Abstract
It is known that youth engaged in the juvenile justice system show high rates of psychiatric disorders. However, little is known about the course of those disorders over time, or about mental health service use on the part of children and families during justice system involvement. Boys and girls recruited from their first contact with juvenile court (n = 75), at a mean age of 13.6 years, completed three waves of interviews, each consisting of a structured clinical interview and questionnaires regarding service use, family functioning, parental burden, and parental psychopathology. High rates of psychiatric disorders were evident. Three quarters (n = 56) met criteria for a mood, anxiety or behavioral disorder by parent or child report. Despite the high prevalence of mental health concerns, relatively few youth (approximately 20 %) were involved in mental health services in follow-up waves. The presence of ODD and higher levels of family communication problems were associated with involvement in mental health services. Although parents experienced burden associated with their child’s mental health problems, burden was not a strong correlate of help-seeking. Mental health problems declined from the point of initial involvement with juvenile justice; only ODD symptoms showed stability over time. Low rates of engagement in mental health services are found for juveniles subsequent to their first contact with juvenile justice. ODD and family communication problems most influenced service engagement, while burden due to mental health problems did not. The results provide potential targets for efforts to enhance parental motivation towards service engagement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 50–70 % of youth involved in the juvenile justice system (JJS; about 1.4 of 2.4 million adolescents annually; Snyder 2006) have a diagnosable mental health (MH) condition (Skowyra and Cocozza 2006), in contrast to 10–20 % in the general juvenile population (US Department of Health and Human Services 1999). Estimated rates of psychiatric disorder tend to be higher among residential (Wasserman et al. 2002) or detention facilities (Teplin et al. 2002) than at probation intake (Wasserman et al. 2005), although few studies of samples drawn from less intensive settings are available.
Addressing the MH needs of adolescents in the JJS makes sense from two perspectives. First, if MH needs are related to either continued offending or difficulty adjusting in the community, identifying these cases early and providing appropriate treatment could reduce future delinquency, future JJS system involvement, or further multiple systems penetration. Second, taking a broader societal perspective, the point of initial engagement in JJS may represent a valuable point at which linkage could be made between needs and services for youths at high risk for poor outcomes, including persisting MH problems. Enhanced efforts to identify and refer to MH services for these youth, regardless of their future JJS involvement, would address the overall level of unmet need for MH services. Many of these youth struggle over a long developmental period with unidentified MH concerns, a course that often remains unchanged despite the red flag of JJS involvement. Failing to identify and link these youth with MH problems to services represents a missed opportunity. Despite the clear potential utility, there is very limited evidence about the efficiency with which the JJS links youth to services when need is identified (Aalsma et al. 2012; Cuellar et al. 2006; Rogers et al. 2001).
There is also a dearth of information on parental decisions regarding youth engagement in MH services after initial JJS contact, even though it is clear that parents often act as gatekeepers for children’s service use. In the child welfare system, factors such as parental competency, parenting stress, parental depression and social support have been shown to be predictive of service use among children (Villagrana 2010). For parents involved in the JJS, there is little evidence regarding which factors influence parents’ service-seeking behaviors subsequent to JJS involvement. There are myriad factors that might conceivably influence a parent’s decisions about whether or not to engage in MH services for a child, but the presence of “action signs,” of atypical behavior including aggression, leads only a small proportion of children to engage in services (Jensen et al. 2011). The fact that a child has become involved with the JJS might denote for many parents that some problem exists, especially in combination with the presence of psychopathology. However, for behavioral disorders, which are the most common among youth in JJS populations, there may be greater barriers to engagement in MH services (Burns et al. 2000; Stouthamer-Loeber et al. 1992; Stouthamer-Loeber et al. 1995). In the MH services literature, there is evidence that help-seeking behavior, perhaps counterintuitively, may be lower for youth who show conduct disorder (CD) relative to oppositional defiant disorder (ODD; Bussing et al. 2003a, b; Cornelius et al. 2001), even though the former consists of more severe behaviors reflecting delinquent acts.
