Abstract
Parents of preterm children are more likely to adopt non-optimal parenting behaviors than parents of full-term (FT) children. However, there is a lack of studies on parents of children born moderate to late preterm (MLP; 32–36 gestational weeks). In this study, we aimed to examine: (1) the association between MLP birth status and the trajectory of parental overprotection throughout preschool years, and (2) the role of parental overprotection, MLP birth status, and their interaction in the prediction of the trajectories of hyperactivity-impulsivity and inattention throughout childhood. Data comes from a Canadian representative population-based cohort including 2028 FT, 100 MLP children, and their parents. Overprotective parenting was measured when children were 5, 17, and 29 months old. Hyperactivity-impulsivity and inattention symptoms were measured repeatedly from 4 to 8 years of age. Trajectories of parents’ overprotectiveness and children’s hyperactivity-impulsivity and inattention were modeled. MLP birth status was associated with an increase in parental overprotectiveness across the preschool period. MLP birth status and parental overprotection were both found to be associated with higher levels of hyperactivity-impulsivity symptoms across childhood. No interaction was found between birth status and parental overprotection. The results suggest that parents of MLP children become more overprotective across time compared to parents of FT children and that children born MLP and/or exposed to higher levels of parental overprotection demonstrated higher levels of hyperactivity-impulsivity symptoms across childhood.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Around the world, approximately 10% of births occur before the pregnancy reaches full term (<37 weeks of gestation) (Blencowe et al., 2012). Moderate to late preterm (MLP) births (32–36 gestational weeks) have been less extensively studied than very preterm births, despite the fact that they represent up to 85% of all preterm deliveries (Frey & Klebanoff, 2016). Even though MLP newborns are often comparable in appearance to full-term (FT) neonates, an increasing body of research demonstrates that they are at a greater risk of experiencing a wide range of negative developmental outcomes in comparison to their FT peers throughout their lives (for a literature review, see de Jong et al., 2012). Several aspects of MLP children’s development appear to be impaired, including their motor, socioemotional and cognitive skills (Baron et al., 2014; Brumbaugh et al., 2016; Cheong et al., 2017; de Jong et al., 2015; Potijk et al., 2013). MLP children are also at greater risk of poorer school achievement (Lipkind et al., 2012; van Baar et al., 2009; Williams et al., 2013). Studies have also demonstrated higher risks of internalizing and externalizing behavioral problems among these children (Bul & van Baar, 2012; Dotinga et al., 2019; Palumbi et al., 2018; Perricone et al., 2013; Rogers et al., 2014). In a previous longitudinal study investigating the developmental trajectories of MLP children, we found that MLP children were at greater risk of hyperactivity and impulsivity during childhood in comparison to their FT peers (Faleschini et al., 2020). However, the longer-term outcomes of MLP children and the mechanisms through which MLP birth might impact children’s developmental trajectories remains unclear.
Not all MLP children actually show developmental problems. Some authors suggest that differences within this preterm group might be explained by parent–child interactions and the quality of the caregiving environment (de Jong et al., 2012). Given the increased risk of medical complications and the neonatal difficulties that preterm children encounter, preterm birth might be stressful and emotionally challenging for parents. In comparison to parents of FT children, parents of preterm newborns, including MLP, often report high levels of stress during the neonatal period (Polic et al., 2016; Suttora et al., 2014). Studies also suggest that they are at a greater risk of psychological difficulties, including anxiety and stress, compared to parents of FT babies (McDonald et al., 2013; Suttora et al., 2014). Over time, parental mental health problems can negatively impact the quality of parenting behaviors (Smith, 2010). Studies suggest that parents of very preterm children are more intrusive, controlling, and overprotective than parents of FT children (Forcada-Guex et al., 2006; Korja et al., 2012; Wightman et al., 2007). These behavioral tendencies might be explained by a high parental perception of child vulnerability (Green & Solnit, 1964; Thomasgard & Metz, 1993). This tendency is referred to as the “vulnerable child syndrome” (Green & Solnit, 1964). This syndrome is characterized by excessive preoccupation with the child’s security or health that can lead to overprotecting the child (Thomasgard & Metz, 1993). Thus, parents of preterm children might perceive their child as highly vulnerable and might adopt overprotective practices in order to reduce their anxiety about the child’s safety.
While overprotective behaviors were documented among parents of very preterm children, it is difficult to confirm that these behaviors also characterize parents of children born MLP. Patterns of parenting practices among parents of MLP children are understudied (de Jong et al., 2012). A growing, but small body of research suggests that parents of MLP children are more likely to present intrusive, irritable, and less sensitive parenting in interactions with their child compared to parents of FT children (Hoffenkamp et al., 2015; Westrupp et al., 2012). However, other studies demonstrated no differences between the parenting practices of parents of MLP and FT children (Bilgin & Wolke, 2015; Brown et al., 2014). More research is necessary in order to better understand parenting in the context of MLP birth. While overprotective parenting practices might impact the development of children, there is a lack of knowledge about patterns of overprotective practices among parents of children born MLP.
The important role that parenting practices play in children’s development and behavioral functioning is now well documented (Pinquart, 2017; Smith, 2010; Yeung et al., 2017). Through positive interactions with their parents, children learn to interact appropriately with others and to regulate their behaviors (Bell & Calkins, 2000; Fox & Calkins, 2003). In contrast, children exposed to more negative parenting practices, such as controlling practices, are at greater risk to adopt more negative behaviors and to develop behavioral problems such as inattention, hyperactivity, and impulsivity (Breaux & Harvey, 2019; Deault, 2010; Kawabata et al., 2011, 2012; Keown, 2012; Nelson et al., 2013; Shelleby & Ogg, 2020). Parenting practices characterized by high levels of control may interfere with the development of self-regulating strategies in limiting the opportunities of children to develop their self-control strategies and to deal with potentially anxious or challenging situations (Bell & Calkins, 2000; Fox & Calkins, 2003; Gere et al., 2012; Ungar, 2009). Research suggests that behavioral problems associated with deficits in self-regulation, such as hyperactivity, impulsivity, and inattention, may be influenced by controlling parenting practices, such as overprotection (i.e., providing a level of protection that is excessive, taking into consideration the developmental level of the child). Recent research has shown that controlling and overprotective practices are more frequent among parents of children with a diagnosis of attention-deficit/hyperactivity disorder (ADHD) or showing hyperactivity and inattention, compared to parents of children without these problems (Gau & Chang, 2013; Gere et al., 2012; Molina & Musich, 2016). Thus, parenting practices, including parental overprotection, may be associated with the developmental trajectories of behaviors such as hyperactivity-impulsivity and inattention, and may interact with birth status in the prediction of these outcomes.
As preterm birth is associated with more overprotective parenting practices, and as both are associated with hyperactivity, impulsivity, and inattention, overprotection could play a mediating role in the relations between preterm birth and children’s hyperactivity, impulsivity, and inattention. MLP birth might lead to more parental overprotection and, in turn, overprotective parenting might lead to more hyperactive, impulsive, and inattentive behaviors among children. Moreover, it is also possible that MLP birth and parental overprotection interact together in the prediction of these behavioral problems. It is possible that MLP birth makes children more vulnerable to the influence of environmental factors such as parenting practices (Pluess & Belsky, 2010) or that less overprotective parenting practices act as a protective factor (a moderator) in the relations between MLP birth status and hyperactive, impulsive, and inattentive behaviors. However, the relations between MLP birth, parental overprotection and their interactions in the prediction of child development remains unclear.
Despite the growing research demonstrating that MLP children are at risk of negative behavioral or developmental outcomes including hyperactivity, impulsivity, and inattention, few studies have used longitudinal designs and repeated measures of MLP development (Ask et al., 2018; Gurka et al., 2010; Hornman et al., 2016; Robinson et al., 2013). Therefore, little is known about the developmental trajectories of these at-risk children and the longitudinal developmental processes that may influence their longer-term behavioral outcomes; notably, the predictive effect of being MLP on the hyperactivity, impulsivity, and inattention trajectories and its persistence over years. Moreover, little is known about the parenting practices of parents of MLP children, specifically their patterns over time and their role in MLP developmental trajectories. This dearth of research dramatically limits our understanding of the behavioral development of these children and precludes the identification of the factors that may promote or hinder healthy behavioral functioning and trajectories within this at-risk population.
