Abstract
Purpose
The aims of this study were to assess the outcome of in vitro fertilization (IVF) in women with very low circulating anti-müllerian hormone (AMH) and to investigate factors affecting their probability of pregnancy.
Methods
The outcome of 448 IVF cycles in 361 women with circulating AMH <0.5 ng/ml was retrospectively analyzed.
Results
Cycle cancellation rate was 14.5 %; patients whose cycle was cancelled had significantly lower AMH than women who reached oocyte pickup (OPU). Among those who reached OPU, age significantly affected the success rate: despite comparable AMH levels, patients below 35 years obtained significantly more oocytes and a better clinical pregnancy rate (CPR)/OPU than patients aged 35–39 or 40–43 (31 % vs. 23.2 % vs. 10.2 %, respectively; p = 0.001). Differently, comparable IVF results were observed stratifying patients for AMH levels in the range 0.14–0.49 ng/ml. Multivariable logistic regression analysis confirmed that the probability of pregnancy was significantly affected by age, but not by small differences in AMH level.
Conclusions
Women with very low (<0.5 ng/ml) AMH levels undergoing IVF still have reasonable chances of achieving a pregnancy, but their prognosis is significantly affected by chronological age. Very low AMH levels are associated with a relevant risk of cycle cancellation but should not be considered a reason to exclude a couple from IVF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian aging is the result of the continuous decline in the extent and quality of the follicular ovarian reserve (OR) [1, 2], which may vary substantially among women of the same age [3]. Anti-müllerian hormone (AMH) is an established marker of OR and is considered the most reliable predictor of ovarian responsiveness to controlled ovarian stimulation (COS) [4]. A circulating AMH level of 0.7 ng/ml has been claimed to be the threshold value for poor ovarian responsiveness to COS [5, 6], whereas levels below 0.1–0.35 ng/ml have been associated with a high risk of cycle cancellation due to extremely poor response [7, 8].
In spite of the clear correlation between serum AMH concentration and ovarian response to COS, the role of AMH as a tool to predict IVF outcome in clinical settings is a matter of current debate. Women with serum AMH below the 10th percentile of the general population have been reported to have an overall low global chance of achieving a viable pregnancy [9], and some authors suggested 0.15–0.2 ng/ml as the AMH cutoff value below which a clinical pregnancy may rarely be obtained after in vitro fertilization (IVF) [10, 11]. Differently, other studies described ongoing pregnancies after IVF even in patients with low [12, 13] or extremely low AMH levels (<0.1 ng/ml) [14], also including patients older than 40 [15]. Obviously, these somehow conflicting results make it difficult to consider circulating AMH as the sole discriminant between women who should be offered IVF treatment and those who should be discouraged.
The aim of the present study was to assess (a) which is the probability of pregnancy of women with very low AMH concentrations (≤0.5 ng/ml) undergoing IVF and (b) which factors other than AMH may affect the possibility of conception in these women.
Materials and methods
Patients
All patients undergoing IVF at the Physiopathology of Reproduction and IVF Unit of S. Anna Hospital between March 2010 and March 2014 were retrospectively studied.
All women were below 43 years of age, because this was (and still is) the age limit to be admitted to IVF program at our institution. Overall, 2214 women underwent AMH measurement in our lab before scheduling COS, and 361 of them were found to have serum AMH <0.5 ng/ml and were enrolled in the study. This AMH level was chosen as the threshold value to be included in the study as it represented the 10th percentile value of the AMH concentration distribution in that large series of patients. Some of the enrolled women underwent more than one IVF cycle; thus, in total, 448 IVF cycles performed in 361 women were included in the analysis.
IVF procedure
Either the “long” gonadotropin-releasing hormone (GnRH)-agonist protocol or the “short” GnRH-antagonist regimen was used. The COS protocol (long or short) was decided by doctors scheduling the IVF treatment according to a real-life approach, without any specific criteria to use one or the other in each given case.
