Abstract
Comorbid psychiatric presentations, defined as those who present with more than one mental and/or behavioral health diagnosis at the same time, during adolescence are on the rise. Mindfulness-based interventions can alleviate psychological symptoms and improve emotion regulation in youth. Mindfulness is a multifaceted phenomenon, with five underlying facets (Observing, Describing, Acting with Awareness, Non-Judgment and Non-Reactivity of Inner Experience). Little evidence has documented which facets produce pronounced psychiatric symptom reduction for adolescents. This pilot study examined the efficacy of an online mindfulness-based intervention delivered to adolescents undergoing mental health treatment during COVID-19 to reduce psychiatric outcomes. Fifty-six adolescents (m = 14.5 years, 66.1% female) categorized as moderate-risk (treatment histories of outpatient therapy only) or high-risk (treatment histories with intensive service participation) participated in the 8-session mindfulness-based intervention. Significant reductions in psychiatric symptoms and increases in adaptive coping strategies were observed at post-test, particularly for those at moderate-risk. Multivariate stepwise regression found significant associations between mindfulness facet use and anxiety, depression, and somatic symptoms (R2 ranging from 42.5 to 52.8%). Results indicate preliminary efficacy for an online mindfulness-based intervention for adolescents, particularly those at moderate-risk, due to the introduction of new coping skills, given their history of less intense treatment. Further investigation is warranted to understand which mindfulness facet intervention components produce the most prominent outcomes.
Highlights
-
Preliminary efficacy for an online MBI for adolescents deemed moderate- and high-risk (outpatient only versus outpatient plus intensive care).
-
Significant reduction in psychiatric symptoms and increases in adaptive coping strategies observed at post-test.
-
Pre-test mindfulness facet use explained 42.5–52.8% of the variance in anxiety, depression and somatic symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Comorbid presentations of major depressive episodes, anxiety disorders, and somatic symptoms in adolescence are common (SAMHSA, 2020), and increase into early adulthood if not properly treated (Lallukka et al., 2019). Adolescents with comorbid diagnoses, defined as those who present with more than one mental and/or behavioral health diagnosis at the same time, report increased difficulty using emotion regulation strategies to problem solve (Compas et al., 1993; Garnefski and Kraaij, 2018), suggesting this regulatory process may be an important mechanism when developing interventions to improve mental health outcomes. Emotion regulation consists of adaptive/maladaptive strategies to identify, understand, and modulate the type and degree of emotional experiences (Gross and Thompson, 2010). Significant links are noted between maladaptive strategy use, reduced self-efficacy and increased depression and anxiety symptoms (Carthy et al., 2010; Compas et al., 2017; Ehring et al., 2010). Coping strategies, such as distress tolerance or mindfulness, are the effortful cognitive-affective techniques that are goal directed and aim to regulate negative emotions (Compas, 2009; Lazarus and Folkman, 1987; Russell and Park, 2018).
Distress tolerance is the ability to engage in goal-directed behaviors despite discomfort (Simons & Gaher, 2005). Those considered high in distress tolerance approach negative emotions and aversive contexts by paying attention to emotions and modulating their responses, while those reporting difficulties may increase maladaptive responses and negative affect through avoidance-oriented coping (Linehan and Wilks, 2015; Van Eck et al., 2017). Mindfulness is a state, dispositional trait, and skill of nonjudgmental awareness created by purposefully paying attention to each moment (Kabat-Zinn, 2003), and is linked to reduced emotional distress, increased positive mindset and self-efficacy (Carmody and Baer, 2008; Kingston et al., 2007; Pepping et al., 2016). Self-efficacy is a broad and stable sense of personal competence that aids in problem recognition and the belief that one is capable of overcoming them (Schwarzer and Jerusalem, 1995) and may be crucial for adolescents’ well-being (Moksnes and Espnes, 2012). This evidence indicates a critical need for approaches focused on bolstering distress tolerance, mindfulness and self-efficacy that engage adolescents with comorbid diagnoses to reduce symptomology and improve wellbeing.
Emotion regulation skills have broad evidence of efficacy, with less consistent results noted for maladaptive responses to stress during adolescence (Hu et al., 2014). Early evidence suggests a link between maladaptive cognitive coping strategies of self-blame, rumination, or catastrophizing about negative life events, and increased somatic symptoms (Brown, 2004; Garnefski et al., 2017), with those engaging in maladaptive coping about negative life events more vulnerable to anxiety, depression and somatic complaints (Pepping et al., 2016). Preliminary evidence suggests those who employ a greater variety of adaptive coping strategies report reduced anxiety and depression, and increased psychological functioning and self-efficacy (Compas et al., 2017; Suhr et al., 2017). These mechanisms may be specific targets for mind-body interventions with adolescent samples to mitigate psychological and physical distress and associated adverse symptoms.
Mindfulness-Based Interventions
Mindfulness-based interventions (MBI) alleviate psychological symptoms and lead to improved emotion regulation and coping in youth (Lyvers et al., 2014; Zoogman et al., 2015). Adolescents with psychiatric-only or comorbid diagnoses engaged in MBIs indicated significant improvements in anxiety, depression, and somatic distress, and positive impacts on psychosocial outcomes of well-being, self-regulation, and self-awareness (Biegel et al., 2009; Russell et al., 2019). To date, however, no MBIs with adolescents have examined their efficacy in an online format, leaving a significant gap in our understanding.
Mindfulness is a multifaceted phenomenon, and is theorized to have five underlying facets that describe its various dimensions (Baer et al., 2008): Observing, attending to internal and external experiences, Describing, labeling internal experiences with words, Acting with Awareness, attending to activities in the moment, Non-Judging of Inner Experience, holding a non-evaluative stance toward internal experiences, and Non-Reactivity of Inner Experience, allowing internal experiences to come and go without ruminating on them. Only a handful of studies have examined the differential impact of mindfulness facet use to produce symptom reduction in samples with adolescents. Of those that have, Non-Reactivity and Non-Judging of Inner Experience and Acting with Awareness may be particularly associated with deficits in awareness of emotional consequences, and increased dysphoric affect, stress, and depressive symptoms (Abujaradeh et al., 2019; Ciesla et al., 2012; Royuela-Colomer and Calvete, 2016). Vulnerable youth may be more prone to reject, avoid, ruminate or suppress their thoughts and feelings, indicating a critical need to improve upon distress tolerance skills to teach vulnerable adolescents to engage in valued life directions in the face of challenging situations and/or emotions, as these skills may mitigate adverse outcomes, including suicidal behaviors and substance use (O’Neil Rodriguez and Kendall, 2014; Schneider et al., 2018).
