Abstract
Purpose
To evaluate live birth rates (LBRs) for in vitro fertilization (IVF) cycles with ≤5 follicles at trigger, with the goal of helping patients with low follicle counts decide whether to proceed to retrieval.
Methods
This is a retrospective cohort study from an urban, university-affiliated fertility center. All IVF cycles that yielded <10 oocytes between 2016 and 2020 were reviewed. Cycles were included if <5 follicles measuring >14 mm were verified on trigger day. The primary outcome was LBR per retrieval after fresh or frozen transfer. Secondary outcomes were number of oocytes, mature oocytes, 2-pronuclear zygotes (2-PNs), blastocysts for transfer/biopsy, and euploid blastocysts (if preimplantation genetic testing for aneuploidy (PGT-A) was used).
Results
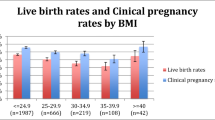
1502 cycles (900 with PGT-A) from 972 patients were included. Mean number of oocytes, mature oocytes, 2-PNs, blastocysts for transfer/biopsy, and euploid blastocysts differed by follicle number (p < 0.001). Across all age groups, there were differences in LBR associated with follicle number (p < 0.001). However, within age groups, not all results were significant. For example, for patients <35 years, LBR did not differ by follicle number and among patients 35–37 years; LBR with two or three follicles was lower than with five (p < 0.02). LBR for patients 35–40 years was <20% with 1–3 follicles and 25–40% with 4–5 follicles. LBR for patients >41 years was <5% with 1–3 follicles and <15% with 4–5 follicles.
Conclusion
As expected, LBR is higher with more follicles. Providing patients with <5 follicles with specific data can help them weigh the emotional, physical, and financial costs of retrieval.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In vitro fertilization patients (IVF) with five or fewer follicles at the time of trigger face a difficult choice: should they cancel or proceed with oocyte retrieval? Patients with a low follicle count often consider cancelling because their cycles may be less likely to result in live birth, and oocyte retrieval is uncomfortable and poses surgical risks. Furthermore, many patients have limited or no insurance coverage for IVF and oocyte retrieval is costly [1]. However, by the time these patients reach trigger and are faced with this decision, they have already made significant financial, time, and emotional investments in their cycle. Moreover, there is no guarantee they will have an improved response to ovarian stimulation in a future cycle. Thus, the decision of whether to cancel or proceed to oocyte retrieval with a low follicle count is very personal. Nevertheless, if physicians are armed with relevant and accurate data, they can better guide patients as they navigate this challenging decision.
At present, limited data are available to help counsel patients with five or fewer follicles, as existing studies have focused on patients with three or fewer follicles. Klinkert et al. found that approximately 30% of patients with three or fewer follicles after stimulation chose to cancel their cycles [2]. Biljan et al. compared outcomes for patients with three or fewer follicles to outcomes for patients with more than three follicles [3]. They identified similar live birth rates (LBRs) per cycle started for patients younger than 40 years old, and a non-significant trend towards lower LBRs per cycle started for women aged 40 years or older with three or fewer follicles. However, this study had a very small number of patients with three or fewer follicles who proceeded to retrieval. Shrem et al. examined LBRs among women with one or two follicles on the day of trigger [4]. They found increases in LBR with lower patient age and higher follicle counts. Reichman et al. compared patients with three or fewer follicles who either chose to continue with oocyte retrieval or convert to intrauterine insemination (IUI) [5]. They found an advantage to oocyte retrieval for patients with two or three follicles but not one follicle. However, patients in the study with three follicles were encouraged to proceed with oocyte retrieval, and patients with one follicle were encouraged to pursue IUI, introducing bias. None of these studies incorporate the use of preimplantation genetic testing for aneuploidy (PGT-A), which is increasingly utilized in modern assisted reproduction practices.
While current data may inform patients with a low (three or fewer) follicle count, to our knowledge, there are no studies examining outcomes for patients in a greyer area, with four or five follicles at trigger. For these women, it is more challenging to decide whether oocyte retrieval is worthwhile, or cancellation is more prudent. Therefore, our aim was to evaluate LBRs for women with five or fewer follicles at the time of trigger, with the goal of providing data for clinicians to counsel their patients with low follicle counts at trigger about whether to cancel or proceed with oocyte retrieval. Secondarily, we also investigated number of oocytes, M2s, 2PNs, blastocysts available for transfer or biopsy, and euploid blastocysts.
