Abstract
Purpose
We explored and compared perspectives of reproductive endocrinology and infertility specialists (REIs) and in vitro fertilization (IVF) patients regarding polygenic embryo screening (PES), a new type of preimplantation screening that estimates the genetic chances of developing polygenic conditions and traits in the future.
Methods
Qualitative thematic analysis of semi-structured interviews with US-based REIs and IVF patients.
Results
Clinicians and patients often held favorable views of screening embryos for physical or psychiatric conditions, though clinicians tended to temper their positive attitudes with specific caveats. Clinicians also expressed negative views about screening embryos for traits more frequently than patients, who generally held more positive views. Most clinicians were either unwilling to discuss or offer PES to patients or were willing to do so only under certain circumstances, while many patients expressed interest in PES. Both stakeholder groups envisioned multiple potential benefits or uses of PES and raised multiple potential, interrelated concerns about PES.
Conclusion
A gap exists between clinician and patient attitudes toward PES; clinicians generally maintained reservations about such screening and patients indicated interest in it. Clinicians and patients sometimes imagined using PES to prepare for the birth of a predisposed or “affected” individual—a rationale that is often associated with prenatal testing. Many clinicians and patients held different attitudes depending on what is specifically screened, despite the sometimes blurry distinction between conditions and traits. Considerations raised by clinicians and patients may help guide professional societies in developing guidelines to navigate the uncertain terrain of PES.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Polygenic embryo screening (PES), also known as preimplantation genetic testing for polygenic diseases (PGT-P), differs from preimplantation genetic testing for aneuploidies (PGT-A) or monogenic conditions (PGT-M) in meaningful ways.Footnote 1 Compared to PGT-A and PGT-M, PES has the capacity to screen for physical and psychiatric health conditions (e.g., diabetes, depression) as well as physical and cognitive traits (e.g., height, intelligence) [1]. However, PES relies on inherently probabilistic polygenic risk scores, which are not yet standardized [2] and have limited portability to individuals of non-European ancestry [3]. Further, PES may have limited utility in the selection of traits [4], while the potential utility for reducing the risk of disease is more complex [5,6,7].
PES is currently available in the USA and other countries that do not regulate what kind of genetic testing may be conducted on embryos [8]. Though a few professional organizations currently oppose the use of PES [9,10,11,12], uptake of PES will be determined largely by how clinicians, IVF patients, and the public view its potential utility, costs, and harms—at both individual and societal levels. To understand the potential future trajectory of PES, elaborate on the full range of considerations, both for and against the use of PES, and inform relevant guidelines that may be developed by professional societies, this qualitative study is the first to investigate the perspectives of US-based reproductive endocrinology and infertility specialists (REIs) and IVF patients regarding this new type of embryo screening.
Methods
Our multidisciplinary team (bioethicists, social scientists, and statistical geneticists) developed interview guides based on a literature review of PES, including its utility and ethical concerns. Interview questions investigated interests in, potential uses, and concerns about PES (see Supplementary Materials 1 and 2). We piloted the interview guides with two clinicians and two patients and no substantive changes were necessary. Interviews included an explanation of PES with visualizations of mock embryo reports based on published examples from a commercial lab [13]. We intentionally mimicked the types of information that patients would receive to solicit stakeholders’ attitudes and forecast the technology’s potential trajectory. Participants self-reported demographic information, data collection that is required by our funders.
This study was approved by the Baylor College of Medicine Institutional Review Board (IRB), protocol H-49262, with a waiver of written documentation of consent. All participants provided verbal consent and received a US$50 gift card. All semi-structured individual interviews, conducted over internet-secured video calls, were audio-recorded and professionally transcribed.
Recruitment
Between January and December 2022, we recruited clinicians and patients via convenience, random, and snowball sampling until we assessed that we reached “saturation"—the point at which subsequent data collection no longer generated novel insights [14].
Clinician participants were US-based practicing REIs. For convenience sampling, we invited clinician acquaintances known to the research team. For random sampling, we conducted a search of US-based members of the Society for Reproductive Endocrinology and Infertility (SREI) [https://www.socrei.org/sectiondirectory] which resulted in a list of 776 individuals. We used a random number generator to target 250 clinicians and made up to three attempts to invite them to participate.
