Abstract
Purpose
Adolescents and adults with Down syndrome are noted to display symptoms and behaviors consistent with a diagnosis of Obsessive Compulsive Disorder. While evidenced-based interventions, including psychopharmacology and therapeutic interventions including exposure and response prevention, exist and effectively treat obsessive-compulsive symptoms in neurotypical populations, less is known about effective treatments for similar presentations in persons with Down syndrome.
Methods
A scoping rapid review was conducted in April 2023 to determine what treatments are being used to target obsessive-compulsive symptoms and related behaviors in adolescents and adults with Down syndrome, the quality of those treatments, and their alignment with current evidenced-based interventions.
Results
A total of eleven articles, all single case or case series, published between 1992 and 2017 were identified describing the treatment of 32 adolescents and adults with Down syndrome and obsessive-compulsive traits and behaviors including: hoarding, cleaning, gross motor compulsions, and food, hygiene, dressing, and checking rituals. Interventions used most often aligned with evidenced-based guidelines for treating obsessive compulsive disorder and included psychopharmacology, psychotherapy, and complementary and alternative medicine.
Conclusions
While the outcomes of most interventions yielded partial or significant reduction in symptoms, poor research quality and limited generalizability noted across all studies make it difficult to inform guidelines for caring for this high-needs population. In the future, we believe it is necessary to perform more rigorous research focused on treating obsessive compulsive symptoms in individuals with Down syndrome with sufficient follow-up to fully assess treatment effectiveness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Down syndrome (DS) is the most common genetic cause of intellectual disability (Gratias et al., 2022), affecting approximately 1 in every 700 births in the United States alone (Centers for Disease Control and Prevention, 2023). Individuals with DS are at an elevated risk of developing a variety of medical conditions such as vision and hearing problems, obstructive sleep apnea, and autoimmune conditions, as well as developmental complications such as autism spectrum disorder and behavioral problems for which screening for is recommended by the American Academy of Pediatrics (Bull et al., 2022; Weijerman & de Winter, 2010). While routine screening for medical conditions is easily obtained with physical examinations and laboratory testing, it is more difficult and time intensive to screen for mental health conditions and psychosocial factors affecting a person’s wellbeing (Ballester et al., 2005).
Given the unique DS genetic profile, psychiatric symptoms often present in a non-classical form, creating challenges with regards to diagnostic clarity (Patti & Tsiouris, 2006). Therefore, it is not surprising that there are disparities in diagnosis and subsequent treatment of mental health conditions in the DS population (Rivelli et al., 2022). Unfortunately, approximately 28.9% of individuals with DS have a co-morbid psychiatric condition (Prasher, 1995). Of these, the most common mental health concerns are mood and anxiety disorders, including major depressive disorder, generalized anxiety disorder, and obsessive-compulsive disorder (Chicoine et al., 2021).
Obsessive-compulsive disorder (OCD), as described in the DSM 5, is characterized by the presence of obsessions and compulsions. Obsessions are unwanted mental images, thoughts, urges, or impulses which are considered undesirable or disturbing to the individual experiencing them. In turn, compulsions are repetitive behaviors or actions, which are often performed in order to decrease anxiety caused by obsessions (American Psychiatric Association, 2013). The prevalence of OCD and obsessive-compulsive behaviors and traits ranges from 0.8 to 4.5% in the DS population (Myers & Pueschel, 1991; Prasher & Day, 1995). For neurodivergent and neurotypical individuals, the presence of OCD-related behaviors can be very distressing and have a significant impact in an individual’s quality of life, making it difficult to perform daily activities such as eating and drinking, and often negatively impacting social relationships (Huppert et al., 2009).
Despite the prevalence and distress caused by this condition, it remains difficult for clinicians to effectively diagnose and treat OCD in individuals with DS. Some argue that the diagnostic difficulty is because clinicians may incorrectly attribute OCD behaviors to co-occurring intellectual disability which is a phenotypic DS trait (Tassé et al., 2016). Further, due to cognitive impairments, persons with DS may have poor insight or difficulty clearly communicating their emotional state, making it hard to diagnose OCD which relies on both insight and emotional awareness. Finally, the individual’s level of adaptive abilities can mask OCD symptoms resulting in hindering a clear evaluation of OCD symptoms. While standardized screening forms exist and have been approved for neurotypical individuals, there are few reliable measures available for individuals with DS. As a result, clinicians must often rely on subjective report provided by collateral caregivers in order to diagnose and assess treatment response.
