Abstract
Purpose
This study aims to better understand the knowledge and attitudes of men and women internationally towards oocyte cryopreservation (OC).
Methods
An online 25-question survey was distributed internationally via email and social media. Knowledge and attitudes towards OC among different regions and genders were assessed. The study population consisted of adults from North America (NA, 15.7%), Southeastern and Eastern Europe (SE, 34.7%), Central and Western Europe (CWE, 12.7%), Asia (12.7%), and Middle East (ME, 8.9%).
Results
A total of 496 respondents initiated the survey and the completion rate was 80.2%. The mean (SD) age was 35.2 (12.1) years. Over 70% were aware of OC, but only 4.8% had previously undergone the procedure. Most considered ages 26–31 as optimal for OC and correctly identified conditions that could impact the chance of spontaneous conception.
Significant differences were observed regarding etiologies that would render OC acceptable. Only in NA and ME did solid majorities strongly agree that it is acceptable to proceed with OC to allow more time to find the right partner or for professional opportunities. More similar opinions were observed between genders. When medical conditions existed, large majorities across all nationalities and genders strongly agreed that OC is acceptable.
In NA, SE, and ME most respondents would consider or recommend OC for any reason, whereas most respondents in CWE and Asia would do that only for certain social reasons or medical necessity.
Conclusion
A good understanding of OC was observed. Nationality appeared to impact opinions on appropriate indications for this procedure, though overall positive attitudes were documented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As techniques to cryopreserve oocytes have improved in recent years, oocyte cryopreservation for both medical and non-medical (planned) reasons (“social egg freezing”) has increased in use [1,2,3,4,5]. In the USA, cycle numbers are well documented and increased from 2719 oocyte cryopreservation cycles in 2012 to 13,824 cycles in 2018 [6]. Similarly, in the United Kingdom oocyte cryopreservation cycles increased tenfold in the last decade; however, the numbers are still significantly lower compared to the USA [7]. Although less detailed data exists for other countries, oocyte cryopreservation cycles are increasing in the rest of Europe and other parts of the world, as well [8, 9].
Oocyte cryopreservation is an overall safe procedure that is associated with risks from ovarian stimulation, such as ovarian hyperstimulation and ovarian torsion, and the surgical and anesthesia risks of undergoing an egg retrieval [10]. After ovarian stimulation and egg retrieval, mature oocytes are cryopreserved for later use. With the improvement in vitrification technology, treatment outcomes using autologous frozen-thawed oocytes are similar to cycles using autologous fresh oocytes [3, 11]. Importantly, existing studies indicate that few women regret their decision to cryopreserve oocytes [12, 13].
While oocyte cryopreservation for medical reasons, such as imminent treatment with gonadotoxic medications or other fertility impairing procedures, is overall well-received [14], there is debate in the public opinion regarding oocyte cryopreservation for non-medical, or social, reasons (“planned oocyte cryopreservation”) [15, 16]. Additionally, there are countries where planned oocyte cryopreservation is still not permitted [8, 9, 17]. Topics of controversy, among others, include the general concept of reproductive ageing, reproductive autonomy, commercialization, or equality in access [18]. Opinions on these matters can be influenced by sociocultural backgrounds and personal experience with fertility treatments. More discussions regarding the scope and financial responsibility of this procedure arose when large technological companies started to offer oocyte cryopreservation benefits to female employees [19]. In contrast, many health plans of US medical, law, or full-time business schools include no coverage in their health policies [20]. Questions on who is responsible to cover such costs and if access to fertility care is equal for everyone are more relevant than ever.
Previous studies have investigated the knowledge and attitudes of reproductive-age women towards planned oocyte cryopreservation in one or two countries or within a specific demographic group in a country [18, 21,22,23,24,25]. We conducted this study to assess the awareness and attitudes among men and women towards oocyte cryopreservation and its financial burden in multiple different regions.
Materials and methods
The study was approved by the University of Massachusetts Institutional Review Board (STUDY00000261). An online 25-question survey was developed using Qualtrics and distributed via email and social media. Colleagues at our areas of interest used social media platforms, including Twitter, Facebook, and Instagram to distribute the study. Access was open to everyone. The study was disseminated in multiple waves via email outreach and social media posts in multiple waves (approximately monthly during the study enrollment period) to allow adequate participation.
