Abstract
Early environmental influences are increasingly of interest in understanding ADHD as a neurodevelopmental condition, particularly in light of recognition that gene by environment interplay are likely involved in this condition. Breastfeeding duration predicts cognitive development, as well as development of brain white matter connectivity, in areas similar to those seen in ADHD. Prior studies show an association between breastfeeding and ADHD but without adequate evaluation of ADHD. A case control cohort of 474 children aged 7–13 years was examined, 291 with wellcharacterized ADHD (71.5 % male) and the rest typically developing controls (51.9 % male). Mothers retrospectively reported on breast feeding initiation and duration. Initiation of breastfeeding was not associated with child ADHD, but shorter duration of breastfeeding was associated with child ADHD with a medium effect size (d = 0.40, p < 0.05); this effect held after covarying a broad set of potential confounders, including child oppositional defiant and conduct problems and including maternal and paternal ADHD symptoms. Effects were replicated across both parent and teacher ratings of child ADHD symptoms. Shorter duration of breastfeeding is among several risk factors in early life associated with future ADHD, or else longer duration is protective. The direction of this effect is unknown, however. It may be that some children are more difficult to breastfeed or that breastfeeding provides nutrients or other benefits that reduce future chance of ADHD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Neurodevelopmental disorders like ADHD likely emanate from the interplay of genetic and environmental factors, perhaps via epigenetic mechanisms. Determination of early experiential correlates is thus crucial. While there has been substantial focus on perinatal and delivery problems in ADHD (Astbury, Orgill, and Bajuk 1987; Ben Amor et al. 2005; Kotimaa et al. 2003; McGrath, Sullivan, Lester, and Oh 2000; Mick, Biederman, Faraone, Sayer, and Kleinman 2002; Milberger, Biederman, Faraone, Guite, and Tsuang 1997), postnatal correlates in the first year of life are less well studied. Yet the importance of postnatal, or early infant, programming of later disease risk is now relatively well-recognized (Kaplan, Evans, and Monk 2008; Wells, Chomtho, and Fewtrell 2007). Etiology of neurodevelopmental conditions such as ADHD likely involves both pre- and post-natal inputs.
Because ADHD is thought to be rooted in altered neural development, early experiences that support neurodevelopment are of particular interest. Perhaps the best-studied early post-natal influence, aside from socialization itself, is initiation and duration of breastfeeding. It can be noted that breastfeeding and psychosocial influences are not entirely distinct. For example, whereas much research on the benefits of breastfeeding focuses on the nutritional and immunological advantages of breast milk, especially the impact of long-chain polyunsaturated fatty acids (e.g., omega 3 fatty acids; (Forsyth et al. 2003; Willatts et al. 2013), breastfeeding may also promote or be associated with the development of healthy infant-mother attachments highlighted by enhanced maternal sensitivity and responsiveness to the infant (Allen, Lewinsohn, and Seeley 1998).
In relation to ADHD, breastfeeding initiation or duration are expected to be particularly important among early experiences for several reasons. First, at a general level, ADHD is a neurodevelopmental disorder theorized to emanate from suboptimal early neural development. The early postnatal period is characterized by continued developmental plasticity; nutrition is among the most important supports for such development, such that suboptimal infant nutrition can induce adaptations that may be detrimental to brain development. Breast milk is the best source of nutrition for most infants because of its unique composition (Ballard and Morrow 2013). By extension, breastfeeding onset or duration should influence neurodevelopmental risk.
Second, ADHD is associated with higher order cognitive delays, including subtle reduction in IQ. Consistent with the preceding, breastfeeding predicts subsequent cognitive outcomes in children (Al Hamed, Taha, Sabra, and Bella 2008; Huang, Peters, Vaughn, and Witko 2014; Quigley et al. 2012), an effect that tends to be dose-dependent in relation to duration of breastfeeding, as noted in a meta-analysis over a decade ago (Anderson, Johnstone, and Remley 1999). Subsequently, this picture has grown stronger. Effects on cognition appear especially important for boys (Oddy, Li, Whitehouse, Zubrick, and Malacova 2011); ADHD is more common in boys than girls. National and international health organizations recommend that almost all infants be exclusively breastfed for the first 6 months of life to achieve optimal growth, development, and health (American Academy of Family Physicians 2007; American College of Obstetricians Gynecologists 2007; American Public Health Association 2007; Gartner et al. 2005). When infants are breastfed for at least 6 months, cognitive gains are apparent and persistent in childhood (Angelsen, Vik, Jacobsen, and Bakketeig 2001; Huang et al. 2014; Oddy et al. 2011; Wigg et al. 1998). Moreover, in the United States, only about half of mothers maintain some breastfeeding for at least 6 months (Center for Disease Control 2013), suggesting widespread opportunity for susceptible infants to be exposed to reduced breastfeeding, if in fact reduced breastfeeding is part of the developmental risk profile or ADHD.
