Abstract
Purpose
To evaluate the clinical outcomes following bilateral implantation of the AcrySof™ IQ Vivity™ toric extended depth of focus (EDOF) intraocular lens (IOL).
Design
Prospective interventional case series.
Methods
Patients with bilateral significant cataracts and pre-existing corneal astigmatism underwent cataract surgery and implantation with the AcrySof™ IQ Vivity™ toric IOL. Dominant eyes were targeted at emmetropia and non-dominant eyes at -0.50D. Primary endpoints were binocular uncorrected distance (UDVA), intermediate (UIVA at 66 cm) and near (UNVA at 40 cm) acuities at 3 months. Secondary outcomes were corrected distance (CDVA), distance corrected intermediate (DCIVA) and distance corrected near (DCNVA), refractive predictability, rotational stability, binocular defocus curve, contrast sensitivity, Questionnaire for Visual Disturbances (QUVID) and Visual Function Index (VF-14) questionnaire scores. All visual acuities were converted to logarithm of minimum angle of resolution (logMAR) for analysis.
Results
30 patients underwent uneventful phacoemulsification. The mean binocular UDVA, UIVA and UNVA were 0.06 ± 0.12, 0.11 ± 0.10 and 0.26 ± 0.10 respectively. The mean refractive spherical equivalent (MRSE) for dominant and non-dominant eyes were − 0.07D ± 0.27 and − 0.12D ± 0.54 respectively. 92.4% of dominant eyes and 84.6% of non-dominant eyes within 0.50D of target. The mean IOL rotation was 3.85° ± 5.09 with 86.7% of eyes with less than 5° of rotation. 26.7%, 20% and 36.7% of patients reported starbursts, haloes and glare respectively. The mean VF-14 score was 91.77.
Conclusion
Bilateral implantation of the AcrySof™ IQ Vivity™ Toric IOL resulted in very good unaided visual acuities for far and intermediate distance with functional near vision. Dysphotopsias were reported but despite this, a high level of visual function was achieved.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The relentless pursuit for presbyopia correction after cataract surgery has resulted in continuous innovation in the field of intraocular lens (IOL) technology. This segment of presbyopia correcting intraocular lenses (PCIOL) has seen in recent years, the introduction of extended depth of focus (EDOF) [1]. IOLs which has created another option for patients seeking more spectacle independence after cataract surgery.
The conventional design for PCIOLs have utilised diffractive or refractive technology to achieve multifocality but this results in photic phenomena such as haloes, starbursts and glare [2]. Together with the loss of contrast sensitivity also inherent to such IOL designs, these phenomena restrict the use of such IOLs in certain individuals who are more demanding or in those who have had previous refractive surgery or other ocular pathology.
A new EDOF IOL entered the market recently which utilises a novel optical design to achieve an extended range of vision for the patient. The AcrySof™ IQ Vivity™ (Alcon Laboratories, Inc.) is a non-diffractive UV-absorbing and blue light filtering hydrophobic aspheric IOL which has been reported to provide an extended range of vision with a low incidence of visual disturbances. In the United States Food and Drug Administration (USFDA) trials [3], all eyes had refractive target of emmetropia and the intermediate and near vision were significantly better than a monofocal IOL but near vision was not as good as what can be achieved with a multifocal IOL. In another study of the AcrySof™ IQ Vivity™ IOL which induced low myopia in the non-dominant eye, a target of -0.50D to -1.00D significantly improved near vision [4]. The use of monovision to extend the range of patients after cataract surgery has been a well-documented approach [5, 6] but functional near vision may not be achieved with the use of monofocal IOLs. A mini-monovision approach using the AcrySof™ IQ Vivity™ [7,8,9] has been described with the non-dominant eye targeted from -0.25D to -0.75D and with good near vision achieved.
The objective of this study was to evaluate the visual outcomes following bilateral implantation of the AcrySof™ IQ Vivity™ toric IOL using the mini-monovision approach in a cohort of Asian patients.
Patients and methods
Study design
This is a prospective interventional case series of patients with bilateral cataracts and significant corneal astigmatism who desired more spectacle independence after cataract surgery. Enrolment of patients took place at LEC Eye Centre, a private ophthalmic day surgical centre in Ipoh, Malaysia from April 2022 to January 2023.