Once a diagnosis of OCD is provided, a clinician should provide evidence-based treatments to help the patient cope with the symptoms and behaviors which are negatively impacting their ability to function and perform activities of daily life. In neurotypical patients, OCD and related symptoms are treated using evidence-based interventions which usually entails a combination of pharmacologic treatment and therapeutic interventions including exposure and response therapy (Fineberg et al., 2012). Current guidelines from the American Psychiatric Association recommend use of selective serotonin reuptake inhibitors (SSRIs) with trial of alternative SSRI or augmentation with antipsychotics endorsed for treatment resistant OCD symptoms. Concurrent treatment with Cognitive Behavioral Therapy or Exposure Response Prevention therapy (ERP) is also recommended for those who can participate (Koran et al., 2007). The use and safety of these therapeutics for the DS population is unknown. Given that individuals with DS are more prone to adverse reactions and side effects from medications, it cannot be assumed that interventions approved for neurotypical patients are both safe and efficacious (Hefti & Blanco, 2017). Therefore, it is imperative that clinicians have access to evidence-based treatment recommendations to adequately address OCD and related behaviors.
There must be understanding as to what treatments are currently being used to address OCD in individuals with DS and their utility. Via a rapid scoping review of current existing literature, this project aims to identify therapeutics used to target obsessive-compulsive traits and behaviors in teens and adults with DS and examine their efficacy. Specifically, we aim to (1) identify strategies used to target and treat symptoms of OCD or related behaviors, (2) determine the alignment of these strategies with current guidelines for evidenced-based OCD treatment; (3) assess the quality of the available research, and (4) identify the presence and type of any knowledge gaps.
Methods
In April 2023, a scoping rapid review was conducted to identify OCD treatments targeted for DS teens and adults. The following inclusion criteria were used: (1) participants must be aged 13 years or older, (2) participants must have a diagnosis of Down Syndrome (if the study included a case series or group study at least 1 participant must have DS), (3) participants must have co-occurring obsessive-compulsive symptoms (e.g., repetitive behaviors, hoarding), (4) OCD symptoms were unrelated to another co-occurring medical or neurological condition, (5) treatment must target OCD symptoms (not anxiety or depressive behaviors), and (6) study must be written in English. Non-published theses or dissertations could be included. Studies were excluded if they did not meet the inclusion criteria. Additionally, literature reviews, editorials, posters, book chapters, and opinion pieces without a clear case study were excluded.
Literature Search and Article Selection
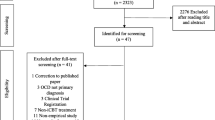
Using Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) standards (Page et al., 2021), we searched the following databases including PubMed, CINAHL, EMBASEE, PsychINFO, and Scopus (Medline). The search terms included combined terms related to OCD (e.g., “obsessive compulsive disorder,” “obsessi”, “compulsi”, “ocd”, “repetiti”), down syndrome (e.g., “down syndrome”, “trisomy 21”), and treatment (e.g., “therapy”, “treatment”, “intervention”, “pharmacotherapy”, “drug”). When searching PubMed, MESH terms were used for “down syndrome” and “obsessive compulsive disorder.” Search limits were applied for age (i.e., 13 years or older), subjects (i.e., human subjects only), and language (i.e., English only). After conducting the initial search in each database, titles and abstracts were screened to determine if the study met inclusion criteria. The remaining full-text articles were then read and any study that did not meet the inclusion criteria was eliminated. All titles, abstracts, and full-text articles were read and evaluated by two independent raters (IRR = 97.3%).