Third, duration of breastfeeding has been associated directly with subsequent human brain development, particularly white matter development in infants and toddlers (Herba et al. 2013; Tawia 2013). More recently, it is notable that breastfeeding duration was associated with increased white matter development in 8 year-old children (although again, mainly in boys) in key fiber tracts including superior longitudinal fasciculus, cingulum, body of corpus callosum, and posterior thalamic radiations (Ou et al. 2014). These brain regions are similar to brain regions with altered white matter development in 8 year-olds with ADHD that we observed previously (Nagel et al. 2011).
Thus, we suspect that breastfeeding or breastfeeding duration, particularly beyond 6 months, is crucial not only for neurodevelopment and cognition generally, but for the particular aspects of neural development and connectivity that support self-regulation and self-control, and when they are perturbed, contribute to emergence of the ADHD syndrome. A steady supply of adequate nutrients and other bioactive components may be crucial to support brain development, particularly white matter growth, during the critical first 9 months of life.
While the preceding pieces of evidence are rather circumstantial, direct support for this basic proposal of an association between breastfeeding and ADHD has begun to emerge. Findings that children with ADHD were less likely than other children to be breastfed for the recommended 6-month period were noted in retrospective, maternal-recall studies in Turkey (Sabuncuoglu, Orengul, Bikmazer, and Kaynar 2014), a community study in Iran (Golmirzaei et al. 2013), clinic referrals in Israel (Mimouni-Bloch et al. 2013), school children in Egypt, (Al Hamed et al. 2008), a case control study in Poland (Kadziela-Olech and Piotrowska-Jastrzebska 2005), a hospital chart review in Alabama (Field 2014), a community study in Saudi Arabia (Al Hamed et al. 2008), as well as a prospective study of 4 year olds in Spain (Julvez et al. 2007). The association between breastfeeding and reduced likelihood of child ADHD is also supported by two population wide surveys, one in Germany (Schmitt and Romanos 2012) and one in the United States (Shamberger 2012).
However, a key limitation is that in none of these studies was ADHD fully evaluated by accepted research criteria; all relied on single questionnaires of ADHD symptoms or on clinician evaluations using unspecified methods and criteria. None of the prior studies appeared to complete full, state of the art evaluations of ADHD using multiple informants and structured clinical interviews, leaving them vulnerable to informant-effects and false-positives. There is also a dearth of data on the association between breastfeeding duration and ADHD in North America, where ADHD, which has been increasing in prevalence over time, and is now identified in over ten percent of youth (Visser et al. 2014).
Clarifying and confirming this association would help further the specification of early life mechanisms and processes that may influence not only self-regulation, but also ADHD. The present study sought, in a retrospective case–control design with extensive, standardized, formal evaluation of ADHD, to address the basic question: Do mothers of children with well-characterized ADHD initiate breastfeeding less frequently and maintain breastfeeding for shorter periods of time than mothers of typically developing children?
Method
Participants
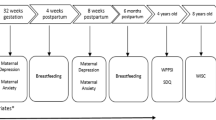
Participants included 474 children, aged 7–13 years; 291 met DSM-5 (American Psychiatric Association, 2013) criteria for ADHD (232 combined presentation, 59 inattentive presentation of whom 208 (71.5 %) were male), and 183 were non-ADHD, typically developing comparison youth of whom 95 (51.9 %) were male. To meet criteria for the combined presentation, children had six or more symptoms of inattention and hyperactivity/impulsivity, while to meet criteria for the inattentive presentation, children had six or more symptoms of inattention without the requisite number of hyperactivity/impulsivity symptoms, per DSM-5 (American Psychiatric Association, 2013). The mother of each child reported their recalled information about breastfeeding initiation and duration.
Recruitment and Identification
Families were recruited through advertisements and mailings to obtain a broadly representative sample that would not be biased by clinic referred youth. Families volunteering for the study completed a multi-gate screening process to establish eligibility and diagnostic group assignment. A structured clinical diagnostic interview with the primary caregiver (Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version [KSAD-S-E]; (Puig-Antich and Kiddie 1996), parent and teacher standardized ratings (Conners 2008; DuPaul, Power, Anastopoulos, and Reid 1998), and an IQ screen were completed. The KSADS interviewer and the child test administrator observed the child briefly and made detailed notes on the parent and child visit as well. KSADS interviewers were reliability checked against a gold-standard interviewer to achieve inter-interviewer reliability on ADHD and all other child diagnoses (all trained to a standard of κ > 0.70 on all disorders observed in our sample at greater than five percent base rate). Clinical interviewers were regularly monitored and fidelity checks were carried out by supervisor review of videotapes, and re-calibration training was conducted annually.