Patient participants had to be currently undergoing IVF or had done so within the last 5 years. As part of convenience sampling, we invited IVF patient acquaintances known to the research team. To obtain a random sample of IVF patients, we collated a list of 453 fertility clinics across the USA from a public fertility services webpage, which is no longer active [https://cofertility.com/get-to-know-us/], and invited them to post a flyer in their clinics. These flyers gave interested patients instructions for contacting the study team. Five fertility clinics posted the flyer (two each in the West and South, and one in the Midwest).
Analysis
Using thematic analysis [15], we developed a codebook based on deductive themes driven by the interview questions and unanticipated themes generated inductively from the interview data. Using Dedoose, a qualitative analysis program, at least two team members independently coded each transcript. Subsequently, one team member abstracted subthemes from coded excerpts, with a second team member reviewing the abstractions to confirm or discuss and reconcile subthemes [16]. Because concerns were numerous and clustered, we grouped them thematically according to a third level of abstraction [16]. Finally, for each code, one team member developed a memo, highlighting key subthemes and exemplary quotes, and a second team member reviewed it for accuracy and comprehensiveness.
Manuscript development followed Standards for Reporting Qualitative Research [17].
Results
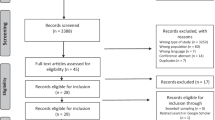
See Fig. 1 for recruitment details. In total, 27 of 235 invited REIs agreed to be interviewed, resulting in an enrollment rate of 11%. Because of our passive approach (i.e., clinic flyers) for patient recruitment, we are unable to report an enrollment rate for patients.
Theoretical saturation was reached by interviewing 27 clinicians and 26 patients. Interviews lasted between 29 and 86 minutes, with an average of 52 minutes for clinicians and 54 minutes for patients. Our sample of mostly White or European-American clinicians was situated across all US regions, working in various practice types, and had a range of 3–40 years of REI experience, with a mean of 21.4 years. Patients were well-educated and wealthy, and most self-identified as female and White or European-American. Many had used or were planning to use preimplantation genetic testing. (For additional demographic details, see Tables 1 and 2.)
The following thematic findings are grouped according to the main topics explored in our interview guides (see Supplementary Materials 1 and 2).
Attitudes about screening for conditions and/or traits
Clinicians and patients often held positive attitudes about screening embryos for physical and psychiatric conditions. However, clinicians tended to temper their positive attitudes with specific caveats, such as limiting embryo screening to conditions that are in one’s family history and/or considered severe. One clinician stipulated, “If there are specific genes or clusters of genes that are highly predictive of a severe, life-threatening disease like breast cancer or other cancers, or families of cancers, I think that that would be reasonable [to screen for in embryos]” (C14).
A minority of clinicians and patients opposed or felt ambivalent about screening for various conditions because of their variable severity, most often discussed with respect to psychiatric conditions (e.g., depression), or concern over how such information would be applied (e.g., discomfort with using it for selection). One such clinician explained,
“I think there are certain people who‘ve been so impacted by [psychiatric conditions], and this is something I’ve had patients, like autism and schizophrenia or severe mental health disorders are two things that I’ve had patients ask me more about because I think it’s really affected their... Whether it was a close family member or friend that they saw suffer, and they really want to avoid that. But then it’s a fine line because where does it become discriminatory almost?” (C17)
In contrast, screening embryos for traits generated greater variation of opinion. Clinicians expressed negative views about screening for traits more often than patients, who generally held more positive views. A minority of both sets of stakeholders were ambivalent about various traits. Intelligence was the most contentious trait; most clinicians who mentioned intelligence were against such screening, whereas most patients who mentioned it favored its screening.
Opposition to screening embryos for traits was largely due to the belief that it is trivial, irrelevant to health or well-being, and/or beyond the role of medical professionals, as well as discomfort with using such information for embryo selection. For instance, one clinician said, “I don’t think [screening embryos for physical traits like height or hair color is] really what I want to be doing as a medical professional in reproductive endocrinology, and it doesn’t really have a role” (C3).
Reasons for favoring screening for traits were largely based on respect for patients’ reproductive autonomy, even when some patients reported they were not interested in doing so themselves. As one patient put it, “I mean, I don’t want to tell people you shouldn’t do that, because if I had the option, I might” (P2).
