Abstract
Autism spectrum disorder (ASD) is a neurodevelopmental condition classified based on needs of support, in order to address impairments in the areas of social communication and restricted and repetitive behavior. The aim of this work is to describe the main clinical features of the ASD severity levels in a group of Mexican pediatric patients. The results show firstly that this condition was more frequent in males than females. Secondly, an inverse relationship was found between the intellectual coefficient and the level of severity of the disorder. Thirdly, deficits in social reciprocity and communication were more evident in Level 3, than in Levels 1 and 2, while the difference was less evident in restricted and repetitive patterns of behavior.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Autism spectrum disorder (ASD) is a neurodevelopmental condition characterized by impairments in social communication and restrictive and repetitive behaviors that persist throughout life (American Psychiatric Association 2013). The marked prevalence of this disorder deserves much attention, as it has increased significantly over the past decade, and 20 times since 1980 (Yip et al. 2017). In Asia, for example, the average ASD prevalence for 1980 was 1.9 cases per 10,000, increasing to 14.8 between 1980 and 2010 (Sun and Allison 2010). In the United Kingdom, the United States, Japan, and Scandinavia, ASD prevalence was approximately in the range of 30 to 60 cases per 10,000, as indicated by a review of epidemiological studies published between 1996 and 2001 (Rutter 2005). The most recent estimates are as high as 1 in 59, based on a study of 8-year-old children in the United States (CDC 2014). In Mexico, the estimated prevalence is 1 in 115 (Fombonne et al. 2016).
Establishing the prevalence of ASD is of particular complexity due to several factors: the high heterogeneity in the presentation of symptoms, the lack of diagnostic biological markers, and the modification of the disorder classification from the diagnostic and statistical manual of mental disorders fourth edition (DSM-IV) to the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V)—which resulted in changes in the diagnostic criteria (Rice et al. 2007). To add to this complexity, ASD is a dimensional process of extensive symptomatology and comorbidity with a widely variable onset. Moreover, ASD affects all aspects of development, including language deficiencies and various behavioral and psychological conditions, such as aggression, attention deficit, hyperactivity, and anxiety (Esler and Hall-Lande 2017). Another notable characteristic of ASD is an atypical sensory performance in the visual, tactile, auditory, and olfactory systems (Koehler et al. 2018). Evidence suggests, for example, that up to 95% of parents of children with ASD describe some atypical sensory behavior in the child, such as indifference to pain, avoidance of unusual smells of objects, of certain sounds and textures, and the seeking of visual experiences involving lights and movements (Rogers and Ozonoff 2005; Nieto et al. 2017). The DSM-V from the American Psychiatric Association (APA) classifies such “hyper or hypo-reactivity to sensory stimuli and unusual interest in environmental stimuli,” as a type of restricted or repetitive behavior. In support of this, there is behavioral, anecdotal, and neurophysiological evidence of sensory impairment being a characteristic and persistent feature of ASD (Thye et al. 2018). Consequently, the standard reference evaluation (gold standard) for diagnosis requires substantial time and clinical judgment, involving multiple evaluation mechanisms and research from numerous professionals (Randall et al. 2018).
Albeit the severity of symptoms, the spectrum of needs in terms of the assistance and services that enable an ASD patient’s integration into daily life, is extremely vast (Masi et al. 2017). First of all, symptoms associated with ASD range from mild to profound deficiencies, which can affect all functions of everyday life. Second of all, the severity of symptoms increases when demands in certain environments exceed the individual’s ability to function at a required level. For this reason, the severity classification of ASD is based on personalized levels of support needed to address patients’ deficiencies in social communication and interaction, behavior patterns, and restricted and repetitive interests or activities (American Psychiatric Association 2013). The DSM-V classifies ASD into three severity levels: Level 1 indicates that the patient requires support in some areas; Level 2 requires substantial support; and Level 3 requires a significant increment of substantial support (American Psychiatric Association 2013). It is important to note that the ASD severity level is not a measure that remains fixed over time, as it varies depending on the quality of medical, educational, psychological and alternative supports that patients receive.
Since autism is essentially dynamic, it is necessary to stress that the degree of advancement and regression or stagnation of a person depends on the quality of the intervention provided by the environment. Although the interference of organic variables in the learning and development process of patients with ASD cannot be denied, this does not mean that their condition cannot improve (Vázquez-Ramírez 2017). A recent study testing a method of identifying children with ASD has demonstrated that there is a wide range of clinical features and progression, as well as a great variability in prognosis (Masi et al. 2017). This result challenges the concept that ASD phenotypes are fixed or stable and insensitive to treatment, suggesting that developmental trajectories may diverge significantly between different individuals (Masi et al. 2017). Moreover, the direct and indirect requirements of patients with ASD extend to many areas including health, education, social assistance, and employment and social benefits, which entails a considerable economic burden for families and the immediate society (Buescher et al. 2014; Ganz 2007). It is therefore crucial to identify ASD cases as early as possible, since educational planning and early intervention result in better outcomes for these children (NIH 2007).
To date, there is little scientific evidence to support differences in behavioral characteristics of ASD among different populations (Esler and Hall-Lande 2017). In Mexico’s population particularly, no data exists to accurately describe the status of ASD according to the DSM-V classification. Consequently, the objective of this research is to describe the main characteristics of ASD in a sample of the Mexican pediatric population.
Method
Study Population
This paper presents a descriptive study in which 203 children diagnosed with ASD between 2014 and 2018 were analyzed at the Centro de Investigación y Atención del Autismo (CIAA) and the Centro de Rehabilitación Integral (CRI) in Torreón, Coahuila, Mexico. Both institutions are part of the National System for the Integral Development of the Family (DIF) of the State of Coahuila, Mexico. A total of 1138 children from 1 to 12 years old received services at the CRI and the CIAA between 2014 and 2018. Of these, 845 children were referred to the Department of Speech-Language, where the presumptive diagnosis of ASD was stablished at 690 children. The diagnosis was confirmed by the Department of Neuropsychology in 431 of them (37.87%). Finally, of these 431 children with confirmed diagnosis, 203 clinical records of children who receive intervention services (integral therapy, family therapy and nutrition intervention) were obtained. It is important to note that most of the children that come to the Department of Speech-Language are referred for suspected ASD in other institutions such as schools, or because of parental concern when observing development difficulties in the child.
