Abstract
Several studies have shown that mindfulness-based programs (MBPs) may bring promising benefits for youth. However, little is known about its efficacy in specific clinical populations and even less about the psychological processes that underlie the changes. This study investigates the efficacy of a MBP among a population of adolescent boys with behavior disorders and explores the mediating role of impulsivity in the observed changes. Participants included 48 adolescents presenting conduct disorders and mild cognitive impairments, living in a residential service for youth in Belgium. Two groups of 24 adolescents aged 12 to 19 years have been constituted. Only the experimental group followed a MBP. The program was divided into two parts: the first 6 sessions were devoted to group dynamic and introduction to emotional skills whereas the second part focused on mindfulness exercises. The level of depression and impulsivity as well as the symptomatology of attention deficit hyperactivity disorder were assessed before, during and after the program for both groups. Results showed that both groups decreased their depressive symptomatology but only the MBP group decreased in impulsivity and externalizing symptomatology. No mediating effects of the facets of impulsivity on the outcomes were found. MBPs may bring psychological benefits for adolescents who suffer from behavior disorders but further research on the efficacy of MBPs among this population is needed.
Highlights
-
Mindfulness-based interventions are well-accepted among adolescents with behavior disorders.
-
Mindfulness-based interventions may be useful to treat externalizing symptomatology in behavior disorders.
-
The effects of mindfulness training on externalizing symptomatology may be mediated by changes in impulsivity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adolescence is a sensitive period during which psychological processes mature importantly (Casey et al. 2010). In this context, some adolescents may develop psychological difficulties associated with puberty changes (Avenevoli et al. 2015). One adolescent in five between 12 and 19 years of age suffers from a psychiatric disorder (Costello et al. 2011). Even though most teenagers do not go through a problematic period, some may experience difficulties that required the help of professionals. For instance, a study on adolescent mental health reported an increase in the 12-month prevalence of major depressive episodes between 2005 (8.7%) and 2014 (11.3%) (Mojtabai et al. 2016). This is particularly the case for adolescents with behavior disorders who are more likely to develop externalizing and internalizing problems (Lam and Ho 2010; Lee et al. 2011). A longitudinal study showed that adolescents who presented conduct problems were likely to develop a comorbid depression, while adolescents with depression were no more likely to develop conduct problems (McDonough-Caplan et al. 2018). These results suggest that adolescents suffering from behavior disorders are a high-risk population and that internalizing symptoms, such as anxiety and depressive symptoms, should be addressed. Despite these observations, externalizing problems remain the core symptoms of behavior disorders or, at least, the most salient. Globally, externalizing disorders affect 9.5% of the adolescents in a high severity form and 28.8% of them in a mild severity form (Colman et al. 2009). In addition, the literature demonstrated that boys are more at risk to develop behavior disorders than girls (Boden et al. 2010; Keenan et al. 2010).
Taken together, attention deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and conduct disorder (CD) are the second type of psychological problems encountered in adolescence and affect more than 19% of youth (after anxiety disorders with 31.9%; Merikangas et al. 2010). These disorders are characterized by externalizing symptoms, such as anger, frustration, low activation and inhibitory control, hyperactive and aggressive behaviors, but can also lead to internalizing problems like depression or anxiety (Liu 2004; Muris et al. 2007). Interestingly, the DSM-5 separated ADHD (in the Neurodevelopmental Disorders category) from ODD and CD (in the Disruptive, Impulse-Control, and Conduct Disorders category) due to early developmental deficits (e.g., executive functions impairment) that are supposed to be specific to ADHD. However, these diagnoses present a high comorbidity and the overlaps between ADHD and externalizing problems included in ODD and CD were frequently highlighted (e.g., Witkiewitz et al. 2013). In this way, the DSM-5 states that “on the basis of patterns of symptoms, comorbidity, and shared risk factors, attention-deficit/hyperactivity disorder was placed with neurodevelopmental disorders, but the same data also supported strong arguments to place ADHD within disruptive, impulse-control, and conduct disorders” (American Psychiatric Association 2013, p. 11). As a result, we choose the label “behavior disorders” in reference to the following diagnoses: ADHD, ODD, and CD.
Yet, solely relying on diagnostic categories may limit our understanding of the underlying psychological dynamics. Another way to grasp behavior disorders is to identify their underlying psychological processes as suggested by the processual approach (Nolen-Hoeksema and Watkins 2011; Philippot et al. 2019). The processual approach poses that interventions should target transdiagnostic psychological mechanisms (i.e., attitudes or functioning common to several diagnoses, such as rumination, that maintain the psychological problems). In accordance with this view, research has suggested several psychological processes that may play a central role in behavior disorders. For example, impulsivity, that is to say the deficit in the ability to analyze responses to a stimulus and a tendency to act rashly, could be one of the major psychological processes underlying behavior disorders (Ahmad and Hinshaw 2016; Barkley 1997). Whiteside and Lynam (2001) have identified four dimensions underlying impulsivity: Urgency, Lack of Premeditation, Lack of Perseverance and Sensation seeking. High levels of impulsivity can be observed in ADHD as well as in ODD and CD. This lack of inhibition constitutes a central issue in behavior disorders due to its high prevalence and its strong associations with internalizing and externalizing symptomatology (d’Acremont and Van der Linden 2007; Flory et al. 2003). Congruently, interventions, such as cognitive behavioral therapy, have been proposed to help adolescents to manage their impulsivity and improve their inhibition capacities (Cartwright-Hatton et al. 2004; Sonuga-Barke et al. 2013).
In line with the desire to act on transdiagnostic processes, Mindfulness-Based Programs (MBPs) have received increasing attention. Mindfulness is the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment (Kabat-Zinn 2003). It can be defined by several mechanisms such as attention regulation, body awareness, emotion regulation, and change in perspective of the self (Hölzel et al. 2011). Mindfulness training does not directly focus on problem solving but fosters emotional acceptance and awareness of ongoing experience (Kahl et al. 2012). Exercises, such as breathing meditation, body scan, or mindful hatha yoga, are proposed to participants in order to develop their capacities to be mindful and to bring attention to the present moment. MBPs have proven effective in alleviating psychological problems such as anxiety, depression, or ruminations and in potentiating emotion regulation in adult populations (Chambers et al. 2009; Deyo et al. 2009; Grossman et al. 2004; Heeren and Philippot 2011). Several meta-analyses were conducted and supported the MBPs efficacy with a small to moderate effect size (Grossman et al. 2004; Khoury et al. 2015; Sedlmeier et al. 2012). While a large number of studies have been conducted in adults, the implementation of MBPs has only recently been initiated among youth (Broderick and Jennings 2012).