A clinical diagnostic team comprising a board-certified psychiatrist and licensed clinical psychologist independently reviewed all case information, including behavioral observations, to arrive at diagnoses using DSM IV (American Psychiatric Association 1994) and DSM-5 (American Psychiatric Association, 2013) criteria. Their agreement rate was acceptable for all child diagnoses with base rates greater than five percent in the sample (all κ > 0.75), and agreement for child ADHD was also acceptable (all κ > 0.80).
Parental Psychopathology
The most parsimonious explanation of any ante-natal correlate of ADHD is passive gene-environment correlation (rGE), in that parents with ADHD may both transmit ADHD to the offspring and fail to breastfeed. To provide partial control against this possibility, parent symptoms of ADHD were obtained by parent self-report on the ADHD Rating Scale (DuPaul et al. 1998) adapted for adults. When self-report was not available, spousal report was obtained. Parental ADHD diagnosis was also obtained on a structured clinical interview (KSADS-E, adapted), but because it was less strongly related to breastfeeding and child ADHD, it was omitted from analysis in lieu of the parent symptom scores to provide a stronger test of the primary hypothesis. Because maternal depression could account for discontinuation of breastfeeding, maternal major depression (lifetime) was evaluated via clinician-administered Structured Clinical Interview for DSM Disorders (SCID) (First, Spitzer, Gibbon, and Williams 2002). Paternal depression was not theorized to influence duration of breastfeeding and so was not studied here.
Ethical Standards
The study was approved by the Oregon Health & Science University Institutional Review Board and all procedures conformed to the American Psychological Association Ethical Principles of Psychologists and Code of Conduct (American Psychology Association 2002) and NIH guidelines for protection of human subjects. Parents provided written informed consent and children provided written informed assent, before participating in any study-related activities.
Exclusion Criteria
Children were excluded if parents reported a history of neurological impairments, seizures, traumatic brain-injury, other major medical impairments, or long-acting psychoactive medication use (not including stimulants); if the clinical diagnostic team identified current mood disorder, lifetime history of any psychosis, or pervasive developmental disorder, or “sub-threshold” ADHD (defined as five symptoms of either inattention or hyperactivity-impulsivity), or if estimated IQ < 75. In addition, typically developing control children were required to have no prior diagnosis of ADHD, to have four or fewer symptoms of both inattention and hyperactivity-impulsivity, and to not meet criteria for conduct disorder. Their other psychiatric diagnoses were free to vary, to avoid a super-normal comparison group.
Assessment of Breastfeeding Duration
Breastfeeding duration was assessed retrospectively by a single item on our developmental history form, in which the mother was asked “To what extent was this baby breastfed?” The response options were 0 months or not breastfed, 1–3, 4–6, 7–12, 13–18, or 19+ months of breastfeeding. The literature suggests that maternal recall of breastfeeding duration is valid even over several years, agreeing with prospective assessment at κ > 0.8 (Li, Scanlon, and Serdula 2005; Natland, Andersen, Nilsen, Forsmo, and Jacobsen 2012). Although a primary predictor of inaccurate recall is having four or more children,(Cupul-Uicab, Gladen, Hernandez-Avila, and Longnecker 2009) in the present sample 94 % of mothers had fewer than four children.
Data Reduction and Data Analysis
Data Reduction
All data were double entered to prevent data entry errors. Data were evaluated for outliers and appropriate distributions for the procedures at hand. The breastfeeding and ADHD rating scale scores in particular were scrutinized; these variables had satisfactory skew (all skew ≤ 0.40 except parent rated hyperactivity, with moderate skew = 0.7), and kurtosis (range −1.3 to −0.88). To evaluate child ADHD categorically, we utilized the diagnostic team consensus diagnosis, which relied on all available information but was blind to breastfeeding history. To evaluate child ADHD symptoms dimensionally, we utilized parent and teacher ratings of child ADHD symptoms using the ADHD Rating Scale (DuPaul et al. 1998) total raw score (each ranging 0–27). These were analyzed separately to enable disaggregating of reporter effects and remove source-variance confound.