In the long protocol, pituitary suppression was obtained by administering 600 μg intranasal buserelin (Suprefact, Hoechst, Germany) starting in the mid-luteal phase of the incoming cycle and then reducing the dose to half after 14 days, at the beginning of gonadotropin administration. In the short protocol, a GnRH antagonist (Cetrotide, Merck-Serono, Germany, or Orgalutran, MSD, Germany) was given subcutaneously from stimulation day 7 (fixed regimen) at a daily dose of 0.25 mg. Either recombinant FSH (rFSH; Gonal-F, Merck-Serono, Germany, or Puregon, MSD, Germany) or the association of rFSH plus recombinant LH in a 2:1 ratio (rFSH + rLH; Pergoveris, Merck-Serono, Germany) or human menopausal gonadotropin (hMG; Meropur, Ferring, Germany) was administered to stimulate the ovary. The starting daily dose of gonadotropins was 300 IU, as established by our guidelines for women with very low AMH, but it was adjusted according to the individual response from stimulation day 6 to 7, reaching a maximum of 450 IU/die. The ovarian response to COS was monitored by transvaginal US and serum estradiol (E2) measurement every second day from stimulation day 6 to 7. Ovulation was triggered by a single injection of 10,000 IU subcutaneous hCG (Gonasi HP, Ibsa, Switzerland) when the leading follicle reached 18–20 mm diameter and estradiol concentrations were appropriate.
Oocyte pickup (OPU) was performed by transvaginal US-guided aspiration approximately 36 h after hCG injection, under local anesthesia (paracervical block). Mature, metaphase II (MII) oocytes were retrieved from the cumulus-oocyte complexes (COCs) and later inseminated using IVF or ICSI, according to clinical indication.
After 48 h of in vitro culture, one to two embryos were transferred in utero using a soft catheter (Sydney, Cook, Australia) under US guidance. No more than two embryos were transferred regardless of patient’s age, clinical history, and ovarian responsiveness; according to this policy, if more than two embryos with high morphological score were obtained, they were frozen and kept in liquid nitrogen until further use. A single embryo transfer was performed when only one embryo was available.
Intravaginal progesterone (Crinone 8, Merck-Serono, Germany, 180 mg/day) was used to support the luteal phase, starting the day of embryo transfer (ET) and keeping on for 15 days. Pregnancy was assessed by serum hCG measurement 14–15 days after ET and was then confirmed when at least one gestational sac was visualized at transvaginal US after two further weeks. Pregnant patients were further followed up by transvaginal US at 10 weeks of gestational age in order to make sure that pregnancy was going on.
Measurements
AMH was measured in the endocrinology lab of our hospital using two commercially available enzyme immunoassay kits (Immunotech® and AMH Gen II ELISA®, Beckman Coulter, Galway, UK) following the manufacturer’s instructions. The lowest detection limit of this assays is 0.14 and 0.08 ng/ml, and the maximal coefficients of variation are 12.3 and 7.7 %, respectively. The first kit was used in 2010 and first half of 2011, and the second was used later. All cases in this study were analyzed together without distinction according to the AMH assay kit because when the two kits were tested on the same samples, the consistency of results was very high (95 %).
FSH was measured in the same lab using the commercially available kit Cobas-e-601® (Roche Diagnostics, Mannheim, Germany), having a detection range 0.1–200 IU/l and coefficients of variation 3.6 and 4.5 %, respectively.
Besides AMH, the following variables were registered for each patient at every IVF cycle: age, body mass index (BMI; kg/m2), circulating basal (day 3) FSH, antral follicle count (AFC), type of COS protocol, type and total dose of administered gonadotropins, number of retrieved COCs, number of MII oocytes, number of fertilized oocytes, number of embryos available for transfer/freezing, embryo morphological score according to Holte et al. [16], and proportion of top-quality embryos (score ≥ 8 out of 10).
Clinical pregnancy was defined as the presence of one to two intrauterine gestational sacs at the first US examination, whereas ongoing pregnancy was defined as the presence of one to two viable embryos at 10 weeks of gestational age. The clinical pregnancy rate (CPR) per started cycle, per OPU, and per ET; the implantation rate (IR); the abortion rate (AR); and the ongoing pregnancy rate (OPR) per ET were calculated.
Statistical analysis
For continuous variables, the normality of distribution with or without log transformation was assessed using the Shapiro-Wilk test. Data were expressed as mean ± SD or percentages. Qualitative data were analyzed using the chi-square test or Fisher’s exact test. The significance of between-group differences was assessed using ANOVA or Kruskal-Wallis rank tests, as appropriate. Bonferroni adjustment for multiple comparisons was used when indicated.
A multivariable logistic regression model was used to assess the likelihood of becoming pregnant using age (<35, 35–39, and 40–43 years), circulating AMH levels (<0.14, 0.14–0.19, 0.2–0.29, 0.3–0.39, and 0.4–0.49 ng/ml), and AFC as covariates. All tests were two-tailed with a significance threshold set at p < 0.05.
