Abstract
Purpose
Implantation is essential for a successful pregnancy. Despite the increasing number of studies, implantation is still an unknown process. This study aimed to determine whether sirtuin-1 has a role in embryo implantation in oxidative stress–induced mice.
Methods
Pregnant mice were separated into 5 groups: control, vehicle, paraquat, SRT1720, and SRT1720+Paraquat. Paraquat is a herbicide and is used to induce oxidative stress. SRT1720 is a specific sirtuin-1 activator. Implantation and inter-implantation sites were removed in the morning of the 5th day of pregnancy after Chicago blue injection was performed. Sirtuin-1 and Forkhead box O1 (FoxO1) were detected by immunohistochemistry and Western blot while acetylated lysine was evaluated by Western blot analysis. Reactive oxygen and nitrogen species (ROS/RNS) and superoxide dismutase (SOD) activity were determined by fluorometric and spectrometric methods, respectively.
Results
Although there was no embryo implantation in paraquat-treated mice, 5 out of 9 SRT1720+Paraquat-treated mice had implantation sites which were significantly higher compared to the paraquat-treated group. Sirtuin-1 and FoxO1 expressions were increased at implantation sites of SRT1720-treated mice. ROS/RNS levels were decreased, while deacetylated FoxO1 levels and SOD activity were increased in SRT1720-treated mice.
Conclusion
Our findings suggest that sirtuin-1 may play a role in embryo implantation against oxidative stress through FoxO1-SOD signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human fertility is an inefficient process whereby 30% of pregnancies cease before the second trimester [1]. Although assisted reproductive technology (ART) provides solutions to some fertility problems, the implantation rate has not been greatly improved; and challenges continue regarding the poor accuracy of the methods for assessing embryonic viability and endometrial receptivity. Thus, more investigations are needed to provide practical solutions to these problems [2]. The implantation of the blastocyst into the maternal uterus is a crucial step in establishing pregnancy and thus ensuring further embryonic development. Similar to many developmental processes, implantation involves an intricate succession of molecular and cellular interactions which must be executed within an optimal time frame [3]. Embryonic development to the blastocyst stage and uterine differentiation to the receptive environment are essential to the establishment of the embryo-uterine “cross-talk,” which ultimately leads to the initiation and progression of successful implantation [4]. Uterine sensitivity to implantation-competent blastocysts is classically divided into three stages: pre-receptive, receptive, and refractory phases [5]. Uterine receptivity for implantation that supports blastocyst growth, attachment, and the subsequent events of implantation is time-limited [6].
In a healthy body, ROS and antioxidants remain in balance. When the balance is disrupted towards an overabundance of ROS, oxidative stress occurs [7, 8]. Some of the causes of oxidative stress in the uterus are decreased estrogen and progesterone levels, and it triggers a decrease in SOD expression, leading to endometrial shedding and implantation deficiency [9]. ROS is generated by several endogenous and exogenous processes [10]. One of the oxidative stress–generating exogenous agents is paraquat [11]. Paraquat produces oxidative damage in organisms by producing superoxide anions and subsequently causes an imbalance in the redox state of the cell [12]. Alterations in the oxidative stress mediated by ROS accumulation cause a significant increase in the transcriptional activity of FoxO1, and this has a major impact on SOD and catalase expression [13].
Forkhead box O transcription factor is a key player in an evolutionarily conserved pathway [14]. The members of the mammalian FoxO family consist of FoxO1, 3, 4, and 6, and they are all highly similar in their structure, function, and regulation [14]. These four genes are involved in multiple cellular pathways, which regulate proliferation (FoxO1, FoxO3, and FoxO4), oxidative stress resistance (FoxO1 and FoxO3), metabolism (FoxO1 and FOXO3), cellular differentiation (FoxO3), inflammation (FoxO1, FoxO3, and FoxO4), aging (FoxO1, FoxO3, and FoxO4), and apoptosis (FoxO1, FoxO3, and FoxO4) in mammals [15]. Therefore, the function of these important molecules is tightly controlled by a wide range of protein-protein interactions and post-translational modifications including phosphorylation, acetylation, and ubiquitination [16]. Sirtuin-1 activates several members of the FoxO family of transcription factors which promote the expression of stress response genes including SOD [17].
Sirtuins also play a pivotal role in FoxO function via NAD-dependent deacetylation in response to oxidative stress and thereby may contribute to cellular stress resistance [18]. Sirtuins comprise a highly conserved family of proteins present in virtually all species from bacteria to mammals. Sirtuins are class III histone/protein deacetylases and seven sirtuin genes (sirtuins 1–7) have been identified and characterized in mammals [19, 20]. Sirtuin-1 plays an important role in inflammation, stress resistance, and cellular senescence/aging through the deacetylation of histones, transcription factors, and signaling molecules [20]. Sirtuin activity is linked to metabolic control, apoptosis, cell survival, development, inflammation, and healthy aging [19]. Sirtuin-1 can be induced with several activators. There is a specific sirtuin-1 activator, SRT1720, of which health and lifespan benefits were shown in adult mice fed a high-fat diet [21]. Also, SRT1720 improves the follicle reserve and prolongs the ovarian lifespan of diet-induced obesity in female mice via activating sirtuin-1 [22]. There is only one study showing the role of sirtuin-1 in the regulation of uterine receptivity conducted in vitro [23]. However, it is still unknown whether SRT1720 can promote embryo implantation through activating sirtuin-1 signaling. In this study, we induced oxidative stress in mice via paraquat to characterize the effect of SRT1720 on embryo implantation in order to investigate the roles of sirtuin-1 and FoxO1 in this mechanism.
Material and methods
Animals
Six- to 8-week-old female Balb/C mice (n=49 for all groups) and 12-week-old male Balb/C mice (n=20) were obtained from Akdeniz University Animal Research Unit, Antalya, Turkey. Mice were left at 22–24 °C room temperature with a 12-h light/dark cycle and with free access to mice chow and tap water ad libitum.
Two or three female mice were kept with a male mouse overnight for mating, and the female mice were checked for a vaginal plug the next morning. Female mice observed to have vaginal plugs were admitted on the 1st day of pregnancy [24]. Pregnant mice were randomly separated into 5 groups: control group (n=10), vehicle group (n=10), paraquat group (n=10), SRT1720 group (n=10), and SRT1720+Paraquat group (n=9). The control group received no injection; the vehicle group was injected with the solvent of sirtuin-1 activator SRT1720 on the 1st, 2nd, 3rd, and 4th days of pregnancy, and the solvent of paraquat on the 4th day of pregnancy. The paraquat group was injected with 30 mg/kg paraquat (#36541, Sigma Aldrich, St. Louis, MO, USA) (prepared in 0.9% NaCl #106404, Merck, Darmstadt, Germany) on the 4th day of pregnancy; SRT1720 group was injected with 50 mg/kg SRT1720 (#A10862, Generon, Whittle Parkway, Slough, UK, prepared in 5% DMSO, 30% PEG400 -Polyethylene Glycol 400- #8074850050, Merck, Darmstadt, Germany, and 2% Tween-80 #P4780, Sigma Aldrich, St. Louis, MO, USA) on the 1st, 2nd, 3rd, and 4th days of pregnancy; and SRT1720+Paraquat group was injected with 50 mg/kg SRT1720 on the 1st, 2nd, 3rd, and 4th days of pregnancy along with 30 mg/kg paraquat in the morning of the 4th day of pregnancy, 30 min after SRT1720 injection. All injections were done early in the morning (Table 1).