The range of factors that might influence parental decision making about seeking services for their adolescent is broad. Parents’ decisions to seek MH services may be driven greatly by issues other than the child’s symptomatology; difficulties in family interactions, parenting behaviors, distress associated with their own psychopathology, adequacy of family resources, or the child’s functioning in school may all play a role. Further, children’s MH problems typically cause distress for parents both directly, in terms of coping with the immediate displays of MH problems, and indirectly, such as losing time from work, feeling stigmatized by family members or in the community, experiencing increasingly maladaptive parenting behaviors over time (Burke et al. 2008) or experiencing inter-parental relationship problems (Schermerhorn et al. 2012) as a result of their children’s behavioral problems. Parental burden or strain may possibly serve as a cumulative index of a parent’s difficulty coping with an adolescent’s MH problems (Bussing et al. 2003a, b ).
Finally, more macro level circumstances, such as socioeconomic disadvantage or limited availability and/or access to services can all influence decisions to engage in services (Kazdin et al. 1995; McKay et al. 1996; Nock and Kazdin 2001). Ethnic differences in services usage have also been well documented. Angold et al. (2002) found that although African American and Caucasian children did not differ in prevalence rates of disorders, apart from depression, Caucasian children were more likely to use specialty MH services. Additionally, African American children may be more likely to terminate prematurely from services (Gonzalez et al. 2011).
The present study examined the patterns of MH concerns and service use among a sample of youth at the point of their initial involvement in juvenile justice who did not have any prior history of MH service use. Structured clinical interviews and measures of service use were collected at baseline and at each of two annual follow up assessments. Measures of factors potentially related to services use were also collected. Hypotheses guiding the study were:
-
1.
Engagement in MH services will not be significantly associated with CD, depression or anxiety, but will be associated with ODD and ADHD.
-
2.
This relationship will hold after accounting for other significant factors associated with service engagement, including gender, race, socioeconomic status, and parental MH.
-
3.
Among disorders, ODD will be most associated with high levels of parental burden, and parental burden will mediate the relationship between ODD and service use.
Method
Participants
A total of 75 parent–child pairs were recruited into the study. The sample was 84 % African American and 12 % Caucasian. The majority (64 %) of the sample were boys. The mean age at baseline interview was 13.6, ranging from 10.9 to 15.12. Retention in year 2 was 88 % (66/75), and 69 % in year 3 (52/75). The demographics for the sample are presented in Table 1.
Procedure
Adolescents, along with one parent each, were recruited in two ways. Primarily, they were recruited from the waiting room of the juvenile court. Parents checking into wait for a hearing were informed of the study, and those indicating an interest were directed to discuss the study with a study staff member who was available in the waiting room. A brief screening was conducted in a separate secluded area attached to the waiting room. Eligible participants were scheduled for a study interview. Alternatively, participants were recruited through advertisements on city buses seeking parents of children who were engaged in juvenile justice services for the first time. These participants contacted study staff via telephone and completed a brief screen to determine study eligibility. Eligibility criteria were: child engaged for the first time with the juvenile justice system; child age between 10 and 15 years (given that the state’s age of criminal responsibility was 10); no MH service sought for the child in the past year; no history of a diagnosis or services for mental retardation; no physical or developmental limitations that interfere with daily living and which would require special assistance to manage.
Interviews were administered using a laptop computer by trained research interviewers. All participants were compensated for their participation. Interviews were conducted primarily in family homes, although office interviews and alternate locations were employed at family request. All interview locations provided for secure and private administration of the interview protocol. All study procedures were approved and monitored by the Institutional Review Board of the University of Pittsburgh.
