Abstract
This study examined the relationship between child emotional and behavioral difficulties, parenting stress and the mental health of caregivers of adolescents living with HIV. Caregiver data from a two-year pilot study for adolescents and their caregivers (N = 89 dyads) in Uganda, were analyzed. Ordinary Least Square regression models were conducted to examine the association between child difficulties reported by caregivers using the Strengths and Difficulties Questionnaire on parenting stress (measured by Parenting Stress Index) and caregiver mental health (measured by the Brief Symptoms Inventory). Results indicate that 12.36% of caregivers reported child difficulty scores within the borderline range and 8.99% reported scores within the abnormal range. Child difficulties (b = 0.52, 95% CI: 0.18, 0.85) were associated with parenting stress. Similarly, the perceived impact of child difficulties was associated with both parenting stress (b = 0.89, 95% CI: 0.24, 1.54) and caregiver mental health (b = 1.73, 95% CI: 1.09, 2.37). Study findings have important implications for developing effective psychosocial interventions targeting children and adolescents living with HIV and their caregivers.
Highlights
-
Child emotional and behavioral difficulties (EBDs) have been documented to predict parental mental health distress.
-
In our study, 12% of caregivers reported EBD scores within the borderline range and 9% reported scores within the abnormal range.
-
EBDs were associated with both caregiver parenting stress and mental health distress.
-
Findings point to the need for the development of effective psychosocial interventions targeting adolescents living with HIV and their caregivers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Children and adolescents living with HIV are at a higher risk of emotional and behavioral difficulties (EBDs) (Dessauvagie et al., 2020; Vreeman et al., 2017). Increased risk of hyperactivity, impulsivity and attention deficit, as well as depression, anxiety, and conduct problems, have been observed among adolescents living with HIV (ALHIV) (Pillay et al., 2021; Too et al., 2021). Among ALHIV in sub-Saharan Africa (SSA), a high prevalence of EBDs has been documented, with 24–27% of adolescents scoring positive for any psychiatric disorders and 30–50% exhibiting emotional, behavioral difficulties or significant psychological distress (Dessauvagie et al., 2020; Musisi & Kinyanda, 2009). Studies have documented correlates of EBDs among ALHIV, including older age, lower income, orphanhood, higher viral load, low level of family functioning, living with non-biological parents (Kalembo et al., 2019; Mellins & Malee, 2013; Ruiseñor-Escudero et al., 2015; Tadesee et al., 2012), as well as caregiver factors, such as low education level, young age and lack of employment (Jantarabenjakul et al., 2020; Kefale et al., 2019; Kinyanda et al., 2019; Webster et al., 2019). If not addressed, children and adolescents with HIV and EBD comorbidities are at a higher risk of poorer health outcomes across the HIV care continuum, including non-engagement in care, non-adherence to medication, elevated viral load and increased opportunistic illnesses (Bucek et al., 2018; Remien et al., 2019).
In addition, caregiver mental health has been documented as a major predictor of child EBDs. For example, in non-HIV population studies, maternal depression was significantly related to higher levels of child internalizing and externalizing behaviors and general psychopathology for children (Alenko et al., 2020; Goodman et al., 2011). Caregiver anxiety and parenting stress were significantly associated with child behavioral problems in Kenya (Laurenzi et al., 2021). Among ALHIV, caregiver depression was associated with child EBDs (Jantarabenjakul et al., 2020; Louw et al., 2016; Webster et al., 2019). Similarly, studies have documented the bidirectional relationship between child EBDs and parental distress (Lin et al., 2021; Rodriguez et al., 2019). In particular, during early childhood (1–5 years), greater child externalizing behavior predicted greater parenting stress (McDaniel & Radesky, 2020), and internalizing behaviors from early to middle childhood (5–10 years) predicted later parenting stress (Woodman et al., 2015).
Very few studies have investigated the mental health of caregivers of ALHIV (Goodrum et al., 2021), especially in SSA settings. However, most studies have focused on young children from early to middle childhood –despite significant changes during early and middle adolescence (McDaniel & Radesky, 2020 Lin et al., 2021; Rodriguez et al., 2019; Woodman et al., 2015). Yet, distressed caregivers may be less responsive to and engaging with their children, more authoritarian and neglectful in their parenting behaviors, and demonstrate poor parent-child communication. In the context of HIV, this may negatively impact child self-regulation, coping strategies, social and behavioral competence (Baumrind, 2013), potentially increasing the risk of non-adherence to medication and overall poor health functioning (Murphy et al., 2010; Rousseau et al., 2013; Schulte et al., 2017). Moreover, given that ALHIV experience unique challenges, the stressors associated with prolonged caregiving can exert an emotional burden on their caregivers. Thus, understanding caregivers’ mental health needs is critical to providing appropriate mental health resources and ensuring that ALHIV receive appropriate support and care from their caregivers in return. To address this gap in the literature, this study examined the relationship between child EBDs and the mental health functioning of caregivers of ALHIV in Uganda.
Theoretical Framework
This study is guided by the stress process model (Pearlin et al., 1990). Within the caregiving context, stressors refer to the problematic conditions and difficult circumstances experienced by caregivers, such as demands and obstacles that exceed an individual’s capacity to adapt (Pearlin et al., 1981; Raina et al., 2004). These stressors arise when demands imposed by a patient’s condition (such as a chronic illness that requires long duration for caregiving) conflict with the caregiver’s ability to respond (Sisk, 2000). Within the context of HIV, prolonged caregiving for children living with a highly stigmatized chronic illiness, as well as managing their social and treatment needs, may place a significant strain on family resources, prevent caregivers from attending to their own health needs, negatively impacting their physical and mental health functioning. As such, we hypothesize that high levels of child EBDs as reported by caregivers will be positively associated with parenting stress and poor mental health functioning.
