Abstract
Objective
Partial hospitalization programs are an increasingly utilized, multidisciplinary treatment for children with social, emotional, and behavioral needs. Although previous work suggests these programs improve children’s mental health functioning, outcomes research has been limited. This study examines moderators of emotional and behavioral outcomes in children with serious mental illness, with particular focus on demographic (age, race, insurance type, and gender) and family (stressors and supports) factors.
Method
The study includes 287 children ages 7–13. Children completed standardized questionnaires at admission and discharge including the Behavior Assessment System for Children-2 the Child Depression Inventory 2, and the Screen for Child Anxiety Related Disorders while caregivers completed the Strengths and Difficulties Questionnaire.
Results
Results indicate improvements in children’s anxiety, depressive symptoms, psychological adjustment, and emotional symptoms. Furthermore, children with private insurance reported significant decreases in depressive (p < 0.001) and emotional symptoms (p< 0.001) compared to children with state funded insurance. Females reported sharper decreases in depressive symptoms (p< 0.001) compared to males (p= 0.019). Finally, children in families with no stressors in the past month demonstrated sharper declines in depressive symptoms (p< 0.001) compared to children in families with one or more stressors in the past month (p= 0.001). Family support did not moderate these outcomes.
Conclusions
This study suggests partial hospitalization programs may be effective in improving emotional and behavioral problems. This study suggests family stressors are important to consider and emphasize in treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mental health problems affect nearly one in five children and are a growing public health concern with nearly 50% of all lifetime cases of mental illness with an onset by age 14 (Merikangas et al. 2010; National Alliance on Mental Illness; Perou et al. 2013). Youth with mental health concerns are at risk for poor educational attainment, suicidal behavior, substance abuse, violence, peer problems, and juvenile justice system involvement (National Alliance on Mental Illness; Patel et al. 2007). It is estimated that in the US alone, approximately $247 billion is spent on child mental health problems annually. Thus, the development and evaluation of effective behavioral health programs and treatments is essential.
With recent shifts in healthcare policy affecting mental health services, measuring the outcomes of behavioral health services has become increasingly relevant and programs are often asked to demonstrate effectiveness (Granello et al. 2000; Martin et al. 2013). In particular, partial hospitalization programs, which are a multidisciplinary, family focused treatment for children with serious mental illness, have been subject to pressure to provide more evidence for their efficacy (Granello et al. 2000).
Children who attend children’s partial hospital programs (CPHPs) have behavioral health needs that warrant higher level of care than outpatient therapy, but do not require the intensive care and safety precautions provided by an inpatient unit. In many cases, CPHPs are utilized as a step down from inpatient care to provide a gradual transition back into the home and school environments. Alternatively, CPHPs can be utilized to treat acute behavioral problems and attempt to prevent inpatient hospitalization. Most CPHPs combine individual therapy, family therapy, group therapy, medication management, and educational services to meet the individual needs of each child and his/her family and to improve social, emotional, and behavioral functioning in a comprehensive manner (Boekamp et al. 2018; Grizenko 1997; Lenz and Del Conte 2018). Length of treatment varies by program, but the intensive, multifaceted nature of the services provided typically warrants several weeks to months of treatment (Bennett et al. 2001; Boekamp et al. 2018). Care teams in CPHPs often include specialists trained in psychiatry, clinical psychology, social work, education, and nursing in order to provide a variety of therapeutic interventions that address diverse factors contributing to children’s psychosocial functioning.
While earlier research demonstrates significant psychosocial improvements for children attending CPHPs, the field is currently limited by the small number of recent studies (Martin et al. 2013; Muller et al. 2015). Furthermore, programs examined in older studies may not be generalizable to current program structures and treatments. However, the limited literature on CPHPs demonstrates that these programs are effective in improving social, emotional and behavioral problems from admission to discharge. Early research suggests that CPHPs were effective in improving academic functioning, personality functioning, and parent-reported internalizing and externalizing symptoms (Grizenko and Sayegh 1990). Moreover, CPHPs reduced externalizing and internalizing behavior problems from a clinical range to a normative or nonclinical range in children from two to 19 years of age (Martin et al. 2013; Milin et al. 2000). These programs have also been shown to elicit greater behavioral improvements than shown in outpatient treatments alone. Specifically, researchers found that partial hospitalization treatment led to improvements in family functioning, social skills, and improvements in behavior when compared to outpatient treatment (Grizenko et al. 1993). Despite these promising research findings, few studies have examined moderators of these outcomes to determine who benefits most from treatment, with particular focus on demographic and family factors. Given the significant role of family involvement in treatment of children in a partial hospitalization setting, increased understanding of family factors that may enhance or hinder treatment outcomes is warranted.