Results
Overall, 361 women undergoing 448 IVF cycles were analyzed. Their mean age was 38.1 ± 3.4 years; their mean AMH and basal FSH serum levels were 0.2 ± 0.1 ng/ml and 10.9 ± 4.6 IU/l, respectively; and their mean AFC was 6.2 ± 3.2. These parameters identified patients as women with a reduced ovarian reserve, and therefore, they were considered expected suboptimal or poor responders to COS.
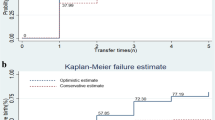
Sixty-five cycles (14.5 %) in 33 patients were cancelled due to extremely poor ovarian response (no follicle reaching 15 mm mean diameter after at least 18 days of ovarian stimulation), whereas 383 cycles in 328 patients reached OPU. Patients whose cycle was cancelled had comparable age, but significantly lower AMH and AFC, and conversely higher basal FSH concentrations, than women who reached OPU (Table 1). Furthermore, patients with cancelled cycles showed a higher prevalence of ovarian endometriosis (in situ endometrioma <4 cm diameter or history of ovarian surgery to remove an endometrioma) than women reaching OPU (Table 1).
When OPU was performed (383 cycles), immature oocytes only were recovered in 37 cycles (9.7 %), whereas in the other 346 cycles, at least one mature (MII) egg was retrieved and inseminated. Total fertilization and/or cleavage failure occurred in 49 cycles, whereas in 297 cycles, at least one viable, transferable embryo was eventually obtained and transferred in uteri.
Overall, a clinical pregnancy was obtained in 75 IVF cycles (performed in 75 patients), whereas no pregnancy occurred in 308 cycles (performed in 235 patients) out of 383 cycles arrived at OPU. Therefore, the overall CPRs were 25.2 % per ET, 19.6 % per OPU, and 16.7 % per started cycle, and the implantation rate was 17.1 %; the abortion rate was 33.3 % (25/75), leading to a 10-week OPR/ET of 16.8 %.
Comparing patients who conceived to those who did not, the first were significantly younger and had a significantly higher AFC than those who did not; however, the two groups had comparable serum basal FSH and AMH (Table 2). The presence of a small endometrioma or a history of previous ovarian surgery did not affect pregnancy chance. Similarly, no differences were observed either in the proportion of concomitant co-factors of infertility or in the type of COS protocol and administered gonadotropins (Table 2). Overall, the average number of retrieved COCs and of mature oocytes was low, as expected in patients with very low AMH levels; however, women who conceived had significantly higher oocyte yield, fertilization rate, and embryo availability than those who did not (Table 2).
When data of women who underwent OPU were stratified according to chronological age, patients below 35 years displayed a significantly higher oocyte yield and a remarkable CPR/OPU (31 %) despite their low AMH level; conversely, the oldest patients (40–43) showed a significantly lower CPR/OPU (10.2 %) and those between 35 and 39 years obtained intermediate results (CPR/OPU = 23.2 %) (Table 3).
Stratifying patients according to small increments of circulating AMH (Table 4), a better outcome was observed at the extreme values (CPR/ET = 32.1 % with AMH between 0.4 and 0.49 ng/ml vs. 17.4 % with AMH < 0.14 ng/ml), but the overall trend was not significant (p = 0.8 for OPR/ET, p = 0.57 for CPR/OPU, and p = 0.15 for CPR/started cycle) and very similar results were observed for AMH levels between 0.14 and 0.39 ng/ml (Table 4).
The multivariable logistic regression analysis confirmed that the likelihood of becoming pregnant was significantly affected by chronological age: patients aged 40–43 years were significantly less likely to get pregnant than patients below 35 (OR 0.29; 95 % CI 0.13–0.65), whereas AFC and circulating AMH (although a subtle, positive trend with increasing levels between 0.14 and 0.49 was observed) did not significantly affect the probability to conceive (Table 5).
Discussion
In the last years, a number of variables, either alone or in combination, have been used to develop prediction models of IVF outcome, so far with limited success [17, 18]. AMH is an established marker of OR, and previous work showed its value in predicting the ovarian response to COS [5, 19]. More recently, the accuracy of AMH in predicting live birth was tested by independent groups: some data showed that AMH could be used as a prognostic factor [20–22], but its predictive value at low or very low concentrations was not clearly clarified. In fact, some authors reported acceptable results in terms of clinical pregnancies even in patients with very low AMH levels (0.1–0.35) whereas others suggested their exclusion from IVF treatment due to a very poor prognosis [12, 13].