The first study on MBPs among children aged 7–8 was conducted by Semple et al. (2005) in a school context. A large number of MBPs followed thereafter (Zack et al. 2014), for instance, the manualized mindfulness program for anxious children (Semple and Lee 2007), an adaptation of the Mindfulness-Based Stress Reduction program (MBSR) for adolescents (Biegel et al. 2009), the learning to breath program (Broderick and Metz 2009), the.b program (Mindfulness in Schools Project; Kuyken et al. 2013) or the program for children and adolescents developed by Deplus et al. (2016). Overall, the MBPs dedicated to youth differ in terms of session number (from 4 to 16), length (from 30 to 90 min), target population (clinical versus non-clinical), and content (presence or absence of elements such as emotion- and stress-related psychoeducation, empathy or yoga exercises). Taken together, MBPs have a small to moderate effect size (ES) for depressive symptomatology (ranged from 0.27 to 0.45; Chi et al. 2018; Dunning et al. 2018), a moderate to large ES for anxiety (ranged from 0.62 to 0.96; Kallapiran et al. 2015; Zenner et al. 2014) and a small to moderate ES for mindfulness (ranged from 0.24 to 0.42, Dunning et al. 2018).
Yet, the large diversity of these MBPs for youth raises some questions about their heterogeneity and their comparability. This concern was addressed by the meta-analysis of Zoogman et al. (2015) that investigated the different modalities of MBPs implementation among youth aged between 6 and 21 years. The authors did not find any moderator on outcome concerning home practice, instructor previous experience, session length, treatment frequency or length, intervention type, age, sample size, gender or racial/ethnic minority composition of the sample, or publication year. Furthermore, all MBPs shared common components such as breath awareness, attention training, working on thoughts and emotions, psycho-education about emotion regulation, awareness of senses, group discussions, body-scan and home practice, which could reduce the apparent diversity of formats (Zenner et al. 2014). These MBPs have been adapted in order to be effective and well received in young populations. Indeed, developmental differences for younger populations compared to adults, such as shorter attention span or lower abstraction capacities, need to be considered. We identified four points that distinguish MBPs for adolescents from MBPs for adults: (1) Sessions are more numerus and shorter in order to respect the attention capacities of youth; (2) Groups are smaller and often have more than one therapist; (3) Mindfulness exercises and time required for home practice are shorter; (4) Playfulness is emphasized by integrating mindfulness through games, stories, movies, and pictures. By including these changes, the first studies that investigated MBPs for youth assessed the feasibility and acceptability of this approach (first step). The overall conclusion was optimistic and provided the green light for further investigations (Ames et al. 2014; Burke 2010; Mendelson et al. 2010; Semple et al. 2005).
It follows that one can ask whether adolescents who suffer from behavior disorders would benefit from MBPs in the same way as the general youth population. A non-controlled study, on 10 adolescents with ADHD aged 11–15 years, tested the efficacy of a MBP for children based on 8 weekly 1.5 h sessions, accompanied with a parallel mindful parenting training for parents (Van de Weijer-Bergsma et al. 2012). Results are mixed but indicated that MBPs may improve externalizing and internalizing symptoms as well as attention. Similar findings were supported by studies in younger populations (e.g., Van der Oord et al. 2012). More generally, adolescents with behavior disorders aged 11–18 reported a reduction of their externalized symptoms (Cohen’s d = 1.1), a better achievement of personal goals (Cohen’s d = 1.4), an enhancement of perceived attention (Cohen’s d = 1.0), and a better score at an attentional task (Cohen’s d = 0.60) after a Mindfulness-Based Cognitive Therapy (MBCT) adapted to youth (Bögels et al. 2008).
When looking at the meta-analyses on the effectiveness of MBPs among individuals who suffer from ADHD, results seems to be consistent. Thus, Cairncross and Miller (2020) showed that MBPs significantly reduced the score of hyperactivity on combined self-reports and observer-reports ratings (d = −0.53; 95% CI [−0.74, −0.32]) as well as inattention (d = −0.66; 95% CI [−0.92, −0.40]), although this last ES was larger for adults compared to children. Same conclusions were drawn by the recent meta-analysis of Chimiklis et al. (2018) conducted on eleven studies that explored the efficacy of MBPs and yoga in children with ADHD symptoms. For teacher-reported ADHD symptoms, the Hedges’g was 0.23 (95% CI [0.076, 0.50]; p = 0.008) while it was 0.57 (95% CI [0.029; 1.11]; p = 0.039) for parent-reported ADHD symptoms, indicating a small to moderate ES.
Two moderators were also identified by the analyses. First, it seems that randomized-controlled trials reported small or insignificant ES compared to controlled or single arm multiple baseline design. This result is in line with previous findings that suggests that MBPs efficacy is often overestimated. Second, longer intervention session was found to be associated with larger ES (but not the number of sessions). This may indicate that ADHD symptoms could improve better with longer time of practice and emotional exposure. It is possible that the strength of learning lies in intensive practice (i.e., the capacity to stay longer in relation to its inner experience). Interestingly, neither the sample size, formal ADHD diagnosis, number of intervention sessions or the type of intervention were found as moderators of the intervention efficacy. For inattention and attention problems, the ES was 0.31 (95% CI [0.12, 0.49]; p = 0.001) when rating by teachers, and 0.34 (95% CI [0.13, 0.56]; p = 0.001) when rating by parents, indicating a small to moderate ES. No moderator was found for this variable. Concerning hyperactivity, the results showed a small to moderate ES according to the parents (g = 0.39; 95% CI [0.04, 0.73]; p = 0.023) and a small ES according to the teachers (g = 0.22; 95% CI [0.02, 0.41]; p = 0.027). Moderator analyses demonstrated that the children with an ADHD diagnosis showed a better decrease in hyperactivity than the children without a formal diagnosis. Yet, it is possible that children with formal diagnosis present higher hyperactivity at baseline and, thus, were more likely to reduce their level of hyperactivity. Furthermore, MBPs seem to have a better impact on hyperactivity than yoga interventions according to moderation analyses. This last conclusion could lead to the hypothesis that mindfulness exercises that require immobility might be more beneficial for hyperactivity than mindful movements.
Importantly, the large majority of studies focuses on ADHD diagnoses and rarely consider other behavior disorders such as ODD or CD. Moreover, the internalizing symptomatology, and particularly depressive symptoms, are ignored even though they are directly related to adolescents’ well-being. The interpretation of the results is also often limited by the lack of adequate control groups or well-validated measures (Burke 2010; Zoogman et al. 2015). Another limitation of this body of literature is that the psychological processes that underlie MBPs efficacy have not been investigated.
Indeed, mindfulness targets different processes that are decisive for adolescents with behaviors disorders. As previously discussed, impulsivity may be a cornerstone of behaviors disorders. Some studies supported the influence of MBPs on impulsivity or aggressive behavior during adolescence (e.g., Singh et al. 2007). Adolescents seem to develop their inhibition capacities through mindfulness exercises and to reduce their propensity to act rashly (Deplus et al. 2016; Tan and Martin 2015; Van Vliet et al. 2016). For instance, adolescents who participated in a MBP qualified themselves at the end of the program as less hyperactive and impulsive, and reported that the intervention had a positive impact on their ability to control physical and verbal aggression (Van Vliet et al. 2016).
In the present study, we addressed these issues by comparing a MBP with a control group, using validated tools for youth, and exploring which facets of impulsivity are potential processes that underlie improvements. This paper presents the implementation of a MBP among adolescent boys with behavior disorders in order to investigate its acceptability and its efficacy in this specific population and to identify whether impulsivity is a central process for these changes. We hypothesized that mindfulness training would lead to a global psychological improvement compared to a control group by reducing depressive, externalizing, internalizing symptoms thanks to a decrease in the processes underlying impulsivity. In this way, it is hypothesized that the changes on impulsivity facets will mediate the benefits on the outcomes. Furthermore, it was expected that the MBP would be well received by adolescents and accompanied by positive feedback.