Early evidence suggests a connection between mindfulness facets and somatic symptoms, with Non-Judging of Inner Experiences indicating the strongest relationship with physical health (Ballantyne et al., 2021). Preliminary evidence suggests MBIs improve mental health and well-being, however, findings are mixed regarding which mindfulness facets lead to improved outcomes among adolescents (Medvedev et al., 2018). This indicates an important direction to understand which mindfulness facets relate to psychological adjustment best, and for whom to develop the most effective treatment options.
The current project highlights a small-group didactic MBI, Promoting Resilience in Self-Management (PRISM) (Russell et al., 2019), that focuses on three core tenets of mindfulness: observing non-judgmentally, attending to positivity, and self-soothing. Previous findings demonstrated reduced depression for a clinical sample of adolescents following a 6-session version of PRISM (Russell et al., 2019). PRISM has since been expanded to 8-sessions to allow additional practice of mindfulness and distress tolerance strategies (See Procedures for full description of session activities). There are several gaps in our understanding that we aim to address, (1) whether an online version of PRISM for adolescents indicates efficacy (improved outcomes of mental and physical health) among a clinical population with comorbid diagnoses, (2) whether this pilot of PRISM generates positive impacts on mental health outcomes for the entire sample, or if differences are noted by risk category, and (3) which mindfulness facets produce the most prominent impact on mental and physical health outcomes for adolescents with comorbid diagnoses.
Current Study
We extend the preliminary work of PRISM to a new clinical population (adolescents engaged in mental health services across two risk categories, defined below) and is the first PRISM that was delivered online. We were guided by three hypotheses: Regardless of risk category, participants will report significantly improved outcomes (i.e., reduced depression, anxiety, and somatic symptoms, and increased emotion regulation) following engagement in PRISM (H1). We expected to see participants categorized as high-risk report significantly improved outcomes from pre- to post-test compared to those deemed moderate risk (H2). Finally, adolescents who present with increased use of Non-Judging of Inner Experience and Acting with Awareness at pre- and post-test will report increased improvements of mental and physical health symptoms following PRISM (H3).
Methods
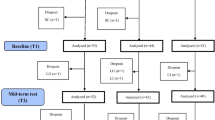
Data presented here include baseline and follow-up survey results for an adjunctive pilot MBI with adolescents enrolled in a community mental health clinic in rural New England receiving therapy from October 2020 to June 2021, during the COVID-19 pandemic. See Fig. 1 for a causal model of the intervention.
Participants
The sample was selected from two sites within one community mental health clinic that had seen 1256 clients within the past 12 months (age range = 3–22, m = 13 years old). Participants were recruited via convenience sampling through use of flyers, emails to clinicians and word of mouth. In total, 222 eligible adolescents were contacted, of which 166 were excluded (n = 139 did not return phone calls; n = 18 were not interested in participating at this time; n = 9 agreed to participate but did not fully enroll or show to sessions). Of the 56 adolescents enrolled, seven were lost to follow-up (n = 5 involved in too many services; n = 2 terminated all mental health treatment services), leaving 49 adolescents retained at post-test. Inclusion criteria were: adolescents aged 12–17 years old, English-speaking, and actively engaged in treatment (defined as attending at least one session a month). The only exclusion criterion stated if participant’s behavior was disrespectful toward others or otherwise inappropriate, they would be removed from the study (no instances occurred during the intervention). The type of therapy engagement was not controlled for, but noted by recording their treatment attendance rates (attended or no-showed/cancelled), frequency of sessions (weekly, bi-weekly, monthly), and their engagement in outpatient only services or higher-levels of care (described below). Given the nature of this pilot study to determine initial feasibility, no control group or waitlisted participants were included. By dint of their engagement in mental health treatment, all participating adolescents face some degree of risk for maladaptive outcomes, with some characterized by more concerning treatment histories. Participants were grouped into two categories by the following criteria, (1) moderate risk due to current engagement in outpatient therapy but no treatment history of referrals to a higher level of care, and (2) high risk due to prior, current, or pending/waitlist treatment of a higher level of care in addition to engagement in outpatient therapy. Higher levels of care indicated through chart review include: (1) Intensive In-home Child and Psychiatric Service (II-CAPS) provides in-home services for 6–18 year old’s with psychiatric, emotional or behavioral difficulties and their families (Intensive In-Home Services, n.d.), (2) Functional Family Therapy (FFT), a strength-based treatment for 11–18 year old’s with behavioral or emotional problems and their families to address delinquency, substance abuse and violence (Functional Family Therapy, n.d.), (3) partial hospitalization program attendance, and (4) hospitalization for suicidal or unstable mental health conditions requiring 24/7 supervision.
Procedures
Study materials were approved by the University of Connecticut IRB (H20-0062). Participants elected to engage in the online version of the PRISM intervention as an adjunctive service to their on-going clinical treatment. Following use of recruitment strategies, parents of interested participants were contacted to confirm the first group session date and time. Both participants and parents attended the first session to complete consenting procedures and pre-test assessment, and the last session for post-test assessment. The average completion time for the pre-test assessment was 26.8 min (sd = 13.9; range = 9.1–57.3), and was 29.2 min (sd = 12.9; range = 10.3–64.1) at post-test. All participants were compensated for their time at intermittent intervals to increase participant attendance, receiving a $5 incentive at pre-test and between sessions 3–4, and a $10 incentive between sessions 5–6 and at session 8 for completion of the post-test survey. Participants were eligible for up to $30 throughout the intervention.
The intervention consisted of 8 1 h long sessions held in an online group format (group size = 4–8 participants) via a HIPAA-compliant videoconferencing system. During each session ample time was provided for didactic discussion and skill building. Each session began with a brief check-in to assess for challenging experiences or emotions felt during the past week and how participants attended to these situations using adaptive or maladaptive strategies covered in previous sessions. Then came a psychoeducation piece to introduce that session’s topic, followed by a discussion to expand understanding, provide context and experiential activities to practice adaptive coping strategies relevant to participants daily lives. The final activity in each session was a guided meditation. At the close of each session participants were asked to state a take-away message or describe how they planned to implement the new strategies in the upcoming week.
