Abstract
Objectives
This study aimed to evaluate the role of intracytoplasmic sperm injection (ICSI) in the treatment of non-male factor infertile patients aged ≥ 39.
Methods
This is a single-center, prospective, randomized controlled clinical trial, between March 2018 and December 2019. Sixty-nine patients were recruited, and sixty patients participated in the study. Their ovaries were randomized prior to the beginning of the ovarian stimulation: the oocytes from one side (n = 257) were allocated to the ICSI (ICSI arm), while those of the contralateral side (n = 258) were allocated to conventional insemination (IVF arm). The fertilization rate per oocyte retrieved, number of zygotes (2PN), and cleavage-stage embryos were assessed and compared between the two study groups.
Results
The average number of zygotes (3.1 vs. 2.7 p = 0.45), the fertilization rate (72.4% vs. 65.1% p = 0.38), the average number of cleavage-stage (2.8 vs. 2.4 p = 0.29), and the average top-quality embryos (TQE) cleavage-stage embryos (1.7 vs. 1.6 p = 0.94) were comparable between the two groups. The TQE rate per randomized oocyte (41.2% vs. 41% p = 0.8) was also similar in both groups.
Conclusions
ICSI does not improve the reproductive outcomes of advanced-age patients undergoing conventional insemination for non-male factor infertility.
Trial registration
NCT03370068
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last decades, the use of intracytoplasmic sperm injection (ICSI) has increased dramatically, especially for non-male factor infertility. In the USA for example, the utilization of ICSI has increased from 34% in 1996 to 76% of in vitro fertilization (IVF) cycles in 2012, with the greatest increase in cycles conducted for non-male factor infertility [1]. Furthermore, in certain fertility clinics in the world, ICSI consists of 100% of the entire IVF treatment cycles [2].
Despite the increased use of ICSI, there is no clear evidence that ICSI is more effective than conventional insemination (IVF) for non-male factor infertility. There are currently few randomized controlled studies that compared the two modalities in young patient population (below 37 years of age), and none of them have shown an advantage for ICSI over conventional insemination [3, 4]. Bhattacharya et al. [3] randomized couples to IVF or ICSI, while in De Munck et al.’s [4] study, oocytes were separated to two dishes that were allocated by an electronically generated randomization list to the different insemination modalities. While using ICSI has not been demonstrated to increase fertilization, blastocyst, or pregnancy rates in non-male factor infertility compared to conventional IVF, it has been shown to reduce the total fertilization failure rate [5, 6]. However, opinions are equivocal regarding the notion whether ICSI should be used as the procedure of choice in all couples requiring assisted reproduction techniques, in order to prevent up to 30% rate of total fertilization failures in the first conventional IVF (insemination) attempt [7]. One of the major concerns in all these retrospective studies is the possibility that upon dividing the oocytes to ICSI and conventional insemination, the embryologist may select the more “mature” oocytes for ICSI, thus skewing the results in favor of ICSI.
A major concern for the use of ICSI is that the procedure prevents natural sperm selection, with equivocal observations regarding the association between ICSI and increased prevalence of neonatal malformations [6, 8].
Whether ICSI improves the fertilization rate and the overall IVF outcome in advanced maternal-age patients, with non-male factor infertility, is even more controversial [9,10,11,12]. To our knowledge, a prospective randomized controlled trial comparing conventional insemination (IVF) vs. ICSI on sibling oocytes for advanced maternal-age patients, without skewing the results by the embryologists, has not been performed yet. Prompted by the aforementioned information, we aimed to evaluate the role of ICSI in the treatment of non-male factor infertile patients aged ≥ 39.
Materials and methods
This is a prospective, randomized clinical trial (ClinicalTrials.gov identifier: NCT03370068) of patients attending our university-affiliated infertility and IVF center, between January 2018 and January 2020. The study was approved by our institutional review board (IRB), and all participants provided a written informed consent before entry.
The inclusion criteria for participating in the study were women age 39–44 years, with BMI (body mass index) of 18–35 kg/m2, and normal sperm count (volume ≥ 1.5 ml, concentration ≥ 15 mil/ml, motility ≥ 40%, and normal morphology ≥ 4%).
Women with a fertilization rate of less than 50% in a prior cycle were not included in the study.
Stimulation protocol
Gonadotropin treatment was initiated on the 3rd day of menses with the use of recombinant FSH (Gonal F, EMD Serono). Once the leading follicle reached a size of 13 mm, or E2 levels exceeded 1200 pmol/L, co-treatment with GnRH antagonist 0.25 mg/day (Cetrotide, Serono or Orgalutran, Merck) and recombinant FSH + LH (Pergoveris, Serono) or highly purified human menopausal gonadotropin (Menopur, Ferring) were commenced. Follicle growth and hormone levels were serially monitored by ultrasound and blood tests. Triggering for final oocyte maturation was performed when the leading follicle reached 17–19 mm. Transvaginal oocyte retrieval was performed 36 h following trigger.
