Abstract
Purpose
To assess whether the GnRH-agonist or urinary-hCG ovulation triggers affect oocyte competence in a setting entailing vitrified-warmed euploid blastocyst transfer.
Methods
Observational study (April 2013–July 2018) including 2104 patients (1015 and 1089 in the GnRH-a and u-hCG group, respectively) collecting ≥1 cumulus-oocyte-complex (COC) and undergoing ICSI with ejaculated sperm, blastocyst culture, trophectoderm biopsy, comprehensive-chromosome-testing, and vitrified-warmed transfers at a private clinic. The primary outcome measure was the euploid-blastocyst-rate per inseminated oocytes. The secondary outcome measure was the maturation-rate per COCs. Also, the live-birth-rate (LBR) per transfer and the cumulative-live-birth-delivery-rate (CLBdR) among completed cycles were investigated. All data were adjusted for confounders.
Results
The generalized-linear-model adjusted for maternal age highlighted no difference in the mean euploid-blastocyst-rate per inseminated oocytes in either group. The LBR per transfer was similar: 44% (n=403/915) and 46% (n=280/608) in GnRH-a and hCG, respectively. On the other hand, a difference was reported regarding the CLBdR per oocyte retrieval among completed cycles, with 42% (n=374/898) and 25% (n=258/1034) in the GnRh-a and u-hCG groups, respectively. Nevertheless, this variance was due to a lower maternal age and higher number of inseminated oocytes in the GnRH-a group, and not imputable to the ovulation trigger itself (multivariate-OR=1.3, 95%CI: 0.9–1.6, adjusted p-value=0.1).
Conclusion
GnRH-a trigger is a valid alternative to u-hCG in freeze-all cycles, not only for patients at high risk for OHSS. Such strategy might increase the safety and flexibility of controlled-ovarian-stimulation with no impact on oocyte competence and IVF efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Throughout the years, each and every step in IVF has been fine-tuned, owing to technological and scientific advances. While on the one hand improving the live birth rate (LBR) per treatment is complex, on the other hand, advanced IVF tools and strategies might lead to a higher patients’ compliance by reducing the risks of complications, such as multiple pregnancies and ovarian hyperstimulation syndrome (OHSS). The efficacy, reliability, and standardization of vitrification for gamete and embryo cryopreservation are among the most important advances in the field of reproductive medicine [1, 2]. In fact, it allowed a widespread implementation of single embryo transfer (SET) strategy, the safe storage of supernumerary embryos, and the introduction of cycle segmentation approach. In this scenario, final oocyte maturation is a crucial step in controlled ovarian stimulation (COS) protocols, the latter being subject to several modifications across the last decades.
The trigger for final oocyte maturation is administered about 35–36 h before oocyte retrieval and it is critical for the re-initiation and completion of the first meiotic division (from the germinal vesicle to metaphase-II (MII) stage), as well as for oocyte cytoplasmic maturation (synthesis and relocation of cortical granules on the surface of the oocyte, organelle relocation, and cumulus expansion/mucification) [3, 4]. The timing of trigger administration is decided by the physician and is based on one or more among the following parameters: size of the growing cohort of follicles, hormonal data, COS duration, ovarian response to COS, the past endocrinological history of the patients, data from previous IVF cycles, the daily workload, and the planned transfer strategy.
Two kind of ovulation induction triggers exist: human chorionic gonadotrophin (hCG) and gonadotrophin-releasing hormone agonist (GnRH-a) [5, 6]. HCG is a glycoprotein historically extracted from urine of pregnant women (u-hCG); however, a recombinant molecule also exists (rec-hCG). U-hCG, utilized in the range 5000–10,000 IU, is still considered the gold standard trigger in conventional IVF treatments.
The application of GnRH-a trigger has been first described in the early 90s together with the introduction of GnRH antagonist COS protocols [7,8,9]. By stimulating the pituitary gland to secrete both endogenous LH and FSH, this molecule represents a more physiological stimulus thanks to its rapid activity and a shorter half-life [10,11,12]. Moreover, the shorter half-life of GnRH-a minimizes the secretion of vasoactive molecules, hence almost eradicating the risk of OHSS [13,14,15]. The stimulation to the corpora lutea and the duration of the luteal phase are reduced [16,17,18] as reflected by lower levels of estradiol, progesterone, inhibin A, and inhibin pro-αC levels [14, 16, 19, 20]. Furthermore, in comparison to hCG, GnRH-a decreases the ovarian volume and abdominal distension.
However, GnRH-a utilization as ovulation trigger is not recommended in the general IVF population with conventional luteal phase support and fresh transfer (https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Ovarian-Stimulation-in-IVF-ICSI), while it is strongly recommended in patients showing high response to COS, thus at risk of OHSS. Moreover, there are studies in literature suggesting GnRH-a utilization also in other circumstances, such as in donor cycles [15, 21,22,23], in fertility preservation [24], and in freeze-all cycles [13, 25, 26].
In literature, authors have reported a difference in oocyte and embryo competence when using GnRH-a instead of u-hCG trigger; the results are however contrasting [27]. These data include mainly fresh embryo transfer cycles with conventional luteal phase support [28, 29]. On the other hand, when the analysis is based on cryopreserved embryo transfers, no difference in maturation and fertilization rates in addition to embryo quality in day 3 has been reported in either group receiving GnRH-a or hCG ovulation trigger [23, 30,31,32,33].
