Abstract
Propose
To investigate embryo retention (ER) rate in embryo transfer (ET) cycles and its effects on reproductive outcomes in a large database.
Methods
A matched retrospective cohort study in a tertiary academic hospital-based reproductive center. A total of 15,321 ET cycles were performed from January 2008 to December 2018. Each woman was matched with three separate control subjects of the same age (± 1 year), embryo condition, main causes of infertility, and type of protocol used for fresh or frozen ET cycles. The main outcomes were ER rate, and implantation, clinical pregnancy, ectopic pregnancy, and live birth rates.
Results
The overall incidence of ER was 1.4% (213/15,321). There was no difference in the rate of ER rate in fresh ET cycles compared with frozen transfer cycles (P = 0.54). We matched 188/213 (88%) of cases in the ER group to 564 non-ER cases. There were no cases of the blood in the catheter seen in the ER group. Pregnancy outcomes were similar between the ER and the non-ER cycles: clinical pregnancy rate (31.3% vs. 36.1%, P = 0.29), implantation rate (26.2% vs. 31.3%, P = 0.2), live birth rate (20.3% vs. 24%, P = 0.53), ectopic pregnancy rate (0.5% vs. 0.4%, P = 0.18), and miscarriage rate (10.7% vs. 11.3%, P = 0.53).
Conclusion
Our results suggest that ER rate does not affect the reproductive outcomes including clinical pregnancy rate, implantation rate, and live birth rate. Patients and physicians should not be concerned about the retention of embryos during transfer since there is no effect on pregnancy outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Embryo transfer (ET) is a vital step that influences pregnancy rates in women undergoing in vitro fertilization (IVF) [1, 2]. Safe placement of embryos in the uterine cavity is essential to obtain an optimal pregnancy rate, but there is no guarantee that embryos will remain in the uterine cavity after the transfer. Embryos have been found retained in the transfer catheters, on the cervix, and on the vaginal speculum [3, 4]. Embryo retention (ER) after an initial transfer is infrequent but a clinically frustrating event, creating anxiety for both the patients and the treating physicians.
The reported incidence of retained embryos following transfers varies between 1 and 8% [5,6,7,8,9], and it is encountered by even the most experienced operators. When ER occurs, the rescue method is to re-transfer the embryo/s. Outcome data on re-transferring retained embryos have been mixed. Previous studies, including a matched case-control study in China, showed that retention of embryos during transfer significantly reduced the pregnancy rate and implantation rate [4, 10, 11]. In contrast, other studies have found no significant difference in the clinical pregnancy rate in procedures that required multiple transfer attempts [8, 9, 12, 13].
The aim of our study was to further explore embryo retention (ER) rate in embryo transfer (ET) cycles and its effects on reproductive outcomes in a large number of cases.
Materials and methods
We performed a matched retrospective cohort study of all IVF cycles between January 2008 and December 2018 that had embryos retained in the transfer catheter with immediate repeat transfer. The study was approved by the McGill University Health Center Research Ethics Board (study # 2021-7493) and complied with the 1964 Helsinki Declaration and its later amendments. All ER cycles in both fresh and frozen ET cycles were included. Each woman in the embryo retention group was matched with three separate control subjects from the control group, of the same age (± 1 year), embryo condition (embryo stage, number of embryos transferred), main causes of infertility (male factor, tubal factor, endometriosis, etc.), and type of protocol used for controlled ovarian hyperstimulation in fresh ET or endometrium preparation protocol in frozen ET. All the cases of PGT-a were excluded from the study analysis. Embryo quality was defined according to Gardner criteria [14].
We performed embryo transfer using a Wallace catheter (Smith Medical International, Plymouth, MN) with a full bladder under trans-abdominal ultrasound guidance. Patients were placed in the lithotomy position without any sedation or anesthesia, and a bivalve speculum was placed in the vagina to visualize the cervix. The cervix was cleaned with sterile cotton swabs with embryo culture medium. An empty outer transfer catheter was passed through the external cervical os to the level of the internal cervical os. The tip of the catheter was placed approximately 1–1.5 cm from the fundus. The embryos were then loaded into an inner catheter with 20 mL of a medium by the embryologist. A 5-mL air bubble at the tip of the inner catheter aided visualization during ultrasound guidance. The physician then expelled the contents of the syringe/catheter, rotated the catheter, and withdrew the entire unit. Following ET, the catheter was returned to the laboratory for examination. The embryologist flushed the catheter with a culture medium and examined it for the presence of blood, mucus, and any retained embryo/s under the microscope. Any retained embryos were reloaded and immediately re-transferred; after which the transfer catheter was again examined for possible retained embryos.
The primary outcome of the study was live birth rates, defined as delivery of a live fetus after 24 completed gestational weeks. The secondary outcomes were ER rate, implantation rate, clinical pregnancy rate, and ectopic pregnancy rate. Clinical pregnancy was defined as the presence of fetal heartbeat on transvaginal ultrasound at 6 to 8 weeks of gestational age (Voluson S8, GE Health Care, Chicago, Ill.). Implantation rate was calculated as the number of gestational sacs per the number of transferred embryos. Ectopic pregnancy was diagnosed by visualization of an extra-uterine gestation on ultrasound or laparoscopy, or by the absence of an intrauterine gestational sac and increasing β-hCG levels or following the failure of dilation and curettage to reveal products of conception.
