Abstract
Objectives
This study examined the relative contribution of parental Attention-Deficit/Hyperactivity Disorder (ADHD) and depression symptoms to the parenting stress of mothers and fathers of adolescents with ADHD.
Methods
The sample comprised 83 families with adolescents 13 to 18-years of age (48 with ADHD, 35 without ADHD). Parents provided ratings of parenting stress and their own ADHD and depression symptoms by completing standardized self-report rating scales. Two domains of parenting stress were investigated: Stress in relation to adolescent behaviors and parent-adolescent relationships (Adolescent-Focused Stress domain; AFS), and stress involving the impact of the adolescent on parental roles, relationships with others and sense of competence (Parent-Focused Stress domain; PFS).
Results
In addition to adolescent ADHD status, mothers’ ADHD and depression symptoms were predictors of maternal AFS (R2 = 0.51, F = 24.50, p < 0.001). Only maternal depression predicted mothers’ PFS (R2 = 0.37, F = 12.11, p < 0.001). Paternal AFS was predicted by adolescent ADHD status (R2 = 0.25, F=4.81, p < 0.01). Paternal PFS was predicted by fathers’ depression symptoms and by mothers’ ADHD symptoms (R2 = 0.30, F = 4.42, p < 0.01).
Conclusions
These findings suggest that mothers’ and fathers’ parenting stress is associated with their adolescent children’s ADHD symptoms and their own depression symptoms. Mothers’ ADHD symptoms are also associated with their own AFS and fathers’ parenting stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Parenthood, viewed by many parents as being their most important role, ranking ahead of their careers and marriage (Aassve et al. 2012; Nelson et al. 2013), demands time, energy, and economic and emotional resources (Ballas and Dorling 2007). Most parents therefore experience parenting stress (Crnic and Greenberg 1990), which is defined as an aversive experience where the demands of parenting are perceived to exceed the physical, economic, and emotional resources available to manage or meet these demands (Deater-Deckard 2004). Having some degree of parenting stress is normal but when parents experience high levels of parenting stress, they are often less effective in their role as parents and less able to implement parenting interventions (e.g., Kazdin 1995; Mash and Johnston 1990). Family support in the form of high levels of consistent and warm parenting and low levels of coercive parenting is associated with adolescent wellbeing (e.g., Lila et al. 2006). Although adolescents are typically more autonomous in terms of decision-making and spend more time with peers than younger children (e.g., Goossens 2006), parents of adolescents continue to experience parenting stress (Putnick et al. 2010) and their parenting stress is negatively associated with positive parenting and adolescent self-esteem (Putnick et al. 2008). It is therefore important to acquire an understanding of predictors of parenting stress in parents of adolescents. In the current study, we examine the extent to which adolescent attention-deficit hyperactivity disorder (ADHD), and parental ADHD and depression symptoms predict mothers’ and fathers’ parenting stress in parents of adolescents with and without ADHD.
Research on parenting stress in parents of children with ADHD has typically been based on Abidin’s (1995) theory of parenting stress (Theule et al. 2013). In accordance with this theory, research has examined stress in relation to characteristics of the child or adolescent (e.g., moodiness, social isolation and withdrawal, failure to achieve, externalizing behavior), stress occurring because of dysfunctional parent-child interactions (e.g., low levels of warmth and high levels of conflict), and stress occurring because of their role as a parent (e.g., life restrictions, relationship with spouse, feelings of incompetence, and social alienation). In a meta-analysis conducted by Theule et al. (2013), mothers and fathers of children with ADHD (none of the studies included child participants older than 12 years of age) were found to experience more parenting stress in all domains than parents of children without ADHD. Effect sizes were large. Parenting stress was predicted by child factors including child inattentive and hyperactive-impulsive symptoms, and child internalizing and externalizing behaviors. Low levels of social support and marital quality were associated with increased parenting stress.
Since the meta-analysis conducted by Theule et al. (2013) was completed, two published studies have investigated parenting stress in parents of adolescents with ADHD. Participants in the Gordon and Hinshaw (2017) longitudinal study were mothers of girls (ages 6 to 12) who were followed for five years, and participants in the Wiener et al. (2016) study were mothers and fathers of male and female adolescents (ages 13 to 17). Both studies included adolescents with ADHD and a typically developing comparison group. The findings from both studies showed that, in comparison with mothers of typically developing adolescents, mothers of adolescents with ADHD experienced higher levels of parenting stress in relation to their adolescent children’s behavior, the quality of the relationship with their children, and their role as a parent. Wiener et al. also found that fathers of adolescents with ADHD experienced higher levels of parenting stress in relation to their children’s behavior and relationships with their children, but did not report higher levels of stress with regard to their role as a parent. Gordon and Hinshaw found that parenting stress due to dysfunctional interactions when the adolescents were children predicted internalizing behaviors in adolescents with ADHD. Wiener et al. found that parenting stress in parents of adolescents with ADHD was predicted by adolescent parent-rated, but not teacher-rated oppositional behaviors.
Although parenting theories have postulated several mechanisms contributing to parenting stress including parents’ cognitive appraisals or attributions for their children’s characteristics and behaviors (Mash and Johnston 1990), extra-familial factors such as low socioeconomic status, and interpersonal factors such as marital distress (e.g., Webster-Stratton 1990), these mechanisms have not been examined in relation to parenting stress in parents of adolescents with ADHD. These theories, however, suggest that, in addition to adolescent characteristics, parent characteristics such as their ADHD and depression symptoms may contribute to their parenting stress. Parental psychopathology, which occurs more frequently in parents of children with ADHD compared with comparison families, exacerbates parenting stress (Fischer 1990; Theule et al. 2013). Psychopathology is thought to increase vulnerability to life stressors because it may reduce access to coping skills that are necessary for decreasing stress levels (Webster-Stratton 1990).
Approximately 30 to 70 percent of children with ADHD continue to show symptoms in adulthood (Barkley et al. 2002) and 40 to 60 percent of parents with ADHD also have a child with ADHD (Minde et al. 2003). ADHD in adulthood has also been linked with impairment across many domains and, most significantly, in the areas of educational attainment and success, social functioning, and employment (Barkley et al. 2008; Kessler et al. 2006; Mannuzza et al. 2011). Adults with ADHD are at an increased risk for comorbid psychiatric disorders, including depression, anxiety, substance abuse, and antisocial behavior (Barkley et al. 2008; Barkley 2015). Furthermore, a significant number of adults are untreated for ADHD and are more likely to access mental health services because of comorbid problems (Fayyad et al. 2007). Given the high heritability of ADHD, it is not surprising that approximately 40 to 60 percent of children with ADHD have one or more parents with the disorder or high levels of self-reported ADHD symptomatology (see Johnston et al. 2012 for review).