The psychoeducation topics and experiential activities from each of the eight didactic session were drawn from freely available activities in the public domain and select concepts common to cognitive behavioral approaches (e.g., Dialectical Behavioral Therapy, Linehan and Wilks, 2015); each unit contained the following: Session one began with the pre-test assessment, followed by an introduction to stress management and awareness of mind, including the interconnection between emotional, reasonable and a balanced mindset between the two, described as “wise mind” (Linehan and Wilks, 2015). Session two focused on distress tolerance, with two experiential activities, (1) refocusing attention on positivity, where participants improved a moment of distress by distracting away from discomfort through the introduction of and focus on a positive thought, and (2) calming statements, defined as any self-soothing thought that can be verbalized, such as a positive affirmation (i.e., “I’ll do my best and that will be good enough”). Session three aimed to develop wise mind skills through experiential activities of (1) observing and describing emotions through a game of emotional charades, and (2) protecting against negativity through which participants build awareness of their emotions to reduce vulnerability to negative emotions and stay out of emotional mind. Session four focused on self-care, with activities of (1) calming statements tied to participants’ breath, and 2) one-mindedness, introduced as bringing awareness to one activity at time and focusing attention on the present moment. Session five revisited distress tolerance and introduced the topic of accepting reality, building participant’s ability to recognize feelings in the present moment to improve it through use of calming statements and a positive affirmation. Session six focused on self-care in action, with activities of (1) observing emotions in a social context, emphasizing discussion of moments where emotional expressions were misread and how this misinterpretation can influence reactions in social exchanges, and (2) revisiting protection against negativity from session three. Session seven addressed understanding felt emotions and reducing emotional vulnerability through a thought diffusion activity, in which participants are taught skills to help ‘unhook’ from overwhelming emotions, such as visualizing your thoughts and emotions and watching them float away without analyzing or ruminating on them. The final session revisited self-soothing through an experiential activity focused on using the five senses to be kind, gentle and comfort oneself through focusing on the sights, sounds, smells, tastes, or textures in your immediate environment to draw attention to pleasing, positive, and rewarding moments.
At the close of each of the eight sessions, the participants were led through two variations of a guided meditation, which utilized the metaphor of your mind as the sky or as the mountains to describe the changing emotions and feelings we experience and the stability of our mind. The facilitator invited the participants to sit in a comfortable position with their eyes closed, focusing on their breath while listening to the visual cues of the metaphor. An example line from the meditations were, “Your mind is the [sky/mountain]. Your thoughts and emotions are the [clouds/seasons]. Notice the thoughts as they come in and pass through. Like the [clouds/seasons], thoughts and emotions are always changing, they are temporary but your mind is still there, your mind is unchanging.”
Measures
Demographics
Adolescents’ self-reported key demographic variables, including, age, gender, sexual orientation, ethnicity, race, and grade level. Descriptive findings from participants’ treatment history were included to provide context on risk level (i.e., referrals to support services, safety plans for suicidal behaviors, and treatment period duration).
Depression symptomology
The Center for Epidemiologic Studies Depression Scale (CES-D; Eaton et al., 2004) is a 20-item measure that assesses current levels of depressive symptomology for the general public and is scored on a 4-point Likert scale (0 = Rarely or none of the time (<1day) to 3 = most or all of the time (5–7 days)). Total scores are calculated by summing all 20-items together; higher scores indicate increased depressive symptoms. Scores 16 or greater indicate an individual is at-risk for clinical depression (Eaton et al., 2004). The CES-D has acceptable reliability scores in the general population and clinical samples, in addition to adolescent samples, respectively (α = 0.85–0.90 and 0.83; Eaton et al., 2004; Skriner and Chu, 2014), as in the current clinical sample 0.91.
Somatic symptomology
The Somatic Symptom Scale-8 (SSS-8; Gierk et al., 2014) is an 8-item measure that assesses somatic symptoms over the last week. Items are scored on a 5-point Likert scale (0 = not at all to 4 = very much). Total scores are calculated by summing responses, with higher scores indicating greater symptom frequency. Severity categories are articulated to aid interpretation of scores (Gierk et al., 2014): 0–3 = No, to minimal; 4–7 = Low; 8–11 = Medium; 12–15 = High; 16–32 = Very high. The SSS-8 has acceptable reliability in adult and adolescent samples, respectively (α = 0.81 and 0.79; Baier et al., 2019; Gierk et al., 2014), as in the current sample 0.81.
Anxiety symptomology
The Generalized Anxiety Disorder (GAD-7; Spitzer et al., 2006) is a 7-item measure that assesses symptoms associated with GAD over the last 14 days. Items are scored on a 4-point Likert scale (0 = not at all sure to 3 = nearly every day). Total scores are calculated by summing all 7 items, such that higher scores indicate more severe anxiety symptoms. A score of 8 or greater indicates a cut-off of GAD diagnosis, with the following severity categories provided to aid interpretation of scores (Spitzer et al., 2006): 0–4 = Minimal; 5–9 = Mild; 10–14 = Moderate; 15+ = Severe. The GAD-7 has excellent reliability in a general and adolescent sample, respectively (α = 0.92 and 0.91; Spitzer et al., 2006; Tiirikainen et al., 2019), as in the current sample 0.90.
Emotion regulation
The Cognitive Emotion Regulation Questionnaire-Short form (CERQ-SF; Garnefski and Kraajj, 2006) is an 18-item measure that assesses attitudes and practices about managing emotions when experiencing negative events. Items are scored on a 5-point Likert scale (1 = almost never to 5 = almost always). The CERQ-SF consists of 9 two-item subscales: Self-Blame, Other-Blame, Rumination, Catastrophizing, Putting into Perspective, Positive Refocusing, Positive Reappraisal, Acceptance, and Planning. Scores are calculated by summing items to that particular subscale; higher scores indicate increased cognitive strategy use. The CERQ-SF has acceptable reliability in adults and general samples (α = 0.70–0.85; Garnefski and Kraajj, 2006), as in the current sample 0.64–0.80. Reliability in adolescents has only been conducted using the full, 36-item scale, but shows acceptable reliability (α = 0.71–0.94; Garnefski and Kraaij, 2018).
Mindfulness
The Five-Facet Mindfulness Questionnaire (FFMQ-15; Baer et al., 2008) is a 15-item measure of mindfulness facets that assesses general tendencies to be mindful in daily life. Items use a 5-point Likert scale (0 = Never or very rarely true to 4 = Very often or always true). The scale contains 5 three-item subscales: Observing, Describing, Acting with Awareness, Non-Judging of Inner Experience, and Non-Reactivity to Inner Experience. Scores from each subscale are summed; higher scores indicate greater tendency for daily mindfulness. Reliability for the FFMQ-15 are high in adult samples (α = 0.80–0.85; Baer et al., 2012). Reliability in adolescent samples using the 39-item scale reports more variable, but still adequate reliability ranges (0.61–0.91; Deplus et al., 2016). In the current sample, reliability was comparable (α = 0.60–0.85), with Non-Reactivity to Inner Experience and Acting with Awareness (0.60 and 0.61, respectively) reporting the lowest alphas.
Distress tolerance
The Distress Tolerance Scale (DTS; Simons & Gaher, 2005) is a 15-item scale that assesses an individual’s perceived ability to tolerate, appraise, absorb and regulate their distress. Items are scored on a 5-point Likert scale (1 = strongly agree to 5 = strongly disagree). The DTS has four subscales: Tolerance, Appraisal, Absorption and Regulation. Subscales are calculated via averages of their items, with a total DTS score calculated from an average of the subscales; higher scores represent higher levels of distress tolerance. The DTS has acceptable reliability in adult and adolescent samples (α = 0.89 and 0.59–0.90; Kechter and Leventhal, 2019; Simons & Gaher, 2005), as in the current sample 0.90.
