Abstract
We investigated gesture production in infants at high and low risk for autism spectrum disorder (ASD) and caregiver responsiveness between 12 and 24 months of age and assessed the extent to which early gesture predicts later language and ASD outcomes. Participants included 55 high-risk infants, 21 of whom later met criteria for ASD, 34 low-risk infants, and their caregivers. Results indicated that (a) infants with ASD outcomes used fewer gestures and a lower proportion of developmentally advanced gesture–speech combinations; (b) caregivers of all the infants provided similar rates of contingent responses to their infants’ gestures; and (c) gesture production at 12 months predicted subsequent receptive language and ASD outcomes within the high-risk group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deficits in nonverbal communicative behaviors are among the hallmark features of autism spectrum disorder (ASD; American Psychiatric Association 2013). In particular, deficits in gestures, which are hand or body movements that speakers produce as forms of intentional communication, have been well documented in the autism literature. Previous studies suggest that infants with ASD produce significantly fewer gestures than infants without ASD as early as 12–14 months (Landa et al. 2007; Zwaigenbaum et al. 2005; see Manwaring et al. 2018 for review), and that atypicality of gesture usage persists into childhood and adulthood (de Marchena and Eigsti 2010; Morett et al. 2016). Furthermore, a number of prospective studies have examined gesture as a potential early sign in infants with an older sibling with ASD, who are at high familial risk for the disorder (hereafter, “high-risk”; Ozonoff et al. 2011). Significant group differences between high-risk infants and infants with no family history of ASD (hereafter, “low-risk”) have been found in previous studies, with high-risk infants producing fewer gestures, compared to their low-risk peers (Cassel et al. 2007; Goldberg et al. 2005; Leezenbaum et al. 2014; Manwaring et al. 2018; Mitchell et al. 2006; Toth et al. 2007; Yirmiya et al. 2006; Zwaigenbaum et al. 2005).
While the studies that examined risk group differences have been informative in suggesting that gesture may be a risk factor for ASD, these studies do not include information on diagnostic outcomes of the high-risk infants, making it impossible to determine whether the differences between high- and low-risk infants were driven by the subset of high-risk infants who were later diagnosed with ASD. However, research comparing high-risk infants who later developed ASD (HRA+) and unaffected high-risk infants (HRA−) suggests large variability in gesture production within the high-risk group (LeBarton and Iverson 2016; Rozga et al. 2011; Talbott et al. 2015a; Winder et al. 2013; Zwaigenbaum et al. 2005). For example, Rozga et al. (2011) found that HRA+ infants produced fewer pointing and showing gestures than HRA− and low-risk comparison (LRC) infants on a semi-structured assessment at 12 months, whereas there were no significant group differences between HRA− and LRC infants. Similarly, Talbott et al. (2015a) reported that HRA+ infants produced significantly fewer total gestures than HRA− and LRC infants during interactions with mothers or examiners at 12 months, and again, there was no significant group difference between HRA− and LRC infants. More recently, LeBarton and Iverson (2016) found that HRA+ toddlers produced fewer overall gestures than their high-risk peers with language delay or with no diagnosis during interactions with mothers at 24 months. Taken together, these findings highlight the need to go beyond the comparisons between high- and low-risk groups and investigate gesture production in infants based on both risk for ASD and diagnostic outcomes (e.g., HRA+, HRA−, LRC).
Another limitation of prior research is that there has been a predominant emphasis on the amount and types of gestures that high-risk infants produce. Relatively little is known about gestures produced in conjunction with or without speech (Manwaring et al. 2018; Özçalışkan et al. 2017). A comprehensive review by Manwaring et al. (2018) reported that only one of the 19 studies on deictic gestures, which indicate objects, people, or locations in the immediate environment, in toddlers with or at risk for ASD examined gesture paired with speech (hereafter, “gesture–speech combinations”). In particular, Winder et al. (2013) found that high-risk infants integrated deictic gestures with communicative non-word vocalizations at a significantly lower rate, compared to low-risk infants, at 13 and 18 months. A related study that included not only deictic but also other types of gestures found that the trajectory of gesture–speech combinations was significantly slower in HRA+ infants than LRC infants between 8 and 18 months (Parladé and Iverson 2015). Recently, Özçalişkan et al. (2017) found that children with ASD or with Down syndrome produced significantly fewer overall gestures and types of gesture–speech combinations than typically developing children. Together, these studies suggest that gesture–speech combinations have been less explored and merit closer examination in high-risk infants. Investigating gesture–speech combinations may be useful in parsing the variability in early communicative profiles of the high-risk ASD population (Ozonoff et al. 2014; Talbott et al. 2016).
An important question related to group differences in infant gesture production is whether the differences in infants’ gestures affect how their caregivers respond to gestures. For example, high-risk infants who produce fewer gestures than low-risk peers may give fewer opportunities for their caregivers to provide contingent input (Leezenbaum et al. 2014). Alternatively, caregivers of high-risk infants may be even more attuned to their infant’s communicative behaviors and provide more contingent responses, compared to caregivers of low-risk infants (Tager-Flusberg 2016). Leezenbaum et al. (2014) studied maternal responses to gestural and vocal communication in high- and low-risk infants at 13 and 18 months of age and found that maternal response rates did not vary across the two groups. More recently, Dimitrova et al. (2016) reported that parents of children with ASD, children with Down syndrome, and typically developing children provided similar rates of contingent responses to their children’s gestures. Considering the significance of reciprocal influences between child and caregiver communicative behaviors, it is surprising that only a few studies have explored whether the differences in infant gesture influence caregivers’ responsiveness. In the current study, we examined both raw numbers (which measure the absolute quantity of parental responses that infants receive) and proportions (which control for differences in infant gestures) of contingent caregiver responses, which, in turn, may shape children’s language development (Goldin-Meadow et al. 2007; Tamis-LeMonda et al. 2014).
Finally, while the relation between early gesture use and later language is well established in typical development (Acredolo and Goodwyn 1988; Iverson and Goldin-Meadow 2005; Rowe and Goldin-Meadow 2009a; Rowe et al. 2008), this relation has not been extensively studied in high-risk infants. In fact, previous findings have been mixed, with some studies showing positive, significant relations between early gesture and later vocabulary in children with ASD (Braddock et al. 2015; Medeiros and Winsler 2014; Özçalışkan et al. 2016), whereas others reported no significant relations between gesture and language in ASD (So et al. 2015). Examining the relation between gesture and language may be useful in revealing whether such relation holds within the high-risk population and in predicting which infants will have subsequent language difficulties. Thus, exploring whether and to what extent early gesture may be related to later language skills within the high-risk population is warranted.
Similarly, it is of both practical and theoretical relevance to identify factors that may be associated with increased probability of receiving an ASD diagnosis. To date, several studies have identified gesture as an early marker for an eventual ASD diagnosis. For example, through using a developmental surveillance assessment, Barbaro and Dissanayake (2013) reported that pointing gestures were recurring early markers for ASD during the second year of life. Veness, Prior, Eadie, Bavin, and Reilly (2014), using parent reports of infant communicative behaviors, also found that gesture use at 8 months was significantly associated with an ASD diagnosis by 7 years. However, to our knowledge, no study has yet evaluated the predictive power of gesture observed during naturalistic interactions in relation to a later ASD diagnosis.
The Present Study
In light of the background and limitations discussed above, we examined infant production of gestures (with or without speech), caregiver responsiveness to gestures, and relations among gesture, caregiver responsiveness, later language, and/or ASD outcomes in HRA+, HRA−, and LRC families, using detailed coding of videotaped sessions of caregiver-infant interactions. Infant gesture and caregiver responsiveness were examined during naturalistic interactions in the lab at 12, 18, and 24 months. Infants’ language skills were measured using Mullen Scales of Early Learning (MSEL; Mullen 1995) at 24 months, and ASD outcomes were determined using a combination of the Autism Diagnostic Observation Scale (ADOS; Lord et al. 2000) and best clinical judgment between 18 and 36 months. Our specific research questions were as follows:
-
(1)
Do HRA+, HRA−, and LRC infants differ in overall production and distribution of gestures (with or without speech) at 12, 18, and 24 months?
