenance of sinus rhythm or prevention of thromboembolic events.
5 Conclusions
The combination of LAA closure device implantation with PVI was safely performed but did not seem to influence the long-term success of PVI in patients with symptomatic refractory AF.
References
Stoddard, M. F., Dawkins, P. R., Price, C. R., & Ammash, N. M. (1995). Left atrial appendage thrombus is not uncommon in patients with acute atrial fibrillation and a recent embolic event: a transesophageal echocardiographic study. Journal of the American College of Cardiology, 25, 452–459.
Holmes, D. R., Reddy, V. Y., Turi, Z. G., Doshi, S. K., Sievert, H., Buchbinder, M., et al. (2009). Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet, 374(9689), 534–542.
Di Biase, L., Burkhardt, J. D., Mohanty, P., Sanchez, J., Mohanty, S., Horton, R., et al. (2010). Left atrial appendage: an underrecognized trigger site of atrial fibrillation. Circulation, 122(2), 109–118.
Takahashi, Y., Sanders, P., Rotter, M., & Haissaguerre, M. (2005). Disconnection of the left atrial appendage for elimination of foci maintaining atrial fibrillation. Journal of Cardiovascular Electrophysiology, 16, 917–919.
Swaans, M. J., Post, M. C., Rensing, B. J., & Boersma, L. V. (2012). Ablation for atrial fibrillation in combination with left atrial appendage closure: first results of a feasibility study. The Journal of American Heart Association, 1(5), e002212.
Han, F. T., Bartus, K., Lakkireddy, D., Rojas, F., Bednarek, J., Kapelak, B., et al. (2014). The effects of LAA ligation on LAA electrical activity. Heart Rhythm, 11(5), 864–870.
Joshi, S., Choi, A. D., Kamath, G. S., Raiszadeh, F., Marrero, D., Badheka, A., et al. (2009). Prevalence, predictors, and prognosis of atrial fibrillation early after pulmonary vein isolation: findings from 3 months of continuous automatic ECG loop recordings. Journal of Cardiovascular Electrophysiology, 20, 1089–1094.
Pokushalov, E., Romanov, A., Corbucci, G., Artyomenko, S., Turov, A., Shirokova, N., et al. (2011). Ablation of paroxysmal and persistent atrial fibrillation: 1-year follow-up through continuous subcutaneous monitoring. Journal of Cardiovascular Electrophysiology, 22, 369–375.
Reddy, V., Doshi, S., Sievert, H., Buchbinder, M., Neuzil, P., Huber, K., et al. (2013). Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-year follow-up of the PROTECT AF (Watchman Left Atrial Appendage System for Embolic Protection in Patients with Atrial Fibrillation) Trial. Circulation, 127, 720–729.
Holmes, D., Kar, S., Price, M., Whisenant, B., Sievert, H., Doshi, S., et al. (2014). Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. Journal of the American College of Cardiology, 64, 1–12.
Steinberg, J. S., Palekar, R., Sichrovsky, T., Arshad, A., Preminger, M., Musat, D., et al. (2014). Very long-term outcome after initially successful catheter ablation of atrial fibrillation. Heart Rhythm, 11, 771–776.
Bertaglia, E., Tondo, C., De Simone, A., Zoppo, F., Mantica, M., Turco, P., et al. (2010). Does catheter ablation cure atrial fibrillation? Single-procedure outcome of drug-refractory atrial fibrillation ablation: a 6-year multicentre experience. Europace, 12(2), 181–187.
Tilz, R., Rillig, A., Thum, A., Arya, A., Wohlmuth, P., Metzner, A., et al. (2012). Catheter ablation of long-standing persistent atrial fibrillation: 5-year outcomes of the Hamburg Sequential Ablation Strategy. Journal of the American College of Cardiology, 60(19), 1921–1929.
Lin, W., Tai, C. T., Hsieh, M., Tsai, C., Lin, Y., Tsao, H., et al. (2003). Catheter ablation of paroxysmal atrial fibrillation initiated by non-pulmonary vein ectopy. Circulation, 107, 3176–3183.
Tsai, C., Tai, C., Hsieh, M., Lin, W., Yu, W., Ueng, K., et al. (2000). Initiation of atrial fibrillation by ectopic beats originating from the superior vena cava: electrophysiological characteristics and results of radiofrequency ablation. Circulation, 102, 67–74.
Elayi, C., Fahmy, T., Wazni, O., Patel, D., Saliba, W., & Natale, A. (2006). Left superior vena cava isolation in patients undergoing pulmonary vein antrum isolation: impact on atrial fibrillation recurrence. Heart Rhythm, 9, 1019–10123.
Chan, C., Wong, W., Pumprueg, S., Veerareddy, S., Billakanty, S., Ellis, C., et al. (2009). Inadvertent electrical isolation of the left atrial appendage during catheter ablation of persistent atrial fibrillation. Heart Rhythm, 7, 173–180.
Afzal, M. R., Kanmanthareddy, A., Earnest, M., Reddy, M., Atkins, D., et al. (2015). Impact of left atrial appendage exclusion using an epicardial ligation system (LARIAT) on atrial fibrillation burden in patients with cardiac implantable electronic devices. Heart Rhythm, 12(1), 52–59.
Badhwar, N., Lakkireddy, D., Kawamura, M., Han, F.T., Iyer, S.K. et al. (2015) Sequential percutaneous LAA ligation and pulmonary vein isolation in patients with persistent AF: initial results of a feasibility study. J Cardiovasc Electrophysiol. doi: 10.1111/jce.12655.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical Perspectives
After catheter ablation for atrial fibrillation, some patients with high risk of thromboembolic events are required for continuous use of oral anticoagulants, despite the rhythm status. In the present study, all patients were randomly assigned to receive either pulmonary vein isolation or pulmonary vein isolation combined with left atrial appendage closure device implantation. The findings suggest that left atrial appendage closure device implantation added to pulmonary vein isolation did not significantly increase the freedom from atrial fibrillation recurrences. Atrial fibrillation burden within the blanking period detected by implantable loop recorder was higher in left atrial appendage closure device group, but there was no difference at the end of follow-up in both groups of patients. The results are also demonstrated that in such category of patients with refractory atrial fibrillation and high risk of thromboembolic events and bleeding, who are scheduled for pulmonary vein isolation, left atrial appendage closure device could be safely implanted and did not increase the incidence of postoperative complications. Although the study was randomized, the results need to be confirmed in future larger scale trials with long-term follow-up.
Rights and permissions
About this article
Cite this article
Romanov, A., Pokushalov, E., Artemenko, S. et al. Does left atrial appendage closure improve the success of pulmonary vein isolation? Results of a randomized clinical trial. J Interv Card Electrophysiol 44, 9–16 (2015). https://doi.org/10.1007/s10840-015-0030-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-015-0030-4