Statistical Analysis
Proportions were analyzed using the chi-square test or Fisher’s exact test when appropriate. Since the data were normally distributed, Student’s t-test was used to evaluate continuous parameters. A P value < 0.05 was considered statistically significant.
Results
A total of 15,112 ET cycles were performed during the study period. The overall incidence of ER during the study period was 1.4% (213/15,321), and all retained embryos were immediately re-transferred. No cases required a third attempt at transfer.
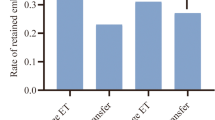
Blastocyst and cleavage ER rates in corresponding transfer cycles were 1.4% (120/8318) and 1.3% (89/6766), respectively (P = 0.55). No significant differences in the frequency of retained embryos were found between fresh (1.3%, 138/10,122) and frozen (1.5%, 75/4986) ET cycles (P = 0.54), in the entire study group. There was no difference between the rate of ER in the case of transferring one embryo vs. 2 or more embryos (1.4%, 142/10,059 vs. 1.4% 71/5028, P = 0.99). The rate of ER in cases of single blastocyst frozen embryo transfer was 1.7%, similar to the general rate in the whole study population (1.4%) (P = 0.18).
From the 213 ER cases, 188 (88%) were able to be fully matched using the five pre-determined criteria to a total of 564 non-ER cycles (1:3). Table 1 shows the cycle characteristics of the groups. Female age at oocyte retrieval, cause of infertility, number, grade and stage of transferred embryos, type of protocol (fresh vs. frozen), or catheter type were comparable. There was no significant difference in the endometrium thickness between the ER group and the non-ER group (9.8 ± 2.6 vs. 9.9 ± 2.3, P = 0.58). The rates of fresh and frozen ET cycles were also comparable. Subjective assessments of the transfer procedure were similar (considered easy in 96.3% of transfers in the ER group and in 96.8% in the non-ER-group). The incidence of ER was not different with different embryologists, P = 0.47
Table 2 demonstrates the main reproductive outcomes of the two matched groups. Pregnancy outcomes were similar between the ER and the non-ER cycles: clinical pregnancy rate (31.3% vs. 36.1%, P = 0.29), implantation rate (26.2% vs. 31.3%, P = 0.2), live birth rate (20.3% vs. 24%, P = 0.53), ectopic pregnancy rate (0.5% vs. 0.4%, P = 0.18), and miscarriage rate (10.7% vs. 11.3%, P = 0.53).
In each year from 2008 until 2018, the rate of ER ranged between 1.0 and − 2.0%; this did not differ with any statistical significance compared to the overall 1.4% ER rate.
Discussion
To the best of our knowledge, our study is the largest and most strictly matched study to date examining the incidence and outcomes associated with ER. Our study shows that the overall ER rate is low, and it does not affect the reproductive outcomes including clinical pregnancy rate, implantation rate, and live birth rate,
The reported rate of ER varied between 1 and 8% of embryo transfers [5,6,7,8,9]. The relatively low ER in our study (1.4%) could be due to the fact that during the ET process, after propelling the embryo, we routinely rotate the catheter before removal from the uterus. This might cause less negative pressure toward the catheter and therefore less ER.
In agreement with some previous studies [5, 6, 8, 9, 12, 13], we found comparable pregnancy rates when all embryos were successfully transferred on the first attempt versus those with re-transfer. However, those previous studies were retrospective in nature with small sample size. Furthermore, most of them were not well matched. Our study had a very strict five matching criteria (1:3). In one study, the authors matched for four criteria (1:2) [11] and reported that retention of embryos during transfer reduced the pregnancy rate and implantation rate. Their patients were about 3 years younger than ours with an overall higher chance of pregnancy. Although we did not evaluate the total time of transfer, our embryologists completed the catheter recheck in a very short time. It is possible that due to a short process of re-transfer, the pregnancy outcomes were not affected.
The limitations of our study included its retrospective nature and that we did not match the ER group among different physicians performing the embryo transfer. Previous studies have shown that the latter does not affect the rate of ER or the result after re-transferring the embryo [9, 11].
Other influencing factors of ET are blood or mucus in the catheter during the transfer [5, 7, 11]. In our study, there were no cases of the blood in the catheter seen in the ER group and one case in the control group. The effect of mucus on the catheter was not assessed. Xu et al. reported that ER was associated with mucus on the catheter but only in fresh ETs [11]. We found that the rate of ER in the fresh transfer was not higher than that in the frozen transfer. Moreover, after controlling for the type of transfer in the matched groups, there was no difference in reproductive outcomes. The number of embryos transferred appeared to be a potential risk factor for ER [9]. Yet, in our study, the rates of ER when transferring one embryo versus two or more embryos were comparable.