The identification of ASD cases was carried out with a multidisciplinary approach conducted in two stages: the clinical and the neuropsychological diagnosis. Patients were firstly clinically evaluated by a speech-language expert who established a pre-diagnosis. Children with suspected ASD were then referred for evaluation to the Department of Neuropsychology, where appropriate tests (described below) were applied to confirm or rule out the diagnosis. During these two stages, a survey about clinical, sociodemographic and treatment was conducted by clinicians. This study was approved by the Bioethics Committee of the Facultad de Medicina (Faculty of Medicine) Unidad Torreón, of the Universidad Autónoma de Coahuila (UAC).
Clinical Diagnosis
The first stage of the presumptive diagnosis or suspicion of ASD was established through a rigorous interview with the child’s parents or guardians, ensuring that the person interviewed was the one who lived most closely with the child. The purpose of such a requirement was to retrieve reliable information about the patient’s characteristics and/or behaviors. This stage also included a physical examination, observation of the child’s behavior during the interview, and a questionnaire about sociodemographic and clinical questions about children and parents.
Neuropsychological Diagnosis
The second stage of the evaluation was conducted by the Department of Neuropsychology of the CIAA. The areas evaluated were: cognitive (attention, memory, visuospatial, visual perception, vasoconstriction, and academic performance); linguistic (amplitude, point and mode of articulation of phonemes, use of language for social communication); and executive and behavioral functions characteristic of ASD (according to the DSM-V criteria). In order to establish the diagnosis according to CI10 and DSM-V, the assessment instruments applied were: Psychoeducational Profile 3 (PEP-3), Autism Diagnostic Observation Schedule (ADOS), Autism Behavior Inventory (ABI), Neuropsychological Battery for Preschoolers (BANPE), Neuropsychological Evaluation for Children (ENI), Adaptive Behavior Assessment System, Second Edition (ABASTM-II), Picture Vocabulary Test (PEABODY), and Childhood Autism-Modified Questionnaire (M-CHAT). For non-verbal children, the Raven’s Progressive Matrix Test, Colored Scale was applied. In addition, Human Development Indexes (HDI) were used, as well as the Bailey Child Development Scale. Furthermore, to assess the intelligence quotient (IQ), the Wechsler Preschool and Primary Scale of Intelligence (WPPSI IV) and the Wechsler Intelligence Scale for Children (WISC IV) were also used. Next, the number of evaluation sessions and the amount of time each patient required was decided accordingly on an individual basis. Finally, the medical record was integrated with the data obtained from the clinical evaluation, as well as the results of the studies, and the treatment indications that were considered necessary after the evaluation.
Statistical Analysis
The variables were described according to their frequencies and distribution measures (arithmetic mean and standard deviation). Statistical differences were established between groups using the t test for continuous and normal distribution variables, and the X2 test for categorical variables. Statistical significance was established with a value of p ≤ 0.05. The program used was STATA 8.0.
Results
A total of 203 children with a confirmed diagnosis of ASD were studied. The mean age of the studied population at diagnosis was 5.52 years (1 to 12-year-old range). The female to male ratio was 1:3.9. According to the severity level classification based on DSM-V criteria, the most frequent diagnosis was Level 2 (47.78%), followed by Level 1 (35.96%), and Level 3 (16.26%). In addition, differences in age at diagnosis were statistically significant when Levels 2 and 3 were compared against Level 1, while there was no significant difference between Levels 2 and 3 (Table 1). Information about clinical treatment and sociodemographic characteristics were also gathered (Tables 1 and 2).
An important factor to underline in this study is that approximately one in four patients have been, or are being, medicated. The most-prescribed medications were risperidone (RIS), methylphenidate (MPH)-risperidone (RIS) combination, and magnesium valproate. Children with ASD Levels 2 and 3 received drug treatment in greater proportion than patients with Level 1 (x2 = 8.24, p = 0.016) (Table 1). No significant differences were found in the type of childbirth, labor complications and parents’ history (Tables 1 and 2). The clinical data related to ASD, as well as its frequencies, are referred to in Table 3.
Moving on to IQ evaluation, more than one-third of the studied population has an IQ within the average (86–115); one-quarter has borderline IQ (71–85); while nearly one-third has a mild (50–70) to moderate (35–49) IQ. This study showed that IQ was inversely related to the severity level (Table 4).
Discussion
As previously stated, the mean age at diagnosis in this study was 5.52 years, which coincide with that reported by CDC, where most children have a first diagnosis of ASD above 4 years old (CDC 2014). The importance of giving attention to the mean age at diagnosis lies in that the earlier the diagnosis (the younger the patient is), the better expectations and possibilities of development in the ASD patient. The importance of giving attention to the mean age at diagnosis lies in that the earlier the diagnosis (the younger the patient is), the better expectations and possibilities of development in the ASD patient. Although ASD can be reliably diagnosed as early as age 2 by an experienced professional, many children are diagnosed later (Johnson and Myers 2007; Lord et al. 2006). As an example, Pringle et al. (2012) found that 40% of children with ASD are 6 years or older when first identified. In a Japanese population sample, the mean age of diagnosis was significantly higher: 7.2 years (Kurasawa et al. 2018). In a Mexican population sample, a recent study conducted in León, Guanajuato, showed that 55.5% of children were diagnosed from ages 3 to 5, while 22% were diagnosed later (Fombonne et al. 2016). What is most important about this data is that the delay in diagnosis means that children with ASD will receive the attention they need until much later.
