Abstract
Children with autism spectrum disorder (ASD) are five times more likely to have feeding difficulties than neurotypical peers, although the majority of evidence describes feeding difficulty in children age 2 years and older. The purpose of this study is to systematically review the literature on feeding characteristics of children age 0–24 months who were later diagnosed with ASD with an emphasis on the measurement tools used to assess these feeding behaviors. We conducted a systematic review of the literature using PRISMA guidelines. Using selected keywords, a search was conducted using PubMed, PsycINFO, and CINAHL databases for relevant articles to identify feeding characteristics in infants and toddlers (age 0–24 months) later diagnosed with ASD. Sixteen studies were selected for this review by two independent reviewers. Among the selected studies, feeding difficulties were reported in all infant oral feeding modalities (breastfeeding, bottle feeding, and complementary feeding) by infants later diagnosed with ASD. However, the evidence was conflicting among studies regarding feeding characteristics, such as sucking differences while breastfeeding, use of the spoon with feedings, and preference of solid food texture, that presented in infants later diagnosed with ASD. A lack of consistent measurement of feeding behaviors in infants later diagnosed with ASD contributes to the difficulty in comparison across studies. Future research should focus on developing targeted, validated instruments for measuring feeding difficulty in this population with emphasis on breastfeeding and bottle feeding difficulty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Autism spectrum disorder (ASD) is a neurodevelopmental condition that impacts an individual throughout the lifespan with manifestations of restricted interests, repetitive behaviors, and deficiencies in social communication (Hodges et al., 2020). Children with ASD age 18 years and younger are five times more likely to have feeding difficulties as compared to their typically developing peers (Sharp et al., 2013). Recent literature states that the median prevalence of feeding difficulties in ASD was 62% with a wide range of 30–84% due to the variability in assessment methods (Dickson Page et al., 2021).
Oral feeding is one of the most complex developmental tasks that infants must learn to attain adequate growth and nutrition (Manella et al., 2020). Although infants depend on caregivers to provide food, the infant must actively participate in feeding by displaying effective regulation during feeding, communicating effectively when hungry or satiated, and successfully adapting to changes in food texture. Through complex neurodevelopmental tasks, the actions of sucking, swallowing, and breathing coordination while eating and chewing allow for an infant to develop proficiency at the oral feeding modalities of breast, bottle, and complementary (solid food) feeding (Manella et al., 2020). Additionally, feeding proficiency is influenced by other factors such as intellectual ability, oral motor strength, and structural differences of the oral pharyngeal area (Kleinert, 2017). Despite the prevalence of feeding difficulties in the ASD population, ASD screening tools used in the general pediatric primary care setting, such as the Modified Checklist for Autism in Toddlers - Revised (MCHAT-R), do not include any questions about feeding behaviors (Van’t Hof et al., 2020).
Pediatric primary care providers (PCPs) are at the forefront of identifying signs of developmental abnormalities and feeding difficulties in infancy as well as initiating referrals for further neurodevelopmental assessment and early intervention. Infants are typically seen by primary care providers (PCPs) seven times in the first year of life according to the American Academy of Pediatrics (AAP) recommended well child exam schedule. Feeding is a main topic discussed at well child exams as is assessment of growth and development (AAP, 2022). In children with ASD, growth is not typically affected even if feeding difficulty is reported by the parents (Ashley et al., 2020). A greater understanding of the feeding difficulties in infants who are later diagnosed with ASD may provide PCPs more information regarding an infant’s development and could warrant additional screening earlier for neurodevelopmental concerns, such as ASD (Emond et al., 2010).
This systematic review builds upon previous work done by Margari et al. (2020) and Vasilakis et al. (2022). Margari et al. (2020) discussed feeding behaviors of children with ASD and the majority of the reviewed articles focus on breastfeeding duration in infants with ASD rather than the characteristics of breastfeeding that may help to explain breastfeeding duration in infants later diagnosed with ASD. Vasilakis et al. (2022) addressed whether feeding difficulties in the first 24 months of life may be associated with ASD but critical issues such as how feeding difficulties were measured and the implications of variability in the timing and method of measuring feeding difficulty were not addressed in that review. The purpose of this systematic review is to comprehensively assess the existing literature on the prevalence and manifestation of infant feeding difficulties in children who were later diagnosed with ASD. This review also addresses parental concern around feeding difficulty in infants later diagnosed with ASD and the timing of these concerns during the child’s developmental milestones. This review includes newly published articles that have emerged since the last review conducted in 2020 (Margari et al., 2020). Special attention is given to the measurement tools and methods employed to ascertain and report these feeding difficulties in the identified studies. By emphasizing the measurement tools used in the literature, the current review seeks to gain a contextual understanding of the relationship between feeding difficulties in early life and the subsequent detection of ASD.
Methods
Search Strategy
A search strategy was constructed with the guidance of a biomedical librarian and search terms presented in Table 1 were used to conduct a comprehensive search in PubMed, CINAHL, and PsycINFO databases.
No search limits were placed besides limiting the age to infants, toddlers, and children. The search term “children” was included so that articles that may have been focused on feeding difficulties in children with ASD but contained data of feeding characteristics at 0–24 months of age could also be included in the search. References of selected studies were also reviewed during the search. Lastly, a Google search of grey literature was done on this topic with similar search terms. The final search was conducted on May 18, 2023.
Study Selection
Prior to the search, inclusion and exclusion criteria of studies were established. Inclusion criteria were retrospective and prospective studies that had a description of feeding behaviors at ages 0–24 months in children with an ASD diagnosis. Initially, there were no limitations set on how ASD was diagnosed nor how feeding difficulties were assessed because we were also interested in reviewing issues of measurement in this review. Case studies (n = 2) were excluded due to limited results in these studies. Articles where children had a comorbid condition that could affect feeding were excluded. Articles that only reported nutrition information without providing data related to feeding behaviors were also excluded. Studies that included feeding characteristics of infants ages 0–24 months but without stratified data for that age group in the findings were also excluded.
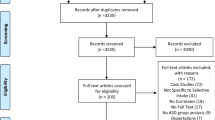
The article selection process is shown in the PRISMA flow diagram (Fig. 1). After duplicates were removed, 880 titles and abstracts identified were screened and 108 articles were found to be eligible for full text review using Endnote©. The most common reasons for article exclusion were specific infant feeding behaviors were not reported (n = 40) and incorrect age of the child (n = 35). Sixteen articles met the inclusion criteria and were included for the final review. No additional articles were selected after screening references of the 16 selected articles. The search for grey literature on this topic through Google also did not produce any additional selected articles. Studies that only reported breastfeeding duration were also excluded due to a previous meta-analysis done recently on this topic by Tseng et al. (2019) and the current review sought to gain a contextual understanding of the relationship between feeding difficulties in early life and the subsequent diagnosis of ASD.