Herein, we studied 361 IVF patients with circulating AMH in the very low range (<0.5 ng/ml, a threshold that represents the 10th percentile in our IVF population) with the aim of assessing their probability of obtaining a clinical pregnancy and which variable(s) could significantly affect IVF outcome. In this population with poor prognosis, we observed 75 clinical pregnancies (leading to 16.7 % CPR/started cycle, 19.6 % CPR/OPU, and 25.3 % CPR/ET, respectively), with 50 ongoing pregnancies at 10 weeks of gestational age (leading to an OPR/ET of 16.8 %); the results suggest that a successful IVF is not very unlikely despite very low levels of serum AMH. Indeed, moderate but still reasonable pregnancy and live birth rates were reported in a series of 128 patients with AMH levels <0.4 ng/ml [13], whereas a pregnancy rate of 7.4 % per started cycle was reported in another series of 188 IVF cycles performed in 101 women with the same very low AMH levels [23]. In the largest study published so far, appreciable cumulative pregnancy rates were observed also in women with AMH concentrations between 0.02 and 0.2 ng/ml [24].
In the present study, patients who underwent cycle cancellation due to extremely poor ovarian response had significantly lower levels of AMH, lower AFC, and higher basal FSH than women who completed the cycle. Noticeably, women who underwent cycle cancellation showed a significantly increased prevalence of ovarian endometriosis or of previous surgery due to ovarian endometriosis, an observation that suggests that women complaining of ovarian endometriosis might represent a specific subgroup of patients, within those with very low AMH, at a particularly increased risk of impaired ovarian response. However, once OPU was reached, the variable endometriosis lost its impact on outcome, as no difference was detected in the prevalence of endometriosis (either current or previous disease) between patients who conceived and those who did not. These data confirm the results of a recent study in which live birth was the end point [23], and support the notion that, at least in the subgroup of women with very low AMH, the presence/story of ovarian endometriosis affects the quantitative response to stimulation, but not the competence of the oocytes and of the derived embryos.
Interestingly, in the present study, women who conceived had AMH levels comparable to those who did not; moreover, we could not observe a significant increase in the probability of pregnancy in parallel with the increase of serum AMH from <0.14 to 0.49 ng/ml. Taken together, these findings support the idea that at the lower extreme of ovarian reserve, where a larger proportion of aneuploid oocytes would be expected [25], AMH could be simply a quantitative index of ovarian responsiveness, but not a reliable marker of oocyte competence to pregnancy.
In our study, age and AFC were the only clinical parameters that were significantly different between the group of patients who conceived and those who did not. However, in the logistic regression analysis, AFC lost significance, leaving age as the only variable significantly related to IVF success. Indeed, women younger than 35 obtained a remarkable CPR/ET of 31 % and a significant trend toward a decreased success rate with increasing age was observed, despite all patients had similar, very low AMH levels. On the contrary, in the present study, no significant trend toward improving IVF outcome was observed with increasing AMH concentration. Results similar to ours were reported in another study, in which women aged <34 years having serum AMH ≤0.29 ng/ml obtained pregnancy and live birth rates comparable to those with higher AMH levels [26]. Also, a large prospective study on 769 IVF cycles reported that AMH in its lower range (0.2–1 ng/ml) was a reliable quantitative marker of the ovarian follicular pool, but performed poorly as a predictor of pregnancy [24]. Of note, no pregnancy was obtained in women above 42 years, suggesting that age, rather than AMH, is the main factor to be considered when dealing with patients with AMH in such a low range [24].
Taken together, these observations suggest that patients of relatively young age with a deeply reduced ovarian reserve may still have a favorable IVF outcome due to a well-preserved oocyte competence. This view is further supported by a recent meta-analysis that found that female age is the most important predictor of pregnancy in IVF in almost all the analyzed studies [27].
