Abstract
The present study aimed to explore clinical trends in the period 2000–2010, along with discriminating clinical factors for autism spectrum disorder (ASD), in young children suspected of ASD. The following trends were observed: (1) a rise in referrals including an increase in referrals among language-abled children, (2) an increase in children assigned an ASD diagnosis after assessment, and (3) a decrease in Autism Diagnostic Observation Schedule total score. The distribution of ASD subtypes and IQ level did not change. Results suggest that a higher proportion of children with less severe autism symptoms were referred and diagnosed. Further, restricted and repetitive behaviors seemed to be a key discriminating factor when distinguishing between ASD and no-ASD children with a discordant symptom profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism spectrum disorder (ASD) has during recent decades changed from a narrowly defined and rare disorder to a rather common and heterogeneous condition with a wide spectrum of severity (American Psychiatric Association 2013; Lord et al. 2018; World Health Organisation 1992). A steep rise in the prevalence, now estimated to be 1.46–1.68% among school-aged children in developed countries, has been seen (Baio et al. 2018; Jensen et al. 2014; Lord et al. 2018) along with a cumulative incidence of 2.47–2.68% in adolescents, although with diverging results relative to whether the cumulative incidence has plateaued (Schendel and Thorsteinsson 2018; Xu et al. 2018). Interestingly, although there has been an increase in ASD prevalence findings suggest that the clinical phenotype of diagnosed cases may not have changed. Two studies investigating this question in Sweden and the USA found that the prevalence of the overall autism symptom phenotype of diagnosed cases remained stable during the last decades, while the prevalence for clinically diagnosed ASD increased substantially (Lundstrom et al. 2015; Myers et al. 2019). However, studies are few, and it remains an important question whether the diagnostic and clinical features of children referred for an autism assessment has changed.
An ASD diagnosis is ideally based on input from multiple sources (Falkmer et al. 2013), including standard diagnostic instruments such as the Autism Diagnostic Observation Schedule (ADOS) (Lord et al. 2000). A final ASD diagnosis is challenged by the phenotypic complexity and presentation of ASD, especially at very young ages and in the milder variants of the spectrum (Carlsson et al. 2013; Constantino 2011; Wiggins et al. 2015). Given that ASD symptoms lie on a continuum, the necessary diagnostic dichotomy—ASD Yes/No—means that some children whose diagnostic profile is less clear may be misclassified (Wiggins et al. 2019). Besides the phenotypic complexity of ASD and the dimensional symptomatology, diagnostic decisions are also challenged by the overlap of core features of ASD and other co-occurring neurodevelopmental and psychiatric conditions (Close et al. 2012; Levy and Perry 2011; Wiggins et al. 2015). For instance, preschool and school-aged children with ASD may also have symptoms of attention deficit hyperactivity disorder (ADHD), intellectual disability (ID) and specific language disorder, which may impede an unambiguous ASD diagnosis until later developmental stages (Carlsson et al. 2013; Close et al. 2012; Salazar et al. 2015; Simonoff et al. 2013; Wiggins et al. 2015), and consequently missed opportunities for early intervention and improved outcomes (Carlsson et al. 2013; Helt et al. 2008; Nassar et al. 2009).
To address these diagnostic challenges, it may be informative to identify the most discriminating factors when assigning a final ASD diagnosis, especially in children with a discordant symptom profile. Focusing on ASD diagnostics in a context of children with a range of developmental and other child psychiatric conditions that often co-occur with ASD may provide valuable information about factors that could be important when distinguishing between ASD and no-ASD. This knowledge may potentially lead to earlier and more accurate clinical diagnoses, and thus the possibility of more effective and targeted treatments, at younger ages.
In the present explorative study, a well-characterized, population-based, 10-year clinical cohort of young children was used to answer the following questions: 1) has there been a change in diagnostic practice and clinical characteristics of children referred for an autism diagnostic assessment across calendar years and 2) which autistic features of ADOS seem to best discriminate between ASD cases and no-ASD cases in children with a discordant symptom profile?
Methods
Using a population-based clinical cohort, this retrospective cross-sectional explorative study was conducted at Aarhus University Hospital, Psychiatry (AUHP), Denmark, and registered at the Regional Data Protection Agency, Aarhus. The study was approved by the Danish Patient Safety Authority, and thereby exempt from obtaining informed consent by Danish law.
The clinical cohort encompassed all consecutive referrals of children referred specifically due to suspicion of ASD and who underwent a diagnostic developmental assessment between January 1, 2000 and December 31, 2010 at AUHP, Department of Child- and Adolescent Psychiatry (the ASD clinic). The ASD clinic was responsible for all assessments of children referred with suspicion of ASD before the age of 7 and residing in the county of Aarhus (catchment area 845,000 citizens) during the study period. In Denmark all citizens have free and equal access to medical services in the public health care system and during the study period there were very few private services. Children eligible for the study were born between January 1, 1993 and December 31, 2006, and enrolled if they were referred to the ASD clinic during the period of inclusion before the age of 7. Due to waiting time, some of the children had become older than 7 years at the time they were evaluated. On the purpose of aim 2 only children with ADOS were included. A total of 939 index children were initially identified as eligible for this study, however, 46 of the children could not be included in the study due to missing data prior to the assessment in the ASD clinic (emigration (n = 13), assessment at a private hospital instead (n = 3), and parent refusal to participate in the ASD clinic assessment (n = 20)), or missing medical records (n = 10).