Methods
Study Sample and Setting
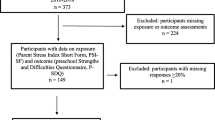
Caregiver data from a pilot study for adolescents and their caregivers (N = 89 dyads) in Uganda, were analyzed. Study participants were identified and recruited from 9 comparable health care clinics across four political districts within the greater Masaka region of Uganda –a region with a high HIV prevalence compared to the national average (Uganda Ministry of Health, 2021). Adolescent inclusion criteria include: 1) living with HIV and aware of their status; 2) between 10–14 years; 3) taking prescribed antiretrovial therapy (ART) and receiving care from participating health clinics; and 4) living within a family, including with extended family. Caregivers were eligible if they identified as the primary caregiver of the adolescent and were willing to complete study activities. Detailed study procedures are provided in the study protocol (Nabunya et al., 2022).
Participant Screening and Recruitment
Screening and recruitment of participants took place between November 2020 and May 2021. Clinics were comparable in terms of the number of adolescents served, facility level and having adolescent clinic days. A clinic staff presented the project idea to adult caregivers of eligible children –per the inclusion criteria –during appointment days. Verbal consent to be contacted by a research staff member was obtained from interested caregivers. A total of 147 dyads were screened; among these, 89 dyads met the inclusion criteria. During a one-on-one meeting with the research staff, caregivers were taken through an informed consent process, after which they provided written consent for themselves and their children to participate. Children provided assent separately from their caregivers to avoid coercion.
Data Collection and Measures
Measures utilized in this study have been tested in the study region among caregivers of ALHIV (Kagotho & Ssewamala, 2012; Nabunya et al., 2014; Wang et al., 2014). Data were collected between January and May 2021 during the COVID-19 lockdown, using a 90-minute interviewer-administered questionnaire. Interviews were conducted based on the participant’s preference in a private space at the health clinics or at the participant’s home. Caregivers reported on all measures. All study procedures, including the study measures, were translated into Luganda (the widely spoken local language), and back-translated into English to ensure consistency. The translation was certified by experts from Makerere University’s Center for Language and Communication Services.
Outcome Variables
Caregiver mental health was measured using 34 items from the Brief Symptom Inventory that measures symptoms of anxiety, somatization and depression (Derogatis, 1993). Respondents were asked to rate how they felt emotionally, on a 5-point Likert scale, with 1 = Never true, 2 = rarely true, 3 = true sometimes, 4 = true most of the time and 5 = always true. Sample items include: Feeling that people are unfriendly or dislike you. Feeling inferior to others. The idea that someone else can control your thoughts. Summated scores were created with higher scores representing higher levels of mental health distress (Cronbach’s alpha = 0.83).
Parenting stress was measured using 33 items from the Parenting Stress Index that assesses parental distress, difficult child and caregiver-child dysfunctional relationships (Abidin, 1990). Respondents were asked to rate their parenting stress, on a 4-point Likert scale, with 1 = strongly disagree, 2 = somewhat disagree, 3 = somewhat agree and 4 = strongly agree. Sample items include: You find yourself giving up more of your life to meet your child’s needs than you ever expected. You feel trapped by your responsibilities as a parent. Since you started taking care of this child you have been unable to do new and different things. Summary scores were created, with higher scores indicating higher levels of parenting stress (Cronbach’s alpha = 0.83).
Independent Variables
Emotional and behavioral difficulties were measured using the Child Strengths and Difficulties Questionnaire (SDQ) (Goodman, 2001). The 25-item brief behavioral screening questionnaire includes five subscales related to emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems and prosocial behavior. The scale has been validated in the study region (Nakigudde et al., 2016; Thumann et al., 2016). Responses were rated on a 5-point Likert scale, with 1 = Never, 2 = rarely, 3 = sometimes, 4 = most of the time and 5 = always. Sample items include: Your child has many worries or often seems worried. Your child steals from home, school or elsewhere Your child is easily distracted, concentration wanders. All subscales (excluding prosocial behavior) are summated to create the total difficulties score, with higher scores indicating elevated child difficulties (Cronbach’s alpha = 0.78). Percentiles were created for each of the four subscales and the total difficulties score. Scores above the 90th percentile were considered abnormal, scores between 80–90th percentile were considered borderline, and scores below 80th percentile were considered normal (Hoofs et al., 2015).
The SDQ was supplemented with a 7-item brief impact scale which assesses the perceived impact of the child’s difficulties in terms of distress, social impairment, burden and chronicity on their life, including interfering with their family life, friendships, classroom learning leisure activities, and home life (Goodman, 1999). Responses were rated on a 5-point Likert scale, with 1 = Never, 2 = rarely, 3 = sometimes, 4 = most of the time and 5 = always. Sample items include: “Do the difficulties interfere with your child’s family life? Do the difficulties interfere with your child’s friendships? Do the difficulties interfere with your child’s classroom learning? Higher scores indicate negative impact (Cronbach’s alpha = 0.91).