Data Analysis
ANCOVA was used to examine group differences while controlling covariates. Follow-up categorical analyses examined whether mothers of children with ADHD were less likely to initiate breastfeeding or to breastfeed for at least 6 months using logistic regression. Parental ADHD-rating scale T-scores served as a covariate as noted earlier. To examine continuous symptom dimensions as outcomes, multiple regression was utilized.
Covariates
With respect to relevant covariates, the following were significantly associated with child ADHD diagnosis: maternal ADHD-Rating Scale total symptom T-scores (p = 0.02), paternal ADHD-Rating Scale total symptom T-scores (p < 0.001), maternal lifetime major depressive disorder (p = 0.01), child sex (p < 0.001), child IQ (p < 0.001), child age (p = 0.01), child anxiety disorder (p < 0.01), and child ODD/CD (p < 0.001). All were included as covariates, therefore, in all models described below. All other potential covariates were not significantly associated with child ADHD (all p > 0.10) and were not examined further.
Results
Study Participant Demographic and Clinical Characteristics
Of the 474 children included in the study, 291 (61.39 %) met formal study criteria for ADHD; the other children included met criteria for our typically developing control group. Table 1 presents demographic and diagnostic characteristics of the sample by group, as well as group differences in these characteristics. In brief, consistent with population prevalence data (and as expected, therefore, from our community recruitment strategy), children with ADHD were more likely than typically developing children to be male, to have a comorbid diagnosis of ODD/CD or an anxiety disorder, to have a lower IQ, to come from lower income families, and to have more ADHD symptoms in parents.
Initiation and Duration of Breastfeeding by Child ADHD Diagnosis
Table 1 summarizes the initiation and duration of breastfeeding data. Initiation of breastfeeding (yes/no) did not differ significantly by child diagnostic group, X 2(1) = 2.63, p = 0.105. However, duration of breastfeeding did. Mothers of children with ADHD reported shorter breastfeeding duration. Assuming the median of each category selected, we estimated that mothers of children with ADHD breastfed for, M = 4.45 months, SD = 1.21 (modal range = 4–6 months; 26 % breast fed for longer than 6 months (7–12 months or longer), compared to mothers of typically developing children, M = 7.21 months, SD = 1.21 (modal range = 7–12 months; 32 % 6 months or longer); F(1472) = 16.67, p = 0.001, Cohen’s d = 0.38. Inclusion of all relevant covariates as noted in methods did not materially change this result, F(1461) = 2.55, p = 0.02, Cohen’s d = 0.41.
With regard to the recommended 6 months duration of breastfeeding (yes/no), the picture was the same. Mothers of children with ADHD (48.5 %) were less likely than mothers of non-ADHD youngsters (65.6 %) to report having breastfed for at least 6 months, X 2(1) = 13.31, p < 0.001, OR = 0.50 (95 % CI = 0.34–0.72). The effect also held with covariates included in a logistic regression model, R 2 = 0.22, Wald = 7.98, beta = 0.562, p < 0.005, OR = 0.56, 95 % CI = 0.39–0.76.
To further evaluate the role of breastfeeding in relation to maternal and child ADHD symptoms, we conducted a logistic regression-based mediation analysis using the PROCESS macro in SPSS (utilizing 1000 bootstrap iterations; Hayes, 2013; Preacher and Hayes 2004). Both the direct effect of maternal ADHD symptoms, beta = 0.816, p < 0.005, z = 2.94, 95 % CI = 0.27–1.34, as well as the indirect effect of duration of breastfeeding, beta = −0.282, p < 0.001, z = 4.11, 95 % CI = −0.41–0.15, were statistically reliable predictors of child ADHD diagnosis, McFadden’s R 2 = 0.059, p < 0.01, suggesting that shortened duration of breastfeeding also may partially mediate inter-generational transmission of ADHD.
Duration of Breastfeeding by Child ADHD Symptom Domains
In regression models detailed in Table 2 we examined the distinct ADHD symptom domains of inattention-disorganization and hyperactivity-impulsivity separately. An association between shorter breastfeeding duration and more child total ADHD symptoms held across both symptom domains and replicated in parent and teacher report of ADHD.
Discussion
Breastfeeding is one of the most widely studied and important influences not only on infant health but on early cortical development and thus, likely on self-regulation and neurodevelopmental conditions. While it may be a proxy for a number of other variables—including socio-economic status or parental psychopathology, and while its mechanisms may be biological (protective effects of breast milk; e.g., via long chain polyunsaturated fatty acids; for a review see (Koletzko et al. 2008)) or psychological (maternal-child contact), establishing its association is necessary to flesh out these diverse models of early emergence of ADHD risk. Because of this, investigations of breastfeeding and ADHD have begun to draw interest. However, to date, no study has examined a well-characterized cohort with carefully validated ADHD diagnoses. The present study’s main contribution is to fill in this critical gap.