Measures
Identification of Mental Health Concerns
The Diagnostic Interview Schedule for Children (DISC) was used to measure parent reported symptoms, associated impairment and diagnoses of ODD, CD, depression, anxiety, substance use and other child psychopathology. The DISC is a highly structured interview designed to assess DSM-IV psychiatric disorders and symptoms in children and adolescents aged 6–17 years. Parent and child report were both obtained for the present study, and were combined in an either/or fashion at the symptom level. Child report on the DISC was missing in one case in year 1, in five cases in year 2 and in 2 cases in year 3. In these instances, parent report alone was used to measure child MH concerns.
A composite of depression diagnoses was made by combining any reported major depressive disorder or dysthymia. Additionally, an anxiety disorder variable reflected the presence of any one of the following anxiety disorders: agoraphobia, panic disorder, generalized anxiety, obsessive compulsive disorder, separation anxiety disorder, post-traumatic stress disorder, social phobia and specific phobia.
Service Use
The Child and Adolescent Services Assessment (CASA; Ascher et al. 1996) was used to measure service utilization. Parents are asked whether help was sought from a wide range of potential sources for behavioral or emotional problems in the child’s lifetime and during the past 3 months in particular. The CASA has been shown to have adequate reliability for most care providers, with lower reliability for school-based and informal sources of care, and to have demonstrated acceptable validity (Ascher et al. 1996).
Past 3 month service use data was used to index service use in the present study. Two constructs were created regarding services. The first indicated any use of specialty MH services in the past 3 months, including inpatient, day treatment, outpatient, intensive wraparound or community based MH treatment. A second construct, referred to here as other services, reflected any use in the preceding 3 months of services other than specialty MH services. Other services included school-based services (e.g. contacts with school counselors, discussions with teachers about emotional or behavioral problems, in-school services, or placement in an approved private school for behavioral problems). Other services also included any juvenile justice related service contact. This was almost exclusively contact with a probation officer, but the measure also included queries regarding detention centers or jails, juvenile justice residential placements or contacts with a juvenile correctional counselor.
Parental Psychopathology
Parental history of MH problems were measured using parent self-report on the Computerized Diagnostic Interview Schedule for DSM IV. This structured clinical interview was administered by study interviewers, and assessed current and lifetime mood, anxiety, behavior and substance use disorders. This information was obtained only at baseline. Constructs for the present study reflected the presence of any mood disorder, any anxiety disorder, or any antisocial behavioral disorder over the parent’s lifetime.
Parental Burden
The Child and Adolescent Impact Assessment (Messer et al. 1996) was used to assess perceptions of burden by the parent associated with emotional or behavioral problems on the part of the child. These include the economic impacts of a child’s problems on the parent and family, their impact on family and other relationships, and restrictions they might place on the parent’s activities. A construct representing total parental burden was created by taking the sum of any reported impacts in any of these domains. In year 1, parents reported a range from 0 to 8 total types of burden (mean = 1.03, sd = 1.84).
Family Functioning
The Family Assessment Device (FAD; Epstein et al. 1983) was developed for screening purposes in a family therapy setting. Parents rated their agreement/disagreement with 53 statements in seven subscales regarding how the youth’s family typically functions. These included: Problem Solving; Communication; Roles; Affective Responsiveness; Affective Involvement; Behavior Control; and General Functioning. Higher scores on these scales indicate more problematic functioning. Reliability for the various scales in year 1 of the present study ranged from an alpha of .69 for Roles to .82 for General Functioning.
Parents also provided demographic information regarding family income, child and parent racial group identification, and number of individuals living in the household. A dichotomous poverty level variable was created using the reported household income and the number of people supported by that income, with reference to the criteria for the 2011 federal guidelines for poverty status.
Data Analyses
The present analyses were conducted using Stata. Because the sample was recruited to have no service use history at baseline, outcomes of service use could be examined only in years 2 and 3. Models were structured to test the contemporaneous relationship between predictors and outcomes of service use. However, it should be kept in mind that the measure of service use was limited to the services used in the preceding 3 months, whereas other factors were assessed for the past year. Mental health service use was dichotomized, so logistic regression models were conducted. Models were clustered by participant to account for correlated observations over repeated measurements.