In this scenario, the aim of our study was to outline putative differences in oocyte/embryo competence, represented by the mean maturation, fertilization, blastulation, euploidy, and implantation rates per cycle across women adopting either trigger and undergoing PGT-A cycles with trophectoderm biopsy and vitrified-warmed SETs. This setting constitutes a strength and novelty in the investigation of the effect of the trigger on oocyte competence. In fact, any analysis not entailing blastulation, euploidy, and cumulative live birth rates should be considered incomplete, and therefore limited to this end.
Material and methods
Study population, inclusion, and exclusion criteria
This is an observational study including 2104 consecutive patients undergoing COS for PGT-A between April 2013 and July 2018 at a private IVF center in Rome. The two groups under analysis were clustered according to the trigger strategy adopted for final oocyte maturation. Specifically, either GnRH-a (dose 0.5 ml, Suprefact, Hoechst Marion Roussel, Germany) or u-hCG (10,000 IU of intramuscular chorionic gonadotropin, IBSA, Switzerland) were administrated during the period under investigation. We did not include patients with symptoms of functional hypothalamic amenorrhea. During the observational period, 31 patients (2 and 29 in the GnRH-a and u-hCG groups, respectively) did not retrieve any cumulus oocyte complex (COC) after oocyte retrieval, and therefore were not included in the analysis (Supplementary Figure 1). The COS cycles where no MII-oocyte was retrieved (n=49) were instead included to assess the maturation rates in the two groups; however, they were not analyzed further (Supplementary Figure 1). Azoospermia was an exclusion criterion as this condition may per se impact oocyte developmental competence to the blastocyst stage [34]. The indications for PGT-A were advance maternal age (AMA), repeated implantation failure (RIF), and/or recurrent pregnancy lost (RPL). Patients requiring PGT because of monogenic conditions and structural rearrangements were not included. Approval for the retrospective analysis of these data was obtained from the IRB of Clinica Valle Giulia.
IVF protocols and procedures
Prior to starting COS, transvaginal ultrasound and basal assessment of the ovaries were performed. In all protocols, COS starts on day 2 or day 3 of the menstrual cycle with a fixed dose of recombinant or urinary gonadotrophin for 4 days. The starting dose of the medications (150–300 IU per day) was based on female age, BMI, and ovarian reserve markers. The COS protocol was chosen based upon patients’ characteristics and gynecologists’ assessment [35, 36]. The pituitary suppression in all patients was performed by administering a GnRH antagonist regimen (cetrorelix, Cetrotide, Merck-Serono; ganirelix, Orgalutran, MSD) and the injection was performed daily after the identification of a leading follicle with a mean diameter ≥13–14 mm. Follicular growth was monitored on day 5 and successively every 2 days. When at least two follicles reached ≥17–18 mm in mean diameter, the trigger for final oocyte maturation was administered either through a subcutaneous bolus of GnRH-a or an intramuscular injection of u-hCG, the choice depended on the patients’ characteristics, ovarian response, and gynecologists’ overall judgement. Oocyte retrieval was performed ~35 h after the trigger. Oocyte retrievals conducted beyond 35 h and 30 min from the trigger were excluded from the analysis. The procedures for oocyte retrieval, ICSI, embryo culture, trophectoderm biopsy, vitrification, and warming have been all described previously in detail [37,38,39]. Briefly, all embryos were cultured in a controlled humidified atmosphere (37°C, 6%CO2 and 5%O2) up to the fully expanded blastocyst stage on days 5–7. No assisted hatching was performed on day 3. Comprehensive chromosome testing was conducted either via quantitative polymerase chain reaction [40] or next generation sequencing [41] at Igenomix. In both cases, only whole chromosome meiotic aneuploidies were reported. If at least one euploid blastocyst was identified, embryo replacement was performed in a subsequent menstrual cycle. After warming, only single euploid blastocyst transfers were performed. Endometrial preparation and transfer procedures were conducted in artificial or modified natural cycles as described earlier [42].
Outcome measures and statistics
The primary outcome was the mean euploid blastocyst rate per cohort of MII oocytes, in cycles using GnRH-a rather than u-hCG. The main secondary outcome was the mean maturation rate per cohort of COCs. We also investigated the intermediate outcomes such as the mean fertilization rate per cohort of inseminated MII oocytes, the mean blastulation rate per cohort of zygotes, and the mean euploidy rate per cohort of biopsied blastocysts. Shapiro-Wilk test was used to assess a normal distribution of the continuous variables. Mann Whitney U tests were used to assess statistically significant differences (p<0.05). All outcomes were then adjusted for confounding in generalized linear models and linear regression analyses. Fisher’s exact tests were adopted to assess statistically significant difference among categorical variables (p<0.05). Whenever required, the data were adjusted through multivariate logistic regression analyses. For instance, this method was adopted to assess a putative association of the trigger strategy with (i) the risk of zero MII-oocytes collected, and (ii) the cumulative live birth delivery rate (CLBdR) per completed cycle (i.e., “The number of deliveries with at least one live birth resulting from one […] aspirated ART cycle, including all cycles in which fresh and/or frozen embryos are transferred, until one delivery with a live birth occurs or until all embryos are used, whichever occurs first” as defined by [43, 44]). All statistical analyses were conducted with SPSS (version 19; IBM, USA).