The inclusion criteria were patients aged 18 years or older with bilateral significant cataracts and significant corneal astigmatism. Patients were deemed to have significant corneal astigmatism when preoperative keratometry values for each eye were input into the Barrett Toric Calculator V1.05 (www.apacrs.org) and the calculated result showed the need for a toric IOL. Exclusion criteria were patients with history of prior refractive surgery, amblyopia, strabismus, ocular co-morbidity which would significantly impact on final visual acuity or pre-existing zonular weakness, or capsular compromise as seen during preoperative examination.
This study was approved by the Medical Research and Ethics Committee of Malaysia and all study procedures followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all individual participants of the study.
Intraocular lens
As previously described, the AcrySof™ IQ Vivity™ IOL utilises a central 2.2 mm zone which stretches and shifts the wavefront of light to achieve an elongated focus. This study specifically used the toric version of the IOL which has a cylindrical power at IOL plane of 1.00D (DFT215), 1.50D (DFT315), 2.25D (DFT415), and 3.00D (DFT515).
Preoperative assessments
All patients received full ophthalmic evaluation, slit lamp biomicroscopy and dilated fundus examination. Biometry measurements were carried out using the Lenstar LS900 (Haag-Streit, Switzerland) and VERION image-guided system (Alcon Laboratories, Inc., Fort Worth, Texas, United States) and corneal tomography was performed with the Oculyzer (Alcon Laboratories, Inc., Fort Worth, Texas, United States). IOL power calculation for spherical prediction was performed using the Barrett Universal II formula and for astigmatic correction using the online Barrett Toric Calculator V1.05 (www.apacrs.org) with the integrated-K function utilising keratometry readings from the Lenstar, VERION and Oculyzer machines. Eye dominance was determined using the Miles test and the dominant eye was targeted for emmetropia (IOL power selected with residual spherical equivalent[SE] closest to but not more than 0D) and the non-dominant eye was targeted for -0.50D (IOL power selected with residual SE closest to but not less than -0.50D). The lens factor (LF) used was based on the value provided by the online calculator.
Surgical technique
All surgeries were performed by a single surgeon through a 2.2 mm temporal corneal incision using a standard ‘stop and chop’ phacoemulsification technique with the CENTURION® Vision System (Alcon Laboratories, Inc., Fort Worth, Texas, United States) under topical anaesthesia. Intraoperative toric IOL alignment was performed using the VERION image-guided system (Alcon Laboratories, Inc., Fort Worth, Texas, United States).
Postoperative assessment
Postoperative examinations were carried out at 1 day, 1 week and 1 month (safety visits) and detailed assessments were carried out at the 3 month visit which is the primary endpoint of this study. At 3 months, monocular and binocular uncorrected (UDVA) and corrected distance visual acuities (CDVA) were measured with the Snellen chart at 6 m, uncorrected (UIVA) and distance corrected intermediate visual acuities (DCIVA) were measured with an Early Treatment Diabetic Retinopathy Study (ETDRS) chart at 66 cm and uncorrected (UNVA) and distance corrected near acuities (DCNVA) were measured with an ETDRS chart at 40 cm. All Snellen acuities were converted to logarithm of minimal angle of resolution (logMAR). Manifest refraction was carried out and distance corrected monocular and binocular defocus curves were produced with 0.5D increments (range + 2.0D to -4.0D) under photopic lighting conditions.
Patients underwent slit lamp biomicroscopy at all visits and dilated fundoscopy at 1 month and 3 months. Toric IOL position was assessed at 1 month postoperatively and measured by aligning the narrow slit lamp light beam with the IOL markings and subsequently aligning the beam with the toricCAM application (Apple Inc.) on the iPhone to determine the axis of the IOL. Analysis of astigmatism correction was carried out using the ASCRS Double Angle Plot Tool (https://ascrs.org/tools/astigmatism-double-angle-plot-tool) [10].
Contrast sensitivity was measured at the 3-month visit using the CSV-1000E (Vector Vision Co, Greenville, Ohio, USA) and was conducted under photopic and mesopic conditions at spatial frequencies of 3, 6, 12 and 18 cycles per degree (cpd).