A robust body of research demonstrated the impact of parental stress on adverse child outcomes including emotional and behavior problems, and lack of school readiness (Steele et al. 2016; O’Neal et al. 2016; Whitson and Kaufman 2016). In one study, parents who reported exposure to higher adverse childhood experiences in their own childhood endorsed higher levels of parenting stress even after controlling for socioeconomic status (SES; Steele et al. 2016). Parenting stress has also been studied in the context of trauma exposure and mental health outcomes in young children where parenting stress mediates the relationship between the number of child experienced potentially traumatic events and caregiver-reported child problem behaviors at baseline (Whitson and Kaufman 2016).
The treatment of parental stress has also been found to enhance therapeutic change in children with aggressive and antisocial presentations (Kazdin and Whitley 2003). In one study, children between 6 and14 years of age and their families received problem-solving and parent management training (Kazdin and Whitley 2003). Families who received an additional component that specifically targeted parental stress demonstrated enhanced therapeutic change for children and their families. Despite this growing body of research regarding parental stress and associations with childhood outcomes, no studies have been conducted examining family stressors and supports as factors that may influence treatment outcomes in a children’s partial hospital setting.
Accordingly, the purpose of the current study is to examine the effectiveness of a children’s partial hospitalization program on child mental health functioning by examining demographic factors including age, race, insurance type, and gender, and family factors including recent stressors and supports, as moderators of mental health functioning. The program evaluated is located in a psychiatric hospital for children and includes principles from the Incredible Years Parenting Program, which focuses on reducing behavioral problems, improving child-parent interactions, and enhancing children’s social and emotional competence (Webster-Stratton 2005). We predicted that children would report improvements in overall emotional and behavioral symptoms over the course of their admission. Next, given that demographic factors have not been reliably examined as moderators of the child’s emotional and behavioral change over time, we examined demographic factors and hypothesized that the child’s age, gender, race, and insurance type will moderate child reported outcomes. Specifically, previous research has found that internalizing disorders in a pediatric youth sample were moderated by gender, age, race, and SES such that greater changes were observed for females and younger children when using a CBT approach in treatment, European/American youths when compared to ethnic minority youth, and for children with moderate to high SES compared to children with low SES (Mansur et al. 2016; Nilsen et al. 2013). Thus, we hypothesize that greater changes in outcomes will be observed for females, younger, Caucasian children, and children from families with private insurance compared to state funded insurance (see Casey et al. 2018 regarding insurance status as an approximation of SES).
We also predicted that family reported stress in the past month and family reported supports would moderate these outcomes. Specifically, we hypothesized that children in families who reported a lower number of stressors will report decreases in emotional and behavioral symptoms while children in families who report a higher number of stressors will not show significant changes in symptoms. We also hypothesized that children in families who reported a higher number of supports will report decreases in emotional and behavioral symptoms while children in families who reported a lower number of supports will not show significant changes over the course of their CPHP admission.
Methods
Participants
Data were collected from archival clinical data from families with a child diagnosed with a serious mental illness who was admitted to the Child Partial Hospitalization Program (CPHP) in the Northeastern United States. Data collected from families between December 2014 and September 2017 were used for the current report. Inclusion criteria included a minimum length of stay of two weeks, completion of an intake assessment within a week of entering the program, and completion of subsequent assessment at the time of discharge from the program. Only data from the first admission were included in analyses for children who were admitted to the program multiple times during the date range analyzed.
Study participants included 287 children ages seven to 13 (M= 10.17, SD= 1.60) and their caregivers. Participants included 180 males and 107 females. Children who were accessing treatment presented with a variety of primary and secondary diagnoses, which included anxiety (67.6% of the sample), depressive (45.6%), attention deficit (41.8%), autism spectrum (16.4%), disruptive, impulse-control and conduct (15.7%), and trauma and stress related (13.9%) disorders. Children were 76.7% Caucasian, 5.2% African American, 1% Asian, 1.7% American Indian/Alaska Native, 12.5% Hispanic/Latino, 3.5% mixed race, or 2.4% other. Furthermore, 59.9% of the sample had state funded insurance (e.g., Medicaid) and 40.1% had commercial/private insurance. There were no self-pay participants. During their admission at CPHP, some children were admitted to the inpatient unit for stabilization and crisis management. Only children who returned to CPHP after inpatient hospitalization were included in these analyses.
Procedure
The CPHP serves children ages seven to 13 who present with significant behavioral, emotional, or social issues at home, school, or in the community. Program census ranges from eight to 14 children who attend the program for six hours Monday through Friday. Staff and clinicians are trained in the Incredible Years Parenting Program, which has demonstrated effectiveness in reducing behavioral problems, enhancing children’s social and emotional competence, and improving child parent interactions (Webster-Stratton 2005; Webster-Stratton et al. 2011; Webster-Stratton and Reid 2010). The CPHP implements a range of interventions including individual, family, social skills group, milieu, occupational, and art therapy. Children also receive tutoring provided by a special education teacher during the school year.
