Abstract
The Emotion Dysregulation Inventory (EDI) was designed and validated to quantify emotion dysregulation (ED) in school-age children, with a particular emphasis on capturing ED in youth with ASD. We saw a need to adapt the EDI for use in young children (ages 2–5) given early childhood is a formative time for emotion regulation development. The present study discusses the adaptation process for the EDI-Young Child (EDI-YC), including item refinement/generation and cognitive interviews (N = 10 with ASD), consistent with the Patient-Reported Outcomes Measurement Information System (PROMIS®) methodology. The item bank was piloted in a sample of 2-year-olds with and without ASD (N = 31), which provided initial support for the EDI-YC as a valid and reliable measure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Emotion regulation, or the ability to modify one’s arousal and emotional state in service of one’s goals, is a transdiagnostic process with relevance to nearly every aspect of development. Although not part of the core diagnostic criteria for autism spectrum disorder (ASD), difficulties with emotion regulation (i.e., emotion dysregulation; ED) are more common and more severe in individuals with ASD than in neurotypical peers (Conner et al., 2021). Research suggests that ED difficulties may start early in children with ASD, however research on the early childhood period has been limited (see Cibralic et al., 2019 for review). The lack of validated ED measures for young children with ASD is one of the key barriers contributing to the dearth of research in this area. The objective of this paper is to describe the development of an ED measure for toddlers and preschool aged children (ages 2–5) with ASD.
Role of Emotion Dysregulation in ASD
The available evidence suggests that ED may manifest in early childhood for children with ASD. For example, toddlers with ASD demonstrate lower positive and higher negative affect and less “soothability” than neurotypical peers (Clifford et al., 2013; Day et al., in press; Garon et al., 2016; Macari et al., 2017). Retrospective studies and prospective studies of the younger siblings of children with ASD suggest that these differences may even begin in infancy (Adrien et al., 1993; Werner et al., 2000; Garon et al., 2016). Research in the preschool age period further suggests that young children with ASD have delays in the use of adaptive emotion regulation strategies compared to their peers without ASD (Jahromi et al., 2012; Konstantareas & Stewart, 2006; Nuske et al., 2017). Early ED in ASD is particularly problematic because it sets the stage for future problems. Manifestations of severe ED during early childhood have been shown to predict later psychiatric symptoms in non-ASD populations, with younger onset of ED predicting greater risk for subsequent internalizing and externalizing disorders (Hofstra et al., 2002; Kim-Cohen et al., 2003). Within ASD, cross-sectional studies in older children, adolescents, and adults have also documented a relationship between ineffective ER and psychiatric symptoms (Mazefsky et al., 2014; Rieffe et al., 2011; Samson et al., 2015), and a study of young children with ASD demonstrated that ED was related to internalizing and externalizing symptoms 10 months later (Berkovits et al., 2016).
Recent estimates from the Centers for Disease Control and Prevention indicate that the majority of children with ASD have at least one behavioral/psychiatric co-occurring condition by 4 years of age; for example, by age 4 over 50% of the sample had temper tantrums and over 50% had a mood disorder documented in their health and/or educational records (Soke et al., 2018). Such symptoms are a critical reason that parents seek psychosocial or pharmacological support services for their child (Croen et al., 2006; Madden et al., 2017), likely because emotional and behavioral challenges take a significant toll on family functioning (Herring et al., 2006; Nuske et al., 2018). Recently, compelling evidence was reported tying ED in youth with ASD to concurrent internalizing and externalizing symptoms (Mazefsky, Yu, et al., 2018b) and to a higher likelihood of psychiatric service use, including hospitalization and the use of emergency services (Conner et al., 2021). Problems with ED in early childhood have also been linked to greater social challenges in middle and late childhood for children with ASD (Blair et al., 2015).
Taken together, this research suggests that early ED has a wide range of cascading effects on psychological and social outcomes. Although ED may be tractable with intervention, particularly if implemented early in childhood (Kasari et al., 2010; Scarpa & Reyes, 2011; Weiss et al., 2017), there are currently no evidenced-based intervention targeting ED that are appropriate for use in preschool-aged children with ASD. One major barrier to intervention development focused on ED in ASD has been a lack of sensitive measures suitable for use across the range of cognitive and verbal functioning in this population.
Measurement of Emotion Dysregulation in ASD
Most existing measures of ED were developed for the general population and excluded youth with ASD when assessing psychometric properties. In response to this need, our group developed the Emotion Dysregulation Inventory (EDI), a parent-report measure of ED developed specifically for school-aged children, adolescents, and young adults with ASD that can be used to assess youth from ages six to 21 across a wide range of verbal and cognitive functioning (Mazefsky et al., 2018a, b). It taps two facets of ED: (1) Reactivity, which captures rapidly escalating, intense, and poorly regulated negative affect; and (2) Dysphoria, which reflects sadness, low positive affect, and unease.
The EDI was developed using guidelines from the NIH Roadmap Initiative focused on developing sensitive outcome measures, Patient-Reported Outcomes Measurement Information System (PROMIS®; http://www.nihpromis.org; Cella et al., 2007, 2010). The multiple-site PROMIS® research network (2013) produced scientific standards for developing effective and sensitive outcome measures for clinical use. There is evidence to suggest that measures developed through PROMIS® methods assess a wider range of functioning with greater precision than legacy measures (e.g., Pilkonis et al., 2011). The PROMIS® methodology has been used to develop over 300 measures, with the EDI being the first to apply this framework for use in ASD. The EDI has been shown to be a valid, reliable, and change-sensitive measure of ED for use in both ASD and general population samples (Mazefsky, Yu et al., 2018b; Mazefsky et al., 2020), with superior precision using fewer items than prior existing measures of ED. Thus, it is a highly efficient and sensitive outcome measure for school-aged youth across populations.
While the development of the EDI represents an important advance in measurement of ED in ASD, there remains a pressing need for measures capturing variability in ED early in childhood. Several features distinguish ED in the early childhood period from ED later in childhood and adolescence. Early childhood (defined within as between 2 and 5 years of age) encompasses a critical time for emotion regulation development during which children are first developing independent regulation skills (Cole et al., 1994). The contexts and behaviors associated with ED are expected to be different in young children (e.g., ED in response to transitions or separation, use of comfort objects in response to ED). Further, ED is common during this time period in typical development (Cole et al., 1994), which makes it challenging to identify when ED is atypical or warrants intervention. Preliminary evidence suggests that ED is even more severe in young children with ASD than their neurotypical peers (Macari et al., 2018; Nuske et al., 2017; Day et al., in press), but there are limitations with existing measures (as described below). A valid measure of ED specifically developed for young children with and without ASD that takes normative peaks in ED into account and is sensitive to a wide range of ED would contribute to our knowledge about deviations of ED in ASD during early childhood.