Implantation sites on the 5th day of pregnancy were visualized by an intravenous injection of Chicago Blue dye solution (1% Chicago blue dye #C8679, Sigma Aldrich, St. Louis, MO, USA, was prepared in 0.9% NaCl) before sacrification and the number of implantation sites, demarcated by distinct blue bands was recorded [25]. Uterine horns that did not exhibit any implantation sites were flushed with phosphate-buffered saline (PBS) to recover blastocysts. Uteri and implantation and inter-implantation sites were collected and fixed in formalin for immunohistochemistry, stored in liquid nitrogen for Western blotting, and stored at −80 °C for biochemical analysis.
Tissue processing
Tissues were fixed in 10% formalin (#15512, Merck, Darmstadt, Germany) (100 mL 37% formaldehyde, 900 mL distilled water, pH~7) at room temperature for 24 h. Formalin was cleaned with tap water; then, tissues were dehydrated with immersion in 70%, 80%, and 90% ethanol (#100986, Merck, Darmstadt, Germany) for 24 h each and 100% ethanol for 4 h. After dehydration, tissues were cleared in xylene (#16446, Sigma Aldrich, Italy) and embedded in paraffin wax (#107337, Merck, Darmstadt, Germany). Cleared tissues were kept in paraffin in an oven at 56 °C and then embedded in paraffin.
Immunohistochemistry
Formalin-fixed and paraffin-embedded tissues were cut into 5-μm sections and placed on slides coated with poly-l-lysine (#J1800AMNZ, Thermo Scientific, Braunschweig, Germany). They were kept in an oven at 56 °C overnight the day before immunostaining. Sections were deparaffinized in xylene and rehydrated through a graded series of ethanol, rinsed in distilled water, and washed three times in PBS (pH: 7.2–7.4). To unmask antigens, an antigen retrieval procedure was performed by treating the samples in 10-mM citrate buffer (#100242, Merck, Darmstadt, Germany), pH 6.0, in a microwave oven at 750 W for 5 min, three times. After cooling for 20 min at room temperature, the sections were washed in PBS for 5 min. Endogenous peroxidase activity was blocked by incubation in methanol containing 3% H2O2 (#108597, Merck, Darmstadt, Germany) for 20 min and washed with PBS three times. Sections were incubated with a blocking solution (Ultra UV Block, #TA-125UB, LabVision Corporation, Fremont, CA, USA) for 7 min at room temperature to block non-specific binding. Excess serum was drained, and sections were incubated with rabbit polyclonal anti-sirtuin-1 (#15404; Santa Cruz Biotechnology, Santa Cruz, CA, USA) at 1:50 dilution and rabbit monoclonal anti-FoxO1 (#2880, Cell Signaling Technology, Danvers, MA, USA) at 1:100 dilution at +4 °C overnight. The primary antibodies were substituted with normal rabbit IgG (#sc-2027, Santa Cruz Biotechnology, Santa Cruz, CA, USA) in the same dilutions as the specific antibodies. The next day, sections were washed with PBS three times. Then, they were incubated with biotinylated anti-rabbit secondary antibody (#BA-1000, Vector Laboratories, Burlingame, USA) at 1:500 dilution in a humid environment at room temperature for 45 min, followed by incubation with HRP-conjugated streptavidin complex (#TS125HR, Thermo Scientific, Fremont, CA, USA) for 20 min at room temperature. Sections were washed 3 times with PBS after each treatment. Sections were treated with diaminobenzidine (DAB) chromogen (#D4168, Sigma Aldrich, St. Louis, MO, USA) for 2 min to improve signaling and then washed in tap water. Mayer’s hematoxylin (#109249 Merck, Darmstadt, Germany) was utilized for counterstaining of the sections, and they were dehydrated and mounted with Entellan (#107961; Merck, Darmstadt, German) mounting medium. Sections were examined and photographed by Nikon Eclipse E200 microscope.
H-SCORE evaluations
In sections of experimental groups, evaluation of the immunohistochemical labeling of FoxO1 in the luminal epithelium was performed using H-SCORE [26]. Immunopositive cells were counted in 5 different areas under ×200 original magnification under the Nikon Eclipse E200 microscope. Three sections were randomly selected from every group. The evaluations were recorded as percentages of positively stained cells of all types in each of four intensity categories which were denoted as 0 (no staining), 1+ (weak but detectable above control), 2+ (distinct), 3+ (intense). The evaluation was conducted by two blinded observers, and an H-SCORE value was derived by summing the percentages of cells that stained at each intensity multiplied by the weighted intensity of the staining (H-SCORE = ∑·Pi (i + 1) for each tissue, where i is the intensity score and Pi is the corresponding percentage of the cells).
Sodium dodecyl sulfate (SDS) polyacrylamide gel electrophoresis and Western blotting
Uteri and implantation and inter-implantation sites were frozen in liquid nitrogen, then thawed and subjected to protein isolation. Protein extraction and immunoblot analysis were performed as described previously [27]. All samples were weighed and put into a homogenization buffer supplemented with a Complete R protease inhibitor cocktail (#11697498001; cOmplete Merck, Mannheim, Germany). After homogenization, samples were centrifuged at 10.000g for 10 min. Supernatants were collected and stored at −80 °C. The protein concentration was determined by BCA kit (bicinchoninic acid solution (#B9643) and copper (II) sulfate solution (#C2284); Sigma Aldrich, St. Louis, MO, USA), and 50 μg of protein was applied per lane. The samples prepared were mixed with distilled water and Laemmli (#S3401, Sigma Aldrich, St. Louis, MO, USA) in line with the protein content of the protein lysates prepared. The samples were then boiled in water at 100 °C. Samples were subjected to SDS polyacrylamide gel electrophoresis (30% acrylamide in 10% gel) at 80 V for approximately 2 h. At the end of electrophoresis, PVDF (polyvinylidene difluoride) membrane (#1620177, Bio-Rad, Portland, ME, USA) was kept in methanol (#106009, Merck, Merck, Darmstadt, Germany) for 30 s. The proteins were transferred onto the membrane in a buffer containing 0.2 mol/L glycine (#1610718, Bio-Rad, Portland, ME, USA), 25 mmol/L Tris (#108387, Merck, Darmstadt, Germany), and 20% methanol overnight at +4 °C and 32 volts and 65 A. The next day, the membranes were blocked for 1 h with 5% BSA (#A9647, Sigma Aldrich, St. Louis, MO, USA) and 0.1% Tween 20 (#TA-125-TW, Lab Vision, Thermo Fisher Scientific, Rockford, USA) in 0.14 mol/L Tris-buffered saline (TBS; pH 7.2–7.4). Membranes were incubated with 1:500 dilution of rabbit polyclonal anti-sirtuin-1 (#15404, Santa Cruz Biotechnology), 1:2000 dilution of rabbit monoclonal anti-FoxO1 (#2880, Cell Signaling Technology, Danvers, MA, USA), and 1:500 dilution of rabbit polyclonal acetylated lysine (#9441, Cell Signaling Technology, Danvers, MA, USA) overnight at +4 °C. Primary antibodies were diluted in 5% BSA. After incubation, they were washed with TBS-T for 30 min. The membranes were incubated with horseradish peroxidase (HRP)–conjugated secondary antibody (#PI-1000, Vector Laboratories, Burlingame, USA) diluted in 5% BSA on a rocker for 1 h at room temperature. They were then washed with TBS-T for 30 min. The membranes were incubated for 5 min within the Super Signal Chemiluminesans (CL)-HRP substrate system (#34080, Thermo Fisher Scientific, Rockford, USA), and the signals on membranes were then transferred on to hyper film (#28-9068-37 Amersham Hyperfilm ECL, GE Healthcare, Buckinghamshire, UK) in a dark room. The film was processed through a developer (#1757855, Ilford, England) and fixative (#1984565, Ilford, England) followed by washing with distilled water and drying. Thus, the quantities of sirtuin-1, FoxO1, and acetylated lysine protein expressions were determined. Membranes were also labeled by an identical protocol for binding of a 1:5000 dilution of a rabbit monoclonal anti-beta actin antibody (#4970, Cell Signaling Technology, Danvers, MA, USA) as an internal control to confirm the equal loading of the samples. The bands were quantified using NIH image analysis software (Image J Version 1.36b; National Institutes of Health, MD, USA).