Johnston et al. (2012) proposed that the relationship between parental ADHD symptoms and parenting practices is mediated by parental cognitions including parenting self-efficacy and parenting stress. Supporting the Johnston et al. model, maternal ADHD has been found to be associated with maternal parenting stress (Theule et al. 2011; Wiener et al. 2016). Furthermore, mothers with ADHD who had challenges with emotion regulation experienced distress when their teens expressed negative emotions, which was associated with harsh responses that were not sensitive to their children’s needs (Mazursky-Horowitz et al. 2015). These findings suggest that the association between parenting stress and maternal ADHD may be related to problems with emotion regulation, which is also a symptom of depression. Although fathers of adolescents with ADHD reported higher levels of parenting stress than fathers of typically developing adolescents in terms of stress associated with their children’s behavior and the quality of the adolescent-parent relationship, they did not differ from comparison fathers in the amount of stress they experienced in their role as parents (Wiener et al. 2016). Furthermore, their self-reported ADHD symptoms were not associated with parenting stress. This research suggests that the level of parenting stress experienced by mothers and fathers of adolescents with ADHD may be differentially impacted by their own ADHD symptoms, possibly due to their different roles in the family. The division of childcare responsibilities may also interact with parental ADHD symptomatology. As mothers tend to take on more parenting responsibilities (Phares et al. 2009) and spend more time interacting with their children even within dual-income families (Bianchi and Raley 2005; Coltrane 2000), their effectiveness in the parenting role may be more likely to be impacted by their ADHD symptoms. Fathers with ADHD, however, may be less burdened by childcare demands; consequently, their ADHD symptoms may not significantly impact their parenting stress. Thus, parental ADHD symptomatology may differentially impact maternal and paternal stress levels.
Previous research has not examined whether ADHD symptoms or diagnosis in one parent is associated with increased parenting stress in the co-parent. Adults with ADHD, however, typically have lower levels of marital satisfaction and are more likely to be separated or divorced than other adults, and men’s anti-social behavior is a strong predictor of marriage dissolution (Wymbs et al. 2008). Furthermore, males without ADHD reported that their partners’ ADHD behaviors had a more negative impact on them did females without ADHD in relation to their partners with ADHD (Robin and Payson 2002). It is therefore likely that the co-parent of parents who have high levels of ADHD symptomatology may experience high levels of parenting stress, and that this might be especially true for fathers.
Within the general population, 1 in 5 women and 1 in 10 men suffer from a depressive episode over the course of their lifetime (Goodman and Gotlib 2002). Among adults with ADHD, co-occurring depression is higher, with rates varying according to the age of the adult, and whether the sample is a community sample or clinic referred (Barkley et al. 2008; Barkley 2015). Co-occurring ADHD and depression in adults is associated with higher levels of impairment (Barkley et al. 2008). Furthermore, women with ADHD are more impacted by negative life events (Garcia et al. 2012) and report more depressive and anxious symptoms than their male counterparts (Wilens et al. 2009). Parents who experience higher levels of depression symptoms are more likely to have difficulties in their marital relationships and display a heightened risk for having children with behavior problems (Cummings et al. 2005). Parental depression is associated with problematic parenting practices among parents of both genders in families of typically developing children and adolescents (e.g., low warmth, greater disengagement, irritability, physical and emotional unavailability, negative or sad affect; see Oyserman et al. 2000 for review).
Maternal depression symptoms have been consistently associated with increased parenting stress among mothers of children with and without ADHD (e.g., Thomason et al. 2014; Theule et al. 2013; van der Oord et al. 2006); however, the relationship between maternal and paternal depression symptoms and parenting stress among parents of adolescents with ADHD is yet to be examined. Cognitive theories (e.g., Beck 2008) suggest that maladaptive cognitions and behavioral avoidance are implicated in depression, and this is the case in adults with ADHD (Knouse et al. 2013). These maladaptive cognitions may include having negative attributions for the challenging behaviors of adolescents with ADHD, which may lead parents to interpret them as more stressful than might parents who are not depressed. In accordance with diathesis-stress theory (e.g., Belsky and Pluess 2009) the impairment associated with parental ADHD might also be seen as a diathesis that predisposes them to higher levels of depression in response to stressors such as their children’s behavior.
The extent to which depression in one parent is associated with parenting stress in the other has not been examined in relation to parents of children and adolescents with ADHD. Individuals living with a depressed partner, however, reported more depressed mood than would be expected in the general population (Benazon and Coyne 2000). Although the direction of causality between depression and marital strain is difficult to ascertain, some findings suggest that depression may precede marital problems and may lead to dysfunctional interactions that later produce conflict (Coyne and Benazon 2001). In addition to increased dysfunction and strain between co-parents, the presence of maternal or paternal depression symptoms may have an additive effect on adolescent ADHD and externalizing disorders including conduct disorder, oppositional-defiant disorder, and substance abuse (Brennan et al. 2002). Given the challenges with parenting faced by adults with ADHD (Johnston et al. 2012) and adults who have a depressive disorder (Gerdes et al. 2007; Goodman et al. 2011), and the high comorbidity of ADHD and depression in adults with ADHD (Barkley 2015; Barkley et al. 2008), this study will examine whether maternal and paternal depression symptoms are associated with their own parenting stress and the parenting stress of their co-parent.
In sum, previous research has separately examined the link between parental depression symptoms and parenting stress, and parental ADHD symptoms and parenting stress; however, in spite of the high comorbidity rates between ADHD and depression in adults, the combined contribution of parental ADHD and depression symptoms in predicting parenting stress, and the association between parental ADHD and depression in one parent and the parenting stress in the co-parent have not been investigated. Acquiring an understanding of the extent to which ADHD versus depression symptoms in mothers and fathers of adolescents with ADHD predict their parenting stress may be helpful in identifying risk factors for ineffective parenting in parents of these teens.
This study was guided by two objectives. The first objective was to investigate the relative contribution of parental ADHD and depression symptoms to parenting stress in mothers and fathers of adolescents with and without ADHD. Two aspects of parenting stress were examined: Stress in relation to adolescent challenging behaviors and their relationships with their parents (Adolescent-Focused Stress; AFS), and stress involving the impact of the adolescent on parental roles, relationships with others and sense of competence (Parent-Focused Stress; PFS). With regard to mothers, on the basis of previous research with children and adolescents with ADHD, it was predicted that both maternal ADHD symptoms (Theule et al. 2011; Wiener et al. 2016) and maternal depression symptoms (Theule et al. 2013) would be associated with higher levels of AFS and PFS. Previous research with fathers of adolescents with ADHD suggests that their parenting stress would be predicted by their children’s ADHD but not their own ADHD symptoms (Wiener et al. 2016). Given the association of depression and parenting stress in parents of children with ADHD (Theule et al. 2013), it was predicted that fathers’ depression symptoms would predict their parenting stress. The second objective was to explore whether ADHD and depression symptoms in one parent is associated with increased parenting stress of a co-parent within intact families. Because of the higher levels of marital discord in families when a parent has ADHD (Wymbs et al. 2008), and a study showing that fathers experience negative impact when their co-parent has ADHD (Robin and Payson 2002), it was predicted that fathers’ PFS would be positively associated with their co-parents’ ADHD symptoms and impairment. On the basis of previous research indicating that depression in one co-parent is associated with increased strain in the other (Benazon and Coyne 2000), it was predicted that depression symptoms in one parent would be associated with increased PFS in the other.