Several early childhood measures capturing features of ED have been developed and validated in non-ASD samples and some—such as the Toddler Behavior Assessment Questionnaire (Goldsmith, 1996) and the Child Behavior Checklist Ages 1.5–5 (Achenbach & Rescorla, 2000)—have even been used in the ASD literature (Garon et al., 2016; Macari et al., 2017; Rescorla et al., 2017; Samson et al., 2014). However, these measures have not been validated with ASD samples and it is not clear that psychometric properties would remain the same. Without the inclusion of ASD children at the development stage, it is also unclear whether these measures would sufficiently capture the range of ED seen in this population. Further, many of these measures do not explicitly measure ED and most were not developed to maximize change sensitivity. Consequently, these measures may not be sensitive to the range of ED that young child with ASD exhibit, and they have questionable utility as outcome measures.
An ideal measure of ED in early childhood would allow for links to be made across developmental periods so that researchers could begin to capture change in ED from early to later childhood and adolescence. One potential method for accomplishing these goals is using PROMIS® methodology to adapt valid measures of ED developed for older populations to a younger sample. A recent paper by Blackwell et al. (2020) illustrated the application of the item generation and refinement process from the PROMIS initiative to a set of 12 new PROMIS early childhood measures, including scales tapping ED (e.g., anger/irritability, self-control/self-regulation). Although this study was in development at the same time as the present study, the authors made a number of recommendations based on their work that are consistent with the approach we took, including obtaining input from diverse experts, balancing the salience of item content for early childhood with coherence across the lifespan, ensuring sensitivity across normative and atypical development, and attending to feasibility for clinical and research applications. Data collection to assess validity was reported to be underway for these newly developed early childhood measures. While this initiative represents an exciting step in developing measures of ED in early childhood, the measures were not developed to be used with young children with ASD and therefore their clinical applicability to this population is unclear. Reliable and sensitive measurement of ED during early childhood in both ASD and general population samples would greatly improve the potential for early prevention and intervention efforts during a developmental period of increased brain plasticity (Dawson, 2008).
The Emotion Dysregulation Inventory-Young Child
The present paper describes the development of a new measure for early childhood ED developed to fill these important gaps in measurement (it will be made available for free through the EDI Request Form at www.reaact.pitt.edu). We describe the development and pilot testing of a new “young child” version of the EDI to be completed by caregivers of children with and without ASD between 2 and 5 years of age. The EDI-Young Child (EDI-YC) builds off the success of the original EDI, which was developed to capture a range of cognitive, verbal, and emotional functioning across children with and without ASD and to be change sensitive. We plan for the EDI-YC to be psychometrically linked to the original EDI for use in longitudinal research and in clinical treatment monitoring. We first describe the process by which the EDI was adapted for use with young children with and without ASD using the PROMIS framework, including expert review and cognitive interviews with parents of young children with ASD (Phase 1). We then report on pilot data from an independent sample of parents of children with and without ASD in the youngest age range (24 to 28 months), showing initial evidence of validity and sensitivity for this measure (Phase 2).
Phase 1: Item Pool Development + Refinement
Phase I Methods
The process to develop and finalize the item bank is described in detail below. The initial item pool development and qualitative review spanned 7 months and cognitive interviewing with further revisions spanned an additional 2 months.
Item Pool Development
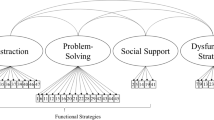
As part of the initial study to develop the EDI for youth ages 6–17.9, a comprehensive literature search was conducted, and a conceptual model was generated (Mazefsky, Day, et al., 2018a). These steps provided the infrastructure for the early childhood adaptation, supplemented by an additional literature search to best understand the key factors of early ED and expert clinical input from the first and senior authors. Candidate items from the original EDI were reviewed, including those that were dropped from the final EDI as some may be more sensitive at younger ages. Additionally, new items were drafted to ensure coverage of the construct in early childhood (Fig. 1).
Response Options
In anticipation of linking the original and young child versions of the EDI to facilitate longitudinal data collection, the instructions remained similar to the original EDI. The structure includes five response options (Not at all, Mild, Moderate, Severe, Very Severe) and a 7-day recall period, as these are optimal guidelines according to the PROMIS® framework (Alwin & Krosnick, 1991; Cella et al., 2010). The response options provide assessment of severity (degree of interference and intensity) and frequency, with a guiding visual response (see Fig. 2). As further detailed below, the instructions were modified based on expert and parental input to provide more clear examples related to this age range.
Qualitative Review
To refine items and support face validity, the initial draft of the EDI-YC was reviewed by experts in early ED in ASD and developmental delays as well as experts outside of ASD. This included personnel from seven academic and hospital sites, including a mixture of clinicians and researchers with various degrees (e.g., psychologists, speech-language pathologists, social workers, early educators).
Cognitive Interviews
Similar to procedures used in the original EDI development and documented in Mazefsky, Day, et al. (2018a), cognitive interviewing methodology was utilized to assess parental comprehension of the measure and to elucidate how parents process the items to make a rating. Five different item orders were created to account for item order effects. Cognitive interviews were conducted with parents (n = 10) of young children with ASD, ages 2–5. All parents completed the cognitive interview process for the full item set (58 items), which exceeds the PROMIS guidelines of a minimum of six interviews per item (Irwin et al., 2009; PROMIS®, 2013).
Parents were asked to read all items of the EDI-YC aloud as well as think aloud as they chose their answers. This allowed the research team to gather information about how parents interpreted the presented content as well as hear their decision-making regarding response options to ensure the questions were capturing a range of ED severity. They were also asked to describe the directions, response options, and items in their own words, which helped the research team to further assess clarity and meaning of the measure as written. Parents were invited to provide general feedback and suggestions. The interviews were conducted by the first author, and she documented parental responses and suggestions throughout the process. Interviews were also audio recorded.