Determination of ROS/RNS levels
OxiSelect™ In Vitro ROS/RNS Assay Kit (#STA-347, Cell Biolabs, Inc. San Diego, CA) was used to measure the levels of ROS and RNS in uteri and implantation sites of experimental groups according to the protocol provided by the company. Briefly, samples in PBS buffer were lysed using a homogenizer. The lysates were collected and centrifuged at 10,000g for 15 min at +4 °C.
Protein concentrations were measured at 595 nm by a modified Bradford assay using Coomassie Plus reagent with bovine serum albumin as a standard (Pierce, Thermo Fisher Scientific, Roskilde, Denmark).
The lysates were adjusted to equal protein concentrations (1:100 dilution) using PBS. We added 50 μL of each sample (triplicate) and 50 μL of catalyst solution to a black 96-well plate and then incubated for 5 min at room temperature. We added 100 μL of dichlorodihydrofluorescein (DCFH) solution to the samples and incubated the mixture at room temperature for 20 min protecting it from the light. Finally, fluorescence was read with a fluorometric plate reader at 480 nm/530 nm [28].
Determination of SOD levels
Total tissue SOD activity was measured using a commercially available kit (#706002, Cayman Chemical, Ann Arbor, USA) that measures all three types of SOD (Cu/Zn-, Mn-, and EC-SOD). One unit of SOD is defined as the amount of enzyme that dismutates 50% of the superoxide radical. Briefly, xanthine oxidase and hypoxanthine generate superoxide radicals that are dismutated by SOD, and in the process, tetrazolium salt is converted to a formazan dye that is read at 450 nm. SOD activity of the samples was calculated from the linear regression of a standard curve that was determined using SOD activity of bovine erythrocytes at various concentrations run under the same conditions. The SOD activity was expressed as units per milliliter of tissue extract [29].
Statistical analysis
Statistical analyses were performed using one-way ANOVA. Probability values of less than 0.05 were considered significant; values are presented as mean ± SEM (standard error of the mean).
Results
Paraquat exposure inhibits embryo implantation
Blastocysts position in the implantation chamber (crypt) in the afternoon of day 4 of pregnancy (day 1 = vaginal plug) [30]. The receptive state of the uterus is defined as the limited time when the uterine milieu is favorable to blastocyst acceptance and implantation [24]. It is known that paraquat can adversely impact the development and implantation of embryos [31, 32]. To minimize the damaging effects of paraquat on embryo growth and activation, paraquat was injected at a 30-mg/kg dose that prevents implantation but does not damage the embryo [32]. Control and vehicle group mice showed implantation sites as demarcated by blue bands. Paraquat group mice did not have any implantation sites (Fig. 1a and b). To eliminate the possibility of lack of implantation due to failure of fertilization, one of the uterine horns was washed with PBS, and the presence of blastocysts was observed. Normal morphology of blastocysts demonstrated that the administered paraquat dose did not adversely affect embryo development (Fig. 1c).
Implantation sites of experimental groups on the 5th day of pregnancy. a–b The average number of implantation sites of experimental groups on the 5th day of pregnancy. c Blastocysts obtained by washing one uterine horn on the 5th day of pregnancy in the paraquat group. Data are plotted as mean ± SEM. Different symbols indicate a significant difference compared to that group (*: Control, #: Paraquat). All the scale bars represent 50 μm
SRT1720 improves embryo implantation in paraquat-treated mice
Activation and increased expression of sirtuin-1 play an important role in uterine receptivity [23]. To stimulate sirtuin-1 activity, we used SRT1720, a synthetic activator specific to sirtuin-1 [21]. To evaluate whether SRT1720 has harmed embryo implantation, the number of implantation sites was compared to that of the control group and no significant differences were observed (Fig. 1a and b). Then, we evaluated whether SRT1720 improves embryo implantation in paraquat-injected mice. While some of the SRT1720-treated mice did not have implantation sites (4/9), the rest of the mice (5/9) had implantation sites. Although the number of implantation sites in the SRT1720+Paraquat group was significantly lower than that in the control group (p <0.05), it was significantly higher than that in the paraquat group (p <0.05) (Fig. 1a and b).
Sirtuin-1 expression in uteri and implantation sites of experimental groups
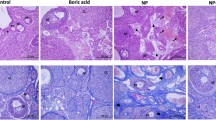
The sirtuin-1 activator SRT1720 improved embryo implantation in paraquat-injected mice; thus, we determined sirtuin-1 spatial distribution and expression in uteri and implantation and inter-implantation sites of experimental groups via immunohistochemistry and Western blotting, respectively. Sirtuin-1 exhibited mainly nuclear expression. Sirtuin-1 expression was in the luminal and glandular epithelium and stroma. Embryos in control, vehicle, SRT1720, and SRT1720+Paraquat groups also showed sirtuin-1 expression (Fig. 2a). Sirtuin-1 expression was significantly increased in SRT1720-treated groups compared to that in the control group (Fig. 2a and b).
Sirtuin-1 expression in the endometrium of experimental groups on the 5th day of pregnancy. a Immunohistochemistry of sirtuin-1. b Western blot and relative densitometric analysis of sirtuin-1. e, embryo; le, luminal epithelium; ge, glandular epithelium, s, stroma; myo, myometrium; AM, antimesometrium; imp, implantation sites; inter, inter implantation sites. Data are plotted as mean ± SEM. Different letters indicate a significant difference compared to that group (a, Control Implantation; b, Control Inter Implantation; c, Paraquat Uterus). All the scale bars represent 50 μm
FoxO1 expression in uteri and implantation sites of experimental groups
Recent studies indicate the roles of FoxO1 in the female reproductive system, especially in the maternal endometrium [33]; and a very recent study shows that FoxO1-ablated mice were infertile due to defective implantation and invasion [1]. Sirtuin-1 is known to modulate upstream signaling of FoxO1 [34] and deacetylates FoxO1, promoting its transcriptional activity [35]. Therefore, we determined FoxO1 spatial distribution and expression in uteri and implantation sites of experimental groups via immunohistochemistry and Western blotting, respectively. FoxO1 exhibited both nuclear and cytoplasmic expression. FoxO1 expression was mainly observed in the luminal and glandular epithelium; there was no expression in stroma except endothelial cells (Fig. 3a). FoxO1 expression was higher at implantation sites compared to that at inter-implantation sites for control, vehicle, SRT1720, and SRT1720+Paraquat groups, and was statistically significant. Also, FoxO1 expression at implantation sites of SRT1720-treated groups was significantly increased compared to that of the control group (Fig. 3b).