Visual disturbances and visual function assessment
Visual disturbances were assessed using the Questionnaire for Visual Disturbances (QUVID) [11] and this questionnaire was administered at the 1 month and 3 month visits. The QUVID quantifies the frequency (0 = Never, 1 = Rarely, 2 = Sometimes, 3 = Most of the time, 4 = Always), severity (0 = None, 1 = A little, 2 = Mild, 3 = Moderate, 4 = Severe) and degree of bother (0 = Not bothered at all, 1 = Bothered a little bit, 2 = Bothered somewhat, 3 = Bothered quite a bit, 4 = Bothered very much) associated with 7 different symptoms – starbursts, haloes, glare, hazy vision, blurred vision, double vision and dark area in temporal vision.
The Visual Function Index 14 (VF-14) [12] questionnaire was used to assess patients’ visual function, and this was conducted at the 3 month visit. This questionnaire uses 14 questions based on activities of daily living and asks how much difficulty the patients have in performing these tasks with patients answers classified as None, A little, Moderate, Great deal or Unable to do and responses are quantified with a calculated score (range from 0 to 100).
Statistical analysis
Sample size calculation was performed using the results from the author’s initial experience with implanting the AcrySof™ IQ Vivity™ IOL in 10 patients. Using a one sample t-test with a reference mean difference of 0.153 logMAR between preoperative and postoperative best corrected distance visual acuity, a standard deviation of 0.239, significance level of 0.05 and a power of 90%, the required number of patients was 26. To allow for possible drop outs, it was planned to include 30 patients in this study.
All data was collected in a Microsoft Excel 2016 (Microsoft Corp., Redmond, USA) spreadsheet designed for the study and descriptive statistics including mean, standard deviation (SD), minimum and maximum values were calculated for all relevant parameters.
Results
A total of 60 eyes of 30 patients were implanted with the AcrySof™ IQ Vivity™ toric IOL and this consisted of DFT215 (n = 28), DFT315 (n = 20), DFT415 (n = 5) and DFT515 (n = 7). The baseline demographics and characteristics of all patients are shown in Table 1.
Visual acuity and refractive outcomes
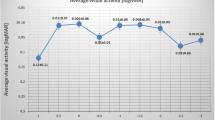
At 3 months, the mean monocular UDVA, UIVA and UNVA for dominant eyes were 0.10 ± 0.12, 0.19 ± 0.14 and 0.43 ± 0.18 logMAR respectively. The mean monocular UDVA, UIVA and UNVA for non-dominant eyes were 0.18 ± 0.24, 0.18 ± 0.10 and 0.29 ± 0.12 logMAR respectively. The mean binocular UDVA, UIVA and UNVA were 0.06 ± 0.12, 0.10 ± 0.10 and 0.27 ± 0.10 logMAR respectively (Fig. 1A). The mean monocular CDVA, DCIVA and DCNVA of all eyes were 0.05 ± 0.10, 0.19 ± 0.12 and 0.42 ± 0.14 logMAR respectively. The mean binocular CDVA, DCIVA and DCNVA were 0.03 ± 0.08, 0.12 ± 0.10 and 0.35 ± 0.10 logMAR respectively (Fig. 1B). The mean refractive spherical equivalent (MRSE) for dominant and non-dominant eyes were -0.07D ± 0.27 and -0.12D ± 0.54 respectively. The mean absolute error (MAE) for dominant and non-dominant eyes was 0.21D ± 0.17 and 0.37D ± 0.40 respectively. 92.4% and 100% of dominant eyes were within 0.50D and 1.00D of target whereas 84.6% and 96.1% of non-dominant eyes were within 0.50D and 1.00D of target (Fig. 1C and D).
A Monocular and binocular uncorrected distance (UDVA), intermediate (UIVA) and near (UNVA) visual acuities at 3 months. B Monocular and binocular corrected distance (CDVA), distance corrected intermediate (DCIVA) and distance corrected near (DCNVA) visual acuities at 3 months. C Accuracy of spherical equivalent prediction in dominant eyes at 3 months. D Accuracy of spherical equivalent prediction in non-dominant eyes at 3 months
Figure 2A shows double-angle plots of the preoperative corneal and postoperative refractive astigmatism. Preoperative corneal astigmatism centroid was 0.34D ± 1.25 @ 92° and the postoperative refractive astigmatism centroid was 0.07D ± 0.47 @ 112°. The centroid and mean absolute error of postoperative refractive astigmatism prediction (Fig. 2B) was 0.06D ± 0.47 @ 117° and 0.39D ± 0.27 respectively. 67% had ≤ 0.50D and 100% of eyes had ≤ 1.00D of postoperative refractive astigmatism respectively. The mean postoperative refractive cylinder was 0.37D ± 0.39 with 73% and 98% of eyes with ≤ 0.50D and ≤ 1.00D of target residual cylinder respectively (Fig. 2C). The mean IOL rotation was 3.85° ± 5.09 with 88.7% of eyes with less than 5° of rotation.