Finally, caregiver and family-level characteristics included in the analysis as control variables were age, gender, relationship to the child, family cohesion and household asset index. Family cohesion was measured using items adapted from the Family Environment Scale (Moos and Moos, 1994) and the Family Assessment Measure (Skinner et al., 1983), all previously used in the study region (Damulira et al., 2019; Osuji et al., 2018). The 7-item scale assess the degree of commitment, help, and support that family members provide for one another, on a 5-point Likert scale, with 1 = never, 2 = sometimes, 3 = about half of the time, 4 = most of the time, and 5 = always. Sample items include: Do your family members ask each other for help before asking non-family members for help? Do your family members like to spend free time with each other? Do your family members feel close to each other? High scores indicate high levels of family cohesion (Cronbach alpha = 0.72). The household asset index was calculated by summing 17-items assessing the availability of assets, including land, a house, means of transportation, livestock and gardens).
Analytical Procedures
All analyses were performed using Stata version 17. Effects that were significant at p < 0.05 were interpreted. Model diagnostic tests were performed. Multicollinearity was examined using variation inflation factors. All values fell into the acceptable range (<10), indicating that variables were not highly correlated. The normality of residuals was examined with kernel density plot and standardized normal probability plot with slight deviations from normal at the upper tail. The OLS model is robust to handle these minor violations. Using descriptive statistics, means and standard deviations, as well as frequencies and measures of central tendency, were generated to describe caregiver characteristics. Caregiver reports were used to examine the prevalence of child EBDs. Ordinary Least Square (OLS) regression models were conducted to examine the association between caregiver reported EBDs and perceived EBD impact on parenting stress and caregiver mental health. Standard errors and test statistics were adjusted for within-clinic correlation using robust Huber–Whiter sandwich variance estimation (White, 1980).
Results
Sample Characteristics
Caregiver characteristics are summarized in Table 1. The average age for caregivers was 47.3 years, and about three quarters (77.5%) were female. Of the total sample, 49% indicated they were the child’s biological parent and 35% were grandparents. The average score on the family cohesion measure was 26.6 (SD = 5.2). Caregivers reported moderate levels of child EBDs (mean = 41.2, SD = 10.39) and perceived EBD impact (mean = 14.90, SD = 6.95). Similarly, caregivers reported moderate levels of parenting distress (mean = 72.08, SD = 18.47) and mental health distress (mean = 74.54, SD = 22.42).
Prevalence of Emotional and Behavioral Difficulties
The current study focuses on child EBDs, as such, the prosocial subscale was excluded from the analysis. Following Hoofs et al. (2015) approach, we calculated cut-offs for the whole sample and each of the four subscales (Table 2). On the total difficulties score, 12.36% of caregivers reported scores within the borderline range and 8.99% reported scores within the abnormal range. Across subscales, the percentage of caregivers reporting scores in the borderline category ranged between 15.75% (emotional symptoms) to 23.6% (peer problems). Within the abnormal category, the percentage of caregiver reports ranged between 4.49% (peer problems) and 6.74% (emotional symptoms, conduct problems and hyperactivity).
Regression on Parenting Stress and Caregiver Mental Health
Results from regression analysis assessing the association between caregiver reported EBDs, perceived EBD impact on parenting stress and caregiver mental health are presented in Table 3. In model 1, adjusting for caregiver characteristics, child EBDs (b = 0.52, 95% CI: 0.18, 0.85), and perceived EBD impact (b = 0.89, 95% CI: 0.24, 1.54), were associated with parenting stress. Specifically, every unit increase in child EBDs and perceived EBD impact score was associated with higher levels of parenting stress. On the other hand, being the child’s grandparent (b = −12.84, 95% CI: −23.28, −2.40) or other caregiver (aunt, uncle, etc.) (b = −10.14, 95% CI: −18.13, −2.15) were both associated with lower levels of parenting stress.
In model 2, perceived child EBD impact was associated with poorer caregiver mental health (b = 1.73, 95% CI: 1.09, 2.37). On the other hand, household asset index (b = −1.54, 95% CI: −2.72, −0.37), and being the child’s other caregiver (b = −12.36, 95% CI: −19.49, −5.24) were associated with better caregiver mental health. Other predictors were not associated with the outcomes.
Discussion
This study examined the relationship between child EBDs, parenting stress and the mental health functioning of caregivers of ALHIV in Uganda. In our sample, 12% of caregivers reported child EBD scores within the borderline range and 9% reported scores within the abnormal range. This prevalence is lower compared to previous studies that have utilized the SDQ among children and ALHIV in SSA (Kalembo et al., 2019; Kefale et al., 2019; Tadesse et al., 2012. The prevalence is also lower compared to previous studies conducted in Uganda (Kinyanda et al., 2019; Ruiseñor-Escudero et al., 2015), although this might be attributed to the difference in the assessment tools used.
Based on previous studies that have documented the correlates of EBDs among ALHIV (Kalembo et al., 2019; Mellins & Malee 2013; Ruiseñor-Escudero et al., 2015; Tadesee et al., 2012), the low prevalence could be due to the study sample. Specifically, participants were younger (10–14 years), the majority (55%) were non orphans, and almost half of the sample (49%) lived with their biological parents, and reported moderate levels of family closeness (Nabunya and Namuwonge, 2022). Moreover, caregivers were older, with an average of 47 years. As such, it could be that these individual and household-level characteristics could potentially act as protective factors mitigating the risk of EBDs. Taken together, given that children and adolescents living with HIV are at a higher risk of EBDs, resulting in negative developmental outcomes (Dessauvagie et al., 2020), interventions to ensure early screening and detection, and enrollment in treatment programs are critical among ALHIV.