International audiences were targeted focusing on North America (NA; USA, Canada), Southeastern and Eastern Europe (SE; Greece, Cyprus, Russia, Ukraine), Central and Western Europe (CWE; Poland, Germany, United Kingdom, Belgium, France, Italy, Austria, Netherlands), Asia (Japan, China, Malaysia, Taiwan, India, Pakistan), and Middle East (ME; Israel and Turkey). All adults over the age of 18 years old were eligible to participate, regardless of gender identity. Data were collected from July 2022 to March 2023. Participants who did not complete the entire survey were excluded from the analysis.
Participation was voluntary and respondents who desired to participate reviewed an informed consent form prior to initiating the survey. All responses were then collected anonymously. The questionnaire was constructed based on previous research and assessed socio-demographic characteristics, parenthood goals, and knowledge and attitudes regarding oocyte cryopreservation (“egg freezing”). The distributed questionnaire is shown in Fig. 1.
Opinions regarding conditions that make oocyte cryopreservation an acceptable option, according to nationality. a Oocyte cryopreservation to allow more time to find the “right” partner is acceptable. b Oocyte cryopreservation to allow more time for professional opportunities is acceptable. c Oocyte cryopreservation for medical indications is acceptable
Outcome measures included whether respondents knew about oocyte cryopreservation as a procedure, and attitudes towards oocyte cryopreservation among different regions. Differences in these outcome measures between gender identities were also assessed. Factors associated with a positive or negative attitude towards oocyte cryopreservation were explored.
Chi square tests were performed to compare responses among our different groups. The level of statistical significance was set at 0.05. SPSS version 29.0 (Armonk, NY) was used for the statistical analysis.
Results
Study population
The demographic characteristics of our population are shown in Table 1. A total of 496 respondents initiated the survey and the completion rate was 80.2%. The average age was 35.2 (12.1) years. Our population came from SE (34.7%), CWE (27.6%), NA (15.7%), Asia (12.7%), and ME (8.9%). Most of our respondents were white (78.8%), female (73.0%), and had a university or professional degree (94.6%). Approximately 25% of the participants identified as religious, 40% not religious at all, and the remaining 35% as somewhat religious. Over 70% were aware of oocyte cryopreservation, mostly from general knowledge or the media. Nineteen of our participants (4.8%) had previously undergone oocyte cryopreservation without significant differences across nationalities, p = 0.086.
Responses by nationality
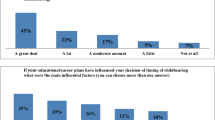
A large proportion of the respondents from SE had completed family building (44.5%), whereas most respondents in other regions were either actively trying to conceive or planning to conceive at some point in the future (p < 0.001). In NA, SE, and Asia participants were approximately split in half regarding their hopes to have their last child when younger or older than 35 years of age. The majority in CWE wished to be ≤ 35 years old when having their last child, whereas the majority in ME wanted to be > 35 years old (68.6%) (p < 0.001). Most respondents regardless of nationality considered ages 26–31 as optimal for oocyte cryopreservation. They also correctly identified medical and surgical complications which could impact the chance of spontaneous conception and justify medical oocyte cryopreservation (> 75%), again irrespective of nationality. Significant differences were observed regarding conditions that would render oocyte cryopreservation an acceptable practice. Only in NA (80.3%) and ME (71.4%) did a solid majority strongly agree with the statement that it is acceptable to proceed with oocyte cryopreservation to allow more time to find the right partner. For SE and CWE respondents, 51.8% and 47.2% strongly agreed, respectively, whereas for Asians the most popular response was “somewhat agree” (48.0%), p < 0.001 (Fig. 1a). A similar trend was observed regarding “egg freezing to allow more time for professional opportunities,” p < 0.001. Although in NA 83.3% and in ME 74.3% strongly agreed, this percentage dropped to 46.3, 41.3, and 52.0 for SE, CWE, and Asia, respectively (Fig. 1b). In contrast, when medical conditions existed, consistently large majorities across all nationalities strongly agreed that oocyte cryopreservation is an acceptable option (Fig. 1c).
Regardless of nationality, most participants agreed that costs should be covered by insurance or national healthcare, especially when there is a medical indication (Fig. 2).