The patients’ ovaries were randomized prior to the beginning of the ovarian stimulation.
A computer-based randomization allocated either ICSI or conventional IVF for each ovary.
The oocytes from one side (right/left) were allocated to the ICSI (ICSI arm), while those of the contralateral side (left/right) were allocated to the conventional insemination (IVF arm).
During the ovum pickup, the oocytes were divided into ICSI/IVF group by the side from where the oocyte was collected.
Classification of embryo quality was based on previously published scoring parameters [13]; a top-quality embryo was defined as four to five blastomeres on day 2, seven or more blastomeres on day 3, equally sized blastomeres and ≤ 10% fragmentation on day 3, and no multinucleation. Luteal support was initiated 1 day after oocyte pickup and consisted of vaginal progesterone gel 90 mg/day 8% (CRINONE; Serono). Following a positive pregnancy test, ongoing pregnancies were confirmed by presence of gestational sac with fetal heart rate on ultrasound at 6–8-week gestation.
Outcomes
The primary outcome was fertilization rate (number of zygotes/number of oocytes). The secondary outcomes included number of cleavage-stage embryos, number of top-quality embryos (TQE) and TQE rate per oocyte retrieved, clinical pregnancy, and ongoing pregnancy rates.
Statistical analysis
Sample size calculation was performed for the primary outcome-fertilization rate. The average fertilization rate in this population in our clinic is 70–75%. In order to increase the fertilization rate from 75 to 85% with an alpha error of 5% and beta error of 80%, the number of oocytes needed is 500, including 250 oocytes in each group. The decision was to recruit patients until receiving 500 oocytes. It should be noted that in the original protocol, we stated that we will include 150 participants with the intent to reach 250 oocytes in each group. However, since following an interim analysis, after recruiting 50% of the patients (69 participants), we already reached the number of oocytes needed for the analysis; thus, we chose to complete the study.
Statistical analysis was performed with Student’s paired t test and chi-square, as appropriate. Results are presented as means + standard deviations; p values < 0.05 were considered significant.
Results
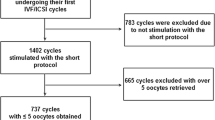
Sixty-nine patients were recruited, and sixty patients participated in the study during their IVF-ICSI cycle. Five patients were canceled during the ovarian stimulation, and 4 patients decided not to participate in the study. A flow chart of the randomization process is presented in Fig. 1.
The demographic characteristics, including age, BMI, length of stimulation, and total dose of gonadotropins used, are presented in Table 1. The number of oocytes retrieved, number of zygotes (2PN), and number of cleavage-stage embryos are present in Table 2. Five hundred and nine oocytes were retrieved, of which 258 were randomized for IVF and 257 for ICSI. The fertilization rate (72.4% vs. 65.1% p = 0.38), the average number of zygotes (3.1 vs. 2.7 p = 0.45), the average number of cleavage-stage (2.8 vs. 2.4 p = 0.29), and the average TQE cleavage-stage embryos (1.7 vs. 1.6 p = 0.94) were comparable between the two groups. The TQE rate per randomized oocyte (41.2% vs. 41% p = 0.8) was also similar in both groups.
28/60 (46.6%) of the samples were thawed donor samples. The performance of these patients was comparable to the other patients.
In one case, there were not any fertilizations in the IVF arm, and in one case, there were not any fertilizations in the ICSI arm.
Of the 60 patients included in the study, 50 performed fresh/frozen transfers. Ten patients cryopreserved their embryos for future use and were not included in the pregnancy analysis.
The overall cumulative clinical pregnancy rate was 19/50 (38%), and the cumulative ongoing pregnancy rate was 15/50 (30%) per started cycle. There was no case of OHSS.
The numbers of embryos transferred from the IVF group and ICSI group were comparable. The majority of the patients underwent a transfer of 2 embryos, one from each group, and therefore, it was not possible to perform an analysis of pregnancy rate according to the mode of insemination (ICSI or IVF).
A total of 97 embryos were transferred, 47 embryos from the IVF group and 50 embryos from the ICSI group. While focusing on the 19 patients who conceived, 4 underwent a transfer of solely ICSI-derived embryos, 3 of solely IVF-derived embryos; 12 patients received embryos derived from both IVF and ICSI.
Discussion
During the last decade, ICSI has become the common practice in many clinics around the world when treating advanced maternal-age patients with non-male infertility, without any evidence that it may improve the outcomes.