Method
Participants
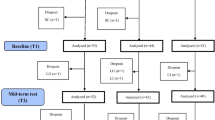
Fifty-six adolescent boys were recruited in a residential service for youth in Belgium. This institution accommodates only adolescent boys with behavior disorders. DSM-5 diagnoses were attributed either by the psychiatrist of the institution or by a consensus between the psychiatrist and the psychologists of the institution. Inclusions criteria were that participants should be between 12 and 19 years of age, expressed motivation to participate in the therapeutic program, fulfilled the DSM-5 criteria of a behavior disorder (ADHD, ODD or CD), were fluent in French, and able to answer to questionnaires. Conversely, we excluded participants who presented a very high symptomatology of depression (scoring more than 76 on MDI-C at pre-test which indicates a severe depression). These adolescents were redirected to other professionals. Also, adolescents with an absenteeism rate of 50 percent or more during the treatment were excluded of analyses. Figure 1 displays the different steps of participants’ selection. After recruiting 56 potential adolescents, 22 participants remained in both groups at post-test (N = 44). Adolescents had at least one behavior disorder: ADHD (n = 24, 54%), ODD (n = 30, 68%) or CD (n = 6, 13%). There was comorbidity between ADHD and ODD (n = 13, 29%) and ADHD and CD (n = 2, 5%). In addition, 59.1% of the total sample presented at least a mild depression according to the questionnaire of depression (MDI-C). The study was approved by the ethic committee of the authors’ university. Written informed consent was provided by the parents and the adolescents, all accepted to participate.
Procedure
To introduce the intervention, the adolescents received a brief presentation of the program with a particular focus on emotion management. Two groups were constituted: a treatment group and a waitlist control group. Adolescents were randomly allocated to the experimental and control groups. Nevertheless, due to the organizational constraints of the institution, five adolescents could not be randomly allocated to groups, three were assigned to the experimental group and two were assigned to the control group based on their schedule constraints. The waitlist control group received the usual treatment of the institution while the experimental group additionally received the MBP. Of note, all participants were enrolled in some other treatments that were part of the usual treatment delivered by the institution. These “treatment as usual” consisted in psychotherapy, psychomotricity, and speech therapy, and did not exceed 3 h per week for each participant. There were no precise data specifying the exact amount of each usual treatment followed by each participant.
The experimental group was subdivided in four subgroups of five and one subgroup of four adolescents of the same age (±1 year). Indeed, as suggested by Lagor et al. (2013), homogeneity in age for a group is more important than homogeneity in gender or diagnosis.
There were three times of assessment during which the adolescents individually completed the MDI-C and the UPPS-P. A psychologist remained at their disposal to answer their questions. Nine participants received assistance from the evaluators (i.e., a psychologist and students in psychology) to read the questionnaires. The same educators completed the SNAP-IV and the CBCL for both groups. They were indirectly aware of the conditions because they knew that some adolescents were absent at times because of the research program. After a preliminary interview, the measures for both groups were collected before the intervention (Pre-test, T1), after the intervention based on emotion psycho-education and group dynamics (Mid-intervention test, T2) and after the MBP (Post-test, T3). The Pre-test was performed in October 2015, the Interim in January 2016 and the Post-test in May 2016.
To assess the acceptability of the program, we conducted a semi-structured interview nine months after the end of the MBP and asked participants if they appreciated the intervention, if they found it difficult and, finally, if they continue to practice mindfulness.
Intervention
As adolescents with externalized disorders might experience difficulties to participate in a group and to directly practice meditation, the MBP was preceded by six group sessions devoted to emotional competencies and group dynamic. The next 10 sessions focused on mindfulness training per se and constituted the MBP. Each weekly session lasted 50 min. Table 1 shows the details of the program. It was inspired by two others programs for adolescents: the adolescent mindfulness-based intervention for enhancing emotional regulation (Deplus et al. 2016; Deplus and Lahaye 2015) and the Taming the Adolescent Mind program (TAM program, Tan and Martin 2013). More specifically, our program followed the session themes proposed by Deplus and Lahaye (2015) such as exploring body sensations, non-judgment, or thoughts observation, but also included exercises from the TAM program such as discussion of examples of difficulties experienced in the week, of how application of mindfulness may be utilized in these instances. The combination of the two interventions allows a more complete program than the only five sessions proposed by Tan and Martin (2013) and more adolescent-tailored activities than the program of Deplus and Lahaye (2015), which focuses on children.
Two professionals, one psychologist trained to MBCT and a psycho-motor therapist working in the institute and trained to MBP for adolescents, animated groups of five adolescents. Each point of the day’s session was discussed before and after each session. The psycho-motor therapist ensured that the time dedicated to the activities was respected.
Measures
Swanson, Nolan, and Pelham-IV (SNAP-IV)
The SNAP-IV measures ADHD based on the criterion symptoms of the DSM-5 (Swanson 1995). The 26 items-version (MTA-version) developed by Swanson et al. (2001) were rated on a four-point Likert scale ranging from 0 (not at all) to 3 (very much). This instrument includes three subscales: Inattention (α = 0.92), Hyperactivity (α = 0.90) and Oppositional behaviors (α = 0.86) and presents satisfactory reliability (α = 0.94). It was completed by educators in this French version (Caci 2008). All Cronbach alphas reported here and in the following parts refer to this study.
Child behavior checklist (CBCL)
The CBCL version for ages 4 to 18 years was proposed by Achenbach (1991) to assess child and adolescent problems. It is one of the most widely used questionnaire to capture behavior problems among young people. Both internalizing (α = 0.80) and externalizing (α = 0.92) behavior subscales were used in this study. Overall, externalizing problems subscale refers to behaviors such as cruelty, bullying, meanness to others, breaking the rules or using substance while internalizing problems subscale refers to emotional difficulties such as crying, having fears or nightmares, being unhappy, or having worries. The French version of the CBCL was reported as a reliable measure (Fombonne 1989) and shows a good reliability (α = 0.93). The questionnaire was completed by educators in charge of the adolescent boys.
Multiscore depression inventory for children (MDI-C)
The MDI-C was developed by Berndt and Kaiser (1996) to assess depressive symptoms in children and adolescents (the French version of Berndt and Kaiser 1999, was used). This questionnaire was created to capture global depression as well as eight facets of the depressive symptomatology (i.e., Anxiety, Self-esteem, Sad mood, Instrumental helplessness, Social introversion, Low energy, Pessimism and Defiance) thanks to 79 true-false items. Internal consistency was high for the total score (α = 0.94). Its strengths lie in its short duration of completion and its easy understanding due to short sentences and a two-option response format.