FoxO1 expression in the endometrium of experimental groups on the 5th day of pregnancy. a Immunohistochemistry of FoxO1. b Western blot and relative densitometric analysis of FoxO1. e, embryo; le, luminal epithelium; ge, glandular epithelium; s, stroma; myo, myometrium; AM, antimesometrium; imp, implantation sites; inter, inter implantation sites. Data are plotted as mean ± SEM. Different letters indicate a significant difference compared to that group (a, Control Implantation; b, Control Inter Implantation; c, Vehicle Implantation; d, Paraquat Uterus; e, SRT1720 Implantation; f, SRT1720+Paraquat Implantation). All the scale bars represent 50 μm
Cellular distribution of FoxO1 in the luminal epithelium of uteri and implantation sites of experimental groups
We observed unique cellular distributions of FoxO1 in the luminal epithelium of uteri and implantation sites of experimental groups. FoxO1 was mainly nuclear at implantation sites and cytoplasmic at inter-implantation sites of control, vehicle, SRT1720, and SRT1720+Paraquat groups. When examined in detail, we observed that FoxO1 was mainly cytoplasmic only in the blastocyst attachment region of control, vehicle, SRT1720, and SRT1720+Paraquat groups. Furthermore, FoxO1 was mainly nuclear in the antimesometrium and cytoplasmic in the mesometrium side of the luminal epithelium of the paraquat group. We evaluated FoxO1 expression in the luminal epithelium of all groups by H-SCORE analysis. FoxO1 expression in the luminal epithelium of implantation sites was higher than that of inter-implantation sites of all experimental groups with a statistically significant difference. SRT1720- and paraquat-treated groups had higher FoxO1 expression than the control group. On the other hand, paraquat and SRT1720 co-treated groups had much higher FoxO1 expression compared to the control group (Fig. 4).
Cellular distribution of FoxO1 at embryo homing sites in experimental groups on the 5th day of pregnancy. e, embryo; le, luminal epithelium; ge, glandular epithelium; s, stroma; myo, myometrium; AM, antimesometrium; imp, implantation sites; inter, inter implantation sites. Data are plotted as mean ± SEM. Different letters indicate a significant difference compared to that group (a, Control Implantation; b, Control Inter Implantation; c, Vehicle Implantation; d, Paraquat Uterus; e, SRT1720 Implantation; f, SRT1720+Paraquat Implantation). All the scale bars represent 50 μm
Deacetylated FoxO1 levels in uteri and implantation sites of experimental groups
FoxO activity is tightly regulated at the post-translational level affecting its localization, stability, DNA binding, or protein-protein interactions [36]. In the presence of oxidative stress, sirtuin-1, located in the nucleus, associates with and deacetylates nuclear FoxOs [37]. The deacetylated form is necessary for the post-translational modification of this transcription factor which is needed for its active modification and cellular defense against oxidative stress [38]. Sirtuin-1 stimulates the deacetylation of FoxO1, which, in turn, plays an essential role in mediating the sirtuin-1-induced upregulation of SOD and the suppression of oxidative stress [39]. Thus, we determined deacetylated FoxO1 levels by subtracting acetylated lysine values from FoxO1 values obtained via Western blot. As indicated in Fig. 5a and b, deacetylated FoxO1 levels at implantation sites were higher than those at inter-implantation sites of control, vehicle, SRT1720, and SRT1720+Paraquat groups and it was statistically significant. Deacetylated FoxO1 levels in the paraquat group were lower than those in the control group. Deacetylated FoxO1 levels in the SRT1720 treated group were higher than those in the control group. Moreover, paraquat and SRT1720 co-treated groups had much higher deacetylated FoxO1 levels than the control group.
Deacetylated FoxO1 levels in uteri or implantation sites of experimental groups. a Western blot and relative densitometric analysis of FoxO1. b Deacetylated FoxO1 levels. Data are plotted as mean ± SEM. Different letters indicate a significant difference compared to that group (a, Control Implantation; b, Control Inter Implantation; c, Vehicle Implantation; d, Paraquat Uterus; e, SRT1720 Implantation; f, SRT1720 Inter Implantation; g, SRT1720+Paraquat Implantation)
ROS/RNS levels in uteri and implantation sites of experimental groups
SOD is one of the antioxidant enzymes directly involved in the neutralization of ROS and RNS [40]. We determined the levels of ROS/RNS which cause oxidative stress, in uteri and implantation and inter-implantation sites of experimental groups. As indicated in Fig. 6, ROS/RNS levels were similar at implantation and inter-implantation sites for control, vehicle, SRT1720, and SRT1720+Paraquat groups. ROS/RNS levels significantly increased in paraquat and SRT1720+Paraquat groups compared to those in the control group. In the SRT1720+Paraquat group, the levels of ROS/RNS were higher than those in the control group, but they were significantly lower than those in the paraquat group. In the SRT1720 group, the levels of ROS/RNS were significantly lower than those in the control group. These results indicated that the levels of ROS/RNS were decreased in SRT1720-treated groups.
ROS/RNS levels in uteri or implantation sites of experimental groups on the 5th day of pregnancy. Data are plotted as mean ± SEM. Different letters indicate a significant difference compared to that group (a, Control Implantation; b, Control Inter Implantation; c, Paraquat Uterus; d, SRT1720 Implantation; e, SRT1720 Inter Implantation)
SOD levels in uteri and implantation sites of experimental groups
Sirtuin-1-mediated deacetylation of FoxO1 directly controls the expression of SOD [41]. In our study, we determined SOD activity in uteri and implantation and inter-implantation sites of experimental groups. As indicated in Fig. 7, SOD activity was similar at implantation and inter-implantation sites for control, vehicle, SRT1720, and SRT1720+Paraquat groups. SOD activity was significantly increased in paraquat, SRT1720, and SRT1720+Paraquat groups compared to that in the control group. The increase in SOD activity was higher in the SRT1720+Paraquat group compared to that in the paraquat and SRT1720 groups.
SOD activity in uteri or implantation sites of experimental groups on the 5th day of pregnancy. Data are plotted as mean ± SEM. Different letters indicate a significant difference compared to that group (a, Control Implantation; b, Control Inter Implantation; c, Paraquat Uterus; d, SRT1720 Implantation; e, SRT1720 Inter Implantation)
Discussion
The mechanisms involved in embryo implantation have not been clarified and are still an intriguing subject in this regard. In one study performed with Ishikawa and RL95-2 endometrial carcinoma cell lines, sirtuin-1 was shown to play an important role in uterine receptivity [23]. However, there is no in vivo study in the literature regarding whether sirtuin-1 is involved in embryo implantation in mice. In this study, we show that embryo implantation can be improved by SRT1720, a specific activator of sirtuin-1, in paraquat-treated mice. To our knowledge, this should be the first in vivo study demonstrating the involvement of sirtuin-1 in embryo implantation.