As expected, this study demonstrated that the age of diagnosis was directly proportional to the severity level: the higher the affectation level, the earlier ASD is diagnosed. Thus, the mean age at diagnosis in Level 1 was 6.44 years, while for Levels 2 and 3 it was 5.05 years and 4.85 years, respectively. These differences of age at diagnosis by level of severity were statistically significant (Table 1). In a previous study, Mayes and Calhoun (2004) had in fact identified that patients with mild ASD (previously classified as Asperger syndrome) are diagnosed later than those whose symptoms are more severe. As a result, in order to avoid delays in treatment, it is critical that primary care physicians are advised to consider ASD as a diagnostic possibility in young children with symptoms of attention deficit and hyperactivity disorder (ADHD) (Miodovnik et al. 2015). This early diagnose is of utmost importance, considering how in Iceland for example, 51% of children with ASD had remained undiagnosed before age 6 (Jónsdóttir et al. 2011). Furthermore, the American Academy of Pediatrics (AAP) recommends that during the medical consultation, doctors should consider the family history, parental concerns, and also conduct careful observation of the child’s development at each regular visit (Council on Children with Disabilities 2006).
Differences by Sex
To briefly report, differences in ASD prevalence by sex have remained consistent with widely reported data, despite changes in diagnostic criteria and improved early detection (Harrop et al. 2018). As the Center for Disease Control and Prevention (CDC) has reported, ASD is four times more common in males than females (CDC 2014). Such data is consistent with the results in this study, where the female to male ratio was 1:3.9. In the population of León, Guanajuato, Mexico, Fombonne et al. (2016) found a ratio of 1:4.1. Similarly, a ratio of 1:4.5 was found in an epidemiological study of autism in the United States, which analyzed 697 children aged 2 to 6 from different ethnicities and autism centers (DiGuiseppi et al. 2016). Given this marked discrepancy in sex ratio, most ASD research has focused on males (Hartley and Sikora 2009). Nevertheless, there seem to be some variations between populations. For example, a recent systematic study reported a female to male ratio of about 1:3 (Loomes et al. 2017). Similarly, a population in Japan found a female to male ratio of 1:3.1 years (Kurasawa et al. 2018).
Although little is known about the reasons for sex differences in ASD diagnosis, some authors have suggested that cases of female children with ASD are in fact underdiagnosed (Evans et al. 2018), since clinical manifestations seem to be more pronounced in male children (Loomes et al. 2017). Some studies indicate that the female to male ratio with ASD without intellectual disability, ranges from 1:6 to 1:16, while the female to male ratio with ASD plus moderate or severe intellectual disability is approximately 1:1 or 1:2 (Werling and Geschwind 2013). In addition, several neurodevelopmental disorders, including ADHD disorder, oppositional defiant disorder (TND), and intellectual disability, are more common in males (Ferri et al. 2018; Werling and Geschwind 2013).
Other studies have attributed the male preponderance of ASD to various genetic modifications, such as sex-specific single nucleotide polymorphisms (SNPs), microdeletions, and copy number variations (CNVs) (Carayol et al. 2011; Sato et al. 2012; Steeb et al. 2014; Tropeano et al. 2013, 2016; Werling and Geschwind 2013). However, in trying to determine a possible susceptibility and protective factors by sex, a review conducted by Ferri et al. (2018) showed contradictory results, perhaps due to the heterogeneity of ASD and the low power of prevalence studies. Due to this discrepancy, the authors have proposed that it would be convenient to carry out studies with a greater number of subjects and better control of the variables involved.
Treatment
Treatment options for ASD are limited and are aimed at reducing symptomatology, mental comorbidity and other medical conditions that exacerbate the severity on presentation (Masi et al. 2017). This study’s findings confirm previous research that demonstrates how early intervention treatments can significantly improve a child’s development (Harris and Handleman 1994). According to reports submitted by the AAP and the National Research Council, the approaches that most assist children with ASD, in terms of improving their behavior and communication, are those that provide structure, direction, and organization for the child, and include family involvement (National Research Council 2001).
Turning now to medical treatment, even when drugs cannot cure ASD, they have a palliative effect that contributes to improving various functions in patients. Some drugs, for example, can help control high levels of hyperactivity, inability to concentrate, depression, and seizures (CDC 2014). As mentioned earlier, one-quarter of the patients in this study received or are receiving some type of medication. The most commonly prescribed drug was risperidone alone or combined with methylphenidate and magnesium valproate. As expected, children at Level 3 were the most frequently treated with drugs. It should also be mentioned that risperidone and aripiprazole are the only drugs approved by the U.S. Food and Drug Administration (FDA) for the treatment of symptoms associated with ASD. Risperidone, which acts by blocking dopaminergic and serotonergic brain receptors, is safe and effective for short-term treatment, with observed improvements in stereotyped behavior and hyperactivity (McCracken et al. 2002). However, side effects include weight gain (due to increased appetite), drowsiness, and increased prolactin (produced by the pituitary gland), of which its prolonged and substantial elevations are associated with adverse effects. Direct effects of elevated prolactin on breast tissue lead to galactorrhea in female and gynecomastia in males (Anderson et al. 2007).
Clinical and Socio-demographic Characteristics
Several clinical and sociodemographic variables have been associated with the risk of developing ASD: cesarean birth, labor complications, low birth weight, and advanced parental age (Burstyn et al. 2010; Curran et al. 2015; Glasson et al. 2004; Langridge et al. 2013; Modabbernia et al. 2017; Polo-Kantola et al. 2014). However, neither the way in which each variable affects patients, nor its overall effect is yet clear (Sandin et al. 2016). In this study’s sample, there does not appear to be any significant statistical differences between the results obtained and those identified for the general Mexican population and reported by the National Institute of Statistics, Geography and Informatics (INEGI 2015), in the Statistical and Geographic Yearbook of Coahuila de Zaragoza.