-
(2)
Do caregivers of HRA+, HRA−, and LRC infants differ in immediate, contingent responsiveness to infant gestures (with or without speech) at 12, 18, and 24 months?
-
(3)
Does early gesture or caregiver responsiveness relate to later language skills?
-
(4)
Does early gesture relate to ASD outcomes?
Methods
Participants
A total of 89 infants and their caregivers participated in this study. Participants were drawn from a larger prospective, longitudinal study of infants at high and low familial risk for ASD. For the present study, we included caregiver-infant dyads who participated in a 10-min free play interaction in the lab at least once at 12, 18, or 24 months and had ASD outcomes determined between 18 and 36 months. There were 70 caregiver-infant dyads at 12 and 18 months and 69 dyads at 24 months (Table 1). Of note, sample attrition was due to visits missed by families, malfunction of video recording equipment, and infants becoming fussy and not doing caregiver-infant interactions during visits.
Fifty-five infants were enrolled as high risk for autism (HRA); parents of these infants reported a community diagnosis of ASD in the older siblings (probands) of these infants. To confirm ASD diagnosis of probands of HRA infants, we used the Social Communication Questionnaire (SCQ; Rutter et al. 2003) and/or the ADOS (Lord et al. 2000). Community diagnosis of ASD were confirmed for 52 probands of HRA infants (95% of the HRA sample). Specifically, both the SCQ and ADOS were used to confirm diagnosis in 27 probands of HRA infants (49%); the SCQ was used for 21 probands (38%); and the ADOS was used for four probands (7%). Three probands of HRA infants (5%) did not have the ADOS or SCQ and therefore were unable to have their diagnosis confirmed. However, all three received their diagnosis by expert clinicians in the community, and data from their younger siblings were included in the study.
Thirty-four infants were enrolled as low risk comparison (LRC), as they had typically developing older siblings and no first- or second-degree family members with ASD. To ensure probands of LRC infants did not have ASD, we used the SCQ and/or ADOS. Specifically, both the ADOS and SCQ were used to verify no ASD diagnosis for 29 older siblings of the LRC infants (85% of the LRC sample); the SCQ was used for four probands (12%); and the ADOS was used for one proband (3%).
For the data analyses, infants were classified based on their risk for ASD (high or low) and also eventual ASD outcomes (ASD or no ASD; see the section “ASD outcome classification”). Of the 55 high-risk infants, 21 were later diagnosed with ASD (HRA+), and 34 were not diagnosed with ASD (HRA−). Notably, we oversampled high-risk infants who later met criteria for ASD to ensure their sufficient representation in the present study. All 34 low-risk infants were not later diagnosed with ASD.
Infant and caregiver characteristics are provided in Table 1 for the three groups. While the groups were comparable in infant race and household income, infant sex and caregiver education differed significantly across the groups. Specifically, the percentage of female infants was significantly lower in the HRA+ group than the HRA− group, p = 0.013. Also, the level of parental education was significantly lower in the HRA+ group than the LRC group, z = − 3.354, p < 0.001. These variables were controlled for in data analyses. All infants were recruited before 12 months of age, were full-term, and had no genetic or neurological disorders. All caregivers spoke English in the home as the primary language (> 80% of the time).
Procedure and Measures
We obtained Institutional Review Board approvals from Boston Children’s Hospital and Boston University and written, informed consent from caregivers of all infants.
Caregiver-Infant Interaction Footnote 1
At 12, 18, and 24 months of age, caregiver-infant dyads were videotaped while engaging in free play in the lab for 10 min. Dyads were instructed to play as they would normally do at home. Age-appropriate toys were provided.
ASD Outcome Classification
At the infant’s final visit to the lab, which occurred either at 18, 24, or 36 months, a final ASD diagnosis (+/−) was determined on the basis of the ADOS (Lord et al. 2000) and with clinical judgment by a licensed clinical psychologist. The ADOS was administered by research staff with extensive experience in testing children with developmental disorders and co-scored by an ADOS-reliable researcher via recording. If infants met criteria for ASD or received a score within three points of the cutoff scores on the ADOS, a licensed clinical psychologist reviewed videos of the behavioral assessments along with the ADOS scores and determined final clinical judgment: ASD, no ASD, or other (e.g., ADHD, anxiety, language concerns). For the purposes of the current study, we excluded infants who were classified as ‘other.’ If there were multiple diagnostic evaluations at 18, 24, and 36 months (e.g., children completed all visits at three time points), we used information from their most recent visit for ultimate categorization. ASD evaluation was made at 18 months for four children (nHRA+ = 3; nHRA− = 1; nLRC = 0), at 24 months for ten children (nHRA+ = 2; nHRA− = 8; nLRC = 0), and 36 months for 75 children (nHRA+ = 16; nHRA− = 25; nLRC = 34). Given the high diagnostic stability of ASD at 18 and 24 months (Ozonoff et al. 2015; Zwaigenbaum et al. 2016), infants with ASD diagnosis made between 18 and 36 months were included in the present study to maximize sample size.
Language Outcomes
At age 24 months, children were administered the MSEL (Mullen 1995). We used children’s standardized t-scores from the MSEL Receptive and Expressive Language subscales as our measures of children’s language outcomes. We chose the MSEL as our language measure, as it is standardized and independent of our gesture and speech production measures from naturalistic interactions.
Control Variables
Because one of our research goals was to examine relations between early gesture and subsequent language skills, we controlled for several variables such as nonverbal cognition (measured from 12-month MSEL Nonverbal Developmental Quotient), infant sex, and parent education, which have all been reported to be associated with children’s gestural or language skills (Hoff 2003; Özçalişkan and Goldin-Meadow 2010; Wray et al. 2016). In addition, we controlled for infants’ 12-month number of different words (from caregiver-infant interactions) and language skills (from the MSEL Verbal Developmental Quotients, which reflect infants’ performance on the MSEL Receptive and Expressive Language subscales) in our analyses to study relations between 12-month gestures and ASD outcomes.
Transcription and Coding
Speech
Speech from the videotaped sessions were transcribed using the CHAT (Codes for the Human Analysis of Transcripts) conventions of the CHILDES (Child Language Data Exchange System; MacWhinney 2000) and verified by two trained research assistants. Following prior work (Pan et al. 2005), speech was transcribed at the level of utterance, which was defined as a sequence of speech that is preceded and followed by a pause, a change in conversational turn, or a change in intonational pattern. Consistent with previous work (Parladé and Iverson 2015), we classified infant vocal utterances into words and communicative non-word vocalizations (e.g., babbling). Dictionary words, onomatopoetic sounds (e.g., “meow”), and evaluative sounds (e.g., “uh-oh”) were counted as words. The number of different words (word types) infants produced during the 10-min interaction served as a measure of productive vocabulary. Vegetative noises, laughter, crying, and other non-speech sounds were not coded.
Infant Gesture
Occurrences of the infants’ gestures were identified and coded to indicate gesture categories and their relation to speech, following earlier work (Özçalışkan and Goldin-Meadow 2009). Specifically, we classified gestures into one of three main categories: deictic, conventional, or representational. Deictic gestures indicate objects, people, or locations in the environment (e.g., pointing, reaching, showing, giving). Conventional gestures are culturally-agreed-upon hand or body movements with a specific meaning (e.g., nodding the head to convey yes). Representational gestures indicate objects, actions, or relations by recreating an aspect of the referent’s shape or movement (e.g., flapping arms in the air to mean flying).
In addition, we coded whether gesture occurred on its own or combined with speech. When gesture occurred with speech, it was first determined whether it occurred with a word or a communicative non-word vocalization. When gesture occurred with a word, it was categorized as reinforcing, supplementary, or disambiguating (e.g., Özçalışkan et al. 2017). Reinforcing gesture–speech combinations provide the same information in both gesture and speech (e.g., pointing to cookie + “cookie”). In supplementary gesture–speech combinations, gesture adds semantic information to the message conveyed in speech (e.g., showing a book + “open”). In disambiguating gesture–speech combinations, gesture clarifies the message conveyed in speech (e.g., pointing to book + “this”).