Results
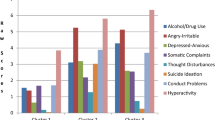
Most of the sample (74.3 %) met criteria for ODD, CD, ADHD, depression or anxiety in wave 1 by combined parent and youth report. The most prevalent disorders were ODD (43 %, n = 32 %), CD (37 %, n = 28) and anxiety disorders (29 %, n = 21). ADHD and depression were each present for 13 % (n = 10) of the sample. Figure 1 shows the percentages meeting separate disorder criteria by parent report, youth report and by combining informant report.
Comorbidity among disorders in the sample was high. More than one-third (37 %) of the overall sample, and 50 % of those meeting criteria for any disorder were comorbid for more than one disorder. The most common comorbidities involved ODD (evident in 24 out of 28 cases with comorbidity), CD (in 19 of 28) and anxiety (in 14 of 28). Depression and ADHD featured in nine and eight cases, respectively. Since the diagnostic prohibition of the DSM IV (American Psychiatric Association 1994) against assigning both ODD and CD was not followed in this study, it should be noted that 6 out of 28 cases of comorbidity involved solely the presence of both ODD and CD.
Few gender differences were observed. At baseline, the only disorder that varied between boys and girls was ODD, which was more prevalent among girls than boys (χ 2 = 7.75, p = .005). There were no gender differences in rates of CD, ADHD, depression or anxiety. There was no difference between boys and girls in their use of non-MH services in year 1 (χ 2 = 0.002, p = .98), nor in their use of MH services in year 2 (χ 2 = 2.14, p = .14) or year 3 (χ 2 = 0.29, p = .59).
Declines in rates of psychopathology were observed over time. At wave 2, 46 % (n = 31) of the overall sample met criteria for at least one disorder. At wave 3, 47 % (n = 24) met criteria for any disorder. For each disorder except one, the course over time was generally declining. The greatest discontinuity was found for anxiety disorders between years 1 and 2; only 3 of 22 individuals with anxiety in year 1 persisted with an anxiety disorder in year 2. Three of 10 individuals with depression at baseline persisted in year 2.
Across both wave-to-wave transitions (year 1–2 and year 2–3), youth with depression at one wave did not meet criteria in the following wave (77 % of the time), and youth with anxiety did not meet criteria in the following wave 76 % of the time. Similar rates were observed in wave to wave discontinuation for CD (71 %) and ADHD (65 %). Only ODD showed a generally persisting course, where 65 % of the time a youth who met criteria in 1 year met them again in the following year. Specifically, the annual prevalence of ODD was 43 % (n = 32) by combined report in year 1, 39 % in year 2 (n = 26) and 35 % in year 3 (n = 18).
In terms of psychopathology on the part of the parents, 20 parents (26.7 % of the reports obtained) reported some history of MH disorder. Parents with MH disorders were more likely to report disorders for their children (χ2 = 5.81, p = .016). On the other hand, children’s self-report of MH was not associated with parental MH status (χ2 = 0.55, p = .46).
Table 2 shows the number of children per year who used specialty MH services or other services associated with concerns about emotional or behavioral functioning. Since probation services were included among other services, a relatively high proportion of youth (69 %) were reported to have used services other than specialty MH services at baseline, although the proportion reporting use of other services declined over time.
A logistic regression model, clustered on study participant was conducted to examine the association between disorders and MH service use over years 2 and 3. Since participants were recruited based on the absence of MH service seeking in year 1, data from that year were not included in the model. The results are provided in Table 3. Among disorders, only ODD (OR 4.64, se = 2.43, p = .003) remained significantly associated with MH service use in years 2 and 3. Of the covariates shown in Table 1, school adjustment was significantly associated with specialty MH service use (OR 1.16, se = .05, p < .001) and parental burden was marginally predictive of suche use (OR 1.28, se = 0.18, p = .09).