PRISMA flow diagram:a Feeding characteristics of infants and toddlers later diagnosed with autism spectrum disorder (1965–2023). aAdapted from Mohrer et al. (2009)
Data extraction was done independently by two reviewers using Covidence© software (AC and SK). Data extracted on each selected study included the location, design, sample, methodology, measures, and outcomes found regarding feeding difficulties in infancy. Disagreement during extraction was discussed between the two reviewers to reach consensus on all selected articles. Study characteristics that were derived from data extraction are shown in Table 2.
The quality of each quantitative study was independently evaluated by two reviewers using the Newcastle-Ottawa Quality Assessment Form for Case-Control Studies, the Newcastle-Ottawa Quality Assessment Form for Cohort Studies, and for cross-sectional studies, the Newcastle-Ottawa Scale Adapted for Cross-Sectional Studies (Wells et al., 2011). Qualitative studies were assessed using the Critical Appraisal Skills Programme (CASP). Study quality is included in Table 2.
Results
Characteristics of Selected Studies
Of the 16 studies, there were 7 case-control studies, 4 cohort studies, 2 cross-sectional studies, and 3 qualitative studies. Four of the studies used prospective data collection and the remaining 12 studies collected data retrospectively. The studies were conducted in the United States (n = 4), Canada (n = 2), England (n = 2), Denmark (n = 1), the Netherlands (n = 1), France and Belgium (n = 1), Brazil (n = 1), Turkey (n = 1), Sweden (n = 1), China (n = 1), and Poland (n = 1).
The total number of participants in all of the included studies was 96,544 (n = 3,925 participants in the ASD group; n = 92,619 in the control group). Each study used convenience sampling as they all contained participants with known ASD diagnosis (15 studies) or siblings of children with ASD, considered a high-risk group for ASD (1 study). Of the included studies, 12 of the 16 included a control group that included the criteria of: typically developing children with no ASD diagnosis (10 studies), no known ASD in the family (1 study), and a control group of typically developing children from a reference study by Provost et al., 2010 (1 study).
Of the 16 studies, 15 used caregiver report to obtain data while the remaining study used coding of infant feeding videos for data collection (Brisson et al., 2011). Ages of the children whose feeding characteristics were reported at the time of data collection for prospective studies ranged from 2 months of age to 54 months of age, but for this review, we are reporting only the data obtained at the 0–24 month age range as these studies included individual data that could be reported for those specific age ranges. The retrospective studies recruited caregivers who had children that ranged in age from 2 years old to 28 years old. One study (Brisson et al., 2011) did not report an age of the children whose caregivers were recruited to report infant feeding behaviors but was included in this review because the analysis was done on feeding data pertaining to the 0–24 month age range. Of the 16 studies, only 7 reported race of the participants and in all 7 of these studies White participants made up the majority (39% or greater) of the ASD study group. Fourteen of the 16 studies reported sex of the participants and of these 14 studies, 13 had males as the majority (57% or greater) of the ASD study group. 5 of the 16 studies provided income level information of the participants and only 3 of those studies differentiated income levels between the ASD group and comparison group.
Measurement of Autism Diagnosis
The measurement of ASD diagnosis varied across the selected studies. Clinician diagnosis by either a multidisciplinary team, psychiatrist, neurologist, or pediatrician was most commonly used (n = 6), although 5 of these studies did not mention which instrument was used by the clinicians to derive a formal diagnosis (Brisson et al., 2011; Dewrang & Sandberg, 2010; Gray et al., 2018; Nadon et al., 2011; Rogers et al., 2012). Four studies (Kara & Alpgan, 2022; Lucas & Cutler, 2015; Provost et al., 2010; Xiang et al., 2023) used the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV or DSM-5 versions), two studies (Ashley et al., 2020; Brzoska et al., 2021) used the Autism Diagnostic Observation Schedule (ADOS-2), and one study (Lemcke et al., 2018) screened hospital charts for an ICD-10 diagnosis of ASD but no tool was mentioned as to how the diagnosis was obtained. One study (Emond et al., 2010) used clinical records of children suspected of a developmental disorder and a national education database that identified children who received special education services due to an ASD diagnosis. The remaining two studies (Huxham et al., 2019; Lazaro & Ponde, 2017) did not state how ASD was diagnosed.
In addition to diagnostic tools, a few studies used other developmental screening tools to establish severity of a child’s ASD diagnosis. The Childhood Autism Rating Scale (CARS) was used in two studies (Kara & Alpgan, 2022; Xiang et al., 2023) while the Autism Behavior Checklist (ABC), Social Responsiveness Scale (SRS), and Child Neuropsychological and Behaviors Scale-Revision (2016) were used as additional tools to assess ASD severity in the study by Xiang et al., 2023. Additionally, Kara and Alpgan (2022) used the Denver Developmental Screening Test (DDST-II) to evaluate the developmental status of the children diagnosed with ASD in the areas of language, personal social, gross motor, and fine motor-adaptive function.
Measurement of Feeding Characteristics in Infants Later Diagnosed with Autism
The selected studies produced a variety of results that encompassed all modes of infant oral feeding that occur in the first 24 months of life: breastfeeding, bottle feeding, and complementary feeding. The feeding behaviors reported in the selected studies is included in Table 3. With this variety of feeding modes comes a varied range of instruments used to measure the feeding behaviors of infants with ASD. The largest number of studies (n = 7) used either unvalidated caregiver questionnaires or did not state if validity was established to obtain information about the various feeding behaviors including breastfeeding experiences, bottle usage and behavior, complementary food introduction and acceptance, and complementary food preferences (Brzoska et al., 2021; Emond et al., 2010; Huxham et al., 2019; Kara & Alpgan, 2022; Lemcke et al., 2018; Van’t Hof et al., 2020; Xiang et al., 2023). The three qualitative studies used semi-structured caregiver interview guides that included questions on initiation and cessation of breastfeeding, breastfeeding pattern and latch, and the transition and feeding of complementary foods (i.e., the introduction of solid / table foods) (Lazaro & Ponde, 2017; Lucas & Cutler, 2015; Rogers et al., 2012). One study used coded videos of feeding episodes comparing infants later diagnosed with ASD and neurotypical infants on how they opened their mouths when a parent approached them with a spoon during feeding (Brisson et al., 2011).