While our main contribution to this question is to provide data using a very well- characterized sample of ADHD and control children, our primary limitation was reliance on retrospective recall of breastfeeding practice through use of a single questionnaire item to assess initiation and duration of breastfeeding; the present study also did not examine the duration of exclusive breastfeeding. However, prior literature suggests that maternal recall of breastfeeding initiation and duration is reasonably accurate, provided relatively small family sizes, as is the case in our sample (Li et al. 2005). Further, the present results converge with prior findings using other kinds of methods and samples and controlling for exclusivity of breastfeeding, but lacking our strong ADHD-related analysis.
With that in mind, the present findings are notable. First, a reliable association was seen between maternally recalled breastfeeding duration and carefully characterized ADHD status in children, supporting the contention that breastfeeding may be an important early addition to ADHD risk and protective factors. Second, the result was robust to a wide range of covariates, including maternal and paternal ADHD symptom level, family size, family composition, parental education, and family income.
Additional research is needed to determine the direction of this effect, as to whether it is driven by child or maternal characteristics or both. It remains possible that children who are going to develop ADHD are more difficult to breastfeed, leading to reduced breastfeeding duration. The present work taken together with other studies in the literature would justify undertaking such prospective studies, which would enable more extensively detailing reasons why breastfeeding is not initiated or is discontinued, what support is provided to each mother to promote and maintain breastfeeding, and more fully characterize breastfeeding practice including: exclusivity versus partial breastfeeding, feeding pumped (expressed) breast milk, and the use of breast milk obtained from breast milk banks in relation to ADHD outcome.
Furthermore, we do not know whether the breastfeeding association is causal or is explained by effects such as passive gene-environment correlation (rGE). While our ability to rule out parental ADHD or ADHD symptoms as an explanation for the present finding provides some assurance that the effects are not simply passive rGE, they do not do so definitively. Complex reasons are associated with the decision to initiate and continue breastfeeding. Direct, causally informative designs, such as sibling comparisons, are still needed to examine this potential effect, now that it has been supported using a retrospective approach. Causally informative designs of this nature have supported a causal association of low birth weight with ADHD (Thapar et al. 2009) but called into question the association of maternal smoking in pregnancy with ADHD (D’Onofrio et al. 2008; Thapar et al. 2009).
Third, it was striking that the association of breastfeeding duration with ADHD was at least partially specific to symptoms of inattention and hyperactivity/impulsivity. Specifically, the effect held even when controlling for child disruptive behavior problems, although there was also a small concurrent association with child oppositional defiant symptoms in some models. This pattern of results may echo other early developmental associations that suggest partially distinct early associations between ADHD and disruptive problems, particularly oppositional defiant disorder. For example, low birth weight appears to be somewhat more strongly associated with ADHD than with oppositional defiant disorder, whereas the opposite pattern holds for smoking in pregnancy (Nigg and Breslau 2007). This type of partial dissociation may help with the gradual development of etiological models that partially differentiate the neurodevelopmental disorders such as ADHD, from relatively psychosocially amplified secondary complications such as ODD and CD (Nigg 2003). However, the etiological interplay of emotional irritability (a possible temperamental root of ODD that overlaps with ADHD) and dysregulation (as a possible neuro-developmental root of ADHD) requires more investigation to explore these speculations (Karalunas et al. 2014; Shaw, Stringaris, Nigg, and Leibenluft 2014).
At the same time, the emerging picture regarding ADHD and breastfeeding from our work here and the literature that preceded us raises other questions. If breastfeeding is causally associated with ADHD, its effect is likely to be part of a liability (or else susceptibility) by experience interplay (or more narrowly, genotype by environment interplay). In that regard, it is likely that for many children, duration of breastfeeding does not lead to ADHD, whereas for others, it may be an important additional risk or protective factor that interacts with pre-existing liability. Examination of breastfeeding in gene x environment interaction studies will be of keen interest. In summary, the present study suggests that claims of an association between breastfeeding duration and child ADHD are valid. Additional focus on early infant developmental risk factors for ADHD appears to be an important future direction for the field.
References
Al Hamed, J. H., Taha, A. Z., Sabra, A. A., & Bella, H. (2008). Attention deficit hyperactivity disorder (ADHD) among male primary school children in Dammam, Saudi Arabia: prevalence and associated factors. Journal Egypt Public Health Association, 83, 165–182.