The monocular and binocular distance corrected defocus curves are illustrated in Fig. 3.
Contrast sensitivity
The mean photopic contrast sensitivity at 3 cpd, 6 cpd, 12 cpd and 18 cpd were 1.73 ± 0.20, 1.87 ± 0.14, 1.50 ± 0.17 and 1.02 ± 0.16 respectively. The mean mesopic contrast sensitivity at 3 cpd, 6 cpd, 12 cpd and 18 cpd were 1.60 ± 0.15, 1.80 ± 0.20, 1.50 ± 0.21 and 1.00 ± 0.14 respectively. These were very similar and comparable to the photopic contrast sensitivity of a series of monofocal eyes (n = 108) from the author’s previous study [13] as shown in Fig. 4.
Photopic and mesopic contrast sensitivities of all eyes at 3 months compared with photopic contrast sensitivity of a monofocal intraocular lens (Clareon)[13]
Visual disturbances, photic phenomena and visual function
Patients did report photic phenomena such as starbursts (n = 8, 26.7%), haloes (n = 6, 20%) and glare (n = 11, 36.7%) as well as visual disturbances such as hazy vision (n = 5, 16.7%) and blurred vision (n = 4, 13.3%) as shown in Fig. 5A. When questioned about the degree of bother, the mean scores for starbursts (1.87), haloes (1.66), glare (1.63), hazy vision (0.75) and blurred vision (0.67) with no patient complaining of double vision or a temporal dark area (negative dysphotopsia) (Fig. 5B).
VF-14 questionnaire results show that majority of patients had no to mild difficulties in performing activities of daily living with the exception of reading small print and sewing whereby patients reported mild to moderate difficulties (Fig. 5C). The mean VF-14 score was 91.77.
Discussion
The use of EDOF IOLs for presbyopia correction after cataract surgery is becoming increasingly popular with many different options available and each claiming to provide extended depth of focus using different optical principles to achieve this [14]. The ultimate objective is to provide the patient with an extended range of vision without significant compromises in visual function.
This study evaluated visual outcomes and patient reported outcomes following bilateral implantation of the AcrySof™ IQ Vivity™ EDOF toric IOL using a mini-monovision approach in a predominantly Asian population.
This study showed good binocular UDVA (0.06 ± 0.12 logMAR), UIVA (0.10 ± 0.10) and UNVA (0.27 ± 0.10). However, in their respective studies which also evaluated patients with bilateral implantation of the AcrySof™ IQ Vivity™ IOL, Van Amelsfort et al. [7] showed binocular UDVA (-0.07 ± 0.10), UIVA (0.04 ± 0.09) and UNVA (0.23 ± 0.12) and Kohnen et al. [15] showed binocular UDVA (0.01 ± 0.05), UIVA (0.07 ± 0.06) and UNVA (0.25 ± 0.11). The slightly poorer visual outcomes in this study could be a result of non-personalisation of the lens constant with consequent refractive surprise particularly in the non-dominant eyes. In our study, the mean SE in non-dominant eyes was -0.12D and the hyperopic surprise would account for the similar UIVA with the dominant eyes and also the overall poorer UNVA when compared to other similar studies [7, 15]. The poorer visual outcomes could also be due to the impact of dry eyes on biometry measurements and postoperative visual outcomes as no assessment of dry eyes was performed preoperatively and significant dry eyes was not set as an exclusion criteria for this study. The differences could also be due to different testing conditions, more specifically in this study, visual acuity was tested with the Snellen chart and subsequently converted to logMAR for analysis and as such, comparison across studies and interpretation of results should be done with caution.