Treatment is provided in a therapeutic milieu which emphasizes safety, emotion regulation, and behavioral compliance and control. In the milieu, children participate in a minimum of two groups per day which emphasize social competence, coping skills, problem solving, emotion regulation and expression, mindfulness, and social skills. Children also participate in art therapy, occupational therapy, yoga, and therapeutic social games throughout the week. Furthermore, milieu therapists assist children with skill acquisition and generalization and implementing individualized behavior contingency programs, and assist caregivers with parenting strategies during two daily check ins, both at drop off and pick up.
Families participate in family therapy twice per week and interventions are implemented based on the family’s treatment goals. Interventions typically consisted of behavior management, safety planning, management of aggressive behaviors, and providing psychoeducation to caregivers to promote a better understanding of their child’s behavior. Family therapy also focuses on enhancing effective communication strategies among family members including active listening and validation, encouraging problem solving among family members, and promoting appropriate emotion identification and expression among family members.
In addition to individual, group, milieu, and family interventions, children are also evaluated by a psychiatrist to address psychiatric symptoms and daily monitoring regarding ineffectiveness and potential side effects. Medications changes and adjustments were made when appropriate and frequently assessed. In addition, clinicians at CPHP also consulted with community systems including outpatient providers, schools, and pediatricians, to coordinate care and facilitate their transition back to the community. Clinicians also met with children’s schools to discuss the child’s diagnoses, treatment at program, share recommendations for treatment, and work collaboratively with the family and school to develop a school transition plan.
While children received these services and interventions offered through the program, they received individualized treatment tailored for each child’s needs. Specifically, Cognitive Behavioral Therapy (CBT) techniques were used to treat disorders such as anxiety (exposure) and depression (behavioral activation) in the context of challenging automatic negative thoughts, learning relaxation techniques, and engaging in coping strategies to manage and regulate emotions.
Measures
The study consisted of a chart review approved by the Institutional Review Board and included admission and discharge information collected as part of standard program procedures. During the child’s initial days in program, caregivers and children were asked to complete several measures on an electronic tablet, complete a paper copy, or via e-mail, which assessed current child symptomatology, family stressors, and family functioning. Data were collected and stored using REDCap electronic data collection, a secure web-based system used for research studies (Harris et al. 2009). The following measures were used for data analysis:
The Child Depression Inventory 2 (CDI-2; Kovacs 1985)—The CDI-2 is a brief self-report measure completed by the child that assesses cognitive, affective, and behavioral signs of depression in children and adolescents between the ages of 7-17 years old. The CDI-2 contains 27 items grouped into five major factor areas with ratings ranging from 0 to 2 with higher sum scores indicating increased depressive symptoms. The recommended cutoff score in clinical settings approximates 13 while the cut-off score for non-clinical samples approximates 19 or 20 (Kovacs 1985). The CDI-2 has demonstrated high reliability and well-established validity (Kovacs 1985; Smucker et al. 1986). The Total Score for depressive symptoms was used for data analysis and subscales were examined post-hoc using simple models of change over time.
The Screen for Child Anxiety Related Disorders (SCARED; Birmaher et al. 1999)—The SCARED is a brief self-report measures completed by the child and caregiver used to screen for anxiety disorders including separation anxiety disorder, generalized anxiety disorder, panic disorder, and social phobia. The SCARED is composed of 41 items with ratings ranging from 0 (not true or hardly ever true) to 2 (very true or often true) where higher scores indicate increased symptoms of anxiety and a cutoff score of 25 or higher on the child version suggests the presence of an anxiety disorder (Birmaher et al. 1999; Canals et al. 2012). The SCARED has demonstrated good internal consistency, test-retest reliability, and discriminant validity (Birmaher et al. 1997). The Total Score for anxiety symptoms was used for data analysis and subscales were examined post-hoc using simple models of change over time.
The Behavior Assessment System for Children-2, Self-Report of Personality (BASC-2 SRP; Reynolds and Kamphaus 2004)—The BASC-2 is a self-report measure completed by children to assess their overall emotional symptoms. Children aged 7 completed the SRP Interview Form which is administered by a trained clinician and consists of 65 items rated either “yes” or “no.” Children aged 8 to 11 completed the SRP Child Form (139 items) and children aged 12 and 13 completed the SRP Adolescent Form (176 items). Both of these forms include “true” or “false” items and items rated on a 4-point Likert scale (0 = never, 1 = sometimes, 2 = often, 3 = almost always). Item raw scores were summed and converted into standardized T scores for interpretation. Analyses focused on the overall global score (Emotional Symptoms Index) with higher scores representing greater symptom severity (T scores 60-69 at-risk, scores ≥ 70 clinically significant). The SRP forms demonstrate good to excellent internal consistency across general and clinical samples (α = .81 to .96; Reynolds and Kamphaus 2010).