The present study tackled this gap by modeling developmental trajectories of hyperactivity-impulsivity and inattention in MLP children and examining patterns of overprotective parenting practices and their impact and interaction with MLP birth status in the prediction of these trajectories. Using data from a large population-based birth cohort of children from Canada, we first aimed to examine the association between MLP birth and the trajectory of overprotective parenting practices during preschool years. We also aimed to determine if parental overprotection might explain the documented relation between MLP birth status and child hyperactivity-impulsivity and inattention symptoms, and whether this parental behavior mediates or interacts with MLP in the prediction of these symptoms. We expected MLP birth status to be associated with a higher trajectory of parental overprotection between 5 and 29-months (i.e. more overprotective practices that persist across time). Furthermore, in line with previous literature, we also expected MLP birth status to be associated with higher trajectories of hyperactivity-impulsivity and inattention between 4 and 8 years of age (i.e. higher levels that persist across time). In addition, we predicted overprotective parenting would be a mediator in the relation between MLP birth status and the trajectory of hyperactivity-impulsivity and inattention between 4 and 8 years of age. Finally, we also expected overprotective parenting to interact with MLP birth status in the prediction of these trajectories. More specifically, we predicted that MLP children who are exposed to high levels of overprotective parenting would present higher trajectories of hyperactivity-impulsivity and inattention compared to MLP children who are exposed to lower levels of overprotective parenting.
Methods
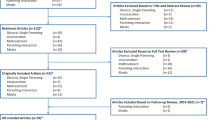
Study Design and Participants
This study used data from the Quebec Longitudinal Study of Child Development (QLSCD), a Canadian representative population-based study of children’s growth and development. This representative sample was drawn from the province’s birth registry and used a stratified procedure based on living area and birth rates. The resulting sample was representative of singleton live births registered in the province’s birth registry during 1997–1998, except for children born on Cree and Inuit territories, on indigenous reservations, or in the Northern region of the province. The sample includes 2128 children born between 32 and 41 gestational weeks for which we have data regarding parental overprotection and hyperactivity-impulsivity or inattention during childhood. This longitudinal study used repeated measures of overprotective parenting when children were 5 (SD = 0.46, range = 3–7 months, N = 2128), 17 (SD = 0.47, range = 16–19 months, N = 1944, 8.67% missing), and 29 months of age (SD = 0.45, range = 28–31 months, N = 1915, 10.01% missing). Hyperactivity-impulsivity and inattention were assessed using primary caregivers’ reports at 4.17 (SD = 0.26, range = 3.67–4.67, N = 1930, 9.31% missing), 5.16 (SD = 0.26, range = 4.67–5.67, N = 1747, 17.91% missing), 6.17 (SD = 0.25, range = 5.67–6.67, N = 1480, 30.45% missing) and 8.16 (SD = 0.26, range = 7.67–8.67, N = 1439, 32.38% missing) years of age. Informed written parental consent and children’s assent were collected prior to each wave of data collection. The research protocol was approved by the research committee of the Institut de la statistique du Québec.
Measures
Gestational Age
Gestational age at birth was ascertained from the birth certificate’s obstetrical estimate of completed weeks of gestation. We used the World Health Organization’s (WHO, 2018) guidelines to define MLP birth. Thus, gestational age (GA) groups were categorized as follows: MLP children (32–36 weeks, N = 100) and FT children (37–41 weeks, N = 2028). Prevalence of MLP birth in this study was found to be 4.93%, which is consistent with the prevalence of preterm birth in Canada (~5% for singleton MLP birth) (Statistics Canada, 2016). A total of 2028 children born FT and 100 children born MLP were included in the final sample. Among the MLP group, 10 children were born moderately preterm (MP; 32–33 gestational weeks) and 90 were born late preterm (LP; 34–36 gestational weeks).
Overprotective Parenting
Overprotective parenting was evaluated using the Parental Cognitions and Conduct Toward the Infant Scale (PACOTIS; Boivin et al., 2005) at 5, 17 and 29 months-old. The PACOTIS measures overprotective parenting using four items. The full list of items and Cronbach’s alphas are presented in Supplemental Table 1. The response scale ranged from “0. Not at all what I think” to “10. Exactly what I think”. Thus, final scores were ranging from 0 to 10, with higher scores indicating higher levels of overprotection. The factor structure of the PACOTIS has been confirmed among twin and singleton samples and this measure has proven to be internally consistent with alphas >0.75 (Boivin et al., 2005). In the current sample, we observed alphas of 0.68 at 5 months, 0.71 at 17 months, and 0.74 at 29 months.
Hyperactivity-Impulsivity and Inattention
Primary caregiver’s ratings of children’s hyperactivity-impulsivity and inattention were obtained at 4, 5, 6, and 8 years using the Social Behavior Questionnaire (SBQ; Tremblay et al., 1991). The SBQ is an omnibus psychopathology inventory that can measure children’s behavioral symptoms in both clinically diagnosed and sub-clinical samples. The SBQ has been proven to be internally consistent (α > 0.70) in samples composed of clinical and normative groups of children and adolescents (Murray et al., 2016, 2017; Pingault et al., 2013; Vitaro et al., 1998). Scores during childhood have been correlated with mental health outcomes and substance use during adolescence and adulthood (Pingault et al., 2013; Zdebik et al., 2019). The hyperactivity-impulsivity subscale consisted of five items and the inattention subscale consisted of three items. Both hyperactivity-impulsivity and inattention symptoms were rated on a 3-point scale, with 0 indicating “Never”, 1 indicating “Sometimes”, and 2 indicating “Often”. Scores were averaged across items, with higher scores indicating higher levels of symptoms. Mean Cronbach’s alphas across time points reveal high internal reliability for both hyperactivity-impulsivity (α = 0.75) and inattention symptoms (α = 0.77). The full list of items and Cronbach’s alphas are presented in Supplemental Table 1.
Covariates
The covariates used in the present study are child sex and maternal education. The information about the child’s sex was ascertained from medical records at birth. Maternal education level was self-reported in a questionnaire completed when children were 5 months old. These two variables are known to be related to both parenting and children’s behavioral problems (Carneiro et al., 2013; Gau & Chang, 2013; Hancock et al., 2014; Willcutt, 2012).
Statistical Analysis
To examine the developmental trajectories of overprotective parenting and hyperactivity-impulsivity and inattention symptoms, multilevel growth curve models were performed using Mplus version 8.1. Multilevel models (MLMs, also known as multilevel regression models, linear mixed models or hierarchical linear models) can easily handle the specific conditions encountered in the present study, including unequal or small groups (groups as small as 50 are sufficient) (Maas & Hox, 2005), unequally spaced time points, data collected across a range of ages within any one occasion, and non-normally distributed scaled repeated measures with missing data (Burchinal et al., 2006; Singer & Willett, 2003). To examine the predictive effect of MLP birth status, the trajectories (growth curves) of overprotective parenting and children’s hyperactivity-impulsivity and inattention were first modeled in the overall sample. MLP birth status was next entered as a dichotomous predictor in the growth models to see if it was associated with inter-individual variation in these overall trajectories. MLMs do not require equal group size to examine the relation between a dichotomous predictor and the trajectories modeled. Keeping the whole sample in the analyses allowed us to have greater statistical power to estimate trajectories and preserved the representativeness of the sample (in this population-based study) and, therefore, the capacity to generalize the results to the population. Full Information Maximum Likelihood estimation was used in order to handle missing data.