Impulsive behavior scale (UPPS-P)
The UPPS impulsivity scale was originally created by Whiteside and Lynam (2001) in order to assess impulsive behavior. This 45-item version includes four factors: Lack of Premeditation (e.g., “I usually think carefully before doing anything”), Lack of Perseverance (e.g., “I finish what I start), Urgency (e.g., “When I am upset I often act without thinking”) and Sensation Seeking (e.g., “I quite enjoy taking risks). This study used the short, 20-item French version of the UPPS-P adapted for youth (Billieux et al. 2014). The answers are self-reported and scored on a four-point Likert scale ranging from 1 (strongly agree) to 4 (strongly disagree). Overall, the psychometric features in the current study were questionable for all dimensions: global Cronbach alpha = 0.60, Urgency (α = 0.69), Lack of Premeditation (α = 0.56), Lack of Perseverance (α = 0.64), Sensation Seeking (α = 0.50).
Data Analyses
Correlations were performed between CBCL externalizing problems and inattention, hyperactivity and oppositional behaviors subscales of the SNAP-IV (respectively: r(44) = 0.53, r(44) = 0.45, r(44) = 0.73, p < 0.01). These correlations are globally consistent, demonstrating the reliability of the educators’ rating. However, when looking at the correlation between the MDI-C (self-reported questionnaire) and the internalizing problems subscale of the CBCL (educators-reported questionnaire), the correlation coefficient was only equal to 0.12 (p = 0.44). This result could indicate a gap between the perception of the adolescents and the one of their educators about emotional difficulties.
In order to proceed to paired comparisons, each participant of the experimental group was matched with a participant of the control group based on similar global pre-scores of the MDI-C, the UPPS-P, the SNAP-IV and the CBCL questionnaires. The score difference for each questionnaire had to not exceed one standard deviation. These pairs constituted a repeated factor in subsequent analyses and improve the statistical power.
To test the MBP efficacy, MANOVAs were performed for each questionnaire. Questionnaire dimensions were considered as a multivariate factor while Time (T1, T2, T3), and Pair (Group variable) as within-subject factors. When the Time*Pair*Dimensions effect was not significant, we did not examine the dimensions of the questionnaire. We also explored the specific effects of the two parts of the program: the psycho-education part (T1 vs. T2) and the MBP part (T2 vs. T3). In order to do that, we used the Reliable Change Index (RCI) proposed by Jacobson and Truax (1991). This index is a reliable tool to assess clinical change with greater accuracy than a simple score difference. After calculating the RCI for each variable between T1 and T2 and between T2 and T3, we compared them with a paired t-test and we reported the number of individuals with a significant improvement (RCI ≥ 1.96) and a significant deterioration (RCI ≤ −1.96).
Finally, the potential mediating role of impulsivity on outcomes was investigated using the PROCESS modeling tool (Hayes 2012, 2013). This statistical approach has the advantage of using bootstrap and does not require evidence of a total effect prior to the estimation of direct and indirect effects. However, we only performed the mediation when the group variable (IV) was significantly correlated to the facet.
Results
Descriptive Analyses
On the 48 participants selected, 22 remained at post-test in each group (N = 44). Reasons of drop out were: (1) refusal to complete questionnaires (n = 1), (2) having left the institution (n = 2), and (3) more than 50% of session missed (n = 1). There was no difference at baseline between the adolescents who did drop out and those who did not (ps > 0.44) nor between the control and experimental group on all scales and subscales (all ps > 0.21). Means and standard deviations for the four questionnaires can be seen in the Table 2.
Behavioral Problems and ADHD
At time 1, the scores of the SNAP-IV ranged from 2 to 52 in the control group (M = 24.23, SD = 13.79) whereas they ranged from 8 to 63 in the mindfulness group (M = 27.45, SD = 15.13). No main effect of Time nor interaction were found for the total score of the SNAP-IV (Table 3). Consistent with these results, no differences on the RCI were found between groups during the psychoeducation part of the program (T1 vs. T2) or during the mindfulness part (T2 vs. T3; see Table 4).
For the internalizing problems subscale of the CBCL at time 1, the scores ranged from 1 to 24 in the control group (M = 10.54, SD = 5.77) and ranged from 1 to 25 in the mindfulness group (M = 11.13, SD = 7.19). For the externalizing problems subscale at time 1, the scores ranged from 3 to 42 in the control group (M = 16.72, SD = 9.55) whereas they ranged from 5 to 52 in the mindfulness group (M = 18.09, SD = 12.07). No significant effect was found for the internalizing problems subscale (Table 3). However, a significant interaction Time × Pair was observed for the externalizing problems subscale, F(2,42) = 5.39, p = 0.008. When looking at the RCI for the different parts of the program, we can observe a significant difference between the group after the MBP, t(21) = −2.93, p = 0.008 (Table 4). Consistent with hypotheses, this result indicates an improvement of behavioral problems for the experimental group compared to the control group after the MBP. However, considering the negative RCI in the control group (RCI = −0.57) and the low RCI in the experimental group (RCI = 0.17), this significant difference could be the consequence of a protective effect of the MBP against a natural deterioration rather than its positive effect on externalizing problems.
Depressive Symptomatology
At time 1, MDI-C scores ranged from 38 to 76 in the control group (M = 570.59, SD = 10.17) whereas they ranged from 39 to 74 in the mindfulness group (M = 56.54, SD = 9.8). The MANOVA revealed a main effect of Time, indicating an improvement of depressive symptomatology over time in the two groups, F(2,42) = 8.13, p = 0.001, but there was no interaction with Pair nor with Pair and Dimension (see Table 3). Consistently, we found no differences on the RCI between groups during the psychoeducation part of the program (T1 vs. T2) or during the mindfulness part (T2 vs. T3; see Table 4).
Impulsivity Symptoms
At time 1, the scores on the UPPS-P ranged from 41 to 67 in the control group (M = 52.77, SD = 6.36) and ranged from 33 to 67 in the mindfulness group (M = 50.13, SD = 7.42). The MANOVA conducted on impulsivity score revealed no significant change (Table 3). However, the results of the RCI demonstrated a trend of improvement for the mindfulness group compared to the control group, t(21) = −2.03, p = 0.055 (Table 4).
Mediating Role of Impulsivity
Prior to test all the four subscales of impulsivity, we checked the correlation of the facets (the RCI score between T2 and T3) with the group variable (Control vs. MBP). Two facets were correlated to the group variable: the Urgency facet (r = 0.32) and the Sensation Seeking facet (r = 0.35). Therefore, we only tested the mediation with these two variables. We used the externalizing problems as the outcome given that it is the only variable that showed a significant improvement. In order to perform the analyses, we used the free PROCESS macro of Hayes (2013) in SPSS 21 with the following script:
Where “x”, the independent variable, is the group variable (i.e., MBP or control group), “y”, the dependent variable, is the outcome variable (i.e., the RCI calculated with the externalizing problems scores at T2 and T3) and “med”, the mediator, is the two facets of impulsivity (i.e., RCI of Urgency and Sensation Seeking).
The code generates a bootstrap confidence interval for the indirect effect using 10,000 bootstrap samples with a 95% confidence level. The Sobel tests indicated no mediating effect of the Urgency (β = 0.03, CI = [−0.21; 0.24], p = 0.80) or the Sensation Seeking (β = −0.16, CI = [−0.38; 0.05], p = 0.22) on the association between MBP and externalizing problems.