The Strengths and Difficulties Questionnaire (SDQ; Goodman 1997)—The SDQ is a 25-item caregiver reported measure used to assess child psychological adjustment on five subscales including hyperactivity, emotional symptoms, conduct problems, peer problems, and prosocial behavior. Caregivers rated child behavior over the past month on a 3-point scale (0 = not true, 1 = somewhat true, 2 = certainly true). The SDQ can be used for screening, as a component of clinical assessment, a research tool, and a treatment-outcome measure (Goodman et al. 2000). The SDQ also differentiates psychiatric samples from non-psychiatric samples and has demonstrated adequate internal consistency and high convergent validity with other child behavior measures (Goodman 1997; 2001).
We assessed family stress using items from the Family Check Up assessment battery, a brief intervention based on motivational interviewing techniques used to promote family management while addressing adjustment problems in children and adolescents (Dishion and Stormshak 2007; Dishion et al. 2014). At the time of the child’s admission, the caregiver responded to a 15 item checklist that assessed the types of family stress that occurred in the past month. Example questions include: moved or had a change of living arrangements, loss of a loved one, gained a household member, financial problems, had problems with child’s school, someone in household had a serious illness or injury, and witnessed violence or witnessed a crime.
Similar to assessing family stressors, we examined family support using items from the Family Check Up assessment battery (Dishion and Stormshak 2007; Dishion et al. 2014). At the time of the child’s admission, a caregiver responded to eight items that assessed family supports received in the past month from a variety of difference sources including spouse, therapist, relative or family member, friend or coworker, counselor or psychologist, etc. Support was calculated using a sum score, which combined the number and frequency of times caregivers sought support from a variety of different sources (e.g., spouse, friend, family member, counselor, etc.).
Results
Change in Emotional and Behavioral Symptoms Over Time
Means and standard deviations for depressive symptoms, anxiety symptoms, emotional symptoms, and psychological adjustment were computed (see Table 1). One-way repeated measures ANOVAs were conducted to evaluate change in all measures over time. Results suggested improvements from admission to discharge including declines in child reported depressive symptoms, anxiety symptoms, emotional symptoms, and caregiver reported child psychological adjustment (see Table 1).
Demographic Factors as Predictors of Emotional and Behavioral Symptoms
We then examined whether demographic variables, including child age, gender, race/ethnicity, and insurance type were associated with reported symptoms at admission and discharge. Gender, race, and insurance type were transformed into dichotomous variables prior to conducting independent sample t tests. We dichotomized race into white and minority samples given the predominantly white sample (77%). Gender was dichotomized into male and female, and two children who identified as transgender were excluded from analyses. Furthermore, we dichotomized insurance type into commercial/private versus public or state funded insurance.
Results suggested there were significant gender differences in anxiety symptoms at admission (t(282) = −4.63, p< .001) and discharge (t(282) = −3.62, p < 0.001), with females reporting higher symptoms of anxiety at both time points. There were also significant gender differences in depressive symptoms at admission (t(282) = −3.96, p < 0.001) with females reporting higher depressive symptoms compared to males and there were significant differences in emotional symptoms at admission (t(276) = −3.78, p< 0.001) and discharge (t(251) = −3.80, p< 0.001) with females reporting higher emotional symptoms compared to males. Results also suggested significant gender differences for psychological adjustment at admission (t(270) = 2.53, p = 0.012) with females reporting lower psychological adjustment. There were significant differences for insurance type in emotional symptoms at admission (t(279) = 1.98, p= 0.049) where children with private insurance report higher symptoms. Additionally, there were significant differences for insurance type in psychological adjustment at discharge (t(203) = −2.06, p= 0.041) where children with private insurance reported lower scores on the psychological adjustment subscale of the BASC-2 compared to children with state funded insurance. Insurance type was not significantly related to depressive or anxiety symptoms at admission or discharge. Race was not significantly related to depressive symptoms, anxiety, emotional symptoms, or psychological adjustment at admission or discharge. Patient age was not significantly correlated with child reported symptoms of anxiety or depression.
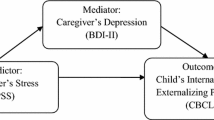
We conducted one-way repeated measures ANOVAs to examine whether demographic variables including gender, age, race/ethnicity, and insurance type predicted change in symptoms over time. Demographic variables were independently entered into the models as predictors. Results indicated that age and race/ethnicity did not significantly predict change in symptoms from admission to discharge. However, insurance type significantly predicted change in depressive symptoms (F(1,285) = 4.77, p = 0.03, ηp2 = 0.02) and emotional symptoms (F(1,250) = 6.11, p = 0.014, ηp2 = 0.02). As shown in Fig. 1, children with private insurance reported significant decrease in depressive symptoms (F(1,171) = 27.15, p < 0.001) in contrast to children with state funded insurance, who did not report significant changes in depressive symptoms (p = 0.095). As shown in Fig. 2, Insurance type also significantly predicted change in child reported emotional symptoms over time where children with private insurance reported greater decreases in emotional symptoms (F(1,154) = 39.15, p< 0.001) compared to children with state funded insurance (F(1,96) = 10.94, p= 0.001). Insurance type did not predict change in anxiety symptoms or child psychological adjustment over time.