The remaining studies (n = 5) used an array of different instruments that had some type of validity established with their use in the ASD population. Two studies measured feeding characteristics with the Mealtime Survey developed by Provost et al. (2003). The survey has four sections that include mealtime environment, parental views, early history, and child likes and dislikes. Content validity was established for this instrument by a group of interdisciplinary clinicians with extensive expertise in ASD (Gray et al., 2018; Provost et al., 2010).
The Behavioral Pediatrics Feeding Assessment Scale (BPFAS) was the instrument used in one of the studies to measure feeding behaviors (Ashley et al., 2020). The BPFAS is a 35 item scale in which the first 25 items focus on child feeding behavior and the last 10 items focus on parental feelings and strategies about feeding problems. Content validity was initiated by experts on feeding problems over the past 30 years and factor analysis was done to assess construct validity of the BPFAS in use in the ASD population to create a three factor model to better measure the feeding behaviors in this population (Allen et al., 2017).
The Symptoms of Autism Before Age 2 Scale (SAB-2), a 144 item survey, was used by Dewrang and Sandberg (2010) and was divided into eight different domains that encompassed communication skills, motor skills, sensory perceptions, play and rituals, early notion of ASD, and feeding and sleep behaviors. The authors used the SAB-2 in their study to investigate if this instrument could help differentiate characteristics of children with ASD and neurotypical children at the age of 2 years or earlier, including feeding characteristics. Limited psychometrics of the SAB-2 were established, with authors only reporting interrater reliability (Dewrang & Sandberg, 2010). Upon further review, no other published reports supporting the psychometric properties of the SAB-2 were found.
Similarly, Nadon et al. (2011) used the Eating Profile in their study, which is a 145 item questionnaire that includes eleven domains such as child’s dietary history, the health of the child, the child’s behavior during mealtime, food preferences, oral motor behaviors, communication skills, and family dietary history. The authors report face validity that was established by five occupational therapists with extensive expertise in the ASD population and also a consultant in the ASD field who is a high functioning autistic adult (Nadon et al., 2011). However, no additional psychometrics were reported at the time of the study that established content validity of the Eating Profile. Additional psychometric information for all of the instruments used in the 16 selected studies is found in Supplementary Table 1.
Quality of Studies
Overall, the quality of the literature on feeding behaviors in infants later diagnosed with ASD was fair. Of the studies included, 5 were rated as good, 7 as fair, and 4 as poor. The main source of potential bias was a lack of validated measurement tools for infant feeding behaviors in relation to later ASD diagnosis. For the quantitative studies, an additional source of bias was a lack of adjustment of potential confounders. While age was the most common confounder adjusted for, adjustment for gender, socioeconomic status, and race was not done in many of the studies. In the qualitative studies, the main source of bias was the lack of the researcher stating their own potential bias and how it may have influenced the recruitment and data collection process as well as if it influenced any changes made during the study. Additionally, recall bias in the retrospective studies could influence caregivers’ responses in interviews and surveys given the large amount of time that had lapsed in these studies (up to 28 years) of when these infant feeding difficulties occurred.
Breastfeeding Behaviors
Nine of the studies described breastfeeding behaviors of infants ultimately diagnosed with ASD. Oral motor behaviors such as sucking, gagging, and choking were discussed in four of the articles with conflicting results (Brzoska et al., 2021; Gray et al., 2018; Lucas & Cutler, 2015; Van’t Hof et al., 2020). Gray et al. (2018) found that up to 43% of the children with ASD in their study had unorganized sucking and up to 19% of the children had choking, grimacing, spitting up or gagging with breastfeeding during infancy. However, in this same study up to 46% of the children with ASD were reported as having a strong, continuous suck and were not difficult to feed as infants. Gagging and choking during the first year of age was also not found to be significantly different when compared to the neurotypical control group, according to Provost et al. (2010). A vigorous sucking pattern described by Lucas and Cutler (2015) that represented a dysregulated breastfeeding pattern was reported by mothers of children with ASD in qualitative interviews while an unorganized sucking pattern was significant (p < .05) in children with ASD in another study (Gray et al., 2018). A shorter sucking time before an infant fell asleep during breastfeeding was also found to be significant (p = .04) in the group of children with ASD while weak or chaotic suck was not significantly different between the ASD group and neurotypical group (Brzoska et al., 2021).
In addition to differences in oral motor behavior during breastfeeding in infants later diagnosed with ASD, two large prospective cohort studies found that infants in the ASD group breastfed significantly slower (p < .05) than their neurotypical peers at 2 months and 6 months of age (Emond et al., 2010; Van’t Hof et al., 2020). Overall breastfeeding difficulty in children with ASD was reported by caregivers in three of the studies, with Provost et al. (2010) finding 47% of mothers had difficulty breastfeeding their child with ASD vs. 20% of mothers of neurotypical children encountering difficulty breastfeeding.
Behavior differences during breastfeeding were also reported in infants later diagnosed with ASD. Up to 14% of children with ASD had frequent release of the nipple and were described as fidgety eaters as infants, although the differences between groups did not reach significance (Gray et al., 2018). Infants that exhibited nursing strike, or sudden breastfeeding refusal, were found to have a reduced risk of later ASD diagnosis by 2.6-fold while infants that exhibited no eye contact with their mother during breastfeeding had an increased risk of ASD by 2.3-fold (Kara & Alpgan, 2022). Additional breastfeeding behavior differences that were significant (p < .01) for later child autistic traits included a lack of satiation or consistently acting hungry, which may be an early demonstration of lack of self-regulation skills (Van’t Hof et al., 2020).
Bottle Feeding and Accessories Used During Feeding
Conflicting results regarding bottle feeding and feeding accessory use in infants later diagnosed with ASD was noted among five of the selected studies (Brisson et al., 2011; Brzoska et al., 2021; Lemcke et al., 2018; Nadon et al., 2011; Rogers et al., 2012). When asked about accessories used during feeding, parents of children with ASD reported that they used a bottle with a nipple significantly more often (p = .005) than the neurotypical control group while sippy cup use and regular cup use were found to not be significantly different between the two groups (Brzoska et al., 2021). Difficulties in acceptance in formula changes in their child with ASD were also reported in maternal interviews (Rogers et al., 2012). Another study did not find a significant difference between pacifier use in the ASD group and neurotypical control group as well as bottle feeding duration between the two groups (Nadon et al., 2011).