Material and methods
Design
With an Institutional Review Board approval (NYU Grossman School of Medicine #S13-00389), we performed a retrospective cohort study of all IVF cycles performed between January 2016 and December 2020.
Subjects
All patients who started an IVF cycle at our center that yielded ten or fewer oocytes during the study period were reviewed. Study participants were identified in this manner because our electronic medical record does not permit a search based on follicle number at trigger. It was therefore assumed that if five or fewer follicles were present at trigger, it was unlikely that greater than ten oocytes were obtained at retrieval. Cycles were included if five or fewer follicles measuring greater than or equal to 14 mm were verified on the day of trigger, and the cycle proceeded to retrieval. The size 14 mm or greater was chosen in order to be consistent with prior studies [3, 5]. Cycles involving oocyte donors or that were intended for oocyte cryopreservation or embryo banking were excluded. PGT-A is offered routinely at our center to all IVF patients, risks and benefits are discussed, and patients decide whether to proceed. No exclusion criteria based on age or infertility diagnosis were applied but cycles without known pregnancy outcomes were excluded. Cycles that did not result in oocyte retrieval were also excluded. Multiple cycles from the same patient were included. Cycles that had not resulted in live birth but had resulted in remaining untested or euploid embryos available for transfer at the time of data collection were excluded from LBR analysis because there were additional embryos that could result in live birth that patients had not utilized. However, these cycles were included for analysis of secondary outcomes and cycle characteristics, which involved information leading up to transfer.
Variable and data collection
Data were collected from the electronic medical record between January and April 2022. Collected data included age at cycle start in years, anti-mullerian hormone (AMH) level in nanograms per milliliter, day two or three follicular follicle stimulating hormone (FSH) level in milli-international units per milliliter, estradiol level on day of trigger in picograms per milliliter, total gonadotropins dose in international units, protocol type (gonadotropin-releasing hormone (GnRH) antagonist, GnRH antagonist with clomiphene citrate, microdose leuprolide acetate, or microdose leuprolide acetate with clomiphene citrate), number of stimulation days, number of oocytes retrieved, number of metaphase II oocytes (M2s) retrieved, number of 2PNs, number of blastocysts available for transfer or biopsy, number of euploid blastocysts (if PGT-A was used), and live birth outcomes. Cycles were in the “non-PGT-A group” if PGT-A was not performed on any of the embryos. Cycles in the PGT-A group had PGT-A performed for all non-fresh transfers.
The primary outcome was LBR. LBR was defined as the rate of at least one live birth per retrieval after fresh and/or frozen embryo transfer. In other words, live birth was a binary outcome, and more than one live birth from a single retrieval cycle (either multiples or multiple singleton births) was counted as a single live birth event. Patients may have had multiple transfers, both fresh and frozen, associated with a single retrieval. The secondary outcomes were number of oocytes, M2s, 2PNs, blastocysts available for transfer or biopsy, and euploid blastocysts.
Statistical analysis
Age at cycle start was subdivided into the Society for Assisted Reproductive Technologies (SART) age groups and treated as categorical data. Medians with the 25th–75th percentile interquartile ranges (IQRs) were used to describe the following variables because they were found to be not normally distributed by the Kolmogorov-Smirnoff test: age, AMH level, early follicular FSH level, estradiol level on day of trigger, total gonadotropins dose, and number of stimulation days. The Kruskal Wallis test was used to assess for differences by follicle number for these variables, and a post hoc analysis was performed to confirm differences between groups to a p-value of <0.05. Oocytes, M2s, 2PNs, blastocysts available for transfer or biopsy, and euploid blastocysts were represented as means with standard deviations after determining that they fit a Poisson distribution. Differences in these variables were analyzed with the chi-square test. LBR by follicle number was also analyzed using the chi-square test when the expected number in a category was greater than or equal to five and Fisher’s exact test when at least one expected value was less than five. Given that some subjects had more than one cycle included, a robust sandwich standard error was used for comparisons of means and proportions as well as a robust regression to confirm the analyses. An alpha error of 0.05 was deemed significant.