Within the domain of family functioning constructs, a stepwise regression, using an alpha of .10 as the criterion for removal from the model, tested each subscale of the FAD. The variables were centered prior to testing to avoid problems with multicollinearity. The FAD subscale of Family Roles (OR 1.28, se = .12, p = .03) was significantly associated with MH service use, and FAD Communication (OR 1.22, se = .13, p = .08) was marginally so.
A final regression model tested ODD, school adjustment, burden, FAD Family Roles, FAD Communication and child communication. After stepwise removal, ODD (OR 4.09, se = 2.34, p = .01, 95 % CI [1.34, 12.53]) and FAD Communication (OR 1.33, se = .12, p = .002, 95 % CI [1.11, 1.59]) were retained as factors associated with service use.
The lack of burden associated with MH problems in the model as a factor in MH service use was contrary to study hypotheses. To test the relationship between disorders and burden, a Poisson regression model was conducted, examining the contemporaneous relationship between all disorders and parental burden. ODD (IRR = 3.11, se = 1.03, p = .001), CD (IRR = 2.57, se = .70, p = .001) and ADHD (IRR = 2.07, se = .57, p = .009) were significantly associated with parental burden in a multivariate model. Post-hoc comparisons of parameter values did not reveal any significant differences between these disorders in their association with burden in either model.
Discussion
In this juvenile justice sample, a high rate of MH problems were identified, with 74 % of youth identified as meeting criteria for at least one disorder. Further, 50 % of those meeting criteria for one disorder also met criteria for another. These rates are consistent with those identified in other samples (Teplin et al. 2002; Wasserman et al. 2004). However, this high rate of MH concerns is particularly notable because this was a sample of youth at their first contact with the juvenile justice system, with no history of MH service use.
On the other hand, this similarity in rates of MH problems in this sample compared to other samples is complicated by our assessment protocol. Specifically, we obtained both parent and youth report of MH problems, whereas by and large, prior studies of the prevalence of disorders in juvenile justice settings have been restricted to youth self-report (Teplin et al. 2002; Wasserman et al. 2002, 2004). Informant biases are well-known in the assessment of child psychopathology (Jensen et al. 1999; Loeber et al. 1989) and may affect certain disorders more than others (e.g. ADHD; Schwab-Stone et al. 1996) and ODD (Jensen et al. 1999; Loeber et al. 1989). This raises the possibility that, as alarmingly high as previously reported rates of mental disorders among juvenile justice populations have been, they may have been even higher if parent report had been collected. For example, in the present sample, if child report alone had been used to identify MH problems at baseline, the overall prevalence for MH disorders would have been 41.9 %, rather than 74.3 %. Further, for most disorders individually, child report alone would have identified approximately half the total identified by parent and child report combined. For example, children and parents each identified the same proportion of instances of CD (although not entirely overlapping). However, for ODD, children reported only one-third of the combined rate, and for depression, child report identified only 1 of the 6 total cases that were identified by combined report.
Rates of anxiety, ODD and CD measured in this sample were markedly greater than typically observed in the general population. On the other hand, rates of ADHD and depression, while elevated, were closer to general population rates. In addition, elevated MH concerns were greatest at baseline, and a steep decline was notable. This was particularly true for anxiety disorders. While the present data do not allow for a specific test, this observation might suggest that initial engagement with juvenile justice elicits or exacerbates problems with anxiety, and that these anxieties diminish over time. As a result, when youth are identified as having MH concerns in juvenile justice, especially for adolescents new to the system, follow-up assessments may help to distinguish episodic concerns from persisting difficulties.