In regards to use of the spoon with feedings, significantly fewer (p < .01) infants in the ASD group opened their mouths to receive the spoon than neurotypical infants at 4 and 6 months of age (Brisson et al., 2011). Two other studies did not show significant differences between infants later diagnosed with ASD and those without in difficulty using a spoon or interest in a spoon (Brzoksa et al., 2021; Lemcke et al., 2018).
Complementary Feeding
Eight of the selected studies discussed the feeding behaviors of infants later diagnosed with ASD as it relates to complementary feeding (Ashley et al., 2020; Brzoska et al., 2021; Dewrang & Sandberg, 2010; Emond et al., 2010; Huxham et al., 2019; Nadon et al., 2011; Rogers, 2012; Xiang et al., 2023). The timing of when complementary foods were introduced was significantly different (p = .004, p < .001) between infants in the ASD group and neurotypical children as more children with ASD started complementary feeding at an age greater than 6 months while neurotypical children were introduced complementary foods at age 6 months or younger (Emond et al., 2010; Xiang et al., 2023). In Brzoska et al. (2021)’s study, foods with more sophisticated textures such as lumpy or solid foods were introduced significantly later (M = 9.6 months and 12.9 months, respectively; p = .02) for the ASD group as compared to 8.4 months and 10.5 months in the neurotypical control group. The acceptance of complementary foods was significantly decreased (p < .001, p = .004) in infants later diagnosed with ASD during complementary food introduction in two studies (Emond et al., 2010; Xiang et al., 2023) and introducing new foods with more trials or with increased difficulty was significantly different (p = .006, p = .02) between infants later diagnosed with ASD and those without ASD in two studies (Brzoska et al., 2021; Emond et al., 2010). Xiang et al. (2023) also found a 2.7-fold risk of children having ASD if they had poor acceptance of complementary foods (p < .001).
Continued picky eating and food selectivity after the age of one year was highlighted in four studies where by 24 months of age there was a significant difference (p < .001, p < .001, p = .003) in food acceptance among those infants ultimately diagnosed with ASD and those who were not (Ashley et al., 2020; Dewrang & Sandberg, 2010; Emond et al., 2010; & Rogers et al., 2012). In addition to food selectivity, texture sensitivity was also prevalent in the selected studies. Brzoska et al. (2021) found that at 6 months of age or later the ASD group had significantly fewer (p = .004) participants who preferred lumpy foods compared to their neurotypical peers but the two groups did not have a significantly different preference for solid food or fluid texture. In Huxham et al. (2019)’s study, 48.7% of the participants with ASD struggled with foods that were soft and lumpy while 55.6% had difficulty with foods that were chunky and lumpy in texture as infants. In a study that used neurotypical siblings as the comparison group, there was a significant difference (p = .025) for infants later diagnosed with ASD to progress to more textured foods compared to their sibling (Nadon et al., 2011). In addition to receiving complementary foods from a spoon, infants also start feeding themselves complementary foods with their fingers. Neurotypical infants were reported to be significantly more likely (p = .006) to finger feed themselves than infants later diagnosed with ASD (Brzoska et al., 2021) and in another study, 38.8% of the ASD participants did not accept finger foods as an infant although there was no comparison group in this study (Huxham et al., 2019).
Infant Mealtime Behaviors
There was conflicting evidence that infants in the ASD group displayed different feeding behaviors than neurotypical comparison groups. Difficulty determining if a child was hungry or not was significant (p < .001) for the ASD group in a study that assessed behavior and development in children with ASD in the first two years of life (Dewrang & Sandberg, 2010). In another study by Gray et al. (2018), 29% of the participants with ASD required more frequent feedings but when these results were compared to the neurotypical control group in Provost et al.’s (2010) prior study there was not a significant difference between the two groups of infants. Lucas and Cutler (2015) found in their qualitative interviews that mothers struggled with their infants later diagnosed with ASD persistently wanting to breastfeed despite being satiated. In another qualitative study that addressed breastfeeding behaviors of infants later diagnosed with ASD, mothers reported that their infant rejected the breast and would cry uncontrollably while at the breast (Lazaro & Ponde, 2017). However, a large cohort study did not find a significant difference in the behavior of 2 month olds regarding refusing to breastfeed and drinking very liberally (Van’t Hof et al., 2020) and there was no significant difference in mealtime behaviors between the ASD group and neurotypical group until age 36 months of age in another study (Ashley et al., 2020).
Parental Concern About Feeding
In addition to feeding behaviors, parental concern regarding their infant’s development or feeding behavior was reported in four of the selected studies (Gray et al., 2018; Lucas & Cutler, 2014; Provost et al., 2010; Rogers et al., 2012). A significant difference (p < .001, p = .002) in parent concerns regarding their infant’s feeding behaviors occurred in the ASD group at 1–2 years of age in two studies (Gray et al., 2018; Provost et al., 2010) and in another study, mothers began having concerns about their infant’s development starting at 6 months of age (Lucas & Cutler, 2014). Although not significantly different than neurotypical infants, 25% of parents of infants later diagnosed with ASD had concerns about their child’s eating in the first week of life and up to 37% had concerns by the first year of life (Provost et al., 2010). In another study, up to 79% of parents with an infant later diagnosed with ASD had feeding concerns during the birth to one year time interval (Gray et al., 2018).
Discussion
This systematic review identifies feeding characteristics of infants later diagnosed with ASD for all oral feeding modalities as well as infant behaviors during mealtime and parental concerns pertaining to the feeding behaviors of their infants later diagnosed with ASD. All of the articles except one (Lemcke et al., 2018) reported feeding difficulties in infants that were later diagnosed with ASD. The main findings of this systematic review were: (1) the measurement of feeding behaviors in infants later diagnosed with ASD is variable, with caregiver questionnaires, qualitative semi-structured interviews, and standardized scales that assess some feeding characteristics, which leads to difficulty in comparing feeding characteristics in this population; (2) the heterogeneity of ASD poses a challenge in identifying feeding characteristics in infants later diagnosed with ASD and the influence that varying autistic traits has on infant feeding behaviors is unclear; (3) difficulty in infant regulation and lack of social cues while breastfeeding may contribute to mothers’ challenges in exclusively breastfeeding their infant later diagnosed with ASD for a longer duration; (4) transition difficulties in breast, bottle, and complementary feeding should be assessed at younger ages during infancy; and (5) parental concern regarding feeding difficulties during infancy should be addressed and further evaluation of these concerns should be done to identify feeding characteristics that may indicate a larger developmental problem.