It is critical to point out that while the percentage of caregivers reporting abnormal scores within the peer problems subscale was the lowest across all subscales, it also received the highest percentage of caregivers (23.6%) reporting scores in the borderline category. While peers can potentially be a unique and powerful source of support (Mark et al., 2019), this finding points to peer support challenges among ALHIV. Indeed, items in this subscale were related to having at least one good friend, being liked by peers, getting along with peers, being picked or bullied by peers, and preference to spend time alone rather than with peers. It could be that HIV-related shame, non-disclosure, fear of stigma and peer violence, prohibits adolescents from engaging in supportive peer relationships (Nabunya and Namuwonge, 2022; Kip et al., 2022). Yet, in our previous study with ALHIV, support from peers (friends and classmates) was associated with lower levels of HIV-related stigma (Nabunya et al., 2020). This finding supports the calls for peer support programs for ALHIV that can help strengthen their peer networks to address the multifaceted challenges of living with HIV, including reducing social isolation, and improving health and mental health outcomes on the HIV care continuum (Abrams et al 2021; Casale et al., 2019; Rencken et al., 2021).
Guided by the stress process model (Pearlin et al., 1990, 1981), we hypothesized that high levels of child EBDs as reported by caregivers would be positively associated with parenting stress and poor mental health functioning. Study results support this hypothesis. Specifically, child difficulties and the perceived impact of these difficulties on children’s wellbeing (including interference with family life, friendships, classroom learning, leisure activities, and home life), was associated with parenting stress. On the other hand, only perceived impact of child difficulties was associated with caregiver mental health. These findings align with previous studies in SSA that have documented the HIV burden on families, including the financial, physical and psychological hardships (Atanuriba et al., 2021; Osafo et al., 2017; Sherr et al., 2016). Moreover, caregivers must meet their children’s medical, nutritional needs and overall health wellbeing –which tend to be costly (Lentoor, 2017; Osafo et al., 2017). These demands, combined with child difficulties and HIV-related stigma, further exacerbate caregiver anxiety and mental distress. Taken together, these findings are consistent with previous studies among caregivers of children living with HIV (Goodrum et al., 2021), and other behavioral challenges (Lin et al., 2021; Rodriguez et al., 2019).
Finally, being the child’s non-biological caregiver was associated with lower levels of parenting stress and mental health distress. It could be that other caregivers (grandparents, aunts and uncle) do not have to bear the burden and guilt of transmitting the disease to the child, as opposed to the biological parent – potentially reducing the burden of mental health distress. In addition, ownership of household assets (e.g., a house, land, means of transportation etc.) was associated with lower levels of caregiver mental health. This finding is consistent with previous studies that have documented the importance of family economic stability in reducing mental health distress among caregivers of children affected by HIV (Nabunya et al., 2014; Wang et al., 2014).
Findings should be interpreted in light of the following limitations. First, we analyzed cross-sectional data from a small pilot sample and could not make causal inferences. This is also likely to impact the strength of the association. Therefore, there is a need for longitudinal well-powered studies to examine the association between child behavioral challenges and caregiver mental health. Second, emotional and behavioral difficulties were reported by caregivers and may suffer from social desirability. Adolescents were not assessed on this measure to report on their own functioning. Third, assessments were conducted during the COVID-19 pandemic. The associated challenges may have worsened the mental health functioning of caregivers.
Even with these limitations, study findings have important implications for the development of effective psychosocial interventions targeting ALHIV and their caregivers. Family-related stress tied to HIV and poverty, may undermine parenting, including family organization, discipline practices, family connectedness, support, communication, and contribute to serious child EBDs (Kazdin & Whitley, 2003). Evidence based interventions, such as those focused on family economic stability, can potentially reduce financial, parenting and caregiver mental distress (Nabunya et al., 2014; Ssewamala et al., 2016; Wang et al., 2014). Similarly, group-based family strengthening interventions targeting family processes, including positive behavioral supports, effective behavioral management, parent-child relationships and parent involvements, problem solving, as well as coping, have been tested both in SSA among families impacted by HIV and poverty (Bhana et al., 2014; McKay et al., Sensoy Bahar et al., 2020; Ssewamala et al., 2018), and have proved efficacious in reducing child behavioral health (Brathwaite et al., 2022). A combination of such interventions may potentially address child EBDs and reduce the risk of caregiver mental distress.
Overall, study findings contribute to the limited literature examining the relationship between child emotional and behavioral difficulties and the mental health of caregivers of ALHIV. Future research is needed to understand the mechanisms through which child EBDs impact caregiver mental health. These findings point to the need for interventions to support caregivers of ALHIV to mitigate the burden of caregiving and the impact on their health and wellbeing.
References
Abidin, R. R. (1990). Parenting Stress Index (PSI) manual. Odessa, FL: Psychological Assessment Resources, Inc.
Abrams, E. A., Burke, V. M., Merrill, K. G., Frimpong, C., Miti, S., Mwansa, J. K., & Denison, J. A. (2021). “Adolescents do not only require ARVs and adherence counseling”: a qualitative investigation of health care provider experiences with an HIV youth peer mentoring program in Ndola, Zambia. PLoS ONE, 16(6), e0252349. https://doi.org/10.1371/journal.pone.0252349.
Alenko, A., Girma, S., Abera, M., & Workicho, A. (2020). Children emotional and behavioural problems and its association with maternal depression in Jimma town, southwest Ethiopia. General Psychiatry, 33(4), e100211. https://doi.org/10.1136/gpsych-2020-100211.