Results
We included 2104 patients undergoing ovarian stimulation for PGT-A between April 2013 and July 2018. Among them, 1015 (48%) used a GnRH-a while 1089 (52%) used an u-hCG trigger. Supplementary Figure 1 displays the flowchart of the study. The two groups analyzed (GnRH-a and u-hCG, respectively) were similar with regard to BMI, years of infertility, previous live births, previous miscarriages, previous implantation failures, and main cause of infertility, except for a higher prevalence of “endocrine-ovulatory” infertility in the GnRH-a group (4.7% versus 1.5% among patients adopting u-hCG, p<0.01) (Supplementary Table 1). The groups were also similar for COS duration (10±1.5 and 9.9±1.8 days), total dosage of medications (2732±1388 and 2816±1491 IU), and sperm factor (normozoospermic: 47% and 51%, moderate male factor, i.e., 1–2 defects: 36% and 34%, oligoasthenoteratozoospermic: 17% and 15%). Significant differences, instead, were reported with respect to maternal age (38.6±3.4 years and 40.1±3.1 years in GnRH-a and u-hCG groups, p<0.01, respectively; Supplementary Figure 2A), AMH (2.8±1.9 ng/ml and 1.5±1.2 ng/ml, p<0.01), and basal-FSH (8.0±3.3 IU/l versus 9.5±4.4 IU/l, p<0.01) (Supplementary Table 1). A significant difference can also be seen in the number of follicles with a mean diameter >15 mm on the day of trigger administration (Supplementary Figure 2B). Specifically, as shown in Supplementary Figure 2C, the administration of GnRH-a increased across the years from April 2013 to July 2018, especially in function of the number of follicles with a mean diameter >15 mm on the day of trigger. Since 2013, we have never reported severe/critical-OHSS and almost eradicated also moderate-OHSS.
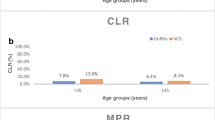
As expected, among the cycles included in this study, a higher number of COCs were retrieved in the GnRH-a group with respect to u-hCG (13.6±7.3 and 7.2±4.6, p<0.01, respectively; Supplementary Figure 3). However, the mean maturation rate per cohort of COCs was similar in the two groups, as shown in Fig. 1 across all ranges of maternal age (i.e., <35, 35–37, 38–40, 41–42, and >42 years). This was confirmed also through a generalized linear model adjusted per maternal age (p-value=0.4, partial eta-squared=0.0004, and power=0.14) and linear regression analyses among ranges of maternal age (Supplementary Table 2). MII oocyte was not retrieved in 8 out of 1015 (1%) and 41 out of 1089 (3.8%) cycles after GnRH-a and u-hCG administration, respectively. However, this risk was not associated with the type of trigger adopted. In fact, a logistic regression analysis corrected for maternal age and number of follicles with a mean diameter >15 mm on the day of trigger resulted in a multivariate-OR 0.7, 95%CI 0.3–1.6, p=0.4 for the use of u-hCG rather than GnRH-a.
The mean fertilization rate per cohort of inseminated MII oocytes was 73±20% and 73±25% and the blastulation rate per cohort of zygotes was 49±27% and 47±33%, in patients undergoing GnRH-a and u-hCG trigger, respectively. These results were confirmed also through generalized linear models adjusted per maternal age (fertilization rate: p-value=0.5, partial eta-squared=0.0002, and power=0.1; blastulation rate: p-value=0.9, partial eta-squared=0.000004, and power=0.05) and linear regression analyses among ranges of maternal age (Supplementary Table 2). The mean euploidy rate per cohort of biopsied blastocysts was higher in the GnRH-a group compared to u-hCG group (45±34% and 41±38%) as a consequence of a lower maternal age. In fact, no significant association was reported in a generalized linear model adjusted per maternal age (p-value=0.2, partial eta-squared=0.001, and power=0.23) and through linear regression analyses among ranges of maternal age (Supplementary Table 2).
The results of the primary outcome under investigation (i.e., the mean euploid blastocyst rate per cohort of inseminated MII oocytes) were different in the two groups: 17±18% and 15±21% in the GnRH-a and u-hCG groups, respectively. Again, this difference was however secondary to diverse maternal ages in the two groups. Also in this case, when the data were adjusted for maternal age, no association in favor of one of the two trigger strategies was reported (Fig. 2). The generalized linear model adjusted for maternal age highlighted a p-value=0.2, a partial eta-squared=0.001, and a power=0.23 regarding the association between the use of u-hCG trigger (rather than GnRH-a) and the mean euploid blastocyst rate per cohort of inseminated MII oocytes. Similarly, the linear regression models conducted according to ranges of maternal age confirmed an absence of significant differences (Table 1).
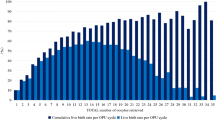
To date, the rate of completed cycles is 88% (n=898/1015) and 95% (n=1034/1089) and the LBR per vitrified-warmed single euploid blastocyst transfer was 44% (n=403/915) and 46% (n=280/608) in GnRH-a and u-hCG trigger groups, respectively. Furthermore, a difference in CLBdR among completed cycles was instead reported in favor of GnRH-a trigger utilization (n=374/898, 42% and n=258/1034, 25%) (Supplementary Table 3); however, it was due to a lower maternal age and a higher number of MII oocytes inseminated. In fact, no association between the ovulation trigger and this critical outcome was reported in the multivariate logistic regression analysis (increasing maternal age: OR=0.78, 95%CI 0.76–0.81 and p-value<0.01; increasing number of MII oocytes inseminated: OR=1.19, 95%CI 1.16–1.22 and p-value<0.01; u-hCG versus GnRH-a: OR=1.3, 95%CI 0.9–1.6 and p-value=0.1). Supplementary Table 3 displays the CLBR among completed cycles in the two ovulation trigger groups clustered according to both maternal age and number of MII oocytes inseminated.