The overall trajectories of overprotective parenting and children’s hyperactivity-impulsivity and inattention symptoms were first modeled and described in terms of their intercepts and slopes. Whereas the intercept reflects the mean group value at the starting point, the slope reflects the average monthly change. Using children’s exact chronological age at each assessment point enabled us to flexibly handle individually varying time scores. Once the overall trajectory was established in the full sample, we investigated the extent to which individual differences in growth curve coefficients could be explained by predictors. MLP birth status was first examined in relation to the intercept and slope of the trajectory of parental overprotection. In separate growth models, both MLP birth status and parental overprotection (measured at 29-months-old) were investigated in relation to the trajectories of children’s hyperactivity-impulsivity and inattention. Goodness of fit was assessed using the -Log-likelihood (-LL; an indicator of deviance), the Akaike information criterion (AIC), and the Bayesian information criterion (BIC), with lower values indicating a better representation of the data by the model (Hox, 2010, 2013). Indices of fit available for every multilevel model are provided in Tables 1 and 2. To increase parsimony, only the best fitting models were selected. Covariate, predictors and interaction effects were trimmed at p > 0.10.
Results
Participants
Supplemental Table 2 presents the sample characteristics. There were significant group differences between MLP and FT children regarding gestational age at birth (35.06 vs 39.20 weeks, p < 0.01) and birth weight (2660.45 vs 3440.16 g, p < 0.01), even though only 36 MLP children had a low-birth-weight (<2500 g). Maternal age at 5 months and the proportion of boys and girls in each group were comparable. Concerning race and ethnicity, parents were asked “To which ethnic or cultural group do (name of the child) ancestors belong”. Participants could declare multiple groups. The three most common ethnic groups reported by the parents were Canadian (63.00%), French (30.00%), and Irish (4.40%). Concerning country of origin, 87.80% of mothers reported being born in Canada, 2.00% were born in European countries such as France, Germany, Italy, United Kingdom, Poland or Portugal, 0.70% were born in the United States, 1.10% were born in Asian countries such as India, Philippines, Vietnam or China, and 8.40% came from other countries that remain unknown to the authors of the present study (not coded in the available data base). A total of 73.30% of mothers had at least some post-secondary education (including 17.60% having some post-secondary studies without having any post-secondary diploma, 10.20% having a vocational/technical school diploma, 18.90% having a college (junior) diploma, and 26.60% having a university degree). Among mothers of MLP children, 63.55% had pursued postsecondary education compared to 73.95% of FT mothers. Family income varied from less than $10,000 to over $80,000 CAD (with a mean between $40,000 and $49,999 CAD). Mothers of MLP children were less likely to have a family income higher than $80,000 (10.57% vs 14.28%) compared to FT mothers, and more likely to have an income lower than $30,000 (37.50% vs 28.84%).
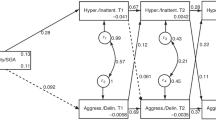
Association Between MLP Birth and the Trajectory of Overprotective Parenting
First, the best-fitting growth model for overprotective parenting (including parents of MLP and FT children) indicates a small, but significant monthly decrease (−0.07, p < 0.01) in overprotection from 5 to 29 months (Table 1 and Fig. 1). On average, parental overprotection decreased by 0.07 points per month (0.84 per year), starting at 5.43 at 5 months. The predictive models showed that MLP birth status was associated with the slope (unstandardized effect estimate = 0.02, p < 0.01). The decrease in parental overprotection was slower in the MLP group compared to the FT group (see Fig. 1). While MLP birth was not found to be associated with the initial level of parental overprotection, it was significantly associated with the level of overprotection at 29 months, even after controlling for child sex and maternal education. On average at 29 months, the level of overprotection among parents of MLP children was 0.56 points higher (p < 0.05) than the level of overprotection of parents of FT children. Thus, the association between MLP birth and parental overprotection became stronger as child age increased (0.03 at 5 months, 0.29 at 17 months, and 0.56 at 29 months) resulting in a less negative slope overtime for the MLP group.
Association of MLP Birth and Overprotection with the Trajectories of Hyperactivity-Impulsivity and Inattention
The results pertaining to children’s hyperactivity-impulsivity and inattention are presented in Table 2. Overall, levels of hyperactivity-impulsivity and inattention remained low over time in the overall sample (see Supplemental Figs. 1 and 2), which is consistent with what is expected in a population-based (sub-clinical) sample. These symptoms were found to be higher among boys and families with lower education levels. Thus, child sex and maternal education were included in the final models.
Hyperactivity-Impulsivity
The final predictive growth model including the covariates and the predictors, children’s birth status and parental overprotection, revealed that both predictors were significantly associated with the initial level of hyperactivity-impulsivity (Table 2, Model 3). MLP birth and higher levels of parental overprotection were both associated with higher initial levels of hyperactivity-impulsivity that remained persistently higher across time (i.e. no interaction with time). On average, MLP children had an initial score of 0.77 while FT children had an initial score of 0.68 on the hyperactivity-impulsivity scale, controlling for parental overprotection, child sex and maternal education. An increase of 1 point on parental overprotection was associated with an increase of 0.01 (p < 0.05) on the initial level of hyperactivity-impulsivity. On average, children experiencing no parental overprotection (score of 0 on a scale ranging from 0 to 10) had an initial score of 0.68 at 4 years of age, while children experiencing a mean-level of parental overprotection (score of 4) had an initial score of 0.72, and children experiencing the highest level of parental overprotection (score of 10) had a score of 0.78. The predictive effects of MLP birth and parental overprotection were small, however, they were persistent across time and remained significant after controlling for child sex and maternal education. In order to examine the interaction between overprotective parenting and MLP birth status in the prediction of children’s symptoms, an interaction term was added as a predictor of the intercept and the slope in the final growth model. The non-significant interaction term indicates that MLP birth status doesn’t interact with parental overprotection in the prediction of the trajectory of children’s hyperactivity-impulsivity.
Inattention
In the final model controlling for child sex and maternal education, MLP birth was found to be associated with the initial level of inattention, while parental overprotection was not associated. The inattention score of MLP children at 4 years of age was found to be 0.10 points (p < 0.05) higher than the score of FT children and remained persistently higher across time (Table 2, Model 3). Moreover, we tested the interaction between MLP birth and overprotection in the prediction of inattention and the results showed that MLP birth status did not interact with overprotective parenting in the prediction of the trajectory.
Mediation Analyses
To test the hypothesis that overprotective parenting mediates the relation between MLP birth status and children’s hyperactivity-impulsivity and inattention, we used the Baron and Kenny’s (1986) classic procedure. Thus, the data were subjected to multilevel regression equations, controlling for child sex and maternal education. Multilevel regression models were estimated independently for hyperactivity-impulsivity and inattention. The results are presented in Table 2 (see Models 2 and 3). The first regression equation (Model 2) revealed that MLP birth was related to initial levels of child hyperactivity-impulsivity (B = 0.08, p < 0.05) and inattention (B = 0.09, p < 0.05). The second regression equation (Model 3) indicated that overprotective parenting was related to the initial level of child hyperactivity-impulsivity (B = 0.01, p < 0.05), while accounting for birth status and the covariates. No association was found between parental overprotection and inattention. Model 3 also revealed that MLP birth status remained significantly related to initial levels of child hyperactivity-impulsivity (B = 0.09, p < 0.05) and inattention (B = 0.10, p < 0.05), when controlling for parental overprotection. In fact, the data doesn’t meet the requirements (Condition 4 of the Baron and Kenny procedure) for mediation: if a mediation effect exists, the effect of X (MLP birth) on Y (the initial status of the trajectory of hyperactivity-impulsivity and inattention) will disappear (or weaken) when M (parental overprotection) is included in the regression. Finally, the indirect effects of parental overprotection in the relations between child birth status and hyperactivity-impulsivity and inattention trajectories were also examined using a multilevel SEM framework following Preacher et al. (2010, 2011) guidelines. The indirect effects of parental overprotection (0.006 and 0.005, for hyperactivity-impulsivity and inattention respectively) were not significant. Thus, parental overprotection doesn’t play a mediational or indirect role in the relations between child birth status and children’s hyperactivity-impulsivity and inattention.