One of the possible hypothetical mechanisms, associated with improving the assisted-reproductive technique (ART) outcomes using ICSI treatment in patients with advanced maternal age, is the thickening of the zona pellucida which is known to be significantly increased in metaphase-II oocytes of older patients [14]. Bertrand et al. demonstrated that the zona pellucida of fertilized oocytes were significantly thinner than the zona pellucida of unfertilized oocytes and concluded that a thick zona pellucida could be an indication to use sperm microinjection [15].
A few retrospective studies compared the outcome of conventional insemination vs. ICSI cycles in advanced-age patients undergoing ART treatments, with non-male infertility. While Farhi et al. [10] and Maman et al. [9] described improved results for patients in the ICSI arm, Tannus et al. [11] and Bar-Hava et al. [12] could not demonstrate any advantage of ICSI over conventional insemination in women aged 40 years and over, when used for non-male factor infertility. Moreover, none of these retrospective studies controlled for skewing the results in favor of ICSI, by the embryologist, who upon dividing the oocytes to ICSI and conventional insemination, may select the more “mature” oocytes for ICSI.
A recent meta-analysis evaluated the effectiveness of ICSI compared to conventional insemination, in improving fertilization rates among women aged 38 years with a non-male factor diagnosis [16]. The meta-analysis consisted of seven studies and could not demonstrate any significant difference in fertilization rates between ICSI and conventional insemination. The authors concluded that further studies are needed to assess the impact of ICSI in this population.
To our opinion, the explanation for the conflicting results derived from these retrospective studies is the fact that the decision on which oocytes are destined to ICSI or conventional insemination is not arbitrary, with an embryologist’s preference to ICSI the more “matured” oocytes. An experienced embryologist can identify the maturity of the oocyte prior to their denudation [17], and can decide to divide the oocytes to the IVF/ICSI group by the oocytes’ maturation. This limitation was overcome in our study by randomizing the patients’ ovaries, one side for ICSI and the other for conventional insemination, leaving no option to subjective embryologist selection.
The theoretical advantage of performing conventional IVF is that the maturity of oocytes is not examined until 16–20 h after insemination and the cumulus-oocyte complex is maintained intact in the culture, allowing the immature oocytes to further complete maturation in vitro and subsequently fertilize over time.
In our study, we did not find any differences between the groups. The fertilization was non-significantly increased in the IVF group, but the number of TQE and the ratio of TQE per oocytes were comparable.
As already emphasized, the uniqueness of our study is the randomization of the ovaries from each patient, excluding the embryologist selection bias of the more matured oocyte for ICSI. Moreover, by evaluating sibling oocytes, we could control for variables, such as the stimulation protocol, patient’s age, mode of triggering, and type of gonadotropins.
Cleavage-stage embryos
One of our secondary outcomes is the number of top-quality embryos at the cleavage stage and not at the blastocyst stage. The reason for that decision was that all the patients included in the study were above the age of 39 years, and for that population, we prefer to transfer/freeze the embryos at the cleavage stage. In a previous study [18], we found that the cumulative pregnancy rate was the same for patients with a small number of cleavage-stage embryos regardless of whether the embryos were transferred on day 3 or day 5. In agreement with Racowsky et al. [19], Xiao et al. [20] have recently reported an improved pregnancy rate when transferring cleavage-stage embryos instead of growing them to the blastocyst stage, when only a single embryo was available.
Weaknesses of the study
One of the weaknesses of the present study is that we were not able to perform a pregnancy analysis per the ICSI/IVF arms, since we transferred two embryos in many cases (one embryo from each group) without knowing which one was implanted. Another weakness of the study is that four patients had only oocytes from one ovary; those patients were included in the analysis, without comparing the differences between the two sides in those cases.
To summarize, as previously mentioned, total fertilization failure, which may occasionally occur, can be extremely frustrating to couples who are undergoing IVF-only cycles [5, 6, 21]. For that reason, we believe that advanced-age patients undergoing their first IVF treatment for non-male factor infertility should be offered ICSI on half of the oocytes and conventional IVF on the majority, in order to avoid the possibility of total fertilization failure.
Conclusion
We conclude that ICSI does not improve the reproductive outcomes of advanced-age patients undergoing IVF for non-male factor infertility.
References
Boulet SL, Mehta A, Kissin DM, Warner L, Kawwass JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015;313(3):255–63.
Dyer S, Chambers GM, de Mouzon J, Nygren KG, Zegers-Hochschild F, Mansour R, et al. International Committee for Monitoring Assisted Reproductive Technologies world report: assisted reproductive technology 2008, 2009 and 2010. Hum Reprod. 2016;31(7):1588–609.
Bhattacharya S, Hamilton MPR, Shaaban M, Khalaf Y, Seddler M, Ghobara T, et al. Conventional in-vitro fertilisation versus intracytoplasmic sperm injection for the treatment of non-male-factor infertility: a randomised controlled trial. Lancet. 2001;357(9274):2075–9.