Self-efficacy
The General Self-Efficacy Scale (GSF; Schwarzer and Jerusalem, 1995) is a 10-item scale assessing the coping ability of daily living. Items are scored on a 4-point Likert (1 = not true at all to 4 = exactly true). Items are summed together; higher scores indicate greater self-efficacy to manage issues of daily living. The GSF has acceptable reliability in adult and adolescent samples (α = 0.76–0.90 and 0.85; Moeini et al., 2008; Schwarzer and Jerusalem, 1995), as in the current sample 0.80.
Analytic Plan
Analyses examining more than one time point include participants with data at both assessments (n = 49). We saw 0% item-level missingness at pre- and post-test for participants who completed both assessments. First, we present descriptive results of participants, including key variables of interest to evaluate what proportion of participants’ responses fell above relative reported cutoffs. We then present paired samples t-tests to examine growth from pre- to post-test for mental health outcomes (H1). Next, paired samples and independent samples t-tests by moderate- and high-risk categories examine group differences from pre- to post-test for mental and physical health outcomes and mindfulness facets (H2). All t-tests were run separately by constructs (i.e., mental/physical health symptomology, emotion regulation subscales, mindfulness subscales). Bonferroni correction was utilized to adjust p values due to increased risk of a type-I error when making multiple statistical tests. Finally, we present multivariate stepwise regressions utilizing pre- and post-test mindfulness facet use, session attendance, and risk category to predict mental and physical health outcomes, controlling for pre-test mindfulness facet use, pre-test mental health symptomology, age and gender (H3). Post-hoc analyses were conducted to further examine the impact of dose response on key outcomes of interest.
Results
Participants (n = 56) had an average age of 14.5 years (sd = 1.6, range = 12–17). Two-thirds of participants identified as female (n = 37, 66.1%), followed by male (n = 10, 17.9%), other (n = 5, 8.9%), transgender (n = 3, 5.4%) and gender fluid (n = 1, 1.8%). Participants self-reported their sexual orientation, with 23 (41.1%) identifying as heterosexual, 17 (30.4%) as bisexual, 13 (23.2%) as other, and 3 (5.4%) as homosexual. The majority of participants identified as Caucasian (n = 47, 83.9%), followed by African American (n = 9, 16.1%). Over one-quarter of the sample (n = 15, 26.8%) identified as Latinx. The majority of participants were in 9th grade (n = 13, 23.2%; range = 5–12th grade). All participants reported comorbid diagnoses, with depressive (n = 28), anxiety (n = 21) and attention-deficit hyperactivity disorders (n = 18) reported as most common. Participants reported significantly higher rates of somatic symptoms at pre-test (m = 14.85) compared to a general population of adults (m = 3.23, Gierk et al., 2014) and adolescent samples (m = 8.78, Baier et al., 2019). No significant differences of demographic characteristics by risk category were found.
Thirty participants (53.6%) were considered to be in the moderate-risk group. On average, participants in the moderate-risk group attended 30 therapy appointments (sd = 30.3, range = 1–101), and cancelled/no-showed 8 appointments (sd = 8.8, range = 0–31). Eleven participants (36.7%) had at least one safety plan in their treatment history (m = 2.8, sd = 2.4, range = 1–11). Four participants (13.3%) had referrals to Emergency Mobile Psychiatric Services (EMPS; ranging from 1 to 3 referrals per child). Twenty-six participants were considered to be in the high-risk group (n = 26, 46.4%). On average, participants in the high-risk group attended 74 therapy appointments (sd = 59.1, range = 8–191), and cancelled/no-showed 30 appointments (sd = 31.5, range = 1–100). Sixteen participants (61.5%) had at least one safety plan in their treatment history (m = 3.1, sd = 3.1, range = 1–14). Fourteen participants (53.8%) had referrals to EMPS (ranging from 1 to 4 referrals per child). In addition, 20 participants (76.9%) had prior engagement in II-CAPS (ranging from 1 to 5 referrals per child), 16 participants (61.5%) had prior engagement in FFT (ranging from 1 to 3 referrals per child), 5 participants (19.2%) had prior engagement with partial hospitalization programs, and 4 participants (15.4%) had prior hospitalizations for their unstable mental health symptoms.
Descriptive Results
We lost seven participants at follow-up, resulting in a retention rate of 87.5%, with high indicators of acceptability and feasibility. While there were no statistically significant differences in baseline study variables for participants lost to attrition from those who completed both assessments, there were systematic differences worth noting: at baseline, participants lost to attrition reported higher rates of Non-Reactivity to Inner Experience (m = 9.57 versus 8.00) and self-efficacy (m = 26.14 versus 24.08), and lower rates of somatic symptoms (m = 11.14 versus 15.18) and use of the cognitive emotion regulation strategy perspective taking (m = 3.86 versus 5.90). For further details on the acceptability, feasibility, and other process variables related to the online intervention, please refer to our related study (Hutchison et al., 2022). Results that follow include all 56 participants who provided data on key variables of interest at pre-test, and at post-test 49 (87.5%) participants provided completed data. At pre-test, 50 (89.3%) adolescents reported a score of 16 or greater, indicating clinical depression (Eaton et al., 2004). At post-test, the number of participants indicating clinical depression decreased to 34 (60.7%). At pre-test, 6, 11, 17 and 22 adolescents reported scores indicating no/minimal, mild, moderate, and severe anxiety, respectively (Spitzer et al., 2006). At post-test, 11, 14, 12, and 12 individuals indicated no/minimal, mild, moderate and severe anxiety, respectively. At pre-test, 5, 9, 8, 8 and 26 adolescents reported scores indicating no-minimal, low, medium, high and very high somatic symptoms, respectively (Gierk et al., 2014). Following the intervention, 11, 6, 7, 8, and 17 individuals indicated no-minimal, low, medium, high and very high somatic symptoms, respectively (see Fig. 2 for visual representation of pre-post impacts).
Hypothesis 1
Several statistically significant pre- to post-intervention differences are evident (see Table 1): participants reported significant reductions in their mental health symptomology of depression, anxiety and somatic symptoms (ts range = 2.77–3.45, all p < 0.01, ds range = 0.36–0.44). Significant increases in mindfulness facet of Describing (t = −2.07, p < 0.05, d = 0.26) and self-efficacy (t = −3.55, p < 0.01, d = 0.58) were noted. Significant increases in cognitive emotion regulation strategies for positive refocusing and positive reappraisal (t = −2.22 and −2.71, respectfully, p < 0.05, d = 0.37 and 0.41), and reductions in self-blame cognitive coping (t = 2.10, p < 0.05, d = 0.32) are also evident. Bonferroni adjusted alpha levels for three, five and nine a priori hypotheses (for mental/physical health symptomology, mindfulness facets, and cognitive emotion regulation strategies, respectfully) were conducted using alpha levels of 0.017, 0.010, and 0.001 per test. All changes for mental and physical health outcomes remained significant, as did the cognitive emotion regulation strategy of positive reappraisal.
