Abstract
Purpose
This study sought to identify the initiation of placental hormonal production as defined by the production of endogenous estradiol (E2) and progesterone (P4) in a cohort of patients undergoing programmed endometrial preparation cycles with single embryo transfers resulting in live-born singletons.
Methods
In this retrospective cohort study, patients undergoing either programmed frozen-thawed embryo transfer (FET) with autologous oocytes or donor egg recipient (DER) cycles with fresh embryos were screened for inclusion. Only patients who underwent a single embryo transfer, had a single gestational sac, and a resultant live-born singleton were included. All patients were treated with E2 patches and intramuscular progesterone injections. Main outcome measures were serial E2 and P4, with median values calculated for cycle days 28 (baseline), or 4w0d gestational age (GA), through 60, or 8w4d GA. The baseline cycle day (CD) 28 median value was compared to each daily median cycle day value using the Wilcoxon signed rank test.
Results
A total of 696 patients, 569 using autologous oocytes in programmed FET cycles and 127 using fresh donor oocytes, from 4/2013 to 4/2019 met inclusion criteria. Serum E2 and P4 levels stayed consistent initially and then began to increase daily. Compared to baseline CD 28 E2 (415 pg/mL), the serum E2 was significantly elevated at 542 pg/mL (P < 0.001) beginning on CD 36 (5w1d GA). With respect to baseline CD 28 P4 (28.1 ng/mL), beginning on CD 48 (6w6d GA), the serum P4 was significantly elevated at 31.6 ng/mL (P < 0.001).
Conclusion
These results demonstrate that endogenous placental estradiol and progesterone production may occur by CD 36 and CD 48, respectively, earlier than traditionally thought.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adequate endogenous steroid hormone production, specifically estradiol (E2) and progesterone (P), is essential to sustain an early pregnancy [1]. The corpus luteum serves as the primary source of E2 and P during the first trimester of pregnancy, and its survival is generally prolonged by increasing levels of human chorionic gonadotropin (hCG) secreted by the implanted blastocyst [1]. Later during the first trimester, the placenta becomes the primary source of E2 and P production [2, 3]. This phenomenon is known as the “luteo-placental shift” and occurs gradually during the first trimester of pregnancy [4]. However, the precise timing of early placental steroidogenesis still remains poorly understood.
Identifying the precise timing of the luteo-placental shift is particularly important for pregnancies conceived via in vitro fertilization (IVF) [1, 2]. Most studies indicate that the luteal phase of IVF cycles is associated with abnormally low P levels compared to normal menstrual cycles, therefore necessitating routine luteal phase support [2, 3]. Although P supplementation during the luteal phase of IVF cycles is almost globally agreed upon, there is no consensus regarding its optimal duration [5, 6]. The optimal duration of luteal support in programmed frozen-thawed embryo transfer (FET) cycles or donor egg recipients (DER) cycles where the corpus luteum is absent is even more elusive.
Navot et al. [7] were among the first to recognize that patients with ovarian failure who conceived via IVF using donor oocytes provided a unique in vivo population to study placental steroidogenesis. As these patients are provided exogenous hormonal support at fixed doses and lack hormonal contribution from the corpus luteum, the investigators postulated that serum E2 and P levels would remain fairly constant until the initiation of placental steroidogenesis. Once placental production of E2 and P began, serum levels of these hormones would rise above basal levels.
Based on this background, the primary objective of this study is to identify the initiation of early placental steroidogenesis using pregnancies conceived via ART without a corpus luteum at our center, namely, with donor egg recipients and patients undergoing programmed frozen-thawed embryo transfer using autologous oocytes.
Materials and methods
Cycle inclusion criteria
The institutional review board at Weill Cornell Medical College approved our study protocol. For this retrospective cohort study, we sought to identify all patients who underwent either fresh or frozen embryo transfer without a corpus luteum. All patients initiating IVF cycles with anonymous donor oocytes or initiating programmed FET cycles at the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine between April 2013 and April 2019 resulting in live births after embryo transfer (ET) were analyzed for potential inclusion. Only patients who underwent a single embryo transfer, had a single gestational sac, and a resultant live-born singleton were included. Cycles not resulting in live births, cycles with multiple gestational sacs, and cycles canceled prior to ET or with incomplete records were excluded. Cycles utilizing surgically retrieved sperm or donor sperm were also excluded.