It has been suggested that oxidative stress affects the entire reproductive life and pregnancy-related disorders [7, 42]. Dietary antioxidants and oxidative stress may influence the timing and maintenance of a viable pregnancy [43]. Additionally, restraining stress leads to a decrease in implantation success in mice [44]. Previous studies showed that paraquat adversely affected embryo development and implantation via inducing oxidative stress [31, 32, 45, 46]. In one of those studies, paraquat prevented embryo implantation without harming embryo development [32]. Likewise, in our study, implantation did not occur in 30-mg/kg paraquat–injected mice. Meanwhile, the normal morphology of blastocysts obtained by washing one of the uterine horns indicated that embryos are healthy and the administered paraquat dose did not affect embryo development.
The sirtuin-1 activator, SRT1720, has been reported to show positive roles in female reproduction, such as improving follicle reserve and extending ovarian life [22]. In our study, although embryo implantation was inhibited by paraquat, the occurrence of embryo implantation with the use of SRT1720 suggests that sirtuin-1 activity may have an important role in this process. There are studies in the literature using different concentrations and applications of SRT1720 [22, 47,48,49]. In our study, 5 out of 9 SRT1720+Paraquat mice had implantation sites while implantation did not occur in 4 out of 9 mice. This might be a result of the applied dose of SRT1720. Administration of higher doses of SRT1720 could result in higher implantation site numbers.
The fact that paraquat inhibited implantation and was partially improved by SRT1720 made us think that sirtuin-1 might play a role in embryo implantation. In general, sirtuin-1 is localized in nuclei but is also known to shuttle between cytoplasm and nuclei in some cell types [50, 51]. The nucleocytoplasmic shuttling of sirtuin-1 has been described in both physiological and pathological conditions where oxidative stress occurs [52]. Sirtuin-1, a protein deacetylase, regulates cellular oxidative stress and its toxicity. Furthermore, sirtuin-1 is also regulated by oxidative stress [52,53,54]. H2O2-mediated oxidative stress may result in cytoplasmic localization of sirtuin-1 in cervix and lung cells [51, 55]. On the other hand, while sirtuin-1 was expressed mainly in the nucleus of rat nucleus pulposus cells, no significant cytoplasmic translocation of sirtuin-1 was observed with H2O2 treatment [54]. In our study, sirtuin-1 was nuclear in SRT1720 and SRT1720+Paraquat mice. This confirms that the nucleocytoplasmic shuttle of sirtuin-1 is specific to cells and tissues. In one study, paraquat exposure upregulated the expression of sirtuin-1; long-term exposure to paraquat significantly decreased sirtuin-1 expression in the lungs of mice. Another sirtuin-1 activator, resveratrol, strongly enhanced sirtuin-1 expression and attenuated lung injury induced by paraquat exposure [56]. In our study, increased expression of sirtuin-1 in SRT1720-treated groups may indicate that SRT1720 enhances sirtuin-1 activity. Mouse type II alveolar epithelial cells (AECs-II) were exposed to low-dose paraquat, and sirtuin-1 expression was upregulated. On the other hand, sirtuin-1 expression gradually decreased with increasing paraquat concentrations [53].
Sirtuins catalyze the deacetylation and adenosine diphosphate (ADP) ribosylation of target proteins using the oxidized form of nicotinamide adenine dinucleotide (NAD+) as a coenzyme [57]. Sirtuin-1 targets histones, transcription factors, and transcriptional regulators in the nucleus, which control gene expression by deacetylation [58]. FoxO1 is a direct and functional target for sirtuin-1 in mammalian systems [59]. Activating sirtuin-1 can promote FoxO1 expression and transition from cytoplasm to nucleus [60]. We observed that the endometrial distribution of FoxO1 was in the luminal and glandular epithelium; although expression was weak in stromal cells, it was distinct in endothelial cells in the stroma. Interestingly, the expression of FoxO1 differed in the luminal epithelium through the mesometrial-antimesometrial (M-AM) axis. Trophoblast cells directly communicating with the luminal epithelium during implantation swallow the luminal epithelial cells without caspase-3 activation (entosis); then, apoptosis occurs in the luminal epithelial cells so the luminal epithelium surrounding the blastocyst is breached on day 5 evening of pregnancy [30]. FoxO1 expression was cytoplasmic in the luminal epithelial cells of the antimesometrium, notably in the blastocyst attachment region, and it was nuclear in the luminal epithelium of the mesometrium [33]. In other words, FoxO1 distribution was only cytoplasmic at embryo homing sites in the luminal epithelium and nuclear in the luminal epithelial cells excluding those surrounding the blastocyst. FoxO1 expression was higher at implantation sites than that at inter-implantation sites of all groups. Similarly, Adiguzel et al. also showed that FoxO1 expression was weak at inter-implantation sites on day 5 of pregnancy [33]. This suggests that FoxO1 is an important molecule for embryo implantation. FoxO1 can be retained in the nucleus by decreasing its acetylation; conversely, FoxO1 can be translocated to the cytoplasm by increasing its acetylation [61]. Cytoplasmic localization of FoxO1 at the mesometrial side of the luminal epithelium might be related to increased acetylation of FoxO1, and nuclear localization of FoxO1 at the antimesometrial side of the luminal epithelium might be an adaptive response to oxidative stress against possible embryo implantation in paraquat-treated mice.
FoxO1 deacetylation by sirtuin-1 regulates transcription activity and consequently provides resistance to oxidative stress [59, 62, 63]. We indicate that FoxO1 acetylation increases in uteri of paraquat-treated mice, and therefore deacetylation decreases. However, there was increased FoxO1 deacetylation both in SRT1720 and SRT1720+Paraquat mice. Furthermore, FoxO1 deacetylation increased more in SRT1720+Paraquat mice compared to that in only SRT1720-treated mice. This might indicate that FoxO1 deacetylation can further be increased by SRT1720 treatment in addition to the induced oxidative stress.
FoxO1 mediates protective effects against oxidative stress through the regulation of antioxidant genes, such as catalase and SOD, [64] and FoxO1 activity is regulated by sirtuin-1 [13, 17]. SOD is responsible for the detoxification of superoxide anions and is required for normal health and reproduction [65]. Oxygen radicals and SOD regulate cellular function by controlling the production or activation of biologically active substances [66]. Our findings show that SOD activity was increased in SRT1720 and SRT1720+Paraquat mice. This increase might be due to increased FoxO1 deacetylation. Furthermore, an increase in SOD activity despite low deacetylation of FoxO1 in the paraquat group may suggest that another mechanism is involved in this increase. ROS and SOD play important roles in the process of reproductive physiology [67]. ROS are like a double-edged sword; they serve as key signaling molecules in physiological processes but also have roles in pathological processes involving the female reproductive tract [7].