ASD-Clinic Procedures and Diagnoses
All children were referred by a specialist (the primary psychologist assigned to the institutions or schools, general medical practitioners, or pediatricians) to the ASD clinic based on concerns from parents and/or professionals. The referral papers contained descriptions of the child's development, autism symptoms, and effect of interventions performed before referral. A triage of the referral paper at the ASD clinic resulted in an invitation to an assessment if the suspicion of ASD was maintained. The assessment was conducted by a multidisciplinary team comprised of trained pedagogues, nurses, developmental psychologists and led by a Specialist Consultant in Child- and Adolescent Psychiatry. Other specialists participated in the process as needed, e.g. a speech therapist. The assessment included a comprehensive developmental evaluation including a test for cognitive ability, physical and neurological examination, interview with the parents and institutional staff, observation of the child in the child's natural home or institutional environment, and, usually, the Danish version of the ADOS (Lord et al. 2000). The decision on whether to include ADOS or not was made by the clinicians in a team conference, and when used, ADOS was normally the first assessment in the clinic aiming to make the assessment as free from bias as possible. The ADOS was administered by experienced certified psychologists. In the first years of the study period an assessment may not include ADOS if the symptoms described in the referral papers or the first impression of the child in the ASD-clinic clearly indicated another developmental disorder as the primary cause of the symptoms. In the last years of the study period, however, ADOS was used more systematically regardless of symptom descriptions in the referral paper or the first impression of the child. However, throughout the period case-specific circumstances could result in the omission of ADOS (e.g., because parents /caregivers were unable to come to the ASD-clinic and the home environment prevented a systematic ADOS assessment). Final diagnoses were team consensus decisions based on the total clinical evaluation of all assessments by the multidisciplinary team. Diagnoses were reported using the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) (World Health Organisation 1992) and diagnostic codes were recorded as either primary (the disorder that seemed to be the most challenging for the child), or secondary (one or more developmental or psychiatric disorders important for the understanding of the child). For this study, the number of diagnoses applied per child were classified in two categories; either “no comorbidity” (1 primary diagnosis), or “1 or more comorbid disorders” (1 primary diagnosis + 1 or more secondary diagnoses). In case of an ASD diagnosis, ASD was always reported as primary, and the specific subtype of ASD was determined using the ICD-10 diagnostic codes childhood autism (F84.0), atypical autism (F84.1), Asperger syndrome (F84.5) and pervasive developmental disorder-not otherwise specified, PDD-NOS (F84.8).
Data Collection and Study Measures
Data were extracted from medical records, and data on clinical characteristics included age at first assessment in the ASD clinic (used in the study as the proxy for “age at diagnosis”), gender, all assigned diagnoses, and cognitive test results.
Data on autistic features were extracted from the ADOS, which is a semi-structured standardized assessment of ASD symptoms. The instrument allows for direct observation of the behavior and thus objective information related to ASD diagnostic criteria. The standard ADOS algorithm yields domain scores for reciprocal social interaction, social communication, play and imaginative use of materials, and restricted, repetitive behaviors and interests (RRBs), along with a total score with empirically derived cut-offs for three classifications, i.e. autism, autism spectrum and non-spectrum. Based on the ADOS total score, a dichotomous classification of ASD according to the ADOS cut-off (autism + autism spectrum = "above cut-off") versus no-ASD (non-spectrum = "below cut-off") was used. Items on the ADOS are scored on a 0–3-point scale, with a higher score reflecting greater severity and/or frequency of impairment, and the cut-off limits are dependent on module number (Lord et al. 2000).Variables used to explore distinguishing autistic features in children with discordant symptom profiles, were items identical in ADOS modules 1, 2 and 3 along with four items previously found to be discriminative between ASD and ADHD (i.e. quality of social overtures, unusual eye contact, facial expression directed to examiner and amount of reciprocal social communication) (Grzadzinski et al. 2016). The reason for choosing these four items was the assumption that a high percentage of children without an ASD diagnosis were diagnosed with ADHD and that these items may also distinguish between ASD and other developmental disorders. Since the assessing clinician's choice of appropriate ADOS module to administer was dependent on the child's expressive language level, the ADOS module number was used as a proxy for language ability. Specifically, Module 1 is used in children with no- or only single words, Module 2 in children who speaks in phrases, and Module 3 in children with fluent speech.
Children were examined with one or more cognitive tests matching their age, developmental level and verbal fluency. Instruments included the Mullen Scales of Early Learning (Mullen 1995), Snijders-Oomen Non-verbal Intelligence Test (Snijders et al. 1997), the Wechsler Preschool and Primary Scale of Intelligence (Wechsler 1989, 2002) or the Wechsler Intelligence Scale for Children (Wechsler 1991). Depending on the child's age and language level, a developmental quotient (and a corresponding calculated IQ), a non-verbal IQ, or a total IQ was used as estimates of cognitive functioning at time of diagnosis. IQ was categorized according to ICD-10 criteria: normal cognitive ability (IQ above 85), developmental delay (IQ 70–85) (R41.8), mild intellectual disability (IQ 50–69) (F71, F78 and F79), and moderate to severe intellectual disability (IQ < 50) (F72 and F73). The children were considered to have an ID if they had an IQ score of < 70. In case of conflicting or partly missing cognitive information in the medical records (n = 201), a specialized psychologist reviewed the cognitive test results and decided on the cognitive level. Four children had missing data on cognitive level.