Interestingly, it is worth noting that the increase in the number of cesarean sections (C-sections) has been parallel to the global diagnosis of autism (Yip et al. 2017). To date, almost half of all births occur by C-sections in several populations across the world (Vogel et al. 2015; Vieira et al. 2015). For this reason, it has been postulated that scheduled cesarean births before the last week (or weeks) of gestation can have a possible effect on ASD (American College of Obstetricians and Gynecologists 2013), since this time period is also important for brain development (MacKay et al. 2013). A similar situation could occur with preterm deliveries (Yip et al. 2017).
In this study, half of the children in the sample were born by C-section, which does not differ significantly to the numbers based on the entire population of the State of Coahuila, where most termination of pregnancies was conducted by C-section (INEGI 2015). Although it is interesting to highlight that a higher proportion of children at Level 3 were born by C-section compared to those at Levels 1 and 2, these differences were not significant. Moreover, several systematic reviews and meta-analyses have summarized evidence on the association between ASD and various pregnancy and labor complications such as: pelvic presentation, umbilical cord circularity, fetal distress, multiple births, hyperbilirubinemia, Rh or ABO incompatibility (Gardener et al. 2009, 2011; Kancherla and Dennis 2006; Kolevzon et al. 2007). In this study, more than one-fifth of births had labor complications (Table 1), while the average birth weight was found in normal values (Shah et al. 2008). Lastly, advanced parental age—albeit unclearly—has been associated with the risk of ASD. To exemplify, Sandin et al. (2016) have demonstrated that the relative risk for ASD is 1.34 for the children of women aged 40–49 years, and 1.66 for the children of men aged ≥ 50 years (Sandin et al. 2016). In this study, however, no significant difference was found in either the maternal (mean 26.27 years) or paternal age (mean 29.04 years) from that identified in the general Mexican population (INEGI 2015).
Symptoms
In general, this study indicates that most patients, regardless of the severity level, present the core signs and symptoms of ASD (Table 3). Firstly, impairments in social communication were more significantly affected in Level 3 than in Levels 1 and 2, which is a difference that is statistically significant. In another study conducted to assess the recognition of emotions by ocular evaluation and electroencephalography, Black et al. (2017) concluded that the visual processing of emotions is different in patients with ASD than in those without it. Similarly, it has been observed that the ability of patients to interpret other people’s nonverbal, facial, and body expressions is strongly impaired (Molnar-Szakacs and Heaton 2012). Although some people with ASD may achieve recognition of emotions, the process of how they do it is nonetheless different from people without ASD (Fitzpatrick et al. 2018). In general, deficits in the recognition of basic emotional expressions seem to be predominantly found in ASD patients who also have intellectual disabilities. Contrastingly, individuals with IQ in the normal range generally perform well in tests regarding facial expressions (Loth et al. 2018). These data are congruent with those found in this study, where Level 3 patients had more difficulty recognizing emotions than those at Levels 1 and 2.
Another area in this study where significant differences were found according to the degree of severity, was in the preference to play alone (Table 3). Dean et al. (2017) found, for example, that typically developing children play games significantly more than children with ASD. In the sample of this study, a higher percentage of children at Level 3 avoided physical contact compared to those at Levels 1 and 2. Similarly, several studies have demonstrated that children with ASD often “stiffen” when touched, try to avoid contact, and prefer to be touched on their terms (e.g., when they initiate contact and when they are receptive to contact) (Kern et al. 2007; Siegel 1998). To explain this behavior, Peled-Avron and Shamay-Tsoory (2017) hypothesize that there may be a degree of neuronal hypervigilance to the social contact in ASD patients. Therefore, the authors examined the correlation between autistic traits and neuronal activity markers, measured through the perception of social eye contact. The results in the analyzed sample demonstrated that individuals with more autistic traits avoided and showed more aversion to social contact, as confirmed by previous literature (Peled-Avron and Shamay-Tsoory 2017). As a matter of fact, when social anxiety disorder is present, physical closeness can be threatening and can cause hypervigilance, which is reflected in the consistency of interpersonal distance (Perry et al. 2013).
In regard to restricted, repetitive patterns of behaviors, interests, and abnormal activities, although the data from this study’s patient sample showed a higher percentage as the degree of severity increases, the differences were not as marked as in the case of the area of deficits in social reciprocity and communication: 81%, 85% and almost 87% respectively (non-significant differences). Incontinence was another factor with significant difference, when analyzing by levels of severity, since an inverse relationship was evidenced between these two variables: considering that an inverse relationship was evidenced between these two variables: 60.87% for Level 1; 86.21% for Level 2; and 88.46% for Level 3 (X2 = 16.19, p = 0.0001). In general, children with special needs, intellectual disabilities, or ASD, are more frequently affected by incontinence than typically developing children (von Gontard et al. 2015).
Furthermore, significant differences in language were also found in relation to the severity level (Table 3). Language delay has been described as one of the first indicators and predictor of cognitive and behavioral outcomes in ASD (D’Mello et al. 2016). Recent studies on language delay in ASD suggest that this occurrence may result in a suboptimal language, with reduced verbal IQ and poorer ability to generate words in adulthood (Lai et al. 2014). In addition, previous neuroimaging studies suggest that language delay may underlie neuronal differences between autistic individuals with and without language delay (D’Mello et al. 2016).
Another symptom pertains to one of the earliest concerns of parents with ASD children: developmental regression (De Giacomo and Fombonne 1998; Shattuck et al. 2009). Previous research has reported that approximately one-third to one-half of the population of children with ASD experienced regression (Hansen et al. 2008; Goin-Kochel et al. 2014; Lord et al. 2004; Wiggins et al. 2009)—while other research suggests lower frequencies (Esler and Hall-Lande 2017). In this study, only 9.84% of children showed regression in development. No study to date, however, presents a clear explanation for such variations.
