Abstract
Purpose
This study was designed to evaluate patient management and quality of information given by French oncologists to cancer women concerning fertility issues and possibilities of fertility preservation.
Methods
An online survey was sent to 1161 physicians in all major cancer centers throughout France between May 2012 and January 2013.
Results
A total of 102 responses were received and analyzed. Only 46% of all physicians surveyed reported discussing infertility risks with patients of reproductive age and 22% referred them to a fertility center before beginning treatments. Only 14% of practitioners considered themselves knowledgeable in FP techniques and ovarian transposition was the most frequently mentioned technique in consultation.
Conclusion
This study is at the best of our knowledge the first nationwide survey to assess the state of the art in oncofertility management. It highlights inadequate management of fertility preservation for female patients in France. Physicians reported lacking knowledge and tools that would allow them to provide patients with appropriate information. A better collaboration between cancer and fertility centers needs to be organized in France as already organized in other countries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the latest statistics of The National Cancer Institute, the incidence of cancer has significantly increased in France in the past 30 years. In 1980, 170,000 new cases were diagnosed vs 400,000 in 2017 among which 214,000 in men (54%) and 186,000 in women (46%) [1].
Cancers that are most commonly diagnosed in France are breast cancer in women and prostate cancer in men. The main cancers associated with infertility risk in women are ovarian and cervical cancers, blood, and breast cancer [2]. Recently, C. Le Bihan-Benjamin has conducted a nationwide study aiming to identify the number of cancer patients eligible to fertility preservation in France. She concluded that in France, between 17,200 and 40,000 cancer patients of reproductive age are eligible to be informed about the risks to their future fertility of the treatments offered and about the available fertility preservation options [3].
Advances in cancer treatment have led to a considerable increase in life expectancy as well as the 5-year survival rate [4]. According to the data of The French National Cancer Institute, the 5-year survival rate exceeds 66% in women with good prognosis cancer (57% of cancers in women are of good prognosis) [5]. The desire of pregnancy and the ability to give birth in this population is therefore a legitimate concern and has become an important indicator of quality of life.
According to French bioethics law, patients must be informed of potential risk of iatrogenic infertility and are entitled to FP if appropriate. However, this practice is underdeveloped, especially for female patients, and is dependent upon the type of cancer, as well as the quality of information received and the motivation of the physician to provide information.
This situation was also described by Letourneau et al., taking into account other criteria such as social, racial, and demographic factors which may limit access to FP [6].
Although the field of Assisted Reproductive Technology (ART) is in constant progress, FP is not always considered as a priority for healthcare providers. Oncologists’ practices concerning their management of potential FP candidates are not well known in France. This study was therefore designated to evaluate the awareness and clinical practice of a panel of French oncologists and physicians involved in the care of female cancer patients.
Material and methods
Study design
This descriptive, observational, and multicentric study targeted all major French cancer centers throughout France territory. The online survey sent to oncologists included 24 questions, most consisting of a single short answer (n = 20), or multiple choice questions (n = 4) and could be completed in less than 10 min (Supplementary data 1). The main subjects consisted of physician characteristics (age, gender, type of institution); characteristics of oncology practice (experience duration in the field of oncology, medical specialty, frequency of young patients); information given by the oncologist on FP (frequency and contents of information given, clinical situations); importance of FP to the physician; knowledge of FP techniques; and suggestions for improving relations between cancer and fertility centers.
Data collection
As there is no registry of oncologists in France, physicians’ names were collected from the websites of all major cancer centers excluding overseas territories: Public University-Hospital centers and Regional Comprehensive Cancer Centers (CRLCC), as well as through search engines and PubMed. Specialists in male cancers and palliative care were excluded. In order to increase the number of respondents, physicians were solicited to forward the e-mail to their colleagues.
Survey sending and collection
An e-mail presenting the study was addressed to the physicians. The online survey was anonymous but allowed respondents to include their e-mail address in order to receive the study results. Telephone interviews were proposed to all physicians and were conducted at the request of the oncologists. Physicians who did not respond were contacted twice more.
Data presentation and statistical analysis
The analysis was performed using SPSS software (IBMSPSS Statistics 20.0). Qualitative data was expressed as numbers (n) and percentages (%), quantitative data as median and interquartile range.