Results
In total, 1502 IVF cycles from 972 patients were included (Fig. 1). During the study period, there were 239 IVF cycles that resulted in 1, 2, 3, 4, or 5 follicles and were cancelled prior to retrieval; these cycles were excluded from analysis. The median age of all included patients at the time of cycle start was 40 years (range, 26–48). By SART age group, 10% (155/1502) of cycles were among patients younger than 35 years, 17% (254/1502) were among patients aged 35–37 years, 27% (407/1502) were among patients aged 38–40 years, 25% (379/1502) were among patients aged 41–42 years, and 20% (307/1502) were among patients older than 42 years. Median age differed significantly by follicle number (p < 0.001), but there were no differences in total gonadotropin dose (p = 0.25) or number of stimulation days (p = 0.68) based on follicle number (Table 1). There were also no differences in stimulation protocol types based on follicle number (p = 0.31).
Overview of in vitro fertilization cycles, embryo transfers and live birth rates. All fresh transfers were of untested embryos, including in the PGT-A group (PGT-A was performed on all other embryos from those cycles). Asterisks (*) indicate cycles excluded from live birth rate analysis. PGT-A, preimplantation genetic testing for aneuploidy; LB, live birth
PGT-A was performed in 900 of the 1502 cycles (59.9%). Among cycles with PGT-A, 329 (36.6%) had at least one euploid blastocyst available for transfer, and among cycles without PGT-A, 217 (36.0%) had at least one untested blastocyst available for transfer. By the time of data extraction, 467 cycles resulted in at least one transfer, 237 cycles (50.7%) resulted in euploid embryo transfers only, 210 cycles (45.0%) resulted in untested embryo transfers only, 18 cycles (3.9%) resulted in mosaic embryo transfers only, one cycle (0.2%) resulted in an untested embryo transfer and a euploid embryo transfer, and one cycle (0.2%) resulted in both a mosaic embryo transfer and a euploid embryo transfer (mosaic embryo was transferred first for sex selection purposes, followed by a euploid embryo from the same retrieval). Among the 19 cycles that resulted in mosaic embryo transfers, 18 had no euploid embryos available.
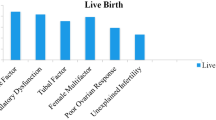
A total of 1384 cycles from 913 patients, 807 of which involved PGT-A (58%), were included in the LBR analysis. These cycles either resulted in live birth (n = 225) or had no remaining euploid or untested blastocysts available for transfer (n = 1159). A total of 118 of 1502 cycles were excluded from the live birth analysis because they did not result in live birth but produced euploid or untested blastocysts that had not yet been transferred at the time of data collection. Of the 196 cycles that involved fresh transfers, there were 41 live births from the fresh transfers. Of the 289 cycles with frozen transfers (including cycles with both fresh and frozen and mosaic embryo transfers), there were 182 live births from the frozen transfers. There were differences in LBR associated with follicle number across all ages combined (p < 0.001) (Table 2, Fig. 2). Overall, LBR was 4% (2/48) for cycles with one follicle, 8% (17/206) for cycles with two follicles, 10% (30/315) for cycles with three follicles, 18% (70/393) for cycles with four follicles, and 25% (106/422) for cycles with five follicles. However, for patients younger than 35 years old, there were no significant differences in LBR by follicle number. In the 35- to 37-year-old age group, LBR with two or three follicles was lower than LBR with five (p < 0.02). In the 38- to 40-year-old group, LBR with three follicles was lower than LBR with four or five follicles (p < 0.02). In the 41- to 42-year-old age group, LBR with two or three follicles was lower than LBR with five follicles (p < 0.03). In the greater than 42-year-old age group, LBR with four follicles was lower than LBR with five (p < 0.03). There were no other differences in LBR by follicle number.
There were 787 PGT-A cycles with at least one blastocyst that either resulted in live birth or had no remaining euploid blastocysts. The cumulative LBR from these PGT-A cycles was 22.4% (176/787). In contrast, there were 206 non-PGT-A cycles with at least one blastocyst that either resulted in live birth or had no remaining blastocysts. The cumulative LBR from these non-PGT-A cycles was 23.8% (49/206). The cumulative LBRs were not significantly different between the PGT-A and non-PGT-A cycles (p = 0.71).