The defocus curve of the non-dominant eyes did show a myopic shift due to the mini-monovision approach adopted and binocular summation is evident with improved binocular visual acuities at all distances. In this study, the refractive target in the non-dominant eye was -0.50D but Newsom et al. [8] showed that a large proportion of patients (88%) had binocular UNVA of 0.2 logMAR or better using a refractive target of -0.75D in the non-dominant eye and perhaps a more myopic target in the non-dominant eye would have achieved better UNVA in our study.
Rotational stability of the AcrySof™ IQ Vivity™ IOL has been shown to be very good [16] and this is reflected in this study as well with 88.7% of eyes with less than 5° of rotation. Van Amelsfort et al. [7] did include 8 eyes with the toric version of the AcrySof™ IQ Vivity™ IOL but no analysis of the accuracy of astigmatic correction was reported aside from IOL misalignment of 1.6° ± 1.3 and with such small numbers, a direct comparison with this study is not possible. Astigmatic correction using the Barrett toric calculator [17] has been shown to be very accurate and this is corroborated in this study as all eyes had less than 1.00D of residual refractive astigmatism postoperatively.
Results from the QUVID questionnaire in this study indicated a larger proportion of patients reporting optical phenomena compared with Van Amelsfort et al. [7] who reported a very low incidence of study subjects experiencing haloes, glare or starbursts (9%, 9% and 0% respectively) using the Likert scale to assess these optical phenomena. Kohnen et al. [15] reported a similar incidence of photic phenomena to our study with 25%, 25% and 7% of study subjects experiencing glare, haloes and ghosting respectively using a Halo and Glare Simulator (Carl Zeiss Meditec, Germany). Newsom et al. [8] who also used the QUVID questionnaire in their study to assess optical phenomena, reported higher incidences of starbursts (39%), haloes (18%) and glare (15%). The higher incidence of optical phenomena reported could be due to how the QUVID questionnaire was administered as these were not self-reported symptoms but instead patients were shown illustrations of the different photic phenomena and asked to grade the frequency, severity and degree of bother with such phenomena and consequently, this method of assessment may result in over-reporting [18]. Despite the higher incidence of optical phenomena, the majority of patients were not significantly bothered. This non-diffractive IOL still showed less optical phenomena when compared with a diffractive trifocal IOL as reported by Kohnen et al. [19] whereby 76% and 52% of study patients experienced haloes and glare respectively.
Patients in this study also scored very well on the VF-14 quality of life questionnaire which was an indication of a high visual function with only mild difficulties encountered when performing fine near tasks such as reading small print or threading a needle. This is corroborated in the study by Van Amelsfort et al. [7] which used the Dutch Catquest-9SF questionnaire and showed difficulties mainly with near activities such as reading and handicrafts.
This study had several unique features and one of which was the use of the low powered toric IOL which can correct 1.00D (or less) of corneal astigmatism and together with the use of the integrated-K function in the Barrett Toric Calculator, toric IOL prediction and astigmatic correction achieved was very good. This study being conducted in a cohort of Asian patients also provided valuable information in this demographic of patients.
This study had several limitations as it was a single arm study with no comparison with alternative intraocular lenses. This study also recruited a relatively small number of patients which may have resulted in selection bias and the short follow up of 3 months may not have accurately reflected the long term outcomes particularly in relation to photic phenomena as neuro-adaptation will have a role to reduce the incidence of such phenomena over time [20]. The lack of a protocol to assess and manage pre-existing dry eyes may also have had a significant impact on the outcomes.
In conclusion, our study had shown that bilateral implantation of this non-diffractive toric intraocular lens using a mini-monovision approach provided good functional vision at all distances with non-bothersome photic phenomena.
Data availability
No datasets were generated or analysed during the current study.