Method
Participants
Participants were 83 13 to 18-year old adolescents (48 previously diagnosed with ADHD, 35 without ADHD) and their parents. Participants with ADHD were recruited through flyers sent to physicians and children’s mental health centers. Adolescents in the comparison sample were recruited through advertisements placed in local newspapers, community centers and libraries. Some participants of previous studies who had agreed to be contacted for future studies in the ADHD lab at the University of Toronto also participated.
The presence of ongoing ADHD symptoms was confirmed using the Conners Rating Scales—Third Edition (Conners 2008). Two methods were used to classify adolescents as having ADHD: 1) participants were required to have a rating in the clinical range (T ≥ 70) on the Conners-3 Parent DSM-IV Inattentive or Hyperactive-Impulsive scales (n = 38); or 2) participants were required to have at least one parent rating in the borderline range (T = 65–69) and at least one borderline or clinical range (T ≥ 65) rating from a second informant (self-report n = 2 or teacher-report, n = 8). Adolescents were included in the typically functioning comparison group in two ways: 1) participants were required to have parent ratings in the average range (T ≤ 60) (n = 21); or 2) participants were required to have all T-scores below 65 according to both parent- and teacher-report (n = 14). Adolescents with Autism Spectrum Disorders, Intellectual Disabilities, and Bipolar Disorder diagnoses as reported by parents were excluded from the study. However, due to high comorbidity rates with ADHD (Pliszka 2015), adolescents who had previously diagnosed learning disabilities, conduct disorder, oppositional defiant disorder, anxiety, or depression according to parent report were included.
Adolescents with and without ADHD did not differ in age or IQ (Table 1) and did not differ in gender (ADHD: 32 boys, 16 girls; comparison: 16 boys, 19 girls; χ² (1, N = 83) = 3.64, p = 0.056). Parents reported that 72.9% (n = 35) of adolescents with ADHD were taking medication to manage their ADHD symptoms. They also reported that 66.7% (n = 32) of adolescents with ADHD had one or more previous comorbid diagnoses (i.e., learning disability, n = 28; anxiety, n = 5; depression, n = 2; oppositional defiant disorder, n = 1). Three adolescents without ADHD had a diagnosis of a learning disability and one adolescent had a diagnosis of oppositional defiant disorder. Adolescents with ADHD had higher scores on the ODD and CD scales on the Conners Rating Scales as reported by both parents and teachers.
The parent sample comprised 74 mothers and 56 fathers. Of the 83 adolescent participants, 56.6% (n = 47) had parenting stress and parental psychopathology ratings provided from both parents. Among parents of adolescents with ADHD, 60.4% (n = 29) provided ratings from both parents, 31.3% (n = 15) provided only mother ratings, and 8.3% (n = 4) provided only father ratings. Within the comparison group, 51.4% (n = 18) provided ratings from both parents and 34.3% (n = 12) provided only mother ratings, and 14.3% (n = 5) provided only father ratings. As shown in Table 1, parents of adolescents with and without ADHD did not differ in age and socio-economic status as measured by highest level of attained education. The majority of parents were married or in common-law relationships (ADHD: 75.0%, n = 36; Comparison: 85.7%, n = 30) and parents of adolescents with and without ADHD did not differ with regard to the proportion of intact families (χ² (1, N = 83) = 1.43, p = 0.23). Families of adolescents with and without ADHD also did not differ with regard to whether English was the primary language spoken in the home (ADHD: 86.7%, n = 39; Comparison: 81.5%, n = 22; χ² (1, N = 72) = 0.35, p = 0.55).The remaining families reported that the primary language of the household was Chinese (n = 9), French (n = 2), Spanish (n = 2), or other (n = 9).
Procedure
This study was approved by the Research Ethics Board of the University of Toronto. Doctoral students in school and clinical child psychology tested the adolescent participants for a period of approximately 5 h (including administering measures for other studies). Prior to the testing session, parent and adolescent consent were obtained and parents (primarily mothers) of adolescents completed the Conners-3- Parent (Conners 2008). If adolescents met criteria for inclusion in the ADHD or comparison group, both mothers and fathers were sent links to complete the other questionnaires electronically. Parents were asked to provide a link to an electronic version of the Conners-3 – Teacher to a teacher whom they felt could best comment on their children’s current level of ADHD symptoms. Adolescent participants received $30 or a certificate for community service hours required for secondary school graduation. A psychoeducational report summarizing the results of academic and behavioral tests was sent to the families.
Measures
The Stress Index for Parents of Adolescents (SIPA; Sheras et al. 1998) is a 112-item screening and diagnostic measure that assesses parenting stress in parents of adolescents ages 11–19 years across three domains (Adolescent, Parent, Adolescent-Parent Relationship). The Adolescent domain measures parenting stress as a function of the characteristics of the adolescent (i.e., moodiness/emotional lability, social isolation/withdrawal, delinquency/antisocial, failure to achieve or persevere). The Parent domain measures parenting stress as a function of the effect of parenting on parents’ other life roles (i.e., life restrictions, relationship with spouse/partner, social alienation, incompetence/guilt). The Adolescent-Parent Relationship domain measures the perceived quality of the relationship parents have with their children (e.g., degree of communication, amount of affection). Items are rated on a 5-point Likert scale ranging from 1 (Strongly Disagree) to 5 (Strongly Agree). As reported by Sheras et al. (1998), the SIPA is a reliable measure in terms of internal consistency and test-test reliability. The internal consistency of the SIPA domains in the current sample, as measured by Cronbach alpha, was high ranging between 0.89 and 0.95.
For the purpose of this study, an Adolescent-Focused Stress (AFS) score was created to provide an overall measure of parenting stress attributed to adolescent attributes and behaviors (Adolescent domain) and stress related to parent-adolescent interactions (Adolescent-Parent Relationship domain). This combined scale was created because correlations between the Adolescent and Adolescent-Parent Relationship domain scores within this sample were high (Mothers: r = 0.72, p = 0.000; Fathers: r = 0.65, p = 0.000) and the internal consistency of the AFS scale in the current sample, as measured by Cronbach alpha, was also high (Mothers: α = 0.96; Fathers: α = 0.95). Parent domain stress (PFS) was maintained as a separate measure of parenting stress as it uniquely captures stress pertaining to the role of parenthood and the life restrictions, relationship and social challenges, and negative self-concepts that may be associated with this role. The internal consistency of the PFS scale in the current sample was high (Mothers: α = 0.94; Fathers: α = 0.91). Because correlations between maternal AFS and PFS scores were moderate (Mothers: r= 0.46, p = 0.000; Fathers: r = 0.78, p = 0.000), it was important to examine predictors of AFS and PFS in a separate set of analyses.