With regard to secondary outcomes, mean number of oocytes, M2s, 2PNs, blastocysts available for transfer or biopsy, and euploid blastocysts all differed significantly by follicle number (p < 0.001) (Table 3). For cycles with one follicle at the time of trigger, 12% (n = 6/50) of cycles had no oocytes retrieved. This number decreased to 5% (n = 11/217) for patients with two follicles, 0% (n = 0/341) for patients with three follicles, 0.4% (n = 2/435) for patients with four follicles, and 0% (n = 0/459) for patients with five follicles. With regard to euploid or untested blastocysts available for transfer, we found that for cycles with one follicle present at trigger, 18% (n = 9/50) resulted in at least one euploid or untested blastocyst. This rate increased to 25% (n = 55/217) for cycles with two follicles, 33% (n = 112/341) for cycles with three follicles, 40% (n = 176/435) for cycles with four follicles, and 44% (n = 201/459) for cycles with five follicles.
Discussion
The concept of “poor ovarian response” was established in 2011 in order to define a population of patients who are likely to obtain a small number of oocytes at retrieval [6, 7]. Because patients who fit the description of a poor ovarian responder are counseled that they are likely to obtain few oocytes if they proceed to retrieval [8], they often inquire about the chance of live birth. After all, live birth, not a certain number of oocytes, is the outcome that is most important for patients [9]. Moreover, some patients might have a reasonable antral follicle count and AMH and nonetheless have five or fewer oocytes at trigger. Thus, detailed, specific data regarding LBR per retrieval for patients with five or fewer follicles at the time of trigger is crucial.
According to the findings of this study, patients older than 41 years can be counseled that live birth rate is likely less than 5% with one to three follicles and less than 15% with four or five follicles. Patients aged 35–40 years can be counseled that LBR is likely less than 20% with one to three follicles and 25–40% with four or five follicles. While our sample size for patients under 35 years old is small and the confidence intervals for their LBRs are large, our data suggest that patients younger than 35 can expect a LBR of approximately 25–30% with one to three follicles and 40% with four or five follicles. Our data on this topic provide patients with realistic expectations and empower them to make informed decisions.
The LBRs in our study for patients with one, two, or three follicles were overall similar to LBRs reported in the literature. For example, Reichman et al. found that for patients aged 40 years or younger, LBR for one follicle was 4.5%, LBR for two follicles was 14.1%, and LBR for three follicles was 19.3%. For patients older than 40 years old, LBR for one follicle was 0%, LBR for two follicles was 3.7%, and LBR for three follicles was 4.0%. Shrem et al. found that for patients with one or two follicles, LBR was 15.6% for patients aged 34 years or younger, 6.5% for patients aged 35–39 years old, and 2.7% for patients aged 40 years or older [4]. Furthermore, for reference, LBRs for patients with five follicles in our cohort were similar to SART-reported LBR per intended retrieval from our clinic for all patients (45.7% for patients <35 years old, 37.8% for patients 35–37 years old, 23.4% for patients 38–40 years old, 13.4% for patients 41–42 years old, and 6.1% for patients >42 years old) [10]. For patients with four or fewer follicles, LBRs were lower in our cohort relative to SART-reported LBRs for our clinic.
We found that, as expected, LBR increased with increasing follicle number across all age groups. However, among patients less than 35 years, LBR did not differ significantly by follicle number. It is unclear whether there were no significant differences noted in this age group because of superior oocyte quality in younger patients or because of an insufficient sample size to detect differences. Biljan et al. also found that younger women had similar pregnancy rates despite a lower number of oocytes retrieved, as compared to women aged 40 or older [3]. However, their study had a very small sample size and may have been underpowered to detect differences between age groups. In our study, there were some significant differences in LBR by follicle number in patients aged 35 or above. Similarly, across all age groups combined, mean number of oocytes, M2s, 2PNs, blastocysts available for transfer or biopsy, and euploid blastocysts decreased by decreasing follicle number. On average, we found that there were more oocytes than follicles (Table 3), which is likely because we counted follicles sized 14 mm or greater in order to align with prior studies, but it is possible to harvest oocytes and M2s from smaller follicles. We also found that cumulative live birth rates were equivalent in PGT-A and non-PGT-A cycles. Thus, unlike other studies suggesting that PGT-A may be detrimental to LBR [11, 12] or could improve LBR in older age groups [13], there was no evidence in our cohort that PGT-A increased or decreased the chance of live birth among patients with a low follicle count.