Allen, N. B., Lewinsohn, P. M., & Seeley, J. R. (1998). Prenatal and perinatal influences on risk for psychopathology in childhood and adolescence. Journal Development and Psychopathology, 10, 513–529.
American Academy of Family Physicians. (2007). Breastfeeding, family physicians supporting (Position paper). Retrieved July, 20, 2014, from http://www.aafp.org/about/policies/all/breastfeeding-support.html.
American College of Obstetricians Gynecologists. (2007). Committee opinion no. 361: breastfeeding: maternal and infant aspects. Obstetrics & Gynecology Journal, 109, 479–480.
American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders. 5th Edition. Washington, DC; Author.
American Psychology Association. (2002). Ethical principles of psychologists and code of conduct. American Psychology Association, 57, 1060–1073.
American Public Health Association. (2007). Policy statement database: A call to action on breastfeeding: A fundamental public health issue. Policy number 200714. Policy Date: November 6, 2007 Retrieved July 20, 2014, from www.apha.org/advocacy/policy/policysearch/default.htm?id=1360.
Anderson, J. W., Johnstone, B. M., & Remley, D. T. (1999). Breast-feeding and cognitive development: a meta-analysis. American Journal of Clinical Nutrition, 70, 525–535.
Angelsen, N. K., Vik, T., Jacobsen, G., & Bakketeig, L. S. (2001). Breast feeding and cognitive development at age 1 and 5 years. Archives of Disease in Childhood, 85, 183–188.
Astbury, J., Orgill, A., & Bajuk, B. (1987). Relationship between 2-year behaviour and neurodevelopmental outcome at 5 years of very low-birthweight survivors. Developmental Medicine and Child Neurology, 29, 370–379.
Ballard, O., & Morrow, A. L. (2013). Human milk composition: nutrients and bioactive factors. Pediatric Clinics of North America, 60, 49–74. doi:10.1016/j.pcl.2012.10.002.
Ben Amor, L., Grizenko, N., Schwartz, G., Lageix, P., Baron, C., Ter-Stepanian, M., Zappitelli, M., Mbekou, V., & Joober, R. (2005). Perinatal complications in children with attention-deficit hyperactivity disorder and their unaffected siblings. Journal of Psychiatry & Neuroscience, 30, 120–126.
Center for Disease Control. (2013). Breastfeeding report card. Last updated : July 31, 2013. Retrieved July, 20, 2014, from http://www.cdc.gov/breastfeeding/data/reportcard.htm.
Conners, K. C. (2008). Multi-Health Systems, Inc. New York.
Cupul-Uicab, L. A., Gladen, B. C., Hernandez-Avila, M., & Longnecker, M. P. (2009). Reliability of reported breastfeeding duration among reproductive-aged women from Mexico. Maternal & Child Nutrition, 5, 125–137.
D’Onofrio, B. M., Van Hulle, C. A., Waldman, I. D., Rodgers, J. L., Harden, K. P., Rathouz, P. J., & Lahey, B. B. (2008). Smoking during pregnancy and offspring externalizing problems: an exploration of genetic and environmental confounds. Development and Psychopathology, 20, 139–164. doi:10.1017/S0954579408000072.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (1998). ADHD rating scale-IV: Checklists, norms, and clinical interpretation. New York: Guilford Press.
Field, S. S. (2014). Interaction of genes and nutritional factors in the etiology of autism and attention deficit/hyperactivity disorders: a case control study. Journal of Medical Hypotheses, 82, 654–661.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (2002). Structured clinical interview for DSM-IV-TR axis I disorders (Vol. Research Version, (SCID-I/NP) Biometrics Research). New York: New York State Psychiatric Institute.
Forsyth, J. S., Willatts, P., Agostoni, C., Bissenden, J., Casaer, P., & Boehm, G. (2003). Long chain polyunsaturated fatty acid supplementation in infant formula and blood pressure in later childhood: follow up of a randomised controlled trial. British Medical Journal, 326, 953. doi:10.1136/bmj.326.7396.953.
Gartner, L. M., Morton, J., Lawrence, R. A., Naylor, A. J., O’Hare, D., Schanler, R. J., & Eidelman, A. I. (2005). Breastfeeding and the use of human milk. Pediatrics, 115, 496–506.
Golmirzaei, J., Namazi, S., Amiri, S., Zare, S., Rastikerdar, N., Hesam, A. A., Rahami, Z., Ghasemian, F., Namazi, S. S., Paknahad, A., Mahmudi, F., Mahboobi, H., Khorgoei, T., Niknejad, B., Dehghani, F., & Asadi, S. (2013). Evaluation of attention-deficit hyperactivity disorder risk factors. International Journal of Clinical Pediatrics, 953103, 953103.