Parents also completed a demographics form and questionnaire data to characterize the sample, including the Social Responsiveness Scale-Second Edition (SRS-2; Preschool or School-Age Form) and Child Behavior Checklist (CBCL). Additionally, parents completed the Wide Range of Achievement Test, Fourth Edition (WRAT-4) Word Reading to assess parental reading level.
Participants
Ten parents of 2- to 5-year-old children with ASD (Mean age = 3.30, SD = 1.16) completed cognitive interviews (Table 1). Parents participating in the cognitive interviews had reading abilities on the Wide Range Achievement Test 4 (WRAT-4) ranging from 6.9 to > 12.9 grade equivalent. Children of participants had a wide range of verbal and intellectual ability and autism symptom severity. Families were recruited through the Florida State University Center for Autism and Related Disabilities (FSU-CARD), a state-funded agency intended to provide information, consultation, technical assistance, and services, or through the Florida State University FIRST WORDS® Project, a prospective longitudinal study focused on screening and early identification of ASD. All children had either a clinical diagnosis of ASD from a provider in the community or were diagnosed with ASD through the context of research via a gold standard evaluation with a clinical best estimate of ASD. Parents were compensated for their time.
Phase I Results
The flow of item generation and refinement is summarized in Fig. 1, including changes made during initial author revisions, expert feedback, and cognitive interviews.
Expert Review
The initial item pool began with the 30 items from the original EDI for ages 6 and above. Based on first and senior author review, an additional 16 items from an early version of the original EDI that were not included in the final EDI were added back to the EDI-YC item bank and 8 new items were drafted to ensure sufficient coverage of how ED manifests in early childhood. Following expert review, 2 items were removed, 6 items were added, and 8 items were reworded. Items were generally removed or added in order to provide greater specificity for use in early childhood. For example, following expert input on the item “cries or stays angry for 5 min or longer,” an additional item was added to attempt to characterize more severe and potentially less normative forms of ED in early childhood: “has tantrums lasting at least 30 min.” Items were typically modified to ensure the target construct was clear. The item bank for the cognitive interview phase included 58 items.
Expert review also suggested a few critical modifications to the instructions. Specific examples relevant to this age range were added to the instructions aimed at helping parents to consider the level of impairment. For example, the following was added to clarify the prompt to consider interference with a child’s daily activities: “e.g., emotions or behaviors make it difficult for child to participate fully in therapies, daycare/preschool, etc.” In addition, expert review suggested that, while parents should rate the frequency and intensity of each item, an instruction should be included about how the dysregulated behaviors may be normative for this age range. The following instruction was added:
Many of the behaviors described on the following pages can be considered age appropriate. Consider how often and how intensely these behaviors occur, not whether the behaviors are commonly seen in young children.
Cognitive Interviews
The overall response to the EDI-YC from parents was very positive. There was uniform enthusiasm for the visual that accompanies the response options. All parents found the directions and items to be generally understandable. Parents noted finding the inclusion of specific examples in the instructions (as described above) particularly helpful and requested additional examples be added. Thus, further age-specific examples were added following the cognitive interviews, such as adding “e.g., parents feel judged by others for the child’s behavior” to the directions and to consider whether the behavior “increases the stress of those around the individual.” Parents expressed feeling confused regarding the qualifications in the instructions that some behaviors may be age appropriate. Subsequently, these statements added following expert review were removed from the directions. Parents generally found the items easy to rate regardless of their child’s verbal ability. Additionally, there was evidence of sensitivity to the range of ED, with variability across items as well as variability across participants. For example, parents endorsed a range of responses across questions rather than selecting the same option across items. With regard to variability between parents, at least three different response options were chosen among parents on 48 of the 58 items (e.g., for “has explosive/out of control outbursts,” 4 parents endorsed Not at All, 3 parents endorsed Mild, 2 parents endorsed Moderate, and 1 parent endorsed Severe), demonstrating preliminary evidence against problems with floor or ceiling effects. For some items, a lack of variability in responses along with parental feedback were helpful in making needed changes to wording. For example, on one item—“destroys property or breaks things when angry or upset”—all parents responded, “not at all.” That item was modified to “breaks or throws things when angry or upset.”
Final Item Bank
After incorporating parental feedback from cognitive interviews, 15 items were dropped due to parental feedback that they were not applicable, 5 items were added to ensure the range of ED was sufficiently covered, and 11 items were reworded (Fig. 1). For example, “has mood swings” was removed after parents repeatedly said that the item was both confusing and not applicable in the context of their child. The final item bank for piloting and psychometric analysis included 48 items. Example items are included in Table 2.
Phase II: Pilot Testing in 2-Year-Olds
Phase II Methods
Participants
Study participants were families from the first author’s dissertation focused on characterizing behavioral and physiological observations of emotional reactivity and regulation in toddlers with and without ASD (n = 37; ages 22–28 months; see Day et al., in press for more details). The participants were originally recruited through the FIRST WORDS® Project, an ongoing, prospective longitudinal study focused on screening and early identification of ASD. Only data of children that were 24 months or older at the time of study visit are included in this paper (n = 31; M = 25.77 months, SD = 1.59). All children had a gold standard evaluation to diagnose or rule out ASD, which included Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) Toddler Module (Luyster et al., 2009), Mullen Scales of Early Learning (MSEL; Mullen, 1995), Vineland Adaptive Behavior Scales, Third Edition (VABS-3; Sparrow et al., 2016), Systematic Observation of Red Flags of ASD (SORF; Dow et al., 2020) based on a home observation, and parent-report questionnaires. Toddlers received a diagnostic determination based on the clinician’s clinical impression and assessment scores; children for whom ASD could not be confirmed or ruled out were excluded from the present study. See Table 3 for sample characteristics. This sample allowed us to explore how the EDI-YC was performing in children with (n = 15) and without (n = 16) ASD at the youngest end of the target age range for the EDI-YC.
Procedures
During the study visit lasting approximately 1–1.5 h, parents were asked to complete a battery of questionnaires, including the pilot version of the EDI-YC (48 items) and the Child Behavior Checklist (CBCL). As part of their participation in the FIRST WORDS® Project, all children also completed a diagnostic evaluation between 18 and 26 months to determine best estimate diagnosis, including the ADOS-2 Toddler Module (Luyster et al., 2009) and MSEL (Mullen, 1995).