De Munck N, et al. Intracytoplasmic sperm injection is not superior to conventional IVF in couples with non-male factor infertility and preimplantation genetic testing for aneuploidies (PGT-A). Hum Reprod. 2020;35(2):317–27.
Aboulghar MA, Mansour RT, Serour GI, Sattar MA, Amin YM. Intracytoplasmic sperm injection and conventional in vitro fertilization for sibling oocytes in cases of unexplained infertility and borderline semen. J Assist Reprod Genet. 1996;13(1):38–42.
Ruiz A, Remohí J, Minguez Y, Guanes PP, Simón C, Pellicer A. The role of in vitro fertilization and intracytoplasmic sperm injection in couples with unexplained infertility after failed intrauterine insemination. Fertil Steril. 1997;68(1):171–3.
Tournaye H, Verheyen G, Albano C, Camus M, van Landuyt L, Devroey P, et al. Intracytoplasmic sperm injection versus in vitro fertilization: a randomized controlled trial and a meta-analysis of the literature. Fertil Steril. 2002;78(5):1030–7.
Davies MJ, Moore VM, Willson KJ, van Essen P, Priest K, Scott H, et al. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012;366(19):1803–13.
Maman E, Geva LL, Yerushalmi G, Baum M, Dor J, Hourvitz A. ICSI increases ongoing pregnancy rates in patients with poor response cycle: multivariate analysis of 2819 cycles. Reprod BioMed Online. 2012;25(6):635–41.
Farhi J, Cohen K, Mizrachi Y, Weissman A, Raziel A, Orvieto R. Should ICSI be implemented during IVF to all advanced-age patients with non-male factor subfertility? Reprod Biol Endocrinol. 2019;17(1):30.
Tannus S, Son WY, Gilman A, Younes G, Shavit T, Dahan MH. The role of intracytoplasmic sperm injection in non-male factor infertility in advanced maternal age. Hum Reprod. 2017;32(1):119–24.
Bar-Hava I, Orvieto R, Ferber A, Ashkenazi J, Dicker D, Ben-Rafael Z. Standard in vitro fertilization or intracytoplasmic sperm injection in advanced female age--what may be expected? Gynecol Endocrinol. 1999;13(2):93–7.
Ziebe S, Lundin K, Janssens R, Helmgaard L, Arce JC, for the MERIT (Menotrophin vs Recombinant FSH in vitro Fertilisation Trial) Group. Influence of ovarian stimulation with HP-hMG or recombinant FSH on embryo quality parameters in patients undergoing IVF. Hum Reprod. 2007;22(9):2404–13.
Kilani SS, Cooke S, Kan AK, Chapman MG. Do age and extended culture affect the architecture of the zona pellucida of human oocytes and embryos? Zygote. 2006;14(1):39–44.
Bertrand E, Van den Bergh M, Englert Y. Does zona pellucida thickness influence the fertilization rate? Hum Reprod. 1995;10(5):1189–93.
Sunderam S, Boulet SL, Kawwass JF, Kissin DM. Comparing fertilization rates from intracytoplasmic sperm injection to conventional in vitro fertilization among women of advanced age with non-male factor infertility: a meta-analysis. Fertil Steril. 2020;113(2):354–63 e1.
Batsry L, Orvieto R, Mor-Hadar D, Yung Y, Gitman H, Shimon C, et al. Can we predict oocyte maturation prior to denudation for intracytoplasmic sperm injection? Gynecol Endocrinol. 2020;36(3):265–7.
Haas J, Meriano J, Bassil R, Barzilay E, Casper RF. What is the optimal timing of embryo transfer when there are only one or two embryos at cleavage stage? Gynecol Endocrinol. 2019;35(8):665–8.
Racowsky C, Jackson KV, Cekleniak NA, Fox JH, Hornstein MD, Ginsburg ES. The number of eight-cell embryos is a key determinant for selecting day 3 or day 5 transfer. Fertil Steril. 2000;73(3):558–64.
Xiao JS, Healey M, Talmor A, Vollenhoven B. When only one embryo is available, is it better to transfer on day 3 or to grow on? Reprod BioMed Online. 2019;39(6):916–23.
Lee SH, Lee JH, Park YS, Yang KM, Lim CK. Comparison of clinical outcomes between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) in IVF-ICSI split insemination cycles. Clin Exp Reprod Med. 2017;44(2):96–104.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by our institutional review board (IRB), and all participants provided a written informed consent before entry.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jigal Haas and Tal Elkan Miller are joint first authors
Rights and permissions
About this article
Cite this article
Haas, J., Miller, T.E., Nahum, R. et al. The role of ICSI vs. conventional IVF for patients with advanced maternal age—a randomized controlled trial. J Assist Reprod Genet 38, 95–100 (2021). https://doi.org/10.1007/s10815-020-01990-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01990-5