Hayes, A.F. & Scharkow, M. (2013). The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: does method really matter? Psychological Science, 24, 1918-1927.
Herba, C. M., Roza, S., Govaert, P., Hofman, A., Jaddoe, V., Verhulst, F. C., & Tiemeier, H. (2013). Breastfeeding and early brain development: the generation R study. Maternal & Child Nutrition, 9, 332–349. doi:10.1111/mcn.12015.
Huang, J., Peters, K. E., Vaughn, M. G., & Witko, C. (2014). Breastfeeding and trajectories of children’s cognitive development. Journal Developmental Science, 17, 452–461. doi:10.1111/desc.12136.
Julvez, J., Ribas-Fito, N., Forns, M., Garcia-Esteban, R., Torrent, M., & Sunyer, J. (2007). Attention behaviour and hyperactivity at age 4 and duration of breast-feeding. Acta Paediatrica, 96, 842–847. doi:10.1111/j.1651-2227.2007.00273.x.
Kadziela-Olech, H., & Piotrowska-Jastrzebska, J. (2005). The duration of breastfeeding and attention deficit hyperactivity disorder. Rocz Akad Med Bialymst Journal, 50, 302–306.
Kaplan, L. A., Evans, L., & Monk, C. (2008). Effects of mothers’ prenatal psychiatric status and postnatal caregiving on infant biobehavioral regulation: can prenatal programming be modified? Early Human Development, 84, 249–256.
Karalunas, S. L., Fair, D., Musser, E. D., Aykes, K., Iyer, S. P., & Nigg, J. T. (2014). Subtyping attention-deficit/hyperactivity disorder using temperament dimensions: toward biologically based nosologic criteria. JAMA Psychiatry, 9, 763.
Koletzko, B., Lien, E., Agostoni, C., Bohles, H., Campoy, C., Cetin, I., Decsi, T., Dudenhausen, J. W., Dupont, C., Forsyth, S., Hoesli, I., Holzgreve, W., Lapillonne, A., Putet, G., Secher, N. J., Symonds, M., Szajewska, H., Willatts, P., Uauy, R., & World Association of Perinatal Medicine Dietary Guidelines Working, G. (2008). The roles of long-chain polyunsaturated fatty acids in pregnancy, lactation and infancy: review of current knowledge and consensus recommendations. Journal of Perinatal Medicine, 36, 5–14. doi:10.1515/JPM.2008.001.
Kotimaa, A. J., Moilanen, I., Taanila, A., Ebeling, H., Smalley, S. L., McGough, J. J., Hartikainen, A. L., & Jarvelin, M. R. (2003). Maternal smoking and hyperactivity in 8-year-old children. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 826–833.
Li, R., Scanlon, K. S., & Serdula, M. K. (2005). The validity and reliability of maternal recall of breastfeeding practice. Nutrition Reviews, 63, 103–110.
McGrath, M. M., Sullivan, M. C., Lester, B. M., & Oh, W. (2000). Longitudinal neurologic follow-up in neonatal intensive care unit survivors with various neonatal morbidities. Pediatrics, 106, 1397–1405.
Mick, E., Biederman, J., Faraone, S. V., Sayer, J., & Kleinman, S. (2002). Case–control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancy. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 378–385.
Milberger, S., Biederman, J., Faraone, S. V., Guite, J., & Tsuang, M. T. (1997). Pregnancy, delivery and infancy complications and attention deficit hyperactivity disorder: issues of gene-environment interaction. Biological Psychiatry, 41, 65–75.
Mimouni-Bloch, A., Kachevanskaya, A., Mimouni, F. B., Shuper, A., Raveh, E., & Linder, N. (2013). Breastfeeding may protect from developing attention-deficit/hyperactivity disorder. Breastfeed Medicine Journal, 8, 363–367.
Nagel, B. J., Bathula, D., Herting, M., Schmitt, C., Kroenke, C. D., Fair, D., & Nigg, J. T. (2011). Altered white matter microstructure in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 283–292. doi:10.1016/j.jaac.2010.12.003.
Natland, S. T., Andersen, L. F., Nilsen, T. I., Forsmo, S., & Jacobsen, G. W. (2012). Maternal recall of breastfeeding duration 20 years after delivery. BMC Medical Research Methodology, 12, 179.