Results
A total of 1161 physicians in 89 different French structures were contacted between May 2012 and January 2013. The final response rate after two reminders was 9% (102 responses).
Respondent characteristics
Of the 102 respondents, 46 are working in university hospitals and 56 in CRLCC. Among respondents, 58 were specialized in medical oncology (56.86%), 17 in gynecology-obstetrics (16.66%), 7 in radiology (6.86%), and 7 in pediatrics (6.86%). The majority of physicians were aged between 30 and 40 years (49%). Most respondents were hospital practitioners with a minimum of 10 years’ experience and the sex ratio was comparable (55% men and 45% women) (Table 1). The great majority of physicians (99%) managed 50 cases/year women of reproductive age. Approximately 25% respondents managed pediatric cases (pre-pubertal girls). Breast cancer represented the most frequent disease, followed by hematological malignancies and colorectal cancers (Table 2).
Patient information on infertility risk and FP management
Of the 102 physicians, nearly half (47%) reported discussing infertility risks resulting from cancer treatment with most female patients of reproductive age; 15% of the physicians reported providing this information rarely if at all. Thirty seven percent of physicians reported discussing the possibility of FP before beginning cancer treatment, and 27% rarely if at all. Twenty-two percent of physicians regularly referred patients wishing to undergo FP to an infertility center before beginning treatment, and 20% referred rarely if at all. Only 10% reported referring patients to fertility centers after receiving cancer treatment (Fig. 1).
For patients interested in FP, the majority of the oncologists (73%) reported regularly referring patients to a fertility center.
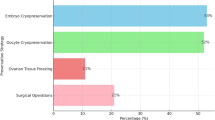
Regarding FP techniques mentioned by physicians during fertility discussion, nearly half mentioned ovarian transposition (47%), oocyte cryopreservation (45%), and ovarian tissue cryopreservation (42%). These physicians mentioned on average one to three techniques to their patients. Embryo cryopreservation was mentioned in 18% and LH-RH analogues in 21% of cases. The remaining 36% reported either not specifying any FP technique (23%) or not discussing fertility with their patients (13%).
Regarding characteristics of the illness which might dissuade oncologists from discussing FP, approximately half of them cited poor prognosis (54%) or cancer requiring urgent treatment (51%). Concerning non-medical reasons, patient age (> 40 years) was cited by 51% respondents and failure of the patient to ask for information was cited by 45% of physicians as reasons why they might not inform their patients (Fig. 2).
There was a strong disparity among physicians concerning the notion of contraindications to FP—58% indicated that FP could be contraindicated in cancer patients, whereas 42% considered there was no contraindication. The main reason given as a possible contraindication was ovarian stimulation in patients with hormone-sensitive tumors.
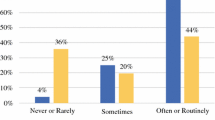
Oncologists judged themselves overall to be misinformed about current FP methods and only 14% considered themselves knowledgeable (Fig. 3).
Despite their actual practices, most physicians (60%) considered it important to inform their patients about fertility preservation. They reported interest in suggestions for improving patient management. Thus, the great majority of specialists consulted (76%) reported that educational material such as brochures might help them discuss fertility. Furthermore, close collaborations with fertility centers, as well as continuing education, were desirable (Fig. 4). Practitioners were also favorable towards the creation of an oncofertility consultation within their cancer center (76%) which to our knowledge does not exist in France.
Discussion
This study shows that oncologists report insufficient knowledge in managing FP in women with cancers. They consider the question of FP an important one and wish to benefit from training and educational materials to improve patient management. They also wish to collaborate with ART professionals to optimize information and coordinate patient care.
To the best of our knowledge, this is the first study focusing on the state of the art about oncologist awareness and attitudes in managing oncofertility throughout the French territory.
A first striking result in the current study is the low response rate (9%) which may reflect a lack of awareness of the interest of the topic of FP among oncologist in France. In another side, such a low response rate could represent a potential selection bias, as we did not have access to information of all oncologists which may be considered as a limitation in the study outcomes. However, we cannot exclude the possibility that respondents were more interested in the question than their colleagues, which may have led to an overestimation of practices.
Despite these biases, our results seem concordant with the few existing data on this subject. On average, only half of oncologists surveyed refer their patients to a fertility center for FP [7,8,9,10,11].