Discussion
To gain insight into the relations between MLP birth and overprotective parenting, the first aim of this study was to examine the association between MLP birth status and the trajectory of overprotective parenting during the preschool period. The present study also investigated the independent and interacting role of MLP birth and overprotective parenting in the prediction of the developmental trajectory of children’s hyperactivity-impulsivity and inattention from 4 to 8 years of age. The results of this study revealed that MLP birth was associated with a slower decrease in parental overprotection across the preschool period and that both MLP birth and parental overprotection were independent predictors of the trajectory of children’s hyperactivity-impulsivity. Moreover, MLP birth, but not parental overprotection, predicted inattention during childhood. We did not find evidence of an interaction or mediation between MLP birth status and parental overprotection in the prediction of the trajectories of children’s hyperactivity-impulsivity and inattention symptoms.
The overall trajectory of parental overprotection from 5 to 29 months revealed a small decrease across time. This finding might reflect a decrease in parents’ general tendency to perceive their newborn as highly vulnerable (Thomasgard & Metz, 1996). In line with this, some studies observed that parents’ levels of anxiety and stress decreased in the months following childbirth (Dipietro et al., 2008; Vismara et al., 2016). While there is a peak of parental anxiety and preoccupation after the child’s birth, parents become less preoccupied and anxious about their infants during the first months’ postpartum. Specifically, parents have been found to be more preoccupied by their child’s well-being during the weeks following the child’s birth and the intensity of parental worries decreases as parents gain more experience in parenting their child (Kim et al., 2013). Parents’ anxiety and concerns regarding their child tend to decrease as parental self-efficacy increases during infancy (Kim et al., 2013; Leahy-Warren & McCarthy, 2011). The decrease in parental overprotection might have indirectly captured the decrease in parental anxiety documented in previous studies. However, as the present study didn’t measure parents’ anxiety, we were unable to investigate this hypothesis, which is a major limitation of the present study. A meta-analysis revealed that maternal psychological factors, parenting stress and anxiety in particular, are associated with higher levels of parental perception of a child’s vulnerability (Tallandini et al., 2015). As perceived child vulnerability can lead to overprotection of the child, a decrease in parental stress or anxiety might lead to a decrease in parents’ overprotective parenting. Consistent with this hypothesis, some studies have found that higher levels of maternal anxiety is associated with higher levels of overprotective parenting during childhood (Clarke et al., 2013; Cooklin et al., 2013). Parents of premature children have more mental health problems than parents of FT children (Suttora et al., 2014), thus while the data available to us did not allow us to examine parental mental health as a predictor, future research should consider it along with child MLP birth status.
The results revealed that MLP birth status is associated with a slower rate of change in parental overprotection across the preschool period. The levels of overprotection among parents of MLP children were found to be similar to the levels of overprotection among parents of FT children at 5 months. However, a relation emerged between MLP birth and overprotection across time, such that parents of MLP children were found to be more overprotective at 29 months than those of FT children. Parents of premature children generally report more stress than parents of FT children (Suttora et al., 2014). Thus, parents’ initial concerns for their child’s health and safety may be less likely to decrease if the child was born premature and it might result in higher levels of overprotection across time. Also, knowing their child’s premature birth status, it is possible that parents of MLP children may be more concerned or anxious about their child’s development. In fact, MLP children are at greater risk of manifesting higher levels of developmental problems during childhood which can represent an additional challenge for parents (de Jong et al., 2012). The significant relation between MLP birth and the slope of parental overprotection might reflect the increasing difficulty of taking care of children having special needs or behavioral difficulties. While previous studies mostly found no difference between MLP and FT children during infancy (de Jong et al., 2012), MLP children tend to manifest higher rates of behavioral and developmental problems later on during childhood (Dotinga et al., 2019; Stene-Larsen et al., 2016). They are also at higher risk of cognitive deficits during childhood which may increase parents’ concerns and difficulty in taking care of their children (Baron et al., 2014; Woythaler et al., 2011). Thus, parents of MLP children might become more concerned by their child’s well-being as children’s difficulties emerge, and it might result in more overprotective parenting across time. However, the present study did not consider children’s developmental outcomes during infancy, which may warrant future examination.
To our knowledge, only two studies have examined overprotection among parents of MLP children. One study measured overprotection among parents of 54 children between 3 and 8 years of age including 13 late preterm children (born between 34 and 36 gestational weeks) (Samra et al., 2010). This study observed no association between late preterm birth status and levels of overprotection. However, this study had a small sample size (low statistical power) and did not include children born at 32 and 33 weeks of gestation, which may have precluded the detection of differences. In the second study, 354 mothers of children born low-to-moderate risk (from 33 to 36 gestational weeks, with low birth weight, or small for gestational age) were compared to 2461 mothers of children with no perinatal risk (normal birth weight and at term) (Westrupp et al., 2012). Mothers in the low-to-moderate risk group were more likely than mothers in the no perinatal risk group to report high level of overprotective parenting. However, the differences between groups didn’t remain significant while controlling for maternal factors, such as psychological distress. In the current study, parents’ psychological factors were not considered. Moreover, in our study, the MLP group was created based on gestational age only and children born at 32 weeks of gestation were included. As only three studies, including the present one, have examined parental overprotection in parents of MLP children, and as their methodology diverge, further investigation is needed in order to clarify the link between MLP birth and overprotective parenting. The link between children’s birth status and parental overprotection emerges across time in the present study, thus, further research would benefit from using a longitudinal design with repeated measures of parental overprotection. As overprotective parenting is associated with poorer child outcomes (Kiel & Maack, 2012; Laurin et al., 2015), it is important to understand the factors that might increase parents’ likelihood to adopt these parenting behaviors.
In the present study, we found that parental overprotection was related to higher levels of hyperactivity-impulsivity across childhood. The association was small but persistent across time and remained while controlling for children’s birth status, child sex and maternal education. Various factors may help explain the relation between parental overprotection and hyperactivity-impulsivity in children. Parenting practices that are characterized by controlling behaviors, such as overprotection, may hinder the development of self-regulation strategies in children by limiting opportunities of experiencing self-control (Bell & Calkins, 2000; Fox & Calkins, 2003). Children with hyperactive and impulsive symptoms often exhibit poor regulation skills (Shiels & Hawk, 2010). However, we cannot rule out the possibility that the relation between parental overprotection and hyperactive-impulsive symptoms is bidirectional. Confronted with children having self-regulation difficulty, parents may react by being more controlling. Only a study including repeated and concomitant measures of parental overprotection and children’s hyperactivity-impulsivity will clarify the direction of this association.
Consistent with previous studies showing that MLP children are at higher risk of hyperactivity and inattention symptoms during school years (Perricone et al., 2013; van Baar et al., 2009), children’s MLP birth status was found to be associated with higher levels of hyperactivity-impulsivity and inattention between 4 and 8 years old. The most common explanation for the developmental problems of MLP children lies in their immature brain development at birth, which is known to be related to later developmental and mental health problems (Kinney, 2006; Schore, 2001). The biological impairments resulting from the extrauterine development of the brain may increase the risk of MLP children to develop neurocognitive problems (Kinney, 2006). However, we cannot rule out the possibility that knowing that their child was born premature, parents of MLP children might perceive their premature children as having more difficulties than they actually have, especially if the parents are prone to anxiety or overprotection. Thus, it might be particularly important for future research to take into account parental mental health and to use more objective measures of children’s hyperactivity-impulsivity and inattention.
As MLP birth remained related to children’s hyperactivity-impulsivity and inattention symptoms while controlling for parental overprotection, our results don’t support a mediating role of parental overprotection in the relation between MLP birth and children’s symptoms. The results suggest that children’s birth status and parental overprotection are independent and unique predictors of children’s hyperactive and impulsive symptoms. Moreover, we did not find any interaction between MLP birth status and parental overprotection in the prediction of the trajectory of hyperactivity-impulsivity and inattention symptoms. Thus, the association between parental overprotection and children’s hyperactivity-impulsivity applies to both FT and MLP children. Further research should, however, include and compare different groups of premature children and FT children in order to increase our understanding of the interaction between preterm birth and parenting in the prediction of children’s behavioral problems.
