Abstract
Purpose
To analyze differences in morphokinetic parameters of chromosomally normal and aneuploid embryos utilizing time-lapse imaging and CGH microarray analysis.
Methods
This retrospective cohort study included patients undergoing IVF treatment and preimplantation genetic diagnosis for sex selection. A total of 460 embryos cultured in incubators with time-lapse imaging system (EmbryoScope) were selected for biopsy on day 3 of development. Subsequently, CGH microarray analysis was performed for aneuploidy screening of 24 chromosomes. Kinetic parameters including time for appearance of second polar body (tPB2), time of pronuclei appearance (tPNa), time of pronuclei fading (tPBf), time to division to 2(t2), 3(t3), 4(t4), 5(t5) cells, length of second and third cell cycle (CC2= t3 t2, CC3=t5-t3), synchrony of cell division from 2 to 4 cells (S2=t4-t3) and interval t5-t2 were analyzed to compare chromosomally normal and abnormal embryos.
Results
The mean time durations for tPNf, t2, t5, CC2, CC3, t5-t2 differed significantly between normal and abnormal embryos.
Conclusions
Time-lapse imaging morphokinetics may play a role in early prediction of aneuploid embryos due to differences in kinetic behavior that may aid in improving clinical outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Efficacy of in vitro fertilization (IVF) treatment has remained low despite advances in the field of reproductive medicine. It is now estimated that about 60 % to 90 % of all transferred embryos in IVF cycles do not implant. Hence, it can be stated that a large proportion of implantation failures are probably attributable to embryonic factors more than anything else, although other factors also play a role (1).
Selecting the best possible embryo for transfer is a major challenge in assisted conception. The primary methods for selection of gametes and embryos for transfer are subjective and static. They are based on punctual, discontinuous observations providing limited information (2,3). Embryos which are deemed most suitable for transfer are the ones that display precise growth observed at fixed times of development e.g. fertilization (observation of pronuclei at16 to 18 h post-insemination), syngamy (at 23 h); early cleavage (at 26 h post-ICSI and 28 h post-IVF); day 2 cleavage (at 44 h); day 3 cleavage (at 68 h); morula (at 92 h) and blastocyst formation (at 116 h). However, these standard checkpoints are not informative of particular cellular events and precise kinetics of embryonic development occurring between any two observations. Recently published studies suggest that the selection of embryo/s or blastocyst/s for transfer with the best potential for implantation should not be based only on number of cells and morphological assessment on the day of transfer (4,5).
There is a need for reliable non-invasive methods for embryonic assessments to aid in the selection of the best embryos from a cohort available. At present, time-lapse imaging has emerged as a promising tool for selecting embryos. The integration of incubation with safe controlled culture environment, together with inspection of dynamic events with the opportunity to observe the fertilization process and early development has provided a new direction in the evaluation of embryos (6).
It is well known that aneuploidy plays a major role in implantation failure and early miscarriage thereby affecting the live birth rates of assisted reproduction. Even the best morphological embryos have been found to be chromosomally abnormal. The inherent imprecision of single embryo transfer has been highlighted in a recent publication where a 44.9 % aneuploidy rate was detected for blastocysts from patients with good prognosis (7). Comparative methodology for aneuploidy screening is rapidly replacing conventional preimplantation genetic screening using the FISH technique. Preimplantation genetic screening, now referred to as comprehensive chromosomal screening for all the 24 chromosomes using the new single nucleotide polymorphic (SNP) or comparative genomic hybridization (CGH) arrays, quantitative PCR (QPCR) or next generation sequencing, is more informative and accurate compared to the prior FISH techniques (8,9).
Pre-implantation genetic screening is being used to improve embryo selection and assisted reproductive outcomes. The approach to using time lapse together with PGS using array comparative genomic hybridization for aneuploidy detection was first presented at ESHRE meeting in 2012 (10). Embryo biopsy remains an essential procedure for PGS which is invasive and the expertise may not be readily available. Additionally, PGS may not be always possible to perform due to legal restrictions, social or simply cost-related issues.