The American Society of Clinical Oncology (ASCO) recommends that health care providers should be knowledgeable about guidelines on fertility preservation in cancer patients in order to provide them with the adequate information about potential fertility problems related to cancer and anticancer treatments [12]. In the USA, despite of the availability of these guidelines, few American oncologists seem to follow them [10].
Concerning the situation in France, the results of our study confirm, on a larger scale, those of Preaubert whose survey was only addressed to oncologists working in Provence Alpes Côte d’Azur region (Southeastern France) and which highlighted oncologists’ need for information concerning fertility preservation techniques [13]. In order to prove that preserving fertility is becoming a real public health problem in France, a member of the National Institute of Cancer has very recently (May 2018) published a paper entitled “Fertility preservation and cancer: How many persons are concerned?” This study started in 2010 and the author has concluded that around 17,200 cancer patients (6800 women) of reproductive age are eligible to be informed about the available fertility preservation options and that access to fertility preservation is not currently offered to all the patients concerned [3].
We have shown that only half (47%) of the respondents in our study reported discussing infertility risks resulting from cancer treatment with their patients. Approximately one third (35%) reported discussing the possibility of FP before beginning cancer treatment and 26% seldom discussed if at all.
French bioethics law states that patients must be informed of toxicity and risks of treatment and are entitled to benefit from FP if appropriate [14]. One of the main components of the 2014–2019 French Cancer Plan is reducing the side effects of anticancer treatments. Furthermore, the French government put in place many research grants in the field of oncology such as “The National League against Cancer” and various other public health initiatives. In the other hand, during the last years, a significant progress has been achieved in FP techniques from which patients with cancer are eligible to benefit.
A part from the lack of awareness of oncologists about their responsibility to discuss with cancer patients’ conditions that may threaten childbearing ability, various social and emotional factors may affect fertility discussion such as age and marital status of patients, reaction to diagnosis [15], patient gender [16], tumor localization, and economic aspects such as out-of-pocket cost of FP [11].
According to our results, only 22% physicians regularly referred their patients to a fertility center before beginning treatment. The insufficient amount of information and FP coordination concur with that described by patients and similar studies. If only 47% oncologists surveyed reported discussing infertility as regular practice according to our study and others reported by the French Biomedicine Agency [17], it can therefore be estimated that only 40–50% patients who could potentially benefit from FP actually receive appropriate information.
This led us to question why physicians failed to provide information. The reasons given by respondents to our study were primarily prognosis, need for urgent cancer treatment, and age, as well as the fact that patients did not directly request the information. Among these reasons, some are surprising: although some cancers require urgent treatment, especially blood or skin cancers, it seemed contradictory that this reason was given by physicians managing other types of cancer such as some gynecological cancers especially when diagnosed in early stages. Moreover, in case of cancers requiring urgent treatment, ovarian tissue cryopreservation is currently an available option with encouraging results. It does not require ovarian stimulation and so there is no need to delay cancer therapy.
It is also surprising that 45% physicians cited “patients did not specifically ask about infertility,” revealing a poor understanding of the legal responsibility to raise the awareness of patients concerning this topic. Why oncologists were reluctant to discuss fertility: In American College of Clinical Oncology guidelines, Lee [18] proposed several hypotheses explaining why oncologists were reluctant to discuss fertility, suggesting that priorities for oncologists are to discuss serious and immediate complications resulting from the illness or treatment and do not realize the importance of fertility for the patients. Moreover, difficulty in discussing fertility is compounded by the lack of scientific data concerning gonadotoxicity of cancer treatments. Lee also mentioned the financial aspect of FP as a deterrent, irrelevant in France where cost is covered by social security. In his study, Snyder described patient characteristics such as parity, marital status, age, sexual orientation, and HIV status that could influence the decision to discuss fertility [19].
According to our study, practitioners considered themselves overall poorly trained regarding current ART techniques. Only 14% judged themselves to have a good level of knowledge on this subject. Although most oncologists considered it important to discuss infertility, and besides the medical reasons previously cited, the lack of training is another barrier to fertility discussion, because 59% of respondents considered that they received training that was insufficient for them to hold such discussions in a satisfactory manner.