The Conners Adult ADHD Self-Report Rating Scale- Short Version (CAARS-S:SV; Conners et al. 1999) was used to screen parents for the core symptoms of ADHD. The CAARS-S:SV is a 30-item measure that contains subscales that are most directly relevant to ADHD diagnosis: DSM-IV inattentive symptoms, DSM-IV hyperactive-impulsive symptoms, DSM-IV Total ADHD symptoms, and ADHD Index. Each symptom is rated on a 4-point scale, ranging from 0 (Not at all true/Never) to 3 (Very Much/Very Frequently). All subscales have been reported to have internal reliability of 0.80 or higher (Conners et al. 1999). In terms of its validity, the CAARS-S: SV produces an overall correct classification rate of 85% for adults with ADHD and strongly correlates with other measures of adult ADHD (Erhardt et al. 1999). In this study, we use the ADHD Index score as our measure of maternal and paternal ADHD symptoms because in addition to ADHD symptoms, the CAARS ADHD Index scale includes items that pertain to the impairment that is associated with ADHD including performance or achievement (e.g., I am an underachiever), self-confidence (My past failures make it hard for me to believe in myself), and social functioning (e.g., I intrude on others’ activities, I have a short fuse/hot temper). In previous research, the CAARS-S:SV ADHD Index was found to have a sensitivity of 0.92 in detecting ADHD in adults and demonstrated strong sensitivity for identifying adults at risk for ADHD (Hines et al. 2012). The internal consistency of the CAARS-S:SV ADHD Index in the current sample, as measured by Cronbach alpha, was adequate for both mothers (0.85) and fathers (0.64).
The Beck Depression Inventory-II (BDI-II; Beck et al. 1996) was used to screen mothers and fathers for depression symptoms. This 21-item self-report questionnaire measures mood, sense of failure, self-satisfaction, guilt, irritability, social withdrawal, body image, punishment, and crying during the past 2 weeks. Symptoms are rated on a 4-point Likert scale ranging from 0 (Never) to 3 (Always). The BDI-II has demonstrated excellent construct validity and test-retest reliability. The BDI-II was also found to demonstrate good convergent and discriminate validity when correlated with measures of depression and anxiety. Similar to the normative sample, the internal consistency of the Total symptom score for the current sample, as measured by Cronbach alpha, was high (Mothers = 0.91, Fathers = 0.83).
The Conners-3 rating scales (Conners 2008; Parent, Teacher, and Self-Report forms) were used to determine whether ADHD symptoms were current in the sampled adolescents. Parents, teachers, and adolescents provided ratings on a 4-point scale ranging from 0 (Not at all/Seldom, Never) to 3 (Very Much True/ Very Often, Very Frequent) to evaluate inattention, hyperactivity, oppositional and aggressive behavior, conduct problems and problems related to peer relations. Two DSM-IV ADHD subscales were used to confirm the ADHD diagnosis and to measure the severity of ADHD symptomology (DSM-IV Inattentive, DSM-IV Hyperactive- Impulsive). In the current sample, these scales demonstrated high internal consistency as measured by Cronbach alpha (Parent: 0.95, 0.95; Teacher: 0.93, 0.94; Adolescent: 0.86, 0.80).
The Wechsler Abbreviated Scale of Intelligence (WASI; Vocabulary and Matrix Reasoning subtests, Wechsler 1999), a standardized abbreviated test of intelligence was administered to obtain an estimate of adolescents’ cognitive functioning and to confirm an IQ of at least 80. These subtests have strong Internal consistency (0.93) and test-retest reliability (ranging from 0.88 to 0.93) are high.
The demographics questionnaire consisted of questions pertaining to the adolescents’ developmental, educational, and health history and parents’ health history, education, and employment status. One parent in each household completed the questionnaire at intake.
Data analysis
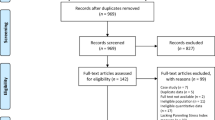
Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 24. Outliers were identified by examining descriptive statistics and creating boxplots of the variables of interest and the distributions of the variables were tested by the Shapiro-Wilk test of normality. Thirteen separate outlier values were identified on ratings of parenting stress, parental ADHD, and depression; significant outlier values were replaced with the most extreme upper value in the range of valid values. A consistent pattern of missing data occurred among single, separated, and divorced parents who did not provide responses to PFS items that assume that the parent has a co-parent. This precluded the calculation of the PFS score for 8 mothers (5 ADHD, 3 Comparison).
Two-tailed t-tests were used to compare adolescents with and without ADHD in their levels of ADHD, ODD and CD symptoms on the Conners-3, and parents of adolescents with and without ADHD on the ADHD Index of the CAARS-S:SV, total symptom score on the BDI-II, and AFS and PFS scores on the SIPA. Analysis of covariance comparing parents of adolescents with and without ADHD in all domains of parenting stress revealed that adolescent gender was not a significant covariate for mothers (AFS: F (1, 71) = 0.06, p = 0.81; PFS: F(1, 63) = 0.12, p = 0.73) or fathers (AFS: F(1, 53) = 0.26, p = 0.61; PFS: F(1, 53) = 0.83, p = 0.37). In addition, socio-economic status, as measured by parent education did not correlate significantly with AFS (Mothers: r = −0.14, p= 0.20; Fathers: r = 0.06, p = 0.65) or PFS (Mothers: r = −0.11, p = 0.40; Fathers: r = −0.21, p = 0.13). Consequently, adolescent gender and SES were not included in the analyses reported below.
Pearson product-moment correlations were calculated between maternal and paternal AFS and PFS and the CAARS ADHD Index and BDI scores. Four step-wise multiple regression analyses were conducted to predict AFS and PFS for mothers and fathers. Adolescent ADHD status was included as a predictor in all of these regressions. Variables that correlated (p < 0.05) with AFS or PFS were added in the relevant analyses. For analyses predicting maternal AFS and PFS, and paternal PFS, their self-reported ADHD as measured by the CAARS ADHD Index and their self-reported depression symptoms as measured on the BDI-II were entered. In addition, fathers’ self-reported ADHD Index scores were entered in the regression predicting maternal PFS, and mothers’ self-reported ADHD Index scores were entered in the regression predicting paternal PFS. As fathers’ self-reported ADHD Index and depression scores were not correlated with paternal AFS, and mothers’ self-reported ADHD Index and depression scores were correlated with paternal AFS, mothers’ scores were entered in the analyses predicting paternal AFS. Analyses predicting PFS were only done with intact families.
Results
Mothers (d = 1.36) and fathers (d = 0.68) of adolescents with ADHD reported higher AFS than parents of adolescents without ADHD. There were no significant differences in PFS (Mothers: d = 0.45; Fathers: d = 0.00). Mothers of adolescents with ADHD reported higher ADHD Index scores than mothers of adolescents without ADHD (d = 0.57). Fathers of adolescents with and without ADHD, however, did not differ in their ADHD Index score (d = 0.30). Mothers (d = 0.20) and fathers (d = 0.35) of adolescents with and without ADHD did not differ with regard to self-reported depression symptoms (Table 1).