Discussion
This study comprehensively analyzes the effect of a specific trigger utilization (GnRH-a or u-hCG) on the competence of the oocytes obtained after COS, in a setting entailing aneuploidy testing, vitrification, and SET. Throughout a 5-year period, there was no decrease in any embryological outcome under investigation (i.e., oocyte maturation, fertilization, blastulation, euploidy, and CLBdR) while the use of GnRH-a generally increased. This scenario is the consequence of a widespread use of GnRH antagonist COS at our center (i.e., the only protocol that allows the pituitary to remain responsive to GnRH-a action). Via a combined adoption of antagonist COS and GnRH-a, we contemporarily aimed at maximizing the number of competent oocytes retrieved in a single ovarian cycle, minimizing the duration of COS together with the total dose of the gonadotrophins used and, most importantly, the risk for OHSS [45]. The increasing adoption of GnRH-a trigger has been supported across these years at our center not only by the compulsory need for a freeze-all strategy necessary for PGT-A but also by the safe implementation of clinical advances, such as blastocyst culture, trophectoderm biopsy, and vitrified-warmed single euploid embryo transfer [2, 46,47,48].
Recently, Thorne and colleagues reported similar euploidy rates among cycles using either GnRH-a or u-hCG triggers [49]. Our data confirm their evidence with a more detailed investigation, including the addition of a thorough analysis of the patients’ population in which GnRH-a was adopted, the prevalence of moderate-OHSS, all the intermediate embryological outcomes like maturation, fertilization, and blastulation rates, a larger number of cycles included (539 in Thorne’s and 2651 in our study), and, lastly, a different kind of GnRH-a trigger (buserelin in our study and leuprolide acetate in theirs). This last point is particularly interesting since it is still debated whether the kind and/or dose of GnRH-a may have an effect on the clinical outcomes [50,51,52]. The reproducibility of Thorne’s data in our clinic is therefore reassuring. Still, as recommended also by the ESHRE in its recent guidelines (https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Ovarian-Stimulation-in-IVF-ICSI), future studies comparing different kinds of GnRH-a, routes of administration (e.g., sub-cutaneous or intranasal), and dose are required.
Likewise, we reported no association between the type of trigger used and the LBR per euploid blastocyst transfer (915 and 608 transfers performed in the GnRH-a and u-hCG groups, respectively), as recently suggested also by Makhijani and colleagues (145 and 118 transfers performed, respectively) [53]. Nonetheless, these authors analyzed only the first transfers, without investigating the effect of the trigger on IVF efficacy defined as CLBdR among completed cycles. For this reason, we included this crucial outcome in our study and, once the data were adjusted for maternal age and number of MII oocytes inseminated, no significant association was reported. Yet, the populations of patients receiving either one or the other trigger are too different to draw any clear conclusion.
Besides its limitations, our study was not designed to define whether a trigger strategy is better compared to the other in a given population of patients. It is rather a large retrospective survey of real-life data aimed at assessing whether the competence of the gametes retrieved was affected by the use of GnRH-a trigger rather than u-hCG. In this context, our data must be considered observational and future randomized controlled trials in identical populations of patients are encouraged. As a matter of fact, though, this analysis testifies how an increasing implementation of GnRH-a trigger across 5 years reported an absence of moderate-OHSS without any impact on IVF efficacy and efficiency. Future analyses not only limited to blastocyst culture, PGT-A, and freeze-all setting are needed. For instance, the use of GnRH-a trigger associated with protocols rescuing the luteal phase has been suggested to permit fresh embryo transfer strategies [54, 55], a possibility that deserves detailed investigations.
Poor responder patients, although representing a peculiar category of women, were not excluded from this investigation mainly for two reasons: (i) a putative impact of the trigger adopted on oocyte competence might be even more detrimental for them in view of the lower number of eggs collected, (ii) normally GnRH-a is not indicated unless the clinician wants to keep the option open for a double stimulation in the same ovarian cycle (DuoStim), an intriguing possibility that deserves valuable further insights.
Another downside of our study is the absence of hormonal assessment during COS, which is not common practice at our center. However, this is in line with the ESHRE guidelines that do not suggest a routine monitoring of LH and estradiol levels during COS since such evaluation might not involve a higher safety nor efficacy compared to ultrasound monitoring alone (https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Ovarian-Stimulation-in-IVF-ICSI).
Future studies specifically conducted in patients showing oligomenorrhea, pituitary dysfunction, or alterations of basal hormone assessment (FSH, LH, and estradiol) are desirable. In fact, these women were not included here since GnRH-a in this population is not advisable [56].
Lastly, this analysis entails only u-hCG, without rec-hCG trigger. Nevertheless, the urinary and the recombinant forms of the molecule are equally recommended from the ESHRE (https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Ovarian-Stimulation-in-IVF-ICSI) as some studies reported the absence of difference among them in terms of IVF outcomes [57, 58].