Nigg, J. T. (2003). Response inhibition and disruptive behaviors: toward a multi-process conception of etiological heterogeneity for ADHD combined type and conduct disorder early onset type. Annals of the New York Academy of Sciences, 1008, 170–182.
Nigg, J. T., & Breslau, N. (2007). Prenatal smoking exposure, low birth weight, and disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 362–369.
Oddy, W. H., Li, J., Whitehouse, A. J., Zubrick, S. R., & Malacova, E. (2011). Breastfeeding duration and academic achievement at 10 years. Pediatrics, 127, e137–e145. doi:10.1542/peds. 2009-3489.
Ou, X., Andres, A., Cleves, M. A., Pivik, R. T., Snow, J. H., Ding, Z., & Badger, T. M. (2014). Sex-specific association between infant diet and white matter integrity in 8-y-old children. Pediatric Research. doi:10.1038/pr.2014.129.
Preacher, K. L. & Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods Instruments & Computers, 36(4), 717-731.
Puig-Antich, J. R., & Kiddie, N. (1996). Schedule for affective disorders and schizophrenia. Pittsburgh: Western Psychiatric Institute.
Quigley, M. A., Hockley, C., Carson, C., Kelly, Y., Renfrew, M. J., & Sacker, A. (2012). Breastfeeding is associated with improved child cognitive development: a population-based cohort study. The Journal of Pediatrics, 160, 25–32. doi:10.1016/j.jpeds.2011.06.035.
Sabuncuoglu, O., Orengul, C., Bikmazer, A., & Kaynar, S. Y. (2014). Breastfeeding and parafunctional oral habits in children with and without attention-deficit/hyperactivity disorder. Breastfeed Medicine Journal, 9, 244–250.
Schmitt, J., & Romanos, M. (2012). Prenatal and perinatal risk factors for attention-deficit/hyperactivity disorder. Archives of Pediatrics and Adolescent Medicine, 166, 1074–1075.
Shamberger, R. (2012). Attention-deficit disorder associated with breast-feeding: a brief report. Journal of the American College of Nutrition, 31, 239–242.
Shaw, P., Stringaris, A., Nigg, J., & Leibenluft, E. (2014). Emotion dysregulation in attention deficit hyperactivity disorder. American Journal of Psychiatry, 171, 276–293.
Tawia, S. (2013). Breastfeeding, brain structure and function, cognitive development and educational attainment. Breastfeeding Review, 21, 15–20.
Thapar, A., Rice, F., Hay, D., Boivin, J., Langley, K., van den Bree, M., Rutter, M., & Harold, G. (2009). Prenatal smoking might not cause attention-deficit/hyperactivity disorder: evidence from a novel design. Biological Psychiatry, 66, 722–727. doi:10.1016/j.biopsych.2009.05.032.
Visser, S. N., Danielson, M. L., Bitsko, R. H., Holbrook, J. R., Kogan, M. D., Ghandour, R. M., Perou, R., & Blumberg, S. J. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child and Adolescent Psychiatry, 53(34–46), e32. doi:10.1016/j.jaac.2013.09.001.
Wells, J. C., Chomtho, S., & Fewtrell, M. S. (2007). Programming of body composition by early growth and nutrition. Proceedings of the Nutrition Society, 66, 423–434.
Wigg, N. R., Tong, S., McMichael, A. J., Baghurst, P. A., Vimpani, G., & Roberts, R. (1998). Does breastfeeding at 6 months predict cognitive development? Australian and New Zealand Journal of Public Health, 22, 232–236.
Willatts, P., Forsyth, S., Agostoni, C., Casaer, P., Riva, E., & Boehm, G. (2013). Effects of long-chain PUFA supplementation in infant formula on cognitive function in later childhood. American Journal of Clinical Nutrition, 98, 536s–542s. doi:10.3945/ajcn.112.038612.
Acknowledgments
DDS, KH, JS, JTN designed the research; EDM conducted research; EDM, JTN analyzed data; DDS, EDM, JTN wrote the paper and had primary responsibility for the final content. All authors read and approved the final manuscript.
Conflict of Interest
The authors report no conflicts of interest. This work was supported by NIMH MH59105 (Nigg) and by the Bob and Charlee Moore Institute for Nutrition & Wellness at Oregon Health & Science University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stadler, D.D., Musser, E.D., Holton, K.F. et al. Recalled Initiation and Duration of Maternal Breastfeeding Among Children with and Without ADHD in a Well Characterized Case–Control Sample. J Abnorm Child Psychol 44, 347–355 (2016). https://doi.org/10.1007/s10802-015-9987-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-015-9987-9