Earlier studies mainly examined the rate of cleavage-stage embryo retention [5, 6, 8]. In the last decade, blastocyst transfer has been shown to be an efficient strategy for avoiding multiple pregnancies while improving the pregnancy rate [15, 16]. In agreement with previous studies, we found that the overall incidence of ER in blastocyst transfer was similar to that in cleavage-stage embryo transfer studies [11, 13]. With proficient single blastocyst transfer and use of frozen ET, we found that the rate of ER is not different or even lower than that previously reported.
One of the concerns of immediate re-transfer of residual embryos is that the volume of fluid within the uterus may be at maximal capacity, risking “flushing out” existing embryo either out of the cervix or worse, into the Fallopian tubes. In our study, we did not find any difference in ectopic pregnancy rates in the group of ER compared to the match control group, which is in agreement with previous studies [5,6,7, 9].
Although increased embryo manipulation could cause a risk to the embryo, our data suggest that ER does not affect the reproductive outcomes including clinical pregnancy rate, implantation rate, and live birth rate following IVF-ET. Our findings should provide some comfort to patients and the treating team that ER does not lower the potential for successful live birth.
Impact statement
Patients and physicians should not be concerned about the retention of embryos during transfer since there is no demonstrable adverse effect on the live birth rate or pregnancy outcomes.
References
Mansour RT, Aboulghar MA. Optimizing the embryo transfer technique. Hum Reprod. 2002;17:1149–53. https://doi.org/10.1093/humrep/17.5.1149.
Neithardt AB, Segars JH, Hennessy S, James AN, McKeeby JL. Embryo after-loading: a refinement in embryo transfer technique that may increase clinical pregnancy. Fertil Steril. 2005;83:710–4.
Poindexter AN, et al. Residual embryos in failed embryo transfer. Fertil Steril. 1986;46:262–7.
Visser DS, Fourie FL, Kruger HF. Multiple attempts at embryo transfer: effect on pregnancy outcome in an in vitro fertilization and embryo transfer program. J Assist Reprod Genet. 1993;10:37–43.
Nabi A, Awonuga A, Birch H, Barlow S, Stewart B. Multiple attempts at embryo transfer: does this affect in-vitro fertilization treatment outcome? Hum Reprod. 1997;12:1188–90.
Lee HC, Seifer DB, Shelden RM. Impact of retained embryos on the outcome of assisted reproductive technologies. Fertil Steril. 2004;82:334–7.
Silberstein, T. Trimarchi JR, Shackelton R, Weitzen S, Frankfurter D, Plosker S. Ultrasound-guided mid-uterine cavity embryo transfer is associated with a decreased incidence of retained embryos in the transfer catheter. Fertil Steril 2005;84:1510–1512.
Tur-Kaspa I, et al. Difficult or repeated sequential embryo transfers do not adversely afect in-vitro fertilization pregnancy rates or outcome. Hum Reprod. 1998;13:2452–5.
Kubilay Vicdan, Ahmet Zeki Işık, Cem Akarsu, Eran Sözen, Gamze Çağlar, Bihter Dingiloğlu, Görkem Tuncay, The effect of retained embryos on pregnancy outcome in an in vitro fertilization and embryo transfer program. Eur J Obstet Gynecol Reprod Biol, 2007;134:79–82, ISSN 0301-2115, https://doi.org/10.1016/j.ejogrb.2007.01.011.
Alvero R, Hearns-Stokes RM, Catherino WH, Leondires MP, Segars JH. The presence of blood in the transfer catheter negatively influences outcome at embryo transfer. Hum Reprod. 2003;18:1848–52.
Jian Xu, Min-Na Yin, Zhi-Heng Chen, Li Yang, De- Sheng Ye, Ling Sun. Embryo retention significantly decreases clinical pregnancy rate and live birth rate: a matched retrospective cohort study. Fertil Steril. 2020;114:0015–0282.
Oraif A, Hollet-Caines J, Feyles V, Rebel M, Abduljabar H. Do multiple attempts at embryo transfer affect clinical pregnancy rates? J Obstet Gynaecol Can. 2014;36:406–7.
Yi HJ, Koo HS, Cha SH, Kim HO, Park CW, Song IO. Reproductive outcomes of retransferring retained embryos in blastocyst transfer cycles. Clin Exp Reprod Med. 2016;43:133–8.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocyst. In: Jansen R, Mortimer D, editors. Towards reproductive certainty: fertility and genetics beyond 1999. UK: Parthenon Publishing Carnforth; 1999. p. 378–88.
Cruz JR, Dubey AK, Patel J, Peak D, Hartog B, Gindoff PR. Is blastocyst transfer useful as an alternative treatment for patients with multiple in vitro fertilization failures? Fertil Steril. 1999;72:218–20.
Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB. Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril. 2000;73:1155–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kadour-Peero, E., Tulandi, T., Feferkorn, I. et al. Effects of embryo retention during embryo transfer on IVF outcomes. J Assist Reprod Genet 39, 1065–1068 (2022). https://doi.org/10.1007/s10815-022-02450-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02450-y