Gesture coding reliability was assessed regularly between two coders. Approximately 20% of the transcripts (n = 45) were randomly selected and double coded to calculate interrater agreement. Percent agreement and Cohen’s kappa were calculated for each gesture category: deictic (99.7%, k = 0.996, n = 336), conventional (95.4%, k = 0.941, n = 86), and representational (80.0%, k = 0.762, n = 5). Percent agreement and Cohen’s kappa were also calculated for classifying gesture based upon its relation to accompanying speech: gestures alone (93.5%, k = 0.934, n = 155), gestures with nonword vocalizations (93.8%, k = 0.935, n = 81), reinforcing combinations (91.5%, k = 0.905, n = 94), supplementary combinations (88.7%, k = 0.875, n = 62), and disambiguating combinations (81.0%, k = 0.769, n = 21).
Caregiver Responsiveness
Immediate responses by the caregiver to the gestures were coded as contingent or noncontingent. Specifically, if a parent’s verbal or nonverbal behavior was related to the infant’s gesture and was produced within the first utterance following the gesture, the response was coded as contingent (e.g., an infant points to a ball, and a parent says “Do you want the ball?”). If a parent produced no response or a response that was unrelated to the infant’s gesture within the first utterance following the gesture, the response was coded as noncontingent (e.g., an infant points to a ball, and a parent redirects the infant’s attention and says “Let’s do this puzzle”). Both raw numbers and proportions of contingent parental responses were calculated. Approximately 15% of the transcripts (n = 33) were double coded to assess interrater agreement (97.5%, k = 0.960, n = 326).
Data Analysis
To address our first research question about group differences in infant production of gesture with or without speech, we converted all gesture variables from frequency to rates per 10 min, as the lengths of the interactions varied across caregiver-infant pairs (M = 9.4 min, SD = 2.2)Footnote 2. Visual examination of the gesture variables showed non-normal distributions of data. Therefore, we employed non-parametric analyses (Kruskal-Wallis H tests) to examine early gesture production in three groups of infants. Mann-Whitney U tests were used as post-hoc pairwise comparison tests. Regarding our second research question about group differences in caregiver responsiveness to the gestures, we calculated frequencies and proportions of contingent caregiver responses to infant gestures. Proportions were calculated for each infant by dividing the total number of contingent responses to gestures by total responses to gestures and then averaged across infants in each group. As these data were proportional, we applied an arcsine transformation to data and compared group differences in caregiver responsiveness using non-parametric analyses (Kruskal-Wallis H tests). Finally, regarding our third and fourth research questions, we performed correlation and/or regression analyses to determine whether early gesture use and caregiver responsiveness were related to later language skills, and whether early gesture was predictive of ASD diagnosis. We conducted all statistical analyses using Stata 14 (StataCorp 2015).
Results
Gesture Production from 12 to 24 Months
Total Number of Gestures
We first investigated a total number of gestures that HRA+, HRA−, and LRC infants produced at 12, 18, and 24 months (Table 2). We found that there were significant group differences in the overall amount of gesturing at 12 months, χ2(2, N = 70) = 9.46, p = 0.009, and 18 months, χ2(2, N = 70) = 7.86, p = 0.020, but not at 24 months. Post-hoc pairwise comparisons revealed that at 12 months, HRA− infants produced significantly more total gestures than HRA+ infants, U = 106, z = − 2.73, p = 0.006, d = 0.9, and than LRC infants, U = 226, z = 2.21, p = 0.027, d = 0.4. At 18 months, LRC infants produced significantly more gestures, compared to both HRA+ infants, U = 142, z = − 2.13, p = 0.033, d = 0.7, and to HRA− infants, U = 217.5, z = − 2.52, p = 0.012, d = 0.6. All other group differences were not statistically significant at 12 and 18 months.
Number of Gestures Produced With or Without Speech
We next broke down the total number of gestures and examined gestures produced with or without speech (Table 2). When examining the number of gestures produced with speech, we found that the three groups differed significantly at 12 months, χ2(2, N = 70) = 6.50, p = 0.038, and 18 months, χ2(2, N = 70) = 9.64, p = 0.008, but not at 24 months. Specifically, at 12 months, HRA− infants produced a significantly larger number of gesture–speech combinations than HRA+ infants, U = 117, z = − 2.48, p = 0.013, d = 0.6. LRC infants showed a trend toward more gesture–speech combinations than HRA+ infants, U = 163, z = − 1.82, p = 0.070, d = 0.4. At 18 months, LRC infants produced a significantly larger number of combinations than HRA+ infants, U = 124, z = − 2.56, p = 0.010, d = 0.7, and than HRA− infants, U = 214, z = − 2.58, p = 0.010, d = 0.7. When comparing the number of gestures produced without speech, the three groups differed significantly only at 12 months, χ2(2) = 8.73, p = 0.013. Post-hoc pairwise comparisons revealed that HRA− infants produced significantly more gestures than HRA+ infants, U = 111.5, z = − 2.59, p = 0.010, d = 0.7, and than LRC infants, U = 220, z = 2.32, p = 0.021, d = 0.6.
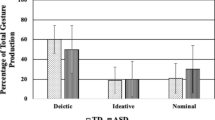
Distribution of Gesture Categories
We examined the distribution of gesture categories (Table 3). The majority of gestures that infants produced at all three ages were deictic gestures, with averages of 86% in HRA+ infants, 83% in HRA− infants, and 86% in LRC infants, across the ages. Infants also produced conventional gestures, with averages of 14% in HRA+ infants, 17% in HRA− infants, and 13% in LRC infants, across the ages. There were almost no representational gestures in our infant data. Specifically, at 24 months only 1% of gestures were coded in the representational category for HRA− and LRC infants. In sum, at all three ages, there was no significant group difference in the proportion of gestures belonging to each category.
Distribution of Types of Gesture–Speech Combinations
We also investigated the distribution of types of gesture–speech combinations (Table 4). At 12 months, there was no significant group difference in the distribution of types of gesture–speech combinations. Most of the gesture–speech combinations that infants produced at 12 months were gestures with non-word vocalizations, with averages of 98% in HRA+ infants, 93% in HRA− infants, and 96% in LRC infants. At 18 months, there was a trend toward significant group difference in reinforcing types, χ2(2, N = 62) = 5.75, p = 0.057, with HRA− and LRC infants producing 21% and 22% reinforcing types, respectively, compared to 8% in HRA+ infants. At 24 months, there was a significant group difference in disambiguating types, χ2(2, N = 68) = 6.70, p = 0.035. Again, HRA− infants and LRC infants produced a significantly higher proportion of disambiguating types, compared to HRA+ infants, U = 109.5, z = − 2.29, p = 0.022, d = 0.4; U = 118.5, z = − 2.42, p = 0.015, d = 0.5, respectively.
Contingent Caregiver Responses to Gestures
Descriptive information on the raw numbers and proportions of contingent caregiver responses is presented in Table 5. Similar to our findings with infant gestures, we found group differences in the number of contingent caregiver responses at 12 and 18 months, but not at 24 months. Specifically, there was a significant group difference at 12 months, χ2(2, N = 70) = 5.98, p = 0.050, and a significant group difference at 18 months, χ2(2, N = 66) = 6.44, p = 0.040. Post-hoc pairwise comparisons revealed that at 12 months, HRA+ caregivers provided significantly fewer contingent responses to infant gestures than HRA− caregivers, U = 118.5, z = − 2.42, p = 0.016, d = − 0.8. At 18 months, HRA+ caregivers made significantly fewer contingent responses than LRC caregivers, U = 129.5, z = − 2.19, p = 0.029, d = − 0.7; HRA− caregivers also provided fewer contingent responses relative to LRC parents, U = 217.5, z = − 1.94, p = 0.053, d = − 0.5.