Importantly, this study has some strengths and limitations that ought to be considered. Two important strengths are the use of a population-based representative sample and a prospective longitudinal design including repeated measures of parenting and children’s behavioral problems. Longitudinal studies within a representative sample at this age range are relatively rare and thus this research substantively adds to the literature on MLP. However, behavioral problems were assessed using parental reports only. Objective evaluations of hyperactivity, impulsivity, and inattention would increase our understanding of the developmental trajectories of these children. While the percentage of MLP children was consistent with what is expected in this population (~5% for singleton MLP birth), the number of children in the MLP group was small. Moreover, the MLP group was mainly composed of children born between 34 and 36 weeks of gestation (N = 90), and thus, the results of this study may not be generalizable to children born at 32–33 gestational weeks (N = 10). In line with this, the small number of low-birthweight children in our sample did not allow us to examine the predictive effect of birth weight. Given that birth weight is known to be an important predictor of child development (Miller et al., 2018; Peralta-Carcelen et al., 2013), further studies should account for this in the prediction of the trajectories of children’s hyperactivity, impulsivity, and inattention.
Moreover, the current study focuses on overprotection as a parenting practice in relation to children’s birth status and hyperactivity-impulsivity and inattention behaviors. However, other aspects of parenting have been associated with both preterm birth and behavioral problems such as hyperactivity and impulsivity in previous research, including parental hostility, stress, and involvement (Cussen et al., 2012; Ellis & Nigg, 2009; Pimentel et al., 2011; Treyvaud, 2014; Treyvaud et al., 2014). Further research should take into account more dimensions of parenting to increase our understanding of the parental factors that promote or hinder the developmental trajectories of MLP children. In order to better understand the practices of parents following MLP birth and the interaction between these practices and MLP birth in the prediction of children’s developmental trajectory, further studies should include multiple dimensions of parenting and other aspects of child development. This study focused on parental overprotection and children’s hyperactivity-impulsivity and inattention symptoms because of their documented relation with preterm birth, but other aspects of parenting and child development have been shown to be related to MLP birth, and thus, should be examined as well. Furthermore, parental overprotection was measured using a self-report questionnaire. Self-report questionnaires are biased in nature. Observational measures would provide a better understanding of the association between MLP birth and parenting. Finally, we did not consider parents’ mental health and it is possibly associated with overprotective parenting. Given the documented predictive effects of parental mental health on parenting practices and child development (Ahun et al., 2018; Faleschini et al., 2019; Smith, 2010), parental mental health problems deserve to be investigated in future research on MLP children.
Conclusion
The present study is the first to examine the relation between MLP birth and the trajectory of parental overprotection across the preschool period. It is also the first to examine the interaction between MLP birth and overprotective parenting in the prediction of children’s hyperactivity-impulsivity and inattention trajectories across childhood. Current results highlight the need to provide interventions for both parents and children. Specifically, parents of MLP children that were found to be at an increased risk of adopting overprotective parenting practices would benefit from interventions aiming to promote more positive parenting practices. Given the observed association between parental overprotection and hyperactivity-impulsivity, it would be important to support parenting practices that allow children to develop their autonomy by providing them opportunities to learn strategies to regulate their behaviors. Moreover, gaining a better understanding of the hyperactivity, impulsivity, and inattention problems that MLP children might encounter through further research could help to implement relevant interventions to reduce negative behavioral outcomes in this vulnerable population. In fact, until recently, MLP children were considered to be at little or no risk of long-term developmental difficulties. However, an increasing number of studies suggest that MLP children are at a greater risk of developmental problems across time. As these children have received limited scientific attention to date despite that they represent the majority of premature children, greater efforts need to be made to promote their developmental trajectories.
References
Ahun, M. N., Consoli, A., Pingault, J. B., Falissard, B., Battaglia, M., Boivin, M., Tremblay, R. E., & Côté, S. M. (2018). Maternal depression symptoms and internalising problems in the offspring: The role of maternal and family factors. European Child and Adolescent Psychiatry, 27(7), 921–932. https://doi.org/10.1007/s00787-017-1096-6.
Ask, H., Gustavson, K., Ystrom, E., Havdahl, K. A., Tesli, M., Askeland, R. B., & Reichborn-Kjennerud, T. (2018). Association of gestational age at birth with symptoms of attention-deficit/hyperactivity disorder in children. JAMA Pediatrics, 172(8), 749–756. https://doi.org/10.1001/jamapediatrics.2018.1315.
van Baar, A. L., Vermaas, J., Knots, E., de Kleine, M. J. K., & Soons, P. (2009). Functioning at school age of moderately preterm children born at 32 to 36 weeks’ gestational age. Pediatrics, 124(1), 251–257. https://doi.org/10.1542/peds.2008-2315.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research. Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173.
Baron, I. S., Weiss, B. A., Baker, R., Khoury, A., Remsburg, I., Thermolice, J. W., Litman, F. R., & Ahronovich, M. D. (2014). Subtle adverse effects of late preterm birth: A cautionary note. Neuropsychology, 28(1), 11–18. https://doi.org/10.1037/neu0000018.
Bell, K. L., & Calkins, S. D. (2000). Relationships as inputs and outputs of emotion regulation. Psychological Inquiry, 11(3), 160–163 Retrieved from https://www.jstor.org/stable/1449794.
Bilgin, A., & Wolke, D. (2015). Maternal sensitivity in parenting preterm children: A meta-analysis. Pediatrics, 136(1), e177–e193. https://doi.org/10.1542/peds.2014-3570.
Blencowe, H., Cousens, S., Oestergaard, M. Z., Chou, D., Moller, A. B., Narwal, R., Adler, A., Vera Garcia, C., Rohde, S., Say, L., & Lawn, J. E. (2012). National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. The Lancet, 379, 2162–2172. https://doi.org/10.1016/S0140-6736(12)60820-4.
Boivin, M., Perusse, D., Dionne, G., Saysset, V., Zoccolillo, M., Tarabulsy, G. M., Tremblay, N., & Tremblay, R. E. (2005). The genetic-environmental etiology of parents’ perceptions and self-assessed behaviours toward their 5-month-old infants in a large twin and singleton sample. Journal of Child Psychology and Psychiatry, 46(6), 612–630. https://doi.org/10.1111/j.1469-7610.2004.00375.x.
Breaux, R. P., & Harvey, E. A. (2019). A longitudinal study of the relation between family functioning and preschool ADHD symptoms. Journal of Clinical Child and Adolescent Psychology, 48(5), 749–764. https://doi.org/10.1080/15374416.2018.1437737.
Brown, H. K., Speechley, K. N., Macnab, J., Natale, R., & Campbell, M. K. (2014). Mild prematurity, proximal social processes, and development. Pediatrics, 134(3), e814–e824. https://doi.org/10.1542/peds.2013-4092.
Brumbaugh, J. E., Conrad, A. L., Lee, J. K., DeVolder, I. J., Zimmerman, M. B., Magnotta, V. A., Axelson, E. D., & Nopoulos, P. C. (2016). Altered brain function, structure, and developmental trajectory in children born late preterm. Pediatric Research, 80(2), 197–203. https://doi.org/10.1038/pr.2016.82.
Bul, K. C. M., & van Baar, A. L. (2012). Behavior problems in relation to sustained selective attention skills of moderately preterm children. Journal of Developmental and Physical Disabilities, 24, 111–123. https://doi.org/10.1007/s10882-011-9258-9.
Burchinal, M., Nelson, L., & Poe, M. (2006). Best practices in quantitative methods for developmentalists: IV. Growth curve analysis: An introduction to various methods for analyzing longitudinal data. Monographs of the Society for Research in Child Development, 71(3), 65–87.