Some clinicians and patients’ responses, however, suggested that the distinction between conditions and traits can be blurry. They occasionally mentioned obesity or achondroplasia when discussing screening for physical traits, and autism, Down syndrome, or learning disabilities when discussing screening for intelligence. For example, in explaining her stance on embryo screening, one clinician explained,
“Unless there was some genetic reason to suspect for, for example, like achondroplasia or something, I would prefer not to check [embryos] for height, and certainly not color of eyes and hair. Intellectual ability maybe a little bit because I don’t know how you separate things like autism on a spectrum, Asperger’s, et cetera. So intellectual ability maybe, but the others I have a hard time.” (C24)
Clinician reluctance to offer or discuss PES
Most clinicians were either unwilling to discuss or offer PES at this time or were willing to do so only under certain circumstances, most often if the topic was patient-initiated or PES was part of a research study. One clinician said, “I think [PES] is not mainstream medicine right now, so I think it’s very much on the research level. So I would not be comfortable offering it as a clinical service. It seems like it still would be under a research protocol” (C27).
Some clinicians were willing to discuss or offer PES depending on the patient (e.g., those who, from the clinician’s perspective, were statistically savvy or had a compelling personal or family history of a polygenic condition), characteristics of the condition (e.g., untreatable), or external circumstances (e.g., more time for counseling; regulatory approval).
Only a few clinicians were unconditionally willing to offer or discuss PES with patients at this time. One such clinician shared, “I think [PES] would be important information for [patients] to [know]. [… C]an they then take proactive steps to minimize the risk with lifestyle changes and controlling their nutrition and exercise and whatever?” (C24).
Patient interest in PES
Despite clinicians’ hesitancy to offer or discuss PES, all 27 thought that at least some patients would be interested in such screening. Indeed, many patients expressed interest in PES during interviews. One patient said,
“We knew IVF was going to be our way to go and if there [are] tests available, which there is, to minimize health complications for myself, for the baby as well as throughout its lifetime, then more information to me is good information. I can opt to decide which embryo is best depending on the information that I have that science allows today.” (P25)
A few patients were interested in PES depending on various factors, such as financial costs or family history. One such patient said, “I think if it’s not crazy expensive and it doesn’t hurt the embryo any more than just the regular biopsy or the biopsy I already did, then I think it’s fine to get this information” (P14).
Additionally, several patients maintained mixed feelings of interest (particularly for conditions they perceived as serious), tempered with multiple concerns (e.g., negative effects on parenting, the potential for information overload, and boundaries around acceptable uses of PES). One such conflicted patient shared,
“There’s days that I debate with myself with whether or not I’d want a test to see if the little girl would have endometriosis, because it is so painful and I wouldn’t want her to go through that, but then I’m also like, by the time think she’s an adult, maybe we’ll actually have a treatment that’s okay. I’m like, I don’t want to necessarily make decisions like that, but also it’s yeah. It’s one of those ones I go back and forth on for that specifically, but then like other ones, if there’s a for sure chance that the kid is going to be severely, mentally handicapped and they won’t have necessarily a good quality of life, then I potentially want to see if there’s a way that we can see that. Otherwise, probably not just because what are you going to do? What are you going to do with that knowledge?” (P3)
Two patients indicated they had no interest in PES, feeling it was too much information or irrelevant to their embryo selection.
Potential uses of PES information
Though many clinicians perceived PES as potentially beneficial or useful for patients, some clinicians did not mention any potential benefits or uses of PES or said it was not beneficial or useful. In contrast, all 26 patients perceived PES as potentially beneficial or useful for themselves and/or other patients.
Clinicians and patients who envisioned potential benefits of PES often mentioned multiple uses, including selection and/or prioritization of certain embryos, receipt of more information about one’s embryo(s), preparation for the birth of a predisposed or “affected” child, informed reproductive decision-making (i.e., using PES information to select embryos versus prepare for the birth of a certain child), reassurance of an embryo(s)’ lack of predisposition to certain conditions, satisfaction of curiosity, and scientific advancement when conducted for research. Clinicians and patients often portrayed embryo selection and prioritization as a means to (a) having a healthy (genetically related) child, (b) focusing on the “best” embryo, (c) minimizing or preventing a future individual’s risk of developing a health condition, and/or (d) improving society by reducing disease and/or creating “productive” members of society. As one patient explained, “I would want to screen for anything because picking the embryo that has the least predispositions is going to give that child the best chance of a healthy life” (P17).
Furthermore, clinicians and patients considered selection and prioritization most relevant in cases of multiple available embryos and/or predisposition for a condition(s) that was perceived as severe, often in terms of repeated or high morbidity, high/early mortality, compromising quality of life, lack of treatment, early onset, and/or affecting others. In contrast, clinicians and patients considered preparation most relevant in cases of few available embryos, regardless of perceived condition severity. Some clinicians and patients consider a family history of a condition(s) to be either a reason or prerequisite for PES benefit or utility, especially in terms of justifying selection against certain embryos or preparation for the birth of a child with specific genetic predispositions.