Campbell et al. described the use of time-lapse imaging and morphokinetic analysis to identify embryos at risk for having single or multiple aneuploid chromosome constitution (11,12). They used SNP array and array CGH from trophectoderm biopsies. The aneuploidy rate was quoted as 60 % in this study. The anueploid embryos showed delayed initiation of blastocyst formation and reached full blastocyst stage later compared to euploid embryos .
A recent prospective randomized controlled trial has shown statistically significant improvement in reproductive outcomes with the use of multivatiate morphokinetic model using timelapse imaging (13). Other studies have inked patterns of embryonic divisions to blastocyst formation, ploidy and implantation success .(8,14,15) .
When both time lapse and preimplantation genetic testing are employed together, the total number of embryos to be biopsied and screened for aneuploidy would be expected to be much less and less costly. Therefore, using risk models created by these studies could significantly reduce the financial burden of aneuploidy screening and enable more couples to afford this costly technique.
As both techniques were already available in our center, in the current study, we aimed to utilize and test this new approach in our patient population. Couples who presented to our clinic with the desire of performing PGS for family balancing or gender selection were included in the study. The current study also explores the potential use of time lapse imaging as a non-invasive assessment of embryonic aneuploidy.
Materials and methods
Patients
Between May 2013 and May 2014, a total of 132 couples who presented to Fakih IVF clinics for IVF and PGD for the purpose of gender selection were included in this retrospective cohort study. For this study, institutional ethical committee approval was obtained for all patients. The study was based on previously validated procedures.
The mean age of women was 32.9 years. Primary indication for IVF was solely gender selection (family balancing) in the majority of couples (n = 98 couples). However, there were also patients who had tubal factor, anovulation and male factor as the primary indication who wanted to combine IVF with gender selection. A total of 132 cycles were initiated resulting in 120 egg retrieval procedures. Some cycles were cancelled due to poor response. Cycles were selected at random for investigation for time lapse image acquisition and subsequent retrospective analysis of morphokinetic parameters of embryo development.
Ovarian stimulation
Ovarian stimulation was performed utilizing the short flare-up agonist or GnRH antagonist protocols. In the short agonist protocol, triptoreline 0.1 mg/daily (Gonapeptyl 0.1 mg; Ferring) was initiated on day 2 of the menstrual cycle followed by day 3 initiation of recombinant FSH (Gonal F; Merck Serono) with a dose ranging from 150 to 300 IU depending on patient age and ovarian reserve. Ovarian reserve was investigated clinically utilizing age, antral follicle count, serum FSH or AMH levels. In the GnRH antagonist protocol, daily doses of Cetrorelix 0,25 mg (Cetrotide, Merck Serono) was initiated on day 6 of stimulation or once the dominant follicle reached 14 mm and/or serum estradiol levels raised above 400 pg/ml. Recombinant hCG (rec hCG) was administered (Ovitrelle, Merck Serono) when the 2–3 follicles reached a size ≥18 mm.
Oocyte retrieval
Oocyte retrieval under sedation was performed 36 h after rechCG administration.
Luteal support was started on the day of oocyte retrieval in the form of vaginal progesterone pessaries 1,200 mg/daily (Cyclogest; L.D. COLLINS and CO.) and oral estradiol valerate 6 mg/daily (Progynova; Schering). Serum ß-hCG levels were measured on day 14 following oocyte collection and the luteal support was continued in women with positive testing until 8 weeks or suspended in women who did not conceive.
Laboratory procedures
After retrieval, the oocytes were kept in global total for fertilization media (Life Global, CT, USA) for 2 to 3 h at 37.0 °C and 6.0 % CO2 until denudation. Denudation was performed both mechanically and enzymatically, using Hyaluronidase (SAGE IVF, Cooper Surgical, USA). Intracytoplasmic sperm injection (ICSI) was performed on all MII oocytes within 3 to 4 h after egg collection. The culture medium used was Global Total for culture of embryos from zygote to blastocyst (Life Global, CT, USA). A total of 946 oocytes underwent microinjection and subsequently cultured in the time lapse system (EmbryoScope, Unisense, FertiliTech) using Global Total culture media (Life Global, USA).
On day 1, 710 oocytes were fertilized to 2 pronuclei stage (5.9 ± 3.9 per cycle) (Table 1).