Study Groups
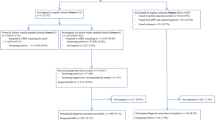
As shown in Fig. 1, the study cohort was divided into groups based on the clinical decision of an ASD diagnosis (ASD versus no-ASD), and the use of ADOS (ADOS versus no-ADOS) (Fig. 1). Children with an ADOS in the assessment were additionally classified into four subgroups based on first the ADOS total score (above versus below ADOS cut-off for autism spectrum) and then the final clinical ASD diagnostic decision (ASD versus no-ASD). These subgroups were designed to extract the children with a discordant symptom profile, i.e. being above ADOS cut-off for autism spectrum but not assigned a clinical ASD diagnosis (“above/no-ASD”) or being below ADOS cut-off for autism spectrum but assigned a clinical ASD diagnosis (“below/ASD”). The discordant groups were compared to the corresponding concordant subgroups, i.e. above ADOS cut-off and assigned an ASD diagnosis (“above/ASD”) or below ADOS cut-off and not assigned an ASD diagnosis (“below/no-ASD”). By comparing features of the discordant versus concordant cases in above and below ADOS cut-off groups, respectively, the study aimed to examine the potential for discrimination on the ADOS score between ASD and no-ASD cases and thereby identify the most discriminating features more likely characterizing young children with a discordant ASD symptom profile.
Flow diagram of the study cohort and subgroups. Study cohort = children referred on suspicion of autism spectrum disorder (ASD); no-ASD = no diagnosis of autism spectrum disorder; ADOS = Autism Diagnostic Observation Schedule; Above cut-off = above cut-off on ADOS algorithm classification (autism spectrum); Below cut-off = below cut-off on ADOS algorithm classification score (non-spectrum)
Analyses
First, identification of the number and proportion of participants who met the criteria for an ASD diagnosis, who were assessed with ADOS and, of the latter, who fulfilled the criteria for the ADOS autism spectrum classification and who did not was carried out (overall, and in both the above or below ADOS cut-off subgroups). Comparisons of characteristics of the groups ASD versus no-ASD, and ADOS versus no-ADOS were made using Student's t-test and chi-square test. To estimate the association between clinical characteristics, ADOS features, and distribution of discordant cases (dependent variables) and year of assessment (independent variable), univariate linear regression and simple logistic regression models were used. Discordant and concordant subgroups (“above/no-ASD” versus “above/ASD” and “below/ASD” versus “below/no-ASD”) were compared using Student's t-test or chi-square test. Between-group comparisons, stratified on above and below ADOS cut-off subgroups, with discordant cases as the dependent variable and clinical characteristics as independent variables, were performed using simple and ordinal logistic regression analyses, followed by multiple regression analyses adjusting for age at diagnosis, gender and year of referral. Autistic features measured by ADOS in discordant versus concordant subgroups were analyzed the same way.
Model assumptions for linear regression analyses were checked visually, and for logistic regression analyses the Hosmer–Lemeshow Goodness of fit test was applied as well. For ordered logistic regression models the proportional-odds assumption was tested using a likelihood-ratio test and Brant test. All statistical analyses were conducted with STATA version 15.2.
Results
Characteristics of Participants
The final study cohort comprised 893 children of whom 547 (61%) received a diagnosis of ASD. The mean age at assessment in the ASD-clinic was 5.3 years (range 1.1–8.7 years), 78.2% were ≥ 4 years, and the cohort included 703 males (78.7%) and 190 (21.3%) females. A total of 701 children were examined with ADOS (92.1% of children with ASD and 55.2% of children with no-ASD), of whom six had missing data on ADOS scores and were excluded from the ADOS sub-analyses (n = 695) (Fig. 1). Characteristics of the total study cohort, children with ASD and no-ASD, and with ADOS and no-ADOS included in the assessment are presented in Table 1.
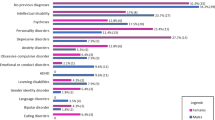
As regards the children who did not receive a diagnosis of ASD (no-ASD), all were assigned at least one non-ASD diagnosis, and the most frequent diagnoses were as follows: ADHD (66.2% percent of ADHD as primary or secondary diagnosis (combined percent)), ID (34.1% (combined percent)), mixed developmental disorder (30.7% (combined percent)) and specific language disorder (25.5% (combined percent)), with most children having more than one diagnosis.
Time Trends in Clinical Characteristics and Autistic Features
Time trends in clinical characteristics are shown in Figs. 2 and 3 (and Figs. 5 and 6 in the supplemental material). Table 2 displays the relationship between year of assessment and clinical characteristics.
The number of assigned ASD diagnoses as well as the proportion of evaluated children assigned an ASD diagnosis increased remarkably up to 2005 followed by a fairly stable proportion of 65–75% from 2005 to 2010 (Fig. 2). At the same time, the odds of a referred child being a boy or of having an IQ ≥ 70 did not change across calendar years. However, the odds of receiving ≥ 1 comorbid disorder increased (Table 2, Fig. 5_supplement).
The odds of ADOS being included in the clinical assessment increased markedly with calendar time, but there were no changes in the odds of receiving an ASD diagnosis among children who were tested with ADOS, or to be above cut-off on ADOS. Similarly, there were no notable changes across time in the odds of being a discordant case in both above and below ADOS cut-off groups. The use of ADOS module 3 increased across the study period, whereas use of modules 1 and 2 decreased, indicating more language-abled children referred over time (Table 2, Fig. 6_supplement).