Opinions regarding who is responsible to cover oocyte cryopreservation costs, according to nationality. a Oocyte cryopreservation should be paid by the woman undergoing the procedure. b All oocyte cryopreservation should be paid by insurance or national healthcare. c Oocyte cryopreservation for a medical reason should be paid by insurance or national healthcare
In NA, SE, and ME most participants would consider or recommend to someone they know to proceed with oocyte cryopreservation for any reason (63.9%, 51.6%, and 52.9%, respectively), whereas most respondents in CWE and Asia would do that only for certain social reasons or medical necessity (32.1% and 40.8%, respectively).
All responses by nationality are shown in Supplementary Table 1.
Responses by gender identity
Female- and male-identifying participants had similar future family building hopes and a significant proportion, 55.2% and 48.1%, respectively, was either actively trying to conceive or was considering it at some point in the future (p = 0.272). Likewise, there were similar opinions regarding the age they would like to have their last child (p = 0.721). Female respondents were more likely to know someone who has struggled achieving conception (p = 0.013) and were more familiar with the concept of oocyte cryopreservation (p < 0.001) compared to their male counterparts. Over 60% of both groups considered ages 26–31 as optimal for oocyte cryopreservation and they both correctly identified medical as well as surgical complications which could impact fertility potential.
Only a slightly higher percentage of female respondents (57.5% vs 46.3%, p = 0.04) considered oocyte cryopreservation acceptable to allow more time to find the right partner. Similar opinions were observed in the two groups regarding how acceptable oocyte cryopreservation is in order to allow more time for professional opportunities (p = 0.377) and prior to treatments that could impact natural fecundity (p = 0.798) (Fig. 3).
Overall, similar opinions were recorded with regards to who is responsible for the costs of oocyte cryopreservation. Most participants in all gender identity groups agreed that oocyte cryopreservation should be covered by insurance or national healthcare (p = 0.264), regardless of indication. When a medical reason is present, 80.8% of female respondents strongly believed that oocyte cryopreservation should be covered by insurance or national healthcare in comparison with 68.8% of male respondents (p = 0.019) (Fig. 4).
Additionally, similar responses were documented among males and females when asked if they would consider oocyte cryopreservation or recommend it to someone they know (p = 0.097). The majority in both groups would do so for any reason and the second most common response was for certain social reasons or medical necessity.
All responses by gender identity are shown in Supplementary Table 2.
Discussion
Oocyte cryopreservation is deemed as an ethically permissible means to protect from future infertility due to reproductive aging or other causes [14]. Declining birth rates is a source of increasing concern in the developed world including the USA, the United Kingdom, other Western European countries, and Japan [26]. Along with the widespread fertility decline at younger ages seen in many countries, there is an increasing tendency to delay parenthood [27]. To our knowledge, this is the first study to assess attitudes towards oocyte cryopreservation in an international, all-gender audience.
We aimed to gain additional insights into factors that shape populations’ attitudes towards planned as well as medical oocyte cryopreservation. Most respondents demonstrated a good understanding of oocyte cryopreservation and overall positive responses were documented. Even though in vitro fertilization is now available in most regions around the globe, nationality appeared to influence opinions on some aspects of oocyte cryopreservation more than gender identity did.
Most of the respondents in our sample were aware of oocyte cryopreservation regardless of nationality or gender identity. Similarly, across all nationality and gender identity groups, our participants were well informed of the natural decline in fertility with increasing age as well as about the presence of medical conditions that can impact natural fecundity. These findings likely reflect the rise in dialogue about fertility and reproductive health on social media and in other forums [28,29,30,31].
As expected, given the variation in public policies and culture discourse surrounding reproductive health, we observed differences regarding reasons that would render oocyte cryopreservation as acceptable among different nationalities. Participants from the USA and ME were more approving of oocyte cryopreservation to allow more time to find the right partner or to follow career goals. It is worth mentioning, though, that participants from the other countries maintained an overall positive attitude for planned oocyte cryopreservation for these two reasons. In fact, the percentages of agreement documented in our population were higher compared to a German study [32], but slightly lower compared to other European studies in the literature [22, 33]. It will be interesting to continue to follow attitudes towards oocyte cryopreservation internationally, as its use becomes even more prevalent across the globe.