Embryo biopsy
Embryo biopsies were performed in pre-equilibrated Ca+ and Mg+ free biopsy media (Cook, Australia). Biopsy was performed on all day 3 embryos that contained 6 blastomeres or more and less than 25 % fragmentation. Individual cleavage-stage embryos were placed in 10–15 μl biopsy media (Cook media, Australia) on a heated (37 °C) micromanipulation stage (Narishige-Olympus 1 × 70). With the use of a holding pipette (Cook, Australia), the embryo was rotated so that a blastomere with a clear and distinct nucleus was at 3-o’clock position, a hole of 20–25 μm was created in the zona pellucida adjacent to the blastomere to be removed using the ZILOS Infrared Laser Optical System (Hamilton Thorne Research, Beverly, MA). Two to three 0.5 millisecond pulses at 100 % power were made depending on the thickness of the zona pellucida. The desired blastomere was gently aspirated with a biopsy pipette (Cook, Australia) while avoiding contact or disruption of the remaining blastomeres.
Microarray protocol
Multiple Displacement Amplification (MDA) protocol
One blastomere per embryo was collected in 0.5 ml PCR tubes containing 5 μl of 1× of Phosphate Buffer Saline (PBS). Blank samples were also run in parallel with the tested samples in order to detect any contamination (if present). Three microliters of alkaline buffer (ALB; 200 mM NaOH, 50 mM dithiothreitol) as described previously (16) were added on the samples and blanks. After 15 min of incubation at 4°, 3 μl of neutralization buffer (900 mmol/l Tris–HCl, 300 mmol/l KCl, 200 mmol/l HCl) were added to the solution. Cell lysates were used directly for whole genome amplification (WGA) using MDA (GE Healthcare, USA) by adding 18 μl of the master mix in total volume of 30 μl. The mix was then incubated at 31 °C for 2 h and heat inactivation was followed at 65 °C for 10 min. MDA yield were quantified on a fluorometer using picogreen quantification kit (Molecular Probes, Inc., Eugene, USA). Blanks did not show any amplification.
Optimization of single cell aCGH
Agilent human genome CGH 8x60k kit (Agilent Technologies, Inc., Santa Clara, CA, USA) was used to detect chromosomal aneuploidies in the blastomeres. The blastomeres were amplified by MDA as previously described (see MDA amplification protocol). In parallel, 0.5 ng of control DNA was amplified, using the same MDA technique, and used as control in the aCGH procedure. Equal quantities DNA from amplified blastomeres and controls were purified using QIAprep Spin Miniprep columns (Qiagen, USA) and collected in 50 μl of water. Amplification samples (blastomeres and control DNA) were systematically labeled with Alexa Fluors 555 and 647 respectively. Labeled products of each sample and control DNA were purified using QIAprep Spin Miniprep columns (Qiagen, USA), mixed together and checked on 2,100 bioanalyzer (Agilent, USA) in order to evaluate the Alexa Fluors 555 integration into the DNA samples. To 16ul of the purified Alexa Fluors 555 and 647 labeled samples, the following hybridization blocking reagents were added: 5ul (1 μg/ul Cot-1 DNA (Invitrogen), and 5 μl 10× control targets (Agilent). The volume was brought to 50 μl with 2× hybridization buffer (Agilent) was added. The hybridization mixture was then denatured at 100 °C for 3 min in a water bath. Samples were immediately transferred to a 37 °C water bath for 30 min to allow pre-annealing of the blocking agents to the labeled sample. Samples were centrifuged for 5 min at 16,000 xg and immediately applied to agilent’s human genome CGH 8x60k Oligo Microarray Kit as per the manufacturer’s recommendations. Hybridizations were performed at 65 °C for 3 h. The microarrays were disassembled in the agilent wash buffer-1 at RT, transferred to a slide holder and incubated for 5 min with steering in the agilent wash buffer-1 at RT. The second washing step was performed for 1 min in wash buffer-2 at 37 °C. The third and fourth washing steps were done with acetonitrile (Fisher, USA) and stabilization solutions (Agilent, USA) for 1 min and 30 s at RT respectively. The microarray slides were immediately scanned in the agilent DNA microarray scanner and analysed using Agilent Cytogenomic V2.9.0.12.