When examining the proportions of contingent caregiver responses that control for the differences in infant gestures, we found that caregivers of the three groups of children did not differ in the proportions of contingent responses: 12 months: χ2(2, N = 70) = 0.07, p = 0.965; 18 months: χ2(2, N = 66) = 0.91, p = 0.634; 24 months: χ2(2, N = 68) = 2.85, p = 0.240. Also, caregivers of the three groups showed high response rates to child gestures, ranging from 82 to 91% across all ages.
Relations Between Early Gesture, Caregiver Responsiveness, and Later Language Skills
Demographic data for the sample included in the correlation and regression analyses are presented in Table 6. We first examined descriptive information on MSEL standardized t-scores and found significant group differences in 24-month receptive and expressive language scores (Table 7). The total number of gestures at 12 months was significantly and positively correlated with receptive language scores at 24 months, r = 0.256, p = 0.039, but not with expressive language scores at 24 months, r = 0.226, p = 0.070. The number of word types infants produced at 12 months was not significantly correlated with receptive or expressive language scores at 24 months, r = − .072, p = 0.572; r = 0.075, p = 0.553, respectively, presumably because there was little variation in the number of word types infants produced at 12 months.
Given the results of these correlational analyses on early gesture, word types, and MSEL language outcomes, we used linear regression models to investigate whether early gesture predicted later receptive language skills (Table 8). Model 1 in Table 8 indicates that the total number of gestures at 12 months on its own significantly positively predicted receptive language scores at 24 months, b = 0.30, t(63) = 2.11, p = 0.039, 95% CI [0.02, 0.58]. We then included the number of word types produced at 12 months in the regression model to control for early speech and found that gesture at 12 months continued to significantly predict 24-month receptive language skills, even after controlling for the number of different words (Table 8, Model 2), b = 0.39, t(62) = 2.58, p = 0.012, 95% CI [0.09, 0.70]. This significant relation between gesture and language continued to hold when we added an infant’s risk status for autism (Table 8, Model 3), b = 0.39, t(61) = 2.66, p = 0.010, 95% CI [0.10, 0.69]. Notably, risk status was also a significant predictor in Model 3 such that high-risk status was associated with lower receptive language scores, while controlling for the other variables, b = − 5.12, t(61) = − 2.41, p = 0.019, 95% CI [− 9.38, − 0.87]. When we included 12-month nonverbal cognition and demographic covariates (i.e., infant sex and caregiver education), gesture remained a significant positive predictor of later language (Table 8, Model 4), b = 0.29, t(51) = 2.06, p = 0.044, 95% CI [0.08, 0.58], and risk status was a marginal negative predictor of later language, b = − 4.30, t(51) = − 1.86, p = 0.069, 95% CI [− 8.95, 0.34]. In short, 12-month gesture was related to 24-month receptive language, even with risk status controlled (and vice versa, although to a lesser extent). Finally, we added an interaction term between gesture and group (not shown) and found no significant interaction effect, suggesting that the gesture–language relation was similar across risk status groups. Taken together, controlling for 12-month language, risk status, nonverbal cognition, and demographic covariates, gesture use at 12 months was a significant positive predictor of Mullen receptive language scores at 24 months in infants.
In the next step, we examined whether the relation we found between early gesture and language skills was driven by caregiver responsiveness. We found that the relation between the number of contingent parent responses and children’s receptive language scores was positive and significant, r = 0.305, p = 0.014. However, this relation was no longer significant when controlling for the number of infant gestures, r = 0.179, p = 0.158. Similarly, the relation between the proportion of contingent parent responses and children’s receptive language scores was weak and not statistically significant, r = 0.077, p = 0.542.
Relation Between Early Gesture and ASD Diagnosis
Finally, we conducted binomial logistic regression analyses to determine whether early gesture use predicted eventual ASD diagnosis among high-risk infants (Table 9). We found that the number of gestures at 12 months was significantly negatively related to autism diagnosis (Table 9, Model 1), z = − 2.46, p = 0.014, 95% CI [− 0.256, − 0.029], suggesting that higher gesture use was associated with a lower probability of receiving an ASD diagnosis in high-risk infants. Early gesture remained a significant predictor of an ASD diagnosis when we controlled for infants’ 12-month word types (Table 9, Model 2), z = − 2.63 p = 0.008, 95% CI [− 0.294, − 0.043]; the same pattern of results emerged when we controlled for infants’ 12-month MSEL Verbal Developmental Quotients (Table 9, Model 3), z = − 1.92, p = 0.055, 95% CI [− 0.238, 0.002], although the effect of gesture was trending towards significant when standardized language scores were included in the model. Finally, the results held when we added infant sex and caregiver education (Table 9, Model 4), z = − 2.26, p = 0.024, 95% CI [− 0.311, − 0.022]. To interpret this significant finding, we used the regression equation from the final model (Table 9, Model 4) and calculated estimated probabilities of receiving an ASD diagnosis for a high-risk male infant whose 12-month gesture use was at the 10th percentile of the sample and a child whose gesture use was at the 90th percentile, holding their word types and caregivers’ education constant at the sample mean (see Supplementary Material for calculations). We found that for a high-risk boy whose gesture use was at the 10th percentile, the probability of receiving an ASD diagnosis was 83.6%, whereas for a boy at the 90th percentile, the probability was 17.4%, holding word types and parental education constant. Therefore, higher gesture use at 12 months was associated with a lower probability of an ASD diagnosis in high-risk infants.Footnote 3
Discussion
In this study on early gesture in high-risk infants, we had three main findings. First, we found group differences in gesture production in high-risk infants later diagnosed with ASD, high-risk infants without ASD diagnosis, and low-risk infants at 12 and 18 months of age. Second, the differences in infant gesture did not alter responsiveness of caregivers of three infant groups, with caregivers of all three groups providing similar, high rates of contingent responses to infant gestures. Third, gesture use at 12 months was a significant predictor of infants’ later receptive language skills and ASD diagnosis. Below we discuss each of these main findings.
Infant Gesture Production
We found that infants in the three groups showed differences in total amount of gesture production at 12 and 18 months. Specifically, at 12 months, high-risk infants later diagnosed with ASD and low-risk infants produced significantly fewer gestures, on average, than high-risk infants who did not develop ASD. Higher gesture production of high-risk infants without ASD, compared to that of low-risk infants, was somewhat unexpected, considering prior work that suggests lower gesture use in high-risk infants than in low-risk infants (e.g., Cassel et al. 2007). This difference could reflect the heterogeneity in early communicative profiles among high-risk infants (Ozonoff et al. 2014; Talbott et al. 2016). It is also possible that higher infant gesture production in high-risk infants without ASD may be due, in part, to higher gesture use in their mothers, as a positive relation between child and parent gesture has been reported in the literature (Iverson et al. 1999; Rowe et al. 2008). In fact, drawing on a subsample of the 12-month-old infants in this study, Talbott et al. (2015a) found that mothers of unaffected high-risk infants produced significantly more total gestures than mothers of low-risk infants.
At 18 months, high-risk infants with and without ASD produced significantly fewer gestures than low-risk infants. This finding is consistent with prior work that reported deficits in gesture production in high-risk infants (Cassel et al. 2007; Goldberg et al. 2005; Mitchell et al. 2006; Yirmiya et al. 2006). Notably, unaffected high-risk infants showed reduction in gesture production between 12 and 18 months, producing six fewer gestures, on average, at 18 months (Table 2). This substantial within-group variability may, again, highlight the heterogeneous profiles in early communicative skills of high-risk infants. Alternatively, this finding could suggest an atypical pattern of gesture development in unaffected high-risk infants, even though they did not eventually develop ASD. Taking the findings at 12 and 18 months together, there were significant differences in total gesture production among the three groups. Thus, these results suggest the need to go beyond the risk group comparisons, when possible, to study the specificity and generalizability of risk factors for ASD (Jones et al. 2014). Future studies may examine early communicative development of populations at risk for other neurodevelopmental disorders and infants at risk for ASD based on other definitions of risk (e.g., prematurity) and compare their development to that of high-risk infant siblings to address the issue of specificity.