Measures
Emotion Dysregulation Inventory-Young Child (EDI-YC). Following phase I, the first and senior author finalized the item bank and created a paper questionnaire for parents to complete. The EDI-YC item bank for pilot testing consisted of 48 items rated on a five-point scale of problem severity over the past 7 days: Not at all = 0, Mild = 1, Moderate = 2, Severe = 3, Very Severe = 4.
Child Behavior Checklist (CBCL). The CBCL is a widely used measure of psychiatric symptoms, with a normed version for ages 1.5–5 (Achenbach & Rescorla, 2001). Items are scored in reference to the past month on a three-point scale (Not at all = 0, Sometimes or Somewhat true = 1, Very true or Often true = 2) and produce scores for numerous specific scales. For the purposes of the present paper, the following scales capturing features related to emotion dysregulation were used: Emotionally Reactive, Anxious/Depressed, Withdrawn, Aggressive Behavior, Internalizing Problems, and Externalizing Problems.
Analyses
Subscale designations for the EDI-YC were based on the two-factor structure of the original EDI, with scales for Reactivity (i.e., rapidly escalating, intense, and labile negative affect characterized by anger and irritability and difficulty downregulating affect) and Dysphoria (i.e., sadness, unease, anhedonia, and low motivation) (Mazefsky, Yu, et al., 2018b). Items from the EDI-YC were summed for each scale, with clinical judgment used to place new items into one of the two subscales. It is important to note that the EDI-YC subscales were not derived from factor analysis and therefore are preliminary. Psychometric analysis will be a part of the next stage of this study.
All analyses were conducted in IBM SPSS Statistics Version 27. One child with ASD had one missing item on the Reactivity scale; the value was imputed based on the mean of the other Reactivity items. Internal validity and item-total statistics were performed to assess reliability. In support of known-groups validity, t-tests were utilized to compare group means (ASD vs. non-ASD) on EDI-YC derived subscales and items. Children with ASD were expected to have higher ED. To examine convergent validity, Pearson correlations were conducted on the EDI-YC derived scales and selected CBCL scales. Positive relationships between these measures were expected.
Phase II Results
EDI-YC Reliability
Reliability and item-total statistics indicated generally acceptable values, with a few exceptions noted below. Internal consistency was high for both the Reactivity (Cronbach’s alpha = 0.98) and Dysphoria scales (Cronbach’s alpha = 0.90).
The corrected item-total correlations were above 0.40 for all of the 36 Reactivity items. The items with the highest item-total correlations were both items from the original final EDI, including: “reactions usually are more severe than the situation calls for” (0.88) and “easily triggered/upset (you have to walk on eggshells)” (0.87). Children with ASD (M = 1.60, SD = 1.24) demonstrated more severe reactions than children without ASD (M = 0.75, SD = 0.68), t (21.46) = − 2.34, p = .03, but were not more easily triggered (ASD: M = 0.87, SD = 1.30; non-ASD: M = 0.38, SD = 0.72), t (19.73) = − 1.33, p = .20. The items with the lowest item-total correlations included: “has repetitive body movements when distressed (e.g., rocking, spinning, pacing)” (0.49) and “cannot calm down without a favorite toy or object (e.g., pacifier, blanket, stuffed animal, fidget or sensory toy)” (0.51). Children with ASD (M = 1.13, SD = 1.41) more frequently demonstrated repetitive body movements than their non-ASD peers (M = 0.19, SD = 0.54), t (17.87) = − 2.44, p = .03. However, the groups did not differ in terms of using a favorite object to regulate (ASD: M = 0.73, SD = 1.03; non-ASD: M = 0.50, SD = 0.82), t (29) = − 0.70, p = .49. The Cronbach’s alpha if item deleted was comparable to the full-scale Cronbach’s alpha (0.98) for all items, indicating that deleting any one item would not substantially impact the internal consistency.
The corrected item-total correlations were above 0.40 for 10 of the 12 Dysphoria items. The items with the highest item-total correlations included: “does not appear to enjoy pleasurable activities (e.g., does not smile, laugh, jump up and down)” (0.77) and “very little makes him/her happy” (0.77). The two items with item-total correlations under 0.4 included: “becomes so nervous that he/she freezes like he/she doesn’t know what to do” (0.31) and “seems sad or unhappy” (0.37). Interestingly, all the items with the highest and lowest item-total correlations were not significantly different between the groups, but it is also important to note the overall incidence rates for these items were low (M = 0.00–0.50, SD = 0.00–1.06). The Cronbach’s alpha if item deleted ranged from 0.88 to 0.90, consistent with the overall Cronbach’s alpha for the Dysphoria scale (0.90).
Descriptives and Group Comparisons
Scores on the EDI-YC Reactivity scale ranged from 5 to 129 (maximum possible score if highest option endorsed on all items is 144), with a mean of 38.71 (SD = 27.46). There was a range of responses reported for all items (i.e., 36 of 36 items had a spread of at least 3 response options selected; e.g., for the item, “appears angry or irritable”, 3 parents endorsed Not at All, 16 parents endorsed Mild, 10 parents endorsed Moderate, 1 parents endorsed Severe, and 1 parent endorsed Very Severe). Reactivity scores were significantly higher in toddlers with ASD (M = 51.93, SD = 30.62, range 12–129) than their non-ASD peers (M = 26.31, SD = 17.14, range 5–74), t (29) = − 2.90, p = .01. This maps onto the typical parental response of “mild” to “moderate” (mean score per item = 1.44) for the ASD group and of “not at all” to “mild” for the non-ASD group (mean score per item = 0.73). Young children with ASD scored significantly higher than children without ASD on 22 of the 36 items, p < .05.