Potential concerns about PES
All 27 clinicians and 26 patients raised multiple potential, interrelated concerns about PES during the interview. Each set of thematically grouped concerns is listed in descending order of frequency across the entire sample of clinicians and patients. Notably, concerns over social harms were most numerous and frequent.
Social harms
The most common concern among all participants was the potential for different types of “biases.” Most often, this concern was in relation to embryo selection based on traits. For example, one patient shared, “I guess my only concern [about screening for traits] would be that it would be superficial things would affect the way that I transfer the embryo because then, I’m just being maybe superficial or these things aren’t like super [important]…” (P8). Some clinicians and patients alluded to or specifically raised concerns about eugenics and political or subversive agendas, often referencing Nazi Germany, blue-eyed blonde Aryans, or the creation of a “master race.” These clinicians and patients worried that eugenic practices of selection following PES may (further) divide society or reduce human diversity. Additionally, some clinicians and patients raised concerns over bias inherent in the screening’s metrics (e.g., racial disparities in genome-wide association studies) or the concept of measuring intelligence. Furthermore, a few patients and one clinician worried about potential physician bias in offering or counseling for PES; for example, offering it only to some patients or having personal perceptions influence how they counsel patients.
A common yet less frequent concern among clinicians and patients was the potential for loss of perspective as to what was important in life and/or IVF (e.g., valuing diversity and/or life itself, achieving pregnancy and live birth). Most of these concerns were made with respect to screening for traits, which was often considered trivial. As one patient said, “[… T]hose types of things just feel like it has nothing to do with [the embryo] surviving in your womb. So why even go there?” (P21).
Another common yet less frequent concern among clinicians and patients was the economic aspects of PES. This concern was portrayed most often in terms of its added expense—which ultimately leads to unequal access to the technology—but also how the opportunity for profit drives its development. One clinician proclaimed, “This is all profit-driven. It’s not driven by any kind of science or good medicine or anything else” (C22).
Some clinicians and patients were worried that knowledge about a selected embryo’s chances of developing a health condition or trait may negatively affect the parent–child relationship. Such negative effects may be due to resulting children either not living up to parental expectations or being treated as patients-in-waiting. One clinician said, “[…] I think that’s just dangerous to tell people what’s going to happen in the future when often it won’t happen, no matter how accurate it is. And then they’re going to be disappointed as parents or just have challenges already with their kids” (C7).
Finally, some participants raised concerns about PES’s consumerist aspects (e.g., designing babies; direct-to-consumer marketing) and the potential for PES to serve as a means for enhancement, in terms of creating “super” or “superior” people.
Individual harms
A common concern among clinicians and patients was the potential to harm IVF patients either psychologically or physically. Psychological harm was framed in terms of confusion, stress, or anxiety over PES information and what to do with it; disappointment if expectations are not met; and/or exploitation by companies offering PES. A few clinicians worried about PES’s potential to physically harm patients in cases when they electively seek to undergo IVF, with its associated risks, just to use PES, or undergo additional cycles of IVF to create or maximize embryo options. Such cases were portrayed as excessive. For instance, one clinician said,
“Then, there’s going to be the person who’s just like, ‘Well, I want as perfect of a child as possible. Can we do all these things?’ And those patients often are unrealistic because they’re not infertile and don’t ... It’s hard. Am I putting them more at risk by putting them through this?” (C17)
Several patients, and even more clinicians, raised concerns about the potential for PES to limit or even eliminate embryos that patients perceive as acceptable for transfer. This concern reflected the use of PES for embryo selection in an IVF context where embryo availability is already limited. One patient shared,
“For myself, I just, I feel like there’s so much you could diagnose and if you diagnose everything, you’re not going to end up with [an] embryo that you want because you’re just going to find something wrong with every, every one. So I know that I don’t want to restrict myself from having a family because we can identify it, because we can identify everything.” (P19)
Clinical and technical aspects
A common concern among clinicians and patients was over the uncertain or probabilistic nature of PES. Clinicians particularly worried that this would complicate counseling, especially amid time constraints, and/or lead to excessive IVF in pursuit of the “perfect” embryo. A few clinicians were unsure how to counsel patients about PES and worried about the lack of data and professional guidance on how to do so. One clinician remarked, “[… W]e don’t know if that embryo that scores high will have a severe case, a mild case, a treatable case. We don’t know. I don’t know how I would counsel a patient effectively for that” (C11).