As shown in Table 2, mothers’ self-reported ADHD Index scores and depression symptoms were positively correlated with maternal AFS and PFS. Mothers’ self-reported ADHD Index scores and depression symptoms were positively correlated with paternal AFS. Fathers’ self-reported ADHD Index scores and depression symptoms, and mothers’ self-reported ADHD Index scores were positively correlated with paternal PFS. The correlations between maternal and paternal AFS were high and between maternal and paternal PFS were moderate. ADHD Index and depression symptoms were also correlated with each other (Mothers: r = 0.51, p = 0.000; Fathers: r = 0.28, p = 0.04).
As shown in the step-wise regressions reported in Table 3, adolescent ADHD status, maternal ADHD Index and maternal depression symptoms all significantly predicted maternal AFS, accounting for 51.2% of the variance. Although maternal ADHD Index scores were correlated with maternal PFS, only maternal depression symptoms was a significant predictor, accounting for 37.0% of the variance. Adolescent ADHD status, and maternal depression symptoms were significant predictors of paternal AFS, accounting for 25.1% of the variance. Paternal depression symptoms and maternal ADHD Index were significant predictors of paternal PFS, accounting for 29.6% of the variance.
Discussion
The overall purpose of the current study was to examine the contribution of parental ADHD and depression to the parenting stress of parents of adolescents with and without ADHD. Consistent with previous studies, mothers and fathers of adolescents with ADHD reported higher AFS than mothers of adolescents without ADHD (Gordon and Hinshaw 2017; Wiener et al. 2016). In addition to adolescent ADHD status, both parental ADHD and depression were important predictors of parenting stress; however, the findings differed for mothers and fathers and varied by domain of parenting stress. There was also some evidence that, in families where both mothers and fathers participated in the study, parenting stress was increased when the co-parent reported ADHD symptoms and impairment and/or depression.
Maternal parenting stress
Adolescent ADHD status, mothers’ self-reports of ADHD symptoms and impairment, and depression symptoms independently and jointly contribute to mothers’ AFS, explaining over 50% of the variance. This indicates that the distress mothers experience in response to their adolescent children’s behavior and the quality of their relationship with their children is exacerbated by their own symptoms of ADHD and depression. In the PFS domain, however, only maternal depression predicted parenting stress, with Adolescent ADHD status and mothers’ reports of their ADHD symptoms and impairment not contributing to the variance in models including maternal depression. Although fathers’ depression was also correlated with maternal stress in the PFS domain, it did not account for a significant portion of the variance when mothers’ depression symptoms were considered.
Consistent with previous research (Theule et al. 2011; Wiener et al. 2016), findings from the current study indicate that maternal parenting stress is exacerbated when the mother reports significant ADHD symptoms and impairment. As discussed by Johnston et al. (2012), deficits in executive functions and self-regulation of emotion that are common in adults with ADHD may interfere with effective parenting behaviors. Among other things, effective parenting requires the ability to monitor child and adolescent behavior while simultaneously focusing on personal, family, and household responsibilities (e.g., Dishion et al. 2003; Kazdin and Nock 2003), inhibition of immediate reactions such as the urge to react negatively to adolescent provocation (Mazursky-Horowitz et al. 2015), and positive communication to facilitate thoughtful problem solving (Johnston et al. 2012; Harvey et al. 2003). These parenting skills may be impacted by the executive functioning problems of mothers with ADHD (Johnston et al. 2012; Mazursky-Horowitz et al. 2018). Furthermore, as suggested by Johnston et al. (2012), the relationship between parental ADHD and parenting behaviors may be indirect and transactional in that problems with the executive functions that are helpful for effective parenting increase parenting stress, which is then associated with less effective parenting behaviors, parent-adolescent conflict, and higher levels of parenting stress.
During the transition to adolescence, parents tend to spend less time with children because of reduced childcare needs and adolescent striving for autonomy (Goossens 2006; Phares et al. 2009). Consequently, monitoring adolescent behavior may be more challenging than monitoring the behavior of younger children. In addition, inadequate parental monitoring is a predictor of adolescent externalizing behavior and deviant peer affiliation (Barkley et al. 2004; Jokela et al. 2009), which are associated with increased parenting stress in parents of adolescents with ADHD (Wiener et al. 2016). Compared to fathers, mothers tend to take on more parenting responsibilities (Phares et al. 2009) and spend more time interacting with their children (Bianchi and Raley 2005; Coltrane 2000); as a result, their parenting stress may be more likely to be impacted by their ADHD symptoms and impairment.
Consistent with previous research on maternal depression and parenting stress of parents of children with ADHD (Theule et al. 2013), the results of this study indicate that maternal depression symptoms are associated with their parenting stress in both the AFS and PFS domains. Mothers who exhibit symptoms of depression may be less tolerant of or may perceive adolescent ADHD symptoms and problem behaviors as more distressing than unaffected mothers. As depression symptoms include low mood, decreased interest or pleasure, fatigue, diminished concentration, indecisiveness, and feelings of guilt or worthlessness (American Psychiatric Association 2013), it is not surprising that the presence of these symptoms may diminish a mother’s motivation, capacity, and enjoyment of her role as a parent, including her ability to have a warm and close relationship with her children and co-parent, and to access support and cultivate relationships with extended family and friends. In addition, and in combination with ADHD symptoms, the concentration and attention difficulties, low motivation, and fatigue associated with depression may further impair a mother’s capacity to monitor her adolescent’s activities and whereabouts.
Mothers’ stress in the PFS domain was correlated with elevations in their co-parent’s ADHD symptoms and impairment, but paternal ADHD Index did not predict PFS when mothers’ depression was considered. It is possible that that the degree to which mothers can rely on their co-parent for assistance in parenting duties may be limited by the fathers’ challenges with executive functioning, but this may only be stressful when the mother is experiencing depression symptoms. As discussed by Wiener et al. (2016), fathers with ADHD may not substantially contribute to the functioning of the household and parenting, thereby increasing mothers’ caregiver burden. As a result, mothers whose co-parents have ADHD may experience more life restrictions, social alienation, feelings of incompetence and guilt, and conflict and strain in their marital relationship.
Paternal parenting stress
Consistent with Wiener et al. (2016), adolescent ADHD status in the current study was associated with paternal AFS. Fathers’ parenting stress in the Wiener et al. study was also associated with their children’s oppositional behavior, which was not examined in the current study. Although fathers’ reports of their own ADHD and depression symptoms were not associated with increased AFS, it is noteworthy that fathers also reported more AFS when their co-parents had higher levels of ADHD symptoms and impairment. This suggests that fathers experience more distress in response to their children’s behavior and the quality of their relationship with their children when they view other family members (i.e., their children and co-parents) as having challenges. It is possible that fathers experience increased parenting stress because mothers who have high levels of ADHD symptoms may be less engaged in parenting and less effective in monitoring and managing the problem behaviors associated with adolescent ADHD. Previous research has shown that mothers tend to take on more parenting responsibilities and spend more time interacting with children than fathers even within dual-income families (Bianchi and Raley 2005; Coltrane 2000); however, it is possible that this division of responsibilities may shift when mothers have elevated ADHD symptoms and impairment. Mothers’ depression was also correlated with fathers’ AFS. It is unclear whether this stress is due to the additive effect of maternal depression on increasing adolescent externalizing behavior (Brennan et al. 2002) or due to increased caregiver burden among the co-parents of mothers with depression. Although these findings are exploratory, they provide a window into the possible familial and parent-child dynamics that occur within a home where both the adolescent and one or both parents exhibit ADHD and/or depressive symptomatology.