Data Extraction and Coding
Once it was determined which full-text articles met inclusion criteria, two raters extracted data on an a-priori defined spreadsheet in which background information and data to support key aims were coded. For background information, the following was coded: first two authors, publication year, number of participants in the study with DS, age of participants, psychiatric diagnoses, medical comorbidities, source of subjects (e.g., hospital), methods (e.g., observational, response to treatment), and study design (e.g., case study, experimental study). For data to support key aims, the following was coded: type of intervention, length of intervention, medication dose/optimization, adverse reactions to medications, primary outcome measure, informant who completed outcome measure, symptom change, maintained gains at follow-up, and limitations of each article. A quality assessment was also completed using an adapted Cochrane Risk of Bias tool for intervention studies (see single-case design risk of bias (SCD RoB) tool developed by Reichow et al., 2018 for further information). The SCD RoB tool serves as a guide to assess each study for sources of potential bias across eight subdomains within the broader categories of selection bias, performance bias, and detection bias. Using the SCD RoB tool, each study was rated for its risk of bias (i.e., low, unclear, or high) across each of the eight subdomains (i.e., sequence generation, participant selection, blinding of participants/personnel, procedural fidelity, blinding of outcomes assessment, selective outcome reporting, dependent variable reliability, and data sampling) by the two independent raters (IRR = 100.0%).
Results
Figure 1 summarizes studies that were retained at each step of the rapid review. Additionally, a summary of relevant study information can be found in Table 1. In total, 11 studies met inclusion criteria and studies ranged in publication year from 1992 to 2017. Across the eleven studies included, there were four case reports and seven case series.
Most of the studies utilized a psychopharmacologic only intervention to treat OCD symptoms in the DS population (n = 5). Across the other six studies included in this review, one tested a psychotherapeutic intervention (Berry et al., 2006), three utilized a combined pharmaceutical and psychotherapeutic intervention (Charlot et al., 2002; Pekrul & Fitzgerald 2015; Raitasuo et al., 1998), and two studies tested the use of complementary and alternative medicine approaches (Fujino et al., 2017; Sheehan et al., 2010).
In our data set, across the eight studies that reported psychopharmacologic interventions to target symptom reduction (some in conjunction with therapy), a variety of medications were used, the majority of which were in line with evidence-based guidelines. A total of 28 patients received pharmacotherapy treatments - SSRIs (i.e., fluoxetine, sertraline, paroxetine, fluvoxamine, and citalopram) at varying doses were used for 21 of these patients (Akahoshi et al., 2012; Charlot et al., 2002; Geldmacher et al., 1997; O’Dwyer et al., 1992; Pekrul & Fitzgerald 2015; Raitasuo et al., 1998; Sutor et al., 2006). SSRI monotherapy was primarily employed; however, four patients were dosed in conjunction with antipsychotics (risperidone, quetiapine, and chlorpromazine: Sutor et al., 2006; Charlot et al., 2002), one patient with memantine (Pekrul & Fitzgerald 2015), one patient with clomipramine (Charlot et al., 2002), and one patient with lorazepam and risperidone (Sutor et al., 2006).
In five patients, clomipramine was used for treatment (Akahoshi et al., 2012; Charlot et al., 2002; O’Dwyer et al., 1992; Pekrul & Fitzgerald 2015). Out of those five patients treated with clomipramine, three received clomipramine only, one received clomipramine in conjunction with an SSRI, and one received clomipramine in conjunction with nitrazepam.
There were five patients who received pharmacotherapy that was prescribed outside of typical treatment guidelines. One patient was sedated once (for MRI) with phenobarbital 30 mg, chlorpromazine 25 mg, and promethazine 12.5 mg and following sedation had a spontaneous remission of repetitive behaviors (Akahoshi et al., 2012). Another patient was treated with risperidone 2 mg daily, levopromazine 10 mg daily, and amantadine 100 mg for two days and saw partial improvement in repetitive hand washing behaviors (Akahoshi et al., 2012). Another patient was treated with carbamazepine monotherapy for primarily depressive symptoms that included obsessive traits and had observed partial improvement (Akahoshi et al., 2012). A fourth patient from the same paper had Obsessive Compulsive Traits with simultaneous psychosis and was treated with Haloperidol, levomepromazine, and promethazine with partial improvement in symptoms. Additionally, there was a published case report of a patient with compulsive behaviors fixated on walking laps around the house that improved with treatment of temazepam 20 mg and dosulepin 50 mg at bedtime (Prasher et al., 1995).