For patients with a small number of follicles, an alternative to cancelling the cycle altogether is conversion from IVF to IUI. Data are mixed on whether conversion to IUI results in the same LBR as proceeding with retrieval. A systematic review by Fujii et al. found that when patients had two or more follicles, oocyte retrieval resulted in no difference in clinical pregnancy rate, but a higher LBR [14]. However, the authors of this study noted a high degree of heterogeneity among included studies, and not all the studies reported both clinical pregnancy rates and LBRs. By contrast, one retrospective study not included in the Fujii review found a similar LBR for women with five or fewer follicles regardless of whether they underwent oocyte retrieval or converted to IUI [15]. There is currently an ongoing multicenter, randomized controlled trial aimed at determining whether women with two to four follicles measuring 14 mm on the day of trigger have higher LBR with IVF or conversion to IUI [16]. Hopefully, the results of this study will provide additional information for patients with a small number of follicles weighing whether to proceed with oocyte retrieval. Until there is a clearer answer regarding the benefit of converting to IUI, the results of our study can help patients with five or fewer follicles who are inquiring about their chances of live birth.
This study has a number of strengths. To the best of our knowledge, it is the largest study to examine LBR for IVF patients with a small number of follicles. Furthermore, our study did not restrict patients by age or infertility diagnosis. Compared with prior studies focusing on patients with three or fewer follicles, our study is the only one to investigate outcomes for patients with four and five follicles present at trigger. It is also the first study of its kind to examine the number of euploid embryos, which was possible because a large percentage of cycles involved PGT-A.
With regard to limitations, the study took place at a single urban academic medical center, which restricts the generalizability of our outcome data. Further studies from a variety of center types and geographic locations are warranted. Since we could not search our electronic medical record by follicle number, we identified patients with five or fewer follicles at trigger by screening patients with ten or fewer oocytes at retrieval. It is possible that some patients with five or fewer follicles had more than ten oocytes at retrieval and were missed in our study sample. However, as the mean number of oocytes retrieved for patients with five follicles at trigger was 6.5, with a standard deviation of 2, it is unlikely that very many patients with greater than ten oocytes at retrieval were missed. Additionally, not all patients had an AMH level that was identifiable in the electronic medical record, although the proportion of patients without an AMH value did not differ significantly by follicle number. Another potential limitation is that we chose to exclude cycles with unused euploid or untested embryos from our LBR analysis, which could have negatively biased our live birth rates, since there were further opportunities to achieve a live birth. We also excluded cycles that were cancelled prior to retrieval, since our goal was to determine LBR for those who chose to continue with retrieval. However, we recognize that there may be a selection bias regarding which cycles resulted in retrieval and which were cancelled. Moreover, we included multiple cycles from a single patient, and although we ran a robust sandwich standard error and robust regression to confirm our analyses, there is still a residual possibility of bias. Finally, we had a small number of patients under 35 years old who had three or fewer follicles and overall few patients with one follicle who chose to proceed to retrieval. Low numbers for these groups might make it difficult to generalize their LBRs to other patients. In the future, patients who had remaining oocytes or embryos may return to use their cryopreserved materials, and we can examine their live birth rates, as well. It would also be interesting to compare live birth rate by fertility diagnosis, to compare the characteristics of patients who cancelled their cycles with patients who proceeded to oocyte retrieval, and to examine how patients who cancelled their retrievals fared in future cycles.
This is the first study to date to examine LBR based on follicle number for patients with five or fewer follicles present at trigger. We provide clear, specific data on LBR per retrieval—the most helpful parameter when counseling patients with a low follicle count about whether to proceed to retrieval. Particularly for patients with limited insurance coverage or financial means to pay for IVF, our data can be instrumental in helping patients decide whether to cancel their cycle or proceed to oocyte retrieval. At the same time, our data can be used to reassure patients younger than 35 with one to five follicles that their chances of live birth remain reasonable.
Data availability
Data for this study can be made available upon request.
References
Peipert BJ, Montoya MN, Bedrick BS, Seifer DB, Jain T. Impact of in vitro fertilization state mandates for third party insurance coverage in the United States: a review and critical assessment. Reprod Biol Endocrinol. 2022;20:111.