The decision to proceed with oocyte cryopreservation remains complex and entails the consideration of several factors. The financial burden surely constitutes a major element of this decision-making process. At the same time, initiatives of companies to offer oocyte cryopreservation benefits to female employees have raised criticism regarding possible coercion to delay pregnancy or the hindering of young mothers’ careers [19]. However, prior studies have shown that potential oocyte freezers were not against employer coverage regardless of their personal likelihood to proceed with oocyte cryopreservation and, either way, they would not delay parenthood because of employer coverage of the procedure [34]. In our study, while results were mixed regarding the financial role of the individual, most participants of all nationalities thought that oocyte cryopreservation costs should be covered by insurance companies or national healthcare, especially when there is a medical indication.
As we expected, female respondents were more likely to know someone with difficulties conceiving. They were also more familiar with the concept of oocyte cryopreservation. However, as mentioned above, male participants demonstrated a good understanding of the natural decline in fecundity with ageing and conditions that are associated with infertility. They had similar views on reasons why it would be acceptable to proceed with oocyte cryopreservation as their female counterparts. The majority believed that oocyte cryopreservation is reasonable to allow more time to find the right partner or to pursue professional opportunities. There is only limited literature assessing men’s knowledge on reproductive health and assess their attitudes towards oocyte cryopreservation. Previous reports showed that men looked on planned oocyte cryopreservation less favorably compared to women [32]. Other reports documented an overall positive attitude of male participants towards oocyte cryopreservation, both for medical and for non-medical reasons [33]. In this study most male respondents would recommend oocyte cryopreservation. This is indicative of a more accepting attitude towards oocyte cryopreservation throughout the population as people are becoming more familiar with it.
A significant strength of our study is the inclusion of multiple nationalities and all genders, which to our knowledge have not been previously assessed. The population demonstrated a good knowledge base in fertility-related issues. This allowed us to explore our outcome measures in people of different sociocultural backgrounds and exposure to fertility treatments. There are several limitations as well. Some questions may have been difficult to interpret for certain individuals, given differences in national healthcare systems and insurance policies around the world [35]. Our population could have been larger to increase the power of the study. Additionally, the questionnaire was written in English and was distributed mainly via social media. Inherently, people with limited English competence and those without social media access were not included. This is reflected by the high percentage of the participants with a professional or university degree. Therefore, the documented opinions may not be completely concordant with the more general population of each region. Finally, given the legal and regulatory restrictions on oocyte cryopreservation in different regions, our findings may not universally guide clinical counseling or practice.
The number of oocyte cryopreservation cycles is rising in the USA and elsewhere. Most respondents demonstrated a good understanding of oocyte cryopreservation. Nationality appeared to impact opinions on appropriate indications for this procedure, though overall positive attitudes were documented. Continued research with larger numbers is warranted as the use of oocyte cryopreservation continues to grow and becomes even more prominent around the globe.
Data availability
Data can be available upon request.
References
Johnston M, Richings NM, Leung A, Sakkas D, Catt S. A major increase in oocyte cryopreservation cycles in the USA, Australia and New Zealand since 2010 is highlighted by younger women but a need for standardized data collection. Hum Reprod. 2021;36(3):624–35. https://doi.org/10.1093/humrep/deaa320.
Peate M, Sandhu S, Braat S, Hart R, Norman R, Parle A, et al. Randomized control trial of a decision aid for women considering elective egg freezing: the Eggsurance study protocol. Womens Health (Lond). 2022;18:17455057221139672. https://doi.org/10.1177/17455057221139673.
Argyle CE, Harper JC, Davies MC. Oocyte cryopreservation: where are we now? Hum Reprod Update. 2016;22(4):440–9. https://doi.org/10.1093/humupd/dmw007.
Katler QS, Shandley LM, Hipp HS, Kawwass JF. National egg-freezing trends: cycle and patient characteristics with a focus on race/ethnicity. Fertil Steril. 2021;116(2):528–37. https://doi.org/10.1016/j.fertnstert.2021.02.032.
Kawwass JF, Shandley LM, Boulet SL, Hipp HS. Oncologic oocyte cryopreservation: national comparison of fertility preservation between women with and without cancer. J Assist Reprod Genet. 2020;37(4):883–90. https://doi.org/10.1007/s10815-020-01715-8.