Four articles included intentional behavioral strategies or psychotherapy, three of which occurred simultaneously with pharmacotherapy techniques. One patient’s described psychological treatment consisted of “supportive measures, psychoeducation, and the role of the personal nurse as the patient’s ‘auxiliary ego’” (Raitasuo et al., 1998). Four patients were treated with reinforcement incentives for desired behaviors which led to a significant improvement. For three of the four patients, papers did not specify how reinforcement was done. Another patient with hoarding tendencies was addressed by reinforcing the absence of hoarding behavior by providing appropriate desired objects (e.g., towels) if hoarding inappropriate items (e.g., stolen items from staff or peers) were not found in room checks (Berry et al., 2006; Charlot et al., 2002; Pekrul & Fitzgerald 2015). Additionally, two of these patients also had pacing strategies implemented due to their OCD rituals being centered around slowness and repetitive behaviors that lasted for hours (e.g., morning and evening bathroom routines; Charlot et al., 2002). Charlot and colleagues (2002) found that the singular intervention of educating caregivers that the obsessional behaviors were not volitional also yielded symptom improvement on external reports.
Across the studies, the most common reported psychopharmacologic side effects (outside of those typically observed in each medication class) included sedation/sleep disturbances and worsening of OCD symptoms. For example, one patient, placed on fluoxetine for repetitive household chores and subsequent crying spells, was noted to have the adverse effect of confusion, myoclonus, and insomnia after the dose was increased to 40 mg daily (Geldmacher et al., 1997). Two additional patients had reported sedation; one patient had been receiving citalopram (who subsequently experienced resolution of symptoms after transitioning to sertraline) while the other patient had been on a polypharmacy regimen including sertraline, risperidone, and lorazepam (Sutor et al., 2006). Per Pekrul & Fitzgerald (2015), one patient was treated with sertraline initially and developed adverse effect of agitation, anxiety, and an increase in compulsive behaviors. He was later transitioned to risperidone and developed weight gain and drooling with no improvement in symptoms. Finally, he was successfully transitioned to fluoxetine with improvement in symptoms.
Quality of the Available Research and Knowledge Gaps
Our analysis of articles showed high risk of bias in all articles (see Fig. 2). All were case study or case series and therefore showed high rates of detection bias, specifically 10 out of 11 articles showed selective outcome reporting, 10 out of 11 articles showed data sampling bias, 10 out of 11 articles showed issues with dependent variable reliability, and finally 11 out of 11 articles failed to blind outcome assessments, participants, or personnel. Eight out of 11 showed high rates of bias in procedural fidelity and 2 out of 11 showed unclear risk of bias. Nine out of 11 articles showed unclear risk of bias regarding participant selection as they did not discuss their process of finding participants. Two out of 11 did have low risk of bias as they reported on all participants in a pre-selected cohort. There was an unclear or high risk of bias in all 11 articles because of lack of fidelity in sequence generation. Finally, only 4 out of 11 studies reported follow-up data. Thus, it is still largely unknown whether the effects of these treatments persist over time.
Discussion & Conclusion
Our scoping review of the literature examining the treatment of OCD identified 290 unique articles, 11 of which met our inclusion criteria. These 11 papers examined a total of 32 patients and the treatment of obsessive-compulsive traits and behaviors including: hoarding, cleaning, gross motor compulsions, and food, hygiene, dressing, and checking rituals.
A total of 28 patients were treated with pharmacologic interventions, four with exclusively behavioral interventions, and three with both pharmacologic and behavioral interventions. Many of the behavioral and pharmacologic treatments implemented in these studies followed standard recommendations for neurotypical patients with OCD including the use of SSRIs, with augmentation from antipsychotics or use of clomipramine. A majority of patients (21 out of 28) that received pharmacologic treatment were given SSRIs at some point in the treatment. All but one case (O’Dwyer et al., 1992) had improvement in symptoms via either self, caregiver, or clinician observation. There were some noted deviations from standard pharmacologic treatment, some papers trialed completely novel agents like mianserin, levomepromazine, and promethazine.