Measurement Issues
While this review presents feeding characteristics in children with ASD at 0–24 months of age, the majority of selected studies report various feeding difficulties, including breastfeeding issues, difficulties with the introduction of complementary foods, and variation in satiety cues during this time period. This is not surprising as children with ASD are five times more likely to have feeding difficulties than their neurotypical peers (Sharp et al., 2013). There are a variety of different conceptualizations of feeding difficulty in the ASD and general pediatric feeding literature. In reviewing the ASD literature, the terms “feeding problem,” “feeding disorder,” and “difficulty feeding” are used synonymously to describe the typical feeding challenges experienced by children with ASD. Definitions include a variety of conceptualizations such as a range of problematic behaviors that are recurrent during meals; extreme food restriction based on sensory characteristics of the food; fear of new foods; negative behavior at mealtimes; prolonged duration of feeding; and a child being unwilling or unable to eat or drink an adequate amount of food despite its availability to appropriately grow, hydrate, and develop (Aponte & Romanczyk, 2016; Ashley et al., 2020; Pados et al., 2018). However, most of these terms are used in reference to children with ASD over the age of 2 years and there is a paucity of data regarding feeding challenges experienced before the age of 2 years by children who are later diagnosed with ASD.
The lack of a consensus definition ultimately leads to difficulty in use of a uniform measurement tool to enable easier comparison of results among studies that operationalize this concept (Mari-Bauset et al., 2014). Goday et al. (2019) derived a consensus definition as well as a conceptual framework of “Pediatric Feeding Disorder” based on the World Health Organization’s International Classification of Functioning, Disability, and Health (ICF). Although this framework is not specific to the ASD population, its concepts can be applied to measurement of feeding difficulties in infants later diagnosed with ASD and the results of the selected studies in this review can be applied within this framework. Since most children with ASD with feeding difficulty do not have growth issues, investigating other reasons for feeding difficulty can be directed by the ICF in relation to medical, feeding skill, or psychosocial dysfunction. This framework also allows for both measurement at different stages of feeding development as well as all oral feeding modalities during the first 24 months of life: breast, bottle, and complementary feeding. Medical dysfunction in feeding may include hypotonia, which is found more often in infants later diagnosed with ASD as compared to neurotypical infants which may cause gagging and choking with feeding that was reported in select studies in this review (Gray et al., 2018). The concept of feeding skill dysfunction is also represented in studies as manifested by preference of smooth textures as compared to chunkier textures of complementary foods, lack of finger feeding, and nipple preferences with bottle feeding (Brzoska et al., 2021; Gray et al., 2018; Huxham et al., 2019). Psychosocial dysfunction during feeding by infants later diagnosed with ASD is portrayed in selected studies as lack of eye contact during breastfeeding, behaviors displaying constant hunger despite just being fed, and uncontrollable crying during breastfeeding (Dewrang & Sandberg, 2010; Kara & Alpgan, 2022; Lazaro & Ponde, 2017; Van’t Hof et al., 2020).
In addition to a lack of a consensus definition of feeding difficulties, the timing of diagnosis may also contribute to a lack of validated measurement tools used in the ASD infant feeding literature. While there are measures available that have been validated in children with ASD, including the Pedi-EAT, Montreal Children’s Feeding Scale, and the Behavioral Pediatrics Feeding Assessment Scale, these scales are for use in children 6 months and older for complementary feeding (Allen et al., 2015; Thoyre et al., 2014; Van Dijk et al., 2021). While most children with ASD are not diagnosed until age 2 years or older, it is difficult to ascertain if infants with feeding difficulties will ultimately be diagnosed with ASD. Although there are a plethora of breastfeeding measurement tools that examine breastfeeding characteristics such as sucking and rooting behaviors in both preterm and term infants (Pados et al., 2018), there are none that are validated for infants later diagnosed with ASD. This is likely due to ASD not being able to be diagnosed at birth, thus making it more difficult to perform psychometric studies for these instruments in infants.
Variability of Autistic Traits on Feeding Behavior
In addition to measurement difficulty due to different oral feeding modalities and evolving feeding development that comes with age, ASD is a spectrum disorder with varying autistic traits. The heterogeneity of ASD further complicates the measurement aspect of diagnosis and assessment of autistic traits. The studies included in this review demonstrate the variability in measurement for the diagnosis of ASD as three different instruments were reported for diagnostic use as well as only two studies that assessed for ASD trait variability (Kara & Alpgan, 2022; Xiang et al., 2023). The variability in both the diagnostic measurement and the differing autism characteristics among the participants in the selected studies adds to the difficulty of comparing findings across studies.
Another challenge in measuring infant feeding behaviors in children with ASD is that intellectual disability occurs in approximately one-third of individuals with ASD (Rydzewska et al., 2018). The severity of oral feeding symptoms is noted to increase as the severity of intellectual disability increases (Kleinert, 2017). Children with intellectual disabilities may be affected in feeding function by self-feeding limitations and ineffective chewing and swallowing, and especially in the case of children with ASD, sensory dysfunction may contribute to these difficulties in handling food both by the hands and the mouth (Ooka et al., 2012). Although intelligence levels cannot be measured in infancy, symptoms of intellectual disability can manifest in infancy. Specific autistic traits and intelligence level could help to explain differences in how infants respond to the spoon, dexterity at holding a bottle, sucking strength and rate, and ability to eat more textured complementary foods. More work is needed to determine if specific autistic traits influence the level of feeding difficulty in infants and if there are differences in presentation of these difficulties in all modalities of oral feeding for better screening and interventions in the future. It would be helpful in future studies that examine infant feeding characteristics in ASD to use measurement tools that provide a more detailed description of autistic traits as well as any intellectual disability to further compare feeding characteristics across studies.
The Impact of Feeding Challenges on Breastfeeding Duration in ASD
Breastfeeding duration has been more widely studied and a recent meta-analysis by Tseng et al. (2019) found that infants later diagnosed with ASD did breastfeed for a shorter period compared to neurotypical infants. The prevalence of children with ASD who were breastfed at the ages of 1 month and 6 months was significantly less than children without ASD in this meta-analysis. However, more specific data is needed that explains why breastfeeding duration is shorter in infants with ASD.