The interaction between age, AMH, and IVF success, however, is still a matter of debate. Some studies, in fact, showed a correlation between AMH and live birth rate after IVF, depending solely on oocyte yield [6, 28, 29], whereas a recent study suggested that AMH is an independent marker of pregnancy and live births after adjustment for female age and oocyte yield [30]. These somehow conflicting evidences could depend on the complexity of the interaction between age and AMH: age could affect mainly the proportion of follicles switching from the primordial to the recruitable pool, whereas AMH per se could mainly reflect the number of FSH-sensitive, recruitable follicles [9]. It was recently suggested that the intraovarian inhibiting effect of AMH on follicle recruitment could be modulated according to the patients’ age [31]. In this complex picture, the positive association between IVF success and ovarian reserve as measured by serum AMH could have variable strength according to the patient’s chronological age.
From a clinical standpoint, the most important finding of the present study is that young patients with very low AMH levels still have reasonable chances of achieving a pregnancy with IVF and they should be reassured about their reproductive prognosis. Furthermore, similar to others [29, 32], we could not identify a threshold AMH value below in which no pregnancy is likely to occur and IVF should be discouraged. Although with a significantly lower rate, we obtained clinical and ongoing pregnancies even in older patients with very low AMH levels.
Overall, our results suggest that the clinical rationale for measuring AMH prior to IVF should be limited to the prediction of ovarian response to COS and of the risk of cycle cancellation, particularly in women of more advanced reproductive age and in those with ovarian endometriosis. In view of our findings, pre-IVF AMH assessment cannot be used to exclude a couple from IVF.
References
Broekmans FJ, Knauff EA, te Velde ER, Macklon NS, Fauser BC. Female reproductive ageing: current knowledge and future trends. Trends Endocrinol Metab. 2007;18:58–65.
Steiner AZ. Clinical implications of ovarian reserve testing. Obstet Gynecol Surv. 2009;64:120–8.
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB. A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update. 2006;12:685–718.
Dewailly D, Andersen CY, Balen A, Broekmans F, Dilaver N, Fanchin R, et al. The physiology and clinical utility of anti-mullerian hormone in women. Hum Reprod Update. 2014;20:370–85.
La Marca A, Giulini S, Tirelli A, Bertucci E, Marsella T, Xella S, et al. Anti-müllerian hormone measurement on any day of the menstrual cycle strongly predicts ovarian response in assisted reproductive technology. Hum Reprod. 2007;22:766–71.
Nelson SM, Yates RW, Fleming R. Serum anti-müllerian hormone and FSH: prediction of live birth and extremes of response in stimulated cycles—implications for individualization of therapy. Hum Reprod. 2007;22:2414–21.
Muttukrishna S, Suharjono H, McGarrigle H, Sathanandan M. Inhibin B and anti-mullerian hormone: markers of ovarian response in IVF/ICSI patients? Bjog. 2004;111:1248–53.
Lekamge DN, Barry M, Kolo M, Lane M, Gilchrist RB, Tremellen KP. Anti-müllerian hormone as a predictor of IVF outcome. Reprod Biomed Online. 2007;14:602–10.
Koshy AK, Gudi A, Shah A, Bhide P, Timms P, Homburg R. Pregnancy prognosis in women with anti-müllerian hormone below the tenth percentile. Gynecol Endocrinol. 2013;29:662–5.
Nelson SM, Yates RW, Lyall H, Jamieson M, Traynor I, Gaudoin M, et al. Anti-müllerian hormone-based approach to controlled ovarian stimulation for assisted conception. Hum Reprod. 2009;24:867–75.
Merhi Z, Zapantis A, Berger DS, Jindal SK. Determining an anti-mullerian hormone cutoff level to predict clinical pregnancy following in vitro fertilization in women with severely diminished ovarian reserve. J Assist Reprod Genet. 2013;30:1361–5.
Tocci A, Ferrero S, Iacobelli M, Greco E. Negligible serum anti-mullerian hormone: pregnancy and birth after a 1-month course of an oral contraceptive, ovarian hyperstimulation, and intracytoplasmic sperm injection. Fertil Steril. 2009;92:395 e399–12.
Weghofer A, Dietrich W, Barad DH, Gleicher N. Live birth chances in women with extremely low-serum anti-mullerian hormone levels. Hum Reprod. 2011;26:1905–9.
Fraisse T, Ibecheole V, Streuli I, Bischof P, de Ziegler D. Undetectable serum anti-müllerian hormone levels and occurrence of ongoing pregnancy. Fertil Steril. 2008;89:723 e729–711.
Tokura Y, Yoshino O, Ogura-Nose S, Motoyama H, Harada M, Osuga Y, et al. The significance of serum anti-müllerian hormone (AMH) levels in patients over age 40 in first IVF treatment. J Assist Reprod Genet. 2013;30:821–5.