We determined ROS/RNS levels to evaluate the relationship between SRT1720 and oxidative stress. As expected, paraquat treatment significantly increased ROS/RNS levels since it causes oxidative stress. In paraquat and SRT1720 co-treated groups, ROS/RNS levels were higher than those in the control group but less than those in only the paraquat-treated group. Besides, SRT1720-treated mice had less oxidative stress. It is possible to state that SRT1720 performs an important role in reducing oxidative stress in the female reproductive system. Reducing the damage caused by paraquat in the female reproductive system by SRT1720 seems promising for embryo implantation. These findings show that SRT1720 might improve reproductive failures caused by increased oxidative stress in the female reproductive system.
Nevertheless, this study has some limitations. The main limitation of our study is the lack of different SRT1720 dose treatments. We used SRT1720 at 50 mg/kg dose. It might be possible that SRT1720 treatment with doses greater than 50 mg/kg may lead to a higher percentage of embryo implantation. The second limitation of our study was that we were unable to investigate whether sirtuin-1 plays a role in decidualization and whether paraquat and SRT1720 treatments had any effects on decidualization. However, a very recent study revealed the essential role of sirtuin-1 in regulating differentiation and maintaining ROS homeostasis in human endometrial stromal cells during decidualization in vitro [68]. Thirdly, we did not follow the mice until the end of pregnancy to compare birth rates. It will be interesting to explore whether SRT1720 has protective roles in paraquat-treated mice regarding pregnancy progression after implantation. Lastly, although animal studies provide a valuable source of knowledge, the need to perform respective human studies is still apparent. The fundamental limitation of research on humans is the availability of human tissue during implantation. We believe our results are fundamental for the potential roles of sirtuin-1 in mouse embryo implantation and will lead to further studies in this field.
Conclusion
Infertility is a social and economic problem. Approximately 30% of human fertilization results in miscarriage. In some individuals, infertility problems can be solved by assisted reproductive techniques, but if the uterus is not receptive, embryo transfer results in implantation failure. Based on these findings, sirtuin-1 may protect embryo implantation against oxidative stress through FoxO1-SOD signaling. It will be worthy to investigate sirtuin-1-FoxO1-SOD signaling in implantation failure and recurrent pregnancy loss cases.
Data availability
Available upon request.
References
Vasquez YM, Wang X, Wetendorf M, Franco HL, Mo Q, Wang T, et al. FOXO1 regulates uterine epithelial integrity and progesterone receptor expression critical for embryo implantation. PLoS Genet. 2018;14(11):e1007787. https://doi.org/10.1371/journal.pgen.1007787.
Liang J, Wang S, Wang Z. Role of microRNAs in embryo implantation. Reprod Biol Endocrinol. 2017;15(1):90. https://doi.org/10.1186/s12958-017-0309-7.
Tu Z, Wang Q, Cui T, Wang J, Ran H, Bao H, et al. Uterine RAC1 via Pak1-ERM signaling directs normal luminal epithelial integrity conducive to on-time embryo implantation in mice. Cell Death Differ. 2016;23(1):169–81. https://doi.org/10.1038/cdd.2015.98.
Paria BC, Song H, Dey SK. Implantation: molecular basis of embryo-uterine dialogue. Int J Dev Biol. 2001;45(3):597–605.
Tu Z, Ran H, Zhang S, Xia G, Wang B, Wang H. Molecular determinants of uterine receptivity. Int J Dev Biol. 2014;58(2-4):147–54. https://doi.org/10.1387/ijdb.130345wh.
Matsumoto H. Molecular and cellular events during blastocyst implantation in the receptive uterus: clues from mouse models. J Reprod Dev. 2017;63:445–54.
Agarwal A, Gupta S, Sharma RK. Role of oxidative stress in female reproduction. Reprod Biol Endocrinol. 2005;3:28. https://doi.org/10.1186/1477-7827-3-28.
Gupta S, Ghulmiyyah J, Sharma R, Halabi J, Agarwal A. Power of proteomics in linking oxidative stress and female infertility. Biomed Res Int. 2014;2014:916212–26. https://doi.org/10.1155/2014/916212.
Chandra A, Surti N, Kesavan S, Agarwal A. Significance of oxidative stress in human reproduction. Arch Med. 2009;5(1A):528–42.
Liguori I, Russo G, Curcio F, Bulli G, Aran L, Della-Morte D, et al. Oxidative stress, aging, and diseases. Clin Interv Aging. 2018;13:757–72. https://doi.org/10.2147/CIA.S158513.
Gawarammana IB, Buckley NA. Medical management of paraquat ingestion. Br J Clin Pharmacol. 2011;72(5):745–57. https://doi.org/10.1111/j.1365-2125.2011.04026.x.
Blanco-Ayala T, Anderica-Romero AC, Pedraza-Chaverri J. New insights into antioxidant strategies against paraquat toxicity. Free Radic Res. 2014;48(6):623–40. https://doi.org/10.3109/10715762.2014.899694.
Xing YQ, Li A, Yang Y, Li XX, Zhang LN, Guo HC. The regulation of FOXO1 and its role in disease progression. Life Sci. 2018;193:124–31. https://doi.org/10.1016/j.lfs.2017.11.030.
Tia N, Singh AK, Pandey P, Azad CS, Chaudhary P, Gambhir IS. Role of Forkhead Box O (FOXO) transcription factor in aging and diseases. Gene. 2018;648:97–105. https://doi.org/10.1016/j.gene.2018.01.051.
Murtaza G, Khan AK, Rashid R, Muneer S, Hasan SMF, Chen J. FOXO transcriptional factors and long-term living. Oxidative Med Cell Longev. 2017;2017:3494289–8. https://doi.org/10.1155/2017/3494289.
Obsil T, Obsilova V. Structure/function relationships underlying regulation of FOXO transcription factors. Oncogene. 2008;27(16):2263–75. https://doi.org/10.1038/onc.2008.20.
Merksamer PI, Liu Y, He W, Hirschey MD, Chen D, Verdin E. The sirtuins, oxidative stress and aging: an emerging link. Aging. 2013;5(3):144–50. https://doi.org/10.18632/aging.100544.
Kobayashi Y, Furukawa-Hibi Y, Chen C, Horio Y, Isobe K, Ikeda K, et al. SIRT1 is critical regulator of FOXO-mediated transcription in response to oxidative stress. Int J Mol Med. 2005;16(2):237–43.
Favero G, Franceschetti L, Rodella LF, Rezzani R. Sirtuins, aging, and cardiovascular risks. Age. 2015;37(4):9804. https://doi.org/10.1007/s11357-015-9804-y.
Yao H, Hwang JW, Sundar IK, Friedman AE, McBurney MW, Guarente L, et al. SIRT1 redresses the imbalance of tissue inhibitor of matrix metalloproteinase-1 and matrix metalloproteinase-9 in the development of mouse emphysema and human COPD. Am J Physiol Lung Cell Mol Physiol. 2013;305(9):L615–24. https://doi.org/10.1152/ajplung.00249.2012.
Mitchell SJ, Martin-Montalvo A, Mercken EM, Palacios HH, Ward TM, Abulwerdi G, et al. The SIRT1 activator SRT1720 extends lifespan and improves health of mice fed a standard diet. Cell Rep. 2014;6(5):836–43. https://doi.org/10.1016/j.celrep.2014.01.031.