Hypothesis 2
Based upon the criteria for risk-categories described above, thirty participants (53.6%) were considered to be moderate risk, and twenty-six participants (46.4%) high risk. Two statistically significant group differences were found: adolescents in the high-risk group reported significantly higher pre-test use of the mindfulness facet of Describing (t = −2.65, p < 0.01, d = 0.71) and those in the moderate risk group reported significantly lower pre-test use of the cognitive emotion regulation strategy of self-blame (t = 2.22, p < 0.05, d = 0.59). Bonferroni adjusted alpha levels for five and nine a priori hypotheses (for mindfulness facets, and cognitive emotion regulation strategies, respectfully) were conducted using alpha levels of 0.010, and 0.001 per test. Changes in describing mindfulness remained significant.
Due to differences in treatment history, paired samples’ t-tests of moderate and high risk sub-groups were conducted to assess patterns of change. Several statistically significant group differences by risk categories were found (see Table 2). The moderate risk group reported significant reductions in mental health symptomology of depression, anxiety and somatic symptoms (ts range = 2.39–4.09, all p < 0.05, ds range = 0.32–0.67). The moderate risk group reported significant increases in mindfulness facets of Describing, and Non-Reactivity of Inner Experience (ts = −2.09 and −2.22, ps < 0.05, ds = 0.43 and 0.61). Adolescents in the moderate risk group reported significant increases in their distress tolerance (t = −3.49, p < 0.01, d = 0.76), self-efficacy (t = −2.73, p < 0.01, d = 0.55), and use of cognitive coping strategies of positive refocusing and positive reappraisal (ts = −2.34 and −2.76, ps < 0.05, ds = 0.60 and 0.60) as well as significant reductions in self-blame and catastrophizing (ts = 2.60 and 2.40, ps < 0.05, d = 0.54 and 0.57). The only significant improvement seen in the high risk group was in self-efficacy (t = −2.40, p < 0.05, d = 0.59). Bonferroni adjusted alpha levels for three, five and nine a priori hypotheses (for mental/physical health symptomology, mindfulness facets, and cognitive emotion regulation strategies, respectfully) were conducted using alpha levels of 0.017, 0.010, and 0.001 per test. Changes in generalized anxiety remained significant, as did the cognitive emotion regulation strategy of positive reappraisal.
Hypothesis 3
Overall, session dosage did not reach significance in any of the models below, where predictions of each outcome is presented separately—for anxiety, depression, and lastly, somatic symptoms (see Table 3).
Anxiety symptomology
Participant’s post-test use of Non-Judging of Inner Experience and moderate and high risk categories together explained 42.5% of the variance in anxiety symptomology at post-test (R2 = 0.425, F(9, 39) = 3.86, p < 0.01). Holding constant all other predictors, higher use of post-test Non-Judging of Inner Experience (β = −0.393, p = 0.013) significantly predicted reduced anxiety symptomology, whereas being in the high-risk group (β = 0.304, p = 0.017) significantly predicted increased anxiety symptomology. No control variables (baseline use of mindfulness facets, baseline symptomology, age or gender) made a significant contribution to the model.
Depression symptomology
Participant baseline depression symptomology (control variable) and post-test use of Describing together explained 47.7% of the variance in depression symptomology at post-test (R2 = 0.477, F(9, 39) = 5.86, p < 0.01). Holding constant all other predictors, higher baseline depression symptomology (β = 0.487, p = 0.001) significantly predicted increased depression symptomology at post-test and post-test use of Describing (β = −0.441, p = 0.004) significantly predicted reduced depression symptomology.
Somatic symptomology
Participants baseline somatic symptomology (control variable) and post-test use of Non-Judging of Inner Experience together explained 52.8% of the variance in somatic symptomology at post-test (R2 = 0.528, F(9, 39) = 6.97, p < 0.01). As seen in the previous models, holding constant all other predictors, higher use of post-test Non-Judging of Inner Experience (β = −0.452, p = 0.002) significantly predicted reduced somatic symptomology, while higher somatic symptomology (β = 0.468, p = 0.001; control variable) significantly predicted increased somatic symptomology at post-test.
Post-Hoc Analysis
While a continuous score for participants’ session attendance was not a significant predictor of study outcomes, prior evidence indicates increased attendance and engagement in interventions produces more pronounced outcomes (Moulton-Perkins et al., 2020). Therefore, we conducted post-hoc analyses to examine a potential dose response. We created a dichotomous variable of attendance for those with low attendance (four sessions or fewer) and those with high attendance (five or more sessions) and ran independent samples t-tests to explore any group differences on key outcomes of interest. Two statistically significant group differences were found: adolescents who had high attendance reported significantly reduced catastrophizing at post-test (t = 2.20, p < 0.05, d = 0.65) and significantly increased distress tolerance at post-test (t = −2.49, p < 0.05, d = 0.64) compared to those in the low attendance group.
Discussion
Previous evidence supports the utility of adjunctive MBI approaches to alleviate psychological symptoms, and improve emotion regulation, self-awareness and coping in youth (DePlus et al., 2016; Pepping et al., 2016). We built on existing literature and preliminary results of the PRISM curriculum (Russell et al., 2019) by demonstrating significant impacts on mental and physical health outcomes for adolescent patients in a community-based mental health clinic. Our first hypothesis was supported, as participants reported reductions in mental and physical health outcomes of depression, anxiety and somatic symptoms and reduced use of self-blame as a cognitive coping strategy following the intervention. Additional significant impacts were seen in increased use of Describing mindfulness, self-efficacy and cognitive emotion regulation strategies for positive refocusing and positive reappraisal.
We expected to see adolescents deemed high risk to report greater improvements in outcomes from pre- to post-test compared to adolescents in a moderate-risk category. Contrary to our expectations, those in the high-risk group did not report symptom reduction and only reported significant improvements in their self-efficacy. Those in the moderate risk group, surprisingly, reported several statistically significant changes: reduced depression, anxiety and somatic symptoms, increased use of Describing, Non-Reactivity and Non-Judging of Inner Experience mindfulness, increased distress tolerance, self-efficacy and use of cognitive coping strategies for positive refocusing and positive reappraisal, and significant reductions in self-blame and catastrophizing. A large effect on distress tolerance following the intervention was seen among those in the moderate risk group. This finding supports prior research (e.g., Linehan and Wilks, 2015) and the efficacy of this intervention to make significant real-world impacts on adolescents’ abilities to engage in goal-directed behaviors despite experiencing discomfort (e.g., maintaining treatment plan goals). This result provides a promising focus for future MBIs with adolescents striving produce the most pronounced impacted on cognitive coping strategies.