Time lapse imaging
The exact timings of each embryo division and developmental parameters were calculated in hours post-ICSI. The images were analyzed every 15 min using Embryo Viewer Software workstation in 5 different focal planes over 72 h of culture. Developmental markers used in this study were defined as follows: division into 2 cells (t2), division into 3 cells (t3), division into 4 cells (t4) and division into 5 cells (t5). Division between 2 consecutive cleavages is defined as duration of second cell cycle (CC2) or the time from division from 2 cells to 3 cells. Second synchrony (S2) is defined as the time taken from division of a 3-blastomere embryo to a 4-blastomere embryo (t4-t3). The duration of the third cell cycle was defined as CC3 (t5-t3) and interval between 2 and 5 cells as the variable t5-t2 which combines the concepts of cell synchrony and cell cycle. The time taken for pronuclei fading and appearance of the second polar body was also noted.
Embryo transfer
Blastocysts were transferred under transabdominal ultrasound guidance following gender determination. The transfer was planned on day 5 of the development (120 h). The mean number of embryos transferred were 2.3 ± 0.5.
Statistical analysis
Descriptive statistics such as mean, median, standard deviation (SD) were calculated for the study variables. Comparison of mean values was done using Student’s t-independent test. Frequency variables across categories were compared using Chi-square/Fisher’s Exact test as appropriate. Binary logistic regression analysis was carried out to determine significant factors that enhanced the chances of obtaining normal embryos. ROC analysis was performed to calculate optimum duration of higher number of normal embryos. A p-value < 0.05 was considered as statistically significant. All the analyses were carried using SPSS statistical package IBM version 19.0.
Results
The mean age of the patients was 32.9 years. A total of 132 ICSI cycles were initiated, finally resulting in 120 egg retrieval procedures.
A total of 1,360 oocytes were collected from 120 oocyte retrieval procedures. The mean number of oocytes, metaphase II oocytes collected per cycle were 11.3 ± 3.3 and 7.8 ± 3.4 respectively.
A total of 946 oocytes underwent microinjection resulting in 710 (75.05 %) fertilizations (2PN oocytes). On day 3 of embryo development, a total of 496 (69.8 %) embryos were selected for biopsy (Table 1).
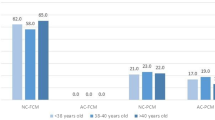
Thirty six embryos (7.25 %) showed no amplification on CGH microarray; therefore final analysis was carried out on 460 embryos (Table 2). Following CGH study, 197 (42.8 %) embryos were determined as euploid, while 263 embryos (57.17 %) were aneuploid (Table 2). The type of abnormalities were detected are summarized in Table 3.
The mean duration of pronuclei fading (tPNf) and division to two cells (t2) for normal embryos were significantly less than that of the abnormal embryos (P < 0.05).
The mean duration of t5, duration of second cell cycle (CC2), duration of the third cell cycle (CC3), and the difference between t5 and t2 (t5-t2) for normal embryos were significantly higher than that of the abnormal embryos (P < 0.05) (Tables 4).
Significantly (p < 0.001) higher correlation coefficients (>0.7) between t2, t3, t4 and t5 for both normal and abnormal embryos indicate strong multicollinearity exists between these variables (Table 5). Furthermore, a significant positive correlation (>0.8) between CC3 and t5-t2 difference was observed for both normal and abnormal embryos again supporting the presence of multicollinearity between CC3 and t5-t2.
Logistic regression analysis
Considering the multicollinearity issues, initially logistic regression analysis (backward elimination by likelihood ratio method) was carried out by taking embryo quality as the dependent variable (1 = normal embryos, 0 = abnormal embryos) and development durations t5, CC2, CC3, S2 as independent variables. Final model with CC3 was found to be an adequate fit (Hosmer and Lemeshow goodness of fit, Chi-square = 4.92; P = 0.670).