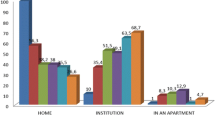
Intelligence Quotient
Congruent with results from previous studies, we found an inverse relationship between the IQ and the level of ASD severity, with highly significant differences (Table 4, Fig. 1). Since the 1960 s, it has been widely known that IQ is the best prognostic factor in cases of autism (Rutter 1970). On one hand, poorer cognitive ability has been associated with greater severity of ASD symptoms (Mayes and Calhoun 2011). On the other hand, other authors such as Bitsika et al. (2018) found that patients in the high severity group had a greater cognitive ability (i.e., higher full-scale IQ WASI-II). These latter studies suggest that even though the cognitive ability should remain a diagnostic consideration in relation to ASD severity level symptoms, this is not a mandatory aspect of the diagnosis of ASD per se.
In the Mexican population analyzed in this study, a greater proportion of children with a normal IQ (41.71%) was observed; 25.6% had borderline IQ; about one-third of the sample (28.88%) had some intellectual disability, with a mild to moderate impairment; while severe impairment was not found in any. Similar proportions were found in the population of León, Guanajuato, Mexico: one-third of the children with a normal IQ (33.3%) and another third (36.1%) had a mild to severe disability (Fombonne et al. 2016). To mention another study, Esler and Hall-Lande (2017) made a comparison of this variable between different ethnic groups of children, and they observed some differences between Hispanics, Whites, Somali Blacks, and Non-Somali Blacks. In spite of these findings, the group sizes were too small to obtain truly meaningful values. Nonetheless, it can be observed that the frequencies found in that study do not differ significantly from those identified in this research.
Following this study’s findings, when the IQ was analyzed by ASD subtype, it was observed that the highest proportion of children have a normal IQ in the Level 1 group, where even a small percentage with an IQ above average was recognized. These findings were not observed in Levels 2 and 3. In Level 3, however, a large percentage (77.77%) of children with some mild to moderate intellectual disability was very evident. These data corroborate the results by Mayes and Calhoun (2011).
The severity of ASD in the sample of this study was clearly associated with IQ (X2 = 90.04; p < 0.0001), a result that confirms the one obtained by Fombonne et al. (2016) in another Mexican pediatric population (X2 = 11.65; df = 2; p = 0.003).
Conclusions
ASD is a global health problem with its prevalence increasing in recent years and its average age of diagnosis remaining high. The diagnostic delay entails that there are children who may not receive the help they need in time for a favorable prognosis. To date, several studies agree that there is a real increase in the number of ASD cases regardless of the improvement in diagnosis, which opens possibilities for new lines of research in order to identify the factors that are influencing such an increase. Likewise, the causes of why ASD is more frequent in men than in women remain to be clarified. In addition, cohort studies with larger samples are needed to conclude how labor complications, low birth weight, and advanced parental age at conception, among other clinical and sociodemographic characteristics, are associated with the development of this condition. Finally, both an early diagnosis and analysis of intellectual capacity are two key elements in determining children’s overall functioning, and in the aim of having a more precise impact on the child’s development through an appropriate and comprehensive intervention—in accordance with his or her characteristics and level of severity.
In this study, as can be directly observed in the Tables, more Level-2 cases than Level-1 cases were found. The authors of this research hypothesize that the reason behind this finding is not that there are fewer Level-1 cases, but that it is possible that a large proportion of them are not diagnosed, which is yet another reason for extensive screening studies in the general population.
References
American College of Obstetricians and Gynecologists. (2013). Committee opinion no. 559: Cesarean delivery on maternal request. Obstetrics and Gynecology, 121, 904. https://doi.org/10.1097/01.aog.0000428647.67925.d3.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: American Psychiatric Association.
Anderson, G. M., Scahill, L., McCracken, J. T., McDougle, C. J., Aman, M. G., Tierney, E., et al. (2007). Effects of short-and long-term risperidone treatment on prolactin levels in children with autism. Biological Psychiatry, 61, 545–550.
Bitsika, V., Arnold, W. M., & Sharpley, C. F. (2018). Cluster analysis of autism spectrum disorder symptomatology: Qualitatively distinct subtypes or quantitative degrees of severity of a single disorder? Research in Developmental Disabilities, 76, 65–75. https://doi.org/10.1016/j.ridd.2018.03.006.
Black, M. H., Chen, N. T. M., Iyer, K. K., Lipp, O. V., Bölte, S., Falkmer, M., et al. (2017). Mechanisms of facial emotion recognition in autism spectrum disorders: Insights from eye tracking and electroencephalography. Neuroscience and Biobehavioral Reviews. https://doi.org/10.1016/j.neubiorev.2017.06.016.
Buescher, A. V., Cidav, Z., Knapp, M., & Mandell, D. S. (2014). Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics. https://doi.org/10.1001/jamapediatrics.2014.210.
Burstyn, I., Sithole, F., & Zwaigenbaum, L. (2010). Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Disease in Canada, 30(4), 125–134.
Carayol, J., Schellenberg, G. D., Dombroski, B., Genin, E., Rousseau, F., & Dawson, G. (2011). Autism risk assessment in siblings of affected children using sex-specific genetic scores. Molecular Autism. https://doi.org/10.1186/2040-2392-2-17.
Centers for Disease Control and Prevention (CDC); Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators. (2014). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveillance Summaries, 63(2), 1–21.
Council on Children with Disabilities; Section on Developmental Behavioral Pediatrics; Bright Futures Steering Committee; Medical Home Initiatives for Children with Special Needs Project Advisory Committee. (2006). Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics. https://doi.org/10.1542/peds.2006-1231.
Curran, E. A., Dalman, C., Kearney, P. M., et al. (2015). Association between obstetric mode of delivery and autism spectrum disorder: A population-based sibling design study. JAMA Psychiatry. https://doi.org/10.1001/jamapsychiatry.2015.0846.
De Giacomo, A., & Fombonne, E. (1998). Parental recognition of developmental abnormalities in autism. European Child and Adolescent Psychiatry, 7(3), 131–136.