Kawwass JF, Crawford S, Hipp HS. Frozen eggs: national autologous oocyte thaw outcomes. Fertil Steril. 2021;116(4):1077–84. https://doi.org/10.1016/j.fertnstert.2021.05.080.
Calhaz-Jorge C, De Geyter CH, Kupka MS, Wyns C, Mocanu E, Motrenko T, et al. 2020) Survey on ART and IUI: legislation, regulation, funding and registries in European countries: The European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE. Hum Reprod Open. 2020;1(2020):hoz044. https://doi.org/10.1093/hropen/hoz044.
Europe EWGoOCi, Shenfield F, de Mouzon J, Scaravelli G, Kupka M, Ferraretti AP, et al. (2017) Oocyte and ovarian tissue cryopreservation in European countries: statutory background, practice, storage and use. Hum Reprod Open. 2017(1):hox003https://doi.org/10.1093/hropen/hox003
Pai HD, Baid R, Palshetkar NP, Pai A, Pai RD, Palshetkar R. Oocyte cryopreservation — current scenario and future perspectives: a narrative review. J Hum Reprod Sci. 2021;14(4):340–9. https://doi.org/10.4103/jhrs.jhrs_173_21.
Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016;105(2):459-66 e2. https://doi.org/10.1016/j.fertnstert.2015.10.026.
Jones BP, Kasaven L, L’Heveder A, Jalmbrant M, Green J, Makki M, et al. Perceptions, outcomes, and regret following social egg freezing in the UK; a cross-sectional survey. Acta Obstet Gynecol Scand. 2020;99(3):324–32. https://doi.org/10.1111/aogs.13763.
Seyhan A, Akin OD, Ertas S, Ata B, Yakin K, Urman B. A survey of women who cryopreserved oocytes for non-medical indications (social fertility preservation). Reprod Sci. 2021;28(8):2216–22. https://doi.org/10.1007/s43032-021-00460-2.
Ethics Committee of the American Society for Reproductive Medicine. (2018) Electronic address aao, Ethics Committee of the American Society for Reproductive M. Planned oocyte cryopreservation for women seeking to preserve future reproductive potential: an Ethics Committee opinion. Fertil Steril. 110(6):1022–8. https://doi.org/10.1016/j.fertnstert.2018.08.027.
Borovecki A, Tozzo P, Cerri N, Caenazzo L. Social egg freezing under public health perspective: just a medical reality or a women’s right? An ethical case analysis. J Public Health Res. 2018;7(3):1484. https://doi.org/10.4081/jphr.2018.1484.
Bracewell-Milnes T, Norman-Taylor J, Nikolaou D. Social egg freezing should be offered to single women approaching their late thirties: AGAINST: women should be freezing their eggs earlier. BJOG. 2018;125(12):1580. https://doi.org/10.1111/1471-0528.15295.
Chronopoulou E, Raperport C, Sfakianakis A, Srivastava G, Homburg R. Elective oocyte cryopreservation for age-related fertility decline. J Assist Reprod Genet. 2021;38(5):1177–86. https://doi.org/10.1007/s10815-021-02072-w.
Kostenzer J, Bos AME, Bont A, Exel JV. Unveiling the controversy on egg freezing in The Netherlands: a Q-methodology study on women’s viewpoints. Reprod Biomed Soc Online. 2021;12:32–43. https://doi.org/10.1016/j.rbms.2020.09.009.
Ismaili M’hamdi H, Hilhorst M, Steegers EAP, de Beaufort I. (2017) Nudge me, help my baby: on other-regarding nudges. J Med Ethics. 43(10):702–6. https://doi.org/10.1136/medethics-2016-103656.
Gupta S, Amir J, Petersen A, Haider S, York S. Insurance coverage for planned oocyte cryopreservation and infertility across US Medical, Law, and Master of Business Administration schools. Fertil Steril. 2023;120(2):384–5. https://doi.org/10.1016/j.fertnstert.2023.04.025.
Tozzo P, Fassina A, Nespeca P, Spigarolo G, Caenazzo L. Understanding social oocyte freezing in Italy: a scoping survey on university female students’ awareness and attitudes. Life Sci Soc Policy. 2019;15(1):3. https://doi.org/10.1186/s40504-019-0092-7.