Carneiro, P., Meghir, C., & Parey, M. (2013). Maternal education, home environments, and the development of children and adolescents. Journal of the European Economic Association, 11, 123–160. https://doi.org/10.1111/j.1542-4774.2012.01096.x.
Cheong, J. L., Doyle, L. W., Burnett, A. C., Lee, K. J., Walsh, J. M., Potter, C. R., Treyvaud, K., Thompson, D. K., Olsen, J. E., Anderson, P. J., & Spittle, A. J. (2017). Association between moderate and late preterm birth and neurodevelopment and social-emotional development at age 2 years. JAMA Pediatrics, 171(4), e164805. https://doi.org/10.1001/jamapediatrics.2016.4805.
Clarke, K., Cooper, P., & Creswell, C. (2013). The parental overprotection scale: Associations with child and parental anxiety. Journal of Affective Disorders, 151(2), 618–624. https://doi.org/10.1016/j.jad.2013.07.007.
Cooklin, A. R., Giallo, R., D’Esposito, F., Crawford, S., & Nicholson, J. M. (2013). Postpartum maternal separation anxiety, overprotective parenting, and children’s social-emotional well-being: Longitudinal evidence from an Australian cohort. Journal of Family Psychology, 27(4), 618–628. https://doi.org/10.1037/a0033332.
Cussen, A., Sciberras, E., Ukoumunne, O. C., & Efron, D. (2012). Relationship between symptoms of attention-deficit/hyperactivity disorder and family functioning: A community-based study. European Journal of Pediatrics, 171(2), 271–280. https://doi.org/10.1007/s00431-011-1524-4.
Deault, L. C. (2010). A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD). Child Psychiatry and Human Development, 41(2), 168–192. https://doi.org/10.1007/s10578-009-0159-4.
Dipietro, J. A., Costigan, K. A., & Sipsma, H. L. (2008). Continuity in self-report measures of maternal anxiety, stress, and depressive symptoms from pregnancy through two years postpartum. Journal of Psychosomatic Obstetrics and Gynecology, 29(2), 115–124. https://doi.org/10.1080/01674820701701546.
Dotinga, B. M., de Winter, A. F., Bocca-Tjeertes, I. F. A., Kerstjens, J. M., Reijneveld, S. A., & Bos, A. F. (2019). Longitudinal growth and emotional and behavioral problems at age 7 in moderate and late preterms. PLoS One, 14(1), e0211427. https://doi.org/10.1371/journal.pone.0211427.
Ellis, B., & Nigg, J. (2009). Parenting practices and attention-deficit/hyperactivity disorder: New findings suggest partial specificity of effects. Journal of the American Academy of Child and Adolescent Psychiatry, 48(2), 146–154. https://doi.org/10.1097/CHI.0b013e31819176d0.
Faleschini, S., Rifas-Shiman, S. L., Tiemeier, H., Oken, E., & Hivert, M. F. (2019). Associations of prenatal and postnatal maternal depressive symptoms with offspring cognition and behavior in mid-childhood: A prospective cohort study. International Journal of Environmental Research and Public Health, 16, 1007. https://doi.org/10.3390/ijerph16061007.
Faleschini, S., Matte-Gagné, C., Côté, S., Tremblay, R. E., & Boivin, M. (2020). Trajectories of behavioral problems among moderate-late preterm children from 4 to 10 years: A prospective population-based study. Early Human Development, 143, 104964. https://doi.org/10.1016/j.earlhumdev.2020.104964.
Forcada-Guex, M., Pierrehumbert, B., Borghini, A., Moessinger, A., & Muller-Nix, C. (2006). Early dyadic patterns of mother-infant interactions and outcomes of prematurity at 18 months. Pediatrics, 118(1), e107. https://doi.org/10.1542/peds.2005-1145.
Fox, N. A., & Calkins, S. D. (2003). The development of self-control of emotion: Intrinsic and extrinsic influences. Motivation and Emotion, 27(1), 7–26. https://doi.org/10.1023/A:1023622324898.
Frey, H. A., & Klebanoff, M. A. (2016). The epidemiology, etiology, and costs of preterm birth. Seminars in Fetal and Neonatal Medicine, 21(2), 68–73. https://doi.org/10.1016/j.siny.2015.12.011.
Gau, S. S. F., & Chang, J. P. C. (2013). Maternal parenting styles and mother-child relationship among adolescents with and without persistent attention-deficit/hyperactivity disorder. Research in Developmental Disabilities, 34(5), 1581–1594. https://doi.org/10.1016/j.ridd.2013.02.002.
Gere, M. K., Villabø, M. A., Torgersen, S., & Kendall, P. C. (2012). Overprotective parenting and child anxiety: The role of co-occurring child behavior problems. Journal of Anxiety Disorders, 26(6), 642–649. https://doi.org/10.1016/j.janxdis.2012.04.003.
Green, M., & Solnit, A. J. (1964). Reactions to the threatened loss of a child: A vulnerable child syndrome – pediatric management of the dying child, part III. Pediatrics, 34, 58–66 Retrieved from https://pediatrics.aappublications.org/content/34/1/58/.
Gurka, M. J., LoCasale-Crouch, J., & Blackman, J. A. (2010). Long-term cognition, achievement, socioemotional, and behavioral development of healthy late-preterm infants. Archives of Pediatrics and Adolescent Medicine, 164(6), 525–532. https://doi.org/10.1001/archpediatrics.2010.83.
Hancock, K. J., Lawrence, D., & Zubrick, S. R. (2014). Higher maternal protectiveness is associated with higher odds of child overweight and obesity: A longitudinal Australian study. PLoS One, 9(6), e100686. https://doi.org/10.1371/journal.pone.0100686.
Hoffenkamp, H. N., Braeken, J., Hall, R. A. S., Tooten, A., Vingerhoets, A. J. J. M., & van Bakel, H. J. A. (2015). Parenting in complex conditions: Does preterm birth provide a context for the development of less optimal parental behavior? Journal of Pediatric Psychology, 40(6), 559–571. https://doi.org/10.1093/jpepsy/jsv007.
Hornman, J., de Winter, A. F., Kerstjens, J. M., Bos, A. F., & Reijneveld, S. A. (2016). Emotional and behavioral problems of preterm and full-term children at school entry. Pediatrics, 137(5), e20152255. https://doi.org/10.1542/peds.2015-2255.
Hox, J. J. (2010). Multilevel analysis: Techniques and applications. New York: Routledge.
Hox, J. J. (2013). Multilevel regression and multilevel structural equation modeling. In T. D. Little (Ed.), The Oxford handbook of quantitative methods in psychology: Vol. 2: Statistical analysis. Oxford: Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199934898.013.0014.
de Jong, M., Verhoeven, M., & van Baar, A. L. (2012). School outcome, cognitive functioning, and behaviour problems in moderate and late preterm children and adults: A review. Seminars in Fetal and Neonatal Medicine, 17(3), 163–169. https://doi.org/10.1016/j.siny.2012.02.003.
de Jong, M., Verhoeven, M., Lasham, C. A., Meijssen, C. B., & van Baar, A. L. (2015). Behaviour and development in 24-month-old moderately preterm toddlers. Archives of Disease in Childhood, 100, 548–553. https://doi.org/10.1136/archdischild-2014-307016.
Kawabata, Y., Alink, L. R. A., Tseng, W. L., van Ijzendoorn, M. H., & Crick, N. R. (2011). Maternal and paternal parenting styles associated with relational aggression in children and adolescents: A conceptual analysis and meta-analytic review. Developmental Review, 31(4), 240–278. https://doi.org/10.1016/j.dr.2011.08.001.
Kawabata, Y., Tseng, W. L., & Gau, S. S. F. (2012). Symptoms of attention-deficit/hyperactivity disorder and social and school adjustment: The moderating roles of age and parenting. Journal of Abnormal Child Psychology, 40(2), 177–188. https://doi.org/10.1007/s10802-011-9556-9.