Clinicians’ most common concern, which several patients also shared, was a lack of data, usually with respect to the predictive value or generalizability of PES, because not enough research (e.g., long-term, prospective studies) has been conducted to support its clinical use. One clinician explained, “If you’re testing it embryonic stage, obviously, that has not been done to then follow out through a lifetime to see how it actually plays out. I guess I'm just not as convinced that these polygenic scores are that accurate” (C2). Some clinicians and patients were concerned specifically about a lack of data regarding antagonistic pleiotropy (i.e., genetic variants that lead to multiple phenotypes affecting evolutionary fitness in opposite ways) and/or more generally about the imperfect state of knowledge regarding genetics, human development, and health effects of IVF conception.
Some participants noted the multifactorial nature (i.e., interactions among genes, environment, and lifestyle) of polygenic conditions and traits as challenging the utility of PES for embryo selection. Often, this concern was made in association with screening embryos for cognitive traits (e.g., intelligence) and/or psychiatric conditions. As one patient explained, “It’s still just a percentage. It’s still a risk thing. There’s still so many other things that can go into whether or not they’ll actually have that condition […]” (P3).
Some participants voiced general concerns about the potential of preimplantation genetic screening to physically harm the embryo(s). This was particularly acute for patients who experienced difficulties conceiving or those who ardently valued embryos’ potential for life.
Values and virtues
The concern of PES potentially leading to excessive or unethical embryo discard was common among clinicians but less so among patients. Most clinicians and patients with this concern specifically worried about discarding embryos characterized as “healthy,” “normal,” “fine,” or “viable.” Some clinicians and a few patients were concerned about discard resulting from a strive for perfectionism, which may lead patients to undergo excessive rounds of IVF. One clinician shared, “I would never want, and this is important, for somebody to refuse to take that embryo because of this theoretical risk. That, to me, would be ethically inappropriate. So I would have a very difficult time of participating in that activity” (C20).
Only a few clinicians but more patients felt PES represented a lack of humility in terms of accepting limitations to human control and/or knowledge. Though this concern was most often made with respect to screening (and selection) for traits, it was sometimes made regarding PES in general or screening for (and selection against) health conditions. One patient commented, “Man, science is crazy. I’m like, ‘Should we even know this information?’” (P23).
Parameters and governance
A rather common concern among clinicians, but not as much for patients, was difficulty in setting limits as to what is acceptable to screen for in embryos and who should be permitted to use PES. Some clinicians and patients felt that screening embryos to select against those with increased genetic risk for manageable or treatable conditions was inappropriate because individuals at increased risk or even with the condition can lead fulfilling and healthy lives. One clinician elaborated,
“I happen to know many people who are perfectly healthy, otherwise, type 1 diabetics who are managed well and know that there are scientific discoveries that could end up curing type one diabetes. […] I’ve known many people who’ve had breast cancer and been treated for it, or have had high risk for breast cancer with BRCA1 and BRCA2, and had the treatment for that and live very full lives. I do not think that this needs to go into the decision making when somebody’s trying to have a child.” (C15)
Additionally, some felt that screening embryos to select against those with (increased genetic risk for) conditions with (a) adult onset is problematic because of the decades required for studies to validate the data and the potential for medicine to develop treatments by the time of onset or (b) low (absolute or relative) risk may not be worthwhile, considering the potential to modify such risk(s) via environment or lifestyle.
Furthermore, several clinicians and patients noted the ever-changing contextual nature of classifying some traits as desirable and selecting embryos based on their likelihood for developing them. One patient said, “Because in a given culture height, might be valuable. If you were to move to another culture where height is not valued, you made this choice for another human being sometime in the past based on current social standards that may not translate throughout their life” (P24).
Several clinicians felt embryo selection based on PES, particularly for traits, was not part of a physician’s role, which is focused on treating disease. As one clinician put it, “We’re not here to create what we think is, or what the patient thinks is ideal. We’re here to help them with a medical condition, which is infertility” (C1). Hence, facilitating such selection would be beyond their medical scope.