Clinical and laboratory protocols
Ovarian stimulation, human chorionic gonadotropin (hCG) trigger, oocyte retrieval, embryo culture, and embryo transfer (ET) were performed per our standard protocols [8]. Anonymous oocyte donors were started on oral contraceptive pills (Ortho-Novum, Janssen Pharmaceuticals, Beerse, Belgium) for pretreatment follicular synchronization. Ovarian stimulation was carried out to maximize follicular response while minimizing the risk of ovarian hyperstimulation syndrome (OHSS). The initial gonadotropin dose was based on age, weight, antral follicle count, and previous response to stimulation, if any. Oocyte donors were stimulated with gonadotropins (Follistim, Merck, Kenilworth, NJ, USA; Gonal-F, EMD-Serono, Geneva, Switzerland; and/or Menopur, Ferring Pharmaceuticals Inc., Parsippany, NJ, USA), with ovulation being suppressed with once daily 0.25-mg Ganirelix Acetate (Merck, Kenilworth, NJ, USA) or Cetrotide (EMD-Serono, Geneva, Switzerland) injections based on a previously described flexible protocol [8].
hCG was used as the ovulation trigger in the majority of cycles in the two earliest years of the study, and a dual trigger with hCG and GnRH agonist was used routinely thereafter. hCG was administered according to a sliding scale (10,000 IU for E2 < 1500 pg/mL, 5000 IU for E2 1501–2500 pg/mL, 4000 IU for E2 2501–3000 pg/mL, and 3300 IU for E2 > 3001 pg/mL) [8]. Generally, the trigger was given when the two lead follicles attained a mean diameter > 17 mm. Oocyte retrieval was performed with transvaginal ultrasound guidance under conscious sedation approximately 35–36 h after hCG administration. All retrieved oocytes were exposed to 40 IU recombinant hyaluronidase (Cumulase, Halozyme Therapeutics Inc., San Diego, CA, USA) to remove the cumulus-corona complex [9, 10].
Our center routinely performs intracytoplasmic sperm injection (ICSI) for all patients undergoing IVF with donor oocytes. Sperm injection was carried out based on previously described protocols [9, 10]. The spermatozoon selected for injection was based on head morphology, midpiece and flagellar shape, and dynamic characteristics such as swimming patterns and progression [9, 10]. Oocytes were examined 12–17 h after ICSI for the presence of two distinct pronuclei (PN) and two clear polar bodies. All embryos were cultured using in-house culture media.
All donor oocyte recipients and patients using autologous oocytes who are ovulatory were downregulated with leuprolide acetate in the preceding luteal phase, and patients using autologous oocytes who were anovulatory were not downregulated. The endometrium was synchronized with estradiol patches 0.1 mg (Vivelle-Dot, Novartis International AG, Basel, Switzerland) changed every other day with number of patches up-titrated as needed. Patients who are downregulated with GnRH agonist have ultrasonography performed at baseline prior to estrogen start to ensure a thin endometrial lining and the absence of follicles and then again prior to progesterone start to ensure the endometrium is >7 mm and has a trilaminar appearance and there are no growing follicles. Patients who do not undergo downregulation have an additional ultrasound performed 1 week after estrogen start to ensure there is no dominant follicle emerging. Intramuscular progesterone (50 mg/mL) was initiated with a half dose (25 mg or 0.5 mL) followed by a full dose (1.0 mL) thereafter. The day of progesterone start defaulted to cycle day (CD) 14. Vaginal progesterone is not used in patients at our center unless there is a contraindication to continued intramuscular use (e.g., allergic reaction or injection site infection), and only patients that used intramuscular progesterone were included. Donor egg recipients underwent fresh embryo transfer of a single embryo, predominantly with blastocysts on day 5 (CD 19) but occasionally with cleavage stage embryos on day 3 (CD 17). Patients using frozen-thawed autologous embryos underwent ET on the 7th day of progesterone administration. Endometrial preparation for programmed FETs with autologous embryos is identical to the preparation protocol described here for donor cycles.