One potential explanation for the lack of our hypothesis support can be seen in the high-risk group’s treatment history. Each participant engaged in at least one type of intensive in-home service anywhere from one to four times, with each service lasting 3–6 months. In-home services are informed by cognitive and communication theories that focus on reducing blame and increasing positive reappraisal (Adnopoz et al., 2012; Celinska et al., 2019). The high-risk group demonstrated higher rates of pre-test use in four of the five mindfulness facets (all but Acting with Awareness) than the moderate risk group. The high-risk group may have received prior exposure and practice of cognitive shifts in non-judgmental perspectives and positive reframing of negative experiences during intensive in-home services and thus report little room for improvement. Further, this group’s treatment trajectory may indicate a level of need beyond what the 8-session adjunctive PRISM curriculum can reasonably meet.
Participants in the moderate risk group may have demonstrated better outcomes due to the introduction of new cognitive emotion regulation strategies and mindfulness skills during PRISM. Given their history of less intense treatment, they may not have been previously aware of or practiced these skills regularly, which provided opportunity for increased use from the intervention to improve mental health outcomes. This finding is supported by the greater mean difference for significant mindfulness facet change in the moderate risk group of Describing and Non-Reactivity of Inner Experience compared to those in the high-risk group, who reported higher values at pre-test and may be indicative of a ceiling effect. Further, greater mean differences for cognitive emotion regulation strategies were seen for self-blame, positive refocus, positive reappraisal, and catastrophizing. Future analyses with larger samples should control for potential differences of treatment history and coping skill use at pre-test in predictive models to examine impacts on mindfulness facets and mental health outcomes by categories of risk.
We found partial support for our third hypothesis, that post-test use of Non-Judging of Inner Experiences significantly predicted reduced anxiety and somatic symptoms. Contrary to expectations, Acting with Awareness did not significantly predict mental or physical health outcomes, and post-test Describing was found to be a significant predictor of reduced depression symptoms. Prior research indicates Non-Judging of Inner Experience as associated with dysphoric affect, stress, and depressive symptoms (Abujaradeh et al., 2019; Royuela-Colomer and Calvete, 2016), and may buffer the effects of life stress on negative affect in adolescent samples (Ciesla et al., 2012; Galla et al., 2020). Further, early evidence suggests a connection between Describing and Non-Judging of Inner Experiences and reduced somatic symptoms (Ballantyne et al., 2021). We provide additional support to these findings, and have implications for future MBIs delivered online or in-person. Such interventions with adolescents can focus on describing emotional experiences from a non-judgmental perspective to reduce mental and physical health symptoms. These facets are particularly helpful to shift engrained cognitive patterns of negative appraisals and rumination on experiences and feelings to increase adaptive describing and judgment of thoughts and feelings, which may impact overall symptomology. Future work that compares the effectiveness of delivery modality will be important for evaluating intervention scalability and sustainability for adolescents at risk of maladaptive outcomes.
Limitations
The small sample size limits the power to run sophisticated analyses and generalize findings to the larger population of at-risk adolescents, and may explain the lack of significance in some of the findings, including those deemed non-significant following Bonferroni adjustments. Many families contacted about the study were reluctant to engage due to the commitment of additional responsibilities and appointments. This is a challenge during traditional service engagement, but was compounded by the work, education and daily routine disruptions noted during the COVID-19 pandemic. The current study provides preliminary efficacy pilot results that can inform future larger trials focused on a hard to reach population.
A second limitation is the variability in participants’ attendance (m = 5.75, range = 1–8). The most common reasons for missing sessions were too many appointments/events scheduled that week (n = 19), transition to a higher level of care (n = 5) and anxiety about the group format (n = 4). An additional limitation was the difficulty of retaining participants to complete the post-test survey. At baseline, participants lost to follow-up were more likely to have higher rates of self-efficacy and use of Non-Reactivity to Inner Experience mindfulness, suggesting they may have believed they could address any mental health concerns with their current level of care and may not have seen the potential benefit of the adjunctive MBI to provide additional skills or support. The most common reasons for attrition were involvement in too many services (n = 4), termination of mental health treatment (n = 2), and not liking the group format (n = 1). Post-hoc analyses indicated participants who attended five or more sessions (62.5% or more of the curriculum), reported significantly increased distress tolerance and reduced use of catastrophizing at post-test compared to those who attended fewer than five sessions, indicating attendance produced more robust impacts. This further supports the practical impact on distress tolerance as a result of this intervention and has meaningful implications for adolescents who present with comorbid diagnoses. The intervention may be addressing multiple treatment plan objectives (i.e., reducing depression, increasing communication) to learn goal-directed behaviors that increase their ability to attend to adverse experiences in the moment with adaptive coping strategies to mitigate distress.
A further barrier to survey completion was the online facilitation due to the COVID-19 pandemic, which removed the possibility of in-person survey completion and other types of follow-up, supports, and encouragement that may have bolstered engagement for the entire sample. Future studies should attempt to address this issue by including additional means of contact during the consent procedure to follow up with patients (i.e., home address to mail survey, permission to contact additional household members), as opposed to the only modalities used in the current study of email, text and phone calls to caregivers—necessary to complete data collection per the social distance guidance following the spread of the COVID-19 virus. Further, the use of online formats for assessments presents a possible risk for common rater, common-method bias that should be addressed in forthcoming studies through the use of additional assessment perspectives, including observational measures and multi-rater methods (i.e., adolescent, parent and therapist perspectives).
A final limitation worth noting is the lack of a control or comparison group in this pilot study. We are unable to determine whether the benefits of the PRISM intervention are due to the specific components taught and skill acquisition learned, or if they were due to confounding variables such as but not limited to: ongoing mental health treatment outside of the adjunctive intervention, social desirability, attention, peer interaction or distraction. Future research is warranted to conduct a larger-scale trial of PRISM with either a wait-list control or treatment as usual comparison group to determine the beneficial effects derived from PRISM specifically.
Conclusion
The preliminary pilot study provides initial support that PRISM can bolster adaptive emotion regulation and coping skills to reduce mental and physical health symptoms for adolescents receiving treatment in a community mental health clinic. Our findings suggest the importance of adjunctive services like MBIs for those at moderate risk, who are engaged in outpatient services, report significant depression, anxiety and somatic symptoms, but fall below threshold indicators for intensive in-home services. Providing adjunctive services to this group is critical to prevent escalations beyond the need of outpatient therapy to higher levels of care, which are costly and time-intensive. Evidence suggests that prevalence and severity of mental health symptoms increases with age (Lallukka et al., 2019), thus is important to target this moderate risk adolescent group to bolster adaptive coping and reduce symptom severity for this traditionally less-supported group of at-risk adolescents.