According to French regional collaborative group Onco-PACA, which surveyed 225 oncology practitioners in southeastern France [13], 58% oncologists judged their knowledge of FP indications and techniques to be poor and for this reason, 33% reported difficulties in addressing this subject with their patients. This study reported exactly the same results in term of relevant training identified by oncologists. According to a survey in the USA [7], gynecological oncologists were more likely to discuss fertility than other oncologists (93 vs 60%), and to establish less gonadotoxic treatment protocols. This was not explored in the present study as gynecologists do not prescribe such treatment in France. In the current study, poor knowledge of FP was also evident from physicians’ responses mentioning ovarian transposition as the most cited FP technique, whereas certain methods such as oocyte or embryo cryopreservation seem more suitable, but were less often cited.
The question of oncologists’ knowledge of FP is made more difficult because of a lack of studies concerning gonadotoxicity of cancer treatments. Better knowledge of gonadotoxicity, although difficult to evaluate, is necessary in order to avoid unnecessary fertility preservation. Also, the scientific evaluation of fertility risk could encourage oncologists to discuss the matter with their patients. Currently, the effects of most cancer treatments have been mainly tested in animals. Pharmacovigilance, as well as cohort studies following women treated for cancers, could improve knowledge of the potential risks.
Furthermore, continuing medical education could allow oncologists who wish to do so the opportunity to improve their knowledge of oncofertility. Short training sessions, information sessions in the form of department meetings, or medical conferences could reach a greater number of oncologists.
In the present study, half of the respondents judged that a simple collaboration between their center and a fertility center could help them improving patient management regarding FP. Our results showed that most practitioners (75%) were in favor of an oncofertility consultation in their cancer center, as can be observed in other countries. To our knowledge, such collaboration is really partially developed in France. The establishment of a network (via an e-mail, a phone number) managing FP dates back to 2 to 3 years ago and the currently available FP centers are four University-Hospital centers belonging the Public Assistance of Paris Hospitals (AP-HP) (Cochin, Tenon, Antoine-Beclère, and Jean-Verdier), one center in Lille (northern France) and another in Marseille (southern France). These public centers are specifically authorized for fertility preservation and are regularly accredited according to specific criteria. However, there are still no FP centers in the private field. Given the lack of guidelines and in order to help clinicians to manage cancer patients in AP-HP institutions, experts in assisted reproduction have reported in April 2016 a repository detailing recommendations in FP. It includes legal framework of exercising FP, side effects of cancer treatments on female fertility, indications of FP, the currently available techniques, and finally the list of centers authorized to manage FP in Paris [20].
Furthermore, a group of 39 experts from different specialties (reproductive biology, oncology, gynecology…) has recently (May 2018) established a French consensus describing guidelines in managing fertility preservation in women treated for rare gynecological cancers [21].
Actually, we think that despite the availability of some recent guidelines aiming to improve patients’ care in terms of fertility preservation, lots of supplementary efforts are needed. The targeted population is still not well defined and access to FP is not currently offered to all the patients concerned [3].
Conclusion
Based on the current study results, the information on fertility preservation given to cancer patients in France is clearly insufficient. Oncologists indicated that despite the French bioethics laws, international guidelines, and their interest for this question, they are unable to give appropriate FP information to their patients. Among the various reasons cited, oncologists report lacking specific knowledge, time, and appropriate tools which would allow them to provide patients with needed information.
Fertility preservation care is currently limited in France. Only a handful of centers have developed FP, in most cases a single technique, without taking part in a true oncofertility network. The lack of knowledge of various FP techniques of certain oncologists has led them to adopt strategies of management that could not be justified. Thus, patients who may have benefited from FP are referred to centers that could not apply the most appropriate method. This may lead, in certain cases, to suboptimal FP care.
A better collaboration between cancer and fertility centers needs to be organized in France as already organized in other countries.
References
Epidémiologie. [Online]. Available: http://lesdonnees.e-cancer.fr/Themes/epidemiologie. Accessed 14 Jan 2018.
SFC. [Online]. Available: http://sfc.asso.fr/. Accessed 07 Dec 2017.
Le Bihan-Benjamin C, Hoog-Labouret N, Lefeuvre D, Carré-Pigeon F, Bousquet PJ. Fertility preservation and cancer: how many persons are concerned? Eur J Obstet Gynecol Reprod Biol. 2018;225:232–5.