Rates of engagement in MH services use were low. In either year 2 or year 3, only 20 % of those in this juvenile justice cohort engaged in MH service use. Consistent with other studies (Bussing et al. 2003a, b; Cornelius et al. 2001), ODD was strongly related to help-seeking behavior whereas CD was not. However, ADHD was not significantly associated with MH service use, nor were depression and anxiety. In part, the declining prevalence of most of these disorders may have influenced help-seeking; if depression or anxiety problems had persisted with greater severity, for example, they may have motivated greater help-seeking.
Somewhat surprisingly, relatively few demographic factors distinguished those who engaged in MH service use from those who did not. At a bivariate level, service use was influenced by a wide variety of domains, including the degree to which parents felt burdened by their children’s behaviors, the nature of contact with teachers, and their child’s school adjustment. However, after accounting for ODD behaviors, only poorer family communication remained independently significantly predictive of service use.
It is likely that children in the juvenile justice cohort had shown a relatively high rate of psychiatric disorders prior to contact with the juvenile justice system, but these parents had no history of having responded with service-seeking behaviors. It was not the case that parents were indifferent to the MH problems shown by their children, even if they may not have necessarily identified them as such. Parental burden was elevated by ODD, CD and ADHD behaviors, even if the experience of parental burden did not translate into increased help-seeking behaviors prior to court involvement.
In terms of motivating help-seeking, parents were apparently responsive to functional indicators of difficulty or impairment in school or in family functioning, with oppositional and defiant behaviors being the primary psychopathological indicators driving help-seeking. It is noteworthy that the rate of CD in this juvenile justice sample was approximately 10 times the rate observed in the general population of youth, and the rate for ODD was approximately six or seven times that of the general population rate. Individual behavioral indicators of CD were likely evident among these children for up to several years. It is plausible that if parents had received services to treat these disorders, the developmental progression from early behavioral indicators to involvement in juvenile justice services may have been short-circuited. Again, these are not indifferent parents—they appear to feel the burden, they report concerns regarding family functioning, and the levels of problems in family functioning are individually associated with help-seeking efforts. It may be that these parents are not conceiving of behavioral disorders as a particularly appropriate target for MH services, with the exception of ODD symptoms (but not CD or ADHD symptoms).
Given these findings, when children show CD behaviors without showing behaviors that are more salient for parents (e.g. those associated with direct non-compliance, parent–child conflict, or family functional problems), and where parents are not getting feedback regarding school adjustment problems, they may be particularly less likely to involve their child in MH services. Methods to enhance the awareness of parents regarding the appropriateness and effectiveness of such services for conduct problems may be necessary. School-based identification and referral practices may enhance the connection between the manifestation of conduct problems and engagement in services.
Limitations
The present data are limited by the small sample size for each cohort. It is possible that several of the marginally significant effects observed in the present analyses would have been clearly significant, and the final models predicting to service engagement may have included additional information about the range of factors that influence service use. Additionally, these cohorts are not representative of the general population. Instead, they were selected to provide information about service use over time among groups of children and parents showing high rates of behavioral difficulties who had either already engaged in services, or who had not engaged in services despite having a child with juvenile justice system contact. The factors that affect continued service engagement among parents recruited from a MH clinic are going to be different from those affecting service engagement decisions among parents in the general population.
Despite these limitations, the present study is one of the first to provide evidence about the degree of MH service engagement among youth with MH concerns in a juvenile justice population. The bottom line seems to be that there is a high level of diagnosable problems in youth encountering juvenile justice for the first time (as high as that seen in samples of youth deeper in the system), and that these youth are unlikely to get services for their MH problems after court involvement. Interestingly, though, many of these disorders wane over 2 years. How much better these youth would have been on numerous dimensions if they had received services is unknown.
The results raise several key questions. It will be important to determine how to intervene to help parents engage in services for MH concerns. Parents in the present study feel a high degree of burden in coping with their children’s behaviors, but this does not lead to service engagement. It may be possible to draw upon this sense of burden to increase parental motivation towards services. It will also be helpful to determine if the interaction with the justice system itself might explain elevated disorder rates. A more proximal and nuanced measurement of the degree of system interaction and the nature of the disposition of charges would help to determine whether declining psychopathology follows declining distress associated with system involvement.