Among children with ADOS included in the assessment, the ADOS total score decreased slightly by a mean of 0.2 points a year (95% CI (0.06; 0.31), p = 0.005). A post hoc analysis that included only children with ASD showed a similar decline of 0.2 points per year (95% CI (0.05; 0.32), p < 0.006), whereas an analysis including only no-ASD showed no change in ADOS total score across time (difference − 0.0001 points per year, 95% CI (− 0.15; 0.15), p = 0.999). Thus, the decrease in ADOS total score among tested children was primarily accounted for by the children with an ASD diagnosis. Overall, the distribution of ASD subtypes was quite stable through the period although more children were assigned a diagnosis of childhood autism over the years compared to atypical autism (∆childhood/atypical p = 0.017), but there were no other subtype differences over time (∆childhood/Asperger p = 0.700, ∆childhood/PDD-NOS p = 0.882, ∆atypical/Asperger p = 0.992, ∆ atypical/PDD-NOS p = 0.149, ∆Asperger/PDD-NOS p = 0.845 (Fig. 3)).
Clinical Characteristics and Autistic Features of “Discordant Cases”
Discordant cases were seen in 24% of children above ADOS cut-off and in 8% of children below ADOS cut-off. Table 3 presents information about clinical characteristics and differences between discordant and concordant cases in the above and below ADOS cut-off groups (Table 3). Comparison of autistic features based on ADOS scores between the same groups are shown in Table 4 and Fig. 4. Children in the discordant subgroup had lower odds of a high score on all ADOS items compared to children in the concordant subgroup. E.g. an OR of 0.20 in the item hand and finger mannerisms means that discordant cases had 0.80 times reduced odds of a high score (Fig. 4).
Odds Ratio (OR) of discordant versus concordant cases on ADOS item scores in the above ADOS cut-off subgroups and below ADOS cut-off subgroup. Analyses: ordinal logistic regression adjusted for age at diagnosis, gender and year of assessment. Reference groups for estimating OR were concordant cases. Above ADOS cut-off subgroups = above cut-off on ADOS algorithm score (discordant cases "above/no-ASD" versus concordant cases "above/ASD"). Below ADOS cut-off subgroup = below cut-off on ADOS algorithm score (discordant cases "below/ASD" versus concordant cases "below/no-ASD. ADOS: Autism Diagnostic Observation Schedule
Groups Above ADOS Cut-Off
Discordant cases in the above ADOS cut-off group were more likely than concordant cases to be older, to have more comorbid diagnoses, and were more likely to have an IQ < 70. Discordant cases had lower mean scores on all ADOS domains and items, except the domain play and fantasy and the item unusual sensory interest in play, than concordant cases (Tables 3 and 4). When adjusting for age at diagnosis, gender and year of referral, all items (except quality of social response and unusual sensory interest in play) still differed between discordant and concordant cases (Fig. 4a). The results in Fig. 4a can be interpreted as follows: e.g. an OR of 0.20 in the item hand and finger mannerisms means that discordant cases had 0.80 times reduced odds of a high score. All three domains of social reciprocity, social communication and RRBs were more affected in concordant cases (children with an ASD diagnosis).
Below ADOS Cut-Off Groups
Discordant cases in the below ADOS cut-off group differed from concordant cases by having higher odds of ≥ 1 comorbid disorder. Most ADOS domain and items scores were higher in discordant cases, but only the ADOS total score and RRBs domain and item scores were significantly different (Tables 3 and 4). When adjusting for age at diagnosis, gender and year of referral, almost no differences were found between concordant and discordant cases, except in the items hand and finger mannerisms and excessive or unusual interests (Fig. 4b). Hence, especially the domain of RRBs was more affected in discordant cases (children with an ASD diagnosis). Interpretation of the results in Fig. 4b is the same as in Fig. 4a, e.g. an OR of 9.52 in the item hand and finger mannerisms means that discordant cases were 9.52 times more likely to have a high score.
Discussion
This study aimed to add to the growing literature examining time trends in ASD diagnosis, and to explore diagnostic differentiation of clinical features associated with an ASD diagnosis in young children. Our study showed time changes in both diagnostic practice and clinical characteristics of children referred for an ASD diagnostic assessment. More children were referred, the use of ADOS in the assessment increased, the use of dual diagnoses increased, and a higher percentage of children referred were assigned an ASD diagnosis across calendar year. We found a decrease in ADOS total score and more language-abled children referred, indicating that over time it seemed that more children with less severe autism symptoms were diagnosed with ASD.
In accordance with previous studies, we found an increase in both the number of referrals and in the probability of getting an ASD diagnosis over the period 2000–2010 (Arvidsson et al. 2018; Lundstrom et al. 2015; Myers et al. 2019). The increase in referrals could be explained by increased knowledge of ASD among parents and professionals and possibly also better access to services facilities (Myers et al. 2019; Nassar et al. 2009). The higher percentage of referred children being diagnosed with ASD could also be explained by a shift in clinical practice with improved diagnostics, e.g. ADOS, used more consistently and systematically in the assessment at the ASD clinic through the years. This shift in clinical practice reflects both a decision made by the ASD-clinic and a broader trend in Denmark for emphasis on more systematic ASD assessments procedures. The change in frequency of ADOS in the assessment seemed mainly explained by year of assessment. The decrease in ADOS total score among children diagnosed with ASD may indicate either a change in clinical ratings required to get scores of unusual behavior on ADOS or in the level of symptom severity. We did not find evidence of a change in clinical ratings, as no change was found in the distribution of discordant cases, nor in the likelihood of children being above or below cut-off on ADOS across years. Consequently, a change in symptom level of referred children may be the cause of the decrease in ADOS total score. Also, we found that more language-abled children were evaluated over time, evidenced by an increase in the use of ADOS module 3. Thus, the results suggest that more children with less severe symptoms were referred and diagnosed over time, in line with previous findings by Lundström (2015), Arvidsson (2018), and Myers (2019).