Salama M, Woodruff TK. Anticancer treatments and female fertility: clinical concerns and role of oncologists in oncofertility practice. Expert Rev Anticancer Ther. 2017;17(8):687–92.
Institut National Du Cancer—Accueil. [Online]. Available: http://www.e-cancer.fr/. Accessed 05 Nov 2017.
Letourneau JM, Smith JF, Ebbel EE, Craig A, Katz PP, Cedars MI, et al. Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer. 2012;118(18):4579–88.
Forman EJ, Anders CK, Behera MA. A nationwide survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. Fertil Steril. 2010;94(5):1652–6.
Forman EJ, Anders CK, Behera MA. Pilot survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. J Reprod Med. 2009;54(4):203–7.
Köhler TS, Kondapalli LA, Shah A, Chan S, Woodruff TK, Brannigan RE. Results from the survey for preservation of adolescent reproduction (SPARE) study: gender disparity in delivery of fertility preservation message to adolescents with cancer. J Assist Reprod Genet. 2011;28(3):269–77.
Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27(35):5952–7.
Quinn GP, Vadaparampil ST, Gwede CK, Miree C, King LM, Clayton HB, et al. Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. J Cancer Surviv. 2007;1(2):146–55.
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(19):2500–10.
Préaubert L, Poggi P, Pibarot M, Delotte J, Thibault E, Saias-Magnan J, et al. Fertility preservation among patients with cancer: report of a French regional practical experience. J Gynecol Obstet Biol Reprod (Paris). 2013;42(3):246–51.
Code de la santé publique—Article L2141–1, vol. L2141–1.
Vadaparampil S, Quinn G, King L, Wilson C, Nieder M. Barriers to fertility preservation among pediatric oncologists. Patient Educ Couns. 2008;72(3):402–10.
Adams E, Hill E, Watson E. Reply: comment on ‘fertility preservation in cancer survivors: a national survey of oncologists’ current knowledge, practice and attitudes’—oncologists must not allow personal attitudes to influence discussions on fertility preservation for cancer survivors. Br J Cancer. 2013;109(7):2021–2.
AMP—Agence de la biomédecine. [Online]. Available: https://www.agence-biomedecine.fr/AMP. Accessed 08 Dec 2017.
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24(18):2917–31.
Snyder KA, Pearse W. Discussing fertility preservation options with patients with cancer. JAMA. 2011;306(2):202–3.
référentiel de préservation de fertilité AP-HP - Recherche Google. [Online]. Available: https://www.google.com/search?ei=HVEFW8_dEM6zsAeH2rDoCA&q=r%C3%A9f%C3%A9rentiel+de+pr%C3%A9servation+de+fertilit%C3%A9+AP-HP&oq=r%C3%A9f%C3%A9rentiel+de+pr%C3%A9servation+de+fertilit%C3%A9+AP-HP&gs_l=psy-ab.3..33i160k1.6066306.6079497.0.6080419.29.29.0.0.0.0.370.2553.24j4j0j1.29.0....0...1c.1.64.psy-ab..0.16.1592...35i39k1j33i21k1j33i22i29i30k1.0.TiaWeHpVqcY. Accessed 23 May 2018.
Rousset-Jablonski C, Selle F, Adda-Herzog E, Planchamp F, Selleret L, Pomel C, et al. Fertility preservation, contraception and menopause hormone therapy in women treated for rare ovarian tumors: guidelines from the French national network dedicated to rare gynaecological cancer. Bull Cancer (Paris). 2018;105(3):299–314.
Acknowledgments
We are grateful to all of the physicians who answered the survey. Special thanks to Miss Joanne Kelvin from Memorial Sloan Kettering, NYC and Miss Sylvie Duquenois from Cochin Port Royal University Hospital, Obstetrics Unit, Paris.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Amira Sallem and Joanna Shore consider that the first two authors should be regarded as joint First Authors.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Sallem, A., Shore, J., Ray-Coquard, I. et al. Fertility preservation in women with cancer: a national study about French oncologists awareness, experience, and feelings. J Assist Reprod Genet 35, 1843–1850 (2018). https://doi.org/10.1007/s10815-018-1251-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1251-0