A few participants worried about potential liability issues when selected embryos do not meet IVF patients’ expectations for their eventual children (e.g., of developing certain traits or not developing certain conditions). One clinician remarked,
“I mean, inevitably, how many lawsuits are going to happen because you’ve supposedly chose an embryo that’s going to be tall, beautiful, and smart, and they’re short, squat, thick, and a little dull. Are the parents going to sue the companies, the IVF facilities because their child didn’t meet their expectations?” (C20)
Discussion
This study, which is the first to compare clinician and patient perspectives of PES, yielded several noteworthy findings. First, there appears to be a gap between clinician and patient attitudes toward PES, whereby clinicians generally maintained reservations about such screening and patients indicated interest in it. This finding aligns with recent studies of American and European healthcare professionals’ attitudes toward PES [18, 19], American IVF patients’ increasing use of preimplantation genetic testing [20], high acceptance of PES [21], and high uptake of PES when offered at no additional financial cost to patients that used PGT-A [22]. Moreover, REIs’ greatest concern about the lack of available data to support PES may reflect their perceptions of the controversial widespread clinical implementation of PGT-A, which some have argued was premature [23, 24].
Our findings suggest that the gap between clinician and patient attitudes toward PES may be due to differences in stakeholder values and roles. Patients tended to perceive the use of PES as a form of reproductive autonomy, which they primarily valued and respected. Though clinicians recognized the importance of respecting their patients’ reproductive autonomy, they also felt compelled to protect patients from what they perceived to be PES’s potential downsides. Therefore, clinician perspectives illustrate a tension between the biomedical principles of respect for autonomy and beneficence/non-maleficence [25].
Interestingly, though PES is marketed and usually discussed as a tool for embryo selection [7], we found that clinicians and patients sometimes envisioned PES being used to prepare for the birth of a predisposed or “affected” individual. Although the intentional or incidental transfer of embryos with pathogenic variants detected in preimplantation testing is rare [26], preparation has not been reported previously as a motivation or decisional factor for using preimplantation genetic testing [27]. However, preparation has been considered a benefit or use of prenatal testing [28]. Thus, a conflation between prenatal and preimplantation genetic testing may be a factor contributing to these comments. Considering clinicians’ and patients’ concerns that embryo selection based on PES promotes eugenic thinking or practices, social desirability may be another factor contributing to these comments. Further research is warranted to determine whether PES’s potential for preparation reflects a real or theoretical use of the screening information.
Another notable finding is the difference in opinion between screening embryos for conditions versus traits among both clinicians and patients, with far less support for traits. This finding aligns with previously measured stances of ASRM’s Ethics Committee regarding embryo sex disclosure and selection [29, 30] and previous studies of pregnant women’s perspectives of noninvasive prenatal testing and whole genome sequencing [31, 32]. Yet, some clinicians’ and patients’ references to certain conditions while discussing screening for traits blurred the distinction between these two categories. Considering such fluidity and clinicians’ concern that PES extends beyond their medical purview, perhaps it may be more apt to consider PES in terms of screening embryos for health-related and non-health-related traits, especially when deliberating on the potential guidance for it.
Relatedly, severity and definitions of health loom large in discussions of PES. Previous studies report condition severity is a main factor in deciding whether to use preimplantation genetic testing, and the ability to control or improve the health of one’s future child(ren) is the main motivation for using it [27, 33]. However, the constitution of severity and health is debatable [34,35,36,37]. Though some scholars believe consensus on defining these terms is impossible [38], others propose developing an adaptable framework that incorporates biomedical, social, and personal meanings [39]. Either way, the prospect of PES invites clinicians, IVF patients, and all of society to contemplate the meanings of these concepts.
Limitations
This qualitative study’s findings may be limited by social desirability response bias (i.e., answering questions in a manner that will be viewed favorably by others) and self-selection bias. Thus, its generalizability to other REIs and IVF patients may be limited. Furthermore, it is important to note that though this study explores the perspectives of REIs and IVF patients, there are other stakeholders, such as genetic counselors, whose perspectives may diverge from those reported here.
Conclusion
Despite patients’ interest in PES, clinicians feel such screening is premature for clinical application. Though now embryos can be screened for their genetic chances of developing polygenic conditions and traits, many clinicians and patients maintain different attitudes depending on what is specifically screened, even though the distinction between conditions and traits is not always clear-cut. This dual-use aspect will prove challenging for governing PES. Professional societies are best positioned to develop guidelines for navigating the uncertain terrain of PES, which is already commercially available. Moreover, there should be greater discussion within medicine and society over the meanings of “severe” and “health.”
Data availability
De-identified coded transcript excerpts will be made available upon reasonable request to the corresponding author.
Notes
While we recognize that the socio-ethical implications of this technology are similar to those of other types of preimplantation genetic tests, our use of the acronym PES (vs. PGT-P) highlights its clinical and technical differences from other types of preimplantation genetic tests.