We provide pilot results of a Stage 1A intervention development effort, where a promising behavioral intervention was modified and adapted to provide initial efficacy in a new clinical sample of adolescents. Next steps in developing the program are to expand the intervention to multiple sites to examine feasibility and pilot testing during Stage 1B (Czajkowski et al., 2015). Specific, recommended strategies for proceeding include repeated practice of Describing and Non-Judging of Inner Experience, as increased use of these at post-test significantly predicted reduced mental and physical health symptoms. Additional examination of the impact of implementation modality on key outcomes is necessary. Recruitment should expand to multiple sites to allow for increased reach of at-risk adolescents to allow randomization by risk-category (moderate and high risk) into one of the following facilitation modalities: online only, in-person only, or a combination of online and in-person formats. Further, the addition of a comparison group, defined as either a wait-list control or treatment as usual is necessary to determine whether outcomes are due to the PRISM intervention itself or if similar benefits are noted for adolescents attending traditional treatment modalities only (i.e., outpatient services). This next step of an implementation trial will test which facilitation modality produces the most pronounced symptom reduction by category of risk to refine future experimental testing during Stage 2 (randomized control trial of efficacy).
References
Abujaradeh, H., Colaianne, B. A., Roeser, R. W., Tsukayama, E., & Galla, B. M. (2019). Evaluating a short-form Five Facet Mindfulness Questionnaire in adolescents: Evidence for a four-factor structure and invariance by time, age, and gender. International Journal of Behavioral Development, 44, 20–30.
Adnopoz, J. A., Woolston, J. L., & Balestracci, K. M. B. (2012). IICAPS: A Treatment Model for Delinquent Youths with Co-occurring Mental Health Disorders. In: E. Grigorenko (ed.) Handbook of Juvenile Forensic Psychology and Psychiatry. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-0905-2_23.
Baer, R. A., Carmody, J., & Hunsinger, M. (2012). Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology, 68, 755–765.
Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., Walsh, E., Duggan, D., & Williams, J. M. G. (2008). Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment, 15, 329–342. https://doi.org/10.1177/1073191107313003.
Baier, D., Hong, J. S., Kliem, S., & Bergmann, M. C. (2019). Consequences of bullying on adolescents’ mental health in Germany: comparing face-to-face bullying and cyberbullying. Journal of Child and Family Studies, 28, 2347–2357. https://doi.org/10.1007/s10826-018-1181-6.
Ballantyne, C., Hunter, P. V., Potter, G. K., & Myge, I. (2021, February 22). Mindfulness and perceptions of physical health: The mediating role of perceived stress. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement. Advance online publication. https://doi.org/10.1037/cbs0000255.
Biegel, G. M., Brown, K. W., Shapiro, S. L., & Schubert, C. M. (2009). Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 77, 855–866. https://doi.org/10.1037/a0016241.
Brown, R. J. (2004). Psychological mechanisms of medically unexplained symptoms: an integrative conceptual model. Psychological Bulletin, 130, 793–812.
Carmody, J., & Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a Mindfulness-Based Stress Reduction program. Journal of Behavioral Medicine, 31, 23–33.
Carthy, T., Horesh, N., Apter, A., & Gross, J. J. (2010). Patterns of emotional reactivity and regulation in children with anxiety disorders. Journal of Psychopathology and Behavioral Assessment, 32, 23–36.
Celinska, K., Sung, H. E., Kim, C., & Valdimarsdottir, M. (2019). An outcome evaluation of functional family therapy for court‐involved youth. Journal of Family Therapy, 41, 251–276.
Ciesla, J. A., Reilly, L. C., Dickson, K. S., Emanuel, A. S., & Updegraff, J. A. (2012). Dispositional mindfulness moderates the effects of stress among adolescents: Rumination as a mediator. Journal of Clinical Child & Adolescent Psychology, 41, 760–770. https://doi.org/10.1080/15374416.2012.698724.
Compas, B. E., Orosan, P. G., & Grant, K. E. (1993). Adolescent stress and coping: Implications for psychopathology during adolescence. Journal of Adolescence, 16, 331–349.
Compas, B. E., Jaser, S. S., Bettis, A. H., Watson, K. H., Gruhn, M., Dunbar, J. P., & Thigpen, J. C. (2017). Coping, emotion regulation and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychological Bulletin, 143, 939–991.
Compas, B. E. (2009). Coping, regulation, and development during childhood and adolescence. In E. A. Skinner & M. J. Zimmer-Gembeck (Eds.), Coping and the development of regulation. New directions for child and adolescent development, 124, (pp. 87–99). San Francisco:Jossey-Bass.
Czajkowski, S. M., Powell, L. H., Adlher, N., Naar-King, S., Reynolds, K. D., Hunter, C. M., & Charlson, M. E. (2015). From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology, 34, 971–982. https://doi.org/10.1037/hea0000161.
Deplus, S., Billieux, J., Scharff, C., & Philippot, P. (2016). A mindfulness-based group intervention for enhancing self-regulation of emotion in late childhood and adolescence: A pilot study. International Journal of Mental Health and Addiction, 14, 775–790. https://doi.org/10.1007/s11469-015-9627-1.
Eaton, W. W., Muntaner, C., Smith, C., Tien, A., & Ybarra, M. (2004). Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R). In: M. E. Maruish (Ed.) The Use of Psychological Testing for Treatment Planning and Outcomes Assessment, 3rd ed. (pp. 363–377). Mahwah, NJ: Lawrence Erlbaum.
Van Eck, K., Warren, P., & Flory, K. (2017). A variable-centered and person-centered evaluation of emotion regulation and distress tolerance: Links to emotional and behavioral concerns. Journal of Youth and Adolescence, 46, 136–150.
Ehring, T., Tuschen-Caffier, B., Schnulle, J., Fischer, S., & Gross, J. J. (2010). Emotion regulation and vulnerability to depression: Spontaneous versus instructed use of emotion suppression and reappraisal. Emotion, 10(4), 563–572.
Functional Family Therapy. (n.d.). https://www.fftllc.com/about-fft-training/clinical-model.html.
Galla, B. M., Tsukayama, E., Park, D., Yu, A., & Duckworth, A. L. (2020). The mindful adolescent: developmental changes in nonreactivity to inner experiences and its association with emotional well-being. Developmental Psychology, 56, 350–363. https://doi.org/10.1037/dev0000877.
Garnefski, N., & Kraaij, V. (2006). Cognitive Emotion Regulation Questionnaire: development of a short 18-item version (CERQ-short). Personality and Individual Differences, 41, 1045–1053.
Garnefski, N., & Kraaij, V. (2018). Specificity of relations between adolescents’ cognitive emotion regulation strategies and symptoms of depression and anxiety. Cognition and Emotion, 32, 1401–1408.
Garnefski, N., van Rood, Y., de Roos, C., & Kraaij, V. (2017). Relationships between traumatic life events, cognitive emotion regulation strategies, and somatic complaints. J Clin Psychol Med Settings, 24, 144–151.