References
Aalsma, M. C., Tong, Y., Lane, K., Katz, B., & Rosenman, M. B. (2012). Use of outpatient care by juvenile detainees upon community reentry: Effects of mental health screening and referral. Psychiatric Services, 63, 997–1003. (Washington, DC).
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association.
Angold, A., Erkanli, A., Farmer, E. M., Fairbank, J. A., Burns, B. J., Keeler, G., & Costello, E. J. (2002). Psychiatric disorder, impairment, and service use in rural African American and white youth. Archives of General Psychiatry, 59, 893–901.
Ascher, B. H., Farmer, E. M. Z., Burns, B. J., & Angold, A. (1996). The child and adolescent services assessment (CASA): Description and psychometrics. Journal of Emotional and Behavioral Disorders, 4, 12–20.
Burke, J. D., Pardini, D. A., & Loeber, R. (2008). Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. Journal of Abnormal Child Psychology, 36, 679–692. doi:10.1007/s10802-008-9219-7.
Burns, B. J., Landsverk, J., Kelleher, K., Faw, L., Hazen, A., & Keeler, G. (2000). Mental health, education, child welfare and juvenile justice service use by very young offenders. In R. Loeber & D. P. Farrington (Eds.), Very young offenders: Development, interventions, and service needs (pp. 273–303). Thousand Oaks, CA: Sage.
Bussing, R., Zima, B. T., Gary, F. A., & Garvan, C. W. (2003a). Barriers to detection, help-seeking, and service use for children with ADHD symptoms. Journal of Behavioral Health Services and Research, 30, 176–189. doi:10.1007/Bf02289806.
Bussing, R., Zima, B. T., Gary, F. A., Mason, D. M., Leon, C. E., Sinha, K., & Garvan, C. W. (2003b). Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 842–850. doi:10.1097/01.Chi.0000046876.27264.Bf.
Cornelius, J. R., Pringle, J., Jernigan, J., Kirisci, L., & Clark, D. B. (2001). Correlates of mental health service utilization and unmet need among a sample of male adolescents. Addictive Behaviors, 26, 11–19.
Cuellar, A. E., McReynolds, L. S., & Wasserman, G. A. (2006). A cure for crime: Can mental health treatment diversion reduce crime among youth? Journal of Policy Analysis and Management, 25, 197–214.
Epstein, N. B., Baldwin, L. M., & Bishop, D. S. (1983). The McMaster family assessment device. Journal of Marital and Family Therapy, 9, 171–180.
Gonzalez, A., Weersing, V. R., Warnick, E. M., Scahill, L. D., & Woolston, J. L. (2011). Predictors of treatment attrition among an outpatient clinic sample of youths with clinically significant anxiety. Administration and Policy in Mental Health and Mental Health Services Research, 38, 356–367.
Jensen, P. S., Goldman, E., Offord, D., Costello, E. J., Friedman, R., Huff, B., & Roberts, R. (2011). Overlooked and underserved: “Action signs” for identifying children with unmet mental health needs. Pediatrics, 128, 970–979. doi:10.1542/peds.2009-0367.
Jensen, P. S., Rubio-Stipec, M., Canino, G., Bird, H. R., Dulcan, M. K., Schwab-Stone, M. E., & Lahey, B. B. (1999). Parent and child contributions to diagnosis of mental disorders: Are both informants always necessary? Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1569–1579.
Kazdin, A. E., Stolar, M. J., & Marciano, P. L. (1995). Risk factors for dropping out of treatment among white and black families. Journal of Family Psychology, 9, 402–417.
Loeber, R., Green, S. M., Lahey, B. B., & Stouthamer-Loeber, M. (1989). Optimal informants on childhood disruptive behaviors. Development and Psychopathology, 1, 317–337.