References
Lázaro-Muñoz G, Pereira S, Carmi S, Lencz T. Screening embryos for polygenic conditions and traits: ethical considerations for an emerging technology. Genet Med. 2021;23:432–4. https://doi.org/10.1038/s41436-020-01019-3.
Wand H, Lambert SA, Tamburro C, et al. Improving reporting standards for polygenic scores in risk prediction studies. Nature. 2021;591, 211–219. https://doi.org/10.1038/s41586-021-03243-6.
Duncan L, Shen H, Gelaye B, et al. Analysis of polygenic risk score usage and performance in diverse human populations. Nat Commun. 2019;10:3328. https://doi.org/10.1038/s41467-019-11112-0.
Karavani E, Zuk O, Zeevi D, et al. Screening human embryos for polygenic traits has limited utility. Cell. 2019;179:1424-1435.e8. https://doi.org/10.1016/j.cell.2019.10.033.
Lencz T, Backenroth D, Granot-Hershkovitz E, et al (2021) Utility of polygenic embryo screening for disease depends on the selection strategy. Elife 10. https://doi.org/10.7554/eLife.64716.
Treff NR, Eccles J, Marin D, et al (2020) Preimplantation genetic testing for polygenic disease relative risk reduction: evaluation of genomic index performance in 11,883 adult sibling pairs. Genes (Basel) 11. https://doi.org/10.3390/genes11060648.
Turley P, Meyer MN, Wang N, et al. Problems with using polygenic scores to select embryos. N Engl J Med. 2021;385:78–86. https://doi.org/10.1056/NEJMsr2105065.
Bayefsky M. Who should regulate preimplantation genetic diagnosis in the United States? AMA J Ethics. 2018;20:1160–7.
Abu-El-Haija A, Reddi HV, Wand H, et al (2023) The clinical application of polygenic risk scores: a points to consider statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med 25. https://doi.org/10.1016/j.gim.2023.100803.
Wand H, Kalia SS, Helm BM, et al. Clinical genetic counseling and translation considerations for polygenic scores in personalized risk assessments: a practice resource from the National Society of Genetic Counselors. J Genet Couns. 2023;32:558–75. https://doi.org/10.1002/jgc4.1668.
Forzano F, Antonova O, Clarke A, et al. The use of polygenic risk scores in pre-implantation genetic testing: an unproven, unethical practice. Eur J Hum Genet. 2022;30:493–5. https://doi.org/10.1038/s41431-021-01000-x.
European Society of Human Reproduction and Embryology (2022) ESHRE supports the position of ESHG on embryo selection based on polygenic risk scores. https://www.eshre.eu/Europe/Position-statements/PRS. Accessed 23 Aug 2023.
Regalado A. The world’s first Gattaca baby tests are finally here. MIT Technol Rev. 2019. https://www.technologyreview.com/2019/11/08/132018/polygenic-score-ivf-embryo-dna-tests-genomic-prediction-gattaca/. Accessed 23 Aug 2023.
Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–907. https://doi.org/10.1007/s11135-017-0574-8.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. https://doi.org/10.1191/1478088706qp063oa.
Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108:103632. https://doi.org/10.1016/j.ijnurstu.2020.103632.
O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. https://doi.org/10.1097/ACM.0000000000000388.
Siermann M, Valcke O, Vermeesch JR, et al. Limitations, concerns and potential: attitudes of healthcare professionals toward preimplantation genetic testing using polygenic risk scores. Eur J Hum Genet. 2023. https://doi.org/10.1038/s41431-023-01333-9.
Terek ST, Gamma A, Zak M, Butts H. Preimplantation testing of embryos for polygenic related conditions: the ethical concerns surrounding it and the position of genetic counselors. Fertility and Sterility. 2021;116(3):e56. https://doi.org/10.1016/j.fertnstert.2021.07.159.
Roche K, Racowsky C, Harper J. Utilization of preimplantation genetic testing in the USA. J Assist Reprod Genet. 2021;38:1045–53. https://doi.org/10.1007/s10815-021-02078-4/Published.
Neuhausser WM, Fouks Y, Lee SW, et al (2023) Acceptance of genetic editing and of whole genome sequencing of human embryos by patients with infertility before and after the onset of the COVID-19 pandemic. Reprod Biomed Online. 47. https://doi.org/10.1016/j.rbmo.2023.03.013.
Eccles J, Marin D, Duffy L, et al (2021) Rate of patients electing for polygenic risk scores in preimplantation genetic testing. In: Fertility and sterility. Elsevier BV, pp e267–e268.