Regarding ASD subtypes, the findings show a fairly stable distribution over time, which may seem counterintuitive given the possible milder symptom profile over time. Nevertheless, results are comparable to Nassar (2009) who examined the same age-group and found a similar result with a simultaneous increase over time in the subtypes of both childhood autism and PDD-NOS, and thus no increase specifically for the milder subtypes. Also, Jensen (2014) examined a wide age range and found an increase in all subtypes in different age groups over time. However, only very few studies have investigated time trends in ASD subtype.
While the cognitive level did not change by calendar year, the number of assigned diagnoses of ID did, reflecting a deliberate change in clinical practice towards addressing a diagnosis of ID when the diagnostic criteria were met rather than including the cognitive level as part of the ASD diagnosis. And just like with ID diagnoses, overall, we found an increase in the number of other diagnoses (co-occurring disorders), which could be a consequence of both increased awareness of other developmental problems, and a rise in request for detailed descriptions of the complexity of the child's difficulties via diagnoses in order to design the most relevant support for the child despite exclusion criteria in ICD-10. Several studies highlight that changes and differences in, e.g. service practices, affect measured prevalence of a condition (Christensen et al. 2019; Hansen et al. 2015; Lundstrom et al. 2015; Nassar et al. 2009). The time trend for reporting co-occurring diagnoses is considered very important, as the presence of these has been suggested as a very significant factor contributing to the need for support beyond the ASD symptoms themselves (Arvidsson et al. 2018; Carlsson et al. 2013). Due to this fact, and since DSM-5 includes the possibility of diagnosing multiple co-occurring disorders (American Psychiatric Association 2013), clinical practice changed during and after the study period, although the official diagnosis system in Denmark remains ICD-10.
Our comparison of discordant and concordant cases indicate that RRBs, especially the ADOS items hand and finger mannerisms and excessive or unusual interests, may discriminate between cases and non-cases of ASD among children with a discordant symptom profile, especially in children below ADOS cut-off. Overall, the differences between ASD and no-ASD were more prominent in the above ADOS cut-off group. The children in the discordant groups (in both above and below ADOS cut-off) had clinical characteristics very similar to the children in their related concordant groups, suggesting that children with a final diagnosis of ASD were not significantly different from children with no diagnosis of ASD based on the clinical variables examined in this study. However, the children without a final diagnosis of ASD had a higher number of total diagnoses (more co-occurring diagnoses), and especially co-occurring diagnoses of mixed developmental disorders and factors influencing health status compared to children with a final ASD diagnosis. The higher number of assigned diagnoses among no-ASD may be a consequence of the need to describe the complexity of the child's difficulties, despite no ASD diagnosis, to improve access to individualized services for the children. In contrast to our result, the study by Carlsson (2013) showed more co-occurring disorders among Swedish children aged 4.5–6.5 years with a clinical ASD diagnosis compared to children with autistic features, measured by a semi-structured interview, but no clinical ASD diagnosis. The contradictory results may reflect differences in national clinical and diagnostic practices and study period. In the above ADOS cut-off group another difference was found, as discordant cases (no-ASD) were more likely to have an IQ < 70 than concordant cases (ASD). We cannot rule out that the result may be spurious, since the same was not found in the below ADOS cut-off group. As core features of ASD and ID often overlap with similar presentations of deficits in communication and age- appropriate social interactions (Close et al. 2012; Pedersen et al. 2017), behavioral features in children with reduced IQ may have been misinterpreted as autistic features and prompted referral for evaluation on suspicion of ASD. Therefore, decreased IQ may have increased the risk of an ADOS total score above cut-off, yet a clinical diagnosis result as no-ASD. Our result, with more cognitive delay in no-ASD compared to ASD in the above ADOS cut-off group, is in conflict with findings by Wiggins (2015) who found significantly more children with cognitive impairments in children with ASD. The different findings might be explained by referral practice and possible also by a younger age of the cohort in Wiggins (2015) compared to our cohort.
Relative to autistic features measured by ADOS, we found differences on several ADOS domains and items scores, with higher scores in the ASD children as expected in both above and below ADOS cut-off groups. The four items of ADOS measuring unusual eye contact, quality of social overtures, facial expression directed to examiner and amount of reciprocal social communication were found to be considerably different between the discordant and concordant subgroups in the above ADOS cut-off groups, corresponding to the four most discriminative items between ASD and ADHD found by Grzadzinski (2016). The result may reflect that clinicians emphasize better social functioning when deciding not to assign an ASD diagnosis despite an ADOS total score above cut-off. Expectedly, it was challenging to detect differences in the below ADOS cut-off groups due to the non-spectrum range of ASD symptoms and low scores on ADOS. However, RRBs scores were significantly different between concordant and discordant cases in both above ADOS cut-off and below ADOS cut-off, both on domain and item level, with higher odds of a higher score in the children with an ASD diagnosis. In line with results from the present study, the study by Grzadzinski (2016) also found RRBs to be different between ASD and ADHD, although not statistically significant. Furthermore, other studies investigating RRBs as a discriminative factor between ASD, other developmental disorders, and typically developing children, have found that it is possible to differentiate ASD from other developmental disorders based on the type and severity of RRBs presented, and especially sensory interests, hand and finger mannerisms, complex mannerisms, and repetitive behavior (Joseph et al. 2013; Kim and Lord 2010; Mandy et al. 2011). Thus, based on results from this and previous studies, clinicians may use the ADOS RRBs domain more heavily than the rest of the ADOS domains in the determinations of severity of ASD symptoms. Consequently, in cases of presence of RRBs despite a cut-off below ADOS threshold, this will lead to higher odds for an ASD diagnosis, and contrarily, no ASD diagnosis in cases with either very few RRBs or no RRBs despite a cut-off above threshold on ADOS. These findings may have implications for clinical practice related to the awareness of the role of RRBs in the diagnostic process. Yet, research is limited, and it will be relevant to investigate this further in future research.