The significant variable CC3 yielded an odds ratio (OR) of 1.07 (95 % CI: 1.03–1.10). Since CC3 was found to be a significant favorable factor for normal embryos, receiver operating curve (ROC) analysis was carried out to find an optimum cut-off value, which is likely to yield higher number of normal embryos. The area under curve (AUC) was 0.631 (P < 0.001) (95 % confidence limits 0.578 to 0.684. The optimum cut of value was found to be 10.00 h. Also, a statistically significant difference was observed in the euploidy status of the embryo when 10.00 h of CC3 was taken as a marker. Embryos grown in more than 10 h of CC3 were more likely to be euploid (chi-square = 20.6; P < 0.001) (52 %: 95 % CI: 46.2–57.6) when compared to embryos with a CC3 less than 10 h of time duration (28.4 %; 95 % CI: 21.4–36.5).
CC3 and t5t2 diff parameters were found to be multicollinearity variables. Revised logistic regression analysis was carried out by inclusion of t5t2diff variable and dropping CC3 variable. Other variables included in the earlier logistic regression analysis were retained. The model with t5t2diff was found to be adequate fit (Hosmer and Lemeshow goodness of fit Chi-square = 14.4; P = 0.073). The significant variable t5t2diff yielded an odds ratio of 1.06 (95 % CI:1.03–1.09). Since t5t2diff was found to be a significant favorable factor for normal embryos, ROC analysis was carried out to find an optimum cut-off value, which is likely to yield higher number of normal embryos. The area under curve (AUC) was 0.632 (P < 0.001) with 95 % confidence limits 0.579 to 0.685. The optimum cut-off value was found to be 20.00 h.
Accordingly, it was shown that significantly more embryos were euploid (52.3 %: 95 % CI: 46.5–58.2) in the group of embryos grown at more than 20.00 h of t5t2diff (Chi-square = 19.5; p < 0.001) as compared to only 29.9 % of the embryos grown at less than 20.00 h of t5t2diff (95 % CI: 23.1–37.8).
Both CC3 and t5t2diff variables were found to be favorable factors for euploid embryos. Duration of CC3 more than 10 h was found to be the optimum time for detecting significantly higher number of normal embryos. Similarly CC3 duration of more than 20 h for t5t2diff was found to be ideal time interval for detecting significantly higher number of normal embryos. Due to multicollinearity issues, analysis of our data has shown that not all variables should be included in the logistic regression.
Discussion
This study compares the morphokinetic behavior of chromosomally normal and abnormal embryos combining two different modalities: preimplantation genetic screening and time lapse imaging.
Preimplantation genetic screening identifies euploid embryos to be transferred. However, there is still considerable debate on the issue of embryo biopsy which may cause harm to the embryo following the removal of a single blastomere. Hence, it is prudent to search for non-invasive alternatives for identification of normal embryos to improve the success in assisted reproduction.
Time-lapse imaging provides continuous visual observation of embryo morphology and kinetics which may help in distinguishing euploid from abnormal embryos. Studies have been attempted to create risk models utilizing morphokinetics to select chromosomally normal embryos (12,22). Based on the dynamic events, embryos can be classified as high risk or low risk with respect to chromosomal abnormalities. Hence, recognition of embryos at risk may aid in the selection of embryos for transfer that are more likely to be chromosomally normal. On the other hand, this approach may also help to reduce the number of embryos to be biopsied, thereby reducing the total cost of the procedure.
In the current study, cleavage stage embryos were analyzed morphokinetically and day-3 biopsy was performed for comprehensive chromosomal screening by CGH microarray. Some studies which have evaluated morphokinetic events and timings in correlation to embryonic aneuploidy have either used day-3 or trophectoderm biopsy and subsequently used FISH, CGH microarray or sequential nucleotide peptide (SNP) as a method of genetic analysis.
The different morphokinetic parameters are discussed below:
Pronuclei fading
In our study, the time of pronuclei fading showed significant difference between normal and abnormal embryos with array CGH analysis. Similarly, Azzarello et al. (17) found that pronuclei breakdown occurred later in embryos resulting in live birth compared to those that resulted in lower live birth rate. Lemmen et al. (18) showed early pronuclei breakdown as a good marker of embryo potential. However, Stevens et al. reported that time of pronuclei appearance, resolution, or size had no correlation to embryo aneuploidy utilizing trophectoderm biopsy and 24 chromosomes analysis with QPCR (19). Another recent publications, also found no correlation between time of pronuclei fading and aneuploidy utilizing trophectoderm biopsy and 24-chromosome microarray (11,12).