References
Breyer DRH, Kaymak H, Ax T et al (2017) Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia-Pacific J Ophthalmol 6(4):339–349
Alio JL, Plaza-Puche AB, Férnandez-Buenaga R et al (2017) Multifocal intraocular lenses: an overview. Surv of Ophthalmol 62(5):611–634
United States Food and Drug Administration. Acrysof IQ Vivity extended vision intraocular lens: Summary of safety and effectiveness data. https://www.accessdata.fda.gov/cdrh_docs/pdf/P930014S126B.pdf
Gunderson KG, Potvin R (2021) The effect of spectacle-induced low myopia in the non-dominant eye on the binocular defocus curve with a non-diffractive extended vision intraocular lens. Clin Ophthalmol 14:3541–3547
Finkelman YM, Ng JQ, Barrett GD (2009) Patient satisfaction and visual function after pseudophakic monovision. J Cataract Refract Surg 35(6):998–1002
Barrett GD (2008) Monovision with monofocal IOLs. In: Chang DF (ed) Mastering refractive IOLs: the art and science. Slack Inc, New Jersey
Van Amelsfort T, Webers VSC, Bauer NJC et al (2022) Visual outcomes of a new nondiffractive extended depth-of-focus intraocular lens targeted for minimonovision: 3-month results of a prospective cohort study. J Cataract Refract Surg 48(2):151–156
Newsom TH, Potvin R (2022) Evaluation of quality of vision and visual outcomes with bilateral implantation of a non-diffractive extended vision intraocular lens with a target of slight myopia in the non-dominant eye. Clin Ophthalmol 16:183–190
Coassin M, Mori T, Di Zazzo A et al (2022) Effect of minimonovision in bilateral implantation of a novel non-diffractive extended depth-of-focus intraocular lens: Defocus curves, visual outcomes and quality of life. Eur J Ophthalmol 32(5):2942–2948
Abulafia A, Koch D, Holladay JT et al (2018) Rethinking astigmatism analysis for intraocular lens-based surgery: suggested terminology, analysis and standards of outcome analysis. J Cataract Refract Surg 44(10):1169–1174
Lasch K, Marcus JC, Seo C et al (2022) Development and validation of a visual symptom-specific patient-reported outcomes instrument for adults with cataract intraocular implants. Am J Ophthalmol 237:91–103
Rosen PN, Kaplan RM, David K (2005) Measuring outcomes of cataract surgery using the quality of well-being scale and VF-14 visual function index. J Cataract Refract Surg 31(2):369–378
Lee MW, Cheong FM, Yeo KC (2022) Clinical evaluation of a new hydrophobic acrylic preloaded intraocular lens with a novel delivery system. Malay J Ophthalmol 4:63–74
Rocha KM (2017) Extended depth of focus IOLs: the next chapter in refractive technology? J Refract Surg 33(3):146–149
Kohnen T, Petermann K, Bohm M et al (2022) Nondiffractive wavefront-shaping extended depth-of-focus intraocular lens: visual performance and patient-reported outcomes. J Cataract and Refract Surg 48(2):144–150
Lee B, Chang D (2018) Comparison of rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmolgy 125(9):1325–1331
Ferreira T, Ribeiro P, Ribeiro F et al (2017) Comparison of methodologies using estimated or measured values of total corneal astigmatism for toric intraocular lens power calculation. J Refract Surg 33(12):794–800
Makhotkina N, Nijkamp M, Berendschot T et al (2018) Effect of active evaluation on the detection of negative dysphotopsia after sequential cataract surgery: discrepancy between incidences of unsolicited and solicited complaints. Acta Opthalmol (Copenh) 96(1):81–87
Kohnen T, Lwowski C, Hinzelmann L et al (2020) Presbyopia correction in Astigmatic eyes using a trifocal intraocular lens with quadrifocal technology. J Refract Surg 36(10):638–644
Mester U, Vaterrodt T, Goes F et al (2014) Impact of personality characteristics on patient satisfaction after multifocal intraocular lens implantation: results from the “happy patient study.” J Refract Surg 30(10):674–678
Acknowledgements
Mrs Jean Lee is the author's research assistant who has assisted in data collection and organisation
Funding
The study was funded by a grant from Alcon Malaysia.
Author information
Authors and Affiliations
Contributions
This study's principal investigator was the author who was responsible for the study design, implementation of study protocol, data collection, data analysis and manuscript preparation.
Corresponding author
Ethics declarations
Conflicts of interest
Financial support was received for this investigator-initiated trial from Alcon Laboratories (Malaysia) Sdn Bhd. The funding source had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation of the manuscript; or the decision to submit the manuscript for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, M.W. Visual outcomes following bilateral implantation of a non-diffractive extended depth of focus toric intraocular lens using a mini-monovision approach. Int Ophthalmol 44, 334 (2024). https://doi.org/10.1007/s10792-024-03247-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03247-x