Another important result from this study was the few differences in clinical characteristics that were found between ASD and no-ASD. Except from autism symptoms measured by ADOS, children were very similar in clinical characteristics such as age, gender, cognitive ability and co-occurring diagnoses. The findings highlight the difficulties in ASD diagnoses, and confirm the challenges clinicians often face when diagnosing children with symptoms of ASD at an early age, especially in children with milder variants of ASD symptoms or co-occurring symptoms of other developmental disorders.
Strengths and Limitations
The present study included all young children referred with suspicion of ASD in a distinct geographical area, thus representing the full range of the ASD spectrum in a total geographic population of children. This large unique cohort also included children with autism symptoms but with other diagnostic outcomes than ASD, and additionally, children across the whole IQ-range, which enhances the clinical generalizability. Furthermore, the homogeneity of one clinical unit overall using the same instruments, procedure and uniform application of the same ICD-10-based clinical diagnostic system throughout the whole study period increases the reliability of the data. In the present study the percentage of children referred on suspicion of ASD and assigned a diagnosis corresponded to another study undertaken during a slightly later time period (2011–2012) (Monteiro et al. 2015), thus increasing the comparability to other time periods and cohorts. Also, in order to make the ADOS assessment as independent as possible, it was administered in the beginning of the assessment period when the examiner had limited knowledge about the child and family. All clinical data were recorded prospectively, and all diagnoses were based on clinical consensus diagnoses after a multidisciplinary diagnostic assessment including information from several sources and settings; hence, the diagnostic validity is likely to be high.
Various limitations must be taken into account. First, the cohort represents data from one specialized clinic in Denmark potentially limiting external validity. Second, all data were obtained by review of information available in the medical records which lacked information on, e.g. systematic assessment of socioeconomic status and systematic assessment of adaptive functional level, which is of great importance in the assignment of a diagnosis. Third, the no-ASD children represent a particular subset of children, who were referred on suspicion of ASD but not diagnosed, and thus reflect clinical practice with regard to distinguishing children with ASD from children with other developmental disorders at a young age. As such, they are not representative of all no-ASD children, but rather representative of children with developmental disorders with autism symptoms, and are best generalizable to similar samples of similar age. Fourth, autistic features were only measured by ADOS domain- and item scores in the present study, and hence identification of other factors from the clinical assessment affecting the clinical diagnostic decision is missing, such as contradictory information or the situational nature of a particular symptom (Myers et al. 2019). Also, an ASD diagnosis based on a combination of clinicians observation and standard diagnostic instruments (e.g. ADOS) and caregiver reports is more reliable than diagnosis based on either observation or reports alone (Constantino 2011; Kamp-Becker et al. 2013; Lord et al. 2018; Falkmer et al. 2013). However, for research purpose ADOS is the single instrument with the best clinical diagnostic reliability (Grzadzinski et al. 2016; Kamp-Becker et al. 2013; Lord et al. 2000). Thus, we believe that the results regarding autistic features measured by ADOS during a clinical assessment are generalizable to other cohorts. Fifth, results regarding discordant cases must be interpreted with caution, because of the small numbers in these subgroups. Also, ADOS alone does not have perfect sensitivity and specificity, meaning that there will always be divergent results in relation to the clinical diagnosis and ADOS classification, and hence some degree of diagnostic uncertainty should be expected (Kamp-Becker et al. 2013; Lord et al. 2000; Lundstrom et al. 2015). Finally, during the study period (2000–2010), ADOS was used since ADOS-2 (Gotham et al. 2007) with the revised algorithm was not introduced in Denmark before 2013 (Lord et al. 2013). As the different ADOS modules were not directly comparable and because the Calibrated Severity Score (CSS) was not part of the ADOS version we did not use CSS to compare autism severity across age and different ADOS modules (Gotham et al. 2007).
Conclusion
Across the decade of this study period this study showed an increase in number of referrals of children with ASD symptoms, less severe autism symptoms in children getting an ASD diagnosis, and changes in clinical practice measured by more systematic use of ADOS in the assessment and increased allocation of co-occurring disorders. Moreover, we found restricted repetitive behaviors (RRBs) as measured by ADOS, and especially the items hand and finger mannerism and excessive or unusual interests or repetitive behaviors, may be specifically important factors in the clinical distinction between ASD and no-ASD in young children with a discordant symptom profile, especially among children with ADOS score below cut-off. The result of this study revealed the clinical importance of RRBs in determining a final diagnosis of ASDs. Recognizing the limitation of the explorative design of our study, the findings suggest that clinicians, in view of all the clinical characteristics available to them, seem to weigh the ADOS RRBs domains more heavily than the rest of the ADOS domains in determining the final clinical diagnosis in discordant cases. This knowledge may be instructive for future clinical practice to be aware of the pattern yet placing RRBs in proper context with all available clinical features when making a final diagnosis. This awareness may increase the diagnostic validity for ASD and other developmental disorders and ensure timely and targeted intervention.
References
Association, A. P. (Ed.). (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington: American Psyciatric Publishing.
Arvidsson, O., Gillberg, C., Lichtenstein, P., & Lundstrom, S. (2018). Secular changes in the symptom level of clinically diagnosed autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 59(7), 744–751. https://doi.org/10.1111/jcpp.12864.