Conclusion
This observational study portrays our 5-year real-life experience with an increased utilization of GnRH-a trigger, in a clinical setting that entails blastocyst culture, trophectoderm biopsy, and vitrified-warmed euploid SET. Once comparing the use of GnRH-a to u-hCG trigger among different ranges of maternal age, similar results were reported in regard of embryological outcomes per cohort of COCs retrieved and MII oocytes inseminated. Furthermore, when adjusted for maternal age and number of MII oocytes inseminated, no significant difference has been reported in the probability of obtaining a chromosomally normal live birth after IVF in either group receiving GnRh-a or u-hCG ovulation trigger. In conclusion, this study supports the fact that GnRH-a trigger is a valid alternative to u-hCG in freeze-all cycles not only for patients at high risk for OHSS (e.g., PGT, oocyte donation, fertility preservation).
References
Iussig B, Maggiulli R, Fabozzi G, Bertelle S, Vaiarelli A, Cimadomo D, et al. A brief history of oocyte cryopreservation: arguments and facts. Acta Obstet Gynecol Scand. 2019;98(5):550–8. https://doi.org/10.1111/aogs.13569.
Rienzi L, Gracia C, Maggiulli R, LaBarbera AR, Kaser DJ, Ubaldi FM, et al. Oocyte, embryo and blastocyst cryopreservation in ART: systematic review and meta-analysis comparing slow-freezing versus vitrification to produce evidence for the development of global guidance. Hum Reprod Update. 2017;23(2):139–55. https://doi.org/10.1093/humupd/dmw038.
Cha KY, Chian RC. Maturation in vitro of immature human oocytes for clinical use. Hum Reprod Update. 1998;4(2):103–20. https://doi.org/10.1093/humupd/4.2.103.
Coticchio G, Dal Canto M, Mignini Renzini M, Guglielmo MC, Brambillasca F, Turchi D, et al. Oocyte maturation: gamete-somatic cells interactions, meiotic resumption, cytoskeletal dynamics and cytoplasmic reorganization. Hum Reprod Update. 2015;21(4):427–54. https://doi.org/10.1093/humupd/dmv011.
Dosouto C, Haahr T, Humaidan P. Advances in ovulation trigger strategies. Panminerva Med. 2019;61(1):42–51. https://doi.org/10.23736/S0031-0808.18.03537-1.
Ortega I, Garcia-Velasco JA, Pellicer A. Ovarian manipulation in ART: going beyond physiological standards to provide best clinical outcomes. J Assist Reprod Genet. 2018;35(10):1751–62. https://doi.org/10.1007/s10815-018-1258-6.
Olivennes F, Fanchin R, Bouchard P, Taieb J, Frydman R. Triggering of ovulation by a gonadotropin-releasing hormone (GnRH) agonist in patients pretreated with a GnRH antagonist. Fertil Steril. 1996;66(1):151–3. https://doi.org/10.1016/s0015-0282(16)58404-0.
Gonen Y, Balakier H, Powell W, Casper RF. Use of gonadotropin-releasing hormone agonist to trigger follicular maturation for in vitro fertilization. J Clin Endocrinol Metab. 1990;71(4):918–22. https://doi.org/10.1210/jcem-71-4-918.
Tay CC. Use of gonadotrophin-releasing hormone agonists to trigger ovulation. Hum Fertil (Camb). 2002;5(1):G35–7; discussion G8-9, G41-8. https://doi.org/10.1080/1464727992000199811.
Eppig JJ. FSH stimulates hyaluronic acid synthesis by oocyte-cumulus cell complexes from mouse preovulatory follicles. Nature. 1979;281(5731):483–4. https://doi.org/10.1038/281483a0.
Andersen CY. Possible new mechanism of cortisol action in female reproductive organs: physiological implications of the free hormone hypothesis. J Endocrinol. 2002;173(2):211–7. https://doi.org/10.1677/joe.0.1730211.
Lamb JD, Shen S, McCulloch C, Jalalian L, Cedars MI, Rosen MP. Follicle-stimulating hormone administered at the time of human chorionic gonadotropin trigger improves oocyte developmental competence in in vitro fertilization cycles: a randomized, double-blind, placebo-controlled trial. Fertil Steril. 2011;95(5):1655–60. https://doi.org/10.1016/j.fertnstert.2011.01.019.
Devroey P, Polyzos NP, Blockeel C. An OHSS-Free Clinic by segmentation of IVF treatment. Hum Reprod. 2011;26(10):2593–7. https://doi.org/10.1093/humrep/der251.
Fauser BC, de Jong D, Olivennes F, Wramsby H, Tay C, Itskovitz-Eldor J, et al. Endocrine profiles after triggering of final oocyte maturation with GnRH agonist after cotreatment with the GnRH antagonist ganirelix during ovarian hyperstimulation for in vitro fertilization. J Clin Endocrinol Metab. 2002;87(2):709–15. https://doi.org/10.1210/jcem.87.2.8197.
Humaidan P, Kol S, Papanikolaou EG, Copenhagen Gn RHATWG. GnRH agonist for triggering of final oocyte maturation: time for a change of practice? Hum Reprod Update. 2011;17(4):510–24. https://doi.org/10.1093/humupd/dmr008.
Engmann L, DiLuigi A, Schmidt D, Nulsen J, Maier D, Benadiva C. The use of gonadotropin-releasing hormone (GnRH) agonist to induce oocyte maturation after cotreatment with GnRH antagonist in high-risk patients undergoing in vitro fertilization prevents the risk of ovarian hyperstimulation syndrome: a prospective randomized controlled study. Fertil Steril. 2008;89(1):84–91. https://doi.org/10.1016/j.fertnstert.2007.02.002.