Zhou XL, Xu JJ, Ni YH, Chen XC, Zhang HX, Zhang XM, et al. SIRT1 activator (SRT1720) improves the follicle reserve and prolongs the ovarian lifespan of diet-induced obesity in female mice via activating SIRT1 and suppressing mTOR signaling. J Ovarian Res. 2014;7:97. https://doi.org/10.1186/s13048-014-0097-z.
Shirane A, Wada-Hiraike O, Tanikawa M, Seiki T, Hiraike H, Miyamoto Y, et al. Regulation of SIRT1 determines initial step of endometrial receptivity by controlling E-cadherin expression. Biochem Biophys Res Commun. 2012;424(3):604–10. https://doi.org/10.1016/j.bbrc.2012.06.160.
Paria BC, Huet-Hudson YM, Dey SK. Blastocyst’s state of activity determines the “window” of implantation in the receptive mouse uterus. Proc Natl Acad Sci U S A. 1993;90(21):10159–62. https://doi.org/10.1073/pnas.90.21.10159.
Song H, Lim H, Paria BC, Matsumoto H, Swift LL, Morrow J, et al. Cytosolic phospholipase A2α is crucial for ‘on-time’embryo implantation that directs subsequent development. Development. 2002;129(12):2879–89.
Acar N, Soylu H, Edizer I, Ozbey O, Er H, Akkoyunlu G, et al. Expression of nuclear factor erythroid 2-related factor 2 (Nrf2) and peroxiredoxin 6 (Prdx6) proteins in healthy and pathologic placentas of human and rat. Acta Histochem. 2014;116(8):1289–300. https://doi.org/10.1016/j.acthis.2014.07.012.
Acar N, Turkay Korgun E, Ustunel I. Cell cycle inhibitor p57 expression in normal and diabetic rat placentas during some stages of pregnancy. 2012;27(1):59–68. https://doi.org/10.14670/HH-27.59.
Zhang Y, Xu Z, Wang H, Dong Y, Shi HN, Culley DJ, et al. Anesthetics isoflurane and desflurane differently affect mitochondrial function, learning, and memory. Ann Neurol. 2012;71(5):687–98. https://doi.org/10.1002/ana.23536.
Dhall S, Do DC, Garcia M, Kim J, Mirebrahim SH, Lyubovitsky J, et al. Generating and reversing chronic wounds in diabetic mice by manipulating wound redox parameters. J Diabetes Res. 2014;2014:562625–18. https://doi.org/10.1155/2014/562625.
Li Y, Sun X, Dey SK. Entosis allows timely elimination of the luminal epithelial barrier for embryo implantation. Cell Rep. 2015;11(3):358–65. https://doi.org/10.1016/j.celrep.2015.03.035.
Hausburg MA, Dekrey GK, Salmen JJ, Palic MR, Gardiner CS. Effects of paraquat on development of preimplantation embryos in vivo and in vitro. Reprod Toxicol. 2005;20(2):239–46. https://doi.org/10.1016/j.reprotox.2005.03.006.
Hirota Y, Acar N, Tranguch S, Burnum KE, Xie H, Kodama A, et al. Uterine FK506-binding protein 52 (FKBP52)-peroxiredoxin-6 (PRDX6) signaling protects pregnancy from overt oxidative stress. Proc Natl Acad Sci U S A. 2010;107(35):15577–82. https://doi.org/10.1073/pnas.1009324107.
Adiguzel D, Sahin P, Kuscu N, Ozkavukcu S, Bektas NI, Celik-Ozenci C. Spatiotemporal expression and regulation of FoxO1 in mouse uterus during peri-implantation period. PLoS One. 2019;14(5):e0216814. https://doi.org/10.1371/journal.pone.0216814.
Sin TK, Yung BY, Siu PM. Modulation of SIRT1-Foxo1 signaling axis by resveratrol: implications in skeletal muscle aging and insulin resistance. Cell Physiol Biochem. 2015;35(2):541–52. https://doi.org/10.1159/000369718.
Costa Cdos S, Rohden F, Hammes TO, Margis R, Bortolotto JW, Padoin AV, et al. Resveratrol upregulated SIRT1, FOXO1, and adiponectin and downregulated PPARgamma1-3 mRNA expression in human visceral adipocytes. Obes Surg. 2011;21(3):356–61. https://doi.org/10.1007/s11695-010-0251-7.
Brown AK, Webb AE. Regulation of FOXO factors in mammalian cells. Curr Top Dev Biol. Elsevier. 2018:165–92.
Nogueiras R, Habegger KM, Chaudhary N, Finan B, Banks AS, Dietrich MO, et al. Sirtuin 1 and sirtuin 3: physiological modulators of metabolism. Physiol Rev. 2012;92(3):1479–514. https://doi.org/10.1152/physrev.00022.2011.
Lipphardt M, Song JW, Goligorsky MS. Sirtuin 1 and endothelial glycocalyx. Pflugers Arch. 2020;472(8):991–1002. https://doi.org/10.1007/s00424-020-02407-z.
Wu B, Feng JY, Yu LM, Wang YC, Chen YQ, Wei Y, et al. Icariin protects cardiomyocytes against ischaemia/reperfusion injury by attenuating sirtuin 1-dependent mitochondrial oxidative damage. Br J Pharmacol. 2018;175(21):4137–53. https://doi.org/10.1111/bph.14457.
Pham-Huy LA, He H, Pham-Huy C. Free radicals, antioxidants in disease and health. Int J Biomed Sci. 2008;4(2):89.
Li S, Zhu Z, Xue M, Yi X, Liang J, Niu C, et al. Fibroblast growth factor 21 protects the heart from angiotensin II-induced cardiac hypertrophy and dysfunction via SIRT1. Biochim Biophys Acta Mol basis Dis. 2019;1865(6):1241–52. https://doi.org/10.1016/j.bbadis.2019.01.019.
Yang L, Zhang B, Yuan Y, Li C, Wang Z. Oxidative stress and DNA damage in utero and embryo implantation of mice exposed to carbon disulfide at peri-implantation. Hum Exp Toxicol. 2014;33(4):424–34. https://doi.org/10.1177/0960327112474849.
Ruder EH, Hartman TJ, Blumberg J, Goldman MB. Oxidative stress and antioxidants: exposure and impact on female fertility. Hum Reprod Update. 2008;14(4):345–57. https://doi.org/10.1093/humupd/dmn011.
Liu G, Dong Y, Wang Z, Cao J, Chen Y. Restraint stress alters immune parameters and induces oxidative stress in the mouse uterus during embryo implantation. Stress. 2014;17(6):494–503. https://doi.org/10.3109/10253890.2014.966263.
Ait-Bali Y, Ba-M’hamed S, Bennis M. Prenatal paraquat exposure induces neurobehavioral and cognitive changes in mice offspring. Environ Toxicol Pharmacol. 2016;48:53–62. https://doi.org/10.1016/j.etap.2016.10.008.
Almeida LL, Teixeira AAC, Soares AF, Cunha FMD, Silva VADJ, Vieira Filho LD, et al. Effects of melatonin in rats in the initial third stage of pregnancy exposed to sub-lethal doses of herbicides. Acta Histochem. 2017;119(3):220–7. https://doi.org/10.1016/j.acthis.2017.01.003.