Baio, J., Wiggins, L., Christensen, D. L., Maenner, M. J., Daniels, J., Warren, Z., et al. (2018). Prevalence of autism spectrum disorder among children aged 8 years: Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. Morbidity and Mortality Weekly Report Surveillance Summaries, 67(6), 1–23. https://doi.org/10.15585/mmwr.ss6706a1.
Carlsson, L. H., Norrelgen, F., Kjellmer, L., Westerlund, J., Gillberg, C., & Fernell, E. (2013). Coexisting disorders and problems in preschool children with autism spectrum disorders. The Scientific World Journal, 2013, 213979. https://doi.org/10.1155/2013/213979.
Christensen, D. L., Maenner, M. J., Bilder, D., Constantino, J. N., Daniels, J., Durkin, M. S., et al. (2019). Prevalence and characteristics of autism spectrum disorder among children aged 4 years: Early autism and developmental disabilities monitoring network, seven sites, United States, 2010, 2012, and 2014. Morbidity and Mortality Weekly Report Surveillance Summaries, 68(2), 1–19. https://doi.org/10.15585/mmwr.ss6802a1.
Close, H. A., Lee, L., Kaufmann, C. N., & Zimmerman, A. W. (2012). Co-occurring conditions and change in diagnosis in autism spectrum disorders. Pediatrics, 129(2), e305–e316. https://doi.org/10.1542/peds.2011-1717.
Constantino, J. N. (2011). The quantitative nature of autistic social impairment. Pediatric Research, 69(5 Pt 2), 55R–62R. https://doi.org/10.1203/PDR.0b013e318212ec6e.
Falkmer, T., Anderson, K., Falkmer, M., & Horlin, C. (2013). Diagnostic procedures in autism spectrum disorders: A systematic literature review. European Child and Adolescent Psychiatry, 22(6), 329–340. https://doi.org/10.1007/s00787-013-0375-0.
Gotham, K., Risi, S., Pickles, A., & Lord, C. (2007). The autism diagnostic observation schedule: Revised algorithms for improved diagnostic validity. Journal of Autism and Developmental Disorders, 37(4), 613–627. https://doi.org/10.1007/s10803-006-0280-1.
Grzadzinski, R., Dick, C., Lord, C., & Bishop, S. (2016). Parent-reported and clinician-observed autism spectrum disorder (ASD) symptoms in children with attention deficit/hyperactivity disorder (ADHD): Implications for practice under DSM-5. Molecular Autism. https://doi.org/10.1186/s13229-016-0072-1.
Hansen, S. N., Schendel, D. E., & Parner, E. T. (2015). Explaining the increase in the prevalence of autism spectrum disorders: The proportion attributable to changes in reporting practices. JAMA Pediatrics, 169(1), 56–62. https://doi.org/10.1001/jamapediatrics.2014.1893.
Helt, M., Kelley, E., Kinsbourne, M., Pandey, J., Boorstein, H., Herbert, M., et al. (2008). Can children with autism recover? If so, how? Neuropsychology Review, 18(4), 339–366. https://doi.org/10.1007/s11065-008-9075-9.
Jensen, C. M., Steinhausen, H., & Lauritsen, M. B. (2014). Time trends over 16 years in incidence-rates of autism spectrum disorders across the lifespan based on nationwide danish register data. Journal of Autism and Developmental Disorders, 44(8), 1808–1818. https://doi.org/10.1007/s10803-014-2053-6.
Joseph, L., Thurm, A., Farmer, C., & Shumway, S. (2013). Repetitive behavior and restricted interests in young children with autism: Comparisons with controls and stability over 2 years. Autism Research: Official Journal of the International Society for Autism Research, 6(6), 584–595. https://doi.org/10.1002/aur.1316.
Kamp-Becker, I., Ghahreman, M., Heinzel-Gutenbrunner, M., Peters, M., Remschmidt, H., & Becker, K. (2013). Evaluation of the revised algorithm of autism diagnostic observation schedule (ADOS) in the diagnostic investigation of high-functioning children and adolescents with autism spectrum disorders. Autism: The International Journal of Research and Practice, 17(1), 87–102. https://doi.org/10.1177/1362361311408932.
Kim, S. H., & Lord, C. (2010). Restricted and repetitive behaviors in toddlers and preschoolers with autism spectrum disorders based on the autism diagnostic observation schedule (ADOS). Autism Research, 3(4), 162–173. https://doi.org/10.1002/aur.142.
Levy, A., & Perry, A. (2011). Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders, 5(4), 1271–1282. https://doi.org/10.1016/j.rasd.2011.01.023.
Lord, C., Elsabbagh, M., Baird, G., & Veenstra-Vanderweele, J. (2018). Autism spectrum disorder. Lancet (London, England), 392(10146), 508–520.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Jr., Leventhal, B. L., Dilavore, P. C., et al. (2000). The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. https://doi.org/10.1023/A:1005592401947.
Lord, C., Rutter, M., Dilavore, P. C., Risi, S., Gotham, K., & Bishop, S. L. (2013). Autism diagnostic observation schedule 2nd ed. (ADOS-2) Danish version. Boston: Hogrefe.
Lundstrom, S., Reichenberg, A., Anckarsater, H., Lichtenstein, P., & Gillberg, C. (2015). Autism phenotype versus registered diagnosis in swedish children: Prevalence trends over 10 years in general population samples. BMJ (Clinical Research Ed.), 350, h1961. https://doi.org/10.1136/bmj.h1961.