Klinkert ER, Broekmans FJ, Looman CW, Te Velde ER. A poor response in the first in vitro fertilization cycle is not necessarily related to a poor prognosis in subsequent cycles. Fertil Steril. 2004;81:1247–53.
Biljan MM, Buckett WM, Dean N, Phillips SJ, Tan SL. The outcome of IVF-embryo transfer treatment in patients who develop three follicles or less. Hum Reprod. 2000;15:2140–4.
Shrem G, Salmon-Divon M, Mahfoudh AM, Balayla J, Volodarsky-Perel A, Henderson S, et al. Influence of maternal age and ovarian reserve on the decision to continue or to cancel IVF cycles in patients with one or two large follicles: a dual effect. Reprod Sci. 2022;29:291–300.
Reichman DE, Gunnala V, Meyer L, Spandorfer S, Schattman G, Davis OK, et al. In vitro fertilization versus conversion to intrauterine insemination in the setting of three or fewer follicles: how should patients proceed when follicular response falls short of expectation? Fertil Steril. 2013;100:94–9.
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26:1616–24.
Cohen Y, Tannus S, Alzawawi N, Son WY, Dahan M, Buckett W. Poor ovarian response as a predictor for live birth in older women undergoing IVF. Reprod Biomed Online. 2018;36:435–41.
Poseidon Group (Patient-Oriented Strategies Encompassing Individualized Oocyte Number), Alviggi C, Andersen CY, Buehler K, Conforti A, De Placido G, et al. A new more detailed stratification of low responders to ovarian stimulation: from a poor ovarian response to a low prognosis concept. Fertil Steril. 2016;105:1452–3.
Barnhart KT. Live birth is the correct outcome for clinical trials evaluating therapy for the infertile couple. Fertil Steril. 2014;101:1205–8.
NYU Langone Fertility Center preliminary clinic summary report. Society for Assisted Reproductive Technology. 2021. https://sartcorsonline.com/Csr/PublicSnapshotReport?ClinicPKID=1895&reportingYear=2021&fromDisclaimer=true. Accessed 1 Sept 2023.
Roberts SA, Wilkinson J, Vail A, Brison DR. Does PGT-A improve assisted reproduction treatment success rates: what can the UK Register data tell us? J Assist Reprod Genet. 2022;39:2547–54.
Kucherov A, Fazzari M, Lieman H, Ball GD, Doody K, Jindal S. PGT-A is associated with reduced cumulative live birth rate in first reported IVF stimulation cycles age ≤ 40: an analysis of 133,494 autologous cycles reported to SART CORS. J Assist Reprod Genet. 2023;40:137–49.
Munné S, Kaplan B, Frattarelli JL, Child T, Nakhuda G, Shamma FN, Silverberg K, Kalista T, Handyside AH, Katz-Jaffe M, Wells D, Gordon T, Stock-Myer S, Willman S, STAR Study Group. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019;112:1071-1079.e7.
Fujii DT, Quesnell JL, Heitmann RJ. Conversion to IUI versus continuance with IVF in low responder patients: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2018;227:35–40.
Shahine LK, Lathi RB, Baker VL. Oocyte retrieval versus conversion to intrauterine insemination in patients with poor response to gonadotropin therapy. Fertil Steril. 2009;92:1315–7.
Delbos L, Parot-Schinkel E, El Hachem H, Legendre G, Descamps P, Boucret L, et al. ConFIRM trial – conversion of in vitro fertilization cycles to intrauterine inseminations in patients with a poor ovarian response to stimulation: a protocol for a multicentric, prospective randomized trial. Trials. 2018;19:565.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. McCulloh has the following conflicts of interest: Director at Biogenetics Laboratory in Mountainside, NJ; Director at the Sperm and Embryo Bank of New York in New York, NY; Director at Biogenetics Laboratory in Brooklyn, NY; Director of Clinical Science at ReproART: the Georgian-American Center for Reproductive Medicine in Tblilis, Georgia; consulting services through McCulloh Associates in Port Washington, NY; recent Scientific Advisory Board member of GranataBio in Duxbury, MA. The other authors of this study have no conflicts of interest to report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bayefsky, M.J., Cascante, S.D., McCulloh, D.H. et al. Live birth rates in in vitro fertilization cycles with five or fewer follicles. J Assist Reprod Genet 41, 223–229 (2024). https://doi.org/10.1007/s10815-023-02985-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02985-8