Dean, M., Harwood, R., & Kasari, C. (2017). The art of camouflage: Gender differences in the social behaviors of girls and boys with autism spectrum disorder. Autism, 5, 4. https://doi.org/10.1177/1362361316671845.
DiGuiseppi, C. G., Daniels, J. L., Fallin, D. M., Rosenberg, S. A., Schieve, L. A., Thomas, K. C., et al. (2016). Demographic profile of families and children in the study to explore early development (SEED): Case-control study of autism spectrum disorder. Disability and Health Journal. https://doi.org/10.1016/j.dhjo.2016.01.005.
D’Mello, A. M., Moore, D. M., Crocetti, D., Mostofsky, S. H., & Stoodley, C. J. (2016). Cerebellar gray matter differentiates children with early language delay in autism. Autism Research. https://doi.org/10.1002/aur.1622.
Esler, A. N., & Hall-Lande, A. (2017). Phenotypic characteristics of autism spectrum disorder in a diverse sample of somali and other children. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-017-3232-z.
Evans, S. C., Boan, A. D., Bradley, C., & Carpenter, L. A. (2018). Sex/gender differences in screening for autism spectrum disorder: Implications for evidence-based assessment. Journal of Clinical Child & Adolescent Psychology. https://doi.org/10.1080/15374416.2018.1437734.
Ferri, S. L., Abel, T., & Brodkin, E. S. (2018). Sex differences in autism spectrum disorder: A review. Current Psychiatry Reports, 20(2), 9. https://doi.org/10.1007/s11920-018-0874-2.
Fitzpatrick, P., Frazier, J. A., Cochran, D., Mitchell, T., Coleman, C., & Schmidt, R. C. (2018). Relationship between theory of mind, emotion recognition, and social synchrony in adolescents with and without autism. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2018.01337.
Fombonne, E., Marcin, C., Manero, A. C., Bruno, R., Diaz, C., Villalobos, M., et al. (2016). Prevalence of autism spectrum disorders in Guanajuato, Mexico: The Leon survey. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-016-2696-6.
Ganz, M. L. (2007). The lifetime distribution of the incremental societal costs of autism. Archives of Pediatrics and Adolescent Medicine, 161(4), 343–349.
Gardener, H., Spiegelman, D., & Buka, S. L. (2009). Prenatal risk factors for autism: Comprehensive meta-analysis. British Journal of Psychiatry. https://doi.org/10.1192/bjp.bp.108.051672.
Gardener, H., Spiegelman, D., & Buka, S. L. (2011). Perinatal and neonatal risk factors for autism: A comprehensive meta-analysis. Pediatrics. https://doi.org/10.1542/peds.2010-1036.
Glasson, E. J., Bower, C., Petterson, B., et al. (2004). Perinatal factors and the development of autism. Archives of General Psychiatry. https://doi.org/10.1001/archpsyc.61.6.618
Goin-Kochel, R. P., Esler, A. N., Kanne, S. M., & Hus, V. (2014). Developmental regression among children with autism spectrum disorder: Onset, duration, and effects on functional outcomes. Research in Autism Spectrum Disorders. https://doi.org/10.1016/j.rasd.2014.04.002.
Hansen, R. L., Ozonoff, S., Krakowiak, P., Angkustsiri, K., Jones, C., Deprey, L. J., et al. (2008). Regression in autism: Prevalence and associated factors in the CHARGE Study. Ambulatory Pediatrics. https://doi.org/10.1016/j.ambp.2007.08.006.
Harris, S., & Handleman, J. S. (1994). Preschool education programs for children with autism (2nd ed.). Austin: Pro-Ed.
Harrop, C., Jones, D., Zheng, S., Nowell, S., Boyd, B. A., & Sasson, N. (2018). Circumscribed interests and attention in autism: The role of biological sex. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-018-3612-z.
Hartley, S. L., & Sikora, D. M. (2009). Sex differences in autism spectrum disorder: an examination of developmental functioning, autistic symptoms, and coexisting behavior problems in toddlers. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-009-0810-8.
Instituto Nacional de Estadística y Geografía (INEGI). (2015). Dirección General de Estadísticas Económicas. Estadísticas de Salud.
Johnson, C. P., & Myers, S. M. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183–1215.
Jónsdóttir, S. L., Saemundsen, E., Antonsdóttir, I. S., Sigurdardóttir, S., & Ólason, D. (2011). Children diagnosed with autism spectrum disorder before or after the age of 6 years. Research in Autism Spectrum Disorders. https://doi.org/10.1016/j.rasd.2010.03.007.
Kancherla, V., & Dennis, L. K. (2006). A meta-analysis of prenatal, perinatal, and neonatal risks for autism. American Journal of Epidemiology. https://doi.org/10.1093/aje/163.suppl_11.s20-d.
Kern, J. K., Trivedi, M. H., Grannemann, B. D., Garver, C. R., Johnson, D. G., Andrews, A. A., et al. (2007). Sensory correlations in autism. Autism, 11(2), 123–134.
Koehler, L., Fournel, A., Albertowski, K., Roessner, V., Gerber, J., Hummel, C., et al. (2018). Impaired odor perception in autism spectrum disorder is associated with decreased activity in olfactory cortex. Chemical Senses. https://doi.org/10.1093/chemse/bjy051.
Kolevzon, A., Gross, R., & Reichenberg, A. (2007). Prenatal and perinatal risk factors for autism: A review and integration of findings. Archives of Pediatrics and Adolescent Medicine. https://doi.org/10.1001/archpedi.161.4.326.
Kurasawa, S., Tateyama, K., Iwanaga, R., Ohtoshi, T., Nakatani, K., & Yokoi, K. (2018). The age at diagnosis of autism spectrum disorder in children in Japan. International Journal of Pediatrics. https://doi.org/10.1155/2018/5374725.