Fathers’ PFS was correlated with their self-reported ADHD and depression symptoms; their ADHD symptoms, however, did not contribute significantly to the variance in PFS when both fathers’ ADHD and depression symptoms were in the equation. Although the directionality of the relationship is not clear, these findings suggests that fathers who experience depression might feel incompetent as parents and unsupported in the parenting role. Paternal PFS was also associated with their co-parents’ ADHD symptoms and impairment. It is possible, as suggested by Robin and Payson (2002), that fathers experience higher levels of PFS when they are required to and take on more parenting duties when their co-parent is impaired by ADHD symptoms. The presence of maternal ADHD may thus limit the degree to which fathers can rely on their co-parent for assistance in parenting duties and as a result, they experience increased life restrictions, social alienation, feelings of incompetence and guilt, and conflict and strain in their marital relationship.
Limitations and future research directions
This study is important because it provides researchers and clinicians with data about the complex relationship between parenting stress and parental ADHD and depression symptoms. Although adolescent ADHD symptoms contribute to parents’ parenting stress, the parents’ ADHD symptoms and impairment as well as depression symptoms emerged as significant predictors of parenting stress among parents of adolescents with ADHD suggesting that the role of parental psychopathology in parenting stress among parents of adolescents is a significant issue that warrants continued investigation. Seventy-five percent of participants in this study were from intact families where both parents participated in the study; this made it possible to examine the shared impact of within-family psychopathology on parenting stress. We found that this within-family psychopathology is important to consider in studies on parenting stress.
Despite the important findings, this study has some limitations. First, items on the PFS scale of the SIPA (e.g. Since my child became a teenager, my spouse/partner and I don’t spend as much time together as a couple as I had expected) could not be adequately answered by parents who were divorced, separated, or single; this precluded the calculation of a PFS domain score for those parents (n = 8). Second, all measures of parental psychopathology were self-reported; thus, parents reported on the level of their ADHD symptoms and impairment, depression symptoms, and parenting stress. Single source bias needs to be considered when interpreting these results. Third, it is important to note that while the CAARS-S:SV and BDI-II have strong concurrent and construct validity, the parents in this study were not necessarily formally diagnosed with ADHD or a depressive disorder, and the analyses examined symptoms as continuous variables. Fourth, according to parent report, 68% of the sample of adolescents with ADHD had a comorbid diagnosis of learning disability, anxiety, depression, or oppositional defiant disorder. This level of comorbidity is common in samples of children and adolescents with ADHD (see Pliszka 2015 for review). The study results, however, may be generalizable only to populations where the majority of adolescents with ADHD have a comorbid diagnosis. Although these parent-reported co-occurring diagnoses were typically given by physicians or psychologists who used diagnostic interviews or psychological tests, the methods used to diagnose these comorbid conditions were likely not consistent among participants in the sample.
Finally, the cross-sectional design of this study does not permit the investigation of causation. For example, with regard to depression symptoms, it is unclear whether parenting stress leads to elevated depression symptoms, whether depression causes higher levels of parenting stress, or whether the relationship is bi-directional. Furthermore, parents who are depressed might have more negative self-appraisals and as a result report elevated ADHD symptoms and parenting stress. Studies using longitudinal designs are needed to investigate the transactional nature of parental ADHD, depression symptoms and parenting stress. Johnston et al. (2012) proposed that parenting stress mediates the relationship between parental ADHD symptoms and parenting behaviors, and that there is a transactional relationship between parenting behaviors and child outcomes. Longitudinal studies with large samples are needed to examine whether this model is supported.
The high level of parenting stress reported by parents of adolescents with ADHD in the current and other studies (Gordon and Hinshaw 2017; Wiener et al. 2016) indicates that the degree of stress and distress parents experience and their ADHD and depression symptoms should be considered in future research on interventions with families of adolescents with ADHD. Thus, when developing and evaluating family interventions for adolescents with ADHD, researchers and clinicians should screen for and assess parenting stress, parental ADHD and depression as these problems may play a significant role in treatment adherence and outcomes. As suggested by Johnston et al. (2012), the presence of parental ADHD symptomatology may necessitate the modification of parenting interventions from lecture-based programming to the inclusion of hands-on and interactive coaching strategies. The current study also suggests that future research should examine whether interventions that provide parents with coping strategies to target the low mood and negative self-appraisals and cognitions associated with depression may be effective in reducing parenting stress. Given the challenges experienced in families where one or both parents experience ADHD or depression, it may be important to determine whether family or couples therapy may address sources of stress or conflict associated with co-parenting.
References
Aassve, A., Goisis, A., & Sironi, M. (2012). Happiness and childbearing across Europe. Social Indicators Research, 108(1), 65–86. https://doi.org/10.1007/s11205-011-9866-x.
Abidin, R. R. (1995). The Parenting Stress Index. 3rd edn. Odessa, FL: Psychological Assessment Resources, Inc.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. 5th edn. Arlington, VA: American Psychiatric Association.
Ballas, D., & Dorling, D. (2007). Measuring the impact of major life events upon happiness. International Journal of Epidemiology, 36(6), 1244–1252. https://doi.org/10.1093/ije/dym182.
Barkley, R. A. (2015). Comorbid psychiatric disorders and psychological maladjustment in adults with ADHD. In R. A. Barkley Ed., Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. 4th edn. (pp. 343–355). New York, NY: Guilford Press.
Barkley, R. A., Fischer, M., Smallish, L., & Fletcher, K. (2002). The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology, 111(2), 279–289. https://doi.org/10.1037/0021-843X.111.2.279.
Barkley, R. A., Fischer, M., Smallish, L., & Fletcher, K. (2004). Young adult follow-up of hyperactive children: antisocial activities and drug use. Journal of Child Psychology and Psychiatry, 45(2), 195–211. https://doi.org/10.1111/j.1469-7610.2004.00214.x.
Barkley, R. A., Murphy, K. R., & Fisher, M. (2008). ADHD in adults: what the science says. New York, NY: Guilford Press.
Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. The American Journal of Psychiatry, 165(8), 969–977. https://doi.org/10.1176/appi.ajp.2008.08050721.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory-II technical manual. San Antonio, TX: Psychological Corporation.
Belsky, J., & Pluess, M. (2009). Beyond diathesis stress: differential susceptibility to environmental influences. Psychological Bulletin, 135(6), 885–908. https://doi.org/10.1037/a0017376.
Benazon, N. R., & Coyne, J. C. (2000). Living with a depressed spouse. Journal of Family Psychology, 14(1), 71–79. https://doi.org/10.1037/0893-3200.14.1.71.