Lallemant C, Vassard D, Nyboe Andersen A, Schmidt L, Macklon N. Medical and social egg freezing: internet-based survey of knowledge and attitudes among women in Denmark and the UK. Acta Obstet Gynecol Scand. 2016;95(12):1402–10. https://doi.org/10.1111/aogs.13024.
Stoop D, Nekkebroeck J, Devroey P. A survey on the intentions and attitudes towards oocyte cryopreservation for non-medical reasons among women of reproductive age. Hum Reprod. 2011;26(3):655–61. https://doi.org/10.1093/humrep/deq367.
O’Brien Y, Martyn F, Glover LE, Wingfield MB. What women want? A scoping survey on women’s knowledge, attitudes and behaviours towards ovarian reserve testing and egg freezing. Eur J Obstet Gynecol Reprod Biol. 2017;217:71–6. https://doi.org/10.1016/j.ejogrb.2017.08.024.
Tan SQ, Tan AW, Lau MS, Tan HH, Nadarajah S. Social oocyte freezing: a survey among Singaporean female medical students. J Obstet Gynaecol Res. 2014;40(5):1345–52. https://doi.org/10.1111/jog.12347.
Nargund G. Declining birth rate in developed countries: a radical policy re-think is required. Facts Views Vis Obgyn. 2009;1(3):191–3.
Mills M, Rindfuss RR, McDonald P, te Velde E, Reproduction E, Society Task F. (2011) Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update. 17(6):848-60https://doi.org/10.1093/humupd/dmr026
Skouteris H, Savaglio M. (2021) The use of social media for preconception information and pregnancy planning among young women. J Clin Med. 10(9). https://doi.org/10.3390/jcm10091892.
Sormunen T, Westerbotn M, Aanesen A, Fossum B, Karlgren K. Social media in the infertile community—using a text analysis tool to identify the topics of discussion on the multitude of infertility blogs. Womens Health (Lond). 2021;17:17455065211063280. https://doi.org/10.1177/17455065211063280.
Matsuda S, Aoki K, Tomizawa S, Sone M, Tanaka R, Kuriki H, et al. Analysis of patient narratives in disease blogs on the Internet: an exploratory study of social pharmacovigilance. JMIR Public Health Surveill. 2017;3(1): e10. https://doi.org/10.2196/publichealth.6872.
Sormunen T, Karlgren K, Aanesen A, Fossum B, Westerbotn M. The role of social media for persons affected by infertility. BMC Womens Health. 2020;20(1):112. https://doi.org/10.1186/s12905-020-00964-0.
Schick M, Sexty R, Ditzen B, Wischmann T. Attitudes towards social oocyte freezing from a socio-cultural perspective. Geburtshilfe Frauenheilkd. 2017;77(7):747–55. https://doi.org/10.1055/s-0043-111412.
Wennberg AL, Rodriguez-Wallberg KA, Milsom I, Brannstrom M. Attitudes towards new assisted reproductive technologies in Sweden: a survey in women 30–39 years of age. Acta Obstet Gynecol Scand. 2016;95(1):38–44. https://doi.org/10.1111/aogs.12781.
Ikhena-Abel DE, Confino R, Shah NJ, Lawson AK, Klock SC, Robins JC, et al. Is employer coverage of elective egg freezing coercive?: a survey of medical students’ knowledge, intentions, and attitudes towards elective egg freezing and employer coverage. J Assist Reprod Genet. 2017;34(8):1035–41. https://doi.org/10.1007/s10815-017-0956-9.
Bloom G, Katsuma Y, Rao KD, Makimoto S, Yin JDC, Leung GM. Next steps towards universal health coverage call for global leadership. BMJ. 2019;365:l2107. https://doi.org/10.1136/bmj.l2107.
Acknowledgements
The authors thank all the colleagues who assisted with the distribution of surveys in the different regions as well as all the respondents who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These findings were presented as an abstract in the American Society for Reproductive Medicine (ASRM) Scientific Congress & Expo 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vagios, S., Sun, B., Yeh, J. et al. International attitudes towards medical and planned oocyte cryopreservation. J Assist Reprod Genet 41, 1771–1781 (2024). https://doi.org/10.1007/s10815-024-03116-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03116-7