All ETs that were performed were performed with Wallace catheters (Smiths Medical Inc., Norwell, MA, USA) at approximately 1 cm less than the uterine depth identified at prior trial transfer. Luteal support consisted of intramuscular progesterone (50 mg daily) and 2 estradiol patches changed every other day. Titration of estrogen patches and progesterone doses were made based on measured serum levels with adjustments of doses as deemed necessary starting at the 9th week of gestation and continued until 10–12 weeks of gestation.
Hormone measurements
Measurements of serum E2, P, and bhCG were performed daily in our center’s laboratory using the IMMULITE 2000 Immunoassay System (Siemens, Berlin, Germany). Analyzers in our laboratory undergo daily quality control monitored by the New York State Department of Health, and clinical validation between machines is performed every 6 months. The sensitivity of the E2, P, and bhCG assay is 20 pg/mL, 0.2 ng/mL, and 0.4 mIU/mL, respectively. All intra- and inter-assay variation coefficients are < 10. All samples with E2 levels greater than 1200 pg/mL are diluted before repeating the assay to obtain results within the range of maximum accuracy.
Study variables
Demographic and baseline characteristics recorded for all recipients included age, BMI (kg/m2), gravidity, parity, and day of embryo transfer. CD 14, 17, 19, and 28 represented the day of oocyte retrieval, day-3 ET, day-5 ET, and pregnancy test, respectively. Once a positive pregnancy test was noted on CD 28 (baseline at 4 weeks gestational age), serum E2, P, and bhCG levels were obtained regularly until CD 60. Serum levels were obtained more frequently in early pregnancy, often between 2 and 4 days apart until normal trends were determine and then spaced out to weekly. The primary outcomes for this study were serum E2 and P levels. Median serum E2 and P levels for each day were compared to the median serum E2 and P levels on CD 28 (baseline). All clinical pregnancies were confirmed using transvaginal ultrasonography, noting the number of gestational sacs and fetuses with cardiac activity. Any viable birth after 24 weeks of gestation was considered a live birth.
Statistical analysis
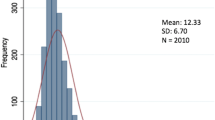
Continuous variables were checked for normality and expressed as mean ± standard deviation (SD). Categorical variables were expressed as number of cases (n) and percentage of occurrence (%). Non-parametric data were expressed as median (interquartile range [IQR]). The Wilcoxon signed rank test was utilized to compare median serum E2 and P levels on each cycle day after a positive pregnancy test to baseline serum E2 and P levels on CD 28. Statistical significance was set at P < 0.05. Statistical analyses were performed using STATA version 13 (College Station, TX: StataCorp LP).
Results
A total of 696 patients, 569 using autologous oocytes in programmed FET cycles and 127 using donor oocytes, who had a single embryo transfer with a resultant single sac and singleton livebirth met inclusion criteria. The majority of embryos transferred were blastocysts (566/569 of autologous embryos in programmed FET and 112/127 in donor cycles).
For patients who received donor oocytes, the mean age of recipients was 42.5 years old and median BMI was 23.5 kg/m2. For patients who used autologous oocytes, the mean age was 37.2 years old and the median BMI was 21.9 kg/m2. Table 1 summarizes the baseline characteristics of the DER and programmed FET patients.
Table 2 summarizes the serum E2 and P levels by CD in all patients with singleton births with a single gestational sac. The serum E2 level (542 pg/mL) on CD 36 (5w1d GA) was the first E2 level to be found significantly higher (P < 0.001) than the baseline serum E2 level (415 pg/mL) on CD 28. All serum E2 levels after CD 36 were found to be higher than the baseline level. Similarly, compared to the baseline P level (28.1 ng/mL) on CD 28, the serum P level (31.6 ng/mL) on CD 48 (6w6d GA) was found to be significantly higher (P = 0.02) and remained significantly higher on most subsequent cycle days. Figures 1 and 2 show the rise of serum E2 and P levels, respectively, for all singleton births. As evident in the figures, an increase in serum E and P levels was noted as the pregnancy progressed, with arrows indicating significant changes in serum E2 and P levels compared to CD 28 levels.
Comment
Our findings, based on a model of pregnancies that lack a corpus luteum, suggest that placental steroidogenesis can occur as early as 5 weeks of gestation, with placental E2 and P production occurring by CD 36 (5w1d GA) and CD 48 (6w6d GA), respectively. Although these cycle days indicate a statistical change in serum E2 and P levels compared to baseline levels on CD 28, the upward trend in serum E2 and P levels prior to CD 36 and CD 48 suggests that the steroidogenic activity of the placenta is ongoing throughout the prior cycle days as well.