Gender also significantly predicted change in depressive symptoms (F(1,285) = 10.39, p = 0.001, ηp2 = .04). As shown in Fig. 3, while males reported significant decreases in depressive symptoms, (F(1,179) = 5.56, p = 0.019), females reported sharper decreases in depressive symptoms (F(1,103) = 25.04, p < 0.001) from admission to discharge. Gender did not predict change in anxiety symptoms, emotional symptoms or child psychological adjustment.
Family Stressors and Supports as Predictors of Symptoms
Simple correlations of family stressors and supports with emotional and behavioral symptoms at admission and discharge were not significant. Likewise, these associations were not significant in partial correlations controlling for insurance type and gender. One-way repeated measures ANOVA was used to examine the effects of family stressors on the child’s symptoms over the course of hospitalization. Results indicated that the number of family stressors in the past month significantly predicted change in symptoms of depression over time (F(1,274) = 6.50, p= 0.011, ηp2 = 0.02). To understand the interaction effect, we split the subjects at the 50th percentile and examined children below the median stress score (no stressors, n = 136) and children at or above the median stress score (one or more stressors, n = 140). As shown in Fig. 4, children in families with no stressors occurring in the past month reported sharper declines in overall depressive symptoms (F(1,136) = 34.27, p< 0.001) compared to children in families with one or more stressors in the past month (F(1,140) = 6.67, p = 0.011). This interaction effect remained significant in sensitivity analyses controlling for insurance type and gender (F(1,272) = 5.67, p = 0.018).
Results also indicated that the number of family stressors in the past month significantly predicted change in emotional symptoms over time (F(1,240) = 4.67, p= 0.031, ηp2 = 0.02). To understand the interaction effect, we examined children with no stressors (n = 136) and children with one or more stressors (n = 140). As demonstrated in Fig. 5, children in families with no stressors occurring in the past month reported sharper decreases in emotional symptoms (F(1,116) = 36.92, p < 0.001) compared to children in families with one or more stressors in the past month (F(1,120) = 12.44, p = 0.001). This interaction effect dropped to trend level in sensitivity analyses controlling for insurance type and gender (p = 0.064). The number of family stressors in the past month did not predict change in anxiety symptoms or psychological adjustment over time, regardless if demographic factors were included in the model.
We also examined whether caregiver support was a predictor of change in emotional and behavioral symptoms during the child’s hospitalization. One-way repeated measures ANOVAs were conducted with and without controlling for insurance type and gender. Given that insurance type and gender were predictive of change of symptoms over time, we conducted ANOVAs with and without controlling for insurance type and gender in order to understand models of stress and support above and beyond these demographic factors. All findings were non-significant, regardless if demographic factors were included in the models suggesting that family support was not a predictor of change in child and reported anxiety symptoms, depressive symptoms, and emotional symptoms, and was not a predictor of change in caregiver reported child psychological adjustment.
Discussion
This study was conducted to evaluate whether participation in a children’s partial hospitalization program was associated with improved emotional and behavioral symptoms for children from admission to discharge, and extends previous literature on CPHPs by examining both demographic and family factors that may moderate these outcomes. Results from the study suggest that the children’s partial hospitalization program is effective in reducing emotional and behavioral difficulties in children with serious mental illness. Furthermore, results suggest family stressors is an important factor to consider and emphasize in treatment.
Consistent with our hypothesis, children reported decreases in symptoms of anxiety, depression, and emotional symptoms from admission to discharge while caregivers reported improved child psychological adjustment. In addition, children with private insurance reported significant decreases in depressive and emotional symptoms compared to children with state funded insurance, who did not report significant changes. Gender also significantly predicted change in depressive symptoms where females reported sharper decreases in depressive symptoms compared to males; however, it did not predict change in anxiety symptoms, emotional symptoms, or child psychological adjustment. One reason for this could be the tendency for gender differences in assessed outcomes, such as internalizing symptoms of anxiety, to appear in early to mid-adolescence rather than in childhood (Zahn-Waxler et al. 2008) In contrast to our hypotheses, age and race did not significantly predict changes in symptoms of anxiety, depression, emotional symptoms, or psychological adjustment.
Results also support the hypothesis that the number of family stressors in the past month predicts change in depressive symptoms. Specifically, we found that children in families with no stressors in the past month reported sharper declines in overall depressive symptoms compared to children in families with one or more stressors in the past month. Results also suggest that children with caregivers who report no stressors in the past month indicate significant improvements in emotional symptoms. In contrast to our hypothesis, results indicate that our measure of family support is not a predictor of change in child reported symptoms and caregiver reported child psychological adjustment.