Atanuriba, G. A., Apiribu, F., Boamah Mensah, A. B., Dzomeku, V. M., Afaya, R. A., Gazari, T., Kuunibe, J. K., & Amooba, P. A. (2021). Caregivers’ experiences with caring for a child living with HIV/AIDS: a qualitative study in Northern Ghana. Global Pediatric Health, 8, 2333794X211003622. https://doi.org/10.1177/2333794X211003622.
Baumrind, D. (2013). Authoritative parenting revisited: History and current status. In R. E. Larzelere, A. S. Morris & A. W. Harrist (Eds.), Authoritative parenting: synthesizing nurturance and discipline for optimal child development 2013, (11–34). Washington, DC: American Psychological Association.
Bhana, A., Mellins, C. A., Petersen, I., Alicea, S., Myeza, N., Holst, H., Abrams, E., John, S., Chhagan, M., Nestadt, D. F., Leu, C. S., & McKay, M. (2014). The VUKA family program: piloting a family-based psychosocial intervention to promote health and mental health among HIV infected early adolescents in South Africa. AIDS Care, 26(1), 1–11. https://doi.org/10.1080/09540121.2013.806770.
Brathwaite, R., Ssewamala, F. M., Sensoy Bahar, O., McKay, M. M., Neilands, T. B., Namatovu, P., Kiyingi, J., Zmachinski, L., Nabayinda, J., Huang, K. Y., Kivumbi, A., Bhana, A., Mwebembezi, A., Petersen, I., Hoagwood, K., & SMART Africa - Uganda Field Team (2022). The longitudinal impact of an evidence-based multiple family group intervention (Amaka Amasanyufu) on oppositional defiant disorder and impaired functioning among children in Uganda: analysis of a cluster randomized trial from the SMART Africa-Uganda scale-up study (2016-2022). Journal of Child Psychology and Psychiatry, and Allied Disciplines. https://doi.org/10.1111/jcpp.13566
Bucek, A., Leu, C. S., Benson, S., Warne, P., Abrams, E. J., Elkington, K. S., Dolezal, C., Wiznia, A., & Mellins, C. A. (2018). Psychiatric disorders, antiretroviral medication adherence and viremia in a cohort of perinatally HIV-infected adolescents and young adults. The Pediatric Infectious Disease Journal, 37(7), 673–677. https://doi.org/10.1097/INF.0000000000001866.
Casale, M., Carlqvist, A., & Cluver, L. (2019). Recent interventions to improve retention in HIV care and adherence to antiretroviral treatment among adolescents and youth: a systematic review. AIDS Patient Care and STDs, 33(6), 237–252. https://doi.org/10.1089/apc.2018.0320.
Damulira, C., Mukasa, M. N., Byansi, W., Nabunya, P., Kivumbi, A., Namatovu, P., Namuwonge, F., Dvalishvili, D., Bahar, O. S., & Ssewamala, F. M. (2019). Examining the relationship of social support and family cohesion on ART adherence among HIV-positive adolescents in southern Uganda: baseline findings. Vulnerable Children and Youth Studies, 14(2), 181–190. https://doi.org/10.1080/17450128.2019.1576960.
Derogatis, L. R. (1993). The brief symptom inventory. Minneapolis, MN: National Computer Systems.
Dessauvagie, A. S., Jörns-Presentati, A., Napp, A. K., Stein, D. J., Jonker, D., Breet, E., Charles, W., Swart, R. L., Lahti, M., Suliman, S., Jansen, R., van den Heuvel, L. L., Seedat, S., & Groen, G. (2020). The prevalence of mental health problems in sub-Saharan adolescents living with HIV: a systematic review. Global Mental Health, 7, e29. https://doi.org/10.1017/gmh.2020.18.
Goodman, R. (1999). The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 40(5), 791–799.
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40(11), 1337–1345. https://doi.org/10.1097/00004583-200111000-00015.
Goodman, S. H., Rouse, M. H., Connell, A. M., Broth, M. R., Hall, C. M., & Heyward, D. (2011). Maternal depression and child psychopathology: a meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. https://doi.org/10.1007/s10567-010-0080-1.
Goodrum, N. M., Armistead, L. P., Masyn, K., Schulte, M., & Murphy, D. A. (2021). Longitudinal bidirectional relations among parenting quality, parenting stress, and child functioning in HIV-affected families. Journal of Youth and Adolescence, 50(8), 1663–1678. https://doi.org/10.1007/s10964-021-01444-w.
Hoofs, H., Jansen, N. W., Mohren, D. C., Jansen, M. W., & Kant, I. J. (2015). The context dependency of the self-report version of the Strength and Difficulties Questionnaire (SDQ): a cross-sectional study between two administration settings. PLoS ONE, 10(4), e0120930. https://doi.org/10.1371/journal.pone.0120930.
Jantarabenjakul, W., Chonchaiya, W., Puthanakit, T., Anugulruengkitt, S., Theerawit, T., Payapanon, J., Sophonphan, J., Veeravigrom, M., Jahanshad, N., Thompson, P. M., Ananworanich, J., Malee, K., & Pancharoen, C., DOET study. (2020). Behavioral problems in perinatally HIV-infected young children with early antiretroviral therapy and HIV-exposed uninfected young children: prevalence and associated factors. AIDS Care, 32(4), 429–437. https://doi.org/10.1080/09540121.2019.1680790.