Gierk, B., Kohlmann, S., Kroenke, K., Spangenberg, L., Zenger, M., Brähler, E., & Löwe, B. (2014). The somatic symptom scale-8 (SSS-8): A brief measure of somatic symptom burden. JAMA Intern Medicine, 174(3), 399–407.
Gross, J. J., & Thompson, R. A. (2010). Emotion regulation: conceptual foundations. In J. J. Gross (Ed.), Handbook of emotion regulation (pp. 135–158). New York:Guilford Press.
Hu, T., Zhang, D., Wang, J., Mistry, R., Ran, G., & Wang, X. (2014). Relation between emotion regulation and mental health: a meta-analysis review. Psychological Reports, 114, 341–362.
Hutchison, M., Russell, B. S., Gans, K. M., & Starkweather, A. R. (2022). Online administration of a pilot mindfulness-based intervention for adolescents: Feasibility treatment perception and satisfaction. Current Psychology. https://doi.org/10.1007/s12144-022-03025-x.
Intensive In-Home Services (IICAPS). (n.d.). https://www.bgvillage.org/programs/behavioral-health/intensive-in-home-services-iicaps-/.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: past, present, and future. Clinical Psychology, 10, 144–156.
Kechter, A., & Leventhal, A. M. (2019). Longitudinal association of sleep problems and distress tolerance during adolescence. Behavioral Medicine, 45, 240–248. https://doi.org/10.1080/08964289.2018.1514362.
Kingston, J., Chadwick, P., Meron, D., & Skinner, T. C. (2007). A pilot randomized control trial investigating the effect of mindfulness practice on pain tolerance, psychological well-being, and physiological activity. Journal of Psychosomatic Research, 62, 297–300.
Lallukka, T., Mekuria, G. B., Nummi, T., Virtanen, P., Virtanen, M., & Hammarstrom, A. (2019). Co-occurrence of depressive, anxiety and somatic symptoms: Trajectories from adolescence to midlife using group-based joint trajectory analysis. BMC Psychiatry, 19, 1–8. 1186/s12888-019-2203-7.
Lazarus, R. S., & Folkman, S. (1987). Transactional theory and research on emotions and coping. European Journal of Personality, 1, 141–169.
Linehan, M. M., & Wilks, C. R. (2015). The course and evolution of dialectical behavior therapy. The American Journal of Psychotherapy, 69, 97–110.
Lyvers, M., Makin, C., Toms, E., Thorberg, F. A., & Samios, C. (2014). Trait mindfulness in relation to emotional self-regulation and executive function. Mindfulness, 5, 619–625.
Medvedev, O. N., Norden, P. A., Krageloh, C. U., & Siegert, R. J. (2018). Investigating unique contributions of dispositional mindfulness facets to depression, anxiety, and stress in general and student populations. Mindfulness, 9, 1757–1767. https://doi.org/10.1007/s12671-018-0917-0.
Moeini, B., Shafii, F., Hidarnia, A., Babaii, G. R., Birashk, B., & Allahverdipour, H. (2008). Perceived stress, self-efficacy and its relations to psychological well-being status in Iranian male high school students. Social Behavior and Personality, 36, 257–266.
Moksnes, U. K., & Espnes, G. A. (2012). Self-esteem and emotional health in adolescents – Gender and age as potential moderators. Scandinavian Journal of Psychology, 53, 483–489. https://doi.org/10.1111/sjop.12021.
Moulton-Perkins, A., Moulton, D., Cavanagh, K., Jozavi, A., & Strauss, C. (2020). Systematic Review of Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction via Group Videoconferencing: Feasibility, Acceptability, Safety, and Efficacy. Journal of Psychotherapy Integration. Advance online publication. https://doi.org/10.1037/int0000216.
O’Neill Rodriguez, K. A., & Kendall, P. C. (2014). Suicidal ideation in anxiety-disordered youth: identifying predictors of risk. Journal of Clinical Child and Adolescent Psychology, 43, 51–62.
Pepping, C. A., Duvenage, M., Cronin, T. J., & Lyons, A. (2016). Adolescent mindfulness and psychopathology: the role of emotion regulation. Personality and Individual Differences, 99, 302–307.
Royuela-Colomer, E., & Calvete, E. (2016). Mindfulness facets and depression in adolescents: rumination as a mediator. Mindfulness, 7, 1092–1102.
Russell, B. S., & Park, C. L. (2018). The role of emotion regulation in chronic pain self-management. Topics in Pain Management: Current Concepts and Treatment Strategies, 33(6), 1–10.
Russell, B. S., Hutchison, M., & Fusco, A. (2019). Emotion regulation outcomes and preliminary feasibility evidence from a mindfulness intervention for adolescent substance use. Journal of Child and Adolescent Substance Abuse, 28(1), 21–31.
Schneider, R. L., Arch, J. J., Landy, L. N., & Hankin, B. L. (2018). The longitudinal effect of emotion regulation strategies on anxiety levels in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 47, 978–991.
Schwarzer, R., & Jerusalem, M. (1995). Generalized Self-Efficacy Scale. In J. Weinman, S. Wright, & M. Johnston (Eds.). Measures in health psychology: Auser’s portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: Nfer-Nelson.
Simons, J. S., & Gaher, R. M. (2005). The Distress Tolerance Scale: Development and Validation of a Self-Report Measure. Motivation and Emotion, 29(2), 83–102. https://doi.org/10.1007/s11031-005-7955-3.
Skriner, L. C., & Chu, B. C. (2014). Cross-ethnic measurement invariance of the SCARED and CES-D in a youth sample. Psychological Assessment, 26, 332–337. https://doi.org/10.1037/a0035092.supp.
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder. Archives Internal Medicine, 166, 1092–1097.
Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality (2020). Results from the 2019 National Survey on Drug Use and Health: Detailed Tables. https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2019-NSDUH.
Suhr, M., Risch, A. K., & Wilz, G. (2017). Maintaining mental health through positive writing: effects of a resource diary on depression and emotion regulation. Journal of Clinical Psychology, 73(12), 1586–1598.
Tiirikainen, K., Haravuori, H., Ranta, K., Kaltiala-Heino, R., & Marttunen, M. (2019). Psychometric properties of the 7-item Generalized Anxiety Disorder Scale (GAD-7) in a large representative sample of Finnish adolescents. Psychiatric Research, 272, 30–35. https://doi.org/10.1016/j.psychres.2018.12.004.
Zoogman, S., Goldberg, S. B., Hoyt, W. T., & Miller, L. (2015). Mindfulness interventions with youth: a meta-analysis. Mindfulness, 6, 290–302.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hutchison, M., Russell, B.S., Starkweather, A.R. et al. Outcomes From an Online Pilot Mindfulness Based Intervention with Adolescents: A Comparison by Categories of Risk. J Child Fam Stud 32, 438–450 (2023). https://doi.org/10.1007/s10826-022-02448-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-022-02448-1