Lai, M. C., Lombardo, M. V., Ecker, C., Chakrabarti, B., Suckling, J., Bullmore, E. T., et al. (2014). Neuroanatomy of individual differences in language in adult males with autism. Cerebral Cortex. https://doi.org/10.1093/cercor/bhu211.
Langridge, A. T., Glasson, E. J., Nassar, N., et al. (2013). Maternal conditions and perinatal characteristics associated with autism spectrum disorder and intellectual disability. PLoS ONE. https://doi.org/10.1371/journal.pone.0050963.
Loomes, R., Hull, L., & Mandy, W. P. L. (2017). What is the male-tofemale ratio in autism spectrum disorder? A systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry. https://doi.org/10.1016/j.jaac.2017.03.013.
Lord, C., Risi, S., DiLavore, P. S., Shulman, C., Thurm, A., & Pickles, A. (2006). Autism from 2 to 9 years of age. Archives of General Psychiatry, 63(6), 694–701.
Lord, C., Shulman, C., & DiLavore, P. (2004). Regression and word loss in autistic spectrum disorders. Journal of Child Psychology and Psychiatry, 45(5), 936–955.
Loth, E., Garrido, L., Ahmad, J., Watson, E., Duff, A., & Duchaine, B. (2018). Facial expression recognition as a candidate marker for autism spectrum disorder: How frequent and severe are deficits? Molecular Autism. https://doi.org/10.1186/s13229-018-0187-7.
MacKay, D. F., Smith, G. C. S., Dobbie, R., Cooper, S. A., & Pell, J. P. (2013). Obstetric factors and different causes of special educational need: Retrospective cohort study of 407,503 school children. BJOG. https://doi.org/10.1111/1471-0528.12071.
Masi, A., DeMayo, M. M., Glozier, N., & Guastella, A. J. (2017). An overview of autism spectrum disorder, heterogeneity and treatment options. Neuroscience Bulletin. https://doi.org/10.1007/s12264-017-0100-y.
Mayes, S., & Calhoun, S. (2004). Influence of IQ and age in childhood autism: Lack of support for DSM-IV Asperger’s disorder. Journal of Developmental and Physical Disabilities, 16(3), 257–272.
Mayes, S., & Calhoun, S. (2011). Impact of IQ, age, SES, gender and race on autistic symtomps. Research in Autism Spectrum Disorder. https://doi.org/10.1016/j.rasd.2010.09.002.
McCracken, J. T., McGough, J., Shah, B., Cronin, P., Hong, D., Aman, M. G., et al. (2002). Risperidone in children with autism and serious behavioral problems. New England Journal of Medicine. https://doi.org/10.1056/NEJMoa013171.
Miodovnik, A., Harstad, E., Sideridis, G., & Huntington, N. (2015). Timing of the diagnosis of attention-deficit/hyperactivity disorder and autism spectrum disorder. Pediatrics. https://doi.org/10.1542/peds.2015-1502.
Modabbernia, A., Velthorst, E., & Reichenberg, A. (2017). Environmental risk factors for autism: An evidence-based review of systematic reviews and meta-analyses. Molecular Autism. https://doi.org/10.1186/s13229-017-0121-4.
Molnar-Szakacs, I., & Heaton, P. (2012). Music: A unique window into the world of autism. Annals of the New York Academy of Sciences. https://doi.org/10.1111/j.1749-6632.2012.06465.x.
National Institute of Health (NIH). (2007). NIH Funds New Program to Investigate Causes and Treatment of Autism. Retrieved from https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml#part_145441. Accessed 3 Sep 2018.
National Research Council. (2001). Educating children with autism. In C. Lord & J. P. McGee (Eds.), Committee on educational interventions for children with autism. Washington, DC: National Academy Press.
Nieto, C., López, B., & Gandía, H. (2017). Relationships between atypical sensory processing patterns, maladaptive behavior and maternal stress in Spanish Children with autism spectrum disorder. Journal of Intellectual Disability Research. https://doi.org/10.1111/jir.12435.
Peled-Avron, L., & Shamay-Tsoory, S. G. (2017). Don’t touch me! autistic traits modulate early and late ERP components during visual perception of social touch. Autism Research. https://doi.org/10.1002/aur.1762.
Perry, A., Rubinsten, O., Peled, L., & Shamay-Tsoory, S. G. (2013). Don’t stand so close to me: A behavioral and ERP study of preferred interpersonal distance. Neuroimage. https://doi.org/10.1016/j.neuroimage.2013.07.042.
Polo-Kantola, P., Lampi, K. M., Hinkka-Yli-Salomäki, S., Gissler, M., Brown, A. S., & Sourander, A. (2014). Obstetric risk factors and autism spectrum disorders in Finland. Journal of Pediatrics. https://doi.org/10.1016/j.jpeds.2013.09.044.
Pringle, B., Colpe, L. J., Blumberg, S. J., Avila, R. M., & Kogan, M. D. (2012). Diagnostic history and treatment of school-aged children with autism spectrum disorder and special health care needs. NCHS Data Brief, 97, 1–8.
Randall, M., Egberts, K. J., Samtani, A., Scholten, R. J., Hooft, L., Livingstone, N., et al. (2018). Diagnostic tests for autism spectrum disorder (ASD) in preschool children. Cochrane Database Systematic Review, 7, CD009044. https://doi.org/10.1002/14651858.cd009044.pub2.
Rice, C. E., Baio, J., Naarden, Van, Braun, K., Doernberg, N., Meaney, F. J., et al. (2007). A public health collaboration for the surveillance of autism spectrum disorders. Paediatric and Perinatal Epidemiology. https://doi.org/10.1111/j.1365-3016.2007.00801.x.
Rogers, S. J., & Ozonoff, S. (2005). Annotation: What do we know about sensory dysfunction in autism? A critical review of the empirical evidence. Journal of Child Psychology and Psychiatry. https://doi.org/10.1111/j.1469-7610.2005.01431.x.