Scores on the preliminary EDI-YC Dysphoria scale ranged from 0 to 28 (maximum score: 48), with a mean of 5.39 (SD = 5.97). Although items on the Dysphoria scale did show significant positive skew (with “not at all” responses being the most common), there was a range of responses reported for all items (i.e., 12 of 12 items had a spread of at least 3 response options selected; e.g., for “shows minimal emotional expression even in situations that are exciting or upsetting”, 22 parents endorsed Not at All, 6 parents endorsed Mild, 2 parent endorsed Moderate, and 1 parent endorsed Severe). Dysphoria scores were significantly higher for the ASD group (M = 8.00, SD = 7.34, range 1–28) than the non-ASD group (M = 2.94, SD = 2.77, range 0–8) on the EDI-YC Dysphoria scale, t (17.68) = − 2.51, p = .02. This score indicates that parents answered, on average, “not at all” to “mild” for both the ASD and non-ASD groups, although parents in the non-ASD group rated “not at all” more frequently than parents in the ASD group (mean score per item for ASD = 0.67, for non-ASD = 0.25). Young children with ASD scored significantly higher than children without ASD on 5 of 12 Dysphoria items.
Convergent Validity
As depicted in Table 4, the EDI-YC Reactivity and Dysphoria subscales were highly related, r (29) = .81, p < .001. Higher scores on the EDI-YC Reactivity and Dysphoria scales corresponded to higher scores on all of the CBCL scales selected a priori. The EDI-YC Reactivity and Dysphoria scales had the strongest relationship with the CBCL Aggressive Behavior scale, r (29) = .80 and r (29) = .68, respectively (p < .001). There was also a strong relationship between EDI-YC Reactivity and CBCL Emotionally Reactive, r(29) = 0.75, p < .001, and EDI-YC Dysphoria with CBCL Internalizing, r(29) = 0.64, p < .001 and with CBCL Withdrawn, r(29) = 0.65, p < .001.
Discussion
The present study aimed to adapt the Emotion Dysregulation Inventory (EDI), originally designed for ages 6–17, for use in young children. The EDI-YC will be suitable for use in children ages 2–5 following psychometric analysis. Although this measure will be appropriate as parent-report for all young children, the EDI-YC will be particularly useful for children with ASD. Existing measures of ED in young children are limited in how they assess the ED construct, and none have been developed and validated in ASD samples (Mazefsky et al., 2021). Moreover, measures developed for older children are not appropriate for use in early childhood given marked differences in parental scaffolding and normative expectations for ED (Kopp, 1989; Thompson & Goodman, 2010). We saw a need for a psychometrically robust measure of ED that can be used in ASD and general population samples and that maximizes change sensitivity in order to characterize the development of ED throughout early childhood.
Similar to the development of the original EDI, we used the PROMIS methodology (Cella et al., 2007, 2010) to ensure that items: (1) covered the full ED range, (2) were developmentally appropriate, and (3) were easily understandable by parents. Items from the original EDI were included in the item bank and others were modified and added based on the clinical expertise and literature review conducted by the first and senior author. Additional input was provided by a panel of experts, including psychologists, speech-language pathologists, social workers, and early educators with specialties in ASD and/or early childhood. Cognitive interviews with parents of 2- to 5-year-olds with ASD were performed and parental feedback was incorporated. Thus, the final item bank incorporated input from stakeholders with different perspectives and was piloted in a small sample of 2-year-old children with and without ASD.
Given the intent to link the young child and school-aged versions of the EDI to measure change in ED over time, the overall approach to the questionnaire remained the same. Likewise, the rating options and time frame did not change, with parents being asked to consider the frequency and severity of behaviors over the last 7 days when selecting among the 5 response options. However, stakeholder input informed modification of the instructions, namely adding more examples to clarify the ways emotional behaviors may cause a problem. For example, one addition included a prompt for parents to consider the extent to which they may make accommodations to avoid behaviors associated with dysregulation. Although experts and parents typically had similar feedback during the development phase of the EDI-YC, they had differing perspectives in one area. Specifically, experts wanted to include a comment on the normative nature of emotion dysregulation in children ages 2–5, but ultimately parents of young children with ASD found that caveat more confusing than helpful. Subsequently, the prompt was removed.
During phase 1 of this study, modifications were also made to specific items. The item bank started with 54 items, 46 of which were from the original EDI item bank with an additional 8 items added. Then throughout the process of expert review and cognitive interviews, 17 items were dropped, 11 items were added, and 19 items were modified. The changes from the EDI to EDI-YC were primarily focused on ensuring items were developmentally appropriate and sensitive to presentations of ED that are more common in early childhood and/or in young children with ASD. This included increasing duration of dysregulation episodes (e.g., 30 min instead of 5 min) and incorporating situations related to transitions and communication difficulties. Stakeholder input, particularly from parents of young children with ASD, was an essential step to ensure the construct was being accurately tapped and that the items were suited to capture a wide range of emotion dysregulation.
Results from phase 2, which included piloting the item bank in the youngest end of the age range (24–28 months), further supported that the EDI-YC is sensitive to capturing heterogeneity in ED. Scores ranged from 5 to 129 (maximum possible = 144) on the derived Reactivity subscale and from 0 to 28 (maximum possible = 48) on the derived Dysphoria subscale. Phase 2 of this study also provides promising evidence for the EDI-YC as a reliable measure with convergent validity. It is important to note that the subscales (Reactivity, Dysphoria) utilized in this study were derived based on the original EDI and do not necessarily represent the most optimal factors in this age range; future psychometric analysis will be conducted to more empirically determine how items hang together. Moreover, results regarding preliminary statistics should be interpreted with caution given the small sample size as well as the demographic distribution. Samples in both phases were predominantly male (for the ASD subgroups only, consistent with the sex distribution in ASD) and White. The psychometric sample (to be published) was collected from a national, online sample and is more representative of the demographic distributions of the US. Further, all items will be carefully assessed for psychometric biases based on demographic factors via differential item functioning in future work.
Young children with ASD had greater Reactivity scores than young children without ASD, and also demonstrated significantly higher scores on the majority of the individual Reactivity items. Moreover, 2-year-olds with elevated Reactivity scores demonstrated higher scores on all selected CBCL subscales, including emotional reactivity, providing evidence of convergent validity. The reliability for this scale was excellent and the items with the highest item-total correlations mapped onto the final items (after psychometric analysis) of the original EDI, with “reactions usually are more severe than the situation calls for” being one of the best performing items for the original EDI. That item also significantly differentiated young children with and without ASD. These findings demonstrate a robust pattern of atypical reactivity for ASD that is present by 2 years of age and is sufficiently captured on the EDI-YC. This is consistent with literature indicating that youth with ASD demonstrate more severe ED than youth without ASD (Conner et al., 2021; Konstantareas & Stewart, 2006; Mazefsky et al., 2018b, 2020; Samson et al., 2014) as well as the few studies documenting atypical ED among young children with ASD (Macari et al., 2018; Nuske et al., 2017; Day et al., in press).