Keown, L. J. (2012). Predictors of boys’ ADHD symptoms from early to middle childhood: The role of father-child and mother-child interactions. Journal of Abnormal Child Psychology, 40(4), 569–581. https://doi.org/10.1007/s10802-011-9586-3.
Kiel, E. J., & Maack, D. J. (2012). Maternal BIS sensitivity, overprotective parenting, and children’s internalizing behaviors. Personality and Individual Differences, 53(3), 257–262. https://doi.org/10.1016/j.paid.2012.03.026.
Kim, P., Mayes, L., Feldman, R., Leckman, J. F., & Swain, J. E. (2013). Early postpartum parental preoccupation and positive parenting thoughts: Relationship with parent-infant interaction. Infant Mental Health Journal, 34(2), 104–116. https://doi.org/10.1002/imhj.21359.
Kinney, H. C. (2006). The near-term (late preterm) human brain and risk for periventricular leukomalacia: A review. Seminars in Perinatology, 30, 81–88. https://doi.org/10.1053/j.semperi.2006.02.006.
Korja, R., Latva, R., & Lehtonen, L. (2012). The effects of preterm birth on mother-infant interaction and attachment during the infant’s first two years. Acta Obstetricia et Gynecologica Scandinavica, 91(2), 164–173. https://doi.org/10.1111/j.1600-0412.2011.01304.x.
Laurin, J. C., Joussemet, M., Tremblay, R. E., & Boivin, M. (2015). Early forms of controlling parenting and the development of childhood anxiety. Journal of Child and Family Studies, 24(11), 3279–3292. https://doi.org/10.1007/s10826-015-0131-9.
Leahy-Warren, P., & McCarthy, G. (2011). Maternal parental self-efficacy in the postpartum period. Midwifery, 27, 802–810. https://doi.org/10.1016/j.midw.2010.07.008.
Lipkind, H. S., Slopen, M. E., Pfeiffer, M. R., & McVeigh, K. H. (2012). School-age outcomes of late preterm infants in New York City. American Journal of Obstetrics & Gynecology, 206, 222.e1–222.e6. https://doi.org/10.1016/j.ajog.2012.01.007.
Maas, C. J. M., & Hox, J. J. (2005). Sufficient sample sizes for multilevel modeling. Methodology, 1(3), 86–92. https://doi.org/10.1027/1614-1881.1.3.86.
McDonald, S. W., Benzies, K. M., Gallant, J. E., McNeil, D. A., Dolan, S. M., & Tough, S. C. (2013). A comparison between late preterm and term infants on breastfeeding and maternal mental health. Maternal and Child Health Journal, 17(8), 1468–1477. https://doi.org/10.1007/s10995-012-1153-1.
Miller, S. E., DeBoer, M. D., & Scharf, R. J. (2018). Executive functioning in low birth weight children entering kindergarten. Journal of Perinatology, 38(1), 98–103. https://doi.org/10.1038/jp.2017.147.
Molina, M. F., & Musich, F. M. (2016). Perception of parenting style by children with ADHD and its relation with inattention, hyperactivity/impulsivity and externalizing symptoms. Journal of Child and Family Studies, 25(5), 1656–1671. https://doi.org/10.1007/s10826-015-0316-2.
Murray, A. L., Eisner, M., & Ribeaud, D. (2016). The development of the general factor of psychopathology ‘p factor’ through childhood and adolescence. Journal of Abnormal Child Psychology, 44(8), 1573–1586. https://doi.org/10.1007/s10802-016-0132-1.
Murray, A. L., Obsuth, I., Eisner, M., & Ribeaud, D. (2017). Evaluating longitudinal invariance in dimensions of mental health across adolescence: An analysis of the social behavior questionnaire. Assessment, 26(7), 1234–1245. https://doi.org/10.1177/1073191117721741.
Nelson, D. A., Yang, C., Coyne, S. M., Olsen, J. A., & Hart, C. H. (2013). Parental psychological control dimensions: Connections with Russian preschoolers’ physical and relational aggression. Journal of Applied Developmental Psychology, 34(1), 1–8. https://doi.org/10.1016/j.appdev.2012.07.003.
Palumbi, R., Peschechera, A., Margari, M., Craig, F., Cristella, A., Petruzzelli, M. G., & Margari, L. (2018). Neurodevelopmental and emotional-behavioral outcomes in late-preterm infants: An observational descriptive case study. BMC Pediatrics, 18(1), 318. https://doi.org/10.1186/s12887-018-1293-6.
Peralta-Carcelen, M., Bailey, K., Rector, R., & Gantz, M. (2013). Behavioral and socioemotional competence problems of extremely low birth weight children. Journal of Perinatology, 33(11), 887–892. https://doi.org/10.1038/jp.2013.78.
Perricone, G., Morales, M. R., & Anzalone, G. (2013). Neurodevelopmental outcomes of moderately preterm birth: Precursors of attention deficit hyperactivity disorder at preschool age. SpringerPlus, 2, 221. https://doi.org/10.1186/2193-1801-2-221.
Pimentel, M. J., Vieira-Santos, S., Santos, V., & Vale, M. C. (2011). Mothers of children with attention deficit/hyperactivity disorder: Relationship among parenting stress, parental practices and child behaviour. ADHD Attention Deficit and Hyperactivity Disorders, 3(1), 61–68. https://doi.org/10.1007/s12402-011-0053-3.
Pingault, J. B., Côté, S. M., Galéra, C., Genolini, C., Falissard, B., Vitaro, F., & Tremblay, R. E. (2013). Childhood trajectories of inattention, hyperactivity and oppositional behaviors and prediction of substance abuse/dependence: A 15-year longitudinal population-based study. Molecular Psychiatry, 18(7), 806–812. https://doi.org/10.1038/mp.2012.87.
Pinquart, M. (2017). Associations of parenting dimensions and styles with internalizing symptoms in children and adolescents: A meta-analysis. Developmental Psychology, 53(5), 873–932. https://doi.org/10.1037/dev000029.
Pluess, M., & Belsky, J. (2010). Differential susceptibility to parenting and quality child care. Developmental Psychology, 46(2), 379–390. https://doi.org/10.1037/a0015203.
Polic, B., Bubic, A., Mestrovic, J., Markic, J., Kovacevic, T., Juric, M., Tesija, R. A., Susnjar, H., & Kolcic, I. (2016). Late preterm birth is a strong predictor of maternal stress later in life: Retrospective cohort study in school-aged children. Journal of Paediatrics and Child Health, 52, 608–613. https://doi.org/10.1111/jpc.13167.
Potijk, M. R., Kerstjens, J. M., Bos, A. F., Reijneveld, S. A., & De Winter, A. F. (2013). Developmental delay in moderately preterm-born children with low socioeconomic status: Risks multiply. The Journal of Pediatrics, 163(5), 1289–1295. https://doi.org/10.1016/j.jpeds.2013.07.001.
Preacher, K. J., Zyphur, M. J., & Zhang, Z. (2010). A general multilevel SEM framework for assessing multilevel mediation. Psychological Methods, 15(3), 209–233. https://doi.org/10.1037/a0020141.
Preacher, K. J., Zhang, Z., & Zyphu, M. J. (2011). Alternative methods for assessing mediation in multilevel data: The advantages of multilevel SEM. Structural Equation Modeling, 18(2), 161–182. https://doi.org/10.1080/10705511.2011.557329.
Robinson, M., Whitehouse, A. J. O., Zubrick, S. R., Pennell, C. E., Jacoby, P., Mclean, N. J., et al. (2013). Delivery at 37 weeks’ gestation is associated with a higher risk for child behavioural problems. Australian and New Zealand Journal of Obstetrics and Gynaecology, 53, 143–151. https://doi.org/10.1111/ajo.12012.
Rogers, C. E., Barch, D. M., Sylvester, C. M., Pagliaccio, D., Harms, M. P., Botteron, K. N., & Luby, J. L. (2014). Altered gray matter volume and school age anxiety in children born late preterm. The Journal of Pediatrics, 165(5), 928–935. https://doi.org/10.1016/j.jpeds.2014.06.063.