Cytokinesis
In the current study, we have analyzed substantially higher number of embryos compared to previous studies. Our results have shown that mean durations of t2, t5, CC2, CC3, and t5-t2 differences are significantly different between normal and abnormal embryos suggesting that early cleavage divisions are delayed in aneuploid embryos compared to euploid embryos. The study by Davies et al. (10) and Basile et al. support our findings. Davies reported a delayed first and second cleavage and prolonged transition between 2 and 4 cells in embryos with complex aneuploidies. Basile et al. (20) studied a total of 504 embryos and found a difference in kinetic behavior. Logistic regression analysis of their data revealed t5-t2, followed by CC3 as the most relevant variables related to normal chromosomal content. On the basis of these results, the authors proposed an algorithm for embryo selection.
In contrast, Campbell et al. (11), found that aneuploid and euploid embryos developed similarly up to the 8-cell stage (day 3) but had significant delay in development in the periblastulation stage. They compared development parameters from 38 euploid embryos with 60 aneuploid embryos (total of 98 blastocysts) and created an aneuploidy risk model based on these observations. Multiple aneuploid embryos were found to be delayed at the initiation of compaction and time to reach the full blastocyst stage. In a study including 76 blastocysts observed with the EmbryoScope, Semeniuk et al. (21) showed that the timings of the first mitotic division, division from 2 to 3 cells, appearance of 4th blastomere and third mitotic division were not different between aneuploid and euploid embryos. In another study by Bayram et al. (22) utilizing day-3 biopsy and FISH, 122 embryos were analyzed and no difference was found in cleavage time to the 8-cell stage, duration or cleavage from 2- to 3-cell or 3- to 4-cell. However, they showed that euploid embryos had a shorter time to cleavage from 5- to 8-cell. In the study by Friedman et al. (23), 62.5 % of all embryos exhibited normal timings for first cytokinesis, time of second mitosis, and synchrony of the third and fourth cell appearance. Using CGH microarray for chromosomal analysis, they showed that only 40 % of the embryos with abnormal timings were euploid.
Conclusion
Substantial percentage of in vitro generated embryos tends to be chromosomally abnormal. Morphological parameters of embryos do not correlate well with chromosomal content. Time-lapse imaging is a non-invasive technique and has become an integral part of the many IVF laboratories. Various studies have suggested dynamic morphokinetic analysis and risk models to identify normal embryos. Preliminary data suggest that this technique may assist in the selection of chromosomally competent embryos. This approach may enhance success of assisted reproduction and promote single embryo transfer. Larger age adjusted data set or randomized controlled trials are necessary to draw clear conclusions.
Funding
No funding was received from any source for this study.
References
Patrizio P, Bianchi V, Lalioti MD, Gerasimova T, Sakkas D. High rate of biological loss in assisted reproduction: it is in the seed, not in the soil. Reprod Biomed Online. 2007;14(1):92–5.
Bromer JG, Seli E. Assessment of embryo viability in assisted reproductive technology: shortcomings of current approaches and the emerging role of metabolomics. Curr Opin Obstet Gynecol. 2008;20(3):234–41.
Payne D, Flaherty SP, Barry MF, Matthews CD. Preliminary observations on polar body extrusion and pronuclear formation in human oocytes using time-lapse video cinematography. Hum Reprod. 1997;12(3):532–41.
Chamayou S, Patrizio P, Storaci G, Tomaselli V, Alecci C, Ragolia C, et al. The use of morphokinetic parameters to select all embryos with full capacity to implant. J Assist Reprod Genet. 2013;30(5):703–10. Apr 13.
Van Montfoort AP, Dumoulin JC, Kester AD, Evers JL. Early cleavage is a valuable addition to existing embryo selection parameters: a study using single embryo transfers. Hum Reprod. 2004;19(9):2103–8.
Cruz M, Garrido N, Herrero J, Pérez-Cano I, Muñoz M, Meseguer M. Timing of cell division in human cleavage-stage embryos is linked with blastocyst formation and quality. Reprod Biomed Online. 2012;25(4):371–81.