Gleicher N, Patrizio P, Brivanlou A. Preimplantation genetic testing for aneuploidy – a castle built on sand. Trends Mol Med. 2021;27:731–42. https://doi.org/10.1016/j.molmed.2020.11.009.
Mastenbroek S, De Wert G, Adashi EY. The imperative of responsible innovation in reproductive medicine. N Engl J Med. 2021;22:385.
Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York: Oxford University Press; 2013.
Ethics Committee of the American Society for Reproductive Medicine. Transferring embryos with genetic anomalies detected in preimplantation testing: an ethics committee opinion. Fertil Steril. 2017;107:1130–5. https://doi.org/10.1016/j.fertnstert.2017.02.121.
Hughes T, Bracewell-Milnes T, Saso S, et al. A review on the motivations, decision-making factors, attitudes and experiences of couples using pre-implantation genetic testing for inherited conditions. Hum Reprod Update. 2021;27:944–66. https://doi.org/10.1093/humupd/dmab013.
Michie M. Is preparation a good reason for prenatal genetic testing? Ethical and critical questions. Birth Defects Res. 2020;112:332–8.
Ethics Committee of the American Society for Reproductive Medicine. Disclosure of sex when incidentally revealed as part of preimplantation genetic testing (PGT): an ethics committee opinion. Fertil Steril. 2018;110:625–7. https://doi.org/10.1016/j.fertnstert.2018.06.019.
Ethics Committee of the American Society for Reproductive Medicine. Use of reproductive technology for sex selection for nonmedical reasons: an ethics committee opinion. Fertil Steril. 2022;117:720–6. https://doi.org/10.1016/j.fertnstert.2021.12.024.
Bowman-Smart H, Savulescu J, Mand C, et al. “Is it better not to know certain things?”: views of women who have undergone non-invasive prenatal testing on its possible future applications. J Med Ethics. 2019;45:231–8. https://doi.org/10.1136/medethics-2018-105167.
Sullivan HK, Bayefsky M, Wakim PG, et al. Noninvasive prenatal whole genome sequencing: pregnant women’s views and preferences. Obstet Gynecol. 2019;133:525–32. https://doi.org/10.1097/AOG.0000000000003121.
Zhang J, Pastore LM, Sarwana M, et al. Ethical and moral perspectives of individuals who considered/used preimplantation (embryo) genetic testing. J Genet Couns. 2022;31:176–87. https://doi.org/10.1002/jgc4.1471.
Wertz DC, Knoppers BM. Serious genetic disorders: can or should they be defined? Am J Med Genet. 2002;108:29–35.
Wasserman D, Asch A, Blustein J, Putnam D. "Disability: health, well-being, and personal relationships". In: Zalta EN, editor. The stanford encyclopedia of philosophy (summer 2022 edition). 2016. https://plato.stanford.edu/archives/sum2022/entries/disability-health/.
Murphy D. "Concepts of disease and health". In: Zalta EN, Nodelman U, editors. The stanford encyclopedia of philosophy (fall 2023 edition). 2020. https://plato.stanford.edu/archives/fall2023/entries/health-disease/.
Huber M, Knottnerus JA, Green L, et al. Health: how should we define it? Br Med J. 2011;343:235–7.
Chen SC, Wasserman DT. A framework for unrestricted prenatal whole-genome sequencing: respecting and enhancing the autonomy of prospective parents. Am J Bioeth. 2017;17:3–18. https://doi.org/10.1080/15265161.2016.1251632.
Kleiderman E, Rahimzadeh V, Knoppers B, et al. The serious factor in expanded prenatal genetic testing. Am J Bioeth. 2022;22:23–5. https://doi.org/10.1080/15265161.2021.2013991.
Acknowledgements
The authors thank the REIs and IVF patients that participated in this study, as well as Jason Bach, Arturo Balaguer, Jonathan Frumovitz, and Page Trotter for their assistance with data analysis and Ana Battaglino for her feedback on the manuscript.
Funding
This work was supported by National Human Genome Research Institute, R01HG011711, Todd Lencz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SC is a paid consultant at MyHeritage. All other co-authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barlevy, D., Cenolli, I., Campbell, T. et al. Patient interest in and clinician reservations on polygenic embryo screening: a qualitative study of stakeholder perspectives. J Assist Reprod Genet 41, 1221–1231 (2024). https://doi.org/10.1007/s10815-024-03074-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03074-0