Bianchi, S. M., & Raley, S. B. (2005). Time allocation in families. In S. M. Bianchi, L. M. Casper & R. B. King (Eds), Work, family, health, and well-being (pp. 21–42). Mahwah: Erlbaum.
Brennan, P. A., Hammen, C., Katz, A. R., & Le Brocque, R. M. (2002). Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Clinical Psychology, 70(5), 1075–1085. https://doi.org/10.1037/0022-006X.70.5.1075.
Coltrane, S. (2000). Research on household labor: modeling and measuring the social embeddedness of routine family work. Journal of Marriage & Family, 62, 1208–33. https://doi.org/10.1111/j.1741-3737.2000.01208.x.
Conners, C. K. (2008). Conners-3. 3rd edn. Toronto, ON: Multi-Health Systems Inc.
Conners, C. K., Erhardt, D., & Sparrow, E. (1999). Conners’ Adult ADHD Rating Scales (CAARS) technical manual. Toronto, Canada: Multi-Health Systems.
Coyne, J. C., & Benazon, N. R. (2001). Not agent blue: effects of marital functioning on depression and implications for treatment. In S. R. H. Beach (Ed.), Marital and family processes in depression: a scientific foundation for clinical practice (pp. 25–43). Washington, DC: American Psychological Association.
Crnic, K., & Greenberg, M. (1990). Minor parenting stress with young children. Child Development, 54(5), 209–217. https://doi.org/10.2307/1130770.
Cummings, E. M., Keller, P. S., & Davies, P. T. (2005). Towards a family process model of maternal and paternal depressive symptoms: exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry, 46(5), 479–489. https://doi.org/10.1111/j.1469-7610.2004.00368.x.
Deater-Deckard, K. (2004). Parenting stress and child adjustment: some old hypotheses and new questions. Clinical Psychology: Science and Practice, 5(3), 314–332. https://doi.org/10.1111/j.14682850.1998.tb00152.x.
Dishion, T. J., Nelson, S. E., & Kavanagh, K. (2003). The family check-up with high-risk young adolescents: preventing early-onset substance use by parent monitoring. Behavior Therapy, 4(4), 553–571. https://doi.org/10.1016/S0005-7894(03)80035-7.
Erhardt, D., Epstein, J. N., Conners, C. K., Parker, J. D. A., & Sitarenios, G. (1999). Self-ratings of ADHD symptoms in adults II. Reliability, validity, and diagnostic sensitivity. Journal of Attention Disorders, 3(3), 153–158. https://doi.org/10.1177/108705479900300304.
Fayyad, J., de Graaf, R., Kessler, R., Alonso, J., Angermeyer, M., Demyttenaere, K., & Jin, R. (2007). Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. The British Journal of Psychiatry, 190, 402–409. https://doi.org/10.1192/bjp.bp.106.034389.
Fischer, M. (1990). Parenting stress and the child with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology, 19, 337–346. https://doi.org/10.1207/s15374424jccp1904_5.
Garcia, C. R., Bau, C. H. D., Silva, K. L., Callegari-Jacques, S., Salgado, C. A. I., Fischer, A. G., & Grevet, E. H. (2012). The burdened life of adults with ADHD: impairment beyond comorbidity. European Psychiatry, 27(5), 309–313. https://doi.org/10.1016/j.eurpsy.2010.08.002.
Gerdes, A. C., Hoza, B., Arnold, L. E., Pelham, W. E., Swanson, J. M., Wigal, T., & Jensen, P. S. (2007). Maternal depressive symptomatology and parenting behavior: exploration of possible mediators. Journal of Abnormal Child Psychology, 35(5), 705–714. https://doi.org/10.1007/s10802-007-9134-3.
Goodman, S. H., & Gotlib, I. H. (2002). Children of depressed parents: mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association.
Goodman, S. H., Rouse, M. H., Connell, A. M., Broth, M. R., Hall, C. M., & Heyward, D. (2011). Maternal depression and child psychopathology: a meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. https://doi.org/10.1007/s10567-010-0080-1.
Goossens, L. (2006). The many faces of adolescent autonomy: parent-adolescent conflict, behavioral decision-making, and emotional distancing. In S. Jackson & L. Goossens (Eds.), Handbook of adolescent development (pp. 135–153). New York, NY: Psychology Press.
Gordon, C. T., & Hinshaw, S. P. (2017). Parenting stress and youth symptoms among girls with and without attention-deficit/hyperactivity disorder. Parenting, 17(1), 11–29. https://doi.org/10.1080/15295192.2016.1262178.
Harvey, E., Danforth, J. S., Eberhardt McKee, T., Ulaszek, W. R., & Friedman, J. L. (2003). Parenting of children with attention-deficit/hyperactivity disorder (ADHD): the role of parental ADHD symptomatology. Journal of Attention Disorders, 7(1), 31–42. https://doi.org/10.1177/108705470300700104.
Hines, J. L., King, T. S., & Curry, W. J. (2012). The adult ADHD self-report scale for screening for adult attention deficit–hyperactivity disorder. Journal of the American Board of Family Medicine, 25(6), 847–853. https://doi.org/10.3122/jabfm.2012.06.120065.
Johnston, C., Mash, E. J., Miller, N., & Ninowski, J. E. (2012). Parenting in adults with attention-deficit/hyperactivity disorder (ADHD). Clinical Psychology Review, 32(4), 215–228. https://doi.org/10.1016/j.cpr.2012.01.007.
Jokela, M., Power, C., & Kivimäki, M. (2009). Childhood problem behaviors and injury risk over the life course. Journal of Child Psychology and Psychiatry, 50(12), 1541–1549. https://doi.org/10.1111/j.14697610.2009.02122.x.
Kazdin, A. E. (1995). Child, parent and family dysfunction as predictors of outcomes in cognitive-behavioral treatment of antisocial children. Behavior Research and Therapy, 33(3), 271–281. https://doi.org/10.1016/0005-7967(94)00053-M.
Kazdin, A. E., & Nock, M. K. (2003). Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44(8), 1116–1129. https://doi.org/10.1111/1469-7610.00195.
Kessler, R. C., Adler, L. A., Barkley, R. A., Biederman, J., Conners, C. K., Demler, O., & Zaslavsky, A. M. (2006). The prevalence and correlates of adult ADHD in the united states: results from the national comorbidity survey replication. American Journal of Psychiatry, 163(4), 716–723. https://doi.org/10.1176/appi.ajp.163.4.716.
Knouse, L. E., Zvorsky, I., & Safren, S. A. (2013). Depression in adults with attention-deficit/hyperactivity disorder (ADHD): the mediating role of cognitive-behavioral factors. Cognitive Therapy and Research, 37(6), 1220–1232. https://doi.org/10.1007/s10608-013-9569-5.
Lila, M., van Aken, M., Musitu, G., & Buelga, S. (2006). Families and adolescents. In S. Jackson & L. Goossens (Eds), Handbook of adolescent development (pp. 154–174). Hove: Psychology Press.