In the normal menstrual cycle, the luteal phase begins with the luteinizing hormone (LH) surge, and lasts between 12 and 16 days with an average of 14 days [1, 2]. During the luteal phase, LH induces biochemical changes in the corpus luteum resulting in granulosa cell production of E2 and P [2]. These hormones, specifically P, increase the thickness and vascularity of the endometrial lining in anticipation of implantation [11, 12]. In the absence of implantation, luteolysis occurs, followed by menses. However, once implantation occurs, the trophoblastic tissue produces hCG, which stimulates the corpus luteum to further produce E2 and P [2, 12]. Thus, the corpus luteum maintains an early pregnancy until the placenta can maintain adequate E2 and P production at approximately 7–8 weeks of gestation, i.e., the luteo-placental shift [2, 3].
Csapo first proposed the timing of the luteo-placental shift based on his landmark luteectomy studies [13, 14]. He demonstrated that excision of the corpus luteum after 8 weeks of gestation would still result in a normal pregnancy, suggesting that placental steroidogenesis occurred before the 8th week of gestation. In contrast, luteectomy before 7 weeks of gestation resulted in an abrupt decrease in serum P levels, ultimately leading to miscarriage. However, supplementation with P in these patients salvaged those pregnancies.
One direct implication of Csapo’s findings is within the realm of luteal phase support for pregnancies conceived via IVF. Even the earliest reports of IVF success noted an abnormal luteal phase following ovarian stimulation [15]. Subsequent studies have confirmed the findings of luteal phase dysfunction in stimulated IVF cycles [16,17,18]. Several theories have been proposed to explain these findings, namely, hCG-induced LH suppression, granulosa cell removal during oocyte retrieval, and GnRH agonist-induced pituitary suppression [2, 3]. Therefore, adequate luteal phase support is essential during IVF cycles. This is frequently achieved with progesterone supplementation, and sometimes with or without hCG, GnRH agonist, or estrogen [3]. The ideal duration of luteal phase support remains a subject of debate, but is generally continued until 8 weeks of gestation or beyond based on Csapo’s studies.
The measurement of serial E2 and P levels in a donor oocyte-recipient model has been used previously to identify early placental steroidogenesis. In one of the earliest studies consisting of 8 patients with ovarian failure, Navot et al. [7] achieved 2 successful pregnancies during which a significant rise in E2 and P levels occurred during the 11th and 12th week of gestation, respectively. Treatment with exogenous estrogen was continued up to the 11th week of gestation, while treatment with progesterone was continued to 18–22 weeks of gestation. In a similar study consisting of 17 patients with primary ovarian failure, Devroey et al. [19] reported 9 live births, including one set of twins. Based on serial measurements of E2 and P levels, Devroey et al. suggested that the luteo-placental shift occurred before the 7th week of gestation in singletons, and as early as 5 weeks of gestation in twin pregnancies. In Scott et al.’s [20] study of nine patients with ovarian failure who conceived with donor oocytes, the E2 and P levels were significantly increased during the 6th and 7th week of gestation, respectively, with secretion for both possibly beginning during the 5th week of gestation. Finally, in a small study of 4 patients with ovarian failure undergoing IVF with donor oocytes, Schneider et al. [21] suggested that the feto-placental unit was competent at 10–12 weeks of gestation. The results of these studies are different due to their small sample sizes. Yet, they established the biological feasibility of simulating the hormonal milieu of early pregnancy with exogenous hormonal supplementation.
Compared to the small sample sizes of the aforementioned studies, the large cohort of the current study is one of its major strengths. By limiting the inclusion criteria to only live births, our analysis possibly identifies early placental steroidogenesis and the luteo-placental shift more accurately compared to earlier studies. By analyzing the rise of E2 and P levels in singleton births from a single embryo transfer with a single observed gestational sac, we are also able to account for variations in placental steroidogenesis based on placental mass.
More recently, Neumann et al. [22] elegantly described progesterone elevation patterns in 88 early pregnancies supported by dydrogesterone, which does not cross-react with progesterone assays. That study found substantial increases in progesterone to occur at the 7th week gestation, similar to this study.