Based on the findings in this systematic review, behaviors such as lack of eye contact while breastfeeding, quality and pattern of sucking during breastfeeding, and satiation cues should be considered in future studies as early behaviors of regulation difficulty and social difficulty seen in ASD. In addition, breastfeeding is highly contextual and there are other external factors that may contribute to duration of breastfeeding such as previous experience with breastfeeding, age of the mother, employment status and maternity leave length, recurrent life stressors, and maternal personal attitude of enjoying breastfeeding; all have been found to predict duration of breastfeeding (McKinley & Hyde, 2004; Schafer et al., 2019). More studies are needed that examine these signs of early regulation and social difficulty in infants later diagnosed with ASD during breastfeeding as well as the external influences that contribute to a mother’s cessation of breastfeeding for better screening and intervention for breastfeeding difficulties in this population. More studies using sibling comparison groups would also aid in exposing some of the contextual factors that may influence breastfeeding duration as well as differences in the breastfeeding behaviors in an infant later diagnosed with ASD and a neurotypical sibling. Only one study in this review used a sibling comparison group and there were no differences in breastfeeding duration reported but no other specific breastfeeding characteristics were presented in this study (Nadon et al., 2011).
Complementary Feeding Difficulty and Age of Onset
Many of the selected studies described feeding difficulties associated with complementary foods but varied in timing of these difficulties. While some studies reported difficulty initiating or transitioning to complementary foods around 6 months of age, some did not find a significant difference in complementary feeding in the ASD samples until 15–24 months of age (Ashley et al., 2020; Emond et al., 2010). The difficulty in initiating complementary feeding and transitioning to more sophisticated textures could be explained by the restrictive and repetitive nature that children with ASD often display and also by sensory sensitivities that so often are found in these children as well. Given that there are already measurement tools that are validated in the ASD population for complementary foods, more studies that use these measures to better compare complementary feeding behaviors across studies would provide more robust evidence of when to monitor for these feeding difficulties and develop interventions to help caregivers handle these feeding challenges.
In addition to focusing on when feeding difficulties occur in infants later diagnosed with ASD as it relates to complementary feeding, additional studies are needed to explore when difficulties with breast or bottle feeding begin to occur. In some studies, infants later diagnosed with ASD started exhibiting signs of feeding difficulty with the bottle or breast after a few months of age (Emond et al., 2010; Van’t Hof et al., 2020). While the qualitative studies addressed initiation of breastfeeding, the larger quantitative studies did not ask questions about breastfeeding or bottle feeding difficulty until 2 months of age or older. Assessing for feeding difficulties at birth in larger samples may allow for a more varied description of feeding characteristics to monitor for in infants possibly at risk for ASD as well as beginning interventions at a young age to aid in better breastfeeding rates in the ASD population.
Addressing Parent Concern
Parents are at the forefront of feeding their infant and due to the repetitive nature of infant feeding, they are the ones who are able to observe firsthand if their infant’s feeding characteristics change or if difficulty with certain feeding modalities occur. Given that Gray et al. (2018) reports that up to 79% of the parents of children with ASD had concerns about their infant’s feeding in the first year of life and that 25% of the parents of children with ASD in Provost et al. (2010)’s study had concerns about their infant’s feeding in the first week of life, these percentages should be considered in future work in this area of research. Even if parents do report these feeding difficulties to a primary care provider, it may be difficult to simulate these behaviors in a clinic setting during well child exams so that a clinician may observe the concerning feeding behaviors of the infant. A mixed method approach that takes into account parental concern around infant feeding behaviors in the first year as well as contextual factors such as home feeding practices, cultural influences, and family dynamics may better inform how parental concern can be better addressed in the pediatric primary care setting and how clinicians can better screen for these feeding concerns in the first year of life while obtaining a patient history during routine well child exams.
Strengths and Limitations
This systematic review has several strengths in that we systematically searched the literature for feeding difficulties in infants later diagnosed with ASD in all oral feeding modalities (breastfeeding, bottle feeding, complementary feeding) during the 0–24 month age range as well as compared measurement modalities in the selected articles. This review adds additional breadth to the reviews done previously by Vasilakis et al. (2022) and Margari et al. (2020) by providing additional articles as well as a focus on measurement issues related to feeding in this patient population. Although we did not find any additional studies in the grey literature, it was searched as well to include dissertation work that may encompass our inclusion criteria. Limitations of this review were that we did not include case studies due to their very small sample size, and we did not include articles that were not available in English. A lack of reported demographic characteristics as well as low representation of female and racially diverse participants with ASD in the selected studies also limits the generalizations that can be made from this systematic review.
Conclusions
Evidence from this review suggests that feeding difficulties during infancy are prevalent in children with ASD and that pediatric primary care providers should be aware when these feeding characteristics are communicated during clinic visits. While not every infant who has difficulty feeding will ultimately be diagnosed with ASD, an understanding of these feeding difficulties can aid in a clinician’s surveillance for other signs of ASD as an infant grows older such as speech delay, motor delays from hypotonia, and impaired social interactions to possibly aid in diagnosing ASD at a younger age. Because these feeding difficulties typically do not affect growth, emphasis is needed on asking the correct questions to parents during infant well child exams regarding the characteristics of feeding to determine if feeding difficulty is truly occurring and how support can be given to the family to help with these difficulties. Taking a thorough history with targeted questions on feeding behaviors can also aid in earlier referral for occupational or speech therapy for feeding difficulties to help improve the feeding experience for the infant and alleviate stress for the parent.
Future research should focus on developing targeted, validated instruments for identifying feeding difficulty in infants later diagnosed with ASD with emphasis on breastfeeding and bottle feeding difficulty. These instruments should include questions that address sucking and swallowing behaviors as well as social behaviors, such as eye contact during feeding. Including bottle and breastfeeding screening questions from already existing instruments that monitor development of infants at risk for ASD, such as the Parent Observation of Early Markers Scale (POEMS), can be integrated into a comprehensive feeding screening tool to be used in the pediatric primary care setting (Feldman et al., 2011). The heterogeneity of ASD itself makes it difficult to measure infant feeding characteristics and future work needs to take into account measuring autistic traits to further parse out infant feeding symptoms that may occur along the autism spectrum. As the total number of children with ASD included in these studies is relatively small, the need for a future large scale study is apparent where more children with ASD that are representative of the general population of children age 0–24 months are included. Developing studies that encompass a more diverse ethnic and socioeconomic population as well as more females with ASD would be helpful in adding more depth to the research in this field. Further longitudinal studies are also needed where feeding difficulties from birth onwards are captured to provide additional insight into feeding challenges experienced within the first six months of life by infants later diagnosed with ASD.
References
Allen, S. L., Smith, I. M., Duku, E., Vaillancourt, T., Szatmari, P., Bryson, S., Fombonne, E., Volden, J., Waddell, C., Zwaigenbaum, L., Roberts, W., Mirenda, P., Bennett, T., Elsabbagh, M., & Georgiades, S. (2015). Behavioral pediatrics feeding assessment scale in young children with autism spectrum disorder: Psychometrics and associations with child and parent variables. Journal of Pediatric Psychology, 40(6), 581–590. https://doi.org/10.1093/jpepsy/jsv006.