Acceptability of the Program
Fifteen of the twenty-two participants who followed the MBP were successfully contacted and interviewed nine months after the end of the program. At the question: “In your memories, was it easy to do the mindfulness exercises? Can you give me a score from 0 to 10? (knowing that 10 means very easy and that 0 means very difficult)”, the 15 participants gave a mean of 7.76. At the question “Did you enjoy participating in the mindfulness program? Can you give me a score from 0 to 10? (knowing that 10 means you really enjoyed participating and that 0 means you did not enjoy at all participating)”, the participants gave a mean of 8.53. Finally, nine participants stated that they continued to practice mindfulness. However, four participants mentioned in the interview that the activities were not appropriate to their age (two because the explanations were too complicated and two others because the activities were too childish). In addition, four participants indicated that they had difficulty remembering the content of the intervention.
Discussion
Some evidence supports that MBPs reduce anxiety and depressive symptomatology in young populations (Zack et al. 2014). In particular, adolescents with behavior disorders might benefit from this kind of intervention, as it focuses on attention, emotions regulation, and impulsivity. However, research on MBPs efficacy among this population focuses almost exclusively on ADHD and presents some limitations such as a lack of well-designed studies (absence of a control group) and a lack of well-established diagnoses (Lee et al. 2017). Several aspects of the present study aimed to address these issues.
According to the results obtained by the RCIs, the externalizing problems, evaluated by the educators, remained stable between T2 and T3 for the mindfulness group while they increased in the control group. These findings suggest that educators perceived adolescents who practiced mindfulness as youth with less inappropriate behaviors. This partly confirms the conclusions of studies that have observed similar results without using a control group. Indeed, in a population of adolescents suffering from externalizing disorders who followed a MBP, Bögels et al. (2008) found a trend improvement of the CBCL externalizing behavior score, rated by the parents, 2 weeks after the end of the program. Similar observations have been reported in small groups of children and adolescents with ADHD who improved their externalizing problems after a MBP (Haydicky et al. 2012, 2015; Van de Weijer-Bergsma et al. 2012; Zhang et al. 2017).
However, in the present data, the improvement in externalizing symptomatology was not evidenced by the SNAP-IV. The SNAP-IV focuses on the features of the ADHD diagnosis: inattention, hyperactivity, and oppositional behaviors (Swanson et al. 2012) while the externalizing subscale of the CBCL take into account ODD symptoms (which are, in fact, partly assessed by the oppositional behavior subscale of the SNAP-IV) plus physical aggressiveness plus CD symptoms. This is probably why the correlation between oppositional behaviors subscale and externalizing problems was so high (r = 0.73, p < 0.01). Consistently, when looking at the oppositional behaviors subscale of the SNAP-IV (see Table 2), we notice the same pattern of evolution as the externalizing problems subscale of the CBCL (i.e., a decrease in the means for the experimental group and an increase for the control group between T2 and T3). Overall, adolescents may have less problems of behavior related to aggressiveness but continue to be hyperactive and inattentive. Yet, some studies suggest an impact of a MBP on ADHD symptoms (e.g., Van der Oord et al. 2012), indicating that more research is needed to precise the effect of mindfulness training on behavior disorders.
Despite the improvement on externalizing problems subscale, no changes were observed for the internalizing problems subscale. Congruently, several studies failed to observe a significant decrease in internalizing problems when assessed by parents or educators (Bögels et al. 2008; Haydicky et al. 2015; Van de Weijer-Bergsma et al. 2012). However, when the internalizing symptomatology was reported by the adolescents, most studies found a decrease in these symptoms. Similar findings were found in our study: the scores of the self-reported questionnaire on depressive symptomatology tended to decrease while no changes were observed for the internalizing subscale completed by the educators. In the same way, the coefficient of correlation between these two questionnaires was surprisingly low and not significant. Educators and parents might experience difficulties in identifying precisely internalizing symptoms contrary to externalizing symptoms. In addition, educators were aware of the group allocation. Their positive expectations could therefore limit the interpretation of the present results.
The results related to depressive symptomatology showed an improvement in both groups. In contrast, Biegel et al. (2009) observed in adolescent psychiatric outpatients a more pronounced decrease in the mindfulness group as compared to the control group. In the present study, the MBP did not bring better benefits on depressive symptomatology than the usual treatment alone, but, interestingly, both groups fell below the clinical threshold of the MDI-C at T3 (<56; Berndt and Kaiser 1999). The overall decrease in depressive symptomatology may be explained by the spontaneous positive evolution of a major part of male adolescents (Dekker et al. 2007) and by the many interventions (psychotherapy, psychomotricity, and speech therapy) routinely provided by the institution as usual care. Considering the intensity of this institutional treatment, MBP could hardly provide additional benefits.
If some improvements in behavior were observed, it seems important to identify the processes that underlie these changes. It was postulated that impulsivity was a central factor in obtaining benefits by providing a space for reflection and a better understanding of inner state before acting. Results showed that impulsivity score tends to decrease between T2 and T3 only for the experimental group. This finding may demonstrate the positive effect of the MBP on inhibition, which is in line with the results obtained by Deplus et al. (2016) in a clinical population of adolescents. Concerning the facets of impulsivity, previous studies have documented that the reduction of urgency predicts a decrease in illegal drug use, alcohol consumption, risky sexual behavior or gambling problems (Cyders et al. 2010; Zapolski et al. 2009). However, no mediating effect was observed for the two facets of impulsivity (Urgency and Sensation Seeking) which were correlated to the group variable. It is possible that impulsivity only plays a minor role as a process of the MBP. Moreover, other processes not evaluated in this study may be involved. For instance, the study of Van der Gucht et al. (2017) showed that cognitive reactivity (i.e., the propensity to have negative thoughts in sad mood), and self-coldness (i.e., the lack of self-compassion), mediated the improvement obtained by the mindfulness intervention on the symptoms of depression, anxiety and stress.
Finally, the qualitative results indicated a good acceptability of the program. The high scores obtained for the question concerning the facility (M = 7.76) and the question concerning the appreciation of the program (M = 8.53) showed that the implementation of a MBP in this population is possible and well received. Also, by considering the participants feedbacks, it seems that the cognitive development differences observed among the adolescents (not only related to their age) should be taken into account. In this way, instructors should be careful about the use of metaphors, vocabulary, or games, and adapt their teaching to their audience. As regard the maintaining of the practice, more than half of the participants contacted nine months after the end of the program continue to practice. However, the 15 participants interviewed were still in the institution, which encouraged them to continue practicing. It is therefore difficult to know if they would have continued practicing without the institutional support.
Limitations and Future Research
Several limitations of this study must be mentioned. Firstly, the conclusions drawn from the results must be considered carefully according to the limited sample size, the focus on adolescent boys and the partial randomization of the participants. Secondly, the control group was inactive, although the institution already provided intensive care to all participants. Still, future studies with active control group, such as education to health program, and full randomization are needed to specifically identify the benefits of the intervention. Thirdly, the use of self-reported questionnaires in a population with low cognitive resources may affect the sensitivity of the measures. The consideration of IQ would have been a plus. In the same way, the low psychometric quality of UPPS-P questionnaire limits the scope of conclusions. Thus, observations in behavioral tasks or experimental situations might lead to a more reliable assessment. Finally, the absence of a follow-up based on quantitative data did not allow to identify the potential long-term effects of the intervention.