Samra, H. A., McGrath, J. M., & Wey, H. (2010). Are former late-preterm children at risk for child vulnerability and overprotection? Early Human Development, 86, 557–562. https://doi.org/10.1016/j.earlhumdev.2010.07.005.
Schore, A. N. (2001). Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Mental Health Journal, 22(1–2), 7–66. https://doi.org/10.1002/1097-0355(200101/04)22:1<7::AID-IMHJ2>3.0.CO;2-N.
Shelleby, E. C., & Ogg, J. (2020). Longitudinal relationships between parent involvement, parental warmth, ADHD symptoms, and reading achievement. Journal of Attention Disorders, 24(5), 737–749. https://doi.org/10.1177/1087054719859075.
Shiels, K., & Hawk, L. W. (2010). Self-regulation in ADHD: The role of error processing. Clinical Psychology Review, 30(8), 951–961. https://doi.org/10.1016/j.cpr.2010.06.010.
Singer, J. D., & Willett, J. B. (2003). Applied longitudinal data analysis: Modelling change and event occurrence. New York: Oxford University Press.
Smith, M. (2010). Good parenting: Making a difference. Early Human Development, 86, 689–693. https://doi.org/10.1016/j.earlhumdev.2010.08.011.
Statistics Canada. (2016). Preterm live births in Canada, 2000 to 2013. Retrieved from https://www150.statcan.gc.ca/n1/pub/82-625-x/2016001/article/14675-eng.htm
Stene-Larsen, K., Lang, A. M., Landolt, M. A., Latal, B., & Vollrath, M. E. (2016). Emotional and behavioral problems in late preterm and early term births: Outcomes at child age 36 months. BMC Pediatrics, 16, 196. https://doi.org/10.1186/s12887-016-0746-z.
Suttora, C., Spinelli, M., & Monzani, D. (2014). From prematurity to parenting stress: The mediating role of perinatal post-traumatic stress disorder. European Journal of Developmental Psychology, 11(4), 478–493. https://doi.org/10.1080/17405629.2013.859574.
Tallandini, M. A., Morsan, V., Gronchi, G., & Macagno, F. (2015). Systematic and meta-analytic review: Triggering agents of parental perception of child’s vulnerability in instances of preterm birth. Journal of Pediatric Psychology, 40(6), 545–553. https://doi.org/10.1093/jpepsy/jsv010.
Thomasgard, M., & Metz, W. P. (1993). Parental overprotection revisited. Child Psychiatry & Human Development, 24(2), 67–80. https://doi.org/10.1007/BF02367260.
Thomasgard, M., & Metz, W. P. (1996). The 2-year stability of parental perceptions of child vulnerability and parental overprotection. Journal of Developmental and Behavioral Pediatrics, 17(4), 222–228.
Tremblay, R. E., Loeber, R., Gagnon, C., Charlebois, P., Larivée, S., & LeBlanc, M. (1991). Disruptive boys with stable and unstable high fighting behavior patterns during junior elementary school. Journal of Abnormal Child Psychology, 19(3), 285–300. https://doi.org/10.1007/BF00911232.
Treyvaud, K. (2014). Parent and family outcomes following very preterm or very low birth weight birth: A review. Seminars in Fetal and Neonatal Medicine, 19(2), 131–135. https://doi.org/10.1016/j.siny.2013.10.008.
Treyvaud, K., Lee, K. J., Doyle, L. W., & Anderson, P. J. (2014). Very preterm birth influences parental mental health and family outcomes seven years after birth. The Journal of Pediatrics, 164, 515–521. https://doi.org/10.1016/j.jpeds.2013.11.001.
Ungar, M. (2009). Overprotective parenting: Helping parents provide children the right amount of risk and responsibility. The American Journal of Family Therapy, 37(3), 258–271. https://doi.org/10.1080/01926180802534247.
Vismara, L., Rollè, L., Agostini, F., Sechi, C., Fenaroli, V., Molgora, S., Neri, E., Prino, L. E., Odorisio, F., Trovato, A., Polizzi, C., Brustia, P., Lucarelli, L., Monti, F., Saita, E., & Tambelli, R. (2016). Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: A 3-to 6-months postpartum follow-up study. Frontiers in Psychology, 7, 1–10. https://doi.org/10.3389/fpsyg.2016.00938.
Vitaro, F., Gendreau, P. L., Tremblay, R. E., & Oligny, P. (1998). Reactive and proactive aggression differentially predict later conduct problems. Journal of Child Psychology and Psychiatry, 39(3), 377–385. https://doi.org/10.1017/S0021963097002102.
Westrupp, E. M., Mensah, F. K., Giallo, R., Cooklin, A., & Nicholson, J. M. (2012). Mental health in low-to-moderate risk preterm, low birth weight, and small for gestational age children at 4 to 5 years: The role of early maternal parenting. Journal of the American Academy of Child and Adolescent Psychiatry, 51(3), 313–323. https://doi.org/10.1016/j.jaac.2011.12.004.
Wightman, A., Schluchter, M., Drotar, D., Andreias, L., Taylor, H. G., Klein, N., Wilson-Costello, D., & Hack, M. (2007). Parental protection of extremely low birth weight children at age 8 years. Journal of Developmental & Behavioral Pediatrics, 28(4), 317–326. https://doi.org/10.1097/DBP.0b013e3180330915.
Willcutt, E. G. (2012). The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics, 9(3), 490–499. https://doi.org/10.1007/s13311-012-0135-8.
Williams, B., Dunlop, A. L., Kramer, M., Dever, B. V., Hogue, C., & Jain, L. (2013). Perinatal origins of first-grade academic failure: Role of prematurity and maternal factors. Pediatrics, 131(4), 693–700. https://doi.org/10.1542/peds.2012-1408.
World Health Organization. (2018). Preterm birth. Retrieved from https://www.who.int/news-room/fact-sheets/detail/preterm-birth
Woythaler, M. A., McCormick, M. C., & Smith, V. C. (2011). Late preterm infants have worse 24-month neurodevelopmental outcomes than term infants. Pediatrics, 127(3), e622. https://doi.org/10.1542/peds.2009-3598.
Yeung, J. W. K., Chen, H.-F., Lo, H. H. M., & Choi, A. W. M. (2017). Relative effects of parenting practices on child development in the context of family processes. Revista de Psicodidáctica (English Ed.), 22(2), 102–110. https://doi.org/10.1016/j.psicoe.2017.05.003.
Zdebik, M. A., Boivin, M., Battaglia, M., Tremblay, R. E., Falissard, B., & Côté, S. M. (2019). Childhood multi-trajectories of shyness, anxiety and depression: Associations with adolescent internalizing problems. Journal of Applied Developmental Psychology, 64(October), 101050. https://doi.org/10.1016/j.appdev.2019.101050.
Funding
This project was supported by grants from the Ministère de la Famille, the Ministère de l’Éducation et de l’Enseignement supérieur, the Fondation Lucie et André Chagnon, the Institut de recherche Robert-Sauvé en santé et en sécurité du travail, the Centre hospitalier universitaire Sainte-Justine and the Institut de la statistique du Québec, all of whom conducted the Quebec Longitudinal Study of Child Development (QLSCD). Michel Boivin is supported by the Canada Research Chairs (Tier 1) program.
Author information
Authors and Affiliations
Contributions
SF drafted the manuscript; SF and CMG performed statistical analysis and interpreted the data; TML, SC, RT and MB designed the study, contributed to interpretation of data, and provided critical revision. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee of Institut de la statistique du Québec and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Written informed consent was obtained from the participating families at each assessment.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 101 kb)
Rights and permissions
About this article
Cite this article
Faleschini, S., Matte-Gagné, C., Luu, T.M. et al. Trajectories of Overprotective Parenting and Hyperactivity-Impulsivity and Inattention Among Moderate-Late Preterm Children: A Population-Based Study. J Abnorm Child Psychol 48, 1555–1568 (2020). https://doi.org/10.1007/s10802-020-00704-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-020-00704-w