American Academy of Pediatrics (2022). AAP schedule of well child care visits. https://www.healthychildren.org/English/family-life/health-management/Pages/Well-Child-Care-A-Check-Up-for-Success.aspx.
Aponte, C. A., & Romanczyk, R. G. (2016). Assessment of feeding problems in children with autism spectrum disorder. Research in Autism Spectrum Disorders, 21, 61–72. https://doi.org/10.1016/j.rasd.2015.09.007.
Ashley, K., Steinfeld, M. B., Young, G., & Ozonoff, S. (2020). Onset, trajectory, and pattern of feeding difficulties in toddlers later diagnosed with autism. Journal of Developmental and Behavioral Pediatrics, 41, 165–171. https://doi.org/10.1097/DBP.0000000000000757.
Brisson, J., Warreyn, P., Serres, J., Foussier, S., & Adrien-Louis, J. (2011). Motor anticipation failure in infants with autism: A retrospective analysis of feeding situations. Autism, 16(4), 420–429. https://doi.org/10.1177/1362361311423385.
Brzoska, A., Kazek, B., Koziol, K., Kapinos-Gorczyca, A., Ferlewicz, M., Babraj, A., Makosz-Raczek, A., Likus, W., Paprocka, J., Matuskik, P., & Emich-Widera, E. (2021). Eating behaviors of children with autism – pilot study. Nutrients, 13, 2687. https://doi.org/10.3390/nu13082687.
Crist, W., McDonnell, P., Beck, M., Gillespie, C. T., Barrett, P., & Mathews, J. (1994). Behavior at mealtimes and the young child with cystic fibrosis. Developmental and Behavioral Pediatrics, 15(3), 157–161. https://doi.org/10.1097/00004703-199406000-00001.
Dewrang, P., & Dahlgren Sandberg, A. (2010). Parental retrospective assessment of development and behavior in Asperger syndrome during the first 2 years of life. Research in Autism Spectrum Disorders, 4, 461–473. https://doi.org/10.1016/j.rasd.2009.11.003.
Dickson Page, S., Souders, M. C., Kral, T. V. E., Chao, A. M., & Pinto-Martin, J. (2021). Correlates of feeding difficulties among children with autism spectrum disorder: A systematic review. Journal of Autism and Developmental Disorders, 52(1), 255–274. https://doi.org/10.1007/s10803-021-04947-4
Emond, A., Emmett, P., Steer, C., & Golding, J. (2010). Feeding symptoms, dietary patterns, and growth in young children with autism spectrum disorders. Pediatrics, 126(2), e337–e342. https://doi.org/10.1542/peds.2009-2391.
Feldman, M. A., Ward, R. A., Savona, D., Regehr, K., Parker, K., Hudson, M., Penning, H., & Holden, J. A. (2011). Development and initial validation of a parent report measure of the behavioral development of infants at risk for autism spectrum disorders. Journal of Autism and Developmental Disorders, 42, 13–22. https://doi.org/10.1007/s10803-011-1208-y.
Goday, P. S., Huh, S. Y., Silverman, A., Lukens, C. T., Dodrill, P., Cohen, S. S., Delaney, A. L., Feuling, M. B., Noel, R. J., Gisel, E., Kenzer, A., Kessler, D. B., de Camargo, K., Browne, O., & Phalen, J., J. A (2019). Pediatric feeding disorder: Consensus definition and conceptual framework. Journal of Pediatric Gastroenterology and Nutrition, 68(1), 124–129. https://doi.org/10.1097/MPG.0000000000002188.
Gray, H. L., Sinha, S., Buro, A. W., Robinson, C., Berkman, K., Agazzi, H., & Shaffer-Hudkins, E. (2018). Early history, mealtime environment, and parental views on mealtime and eating behaviors among children with ASD in florida. Nutrients, 10, 1867. https://doi.org/10.3390/nu10121867.
Hazirah Jaafar, N., Othman, A., Majid, N. A., Harith, S., & Zabidi-Hussin, Z. (2019). Parent-report instruments for assessing feeding difficulties in children with neurological impairments: A systematic review. Developmental Medicine & Child Neurology, 61(2), 135–144. https://doi.org/10.1111/dmcn.13986.
Hodges, H., Fealko, C., & Soares, N. (2020). Autism spectrum disorder: Definition, epidemiology, causes, and clinical evaluation. Translational Pediatrics, 9(Suppl 1), S55–S65. https://doi.org/10.21037/tp.2019.09.09.
Huxham, L., Marais, M., & van Niekerk, E. (2019). Idiosyncratic food preferences of children with autism spectrum disorder in England. South African Journal of Clinical Nutrition, 34(3), 90–96. https://doi.org/10.1080/16070658.2019.1697039.
Kara, T., & Alpgan, O. (2022). Nursing personality and features in children with autism spectrum disorder aged 0–2: An exploratory case-control study. Nutritional Neuroscience, 25(6), 1200–1208. https://doi.org/10.1080/1028415X.2020.1843891.
Kleinert, J. O. (2017). Pediatric feeding disorders and severe developmental disabilities. Seminars in Speech and Language, 38, 116–125. https://doi.org/10.1055/s-0037-1599109.
Lazaro, C. P., & Ponde, M. P. (2017). Narratives of mothers of children with autism spectrum disorders: Focus on eating behavior. Trends in Psychiatry and Psychotherapy, 39(3), 180–187. https://doi.org/10.1590/2237-6089-2017-0004.
Lemcke, S., Parner, E. T., Bjerrum, M., Thomsen, P. H., & Lauritsen, M. B. (2018). Early regulation in children who are later diagnosed with autism spectrum disorder. A longitudinal study within the Danish national birth cohort. Infant Mental Health Journal, 39(2), 170–182. https://doi.org/10.1002/imhj.21701.
Lucas, R. F., & Cutler, A. (2015). Dysregulated breastfeeding behaviors in children later diagnosed with autism. The Journal of Perinatal Education, 24(3), 171–180. https://doi.org/10.1891/1058-1243.24.3.171.
Manella, J. A., Forestell, C. A., Ventura, A. K., & Fisher, J. O. (2020). The development of infant feeding. In J.J. Lockman & C.S. Tamis-LeMonda (Eds.) pp.263–291). The cambridge handbook of infant development (pp. 263–291). Cambridge University Press; 2020. https://doi.org/10.1017/9781108351959.010.