Results of this study contribute to the literature in several ways. First, the current study expands prior work by evaluating an evidence-based treatment program, including multiple informants and assessments. Second, this study provides additional information regarding demographic factors that might influence treatment outcomes in children with serious mental illness. Existing research on children’s partial hospital programs are limited and even fewer studies have examined moderators of outcomes to determine for who greater therapeutic gains and/or change will likely occur. Third, this study provides support for considering recent family stressors when assessing treatment outcomes for children with serious mental illness. Given that children whose families report minimal stressors demonstrate improved outcomes, identifying families who endorse recent stressors and targeting these stressors early in treatment may be a crucial step. Lastly, we demonstrated the feasibility of integration of clinical measures into a busy treatment service at both admission and discharge. These measures were used for diagnosis and treatment planning, but also served to provide a means of evaluating outcomes to ensure treatment effectiveness.
An area of need for additional focus is on potential treatment disparities. Insurance type altered treatment outcomes, most notably in child reported improvement in depressive and emotional symptoms. Since insurance type is a proxy for SES, it is likely that families with state funded insurance had additional stressors that created barriers to treatment utilization, such as difficulties with transportation and inadequate social supports (Casey et al. 2018; Marcin et al. 2003). Another hypothesis is that children with state funded insurance are more aware of the stressors facing their families and this makes modifying emotional symptoms more challenging. These hypotheses would benefit from further exploration and would certainly point to a need for additional case management aimed at identifying services that target these areas.
Limitations and Directions for Future Research
While study findings are promising and suggest that CPHPs can be effective for treating child psychiatric symptoms, potential limitations merit attention. First, given that the study was conducted in a clinical setting, the sample could not be compared to a control group. Although examining a comparable no-treatment psychiatric population would be difficult due to ethical considerations including precluding treatment for a control group, having the ability to compare the clinical group to a control group would allow for a more robust evaluation of treatment effects. Second, there was a possible impact of study attrition as some families did not complete both admission and discharge assessments; however, for a majority of the families, study attrition was for an expected reason such as transfer to a higher level of care or enrollment in the program for less than two weeks. Third, our study design was generalized in overall treatment effectiveness and did not focus on the effectiveness of individual components of treatment. That is, while children received cognitive-behavioral, behavioral, and family systems interventions in a highly supportive and structured environment, the impact on the extent of the effectiveness and necessity of the individual modalities of treatment and individual treatment effects is limited.
Fourth, the generalizability of the current findings may be limited due to variations in treatment approaches and modalities across different programs, which brings to light a necessity for further research in this area. Although the current sample size is not large enough to warrant an investigation of how different combinations of treatments relate to different outcomes, future research should examine specific aspects of treatments and their relation to social, emotional, and behavioral outcomes given the implications for tailoring programs to maximize efficacy. Additionally, race was not significantly related to depressive symptoms, anxiety, emotional symptoms, or adjustment at admission or discharge; however, differences across race may not have been captured given the small percentage of minorities in this sample. Although our sample resembled the racial and ethnic composition of the state in which participants were recruited, our sample was mostly Caucasian and findings may therefore not be generalizable. Fifth, we only assessed recent stressors (in the past month) for families, which may not capture significant stressors that occurred prior and our measure of support may be limited given its focus on discrete types of support. Future research should examine less recent stressors, identify the perceived rating of this stressor on the caregiver’s overall functioning and parenting, and more accurately assess supports including the quality and perceived utility of identified supports. Additionally, given that participants were split (at the 50th percentile) into two groups to obtain the median stress score, the ‘below the median stress score’ and ‘above the median stress score’ groups could be explored in more detail in future research. Although children were given assessments to complete during their intake, we acknowledged that the outcomes analyzed in this manuscript are based on self-report measures rather than formal diagnostic assessment or observational data. Finally, when assessing family stressors using a self-report 15 item checklist, we acknowledge that only the number of stressors in the past month were assessed. Future research could explore the impact and importance of family stressors in terms of their type and relative significance (e.g., loss of a loved one, parent losing a job, moving, etc.). Despite these limitations, the study does provide preliminary evidence for the efficacy of partial hospital treatment for children with severe mental illness. Given the importance findings that suggest family factors may influence treatment outcomes, future studies might examine additional family factors (e.g., caregiver motivation) that may moderate treatment outcomes.
In conclusion, while child mental health problems are a major public health issues that necessitates effective and efficient treatment approaches, partial hospitalization programs provide a more intensive treatment and results from this study suggest they appear to demonstrate effectiveness in improving child emotional and behavioral symptoms. The current study provided evidence of improvements in child functioning over the course of treatment in a multidisciplinary CPHP and supports the conclusion that factors including insurance type, gender, and family stressors in the past month moderate treatment efficacy. Future research should continue to examine additional moderators of treatment efficacy and impacts on the larger family system.