Rutter, M. (1970). Autistic children: Infancy to adulthood. Semin Psychiatry, 2(4), 435–450.
Rutter, M. (2005). Incidence of autism spectrum disorders: Changes over time and their meaning. Acta Paediatrica, 94(1), 2–15.
Sandin, S., Schendel, D., Magnusson, P., Hultman, C., Surén, P., Susser, E., et al. (2016). Autism risk associated with parental age and with increasing difference in age between the parents. Molecular Psychiatry. https://doi.org/10.1038/mp.2015.70.
Sato, D., Lionel, A. C., Leblond, C. S., Prasad, A., Pinto, D., Walker, S., et al. (2012). SHANK1 deletions in males with autism spectrum disorder. American Journal of Human Genetics. https://doi.org/10.1016/j.ajhg.2012.03.017.
Shah, A., Faundes, A., Machoki, M. I., Bataglia, V., Amokrane, F., Donner, A., et al. (2008). Methodological considerations in implementing the WHO global survey for monitoring maternal and perinatal health. Bulletin of the World Health Organization. https://doi.org/10.2471/blt.06.039842.
Siegel, B. (1998). The world of the autistic child: Understanding and treating autistic spectrum disorders. New York: Oxford University Press.
Shattuck, P. T., Durkin, M., Maenner, M., Newschaffer, C., Mandell, D. S., Wiggins, L., et al. (2009). Timing of identification among children with an autism spectrum disorder: Findings from a population-based surveillance study. Journal of the American Academy of Child and Adolescent Psychiatry. https://doi.org/10.1097/CHI.0b013e31819b3848
Steeb, H., Ramsey, J. M., Guest, P. C., Stocki, P., Cooper, J. D., Rahmoune, H., et al. (2014). Serum proteomic analysis identifies sex-specific differences in lipid metabolism and inflammation profiles in adults diagnosed with Asperger syndrome. Molecular Autism. https://doi.org/10.1186/2040-2392-5-4.
Sun, X., & Allison, C. (2010). A review of the prevalence of autism spectrum disorder in Asia. Research in Autism Spectrum Disorders. https://doi.org/10.1016/j.rasd.2009.10.003.
Thye, M. D., Bednarz, H. M., Herringshaw, A. J., Sartin, E. B., & Kana, R. K. (2018). The impact of atypical sensory processing on social impairments in autism spectrum disorder. Developmental Cognitive Neuroscience. https://doi.org/10.1016/j.dcn.2017.04.010.
Tropeano, M., Ahn, J. W., Dobson, R. J. B., Breen, G., Rucker, J., Dixit, A., et al. (2013). Male-biased autosomal effect of 16p13.11 copy number variation in neurodevelopmental disorders. Liu C, editor. PLoS ONE. https://doi.org/10.1371/journal.pone.0061365.
Tropeano, M., Howley, D., Gazzellone, M. J., Wilson, C. E., Ahn, J. W., Stavropoulos, D. J., et al. (2016). Microduplications at the pseudoautosomal SHOX locus in autism spectrum disorders and related. Journal of Medical Genetics. https://doi.org/10.1136/jmedgenet-2015-103621.
Vázquez-Ramírez. (2017). La atención educativa de los alumnos con Trastorno del Espectro Autista. Instituto de Educación de Aguascalientes, México. Orientación andujar. Retrieved from https://www.educacionespecial.sep.gob.mx/pdf/doctos/2Academicos/13Libro_Autismo.pdf. Accessed 10 Oct 2018.
Vieira, G. O., Fernández, L. G., Oliveira, N. F., de Silva, L. R., & Vieira, T. D. O. (2015). Factors associated with cesarean delivery in public and private hospitals in a city of northeastern Brazil: A cross-sectional study. BMC Pregnancy Childbirth, 15, 132. https://doi.org/10.1186/s12884-015-0570-8.
Vogel, J. P., Betran, A. P., Vindevoghel, N., et al. (2015). Use of the Robson classification to assess cesarean section trends in 21 countries: A secondary analysis of two WHO multicountry surveys. The Lancet Global Health. https://doi.org/10.1016/s2214-109x(15)70094-x.
von Gontard, A., Pirrung, M., & Equit, M. (2015). Incontinence in children with autism spectrum disorder. Journal of Pediatric Urology. https://doi.org/10.1016/j.jpurol.2015.04.015.
Werling, D. M., & Geschwind, D. H. (2013). Sex differences in autism spectrum disorders. Current Opinion in Neurology. https://doi.org/10.1097/WCO.0b013e32835ee548.
Wiggins, L. D., Rice, C. E., & Baio, J. (2009). Developmental regression in children with an autism spectrum disorder identified by a population-based surveillance system. Autism. https://doi.org/10.1177/1362361309105662.
Yip, B. H. K., Leonard, H., Stock, S., Stoltenberg, C., Francis, R. W., Gissler, M., et al. (2017). Cesarean section and risk of autism across gestational age: A multi-national cohort study of 5 million births. International Journal of Epidemiology. https://doi.org/10.1093/ije/dyw336.
Acknowledgments
To MD José Roberto Cárdenas Zavala, Lic. Josue Gabino Jiménez Flores and MAP Israel Adolfo Cuellar Hernández, for facilitating the adequate development of this project through their administrative management.
Author information
Authors and Affiliations
Contributions
TG-C and PR-F contributed to the conception of the project. EG-C, CCR-G, DA-C, MPN-H, and FCL-M contributed to the methodology of the project. CS-G contributed to the data curation. Formal analysis and investigation by TG-C, JH-SC, and PKE-S. Writing—original draft preparation by TG-C, PR-F, and EG-C.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
González-Cortés, T., Gutiérrez-Contreras, E., Espino-Silva, P.K. et al. Clinical Profile of Autism Spectrum Disorder in a Pediatric Population from Northern Mexico. J Autism Dev Disord 49, 4409–4420 (2019). https://doi.org/10.1007/s10803-019-04154-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-019-04154-2