Margari, L., Marzulli, Gabellone, A., & De Giambattista, C. (2020). Eating and mealtime behaviors in patients with autism spectrum disorder: Current perspectives. Neuropsychiatric Disease and Treatment, 16, 2083–2102. https://doi.org/10.2147/NDT.S224779.
Mari-Bauset, S., Zazpe, I., Mari-Sanchis, A., Llopis-Gonzalez, A., & Varela, M. M. (2014). Food selectivity in autism spectrum disorders: A systematic review. Journal of Child Neurology, 29(11), 1554–1561. https://doi.org/10.1177/0883073813498821.
McKinley, N. M., & Hyde, J. S. (2004). Personal attitudes or structural factors? A contextual analysis of breastfeeding duration. Psychology of Women Quarterly, 28(4), 388–399. https://doi.org/10.1111/j.1471-6402.2004.00156.x.
Mohrer, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62, 1606–1612. https://doi.org/10.1016/j.jclinepi.2009.06.005.
Nadon, G., Feldman, D. E., Dunn, W., & Gisel, E. (2011). Mealtime problems in children with autism spectrum disorder and their typically developing siblings: A comparison study. Autism, 15(1), 98–113. https://doi.org/10.1177/1362361309348943.
Ooka, T., Takahashi, M., & Mukai, Y. (2012). The relationship between feeding characteristics and feeding function in children with intellectual disability. Pediatric Dental Journal, 22(2), 145–154. https://doi.org/10.1016/S0917-2394(12)70265-3.
Pados, B. F., Thoyre, S. M., Estrem, H. H., Park, J., & McComish, C. (2018). Factor structure and psychometric properties of the neonatal eating assessment tool-breastfeeding. Journal of Obstetric Gynecologic & Neonatal Nursing, 47(3), 396–414. https://doi.org/10.1016/j.jogn.2018.02.014.
Provost, B., Crowe, T. K., Osbourn, P. L., McClain, C., & Skipper, B. J. (2010). Mealtime behaviors of preschool children: Comparison of children with autism spectrum disorder and children with typical development. Physical & Occupational Therapy in Pediatrics, 30(3), 220–233. https://doi.org/10.3109/01942631003757669.
Rogers, L. G., Magill-Evans, J., & Rempel, G. R. (2012). Mothers’ challenges in feeding their children with autism spectrum disorder – managing more than just picky eating. Journal of Developmental and Physical Disabilities, 24, 19–33. https://doi.org/10.1007/s10882-011-9252-2.
Rydewska, E., Hughes-McCormack, L. A., Gillberg, C., Henderson, A., MacIntyre, C., Rintoul, J., & Cooper, S. (2018). Prevalence of long-term health conditions in adults with autism: Observational study of a whole country population. British Medical Journal Open, 8, e023945. https://doi.org/10.1136/bmjopen-2018-023945.
Schafer, E. J., Buch, E. D., Campo, S., & Ashida, S. (2019). From initiation to cessation: Turning points and coping resources in the breastfeeding experience of first-time mothers. Women & Health, 59(4), 449–463. https://doi.org/10.1080/03630242.2018.1487904.
Sharp, W. G., Berry, R. C., McCracken, C., Nuhu, N. N., Marvel, E., Saulnier, C. A., Klin, A., Jones, W., & Jaquess, D. L. (2013). Feeding problems and nutrient intake in children with autism spectrum disorders: A meta-analysis and comprehensive review of the literature. Journal of Autism and Developmental Disorders, 43(9), 2159–2173. https://doi.org/10.1007/s10803-013-1771-5.
Thoyre, S. M., Pados, B. F., Park, J., Estrem, H., Hodges, E. A., McComish, C., Van Riper, M., & Murdoch, K. (2014). Development and content validation of the pediatric eating assessment tool (Pedi-EAT). American Journal of Speech-Language Pathology, 23, 46–59. https://doi.org/10.1044/1058-0360(2013/12-0069).
Tseng, P., Chen, Y., Stubbs, B., Carvalho, A. F., Whitely, P., Tang, C., Yang, W., Chen, T., Li, D., Chu, C., Yang, W., Liang, H., Wu, C., Yen, C., & Lin, P. (2019). Maternal breastfeeding and autism spectrum disorder in children: A systematic review and meta-analysis. Nutritional Neuroscience, 22(5), 354–362. https://doi.org/10.1080/1028415X.2017.1388598.
Van Dijk, M. W. G., Buruma, M. E., & Blijd-Hoogewys, E. M. A. (2021). Detecting feeding problems in young children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 51(11), 4115–4127. https://doi.org/10.1007/s10803-021-04869-1.
Van’t Hof, M., et al. (2020). Do early-life eating habits predict later autistic traits? Results from a population-based study. Appetite, 156, https://doi.org/10.1016/j.appet.2020.104976.
Vasilakis, M., Polychronis, K., Panagouli, E., Tzila, E., Papageorgiou, A., Thomaidou, L., Psaltopoulou, T., Tsolia, M., Sergentanis, T. N., & Tsitsika, A. K. (2022). Food difficulties in infancy and ASD: A literature review. Children, 10(1), 84. https://doi.org/10.3390/children10010084.
Wells, G. A., Shea, B., O’Connell, D., Peterson, J., Welch, V., Losos, M., & Tugwell, P. (2011). The Newcastle-ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Xiang, X., Yang, T., Chen, J., Dai, Y., Zhang, J., Li, L., Jia, F., Wu, L., Hao, Y., Ke, X., Yi, M., Hong, Q., Chen, J., Fang, S., Wang, Y., Wang, Q., Jin, C., & Li, T. (2023). Association of feeding patterns in infancy with later autism symptoms and neurodevelopment: A national multicentre survey. Bmc Psychiatry, 23, 174. https://doi.org/10.1186/s12888-023-04667-2.
Acknowledgements
The authors would like to acknowledge Dr. Julie Barroso for proofreading the final draft of this manuscript.
Funding
No funding was received to assist with this review and was done as part of the first author?s PhD training. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
AAC conducted the systematic review, supervised by SMK. MM provided critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
This systematic reviewed followed PRISMA guidelines. No ethical approval is required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Campbell, A.A., Karp, S.M. & Mogos, M. Feeding Behaviors in Infants and Toddlers Later Diagnosed with Autism Spectrum Disorder: A Systematic Review. J Autism Dev Disord (2024). https://doi.org/10.1007/s10803-024-06303-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s10803-024-06303-8