Michan S, Juan AM, Hurst CG, Cui Z, Evans LP, Hatton CJ et al. Sirtuin1 over-expression does not impact retinal vascular and neuronal degeneration in a mouse model of oxygen-induced retinopathy. PloS one. 2014;9(1):e85031. https://doi.org/10.1371/journal.pone.0085031.
Wan X, Wen JJ, Koo SJ, Liang LY, Garg NJ. SIRT1-PGC1alpha-NFkappaB pathway of oxidative and inflammatory stress during trypanosoma cruzi infection: benefits of SIRT1-targeted therapy in improving heart function in chagas disease. PLoS Pathog. 2016;12(10):e1005954. https://doi.org/10.1371/journal.ppat.1005954.
Nguyen LT, Mak CH, Chen H, Zaky AA, Wong MG, Pollock CA, et al. SIRT1 attenuates kidney disorders in male offspring due to maternal high-fat diet. Nutrients. 2019;11(1):146.
Yanagisawa S, Baker JR, Vuppusetty C, Koga T, Colley T, Fenwick P et al. The dynamic shuttling of SIRT1 between cytoplasm and nuclei in bronchial epithelial cells by single and repeated cigarette smoke exposure. PloS one. 2018;13(3):e0193921. https://doi.org/10.1371/journal.pone.0193921.
Jin Q, Yan T, Ge X, Sun C, Shi X, Zhai Q. Cytoplasm-localized SIRT1 enhances apoptosis. J Cell Physiol. 2007;213(1):88–97. https://doi.org/10.1002/jcp.21091.
Hwang JW, Yao H, Caito S, Sundar IK, Rahman I. Redox regulation of SIRT1 in inflammation and cellular senescence. Free Radic Biol Med. 2013;61:95–110. https://doi.org/10.1016/j.freeradbiomed.2013.03.015.
Ding YW, Zhao GJ, Li XL, Hong GL, Li MF, Qiu QM, et al. SIRT1 exerts protective effects against paraquat-induced injury in mouse type II alveolar epithelial cells by deacetylating NRF2 in vitro. Int J Mol Med. 2016;37(4):1049–58. https://doi.org/10.3892/ijmm.2016.2503.
He J, Zhang A, Song Z, Guo S, Chen Y, Liu Z, et al. The resistant effect of SIRT1 in oxidative stress-induced senescence of rat nucleus pulposus cell is regulated by Akt-FoxO1 pathway. Biosci Rep. 2019;39. https://doi.org/10.1042/BSR20190112.
Caito S, Rajendrasozhan S, Cook S, Chung S, Yao H, Friedman AE, et al. SIRT1 is a redox-sensitive deacetylase that is post-translationally modified by oxidants and carbonyl stress. FASEB J. 2010;24(9):3145–59. https://doi.org/10.1096/fj.09-151308.
Li S, Zhao G, Chen L, Ding Y, Lian J, Hong G, et al. Resveratrol protects mice from paraquat-induced lung injury: the important role of SIRT1 and NRF2 antioxidant pathways. Mol Med Rep. 2016;13(2):1833–8. https://doi.org/10.3892/mmr.2015.4710.
Komatsu T, Park S, Hayashi H, Mori R, Yamaza H, Shimokawa I. Mechanisms of calorie restriction: a review of genes required for the life-extending and tumor-inhibiting effects of calorie restriction. Nutrients. 2019;11(12). https://doi.org/10.3390/nu11123068.
Zhang T, Kraus WL. SIRT1-dependent regulation of chromatin and transcription: linking NAD(+) metabolism and signaling to the control of cellular functions. Biochim Biophys Acta. 2010;1804(8):1666–75. https://doi.org/10.1016/j.bbapap.2009.10.022.
Daitoku H, Hatta M, Matsuzaki H, Aratani S, Ohshima T, Miyagishi M, et al. Silent information regulator 2 potentiates Foxo1-mediated transcription through its deacetylase activity. Proc Natl Acad Sci U S A. 2004;101(27):10042–7. https://doi.org/10.1073/pnas.0400593101.
Song S, Chu L, Liang H, Chen J, Liang J, Huang Z, et al. Protective effects of dioscin against doxorubicin-induced hepatotoxicity via regulation of Sirt1/FOXO1/NF-kappab Signal. Front Pharmacol. 2019;10:1030. https://doi.org/10.3389/fphar.2019.01030.
Qiang L, Banks AS, Accili D. Uncoupling of acetylation from phosphorylation regulates FoxO1 function independent of its subcellular localization. J Biol Chem. 2010;285(35):27396–401. https://doi.org/10.1074/jbc.M110.140228.
Qiao L, Shao J. SIRT1 regulates adiponectin gene expression through Foxo1-C/enhancer-binding protein alpha transcriptional complex. J Biol Chem. 2006;281(52):39915–24. https://doi.org/10.1074/jbc.M607215200.
Banks AS, Kon N, Knight C, Matsumoto M, Gutierrez-Juarez R, Rossetti L, et al. SirT1 gain of function increases energy efficiency and prevents diabetes in mice. Cell Metab. 2008;8(4):333–41. https://doi.org/10.1016/j.cmet.2008.08.014.
Shao D, Zhai P, Del Re DP, Sciarretta S, Yabuta N, Nojima H, et al. A functional interaction between Hippo-YAP signalling and FoxO1 mediates the oxidative stress response. Nat Commun. 2014;5(1):1–10.
Ramandeep K, Kapil G, Harkiran K. Correlation of enhanced oxidative stress with altered thyroid profile: probable role in spontaneous abortion. Int J Appl Basic Med Res. 2017;7(1):20–5. https://doi.org/10.4103/2229-516X.198514.
Sugino N, Karube-Harada A, Sakata A, Takiguchi S, Kato H. Different mechanisms for the induction of copper-zinc superoxide dismutase and manganese superoxide dismutase by progesterone in human endometrial stromal cells. Hum Reprod. 2002;17(7):1709–14. https://doi.org/10.1093/humrep/17.7.1709.
Sugino N. The role of oxygen radical-mediated signaling pathways in endometrial function. Placenta. 2007;28(Suppl A):S133–6. https://doi.org/10.1016/j.placenta.2006.12.002.
Li J, Qi J, Yao G, Zhu Q, Li X, Xu R, et al. Deficiency of sirtuin 1 impedes endometrial decidualization in recurrent implantation failure patients. Front Cell Dev Biol. 2021;9:598364. https://doi.org/10.3389/fcell.2021.598364.
Funding
This work was supported by The Scientific Research Projects Coordination Unit of Akdeniz University (Project Number: TYL-2017-2427)
Author information
Authors and Affiliations
Contributions
KA: investigation, formal analysis, writing – original draft, visualization; EG: formal analysis; MAA: investigation, formal analysis; IU: review and editing; NA: conceptualization, writing – review and editing, funding acquisition
Corresponding author
Ethics declarations
Ethics approval
The experimental protocol was approved by the Animal Care and Use Committee of Akdeniz University Faculty of Medicine (Number of the Ethical Approval 2017.02.15).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aksu, K., Golal, E., Aslan, M.A. et al. The investigation of the role of sirtuin-1 on embryo implantation in oxidative stress–induced mice. J Assist Reprod Genet 38, 2349–2361 (2021). https://doi.org/10.1007/s10815-021-02229-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02229-7