Holte J, Berglund L, Milton K, Garello C, Gennarelli G, Revelli A, et al. Construction of an evidence-based integrated morphology cleavage embryo score for implantation potential of embryos scored and transferred on day 2 after oocyte retrieval. Hum Reprod. 2007;22:548–57.
Marinakis G, Nikolaou D. What is the role of assisted reproduction technology in the management of age-related infertility? Hum Fertil (Camb). 2011;14:8–15.
La Marca A, Sunkara SK. Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers: from theory to practice. Hum Reprod Update. 2014;20:124–40.
Nardo LG, Gelbaya TA, Wilkinson H, Roberts SA, Yates A, Pemberton P, et al. Circulating basal anti-müllerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril. 2009;92:1586–93.
Gleicher N, Weghofer A, Barad DH. Anti-müllerian hormone (AMH) defines, independent of age, low versus good live-birth chances in women with severely diminished ovarian reserve. Fertil Steril. 2010;94:2824–7.
Brodin T, Hadziosmanovic N, Berglund L, Olovsson M, Holte J. Antimüllerian hormone levels are strongly associated with live-birth rates after assisted reproduction. J Clin Endocrinol Metab. 2013;98:1107–14.
Iliodromiti S, Kelsey TW, Wu O, Anderson RA, Nelson SM. The predictive accuracy of anti-müllerian hormone for live birth after assisted conception: a systematic review and meta-analysis of the literature. Hum Reprod Update. 2014;20:560–70.
Lukaszuk K, Kunicki M, Liss J, Bednarowska A, Jakiel G. Probability of live birth in women with extremely low anti-müllerian hormone concentrations. Reprod Biomed Online. 2014;28:64–9.
Kedem A, Haas J, Geva LL, Yerushalmi G, Gilboa Y, Kanety H, et al. Ongoing pregnancy rates in women with low and extremely low AMH levels. A multivariate analysis of 769 cycles. PLoS ONE. 2013;8:e81629.
Gianaroli L, Magli MC, Ferraretti AP, Fortini D, Tabanelli C, Gergolet M. Gonadal activity and chromosomal constitution of in vitro generated embryos. Mol Cell Endocrinol. 2000;161:111–6.
Wang JG, Douglas NC, Nakhuda GS, Choi JM, Park SJ, Thornton MH, et al. The association between anti-müllerian hormone and IVF pregnancy outcomes is influenced by age. Reprod Biomed Online. 2010;21:757–61.
van Loendersloot LL, van Wely M, Limpens J, Bossuyt PM, Repping S, van der Veen F. Predictive factors in in vitro fertilization (IVF): a systematic review and meta-analysis. Hum Reprod Update. 2010;16:577–89.
Lee RK, Wu FS, Lin MH, Lin SY, Hwu YM. The predictability of serum anti-müllerian level in IVF/ICSI outcomes for patients of advanced reproductive age. Reprod Biol Endocrinol. 2011;9:115.
Bhide P, Gudi A, Shah A, Timms P, Grayson K, Homburg R. Anti-müllerian hormone as a predictor of pregnancy following IVF. Reprod Biomed Online. 2013;26:247–52.
Brodin T, Hadziosmanovic N, Berglund L, Olovsson M, Holte J. Comparing four ovarian reserve markers—associations with ovarian response and live births after assisted reproduction. Acta Obstet Gynecol Scand. 2015;94:1056–63.
Honnma H, Baba T, Sasaki M, Hashiba Y, Oguri H, Fukunaga T, et al. Different ovarian response by age in an anti-müllerian hormone-matched group undergoing in vitro fertilization. J Assist Reprod Genet. 2012;29:117–25.
Casadei L, Manicuti C, Puca F, Madrigale A, Emidi E, Piccione E. Can anti-müllerian hormone be predictive of spontaneous onset of pregnancy in women with unexplained infertility? J Obstet Gynaecol. 2013;33:857–61.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule: Women with very low (<0.5 ng/ml) AMH levels undergoing IVF have an increased risk of cycle cancellation, and their prognosis is significantly affected by chronological age.
Rights and permissions
About this article
Cite this article
Revelli, A., Biasoni, V., Gennarelli, G. et al. IVF results in patients with very low serum AMH are significantly affected by chronological age. J Assist Reprod Genet 33, 603–609 (2016). https://doi.org/10.1007/s10815-016-0675-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0675-7