While clomipramine is no longer the first-line recommended agent, the articles reviewed were published over a 25-year period (1992–2017), during which time the mainstay of psychopharmacologic treatment shifted from clomipramine (TCA) to SSRIs due to equivalent effect size and lower side effects profile (Koran et al., 2007). Clomipramine remains a Food and Drug Administration approved medication for treatment of OCD as well as a recommended medication for initial or treatment resistant pharmacotherapy. Additionally, clomipramine is approved to be used for augmentation of SSRIs as it was in one patient (Charlot et al., 2002; Koran et al., 2007).
There was also significant variation in the use of behavioral and therapeutic interventions which included reinforcement strategies for preferred behaviors, psychoeducation, and supportive measures. Importantly, there were no patients in the cases reviewed that were provided ERP, despite ERP being recommended as the first-line therapeutic intervention for neurotypical individuals. Further, emerging evidence supports the effectiveness of ERP in treating anxiety in individuals with intellectual disabilities with the appropriate modification in place (e.g., video modeling of exposures, rewards for engaging in exposures, visual supports aiding in exposure completion, caregiver supports in engaging in exposures; Blakeley-Smith et al., 2021). Thus, the exclusion of ERP is even more notable and should be rigorously tested as a potential treatment for OCD in patients with DS going forward.
While the interventions used in the studies examined reported primarily positive responses, interpretation of the efficacy of treatments is limited by poor research quality and external validity. One notable limitation in the studies examined was the lack of objective monitoring of symptoms and measurements of any perceived changes. Nine of the eleven studies relied on subjective reports from patients, family, or caregivers to determine treatment efficacy. While subjective reports can be useful in understanding an individual’s perspective of treatment response and tolerability, individual biases may have a significant impact on perceived results. Self-reports also require participants to track notable responses and events between follow-ups making self-reported data less reliable. Additionally, the lack of any objective measures significantly limits the ability to generalize any interpreted results.
Additionally, there were many methodological flaws with the measures being used including measures not being validated, symptoms only being reported retroactively, and qualitative observations being the only measure of change. Going forward, it will be important to include multiple well-validated methods of assessment to accurately assess symptom change over time.
Further, all 11 studies included in our analysis were classified as case reports or case series. While these reports are important in describing unique conditions, they lack the rigorous study design of randomized controlled trials, resulting in significant limitations in interpretation and generalization of results. Going forward, it is imperative that randomized controlled trials be conducted to test the efficacy of therapeutic interventions in treating OCD in patients with DS.
Another important limitation in most studies is the lack of consistent follow-up, as seven of the eleven studies neglected to report follow-up assessments. Therefore, while many studies endorsed positive responses to the interventions performed, it is unclear whether these responses were sustained for any significant length of time.
It should also be noted that of 290 articles identified, only 11 articles met the inclusion criteria. This highlights the limited research available. Among all articles, a total of 32 patients and their regimens were described. It is difficult to generalize the results of research performed with such a small sample size, especially given that all these patients had their own unique medical comorbidities and treatment circumstances. Going forward, it will be important to evaluate the efficacy of therapeutic interventions with adequately patient samples.
Regarding future research directions, some of the patients described had symptoms of “ritualized slowness” (Charlot et al. 2002) or social withdrawal (Akahoshi et al. 2012) that appeared to be in line with the ever-expanding body of research on behavioral regression or catatonia in patients with DS (Bonne et al., 2023). None of the included articles mentioned assessment of behavioral regression or catatonia as a possible cause of symptoms. Going forward, it will be important to determine whether OCD symptoms emerged spontaneously or as a result of underlying behavioral regression or catatonia, as treatment recommendations may differ depending on the etiology of symptoms.
Overall, outcomes from this scoping rapid review suggests that many of the treatments currently being used to treat OCD and related behaviors in patients with DS often align with evidence-based strategies used in neurotypical individuals and provide partial or significant reduction in symptoms. However, the poor research quality and rigor significantly limit the interpretation such that it is difficult to use them as the basis for evidence-based treatment. In the future, we believe it is necessary to perform more rigorously controlled randomized trials focused on treating OCD in patients with sufficient follow-up to fully assess treatment effectiveness.