The results regarding Dysphoria were promising, with high internal consistency and preliminary psychometrics that mirror patterns in the original EDI. The items that most related to the Dysphoria total score focused on difficulty with the upregulation of positive emotion, such as “very little makes him/her happy” and “does not enjoy pleasurable activities (e.g., does not smile, laugh, jump up and down)”. The items with the lowest item-total correlations were related to anxiety and sadness. In general, parents of toddlers with ASD rated their children higher on Dysphoria than parents of toddlers without ASD and higher scores on the Dysphoria scale were related to higher scores on the CBCL, including internalizing problems. This provides preliminary evidence of early emerging patterns related to blunted emotional reactivity and/or timid tendencies for some young children with ASD.
The original EDI Dysphoria scale was designed to reflect sadness, unease, anhedonia, and low motivation, which often relate to anxiety and depression in older samples (Mazefsky, Yu, et al., 2018b, Mazefsky et al., 2020). Behaviors associated with dysphoria, including symptoms of anxiety and depression, are relatively uncommon in young children (Whalen et al., 2017). Although parents gave a range of responses to all questions, overall endorsement of items on the Dysphoria scale was low, with “not at all” being the most common response. Subsequently, this led to less variability at the item level and a potentially less robust range of measurement at low levels of Dysphoria. This maps onto the pattern found in the original EDI—the average Dysphoria score was low in youth with ASD and there was somewhat restricted variability at the lower end of the measurement range; yet there was a subset of children with ASD that had high Dysphoria scores, which is a clinically relevant and reliable aspect of ED (Mazefsky, Yu, et al., 2018b). Further psychometric analysis in large samples of young children with and without ASD across the full age range (2–5 years) will help determine whether the Dysphoria subscale is an appropriate measure of emotion dysregulation in early childhood.
Several other steps consistent with the PROMIS® framework (Cella et al., 2007, 2010) are underway. Data have been collected from 1370 parents of 2- to 5-year-olds with ASD and other developmental disorders as part of an NIH-funded study (R01HD079512; PI: Mazefsky); preliminary analysis of these data are underway. The sample is heterogeneous in terms of race, ethnicity, sex, and SES. Inclusion of other developmental disorders in this clinical sample will support the utility of the EDI-YC beyond ASD, which will allow for monitoring and screening in early intervention programs. Future work will analyze the factor structure, identify the best items through item-response theory, assess reliability and validity, and develop a short-form for efficient measurement of ED. Goals of psychometric analysis of the EDI-YC include ensuring it is sensitive to change and also to link it to the school-aged EDI, making it an ideal tool to assess the longitudinal development of ED. Moreover, data have been collected from 769 parents of 2- to 5-year-old children with normative development. Our methodological approach will help identify the items that are most sensitive to deviations from typical emotion development so that parents do not have to consider this when making their ratings. In addition, this will support the development of cut-off scores for screening.
In sum, the aims of the present study—to modify the EDI for use in children ages 2–5 and pilot the EDI-YC item bank—were accomplished. Similar to Blackwell and colleagues (2020), we found that an existing measure (EDI) can be adapted for use in young children by modifying to ensure developmental appropriateness. The advantages of the EDI-YC over existing measures include that it was developed to assess ED exclusively, it focuses on observable manifestations of ED, and it guides the parent to focus on both frequency and intensity (Mazefsky et al., 2021). Moreover, the EDI-YC was designed with input from experts and parents of young children with ASD. The data in phase II of this study were included to illuminate the potential for this measure as a means of characterizing ED in young children and should be interpreted as preliminary but provide initial support for the EDI-YC as a valid and reliable measure.
References
Achenbach, T., & Rescorla, L. (2000). Manual for the ASEBA preschool forms & profiles. University of Vermont, Research Center for Children, Youth, and Families.
Adrien, J. L., Lenoir, P., Martineau, J., Perrot, A., Hameury, L., Larmande, C., & Sauvage, D. (1993). Blind ratings of early symptoms of autism based upon family home movies. Journal of the American Academy of Child & Adolescent Psychiatry, 32(3), 617–626.
Alwin, D. F., & Krosnick, J. (1991). The reliability of survey attitude measurement: The influence of question and respondent attributes. Sociological Methods & Research, 20(1), 139–181. https://doi.org/10.1177/0049124191020001005
Berkovits, L., Eisenhower, A., & Blacher, J. (2016). Emotion regulation in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-016-2922-2
Blackwell, C. K., Wakschlag, L., Krogh-Jespersen, S., Buss, K. A., Luby, J., Bevans, K., Lai, J. S., Forrest, C. B., & Cella, D. (2020). Pragmatic health assessment in early childhood: The PROMIS® of developmentally based measurement for pediatric psychology. Journal of Pediatric Psychology, 45(3), 311–318. https://doi.org/10.1093/jpepsy/jsz094
Blair, B. L., Perry, N. B., O'Brien, M., Calkins, S. D., Keane, S. P., & Shanahan, L. (2015). Identifying developmental cascades among differentiated dimensions of social competence and emotion regulation. Developmental Psychology, 51(8), 1062–1073. https://doi.org/10.1037/a0039472
Cella, D., Riley, W., Stone, A., Rothrock, N., Reeve, B., Yount, S., Amtmann, D., Bode, R., Buysse, D., Choi, S., Cook, K., DeVellis, R., DeWalt, D., Fries, J. F., Gershon, R., Hahn, E. A., Lai, J.-S., Pilkonis, P., Revicki, D., & Hays, R. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. https://doi.org/10.1016/j.jclinepi.2010.04.011
Cella, D., Yount, S., Rothrock, N., Gershon, R., Cook, K., Reeve, B., Ader, D., Fries, J. F., Bruce, B., & Rose, M. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH roadmap cooperative group during its first two years. Medical Care, 45(5 Suppl 1), 3. https://doi.org/10.1097/01.MLR.0000258615.42478.55
Cibralic, S., Kohlhoff, J., Wallace, N., McMahon, C., & Eapen, V. (2019). A systematic review of emotion regulation in children with Autism Spectrum Disorder. Research in Autism Spectrum Disorders, 68, 101422. https://doi.org/10.1016/j.rasd.2019.101422
Clifford, S. M., Hudry, K., Elsabbagh, M., Charman, T., & Johnson, M. H. (2013). Temperament in the first 2 years of life in infants at high-risk for autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(3), 673–686.