References
Bennett, D. S., Macri, M. T., Creed, T. A., Isom, J. A. (2001). Predictors of treatment response in a child day treatment program. Residential Treatment for Children & Youth, 19, 59–72.
Birmaher, B., Brent, D. A., Chiappetta, L., Bridge, J., Monga, S., & Baugher, M. (1999). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1230–1236.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., & Neer, S. M. (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 545–553. https://doi.org/10.1097/00004583-199704000-00018.
Boekamp, J. R., Liu, R. T., Martin, S. E., Mernick, L. R., DeMarco, M., & Spirito, A. (2018). Predictors of partial hospital readmission for young children with oppositional defiant disorder. Child Psychiatry and Human Development, 49, 505–511. https://doi.org/10.1007/s10578-017-0770-8.
Canals, J., Hernandez-Martinez, C., Cosi, S., & Domenech, E. (2012). Examination of a cutoff score of the Screen for Child Anxiety Related Emotional Disorders (SCARED) in a non-clinical Spanish population. Journal of Anxiety Disorders, 26, 785–791. https://doi.org/10.1016/j.janxdis.2012.07.008.
Casey, J. A., Pollak, J., Glymour, M. M., Mayeda, E. R., Hirsch, A. G., & Schwartz, B. S. (2018). Measures of SES for electronic health record-based research. American Journal of Preventive Medicine, 54, 430–439. https://doi.org/10.1016/j.amepre.2017.10.004.
Dishion, T. J., Brennan, L. M., Shaw, D. S., McEachern, A. D., Wilson, M. N., & Jo, B. (2014). Prevention of problem behavior through annual Family Check-Ups in early childhood: Intervention effects from home to early elementary school. Journal of Abnormal Child Psychology, 42, 343–354. https://doi.org/10.1007/s10802-013-9768-2.
Dishion, T. J., & Stormshak, E. A. (2007). Intervening in children’s lives: An ecological, family-centered approach to mental health care. Washington, DC: American Psychological Association. https://doi.org/10.1037/11485-000.
Goodman, R. (1997). The Strengths and Difficulties Questionnaire: A Research Note. Journal of Child Psychology and Psychiatry, 38, 581–586.
Goodman, R. (2001). Psychometric properties of the Strengths and Difficulties Questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40(11), 1337–1345.
Goodman, R., Ford, T., Simmons, H., Gatward, R., & Meltzer, H. (2000). Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British Journal of Psychiatry, 177, 534–539.
Granello, D. H., Granello, P. F., & Lee, F. (2000). Measuring treatment outcome in a child and adolescent partial hospitalization program. Administration and Policy in Mental Health, 27, 409–422.
Grizenko, N. (1997). Outcome of multimodal day treatment for children with severe behavior problems: A five-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 989–996.
Grizenko, N., Papineau, D., & Sayegh, L. (1993). A comparison of day treatment and outpatient treatment for children with disruptive behavior problems. Canadian Journal of Psychiatry, 38, 432–435.
Grizenko, N., & Sayegh, L. (1990). Evaluation of the effectiveness of a psychodynamically oriented day treatment program for children with behaviour problems: A pilot study. Canadian Journal of Psychiatry, 35, 519–525.
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381.
Kazdin, A. E., & Whitley, M. K. (2003). Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. Journal of Consulting and Clinical Psychology, 71, 504–515.
Kovacs, M. (1985). The Children’s Depression Inventory (CDI). Psychopharmacology Bulletin, 21, 995–998.
Lenz, A. S., & Del Conte, G. (2018). Efficacy of Dialectical Behavior Therapy for adolescents in a partial hospitalization program. Journal of Counseling and Development, 96, 15–26. https://doi.org/10.1002/jcad.12174.
Mansur, R. B., Cunha, G. R., Asevedo, E., Zugman, A., Zeni-Graiff, M., Rios, A. C., & Brietzke, E. (2016). Socioeconomic disadvantage moderates the association between peripheral biomarkers and childhood psychopathology. PLoS ONE, 11, 1–14. https://doi.org/10.1371/journal.pone.0160455.
Marcin, J. P., Schembri, M. S., He, J., & Romano, P. S. (2003). A population-based analysis of socioeconomic status and insurance status and their relationship with pediatric trauma hospitalization and mortality rates. American Journal of Public Health, 9, 461–466.
Martin, S. E., McConville, D. W., Williamson, L. R., Feldman, G., & Boekamp, J. R. (2013). Partial hospitalization treatment for preschoolers with severe behavior problems: Child age and maternal functioning as predictors of outcome. Child and Adolescent Mental Health, 18, 24–32.
Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., & Swendsen, J. (2010). Lifetime Prevalence of Mental Disorders in US Adolescents: Results from the National Comorbidity Study-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49, 980–989.