Regarding future prospects, it could be useful to involve the parents into the program. Numerus studies conducted in ADHD populations that demonstrated a positive effect of the MBP, targeted youth and their parents (Cassone 2015; Haydicky et al. 2015; Lo et al. 2020). Particularly, the involvement of the parents could improve the children motivation to keep mindfulness practice. In the same way, future research should address the role of practice time in daily life among this population and the program aspects that improve their involvement. Also, little is known about the benefits differences that can be observed among the several behavior disorders diagnoses. Maybe MBPs are more suitable for ADHD than for ODD and CD. For now, it is not yet possible to draw definitive conclusions. To our knowledge, no studies have examined the need to prepare youth with behavior disorders to mindfulness practice (such as psychoeducation to emotions in our study), which is quite surprising considering the characteristics of the population (who has difficulty sitting quietly for example) and our clinical experience. Still, previous studies did not mention the necessity of a preparation prior to the MBP. Beyond the effect on outcomes, processes that are implied in the efficacy of MBPs among adolescents are still unknown. For instance, mindfulness can bring a better emotional awareness of emotions or unwanted behaviors. Hence, studies should further the investigation of some psychological processes such as emotion regulation, awareness or psychological inflexibility (Chambers et al. 2015; Fung et al. 2019). Overall, MBPs may appear as relevant interventions to help adolescents with behavior disorders.
References
Achenbach, T. M. (1991). Integrative guide for the 1991 CBCL/4-18, YSR, and TRF profiles. Burlington, VT: University of Vermont.
Ahmad, S. I., & Hinshaw, S. P. (2016). Attention-deficit/hyperactivity disorder, trait impulsivity, and externalizing behavior in a longitudinal sample. Journal of Abnormal Child Psychology. https://doi.org/10.1007/s10802-016-0226-9.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. https://doi.org/10.1176/appi.books.9780890425596.
Ames, C. S., Richardson, J., Payne, S., Smith, P., & Leigh, E. (2014). Mindfulness-based cognitive therapy for depression in adolescents. Child and Adolescent Mental Health, 19(1), 74–78.
Avenevoli, S., Swendsen, J., He, J.-P., Burstein, M., & Merikangas, K. R. (2015). Major depression in the National Comorbidity Survey–Adolescent Supplement: prevalence, correlates, and treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 54(1), 37–44. https://doi.org/10.1016/j.jaac.2014.10.010.
Barkley, R. A. (1997). Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65.
Berndt, D. J., & Kaiser, C. F. (1999). Manuel: Echelle composite de dépression pour enfant (MDI-C). Paris: Editions Du Centre de Psychologie Appliquée.
Berndt, D. J., & Kaiser, C. F. (1996). Multiscore depression inventory for children. Los Angeles: Western Psychological Services. http://www.wpspublish.com/store/Images/Downloads/Product/MDI-C_Manual_Chapter_1.pdf.
Biegel, G. M., Brown, K. W., Shapiro, S. L., & Schubert, C. M. (2009). Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: a randomized clinical trial. Journal of Consulting and Clinical Psychology, 77(5), 855.
Billieux, J., Rochat, L., & Van der Linden, M. (2014). L'impulsivité: ses facettes, son évaluation et son expression clinique. Liège, BE: Mardaga.
Boden, J. M., Fergusson, D. M., & Horwood, L. J. (2010). Risk factors for conduct disorder and oppositional/defiant disorder: evidence from a New Zealand birth cohort. Journal of the American Academy of Child & Adolescent Psychiatry, 49(11), 1125–1133.
Bögels, S., Hoogstad, B., van Dun, L., de Schutter, S., & Restifo, K. (2008). Mindfulness training for adolescents with externalizing disorders and their parents. Behavioural and Cognitive Psychotherapy, 36(02), 193–209.
Broderick, P. C., & Jennings, P. A. (2012). Mindfulness for adolescents: a promising approach to supporting emotion regulation and preventing risky behavior. New Directions for Student Leadership, 2012(136), 111–126.
Broderick, P. C., & Metz, S. (2009). Learning to BREATHE: a pilot trial of a mindfulness curriculum for adolescents. Advances in School Mental Health Promotion, 2(1), 35–46.
Burke, C. A. (2010). Mindfulness-based approaches with children and adolescents: a preliminary review of current research in an emergent field. Journal of Child and Family Studies, 19(2), 133–144.
Caci, H. (2008). SNAP-IV: Instructions pour la cotation, version française. https://tdahbe.files.wordpress.com/2013/02/snap_french.pdf.
Cairncross, M., & Miller, C. J. (2020). The effectiveness of mindfulness-based therapies for ADHD a meta-analytic review. Journal of Attention Disorders, 24(5), 627–643. https://doi.org/10.1177/1087054715625301.
Cartwright-Hatton, S., Roberts, C., Chitsabesan, P., Fothergill, C., & Harrington, R. (2004). Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. British Journal of Clinical Psychology, 43(4), 421–436.
Casey, B. J., Duhoux, S., & Cohen, M. M. (2010). Adolescence: what do transmission, transition, and translation have to do with it? Neuron, 67(5), 749–760.
Cassone, A. R. (2015). Mindfulness training as an adjunct to evidence-based treatment for ADHD within families. Journal of Attention Disorders, 19(2), 147–157.
Chambers, R., Gullone, E., & Allen, N. B. (2009). Mindful emotion regulation: an integrative review. Clinical Psychology Review, 29(6), 560–572.
Chambers, R., Gullone, E., Hassed, C., Knight, W., Garvin, T., & Allen, N. (2015). Mindful emotion regulation predicts recovery in depressed youth. Mindfulness, 6(3), 523–534.
Chi, X., Bo, A., Liu, T., Zhang, P., & Chi, I. (2018). Effects of mindfulness-based stress reduction on depression in adolescents and young adults: a systematic review and meta-analysis. Frontiers in Psychology, 9, 1034.
Chimiklis, A. L., Dahl, V., Spears, A. P., Goss, K., Fogarty, K., & Chacko, A. (2018). Yoga, mindfulness, and meditation interventions for youth with ADHD: systematic review and meta-analysis. Journal of Child and Family Studies, 27(10), 3155–3168.
Colman, I., Murray, J., Abbott, R. A., Maughan, B., Kuh, D., Croudace, T. J., & Jones, P. B. (2009). Outcomes of conduct problems in adolescence: 40 year follow-up of national cohort. Bmj, 338, a2981.
Costello, E. J., Copeland, W., & Angold, A. (2011). Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry, 52(10), 1015–1025.
Cyders, M. A., Zapolski, T. C., Combs, J. L., Settles, R. F., Fillmore, M. T., & Smith, G. T. (2010). Experimental effect of positive urgency on negative outcomes from risk taking and on increased alcohol consumption. Psychology of Addictive Behaviors, 24(3), 367.
d’Acremont, M., & Van der Linden, M. (2007). How is impulsivity related to depression in adolescence? Evidence from a French validation of the cognitive emotion regulation questionnaire. Journal of Adolescence, 30(2), 271–282.