While we found group differences in early gesture at 12 and 18 months, there was no group difference in overall gesture production at 24 months. This might be because typically developing children begin to reduce their gesture use and communicate using words around 2 years of age (Özçalışkan and Goldin-Meadow 2009), whereas children with ASD may not yet replace gestures with words. While our findings are in line with several studies that used semi-structured assessments or parent report measures to study gesture in high-risk infants (Goldberg et al. 2005; Mitchell et al. 2006), they conflict with other previous findings that found group differences at 24 months (LeBarton and Iverson 2016; Rozga et al. 2011). For example, LeBarton and Iverson (2016) reported that high-risk infants with ASD produced significantly fewer gestures than high-risk infants without ASD at 24 months (but not at 36 months) using a similar naturalistic observation method as the current study. The difference in findings may be attributed to methodological differences. For instance, the ASD diagnostic process was not the same between LeBarton and Iverson (2016) and the present study. Specifically, children’s diagnostic outcomes were made at 36 months in LeBarton and Iverson (2016), whereas diagnostic outcomes were made at 18, 24, or 36 months, possibly leading to a less conservative sample in the current study. The difference could also be attributed to the fact that most of our high-risk infants came from relatively high socioeconomic families (Table 1) and ultimately had language scores within one standard deviation of the population mean (Table 7). Given the mixed findings in the infant sibling literature, future studies need to further explore the heterogeneity in early gesture production among high-risk infants using more diverse and larger longitudinal samples to depict a comprehensive picture of the developmental trajectory of gesture in high-risk infants.
When we broke down the total number of gestures into the number of gestures produced with or without speech, we found that at 12 months, the ASD outcome group integrated gestures with speech significantly less than high-risk infants without ASD diagnosis. At 18 months, the two high-risk groups produced a significantly fewer number of gesture–speech combinations, compared to low-risk infants. Similar to these findings, previous studies have reported that the ability to combine different communicative behaviors, such as gestures and vocalizations, might be impaired in high-risk infants, especially those who eventually receive an ASD diagnosis, in the first 2 years of life (Parladé and Iverson 2015; Winder et al. 2013). When examining the number of gestures produced without speech, we found group differences only at 12 months, with high-risk infants with ASD and low-risk infants producing significantly fewer gestures alone than high-risk infants without ASD. As discussed above, this finding might be due in part to higher gesture production in caregivers of high-risk infants without ASD (Talbott et al. 2015a), which might have led to higher gesture production in their infants. Taken together, fewer gesture–speech combinations and gestures alone indicate that infants who later developed ASD communicated significantly less using gestures with their caregivers at 12 and 18 months than their typically developing peers.
After examining the quantity of gesture produced by infants, we examined the distribution of gesture categories each group produced. Consistent with prior literature (Özçalışkan et al. 2017), infants diagnosed with ASD did not differ in their proportional use of gesture categories from infants with no diagnosis. That is, infants of all three groups produced mostly deictic gestures between 12 and 24 months of age. The proportions of conventional and representational gestures were also comparable across the groups at three ages. Özçalışkan et al. (2017) suggested that the complexity of gestural representation may account for similar rates of different gesture categories across groups. For example, because a deictic gesture has a clearer mapping to its referent (e.g., pointing to a ball to indicate ball) and is less cognitively demanding to produce than a representational gesture (e.g., flapping arms to convey flying), young children may be more likely to produce deictic gestures than other gesture categories (see Özçalışkan et al. 2017 for detailed discussion). In summary, while we found group differences in the quantity of gestures, there was no qualitative difference in the distribution of gesture categories across the three groups. Notably, our coding of gesture categories (deictic, conventional, representational) is consistent with that of other studies (e.g., Rowe et al. 2008), but there are differences in how gestures are categorized in the extant literature. For example, Özçalışkan et al. (2017) distinguish giving gestures from deictic gestures, while the current study coded giving gestures as part of deictic gestures. Consistent and detailed coding of gestures in future studies can further refine our understanding of how groups resemble or differ from each other in their use of gestures.
Turning to the distribution of types of gesture–speech combinations, we found group differences at 18 and 24 months. At 12 months, all three groups produced a greater proportion of gestures with non-word vocalizations than other types, presumably because most children around this age do not have words yet and therefore depend on gestures and vocalizations to communicate (e.g., Winder et al. 2013). Compared to high- and low-risk infants without ASD, high-risk infants later diagnosed with ASD showed a trend toward a smaller proportion of reinforcing types and a significantly smaller proportion of disambiguating types at 18 and 24 months, respectively. This finding—high-risk infants with ASD producing a relatively lower proportion of developmentally advanced gesture–speech combinations than their peers with no ASD—suggests that infants with ASD might not have been advancing as quickly as nondiagnosed infants in the way that they combined gestures with words. In contrast, there was no significant group difference in the proportion of supplementary types at three ages. One possibility for the non-significant difference in supplementary types, in particular, is that the ability to convey a sentence-like meaning or create a two-unit construction through a supplementary type (e.g., point to cookie + “eat”) may be equally variable or challenging for all groups, whereas reinforcing types (e.g., point to cookie + “cookie”) and disambiguating types (e.g., point to cookie + “that”) do not require a two-unit construction and may be easier to produce. Of note, it is important to highlight that our sample size is relatively small (although the number of HRA+ infants is larger than most infant sibling studies) and thus limits our ability to draw definitive conclusions. Also, a 10-min interaction might be too short a time period in which to capture children’s use of different types of gesture–speech combinations. Hence, future research investigating specific types of gesture–speech combinations, using longer sampling of child communicative behaviors, could be informative in deepening our understanding of the development of gesture–speech integration in high-risk infants.
Caregiver Responsiveness to Infant Gesture
Given significant differences in early gesture profiles of infant groups, we sought to examine whether differences in infant gesture use affected immediate, contingent caregiver responsiveness to the gestures. As expected, there was a significant group difference in the total number of contingent responses that parents provided to their infants’ gestures. That is, because high-risk infants with ASD gestured significantly less than their peers at 12 and 18 months, caregivers of high-risk infants with ASD consequently had fewer opportunities to provide contingent input to the infants’ gestures. In other words, the differences in the sheer number of parental contingent responses were driven by the differences in the number of infant gestures. By implication, fewer infant gestures inherently limit the number of chances for parents to respond, which, in turn, may have cascading effects on children’s language development (Leezenbaum et al. 2014). However, when we controlled for the differences in infant gestures and compared the response rates, we found that caregivers of all three groups provided high and comparable proportions of contingent responses to gestures—a pattern consistent with prior work (Dimitrova et al. 2016; Leezenbaum et al. 2014). Also, the proportions of contingent responses did not change with age, suggesting that parental responsiveness was high and stable over time in all three groups. These findings add to the broader literature that suggests minimal differences between mothers of high- and low-risk infants in response rates to their infant’s communicative behaviors and play during dyadic interactions (Campbell et al. 2015; Leezenbaum et al. 2014; Talbott et al. 2016).
Early Gesture is Associated with Language and ASD Outcomes
Consistent with prior research (Rowe et al. 2008; Sauer et al. 2010), we found that early gesture predicted later receptive language skills, even after controlling for covariates, in both typical and atypical development (Table 8). Our finding that 12-month gesture predicted later receptive language over and above 12-month word types suggests that early gesture may be a more sensitive indicator of potential language difficulties than early productive vocabulary (see also Rowe and Goldin-Meadow 2009b). One possibility for the significant relation between gesture and receptive language is that infant gesture is related to parent gesture, which, in turn, may direct an infant’s attention to objects and have an impact on child language (Rowe and Goldin-Meadow 2009b).