Mash, E. J., & Johnston, C. (1990). Determinants of parenting stress: illustrations from families of hyperactive children and families of physically abused children. Journal of Clinical Child Psychology, 19, 313–328. https://doi.org/10.1207/s15374424jccp1904_3.
Mazursky-Horowitz, H., Felton, J. W., MacPherson, L., Ehrlich, K. B., Cassidy, J., Lejuez, C. W., & Chronis-Tuscano, A. (2015). Maternal emotion regulation mediates the association between adult attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology, 43(1), 121–131. https://doi.org/10.1007/s10802-014-9894-5.
Mazursky-Horowitz, H., Thomas, S. R., Woods, K. E., Chrabaszcz, J. S., Deater-Deckard, K., & Chronis-Tuscano, A. (2018). Maternal executive functioning and scaffolding in families of children with and without parent-reported ADHD. Journal of Abnormal Child Psychology, 46(3), 463–475. https://doi.org/10.1007/s10802-017-0289-2.
Mannuzza, S., Castellanos, F. X., Roizen, E. R., Hutchison, J. A., Lashua, E. C., & Klein, R. G. (2011). Impact of the impairment criterion in the diagnosis of adult ADHD: 33-year follow-up study of boys with ADHD. Journal of Attention Disorders, 15(2), 122–129. https://doi.org/10.1177/1087054709359907.
Minde, K., Eakin, L., Hechtman, L., Ochs, E., Bouffard, R., Greenfield, B., & Looper, K. (2003). The psychosocial functioning of children and spouses of adults with ADHD. Journal of Child Psychology and Psychiatry, 44(4), 637–646. https://doi.org/10.1111/1469-7610.00150.
Nelson, S. K., Kushlev, K., English, T., Dunn, E. W., & Lyubomirsky, S. (2013). In defense of parenthood: children are associated with more joy than misery. Psychological Science, 24(1), 3–10. https://doi.org/10.1177/0956797612447798.
Oyserman, D., Mowbray, C. T., Meares, P. A., & Firminger, K. B. (2000). Parenting among mothers with a serious mental illness. American Journal of Orthopsychiatry, 70(3), 296–315. https://doi.org/10.1037/h0087733.
Phares, V., Fields, S., & Kamboukos, D. (2009). Fathers’ and mothers’ involvement with their adolescents. Journal of Child and Family Studies, 18(1), 1–9. https://doi.org/10.1007/s10826-008-9200-7.
Pliszka, S. (2015). Comorbid psychiatric disorders in children with ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. 4th edn. (pp. 140–168). New York, NY: Guilford.
Putnick, D. L., Bornstein, M. H., Hendricks, C., Painter, K. M., Suwalsky, J. T. D., & Collins, W. A. (2008). Parenting stress, perceived parenting behaviors, and adolescent self-concept in European American families. Journal of Family Psychology, 22(5), 752–762. https://doi.org/10.1037/a0013177.
Putnick, D. L., Bornstein, M. H., Hendricks, C., Painter, K. M., Suwalsky, J. T. D., & Collins, W. A. (2010). Stability, continuity, and similarity of parenting stress in European American mothers and fathers across their child’s transition to adolescence. Parenting: Science and Practice, 10(1), 60–77. https://doi.org/10.1080/15295190903014638.
Robin, A. L., & Payson, E. (2002). The impact of ADHD on marriage. The ADHD Report, 10(3), 9–14.
Sheras, P. L., Abidin, R. R., & Konold, T. R. (1998). Stress Index for Parents of Adolescents. Odessa, FL: Psychological Assessment Resources.
Theule, J., Wiener, J., Jenkins, J., & Tannock, R. (2013). Parenting stress in families of children with ADHD: a meta-analysis. Journal of Emotional and Behavioral Disorders, 21(1), 3–17. https://doi.org/10.1177/1063426610387433.
Theule, J., Wiener, J., Rogers, M., & Marton, I. (2011). Predicting parenting stress in families of children with ADHD: parent and contextual factors. Journal of Child and Family Studies, 20(5), 640–647. https://doi.org/10.1007/s10826-010-9439-7.
Thomason, E., Volling, B. L., Flynn, H. A., McDonough, S. C., Marcus, S. M., Lopez, J. F., & Vazquez, D. M. (2014). Parenting stress and depressive symptoms in postpartum mothers: bidirectional or unidirectional effects? Infant Behavior & Development, 37(3), 406–415. https://doi.org/10.1016/j.infbeh.2014.05.009.
van der Oord, S., Prins, P. J. M., Oosterlaan, J., & Emmelkamp, P. M. G. (2006). The association between parenting stress, depressed mood, and informant agreement in ADHD and ODD. Behavior Research and Therapy, 44(11), 1585–1595. https://doi.org/10.1016/j.brat.2005.11.011.
Webster-Stratton, C. (1990). Stress: a potential disruptor of parent perceptions and family interactions. Journal of Clinical Child Psychology, 19(4), 302–312. https://doi.org/10.1207/s15374424jccp1904_2.
Wechsler, D. (1999). Manual for the wechsler abbreviated scale of intelligence (WASI). San Antonio, TX: Psychological Corporation.
Wiener, J., Biondic, D., Grimbos, T., & Herbert, M. (2016). Parenting stress of parents of adolescents with attention-deficit hyperactivity disorder. Journal of Abnormal Child Psychology, 44(3), 561–574. https://doi.org/10.1007/s10802-015-0050-7.
Wilens, T. E., Biederman, J., Faraone, S. V., Martelon, M., Westerberg, D., & Spencer, T. J. (2009). Presenting ADHD symptoms, subtypes, and comorbid disorders in clinically referred adults with ADHD. Journal of Clinical Psychiatry, 70(11), 1557–1562. https://doi.org/10.4088/JCP.08m04785pur.
Wymbs, B. T., Pelham, Jr., W. E., Molina, B. S. G., Gnagy, E. M., Wilson, T. K., & Greenhouse, J. B. (2008). Rate and predictors of divorce among parents of youths with ADHD. Journal of Consulting and Clinical Psychology, 76(5), 735–744. https://doi.org/10.1037/a0012719.
Author Contributions
D.B. designed and executed the study, analyzed the data, and wrote the first draft of the paper. J.W. obtained funding for the study, collaborated in the design of the study and writing of the paper, and edited the final manuscript. R.M. contributed to the statistical analysis.
Funding
This study was funded by the Social Sciences and Humanities Research Council of Canada (Protocol Number 410-2010-1763).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures in this study were in accordance with the ethical standards of the institutional research committee. The Social Sciences, Humanities and Education Research Ethics Board of the University of Toronto provided IRB approval for the study.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biondic, D., Wiener, J. & Martinussen, R. Parental Psychopathology and Parenting Stress in Parents of Adolescents with Attention-Deficit Hyperactivity Disorder. J Child Fam Stud 28, 2107–2119 (2019). https://doi.org/10.1007/s10826-019-01430-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-019-01430-8