Milin, R., Coupland, K., Walker, S., & Fisher-Bloom, E. (2000). Outcome and follow-up study of an adolescent psychiatric day treatment school program. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 320–328. https://doi.org/10.1097/00004583-2000030000-00014.
Muller, J. M., Averbeck-Holocher, M., Romer, G., Furniss, T., Archtergarde, S., & Postert, C. (2015). Psychiatric treatment outcomes of preschool children in a family day hospital. Child Psychiatry and Human Development, 46, 257–269. https://doi.org/10.1007/s10578-014-0465-3.
National Alliance on Mental Illness. Mental Health Facts Children and Teens. Retrieved from http://www.nami.org/NAMI/media/NAMI-Media/Infographics/Children-MH-Facts-NAMI.pdf.
Nilsen, T. S., Eisemann, M., & Kvernmo, S. (2013). Predictors and moderators of outcome in child and adolescent anxiety and depression: a systematic review of psychological treatment studies. European Child & Adolescent Psychiatry, 22, 69–87. https://doi.org/10.1007/s00787-012-0316-3.
O’Neal, C. W., Richardson, E. W., Mancini, J. A., & Grimsley, R. N. (2016). Parents’ early life stressful experiences, their present well-being, and that of their children. American Journal of Orthopsychiatry, 86, 425–435.
Patel, V., Fisher, A. J., Hetrick, S., & McGorry, P. (2007). Mental health of young people: A global public-health challenge. Lancet, 369, 1302–1313.
Perou, R., Bitsko, R. H., Blumberg, S. J., Pastor, P., Ghandour, R. M., Gfroerer, J. C., & Huang, L. N. (2013). Mental health surveillance among children: United States, 2005-2011. Morbidity and Mortality Weekly Report, 62, 1–35 http://www.cdc.gov/mmwr/preview/mmwrhtml/su6202a1.htm Retrieved from.
Reynolds, C. R., & Kamphaus, R. W. (2004). BASC-2: Behavior assessment system for children, second edition manual. Circle Pines, MN: American Guidance Service.
Reynolds, C. R., & Kamphaus, R. W. (2010). BASC-2: Behavior Assessment System for Children Second Edition: Manual Supplement for the Clinical Report. Bloomington, MN: NCS Pearson, Inc.
Smucker, M. R., Craighead, W. E., Craighead, L. W., & Green, B. J. (1986). Normative and reliability data for the Children’s Depression Inventory. Journal of Abnormal Child Psychology, 14, 25–39.
Steele, H., Bate, J., Steele, M., Dube, S. R., Danskin, K., Knafo, H., Nikitiades, A., Bonuck, K., Meissner, P., & Murphy, A. (2016). Adverse childhood experiences, poverty, and parenting stress. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 48, 32.
Webster-Stratton, C. (2005). The incredible years: A trouble-shooting guide for parents of children 2–8 years (2nd ed.). Seattle, WA: Incredible Years.
Webster-Stratton, C., & Reid, M. J. (2010). The Incredible Years parents, teachers and children training series: A multifaceted treatment approach for young children with conduct problems. In J. Weisz & A. Kazdin (Eds), Evidence-based psychotherapies for children and adolescents (194-210). New York: Guilford Publications.
Webster-Stratton, C., Rinaldi, J., & Jamila, M. R. (2011). Long-term outcomes of Incredible Years Parenting Program: Predictors of Adolescent Adjustment. Child and Adolescent Mental Health, 16, 38–46.
Whitson, M. L., & Kaufman, J. S. (2016). Parenting stress as a mediator of trauma exposure and mental health outcomes in young children. American Journal of Orthopsychiatry, 87, 531–539.
Zahn-Waxler, C., Shirtcliff, E. A., & Marceau, K. (2008). Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology, 4, 275–303. https://doi.org/10.1146/annurev.clinpsy.3.022806.091358.
Acknowledgements
We are grateful to the children and families who have participated in our program. We would also like to thank the clinical team for their dedication and service to our patients.
Funding
This study was conducted without external grant funding.
Author Contributions
MY: developed research question, created database, conducted data analyses, wrote the paper. TP: collaborated with the design, writing, and data analysis of the study. KM: assisted with the creation of the database, assisted with data collection for record review, reviewed and provided feedback on manuscript and revisions. SP: assisted with the database, assisted with conducting data analyses, provided edits on the manuscript and revisions SU: assisted with literature review, assisted with analysis and interpretation of data associated with measures. AW: collaborated with the design of the study, provided edits on the manuscript and revisions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or national research committee through Lifespan- Rhode Island Hospital IRB, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yaptangco, M., Preddy, T.M., Musella, K.E. et al. Family Stress Moderates Emotional and Behavioral Symptoms in a Child Partial Hospital Setting. J Child Fam Stud 28, 2762–2771 (2019). https://doi.org/10.1007/s10826-019-01456-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-019-01456-y