McKay, M. M., McCadam, K., & Gonzales, J. J. (1996). Addressing the barriers to mental health services for inner city children and their caretakers. Community Mental Health Journal, 32, 353–361.
Messer, S. C., Angold, A., Costello, E. J., & Burns, B. J. (1996). The child and adolescent burden assessment (CABA): Measuring the family impact of emotional and behavioral problems. International Journal of Methods in Psychiatric Research, 6, 261–284.
Nock, M. K., & Kazdin, A. E. (2001). Parent expectancies for child therapy: Assessment and relation to participation in treatment. Journal of Child and Family Studies, 10, 155–180.
Rogers, K. M., Zima, B., Powell, E., & Pumariega, A. J. (2001). Who is referred to mental health services in the juvenile justice system? Journal of Child and Family Studies, 10, 485–494.
Schermerhorn, A. C., D’Onofrio, B. M., Slutske, W. S., Emery, R. E., Turkheimer, E., Harden, K. P., & Martin, N. G. (2012). Offspring ADHD as a risk factor for parental marital problems: Controls for genetic and environmental confounds. Twin Research and Human Genetics, 15, 700–713.
Schwab-Stone, M. E., Shaffer, D., Dulcan, M. K., Jensen, P. S., Fisher, P., Bird, H. R., & Canino, G. (1996). Criterion validity of the NIMH diagnostic interview schedule for children version 2.3 (DISC-2.3). Journal of the American Academy of Child and Adolescent Psychiatry, 35, 878–888.
Skowyra, K., and Cocozza, J.J. (2006). A blueprint for change: Improving the system response to youth with mental health needs involved with the juvenile justice system. NCMHJJ Research and Program Brief (pp. 1–12).
Snyder, H. N. (2006). Juvenile arrests 2004. Washington, DC: Office of Juvenile Justice and Delinquency Prevention.
Stouthamer-Loeber, M., Loeber, R., & Thomas, C. (1992). Caretakers seeking help for boys with disruptive and delinquent behavior. Comprehensive Mental Health Care, 2, 159–178.
Stouthamer-Loeber, M., Loeber, R., van Kammen, W., & Zhang, Q. (1995). Uninterrupted delinquent careers: The timing of parental help-seeking and juvenile court contact. Studies on Crime and Crime Prevention, 4, 236–251.
Teplin, L. A., Abram, K. M., McClelland, G. M., Dulcan, M. K., & Mericle, A. A. (2002). Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 59, 1133–1143.
US Department of Health and Human Services. (1999). Mental health: A report of the surgeon general. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office of the Surgeon General.
Villagrana, M. (2010). Mental health services for children and youth in the child welfare system: A focus on caregivers as gatekeepers. Children and Youth Services Review, 32, 691–697. doi:10.1016/j.childyouth.2010.01.005.
Wasserman, G. A., Ko, S. J., & McReynolds, L. S. (2004). Assessing the mental health status of youth in juvenile justice settings. Washington, DC: Office of Juvenile Justice and Delinquency Prevention.
Wasserman, G. A., McReynolds, L. S., Ko, S. J., Katz, L. M., & Carpenter, J. R. (2005). Gender differences in psychiatric disorders at juvenile probation intake. American Journal of Public Health, 95, 131–137.
Wasserman, G. A., McReynolds, L., Lucas, C., Fisher, P. I., & Santos, L. (2002). The voice DISC-IV with incarcerated youths: Prevalence of disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 314–321.
Acknowledgments
This work was supported by a Grant to Dr. Burke (MH 074148) from the National Institute of Mental Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burke, J.D., Mulvey, E.P. & Schubert, C.A. Prevalence of Mental Health Problems and Service Use Among First-Time Juvenile Offenders. J Child Fam Stud 24, 3774–3781 (2015). https://doi.org/10.1007/s10826-015-0185-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-015-0185-8