Hernandez ER, Gomez-Palomares JL, Ricciarelli E. No room for cancellation, coasting, or ovarian hyperstimulation syndrome in oocyte donation cycles. Fertil Steril. 2009;91(4 Suppl):1358–61. https://doi.org/10.1016/j.fertnstert.2008.03.077.
Cerrillo M, Rodriguez S, Mayoral M, Pacheco A, Martinez-Salazar J, Garcia-Velasco JA. Differential regulation of VEGF after final oocyte maturation with GnRH agonist versus hCG: a rationale for OHSS reduction. Fertil Steril. 2009;91(4 Suppl):1526–8. https://doi.org/10.1016/j.fertnstert.2008.08.118.
Nevo O, Eldar-Geva T, Kol S, Itskovitz-Eldor J. Lower levels of inhibin A and pro-alphaC during the luteal phase after triggering oocyte maturation with a gonadotropin-releasing hormone agonist versus human chorionic gonadotropin. Fertil Steril. 2003;79(5):1123–8. https://doi.org/10.1016/s0015-0282(03)00177-8.
Griesinger G, Berndt H, Schultz L, Depenbusch M, Schultze-Mosgau A. Cumulative live birth rates after GnRH-agonist triggering of final oocyte maturation in patients at risk of OHSS: a prospective, clinical cohort study. Eur J Obstet Gynecol Reprod Biol. 2010;149(2):190–4. https://doi.org/10.1016/j.ejogrb.2009.12.030.
Acevedo B, Gomez-Palomares JL, Ricciarelli E, Hernandez ER. Triggering ovulation with gonadotropin-releasing hormone agonists does not compromise embryo implantation rates. Fertil Steril. 2006;86(6):1682–7. https://doi.org/10.1016/j.fertnstert.2006.05.049.
Erb TM, Vitek W, Wakim AN. Gonadotropin-releasing hormone agonist or human chorionic gonadotropin for final oocyte maturation in an oocyte donor program. Fertil Steril. 2010;93(2):374–8. https://doi.org/10.1016/j.fertnstert.2008.12.015.
Galindo A, Bodri D, Guillen JJ, Colodron M, Vernaeve V, Coll O. Triggering with HCG or GnRH agonist in GnRH antagonist treated oocyte donation cycles: a randomised clinical trial. Gynecol Endocrinol. 2009;25(1):60–6. https://doi.org/10.1080/09513590802404013.
Oktay K, Turkcuoglu I, Rodriguez-Wallberg KA. GnRH agonist trigger for women with breast cancer undergoing fertility preservation by aromatase inhibitor/FSH stimulation. Reprod BioMed Online. 2010;20(6):783–8. https://doi.org/10.1016/j.rbmo.2010.03.004.
Garcia-Velasco JA. Agonist trigger: what is the best approach? Agonist trigger with vitrification of oocytes or embryos. Fertil Steril. 2012;97(3):527–8. https://doi.org/10.1016/j.fertnstert.2011.12.010.
Griesinger G, Schultz L, Bauer T, Broessner A, Frambach T, Kissler S. Ovarian hyperstimulation syndrome prevention by gonadotropin-releasing hormone agonist triggering of final oocyte maturation in a gonadotropin-releasing hormone antagonist protocol in combination with a “freeze-all” strategy: a prospective multicentric study. Fertil Steril. 2011;95(6):2029–33, 33 e1. https://doi.org/10.1016/j.fertnstert.2011.01.163.
Youssef MA, Van der Veen F, Al-Inany HG, Mochtar MH, Griesinger G, Nagi Mohesen M, et al. Gonadotropin-releasing hormone agonist versus HCG for oocyte triggering in antagonist-assisted reproductive technology. Cochrane Database Syst Rev. 2014;10:CD008046. https://doi.org/10.1002/14651858.CD008046.pub4.
Kolibianakis EM, Schultze-Mosgau A, Schroer A, van Steirteghem A, Devroey P, Diedrich K, et al. A lower ongoing pregnancy rate can be expected when GnRH agonist is used for triggering final oocyte maturation instead of HCG in patients undergoing IVF with GnRH antagonists. Hum Reprod. 2005;20(10):2887–92. https://doi.org/10.1093/humrep/dei150.
Humaidan P, Bredkjaer HE, Bungum L, Bungum M, Grondahl ML, Westergaard L, et al. GnRH agonist (buserelin) or hCG for ovulation induction in GnRH antagonist IVF/ICSI cycles: a prospective randomized study. Hum Reprod. 2005;20(5):1213–20. https://doi.org/10.1093/humrep/deh765.
Griesinger G, Kolibianakis EM, Papanikolaou EG, Diedrich K, Van Steirteghem A, Devroey P, et al. Triggering of final oocyte maturation with gonadotropin-releasing hormone agonist or human chorionic gonadotropin. Live birth after frozen-thawed embryo replacement cycles. Fertil Steril. 2007;88(3):616–21. https://doi.org/10.1016/j.fertnstert.2006.12.006.
Griesinger G, Berndt H, Schultz L, Schultze-Mosgau A, Diedrich K, von Otte S. Intensified ovarian stimulation in a GnRH antagonist protocol with agonist triggering: a prospective, clinical feasibility study. Reprod BioMed Online. 2011;22(2):133–9. https://doi.org/10.1016/j.rbmo.2010.10.017.