Kagotho, N., & Ssewamala, F. M. (2012). Correlates of depression among caregivers of children affected by HIV/AIDS in Uganda: findings from the Suubi-Maka family study. AIDS Care, 24(10), 1226–1232. https://doi.org/10.1080/09540121.2012.658754.
Kalembo, F. W., Kendall, G. E., Ali, M., & Chimwaza, A. F. (2019). Prevalence and factors associated with emotional and behavioural difficulties among children living with HIV in Malawi: a cross-sectional study. BMC Psychiatry, 19(1), 60. https://doi.org/10.1186/s12888-019-2046-2.
Kazdin, A. E., & Whitley, M. K. (2003). Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. Journal of Consulting and Clinical Psychology, 71(3), 504–515. https://doi.org/10.1037/0022-006x.71.3.504.
Kefale, D., Boka, A., Mengstu, Z., Belayneh, Z., & Zeleke, S. (2019). Emotional and behavioral problems and associated factors among children and adolescents on highly active anti-retroviral therapy in public hospitals of West Gojjam zone, Amhara regional state of Ethiopia, 2018: a cross-sectional study. BMC pediatrics, 19(1), 141. https://doi.org/10.1186/s12887-019-1453-3.
Kinyanda, E., Salisbury, T. T., Levin, J., Nakasujja, N., Mpango, R. S., Abbo, C., Seedat, S., Araya, R., Musisi, S., Gadow, K. D., & Patel, V. (2019). Rates, types and co-occurrence of emotional and behavioural disorders among perinatally HIV-infected youth in Uganda: the CHAKA study. Social Psychiatry and Psychiatric Epidemiology, 54(4), 415–425. https://doi.org/10.1007/s00127-019-01675-0.
Kip, E. C., Udedi, M., Kulisewa, K., Go, V. F., & Gaynes, B. N. (2022). Stigma and mental health challenges among adolescents living with HIV in selected adolescent-specific antiretroviral therapy clinics in Zomba District, Malawi. BMC Pediatrics, 22(1), 253. https://doi.org/10.1186/s12887-022-03292-4.
Laurenzi, C. A., Hunt, X., Skeen, S., Sundin, P., Weiss, R. E., Kosi, V., Rotheram-Borus, M. J., & Tomlinson, M. (2021). Associations between caregiver mental health and young children’s behaviour in a rural Kenyan sample. Global Health Action, 14(1), 1861909 https://doi.org/10.1080/16549716.2020.1861909.
Lentoor, A. G. (2017). Psychosocial challenges associated with caregiving in the context of pediatric HIV in rural Eastern Cape. Frontiers in Public Health, 5, 127. https://doi.org/10.3389/fpubh.2017.00127.
Lin, Y. N., Iao, L. S., Lee, Y. H., & Wu, C. C. (2021). Parenting stress and child behavior problems in young children with autism spectrum disorder: transactional relations across time. Journal of Autism and Developmental Disorders, 51(7), 2381–2391. https://doi.org/10.1007/s10803-020-04720-z.
Louw, K. A., Ipser, J., Phillips, N., & Hoare, J. (2016). Correlates of emotional and behavioural problems in children with perinatally acquired HIV in Cape Town, South Africa. AIDS Care, 28(7), 842–850. https://doi.org/10.1080/09540121.2016.1140892.
Mark, D., Hrapcak, S., Ameyan, W., Lovich, R., Ronan, A., Schmitz, K., & Hatane, L. (2019). Peer Support for Adolescents and Young People Living with HIV in sub-Saharan Africa: emerging Insights and a Methodological Agenda. Current HIV/AIDS Reports, 16(6), 467–474. https://doi.org/10.1007/s11904-019-00470-5.
McDaniel, B. T., & Radesky, J. S. (2020). Longitudinal associations between early childhood externalizing behavior, parenting stress, and child media use. Cyberpsychology, Behavior and Social Networking, 23(6), 384–391. https://doi.org/10.1089/cyber.2019.0478.
Mellins, C. A., & Malee, K. M. (2013). Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. Journal of the International AIDS Society, 16(1), 18593. https://doi.org/10.7448/IAS.16.1.18593.
Moos, R. H., & Moos, B. S. (1994). Family Environment Scale Manual: Development, Applications, Research. (3rd ed.) Palo Alto, CA: Consulting Psychologist Press.
Murphy, D. A., Marelich, W. D., Armistead, L., Herbeck, D. M., & Payne, D. L. (2010). Anxiety/stress among mothers living with HIV: effects on parenting skills and child outcomes. AIDS Care, 22(12), 1449–1458. https://doi.org/10.1080/09540121.2010.487085.
Musisi, S., & Kinyanda, E. (2009). Emotional and behavioural disorders in HIV seropositive adolescents in urban Uganda. East African Medical Journal, 86(1), 16–24. https://doi.org/10.4314/eamj.v86i1.46923.
Nabunya, P., Byansi, W., Sensoy Bahar, O., McKay, M., Ssewamala, F. M., & Damulira, C. (2020). Factors Associated With HIV Disclosure and HIV-Related Stigma Among Adolescents Living With HIV in Southwestern Uganda. Frontiers in Psychiatry, 11, 772. https://doi.org/10.3389/fpsyt.2020.00772.
Nabunya, P., & Namuwonge, F. (2022). HIV-Related Shame, Stigma and the Mental Health Functioning of Adolescents Living with HIV: Findings from a Pilot Study in Uganda. Child Psychiatry and Human Development, 1–8. Advance online publication. https://doi.org/10.1007/s10578-022-01374-z.