References
Akahoshi, K., Matsuda, H., Funahashi, M., Hanaoka, T., & Suzuki, Y. (2012). Acute neuropsychiatric disorders in adolescents and young adults with Down syndrome: Japanese case reports. Neuropsychiatric Disease and Treatment, 339–345. https://doi.org/10.2147/NDT.S32767
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5, No. 5). American psychiatric association.
Ballester, D. A., Filippon, A. P., Braga, C., & Andreoli, S. B. (2005). The general practitioner and mental health problems: Challenges and strategies for Medical Education. Sao Paulo Medical Journal, 123(2), 72–76. https://doi.org/10.1590/s1516-31802005000200008
Berry, C. L., & Schell, R. M. (2006). Reducing hoarding behavior with individualized reinforcement and item return. Behavioral Interventions, 21(2), 123–135. https://doi.org/10.1002/bin.214
Blakeley-Smith, A., Meyer, A. T., Boles, R. E., & Reaven, J. (2021). Group cognitive behavioural treatment for anxiety in autistic adolescents with intellectual disability: A pilot and feasibility study. Journal of Applied Research in Intellectual Disabilities, 34(3), 777–788.
Bull, M. J., Trotter, T., Santoro, S. L., Christensen, C., & Grout, R. W. (2022). Health supervision for children and adolescents with down syndrome. Pediatrics, 149(5). https://doi.org/10.1542/peds.2022-057010
Centers for Disease Control and Prevention (2023, June 28). Data and Statistics on Down Syndrome. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/birthdefects/downsyndrome/data.html
Charlot, L., Fox, S., & Friedlander, R. (2002). Obsessional slowness in Down's syndrome. Journal of Intellectual Disability Research, 46(6), 517–524. https://doi.org/10.1046/j.1365-2788.2002.00419.x
Chicoine, B., Rivelli, A., Fitzpatrick, V., Chicoine, L., Jia, G., & Rzhetsky, A. (2021). Prevalence of common disease conditions in a large cohort of individuals with Down Syndrome in the United States. Journal of Patient-Centered Research and Reviews, 8(2), 86–97. https://doi.org/10.17294/2330-0698.1824
Fineberg, N. A., Reghunandanan, S., Brown, A., & Pampaloni, I. (2012). Pharmacotherapy of obsessive-compulsive disorder: Evidence-based treatment and beyond. Australian & New Zealand Journal of Psychiatry, 47(2), 121–141. https://doi.org/10.1177/0004867412461958
Fujino, H. (2017). Psychological support for young adults with down syndrome: Dohsa-hou program for maladaptive behaviors and internalizing problems. Frontiers in Psychology, 8, 259503. https://doi.org/10.3389/fpsyg.2017.01504
Geldmacher, D. S., Lerner, A. J., Voci, J. M., Noelker, E. A., Somple, L. C., & Whitehouse, P. J. (1997). Treatment of functional decline in adults with Down syndrome using selective serotonin-reuptake inhibitor drugs. Journal of Geriatric Psychiatry and Neurology, 10(3), 99–104. https://doi.org/10.1177/089198879701000302
Gratias, T. M., Purushottam, L., & Descartes, M. (2023, November 28). Downs Syndrome. Practice Essentials, Background, Pathophysiology. https://emedicine.medscape.com/article/943216-overview
Hefti, E., & Blanco, J. G. (2017). Pharmacotherapeutic considerations for individuals with Down Syndrome. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 37(2), 214–220. https://doi.org/10.1002/phar.1880
Huppert, J. D., Simpson, H. B., Nissenson, K. J., Liebowitz, M. R., & Foa, E. B. (2009). Quality of life and functional impairment in obsessive-compulsive disorder: A comparison of patients with and without comorbidity, patients in remission, and healthy controls. Depression and Anxiety, 26(1), 39–45. https://doi.org/10.1002/da.20506
Koran, L. M., Hanna, G. L., Hollander, E., Nestadt, G., Simpson, H. B., & American Psychiatric Association. (2007). Practice guideline for the treatment of patients with obsessive-compulsive disorder. The American Journal of Psychiatry, 164(7 Suppl), 5–53.