Cole, P. M., Michel, M. K., & O’Donnell Teti, L. (1994). The development of emotion regulation and dysregulation: A clinical perspective. Monographs of the Society for Research in Child Development, 59(2/3), 73–100.
Conner, C. M., Golt, J., Shaffer, R., Righi, G., Siegel, M., & Mazefsky, C. A. (2021). Emotion dysregulation is substantially elevated in autism compared to the general population: Impact on psychiatric services. Autism Research, 14, 169–181. https://doi.org/10.1002/aur.2450
Croen, L. A., Najjar, D. V., Ray, G. T., Lotspeich, L., & Bernal, P. (2006). A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics, 118(4), e1203–e1211.
Day, T. N., Mazefsky, C. A., & Wetherby, A. M. (in press). Characterizing difficulties with emotion regulation in toddlers with autism spectrum disorder. Research in Autism Spectrum Disorders.
Dawson, G. (2008). Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology, 20, 775–803. https://doi.org/10.1017/S0954579408000370
Dow, D., Day, T. N., Kutta, T. J., Nottke, C., & Wetherby, A. M. (2020). Screening for autism spectrum disorder in a naturalistic home setting using the systematic observation of red flags (SORF) at 18–24 months. Autism Research, 13(1), 122–133. https://doi.org/10.1002/aur.2226
Garon, N., Zwaigenbaum, L., Bryson, S., Smith, I. M., Brian, J., Roncadin, C., Vaillancourt, T., Armstrong, V., Sacrey, L.-A.R., & Roberts, W. (2016). Temperament and its association with autism symptoms in a high-risk population. Journal of Abnormal Child Psychology, 44(4), 757–769. https://doi.org/10.1007/s10802-015-0064-1
Goldsmith, H. H. (1996). Studying temperament via construction of the toddler behavior assessment questionnaire. Child Development, 67(1), 218–235. https://doi.org/10.1111/j.1467-8624.1996.tb01730.x
Herring, S., Gray, K., Taffe, J., Tonge, B., Sweeney, D., & Einfeld, S. (2006). Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: Associations with parental mental health and family functioning. Journal of Intellectual Disability Research, 50(12), 874–882.
Hofstra, M. B., Van Der Ende, J. A. N., & Verhulst, F. C. (2002). Child and adolescent problems predict DSM-IV disorders in adulthood: A 14-year follow-up of a Dutch epidemiological sample. Journal of the American Academy of Child & Adolescent Psychiatry, 41(2), 182–189.
Irwin, D. E., Varni, J. W., Yeatts, K., & DeWalt, D. A. (2009). Cognitive interviewing methodology in the development of a pediatric item bank: A patient reported outcomes measurement information system (PROMIS) study. Health and Quality of Life Outcomes, 7(1), 1–10. https://doi.org/10.1186/1477-7525-7-3/TABLES/5
Jahromi, L. B., Meek, S. E., & Ober‐Reynolds, S. (2012). Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. Journal of Child Psychology and Psychiatry, 53(12), 1250–1258.
Kim-Cohen, J., Caspi, A., Moffitt, T. E., Harrington, H., Milne, B. J., & Poulton, R. (2003). Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry, 60(7), 709–717. https://doi.org/10.1001/archpsyc.60.7.709
Kasari, C., Gulsrud, A. C., Wong, C., Kwon, S., & Locke, J. (2010). Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. Journal of Autism and Developmental Disorders, 40(9), 1045–1056.
Konstantareas, M. M., & Stewart, K. (2006). Affect regulation and temperament in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 36(2), 143–154. https://doi.org/10.1007/s10803-005-0051-4
Kopp, C. B. (1989). Regulation of distress and negative emotions: A developmental view. Developmental Psychology, 25(3), 343–354. https://doi.org/10.1037/0012-1649.25.3.343
Luyster, R., Gotham, K., Guthrie, W., Coffing, M., Petrak, R., Pierce, K., Bishop, S., Esler, A., Hus, V., Oti, R., Richler, J., Risi, S., & Lord, C. (2009). The autism diagnostic observation schedule—Toddler Module : A new module of a standardized diagnostic measure for Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 39, 1305–1320. https://doi.org/10.1007/s10803-009-0746-z
Macari, S. L., DiNicola, L., Kane-Grade, F., Prince, E., Vernetti, A., Powell, K., Fontenelle, S., & Chawarska, K. (2018). Emotional expressivity in toddlers with Autism Spectrum Disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 57(11), 828–836. https://doi.org/10.1016/j.jaac.2018.07.872
Macari, S. L., Koller, J., Campbell, D. J., & Chawarska, K. (2017). Temperamental markers in toddlers with autism spectrum disorder. Journal of Child Psychology and Psychiatry and Allied Disciplines, 58(7), 819–828. https://doi.org/10.1111/jcpp.12710
Madden, J. M., Lakoma, M. D., Lynch, F. L., Rusinak, D., Owen-Smith, A. A., Coleman, K. J., Quinn, V. P., Yau, V. M., Qian, Y. X., & Croen, L. A. (2017). Psychotropic medication use among insured children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(1), 144–154.
Mazefsky, C. A., Borue, X., Day, T. N., & Minshew, N. J. (2014). Emotion regulation patterns in adolescents with high-functioning autism spectrum disorder: Comparison to typically developing adolescents and association with psychiatric symptoms. Autism Research, 7(3), 344–354. https://doi.org/10.1002/aur.1366
Mazefsky, C. A., Conner, C. M., Breitenfeldt, K., Leezenbaum, N., Chen, Q., Bylsma, L. M., & Pilkonis, P. (2021). Evidence base update for questionnaires of emotion regulation and reactivity for children and adolescents. Journal of Clinical Child & Adolescent Psychology, 50(6), 683–707. https://doi.org/10.1080/15374416.2021.1955372
Mazefsky, C. A., Day, T. N., Siegel, M., White, S. W., Yu, L., & Pilkonis, P. A. (2018a). Development of the emotion dysregulation inventory: A PROMIS®ing method for creating sensitive and unbiased questionnaires for Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 48(11), 3736–3746. https://doi.org/10.1007/s10803-016-2907-1
Mazefsky, C. A., Yu, L., White, S. W., Siegel, M., & Pilkonis, P. A. (2018b). The emotion dysregulation inventory: Psychometric properties and item response theory calibration in an autism spectrum disorder sample. Autism Research, 11(6), 928–941. https://doi.org/10.1002/aur.1947
Mazefsky, C. A., Yu, L., & Pilkonis, P. A. (2020). Psychometric properties of the emotion dysregulation inventory in a nationally representative sample of youth. Journal of Clinical Child & Adolescent Psychology. https://doi.org/10.1080/15374416.2019.1703710
Mullen, E. (1995). Mullen scales of early learning. American Guidance Service.