Nabunya, P., Ssewamala, F. M., & Ilic, V. (2014). Family Economic Strengthening and Parenting Stress Among Caregivers of AIDS-Orphaned Children: Results from a Cluster Randomized Clinical Trial in Uganda. Children and Youth Services Review, 44, 417–421. https://doi.org/10.1016/j.childyouth.2014.07.018.
Nabunya, P., Ssewamala, F. M., Bahar, O. S., Michalopoulos, L., Mugisha, J., Neilands, T. B., Trani, J. F., & McKay, M. M. (2022). Suubi4Stigma study protocol: a pilot cluster randomized controlled trial to address HIV-associated stigma among adolescents living with HIV in Uganda. Pilot and Feasibility Studies, 8(1), 95. https://doi.org/10.1186/s40814-022-01055-7.
Nakigudde, J., Bauta, B., Wolf, S., & Huang, K. Y. (2016). Screening child social-emotional and behavioral functioning in low-income african country contexts. Jacobs Journal of Psychiatry and Behavioral Science, 2(2), 016.
Osafo, J., Knizek, B. L., Mugisha, J., & Kinyanda, E. (2017). The experiences of caregivers of children living with HIV and AIDS in Uganda: a qualitative study. Globalization and Health, 13(1), 72. https://doi.org/10.1186/s12992-017-0294-9.
Osuji, H. L., Nabunya, P., Byansi, W., Parchment, T. M., Ssewamala, F., McKay, M. M., & Huang, K. Y. (2018). Social support and school outcomes of adolescents orphaned and made vulnerable by HIV/AIDS living in South Western Uganda. Vulnerable Children and Youth Studies, 13(3), 228–238. https://doi.org/10.1080/17450128.2018.1439211.
Pearlin, L. I., Lieberman, M. A., Menaghan, E. G., & Mullan, J. T. (1981). The stress process. Journal of Health and Social Behavior, 22(4), 337–356.
Pearlin, L. I., Mullan, J. T., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the stress process: an overview of concepts and their measures. The Gerontologist, 30(5), 583–594. https://doi.org/10.1093/geront/30.5.583.
Pillay, K., Tomita, A., & Paruk, S. (2021). Patterns of emotional and behavioural challenges in children living with HIV: results from a hyperendemic South African setting. Vulnerable Children and Youth Studies, 16(3), 232–244. https://doi.org/10.1080/17450128.2020.1869361.
Raina, P., O’Donnell, M., Schwellnus, H., Rosenbaum, P., King, G., Brehaut, J., Russell, D., Swinton, M., King, S., Wong, M., Walter, S. D., & Wood, E. (2004). Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatrics, 4, 1. https://doi.org/10.1186/1471-2431-4-1.
Remien, R. H., Stirratt, M. J., Nguyen, N., Robbins, R. N., Pala, A. N., & Mellins, C. A. (2019). Mental health and HIV/AIDS: the need for an integrated response. AIDS, 33(9), 1411–1420. https://doi.org/10.1097/QAD.0000000000002227.
Rencken, C. A., Harrison, A. D., Mtukushe, B., Bergam, S., Pather, A., Sher, R., Davidson, B. J., Carrihill, M., Matiwane, M., Kuo, C., Galárraga, O., & Hoare, J. (2021). “Those people motivate and inspire me to take my treatment.” Peer Support for Adolescents Living With HIV in Cape Town, South Africa. Journal of the International Association of Providers of AIDS Care, 20, 23259582211000525 https://doi.org/10.1177/23259582211000525.
Rodriguez, G., Hartley, S. L., & Bolt, D. (2019). Transactional relations between parenting stress and child autism symptoms and behavior problems. Journal of Autism and Developmental Disorders, 49(5), 1887–1898. https://doi.org/10.1007/s10803-018-3845-x.
Rousseau, S., Grietens, H., Vanderfaeillie, J., Hoppenbrouwers, K., Wiersema, J. R., & van Leeuwen, K. (2013). Parenting stress and dimensions of parenting behavior: cross-sectional and longitudinal links with adolescents’ somatization. International Journal of Psychiatry in Medicine, 46(3), 243–270. https://doi.org/10.2190/PM.46.3.b.
Ruiseñor-Escudero, H., Familiar, I., Nakasujja, N., Bangirana, P., Opoka, R., Giordani, B., & Boivin, M. (2015). Immunological correlates of behavioral problems in school-aged children living with HIV in Kayunga, Uganda. Global Mental Health, 2, e9. https://doi.org/10.1017/gmh.2015.7.
Schulte, M. T., Armistead, L., Marelich, W. D., Payne, D. L., Goodrum, N. M., & Murphy, D. A. (2017). Maternal parenting stress and child perception of family functioning among families affected by HIV. The Journal of the Association of Nurses in AIDS Care, 28(5), 784–794. https://doi.org/10.1016/j.jana.2017.05.004.
Sensoy Bahar, O., Byansi, W., Kivumbi, A., Namatovu, P., Kiyingi, J., Ssewamala, F. M., McKay, M. M., & Nyoni, T. (2020). From “4Rs and 2Ss” to “Amaka Amasanyufu” (Happy Families): Adapting a U.S.-based Evidence-Based Intervention to the Uganda Context. Family Process, 59(4), 1928–1945. https://doi.org/10.1111/famp.12525.