Limitations
Luteal phase support can be achieved with various regimens and different routes of administration [2, 3]; therefore, we remain uncertain whether the rise in E2 and P levels and subsequent placental steroidogenesis noted in this study would remain the same with other forms of luteal support. Furthermore, since in this study model there is exogenous hormone supplementation, the precise detection of the initiation of steroidogenesis from the placenta is masked by the serum steroid hormones levels attributed to the exogenous support, and even constant exogenous support may have inherent serum fluctuations as detected by immunoassay as seen with the estradiol levels. Furthermore, the study did not control for adjustments to the dose of support that were made based on prior serum values, which are done as per attending physician discretion. This is reflected in the analysis of progesterone levels, where the range of the median values for each cycle day is small. It should be noted that while the majority of embryos transferred were blastocysts, a small minority were at the cleavage stage and this may factor into the study’s interpretation. Our study is also limited by its retrospective nature and did not account for individual patient characteristics that may influence serum levels. Thus, recommendations for the duration of luteal support, specifically P supplementation, in IVF cycles utilizing donor oocytes or in programmed FET cycles cannot be made based on the data provided here.
Some prospective data allow limited extrapolation of our results to IVF cycles with autologous oocytes. In a prospective, controlled trial of 220 patients undergoing IVF-ICSI, Kohls et al. [6] randomized patients to cessation of luteal phase vaginal P at 5 weeks (early) or 8 weeks (standard). Despite more bleeding episodes in the early cessation group, the overall ongoing pregnancy and spontaneous miscarriage rates were similar in the two groups. In another prospective, randomized, controlled trial of 200 IVF-ICSI patients, Kyrou et al. [23] found no difference in ongoing pregnancy or spontaneous miscarriages rates between patients who stopped luteal phase vaginal P as early as 16 days after ET compared to patients who received 7 weeks of standard luteal phase vaginal P. The findings of these studies further corroborate our data.
Conclusion
Our study demonstrates that placental steroidogenesis occurs as early as 5 weeks of gestation, suggesting that the luteo-placental shift may start earlier than previously reported. Yet, the optimal duration of luteal phase support either in fresh IVF cycles or IVF cycles with donor oocytes or programmed FET cycles remains contentious. In a large survey of 84 IVF centers, spanning 35 countries, accounting for over 50,000 IVF cycles, luteal phase P was continued until 10–12 weeks of gestation in 67% of these cycles [24, 25]. However, robust evidence from prospective, randomized, controlled trials suggests that luteal phase support beyond 7 weeks may be unnecessary for fresh IVF cycles. In light of this data, shortening the duration of luteal phase support warrants further investigation and consideration in patients undergoing fresh ET with donor oocytes or programmed FET using autologous oocytes. Prospective studies will ultimately be required to validate any modifications of existing protocols of luteal phase support in these patients.
Data availability
Data is available upon request.
References
Or Y, Vaisbuch E, Shoham Z. Luteal phase support in ART treatments. Methods Mol Biol. 2014;1154:251–60.
van der Linden M, Buckingham K, Farquhar C, Kremer JA, Metwally M. Luteal phase support for assisted reproduction cycles. Cochrane Database Syst Rev. 2015;7:CD009154.
Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Reproductive Endocrinology and Infertility. Progesterone supplementation during the luteal phase and in early pregnancy in the treatment of infertility: an educational bulletin. Fertil Steril. 2008;90(5 Suppl):S150–3.
Csapo A. The luteo-placental shift, the guardian of pre-natal life. Postgrad Med J. 1969;45(519):57–64.
Liu XR, Mu HQ, Shi Q, Xiao XQ, Qi HB. The optimal duration of progesterone supplementation in pregnant women after IVF/ICSI: a meta-analysis. Reprod Biol Endocrinol. 2012;10:107.
Kohls G, Ruiz F, Martínez M, Hauzman E, de la Fuente G, Pellicer A, et al. Early progesterone cessation after in vitro fertilization/intracytoplasmic sperm injection: a randomized, controlled trial. Fertil Steril. 2012;98(4):858–62.
Navot D, Laufer N, Kopolovic J, Rabinowitz R, Birkenfeld A, Lewin A, et al. Artificially induced endometrial cycles and establishment of pregnancies in the absence of ovaries. N Engl J Med. 1986;314(13):806–11.