Eldar-Geva T, Zylber-Haran E, Babayof R, Halevy-Shalem T, Ben-Chetrit A, Tsafrir A, et al. Similar outcome for cryopreserved embryo transfer following GnRH-antagonist/GnRH-agonist, GnRH-antagonist/HCG or long protocol ovarian stimulation. Reprod BioMed Online. 2007;14(2):148–54. https://doi.org/10.1016/s1472-6483(10)60781-x.
Melo M, Busso CE, Bellver J, Alama P, Garrido N, Meseguer M, et al. GnRH agonist versus recombinant HCG in an oocyte donation programme: a randomized, prospective, controlled, assessor-blind study. Reprod BioMed Online. 2009;19(4):486–92. https://doi.org/10.1016/j.rbmo.2009.06.001.
Mazzilli R, Cimadomo D, Vaiarelli A, Capalbo A, Dovere L, Alviggi E, et al. Effect of the male factor on the clinical outcome of intracytoplasmic sperm injection combined with preimplantation aneuploidy testing: observational longitudinal cohort study of 1,219 consecutive cycles. Fertil Steril. 2017;108:961–972.e3. https://doi.org/10.1016/j.fertnstert.2017.08.033.
Rienzi L, Ubaldi FM, Iacobelli M, Minasi MG, Romano S, Ferrero S, et al. Significance of metaphase II human oocyte morphology on ICSI outcome. Fertil Steril. 2008;90(5):1692–700. https://doi.org/10.1016/j.fertnstert.2007.09.024.
Ubaldi F, Vaiarelli A, D’Anna R, Rienzi L. Management of poor responders in IVF: is there anything new? Biomed Res Int. 2014;2014:352098. https://doi.org/10.1155/2014/352098.
Capalbo A, Rienzi L, Cimadomo D, Maggiulli R, Elliott T, Wright G, et al. Correlation between standard blastocyst morphology, euploidy and implantation: an observational study in two centers involving 956 screened blastocysts. Hum Reprod. 2014;29(6):1173–81. https://doi.org/10.1093/humrep/deu033.
Cimadomo D, Capalbo A, Levi-Setti PE, Soscia D, Orlando G, Albani E, et al. Associations of blastocyst features, trophectoderm biopsy and other laboratory practice with post-warming behavior and implantation. Hum Reprod. 2018;33:1992–2001. https://doi.org/10.1093/humrep/dey291.
Maggiulli R, Cimadomo D, Fabozzi G, Papini L, Dovere L, Ubaldi FM, et al. The effect of ICSI-related procedural timings and operators on the outcome. Hum Reprod. 2020;35(1):32–43. https://doi.org/10.1093/humrep/dez234.
Treff NR, Tao X, Ferry KM, Su J, Taylor D, Scott RT Jr. Development and validation of an accurate quantitative real-time polymerase chain reaction-based assay for human blastocyst comprehensive chromosomal aneuploidy screening. Fertil Steril. 2012;97(4):819–24. https://doi.org/10.1016/j.fertnstert.2012.01.115.
Vera-Rodriguez M, Michel CE, Mercader A, Bladon AJ, Rodrigo L, Kokocinski F, et al. Distribution patterns of segmental aneuploidies in human blastocysts identified by next-generation sequencing. Fertil Steril. 2016;105(4):1047–55 e2. https://doi.org/10.1016/j.fertnstert.2015.12.022.
Vaiarelli A, Cimadomo D, Patrizio P, Venturella R, Orlando G, Soscia D, et al. Biochemical pregnancy loss after frozen embryo transfer seems independent of embryo developmental stage and chromosomal status. Reprod BioMed Online. 2018;37(3):349–57. https://doi.org/10.1016/j.rbmo.2018.05.019.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The International Glossary on Infertility and Fertility Care, 2017. Hum Reprod. 2017;32(9):1786–801. https://doi.org/10.1093/humrep/dex234.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The International Glossary on Infertility and Fertility Care, 2017. Fertil Steril. 2017;108(3):393–406. https://doi.org/10.1016/j.fertnstert.2017.06.005.
Toftager M, Bogstad J, Bryndorf T, Lossl K, Roskaer J, Holland T, et al. Risk of severe ovarian hyperstimulation syndrome in GnRH antagonist versus GnRH agonist protocol: RCT including 1050 first IVF/ICSI cycles. Hum Reprod. 2016;31(6):1253–64. https://doi.org/10.1093/humrep/dew051.
Ubaldi FM, Capalbo A, Colamaria S, Ferrero S, Maggiulli R, Vajta G, et al. Reduction of multiple pregnancies in the advanced maternal age population after implementation of an elective single embryo transfer policy coupled with enhanced embryo selection: pre- and post-intervention study. Hum Reprod. 2015;30(9):2097–106. https://doi.org/10.1093/humrep/dev159.
Capalbo A, Ubaldi FM, Cimadomo D, Maggiulli R, Patassini C, Dusi L, et al. Consistent and reproducible outcomes of blastocyst biopsy and aneuploidy screening across different biopsy practitioners: a multicentre study involving 2586 embryo biopsies. Hum Reprod. 2016;31(1):199–208. https://doi.org/10.1093/humrep/dev294.