While we found a significant relation between gesture and later receptive language, we found no such relation between gesture and later expressive language, as indicated by the lack of the significant correlation. Similar to our findings, Manwaring et al. (2017) and O’Neill and Chiat (2015) have reported significant associations between gesture and receptive language, but not expressive language, in children with ASD and children with language delay, respectively. In fact, expressive language skills have been reported to be less impaired than receptive language skills in children with ASD who acquire language before the age of five (Tager-Flusberg 2016; Weismer et al. 2010), which was the case for every child in the current study. Another explanation is that both early gesture use and receptive language skills may reflect an infant’s ability to socially engage and interact with a caregiver or an experimenter and have less to do with language production abilities. A meta-analysis reported a stronger relation between pointing gestures and receptive language than expressive language in typical development (Colonnesi et al. 2010), lending support to this explanation. Given that the implications of a significant relation between early gesture and language outcomes are important in creating targeted interventions, future studies should use experimental manipulation of gesture (e.g., LeBarton et al. 2015) to identify the precise mechanism(s) underlying the effect of gesture on children’s receptive and expressive language skills in both typical and atypical development.
Unlike infant gesture, caregiver responsiveness to infant gesture was not associated with later language skills, when infant gesture was controlled. The fact that we did not find a relation between caregiver responsiveness and children’s subsequent language skills was contrary to our hypothesis based on previous work (Dimitrova et al. 2016; Goldin-Meadow et al. 2007; Leezenbaum et al. 2014; McDuffie and Yoder 2010). However, this finding likely reflects the differences in how responsiveness was defined and coded across the studies. The current study investigated overall responsiveness (i.e., did a caregiver provide an immediate, contingent response to child gesture?), while prior studies have examined specific types of parent verbal responses (e.g., translations, follow-in comments) in relation to child language outcomes. Thus, our follow-up work is currently examining type and modality of caregiver responses to address this limitation, with the goal of studying potential mechanism(s) underlying children’s language-learning process in high-risk infants.
Finally, we found that the total number of gestures at 12 months predicted which high-risk infants would likely receive an ASD diagnosis, even when controlling for early speech or language and demographic covariatesFootnote 4. This replicates previous work that found early gesture use was predictive of ASD outcomes (Chawarska et al. 2014; Colgan et al. 2006; Veness et al. 2014). By implication, careful monitoring of early communicative behaviors such as gestures may be important in differentiating infants who will eventually develop ASD from those who will not. However, it is important to keep in mind that although the effect was significant, it was small, and that gesture alone is not likely to be indicative of eventual ASD outcomes in clinical practice due to low specificity and sensitivity (Luyster et al. 2011). For example, gesture has been found to predict outcomes in other clinical populations (e.g., late talkers; Thal et al. 1991), suggesting that atypicality in early gesture is not specific to ASD. Nevertheless, the current data indicates that early gestural abilities of high-risk infants should be closely monitored by primary care professionals, educators, and caregivers to ensure timely referral for intervention and access to services. Shire et al. (2018) reported that educational professionals could be reliably trained to assess nonverbal communicative skills and set appropriate intervention targets for children with ASD, showing the potential of training for stakeholders to facilitate earlier detection of risks and intervention.
One important limitation of the current study that warrants discussion is that the overall recurrence rate in our larger study was approximately 30%, which is higher than the expected rate reported in the prior literature (e.g., 18.7%; Ozonoff et al. 2011). This might be due to sampling bias; for example, mothers of high-risk infants who were concerned about the infant’s development (e.g., reduced gesture use) might have been more likely to enroll their infant in our study than those of high-risk infants who did not display atypicality in early development. In fact, a previous study using an overlapping sample as the current study found that mothers of high-risk infants reported significantly more concerns about infants’ social communication within the first year of life, compared to mothers of low-risk infants (Talbott et al. 2015b). Considering this issue, our findings on infant gesture production may be biased and may not generalize to the larger population of high-risk infants, especially those who may not show atypicality in gesture use within the first year of life.
Conclusions
In summary, the current study provides a detailed description of gesture production in infants at high and low risk for ASD and caregiver responsiveness in relation to language or ASD outcomes between 12 and 24 months of age. Our findings indicate that low gesture use may be predictive of later developmental outcomes in high-risk infants. By implication, early gesture use should be closely monitored and assessed in high-risk infants to identify those who will have difficulties with language or ASD at a later age. Early identification of those at-risk children can lead to timely access to resources and intervention services that have been shown to promote positive outcomes for our children (Dawson 2008; Kasari et al. 2012).
Notes
Of note, caregiver-infant interactions were also collected at 36 months as part of the larger study; however, recordings from 36-month interactions were not transcribed, as we were primarily interested in studying early gesture production in the first two years of life in relation to later language and ASD outcomes.
There was no group difference in mean lengths of caregiver-infant interaction videos (HRA+: M = 9.21, SD = 1.90; HRA-: M = 9.31, SD = 2.25; LRC: M = 9.77, SD = 2.04).
We conducted a sensitivity analysis in which we removed data from four high-risk infants whose ASD outcomes were determined at 18 months. We found the same results even after we removed data from these infants.
Of note, caregiver education was also significantly and negatively associated with ASD diagnosis, such that infants whose parents had higher levels of education had a lower probability of receiving ASD diagnosis later. This finding, however, contrasts with previous findings that reported a positive association between maternal education and rates of ASD in the United States (e.g., Fountain et al. 2011), and is difficult to interpret considering that we have limited information on potential confounders of parental education and that parents of both HRA + and HRA- infants had relatively high levels of education in the current study (Table 6). Further research may help elucidate potential mechanisms of association between parental education and ASD within a high-socioeconomic sample.
References
Acredolo, L. P., & Goodwyn, S. W. (1988). Symbolic gesturing in normal infants. Child Development, 59, 450–466.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. (5th edn.). Washington, DC: American Psychiatric Association.
Barbaro, J., & Dissanayake, C. (2013). Early markers of autism spectrum disorders in infants and toddlers prospectively identified in the Social Attention and Communication Study. Autism: The International Journal of Research and Practice, 17(1), 64–86. https://doi.org/10.1177/1362361312442597.
Braddock, B. A., Pickett, C., Ezzelgot, J., Sheth, S., Korte-Stroff, E., Loncke, F., & Bock, L. (2015). Potential communicative acts in children with autism spectrum disorders. Developmental Neurorehabilitation, 18(4), 260–271.
Campbell, S. B., Leezenbaum, N. B., Mahoney, A. S., Day, T. N., & Schmidt, E. N. (2015). Social engagement with parents in 11-month-old siblings at high and low genetic risk for autism spectrum disorder. Autism, 19(8), 915–924. https://doi.org/10.1177/1362361314555146.
Cassel, T. D., Messinger, D. S., Ibanez, L. V., Haltigan, J. D., Acosta, S. I., & Buchman, A. C. (2007). Early social and emotional communication in the infant siblings of children with autism spectrum disorders: An examination of the broad phenotype. Journal of Autism and Developmental Disorders, 37(1), 122–132. https://doi.org/10.1007/s10803-006-0337-1.
Chawarska, K., Shic, F., Macari, S., Campbell, D. J., Brian, J., Landa, R., … Bryson, S. (2014). 18-month predictors of later outcomes in younger siblings of children with autism spectrum disorder: A Baby Siblings Research Consortium study. Journal of the American Academy of Child and Adolescent Psychiatry, 53(12), 1317–1327.e1. https://doi.org/10.1016/j.jaac.2014.09.015.
Colgan, S. E., Lanter, E., McComish, C., Watson, L. R., Crais, E. R., & Baranek, G. T. (2006). Analysis of social interaction gestures in infants with autism. Child Neuropsychology, 12(4–5), 307–319. https://doi.org/10.1080/09297040600701360.
Colonnesi, C., Stams, G. J. J. M., Koster, I., & Noom, M. J. (2010). The relation between pointing and language development: A meta-analysis. Developmental Review, 30(4), 352–366. https://doi.org/10.1016/j.dr.2010.10.001.