Huang JY, Rosenwaks Z. Assisted reproductive techniques. Methods Mol Biol. 2014;1154:171–231.
Palermo GD, Neri QV, Schlegel PN, Rosenwaks Z. Intracytoplasmic sperm injection (ICSI) in extreme cases of male infertility. PLoS One. 2014;9(12):e113671.
Palermo GD, Kocent J, Monahan D, Neri QV, Rosenwaks Z. Treatment of male infertility. Methods Mol Biol. 2014;1154:385–405.
Munro SK, Farquhar CM, Mitchell MD, Ponnampalam AP. Epigenetic regulation of endometrium during the menstrual cycle. Mol Hum Reprod. 2010;16(5):297–310.
Norwitz ER, Schust DJ, Fisher SJ. Implantation and the survival of early pregnancy. N Engl J Med. 2001;345(19):1400–8.
Csapo AI, Pulkkinen MO, Ruttner B, Sauvage JP, Wiest WG. The significance of the human corpus luteum in pregnancy maintenance. I. Preliminary studies. Am J Obstet Gynecol. 1972;112(8):1061–7.
Csapo AI, Pulkkinen MO, Wiest WG. Effects of luteectomy and progesterone replacement therapy in early pregnant patients. Am J Obstet Gynecol. 1973;115(6):759–65.
Steptoe PC, Edwards RG, Purdy JM. Clinical aspects of pregnancies established with cleaving embryos grown in vitro. Br J Obstet Gynaecol. 1980;87(9):757–68.
Kerin JF, Broom TJ, Ralph MM, Edmonds DK, Warnes GM, Jeffrey R, et al. Human luteal phase function following oocyte aspiration from the immediately preovular graafian follicle of spontaneous ovular cycles. Br J Obstet Gynaecol. 1981;88(10):1021–8.
Garcia J, Jones GS, Acosta AA, Wright GL Jr. Corpus luteum function after follicle aspiration for oocyte retrieval. Fertil Steril. 1981;36(5):565–72.
Feichtinger W, Kemeter P, Szalay S, Beck A, Janisch H. Could aspiration of the Graafian follicle cause luteal phase deficiency? Fertil Steril. 1982;37(2):205–8.
Devroey P, Camus M, Palermo G, Smitz J, van Waesberghe L, Wisanto A, et al. Placental production of estradiol and progesterone after oocyte donation in patients with primary ovarian failure. Am J Obstet Gynecol. 1990;162(1):66–70.
Scott R, Navot D, Liu HC, Rosenwaks Z. A human in vivo model for the luteoplacental shift. Fertil Steril. 1991;56(3):481–4.
Schneider MA, Davies MC, Honour JW. The timing of placental competence in pregnancy after oocyte donation. Fertil Steril. 1993;59(5):1059–64.
Neumann K, Depenbusch M, Schultze-Mosgau A, Griesinger G. Characterization of early pregnancy placental progesterone production by utilization of dydrogesterone in programmed frozen-thawed embryo transfer cycles. Reprod Biomed. 2020;40(5):743–51.
Kyrou D, Fatemi HM, Zepiridis L, Riva A, Papanikolaou EG, Tarlatzis BC, et al. Does cessation of progesterone supplementation during early pregnancy in patients treated with recFSH/GnRH antagonist affect ongoing pregnancy rates? A randomized controlled trial. Hum Reprod. 2011;26(5):1020–4.
Ory S. Progesterone supplementation after oocyte retrieval: how long is it really needed? Fertil Steril. 2012;98(4):812.
Vaisbuch E, Leong M, Shoham Z. Progesterone support in IVF: is evidence-based medicine translated to clinical practice? A worldwide web-based survey. Reprod BioMed Online. 2012;25(2):139–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Poster Presentation at the 2019 Annual Meeting, American Society of Reproductive Medicine, Philadelphia, Pennsylvania, October 12 to 16, 2019
Rights and permissions
About this article
Cite this article
Setton, R., McCarter, K., Zimmerman, L.D. et al. Detection of early placental hormone production in embryo transfer cycles lacking a corpus luteum. J Assist Reprod Genet 38, 413–419 (2021). https://doi.org/10.1007/s10815-020-02049-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-02049-1