Sherr, L., Skeen, S., Hensels, I. S., Tomlinson, M., & Macedo, A. (2016). The effects of caregiver and household HIV on child development: a community-based longitudinal study of young children. Child: Care, Health and Development, 42(6), 890–899. https://doi.org/10.1111/cch.12387.
Sisk, R. J. (2000). Caregiver burden and health promotion. International Journal of Nursing Studies, 37(1), 37–43. https://doi.org/10.1016/s0020-7489(99)00053-x.
Skinner, H. A., Steinhauer, P. D., & Santa-Barbara, J. (1983). The family assessment measure. Canadian Journal of Community Mental, 2(2), 91–103.
Ssewamala, F. M., Karimli, L., Torsten, N., Wang, J. S., Han, C. K., Ilic, V., & Nabunya, P. (2016). Applying a family-level economic strengthening intervention to improve education and health-related outcomes of school-going AIDS-orphaned children: lessons from a randomized experiment in Southern Uganda. Prevention Science: the Official Journal of the Society for Prevention Research, 17(1), 134–143. https://doi.org/10.1007/s11121-015-0580-9.
Ssewamala, F. M., Sensoy Bahar, O., McKay, M. M., Hoagwood, K., Huang, K. Y., & Pringle, B. (2018). Strengthening mental health and research training in Sub-Saharan Africa (SMART Africa): Uganda study protocol. Trials, 19(1), 423. https://doi.org/10.1186/s13063-018-2751-z.
Tadesse, A. W., Berhane Tsehay, Y., Girma Belaineh, B., & Alemu, Y. B. (2012). Behavioral and emotional problems among children aged 6-14 years on highly active antiretroviral therapy in Addis Ababa: a cross-sectional study. AIDS Care, 24(11), 1359–1367. https://doi.org/10.1080/09540121.2011.650677.
Thumann, B. F., Nur, U., Naker, D., & Devries, K. M. (2016). Primary school students’ mental health in Uganda and its association with school violence, connectedness, and school characteristics: a cross-sectional study. BMC Public Health, 16, 662. https://doi.org/10.1186/s12889-016-3351-z.
Too, E. K., Abubakar, A., Nasambu, C., Koot, H. M., Cuijpers, P., Newton, C. R., & Nyongesa, M. K. (2021). Prevalence and factors associated with common mental disorders in young people living with HIV in sub-Saharan Africa: a systematic review. Journal of the International AIDS Society, 24(Suppl 2), e25705. https://doi.org/10.1002/jia2.25705. Suppl 2.
Uganda Ministry of Health (2021). Factsheet: Facts on HIV and AIDS in Uganda 2021. Accessed 23 April 2022. https://uac.go.ug/media/attachments/2021/09/13/final-2021-hiv-aids-factsheet.pdf.
Vreeman, R. C., McCoy, B. M., & Lee, S. (2017). Mental health challenges among adolescents living with HIV. Journal of the International AIDS Society, 20(Suppl 3), 21497. https://doi.org/10.7448/IAS.20.4.21497.
Wang, J. S., Ssewamala, F. M., & Han, C. K. (2014). Family economic strengthening and mental health functioning of caregivers for AIDS-affected children in rural Uganda. Vulnerable Children and Youth Studies, 9(3), 258–269. https://doi.org/10.1080/17450128.2014.920119.
Webster, K. D., de Bruyn, M. M., Zalwango, S. K., Sikorskii, A., Barkin, J. L., Familiar-Lopez, I., Musoke, P., Giordani, B., Boivin, M. J., & Ezeamama, A. E. (2019). Caregiver socioemotional health as a determinant of child well-being in school-aged and adolescent Ugandan children with and without perinatal HIV exposure. Tropical Medicine & International Health, 24(5), 608–619. https://doi.org/10.1111/tmi.13221.
White, H. (1980). A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica: Journal of the Econometric Society, 817–838. https://doi.org/10.2307/1912934.
Woodman, A. C., Mawdsley, H. P., & Hauser-Cram, P. (2015). Parenting stress and child behavior problems within families of children with developmental disabilities: Transactional relations across 15 years. Research in Developmental Disabilities, 36C, 264–276. https://doi.org/10.1016/j.ridd.2014.10.011.
Acknowledgements
We are grateful to the staff and the volunteer team at the International Center for Child Health and Development (ICHAD) in Masaka, Uganda, for monitoring the study implementation process, Reach the Youth Uganda (implementing partner), participating health clinics in the study region, and the investigative team based at the Brown School at Washington University in St. Louis. Our special thanks go to all the children and their caregiving families who agreed to participate in the study.
Funding
Financial support for the Suubi4Stigma study came from the National Institute of Mental Health (NIMH; Grant # R21MH121141, MPIs: Proscovia Nabunya, PhD and Fred M. Ssewamala, PhD). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethical Approval
All study procedures were approved by Washington University in St. Louis Institutional Review Board (IRB # 202009185), the Uganda Virus Research Institute (GC/127/20/10/792), and the Uganda National Council for Science and Technology (SS632ES). Participation in the study was voluntary.
Informed Consent
Informed written consent and assent were obtained from caregivers and adolescents respectively, prior to study participation. Children were asked to provide written assent separately to avoid coercion. The study is registered in ClinicalTrials.gov # NCT04528732.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nabunya, P., Byansi, W., Bahar, O.S. et al. Emotional and Behavior Difficulties and the Mental Health of Caregivers of Adolescents Living with HIV. J Child Fam Stud 32, 3766–3774 (2023). https://doi.org/10.1007/s10826-023-02609-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-023-02609-w