Nuske, H. J., Hedley, D., Tseng, C. H., Begeer, S., & Dissanayake, C. (2018). Emotion regulation strategies in preschoolers with autism: Associations with parent quality of life and family functioning. Journal of Autism and Developmental Disorders, 48(4), 1287–1300.
Nuske, H. J., Hedley, D., Woollacott, A., Thomson, P., Macari, S. L., & Dissanayake, C. (2017). Developmental delays in emotion regulation strategies in preschoolers with autism. Autism Research, 10(11), 1808–1822. https://doi.org/10.1002/aur.1827
Pilkonis, P. A., Choi, S. W., Reise, S. P., Stover, A. M., Riley, W. T., & Cella, D. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. https://doi.org/10.1177/1073191111411667
PROMIS® Validity Standards Committee on behalf of the PROMIS® Network. (2013). PROMIS® Instrument Development and Validation Scientific Standards, Version 2.0, (revised May 2013). http://www.nihpromis.org/science/methodology?AspxAutoDetectCookieSupport=1.
Rescorla, L. A., Winder-Patel, B. M., Paterson, S. J., Pandey, J., Wolff, J. J., Schultz, R. T., & Piven, J. (2017). Autism spectrum disorder screening with the CBCL/1½–5: Findings for young children at high risk for autism spectrum disorder. Autism. https://doi.org/10.1177/1362361317718482
Rieffe, C., Oosterveld, P., Terwogt, M. M., Mootz, S., van Leeuwen, E., & Stockmann, L. (2011). Emotion regulation and internalizing symptoms in children with autism spectrum disorders. Autism, 15(6), 655–670. https://doi.org/10.1177/1362361310366571
Samson, A. C., Hardan, A. Y., Lee, I. A., Phillips, J. M., & Gross, J. J. (2015). Maladaptive behavior in autism spectrum disorder: The role of emotion experience and emotion regulation. Journal of Autism and Developmental Disorders, 45(11), 3424–3432. https://doi.org/10.1007/s10803-015-2388-7
Samson, A. C., Phillips, J. M., Parker, K. J., Shah, S., Gross, J. J., & Hardan, A. Y. (2014). Emotion dysregulation and the core features of autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(7), 1766–1772. https://doi.org/10.1007/s10803-013-2022-5
Scarpa, A., & Reyes, N. M. (2011). Improving emotion regulation with CBT in young children with high functioning autism spectrum disorders: A pilot study. Behavioral and Cognitive Psychotherapy, 39(4), 495–500.
Soke, G. N., Maenner, M. J., Christensen, D., Kurzius-Spencer, M., & Schieve, L. (2018). Prevalence of co-occurring medical and behavioral conditions/symptoms among 4-and 8-year-old children with autism spectrum disorder in selected areas of the United States in 2010. Journal of Autism and Developmental Disorders, 48(8), 2663–2676.
Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2016). Vineland adaptive behavior scales (3rd ed.). Psychological Corporation.
Thompson, R. A., & Goodman, M. (2010). Development of emotion regulation: More than meets the eye. In Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment (pp. 38–58). The Guilford Press.
Weiss, J. A., Riosa, P. B., Mazefsky, C. A., & Beaumont, R. (2017). Emotion regulation in autism spectrum disorder in emotion regulation and psychopathology in children and adolescents (pp. 235–258).
Werner, E., Dawson, G., Osterling, J., & Dinno, N. (2000). Brief report: Recognition of autism spectrum disorder before one year of age: A retrospective study based on home videotapes. Journal of Autism and Developmental Disorders, 30(2), 157.
Whalen, D. J., Sylvester, C. M., & Luby, J. L. (2017). Depression and anxiety in preschoolers: A review of the past 7 years. In Child and Adolescent Psychiatric Clinics of North America (Vol. 26, Issue 3, pp. 503–522). https://doi.org/10.1016/j.chc.2017.02.006
Acknowledgments
This study included a subsample of children from the first author’s dissertation; the project was executed as a side project in collaboration with the senior author. Support for the present study included an internal award from Florida State University (awarded to Taylor N. Day), Eunice Kennedy Shriver National Institute of Child Health & Human Development under Award Number R01HD078410 (PI: Amy M. Wetherby), and Eunice Kennedy Shriver National Institute of Child Health & Human Development under Award Number R01HD079512 (PI: Carla A. Mazefsky). Special acknowledgement belongs to Dr. Wetherby, the first author’s graduate school mentor, as well as Dr. Lan Yu and Dr. Paul Pilkonis who contributed to the development of this measure. An additional thanks to the participating families and staff at FIRST WORDS® Project. During the preparation of this manuscript, Dr. Day was supported by National Institute of Mental Health under Award Number T32MH016804 and Dr. Northrup was supported by National Center for Advancing Translational Sciences under Award Number KL2TR001856.
Author information
Authors and Affiliations
Contributions
Dr. TND and Dr. CAM co-led the development of the EDI-YC as well as made decisions regarding the modification of the item bank. Dr. TND was responsible for data collection. All authors (TND, JBN, CAM) contributed to the data analysis and the preparation and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed involving human participants were in accordance with the ethical standards of the Florida State University Institutional Review Board (IRB) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for Publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Day, T.N., Northrup, J.B. & Mazefsky, C.A. A PROMIS®ing New Measure for Quantifying Emotion Dysregulation in Toddlers and Preschoolers: Development of the Emotion Dysregulation Inventory-Young Child. J Autism Dev Disord 53, 2261–2273 (2023). https://doi.org/10.1007/s10803-022-05536-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05536-9