Myers, B. A., & Pueschel, S. M. (1991). Psychiatric disorders in persons with down syndrome. The Journal of Nervous and Mental Disease, 179(10), 609–613. https://doi.org/10.1097/00005053-199110000-00004
O'Dwyer, J., Holmes, J., & Collacott, R. A. (1992). Two cases of obsessive-compulsive disorder in individuals with Down's syndrome. The Journal of Nervous and Mental Disease, 180(9), 603–604. https://doi.org/10.1097/00005053-199209000-00015
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., & Moher, D. (2021). Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. Journal of Clinical Epidemiology, 134, 103–112. https://doi.org/10.1016/j.jclinepi.2021.02.003
Patti, P. J., & Tsiouris, J. A. (2006). Psychopathology in adults with Down Syndrome: Clinical findings from an outpatient clinic. International Journal on Disability and Human Development, 5(4). https://doi.org/10.1515/ijdhd.2006.5.4.357
Pekrul, S. R., & Fitzgerald, K. D. (2015). Memantine augmentation in a Down's syndrome adolescent with treatment-resistant obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology, 25(7), 593–595. https://doi.org/10.1089/cap.2015.0073
Prasher, V. P. (1995). Prevalence of psychiatric disorders in adults with Down syndrome. The European Journal of Psychiatry, 9(2), 77–82.
Prasher, V. P., & Day, S. (1995). Brief report: Obsessive-compulsive disorder in adults with Down’s syndrome. Journal of Autism and Developmental Disorders, 25(4), 453–458. https://doi.org/10.1007/bf02179379
Raitasuo, S., Virtanen, H., & Raitasuo, J. (1998). Anorexia nervosa, major depression, and obsessive-compulsive disorder in a Down’s syndrome patient. International Journal of Eating Disorders, 23(1), 107–109. https://doi.org/10.1002/(sici)1098-108x(199801)23:1%3C107::aid-eat15%3E3.0.co;2-z
Rivelli, A., Fitzpatrick, V., Chaudhari, S., Chicoine, L., Jia, G., Rzhetsky, A., & Chicoine, B. (2022). Prevalence of mental health conditions among 6078 individuals with Down Syndrome in the United States. Journal of Patient-Centered Research and Reviews, 9(1), 58–63. https://doi.org/10.17294/2330-0698.1875
Sheehan, K. & Mers, R. (2010). Using neurofeedback to treat OCD symptoms in a low functioning Down syndrome client. Journal of Neurotherapy, 14(4), 345–346. https://doi.org/10.1080/10874208.2010.52335
Sutor, B., Hansen, M., & Black, J. (2006). Obsessive compulsive disorder treatment in patients with Down syndrome: A case series. Down Syndrome Research and Practice, 10(1), 1–3. https://doi.org/10.3104/casestudies.299
Tassé, M. J., Navas Macho, P., Havercamp, S. M., Benson, B. A., Allain, D. C., Manickam, K., & Davis, S. (2016). Psychiatric conditions prevalent among adults with down syndrome. Journal of Policy and Practice in Intellectual Disabilities, 13(2), 173–180. https://doi.org/10.1111/jppi.12156
Weijerman, M. E., & de Winter, J. P. (2010, July 15). Clinical Practice - European Journal of Pediatrics. SpringerLink. https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s00431-010-1253-0
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
Dr. Fodstad is on the Editorial Board of the Journal of Autism and Developmental Disorders; however, the authors have no other disclosures and no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional Author Note
This paper, or a portion of this paper, is not presently under consideration for publication nor has it been published in any other peer reviewed or non-peer reviewed publication. All authors had a contributing role to the development of this manuscript/project. All have read the paper in its current form and have agreed to its content as well as to the author order.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fodstad, J.C., Russell, R., Bullington, M. et al. Treating Obsessive Compulsive Disorder in Adolescents and Adults with Down Syndrome: Results from a Scoping Rapid Review. J Autism Dev Disord (2024). https://doi.org/10.1007/s10803-024-06336-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s10803-024-06336-z