Dekker, M. C., Ferdinand, R. F., Van Lang, N. D., Bongers, I. L., Van Der Ende, J., & Verhulst, F. C. (2007). Developmental trajectories of depressive symptoms from early childhood to late adolescence: gender differences and adult outcome. Journal of Child Psychology and Psychiatry, 48(7), 657–666.
Deplus, S., Billieux, J., Scharff, C., & Philippot, P. (2016). A mindfulness-based group intervention for enhancing self-regulation of emotion in late childhood and adolescence: a pilot study. International Journal of Mental Health and Addiction, 14(5), 775–790.
Deplus, S., & Lahaye, M. (2015). La pleine conscience chez l’enfant et l’adolescent. Mardaga: Programmes d’entraînement à la pleine conscience. https://books.google.fr/books?hl=fr&lr=&id=0yQiCwAAQBAJ&oi=fnd&pg=PT3&dq=La+pleine+conscience+chez+l%27enfant+et+l%27adolescent&ots=B4JPRB16h7&sig=IW6d-gWdVUxw55BA4jCkNi9ys4E.
Deyo, M., Wilson, K. A., Ong, J., & Koopman, C. (2009). Mindfulness and rumination: does mindfulness training lead to reductions in the ruminative thinking associated with depression? EXPLORE: The Journal of Science and Healing, 5(5), 265–271.
Dunning, D. L., Griffiths, K., Kuyken, W., Crane, C., Foulkes, L., Parker, J., & Dalgleish, T. (2018). Research review: The effects of mindfulness-based interventions on cognition and mental health in children and adolescents—a meta-analysis of randomized controlled trials. Journal of Child Psychology and Psychiatry, 60(3), 244–258.
Flory, K., Milich, R., Lynam, D. R., Leukefeld, C., & Clayton, R. (2003). Relation between childhood disruptive behavior disorders and substance use and dependence symptoms in young adulthood: Individuals with symptoms of attention-deficit/hyperactivity disorder are uniquely at risk. Psychology of Addictive Behaviors, 17(2), 151.
Fombonne, E. (1989). The child behaviour checklist and the rutter parental questionnaire: a comparison between two screening instruments. Psychological Medicine, 19(03), 777–785.
Fung, J., Kim, J. J., Jin, J., Chen, G., Bear, L., & Lau, A. S. (2019). A randomized trial evaluating school-based mindfulness intervention for ethnic minority youth: exploring mediators and moderators of intervention effects. Journal of Abnormal Child Psychology, 47(1), 1–19.
Grossman, P., Niemann, L., Schmidt, S., & Walach, H. (2004). Mindfulness-based stress reduction and health benefits: a meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43.
Haydicky, J., Shecter, C., Wiener, J., & Ducharme, J. M. (2015). Evaluation of MBCT for adolescents with ADHD and their parents: Impact on individual and family functioning. Journal of Child and Family Studies, 24(1), 76–94.
Haydicky, J., Wiener, J., Badali, P., Milligan, K., & Ducharme, J. M. (2012). Evaluation of a mindfulness-based intervention for adolescents with learning disabilities and co-occurring ADHD and anxiety. Mindfulness, 3(2), 151–164.
Hayes, A. F (2012). PROCESS: a versatile computational tool for observed variable mediation, moderation, and conditional process modeling. KS: University of Kansas. https://is.muni.cz/el/1423/podzim2014/PSY704/50497615/hayes_2012_navod_process.pdf.
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New-York, NY: Guilford Press. https://books.google.fr/books?hl=fr&lr=&id=iWFSpQFh-y4C&oi=fnd&pg=PP1&dq=Hayes+process+spss&ots=1zY3ozZHT_&sig=o1xQBM84xW5qjThH8QD49qWi3sQ.
Heeren, A., & Philippot, P. (2011). Changes in ruminative thinking mediate the clinical benefits of mindfulness: Preliminary findings. Mindfulness, 2(1), 8–13.
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559.
Jacobson, N. S., & Truax, P. (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice, 10(2), 144–156.
Kahl, K. G., Winter, L., & Schweiger, U. (2012). The third wave of cognitive behavioural therapies: what is new and what is effective? Current Opinion in Psychiatry, 25(6), 522–528.
Kallapiran, K., Koo, S., Kirubakaran, R., & Hancock, K. (2015). Review: effectiveness of mindfulness in improving mental health symptoms of children and adolescents: a meta-analysis. Child and Adolescent Mental Health, 20(4), 182–194.
Keenan, K., Wroblewski, K., Hipwell, A., Loeber, R., & Stouthamer-Loeber, M. (2010). Age of onset, symptom threshold, and expansion of the nosology of conduct disorder for girls. Journal of Abnormal Psychology, 119(4), 689.
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: a meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528. https://doi.org/10.1016/j.jpsychores.2015.03.009.
Kuyken, W., Weare, K., Ukoumunne, O. C., Vicary, R., Motton, N., Burnett, R., Cullen, C., Hennelly, S., & Huppert, F. (2013). Effectiveness of the mindfulness in schools programme: non-randomised controlled feasibility study. The British Journal of Psychiatry, 203(2), 126–131.
Lagor, A. F., Williams, D. J., Lerner, J. B., & McClure, K. S. (2013). Lessons learned from a mindfulness-based intervention with chronically ill youth. Clinical Practice in Pediatric Psychology, 1(2), 146.
Lam, A. K., & Ho, T. P. (2010). Early adolescent outcome of attention-deficit hyperactivity disorder in a Chinese population: 5-year follow-up study. Hong Kong Medical Journal, 16(4), 257–264.
Lee, C. S., Ma, M., Ho, H., Tsang, K., Zheng, Y., & Wu, Z. (2017). The effectiveness of mindfulness-based intervention in attention of individuals with ADHD: a systematic review. Hong Kong Journal of Occupational Therapy, 30, 33–41.
Lee, S. S., Humphreys, K. L., Flory, K., Liu, R., & Glass, K. (2011). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clinical Psychology Review, 31(3), 328–341.
Liu, J. (2004). Childhood externalizing behavior: theory and implications. Journal of Child and Adolescent Psychiatric Nursing, 17(3), 93–103.
Lo, H. H., Wong, S. W., Wong, J. Y., Yeung, J. W., Snel, E., & Wong, S. Y. (2020). The effects of family-based mindfulness intervention on ADHD symptomology in young children and their parents: a randomized control trial. Journal of Attention Disorders, 24(5), 667–680. https://doi.org/10.1177/1087054717743330.
McDonough-Caplan, H., Klein, D. N., & Beauchaine, T. P. (2018). Comorbidity and continuity of depression and conduct problems from elementary school to adolescence. Journal of Abnormal Psychology, 127(3), 326.
Mendelson, T., Greenberg, M. T., Dariotis, J. K., Gould, L. F., Rhoades, B. L., & Leaf, P. J. (2010). Feasibility and preliminary outcomes of a school-based mindfulness intervention for urban youth. Journal of Abnormal Child Psychology, 38(7), 985–994.
Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., & Swendsen, J. (2010). Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989.
Mojtabai, R., Olfson, M., & Han, B. (2016). National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics, 138(6), e20161878.
Muris, P., Meesters, C., & Blijlevens, P. (2007). Self-reported reactive and regulative temperament in early adolescence: relations to internalizing and externalizing problem behavior and “Big Three” personality factors. Journal of Adolescence, 30(6), 1035–1049.
Nolen-Hoeksema, S., & Watkins, E. R. (2011). A heuristic for developing transdiagnostic models of psychopathology: explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6(6), 589–609.
Philippot, P., Bouvard, M., Baeyens, C., & Dethier, V. (2019). Case conceptualization from a process-based and modular perspective: rationale and application to mood and anxiety disorders. Clinical Psychology & Psychotherapy, 26(2), 175–190.
Sedlmeier, P., Eberth, J., Schwarz, M., Zimmermann, D., Haarig, F., Jaeger, S., & Kunze, S. (2012). The psychological effects of meditation: a meta-analysis. Psychological Bulletin, 138(6), 1139.
Semple, R. J., & Lee, J. (2007). Mindfulness-based cognitive therapy for anxious children: a manual for treating childhood anxiety. Oakland, CA: New Harbinger Publications. https://books.google.fr/books?hl=fr&lr=&id=qT6nSwnipiMC&oi=fnd&pg=PP3&dq=Mindfulness-Based+Cognitive+Therapy+for+Anxious+Children:+A+Manual+for&ots=gJRqhgVlTz&sig=ZAYlAFlxYOaF6n2igUqGZYUp_70.
Semple, R. J., Reid, E. F., & Miller, L. (2005). Treating anxiety with mindfulness: an open trial of mindfulness training for anxious children. Journal of Cognitive Psychotherapy, 19(4), 379–392.
Singh, N. N., Lancioni, G. E., Singh Joy, S. D., Winton, A. S., Sabaawi, M., Wahler, R. G., & Singh, J. (2007). Adolescents with conduct disorder can be mindful of their aggressive behavior. Journal of Emotional and Behavioral Disorders, 15(1), 56–63.
Sonuga-Barke, E. J., Brandeis, D., Cortese, S., Daley, D., Ferrin, M., Holtmann, M., Stevenson, J., Danckaerts, M., Van der Oord, S., & Döpfner, M., et al. (2013). Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. American Journal of Psychiatry, 170(3), 275–289.
Swanson, J. M. (1995). SNAP-IV Scale. Irvine, CA: University of California Child Development Center.
Swanson, J. M., Kraemer, H. C., Hinshaw, S. P., Arnold, L. E., Conners, C. K., Abikoff, H. B., Clevenger, W., Davies, M., Elliott, G. R., & Greenhill, L. L., et al. (2001). Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 40(2), 168–179.
Swanson, J. M., Schuck, S., Porter, M. M., Carlson, C., Hartman, C. A., Sergeant, J. A., Clevenger, W., Wasdell, M., McCleary, R., & Lakes, K. (2012). Categorical and dimensional definitions and evaluations of symptoms of ADHD: history of the SNAP and the SWAN rating scales. The International Journal of Educational and Psychological Assessment, 10(1), 51.
Tan, L., & Martin, G. (2013). Taming the adolescent mind: preliminary report of a mindfulness-based psychological intervention for adolescents with clinical heterogeneous mental health diagnoses. Clinical Child Psychology and Psychiatry, 18(2), 300–312. https://doi.org/10.1177/1359104512455182.
Tan, L., & Martin, G. (2015). Taming the adolescent mind: a randomised controlled trial examining clinical efficacy of an adolescent mindfulness‐based group programme. Child and Adolescent Mental Health, 20(1), 49–55. https://doi.org/10.1111/camh.12057.
Van de Weijer-Bergsma, E., Formsma, A. R., de Bruin, E. I., & Bögels, S. M. (2012). The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. Journal of Child and Family Studies, 21(5), 775–787.
Van der Gucht, K., Takano, K., Raes, F., & Kuppens, P. (2017). Processes of change in a school-based mindfulness programme: Cognitive reactivity and self-coldness as mediators. Cognition and Emotion, 32(3), 658–665.
Van der Oord, S., Bögels, S. M., & Peijnenburg, D. (2012). The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. Journal of Child and Family Studies, 21(1), 139–147.
Van Vliet, K. J., Foskett, A. J., Williams, J. L., Singhal, A., Dolcos, F., & Vohra, S. (2016). Impact of a mindfulness-based stress reduction program from the perspective of adolescents with serious mental health concerns. Child and Adolescent Mental Health. https://doi.org/10.1111/camh.12170/full.
Whiteside, S. P., & Lynam, D. R. (2001). The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689.
Witkiewitz, K., King, K., McMahon, R. J., Wu, J., Luk, J., Bierman, K. L., Coie, J. D., Dodge, K. A., Greenberg, M. T., & Lochman, J. E. (2013). Evidence for a multi-dimensional latent structural model of externalizing disorders. Journal of Abnormal Child Psychology, 41(2), 223–237.
Zack, S., Saekow, J., Kelly, M., & Radke, A. (2014). Mindfulness based interventions for youth. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 32(1), 44–56.
Zapolski, T. C., Cyders, M. A., & Smith, G. T. (2009). Positive urgency predicts illegal drug use and risky sexual behavior. Psychology of Addictive Behaviors, 23(2), 348.
Zenner, C., Herrnleben-Kurz, S., & Walach, H. (2014). Mindfulness-based interventions in schools—a systematic review and meta-analysis. Frontiers in Psychology, 5, 603.
Zhang, D., Chan, S. K. C., Lo, H. H. M., Chan, C. Y. H., Chan, J. C. Y., Ting, K. T., Gao, T. T., Lai, K. Y. C., Bögels, S. M., & Wong, S. Y. S. (2017). Mindfulness-based intervention for Chinese children with ADHD and their parents: a pilot mixed-method study. Mindfulness, 8(4), 859–872.
Zoogman, S., Goldberg, S. B., Hoyt, W. T., & Miller, L. (2015). Mindfulness interventions with youth: a meta-analysis. Mindfulness, 6(2), 290–302.
Acknowledgements
Data collection has been made possible by the help of the residential service for youth Reumonjoie and with the help of Francine Gitton, Isabelle Melin, Carine Lefèvre, Annick Marchale, Carine Hamende and all the educators of this institution. We would particularly like to thank the Huoshen foundation for its financial support that has enabled many underserved youths to have access to mindfulness programs.
Author Contributions
B.R.: designed and executed the study, analyzed the data, and wrote the paper. P.P.: collaborated with the design, data analyses and writing of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All authors complied with ethical standards in the treatment of participants. The study was approved by the ethic committee of Catholic University of Louvain.
Informed Consent
All participants and their parents provided written informed consent prior to participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roux, B., Philippot, P. A Mindfulness-Based Program among Adolescent Boys with Behavior Disorders: A Quasi-Experimental Study. J Child Fam Stud 29, 2186–2200 (2020). https://doi.org/10.1007/s10826-020-01751-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-020-01751-z