Cimadomo D, Scarica C, Maggiulli R, Orlando G, Soscia D, Albricci L, et al. Continuous embryo culture elicits higher blastulation but similar cumulative delivery rates than sequential: a large prospective study. J Assist Reprod Genet. 2018;35:1329–38. https://doi.org/10.1007/s10815-018-1195-4.
Thorne J, Loza A, Kaye L, Nulsen J, Benadiva C, Grow D, et al. Euploidy rates between cycles triggered with gonadotropin-releasing hormone agonist and human chorionic gonadotropin. Fertil Steril. 2019;112(2):258–65. https://doi.org/10.1016/j.fertnstert.2019.03.040.
Vuong TN, Ho MT, Ha TD, Phung HT, Huynh GB, Humaidan P. Gonadotropin-releasing hormone agonist trigger in oocyte donors co-treated with a gonadotropin-releasing hormone antagonist: a dose-finding study. Fertil Steril. 2016;105(2):356–63. https://doi.org/10.1016/j.fertnstert.2015.10.014.
Pabuccu EG, Pabuccu R, Caglar GS, Yilmaz B, Yarci A, et al. J Hum Reprod Sci. 2015;8(1):25–9. https://doi.org/10.4103/0974-1208.153123.
Zarcos SM, Mejia PV, Stefani CD, Martin PS, Martin FS. Comparison of two different dosage of GnRH agonist as ovulation trigger in oocyte donors: a randomized controled trial. JBRA Assist Reprod. 2017;21(3):183–7. https://doi.org/10.5935/1518-0557.20170036.
Makhijani R, Thorne J, Bartels C, Bartolucci A, Nulsen J, Grow D, et al. Pregnancy outcomes after frozen-thawed single euploid blastocyst transfer following IVF cycles using GNRH agonist or HCG trigger for final oocyte maturation. J Assist Reprod Genet. 2020;37(3):611–7. https://doi.org/10.1007/s10815-019-01646-z.
Humaidan P, Nelson SM, Devroey P, Coddington CC, Schwartz LB, Gordon K, et al. Ovarian hyperstimulation syndrome: review and new classification criteria for reporting in clinical trials. Hum Reprod. 2016;31(9):1997–2004. https://doi.org/10.1093/humrep/dew149.
Humaidan P, Engmann L, Benadiva C. Luteal phase supplementation after gonadotropin-releasing hormone agonist trigger in fresh embryo transfer: the American versus European approaches. Fertil Steril. 2015;103(4):879–85. https://doi.org/10.1016/j.fertnstert.2015.01.034.
Kummer NE, Feinn RS, Griffin DW, Nulsen JC, Benadiva CA, Engmann LL. Predicting successful induction of oocyte maturation after gonadotropin-releasing hormone agonist (GnRHa) trigger. Hum Reprod. 2013;28(1):152–9. https://doi.org/10.1093/humrep/des361.
Youssef MA, Abou-Setta AM, Lam WS. Recombinant versus urinary human chorionic gonadotrophin for final oocyte maturation triggering in IVF and ICSI cycles. Cochrane Database Syst Rev. 2016;4:CD003719. https://doi.org/10.1002/14651858.CD003719.pub4.
Madani T, Mohammadi Yeganeh L, Ezabadi Z, Hasani F, Chehrazi M. Comparing the efficacy of urinary and recombinant hCG on oocyte/follicle ratio to trigger ovulation in women undergoing intracytoplasmic sperm injection cycles: a randomized controlled trial. J Assist Reprod Genet. 2013;30(2):239–45. https://doi.org/10.1007/s10815-012-9919-3.
Author information
Authors and Affiliations
Contributions
DC, AV, LR, and FMU conceived the study. DC and AV analyzed the data and drafted the manuscript. All authors contributed to data collection and discussion of the results.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Danilo Cimadomo and Alberto Vaiarelli are co-first authors.
Supplementary information
Supplementary Figure 1
Flowchart of the study. COS, controlled ovarian stimulation; COC, cumulus oocyte complex; MII, metaphase II. (PNG 221 kb)
Supplementary Figure 2
Distribution of the PGT-A cycles in the two groups under investigation (i.e. GnRH-agonist and urinary-hCG trigger) according to maternal age (A) and number of follicles with a mean diameter >15 mm on the day of trigger (B). Figure (C) shows the percentage of administration of GnRH-agonist and urinary-hCG trigger according to the ranges of number of follicles with a mean diameter >15 mm on the day of trigger, across the observational period (April 2013 to July 2018). The prevalence of severe and moderate-OHSS (ovarian hyperstimulation syndrome) is also reported. Statistically significant differences were assessed with Mann-Whitney U tests. (PNG 428 kb)
Supplementary Figure 3
Distribution of the PGT-A cycles in the two groups under investigation (i.e. GnRH-agonist and urinary-hCG trigger), according to the number of cumulus oocyte complexes (COCs) retrieved after oocyte pick-up. Statistically significant difference was assessed with Mann-Whitney U test. (PNG 182 kb)
ESM 1
(DOCX 33 kb)
ESM 2
(DOCX 33 kb)
ESM 3
(DOCX 44 kb)
Rights and permissions
About this article
Cite this article
Cimadomo, D., Vaiarelli, A., Petriglia, C. et al. Oocyte competence is independent of the ovulation trigger adopted: a large observational study in a setting that entails vitrified-warmed single euploid blastocyst transfer. J Assist Reprod Genet 38, 1419–1427 (2021). https://doi.org/10.1007/s10815-021-02124-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02124-1