Yang Z, Liu J, Collins GS, Salem SA, Liu X. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: results from a randomized pilot study. Mol Cytogenet. 2012;5(1):24.
Meseguer M, Herrero J, Tejera A, et al. The use of morphokinetics as a predictor of embryo implantation. Hum Reprod. 2011;26(10):2658.
Fragouli E, Wells D. Aneuploidy in the human blastocyst. Cytogen Genome Res. 2011;133(2–4):149–59.
Davies S, Christopikou D, Tsorva E, Kragianni A. Delayed cleavage division and prolonged transition between 2 and 4 cell stages in embryos identified as aneuploidy at 8 cell stage in array CGH. Hum Reprod. 2012;27:ii84–6.
Campbell A, Fishel S, Bowman N, Duffy S, Sedler M. Retrospective analysis of outcomes after IVF using an aneuploidy risk model derived from time-lapse imaging without PGS. Reprod Biomed Online. 2013;27(2):140–6.
Campbell A, Fishel S, Bowman N, Duffy S, Sedler M. Modelling a risk classification of aneuploidy in human embryos using non-invasive morphokinetics. Reprod Biomed Online. 2013;26(5):477–85.
Rubio I, Galan A, Larreategui Z, Ayerdi F . Controlled validation of embryo culture and selection by morphokinetic analysis : a randomized controlled trial of the embryoscope . Fertl Steril 2014, Sept 10 . (pubmed)
Hashimoto S, Kato N, Saeki K. Selection of high potential embryos for culture in polydimethyl siloxane microwells and time lapse imaging. Fertil Steril. 2012;97(2):332–7.
Wong CC, Loewke KE, Bossert NL, Behr B, De Jonge CJ. Non-invasive imaging of human embryos before embryonic genome activation predicts development to the blastocyst stage. Nat Biotechnol. 2010;28(10):1115–21.
Le Caignec C, Spits C, Sermon K, De Rycke M, Thienpont B, Debrock S, et al. Single-cell chromosomal imbalances detection by array CGH. Nucleic Acids Res. 2006;34(9):e68.
Azzarello A, Hoest T, Mikkelsen A. The impact of time-lapse assessment on nuclearity: is multinucleation a proper character for embryo selection. Hum Reprod. 2012;27(2):ii103–5.
Lemmen JG, Agerholm I, Ziebe S. Kinetic markers of human embryo quality using time-lapse recordings of IVF/ICS fertilized oocytes. Reprod Biomed Online. 2008;17(3):385–91.
J. Stevens, M. Rawlins, A. Janesch, N. Treff, W.B. Schoolcraft . Time lapse observation of embryo development identifies later stage morphology based parameters associated with blastocyst quality but not chromosome constitution. Volume 98, Issue 3, Supplement, Page S30, September 2012
Semeniuk L, Mazur P, Mikitenko D, et al. Time lapse and aCGH, is there any connection between ploidy and embryo cleavage timing on early stages of embryo development. Fertil Steril. 2013;99(35):s6.
Basile N, Nogales Mdel C, Bronet F, Florensa M, Riqueiros M, Rodrigo L, et al. Increasing the probability of selecting chromosomally normal embryos by time-lapse morphokinetics analysis. Fertil Steril. 2014;101(3):699–704.
Bayram A, Ciray H, Sahin O, et al. Comparison of morphokinetic parameters between euploid and aneuploid embryos by time-lapse monitoring. Hum Reprod. 2012;27(2):ii103–5.
Friedman B, Chavez S, Behr B, et al. Non invasive imaging for the detection of human embryonic aneuploidy at the balstocyst stage. Fertil Steril. 2012;98(35 (suppl 3)):s38.
Author information
Authors and Affiliations
Corresponding author
Additional information
CapsuleDifferences in kinetic behavior were detected between normal and abnormal embryos during early embryonic development.
Rights and permissions
About this article
Cite this article
Chawla, M., Fakih, M., Shunnar, A. et al. Morphokinetic analysis of cleavage stage embryos and its relationship to aneuploidy in a retrospective time-lapse imaging study. J Assist Reprod Genet 32, 69–75 (2015). https://doi.org/10.1007/s10815-014-0372-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-014-0372-3