Dawson, G. (2008). Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology, 20(3), 775–803. https://doi.org/10.1017/S0954579408000370.
de Marchena, A., & Eigsti, I.-M. (2010). Conversational gestures in autism spectrum disorders: Asynchrony but not decreased frequency. Autism Research: Official Journal of the International Society for Autism Research, 3(6), 311–322. https://doi.org/10.1002/aur.159.
Dimitrova, N., Özçalışkan, Ş, & Adamson, L. B. (2016). Parents’ translations of child gesture facilitate word learning in children with autism, Down syndrome and typical development. Journal of Autism and Developmental Disorders, 46(1), 221–231. https://doi.org/10.1007/s10803-015-2566-7.
Fountain, C., King, M. D., & Bearman, P. S. (2011). Age of diagnosis for autism: Individual and community factors across 10 birth cohorts. Journal of Epidemiology and Community Health, 65(6), 503–510. https://doi.org/10.1136/jech.2009.104588.
Goldberg, W. A., Jarvis, K. L., Osann, K., Laulhere, T. M., Straub, C., Thomas, E., … Spence, M. A. (2005). Brief report: Early social communication behaviors in the younger siblings of children with autism. Journal of Autism and Developmental Disorders, 35(5), 657–664. https://doi.org/10.1007/s10803-005-0009-6.
Goldin-Meadow, S., Goodrich, W., Sauer, E., & Iverson, J. (2007). Young children use their hands to tell their mothers what to say. Developmental Science, 10(6), 778–785. https://doi.org/10.1111/j.1467-7687.2007.00636.x.
Gotham, K., Pickles, A., & Lord, C. (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(5), 693–705.
Hoff, E. (2003). The specificity of environmental influence: Socioeconomic status affects early vocabulary development via maternal speech. Child Development, 74(5), 1368–1378.
Iverson, J. M., Capirci, O., Longobardi, E., & Cristina Caselli, M. (1999). Gesturing in mother-child interactions. Cognitive Development, 14(1), 57–75. https://doi.org/10.1016/S0885-2014(99)80018-5.
Iverson, J. M., & Goldin-Meadow, S. (2005). Gesture paves the way for language development. Psychological Science, 16(5), 367–371. https://doi.org/10.1111/j.0956-7976.2005.01542.x.
Jones, E., Gliga, T., Bedford, R., Charman, T., & Johnson, M. H. (2014). Developmental pathways to autism: A review of prospective studies of infants at risk. Neurosci Biobehav Rev., 39, 1–33.
Kasari, C., Gulsrud, A., Freeman, S., Paparella, T., & Hellemann, G. (2012). Longitudinal follow-up of children with autism receiving targeted interventions on joint attention and play. Journal of the American Academy of Child and Adolescent Psychiatry, 51(5), 487–495. https://doi.org/10.1016/j.jaac.2012.02.019.
Landa, R. J., Holman, K. C., & Garrett-Mayer, E. (2007). Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry, 64(7), 853–864. https://doi.org/10.1001/archpsyc.64.7.853.
LeBarton, E. S., Goldin-Meadow, S., & Raudenbush, S. (2015). Experimentally-induced increases in early gesture lead to increases in spoken vocabulary. Journal of Cognition and Development 16(2), 199–220. https://doi.org/10.1080/15248372.2013.858041.
LeBarton, E. S., & Iverson, J. M. (2016). Gesture development in toddlers with an older sibling with autism. International Journal of Language & Communication Disorders, 51(1), 18–30. https://doi.org/10.1111/1460-6984.12180.
Leezenbaum, N. B., Campbell, S. B., Butler, D., & Iverson, J. M. (2014). Maternal verbal responses to communication of infants at low and heightened risk of autism. Autism, 18(6), 694–703. https://doi.org/10.1177/1362361313491327.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Leventhal, B. L., DiLavore, P. C., … Rutter, M. (2000). The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223.
Luyster, R. J., Seery, A., Talbott, M. R., & Tager-Flusberg, H. (2011). Identifying early-risk markers and developmental trajectories for language impairment in neurodevelopmental disorders. Developmental Disabilities Research Reviews, 17(2), 151–159. https://doi.org/10.1002/ddrr.1109.
MacWhinney, B. (2000). The CHILDES project: Tools for analyzing talk. Mahwah: Lawrence Erlbaum Associates.
Manwaring, S. S., Mead, D. L., Swineford, L., & Thurm, A. (2017). Modelling gesture use and early language development in autism spectrum disorder. International Journal of Language & Communication Disorders, 52(5), 637–651. https://doi.org/10.1111/1460-6984.12308.
Manwaring, S. S., Stevens, A. L., Mowdood, A., & Lackey, M. (2018). A scoping review of deictic gesture use in toddlers with or at-risk for autism spectrum disorder. Autism & Developmental Language Impairments, 3, 2396941517751891. https://doi.org/10.1177/2396941517751891.
McDuffie, A., & Yoder, P. (2010). Types of parent verbal responsiveness that predict language in young children with autism spectrum disorder. Journal of Speech, Language, and Hearing Research, 53(4), 1026–1039. https://doi.org/10.1044/1092-4388(2009/09-0023).
Medeiros, K., & Winsler, A. (2014). Parent-child gesture use during problem solving in autistic spectrum disorder. Journal of Autism and Developmental Disorders, 44(8), 1946–1958.
Mitchell, S., Brian, J., Zwaigenbaum, L., Roberts, W., Szatmari, P., Smith, I., & Bryson, S. (2006). Early language and communication development of infants later diagnosed with autism spectrum disorder. Journal of Developmental and Behavioral Pediatrics: JDBP, 27(2 Suppl), 69–78.
Morett, L. M., O’Hearn, K., Luna, B., & Ghuman, A. S. (2016). Altered gesture and speech production in ASD detract from in-person communicative quality. Journal of Autism and Developmental Disorders, 46(3), 998–1012. https://doi.org/10.1007/s10803-015-2645-9.
Mullen, E. M. (1995). Mullen scales of early learning (AGS edition). Circle Pines: American Guidance Service.
O’Neill, H., & Chiat, S. (2015). What our hands say: Exploring gesture use in subgroups of children with language delay. Journal of Speech, Language, and Hearing Research, 58(4), 1319–1325. https://doi.org/10.1044/2015_JSLHR-L-14-0187.
Özçalişkan, S., & Goldin-Meadow, S. (2010). Sex differences in language first appear in gesture. Developmental Science, 13(5), 752–760. https://doi.org/10.1111/j.1467-7687.2009.00933.x.
Özçalışkan, Ş, Adamson, L. B., & Dimitrova, N. (2016). Early deictic but not other gestures predict later vocabulary in both typical development and autism. Autism, 20(6), 754–763. https://doi.org/10.1177/1362361315605921.
Özçalışkan, Ş, Adamson, L. B., Dimitrova, N., & Baumann, S. (2017). Do parents model gestures differently when children’s gestures differ? Journal of Autism and Developmental Disorders, 1–16. https://doi.org/10.1007/s10803-017-3411-y.
Özçalışkan, Ş, & Goldin-Meadow, S. (2009). When gesture–speech combinations do and do not index linguistic change. Language and Cognitive Processes, 24(2), 190. https://doi.org/10.1080/01690960801956911.
Ozonoff, S., Young, G. S., Belding, A., Hill, M., Hill, A., Hutman, T., … Iosif, A.-M. (2014). The broader autism phenotype in infancy: when does it emerge? Journal of the American Academy of Child and Adolescent Psychiatry, 53(4), 398–407.e2. https://doi.org/10.1016/j.jaac.2013.12.020.
Ozonoff, S., Young, G. S., Carter, A., Messinger, D., Yirmiya, N., Zwaigenbaum, L., … Stone, W. L. (2011). Recurrence risk for autism spectrum disorders: A Baby Siblings Research Consortium study. Pediatrics, e1–e8. https://doi.org/10.1542/peds.2010-2825.