Mandy, W., Charman, T., Gilmour, J., & Skuse, D. (2011). Toward specifying pervasive developmental disorder-not otherwise specified. Autism Research: Official Journal of the International Society for Autism Research, 4(2), 121–131. https://doi.org/10.1002/aur.178.
Monteiro, S. A., Spinks-Franklin, A., Treadwell-Deering, D., Berry, L., Sellers-Vinson, S., Smith, E., et al. (2015). Prevalence of autism spectrum disorder in children referred for diagnostic autism evaluation. Clinical Pediatrics, 54(14), 1322–1327. https://doi.org/10.1177/0009922815592607.
Mullen, E. M. (1995). Mullen scales of early learning (MSEL). Circle Pines, MN: American Guidance Service.
Myers, S. M., Voigt, R. G., Colligan, R. C., Weaver, A. L., Storlie, C. B., Stoeckel, R. E., et al. (2019). Autism spectrum disorder: Incidence and time trends over two decades in a population-based birth cohort. Journal of Autism and Developmental Disorders, 49(4), 1455–1474. https://doi.org/10.1007/s10803-018-3834-0.
Nassar, N., Dixon, G., Bourke, J., Bower, C., Glasson, E., de Klerk, N., et al. (2009). Autism spectrum disorders in young children: Effect of changes in diagnostic practices. International Journal of Epidemiology, 38(5), 1245–1254. https://doi.org/10.1093/ije/dyp260.
Pedersen, A. L., Pettygrove, S., Lu, Z., Andrews, J., Meaney, F. J., Kurzius-Spencer, M., et al. (2017). DSM criteria that best differentiate intellectual disability from autism spectrum disorder. Child Psychiatry and Human Development, 48(4), 537–545. https://doi.org/10.1007/s10578-016-0681-0.
Salazar, F., Baird, G., Chandler, S., Tseng, E., Osullivan, T., Howlin, P., et al. (2015). Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-015-2361-5.
Schendel, D. E., & Thorsteinsson, E. (2018). Cumulative incidence of autism into adulthood for birth cohorts in Denmark, 1980–2012. JAMA, 320(17), 1811–1813. https://doi.org/10.1001/jama.2018.11328.
Simonoff, E., Jones, C. R. G., Baird, G., Pickles, A., Happé, F., & Charman, T. (2013). The persistence and stability of psychiatric problems in adolescents with autism spectrum disorders. Journal of Child Psychology and Psychiatry and Allied Disciplines, 54(2), 186–194. https://doi.org/10.1111/j.1469-7610.2012.02606.x.
Snijders, J. T., Tellegen, P. J., & Laros, J. A. (1997). Snijders-oomen nonverbaler intelligenztest SON-R 55–17. Göttingen: Hogrefe.
Wechsler, D. (1989). Wechsler preschool and primary scale of intelligence: revised. San Antonio, TX: Psychological Corporation.
Wechsler, D. (1991). Wechsler intelligence scale for children (3rd ed.). San Antonio, TX: Psychological Corporation.
Wechsler, D. (2002). Wechsler preschool and primary scale of intelligence (3rd ed.). San Antonio, TX: Psychological Corporation.
Wiggins, L. D., Levy, S. E., Daniels, J., Schieve, L., Croen, L. A., DiGuiseppi, C., et al. (2015). Autism spectrum disorder symptoms among children enrolled in the study to explore early development (SEED). Journal of Autism and Developmental Disorders, 45(10), 3183–3194. https://doi.org/10.1007/s10803-015-2476-8.
Wiggins, L. D., Rice, C. E., Barger, B., Soke, G. N., Lee, L. C., Moody, E., et al. (2019). DSM-5 criteria for autism spectrum disorder maximizes diagnostic sensitivity and specificity in preschool children. Social Psychiatry and Psychiatric Epidemiology, 54(6), 693–701. https://doi.org/10.1007/s00127-019-01674-1.
World Health Organisation (Ed.). (1992). The ICD-10 classification of mental health and behavioral disorders. diagnostic criteria for research (Geneva, Switzerland ed.) World Health Organisation.
Xu, G., Strathearn, L., Liu, B., & Bao, W. (2018). Prevalence of autism spectrum disorder among US children and adolescents, 2014–2016. JAMA, 319(1), 81–82. https://doi.org/10.1001/jama.2017.17812.
Acknowledgments
None of the authors have any financial or personal relationships with people or organizations that could influence the work of this article. This work was supported by Aarhus University Hospital, Department of Child and Adolescent Psychiatry, and by grants from the Research fund of Child and Adolescent Psychiatry, Central Denmark Region, Denmark, Sofie Foundation, Butcher Wörzner and Wife Memorial Fund, and Mrs C. Hermansen Memorial Fund. The funders had no involvement in any aspects of the study. The authors would like to thank Emilie Riis Kjeldsen and Katrine Jaquet Mavraganis for assistance in the data collection process, Astrid Voldstedt Lund Høy for reviewing cognitive test results, and Jens Søndergaard Jensen for invaluable statistical assistance.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, design and interpretation of results. Data collection and analyses were performed by Sara Højslev Avlund. The first draft of the manuscript was written by Sara Højslev Avlund and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the present paper was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Avlund, S.H., Thomsen, P.H., Schendel, D. et al. Time Trends in Diagnostics and Clinical Features of Young Children Referred on Suspicion of Autism: A Population-Based Clinical Cohort Study, 2000–2010. J Autism Dev Disord 51, 444–458 (2021). https://doi.org/10.1007/s10803-020-04555-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-020-04555-8