Ozonoff, S., Young, G. S., Landa, R. J., Brian, J., Bryson, S., Charman, T., … Iosif, A.-M. (2015). Diagnostic stability in young children at risk for autism spectrum disorder: a Baby Siblings Research Consortium study. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 56(9), 988–998. https://doi.org/10.1111/jcpp.12421.
Pan, B. A., Rowe, M. L., Singer, J. D., & Snow, C. E. (2005). Maternal correlates of growth in toddler vocabulary production in low-income families. Child Development, 76(4), 763–782. https://doi.org/10.1111/j.1467-8624.2005.00876.x.
Parladé, M. V., & Iverson, J. M. (2015). The development of coordinated communication in infants at heightened risk for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(7), 2218–2234. https://doi.org/10.1007/s10803-015-2391-z.
Rowe, M. L., & Goldin-Meadow, S. (2009a). Differences in early gesture explain SES disparities in child vocabulary size at school entry. Science, 323(5916), 951–953. https://doi.org/10.1126/science.1167025.
Rowe, M. L., & Goldin-Meadow, S. (2009b). Early gesture selectively predicts later language learning. Developmental Science, 12(1), 182–187. https://doi.org/10.1111/j.1467-7687.2008.00764.x.
Rowe, M. L., Özçalişkan, Ş, & Goldin-Meadow, S. (2008). Learning words by hand: Gesture’s role in predicting vocabulary development. First Language, 28(2), 182–199. https://doi.org/10.1177/0142723707088310.
Rozga, A., Hutman, T., Young, G. S., Rogers, S. J., Ozonoff, S., Dapretto, M., & Sigman, M. (2011). Behavioral profiles of affected and unaffected siblings of children with autism: Contribution of measures of mother-infant interaction and nonverbal communication. Journal of Autism and Developmental Disorders, 41(3), 287–301. https://doi.org/10.1007/s10803-010-1051-6.
Rutter, M., Bailey, A., & Lord, C. (2003). The social communication questionnaire. Los Angeles: Western Psychological Services.
Sauer, E., Levine, S. C., & Goldin-Meadow, S. (2010). Early gesture predicts language delay in children with pre- or perinatal brain lesions. Child Development, 81(2), 528–539. https://doi.org/10.1111/j.1467-8624.2009.01413.x.
Shire, S. Y., Shih, W., Chang, Y.-C., & Kasari, C. (2018). Short Play and Communication Evaluation: Teachers’ assessment of core social communication and play skills with young children with autism. Autism, 22(3), 299–310. https://doi.org/10.1177/1362361316674092.
So, W.-C., Wong, M. K.-Y., Lui, M., & Yip, V. (2015). The development of co-speech gesture and its semantic integration with speech in 6- to 12-year-old children with autism spectrum disorders. Autism: The International Journal of Research and Practice, 19(8), 956–968. https://doi.org/10.1177/1362361314556783.
StataCorp. (2015). Stata statistical software: Release 14. College Station: StataCorp LP.
Tager-Flusberg, H. (2016). Risk factors associated with language in autism spectrum disorder: Clues to underlying mechanisms. Journal of Speech, Language, and Hearing Research, 59(1), 143–154. https://doi.org/10.1044/2015_JSLHR-L-15-0146.
Talbott, M. R., Nelson, C. A., & Tager-Flusberg, H. (2015a). Maternal gesture use and language development in infant siblings of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(1), 4–14. https://doi.org/10.1007/s10803-013-1820-0.
Talbott, M. R., Nelson, C. A., & Tager-Flusberg, H. (2015b). Diary reports of concerns in mothers of infant siblings of children with autism across the first year of life. Journal of Autism and Developmental Disorders, 45(7), 2187–2199.
Talbott, M. R., Nelson, C. A., & Tager-Flusberg, H. (2016). Maternal vocal feedback to 9-month-old infant siblings of children with ASD. Autism Research, 9(4), 460–470. https://doi.org/10.1002/aur.1521.
Tamis-LeMonda, C. S., Kuchirko, Y., & Song, L. (2014). Why is infant language learning facilitated by parental responsiveness? Current Directions in Psychological Science, 23(2), 121–126. https://doi.org/10.1177/0963721414522813.
Thal, D., Tobias, S., & Morrison, D. (1991). Language and gesture in late talkers: A 1-year follow-up. Journal of Speech and Hearing Research, 34(3), 604–612.
Toth, K., Dawson, G., Meltzoff, A. N., Greenson, J., & Fein, D. (2007). Early social, imitation, play, and language abilities of young non-autistic siblings of children with autism. Journal of Autism and Developmental Disorders, 37(1), 145–157. https://doi.org/10.1007/s10803-006-0336-2.
Veness, C., Prior, M., Eadie, P., Bavin, E., & Reilly, S. (2014). Predicting autism diagnosis by 7 years of age using parent report of infant social communication skills. Journal of Paediatrics & Child Health, 50(9), 693–700.
Weismer, S. E., Lord, C., & Esler, A. (2010). Early language patterns of toddlers on the autism spectrum compared to toddlers with developmental delay. Journal of Autism and Developmental Disorders, 40(10), 1259–1273. https://doi.org/10.1007/s10803-010-0983-1.
Winder, B. M., Wozniak, R. H., Parladé, M. V., & Iverson, J. M. (2013). Spontaneous initiation of communication in infants at low and heightened risk for autism spectrum disorders. Developmental Psychology, 49(10), 1931–1942. https://doi.org/10.1037/a0031061.
Wray, C., Norbury, C. F., & Alcock, K. (2016). Gestural abilities of children with specific language impairment. International Journal of Language & Communication Disorders, 51(2), 174–182. https://doi.org/10.1111/1460-6984.12196.
Yirmiya, N., Gamliel, I., Pilowsky, T., Feldman, R., Baron-Cohen, S., & Sigman, M. (2006). The development of siblings of children with autism at 4 and 14 months: Social engagement, communication, and cognition. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 47(5), 511–523. https://doi.org/10.1111/j.1469-7610.2005.01528.x.
Zwaigenbaum, L., Bryson, S., Rogers, T., Roberts, W., Brian, J., & Szatmari, P. (2005). Behavioral manifestations of autism in the first year of life. International Journal of Developmental Neuroscience, 23(2–3), 143–152. https://doi.org/10.1016/j.ijdevneu.2004.05.001.
Zwaigenbaum, L., Bryson, S. E., Brian, J., Smith, I. M., Roberts, W., Szatmari, P., … Vaillancourt, T. (2016). Stability of diagnostic assessment for autism spectrum disorder between 18 and 36 months in a high-risk cohort. Autism Research: Official Journal of the International Society for Autism Research, 9(7), 790–800. https://doi.org/10.1002/aur.1585.
Acknowledgments
We would like to thank all children and families who participated in this study as well as the former and current Infant Sibling Project team members for their help in the data collection. We also thank two anonymous reviewers for their constructive feedback on an earlier version of the manuscript, Kathryn A. Leech for training on transcription, and Phoebe Stoye for assistance with transcription. This work was presented at the 2018 International Society for Autism Research, Rotterdam, Netherlands. This manuscript was prepared from part of a doctoral dissertation completed by Boin Choi.
Funding
This study was funded by the grants from the National Institutes of Health (R01-DC010290 to HTF and CAN; R21-DC08637 to HTF), Autism Speaks (1323 to HTF), and Simons Foundation (137186 to CAN). The funding bodies did not have any role in the design, collection, analyses, and interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
BC transcribed and coded videotaped sessions, performed data analysis, and drafted the manuscript. PS contributed to transcription and coding of videotaped sessions. MR supervised the data interpretation and revised the manuscript critically for important intellectual content. CAN and HTF were the principal investigators of the larger Infant Sibling Project and critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choi, B., Shah, P., Rowe, M.L. et al. Gesture Development, Caregiver Responsiveness, and Language and Diagnostic Outcomes in Infants at High and Low Risk for Autism. J Autism Dev Disord 50, 2556–2572 (2020). https://doi.org/10.1007/s10803-019-03980-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-019-03980-8