Abstract
Purpose
To characterize glaucoma progression in early-stage patients with retinal nerve fiber layer (RNFL) using the change analysis software (CAS), which was utilized to track RNFL thinning.
Methods
We retrospectively analyzed 92 eyes of 92 patients with early-stage glaucoma. Patients were divided into two subgroups based on their diagnosis of pseudoexfoliation glaucoma (PEG) and primary open-angle glaucoma (POAG). A complete ophthalmologic examination was performed on all patients. Additionally, automated perimetry was conducted on each patient. Furthermore, Fourier-domain optical coherence tomography (OCT) was employed to measure RNFL and central corneal thickness. Using the OCT device’s CAS, we computed the annual rate of total and glaucomatous RNFL thinning for each patient.
Results
A total of 44 PEG and 48 POAG patients were included in the study. The right eye measurements of these patients were analyzed and compared. The two groups were not significantly different in age, gender, and the number of visits per year (p > 0.05, for each). However, the difference between the mean RNFL thickness at baseline (91.39 ± 10.71 and 96.9 ± 8.6 µm) and at the last visit (85.2 ± 15.76 µm and 91.56 ± 9.58 µm) was statistically significant between the two groups (p = 0.043, p = 0.039, respectively). Additionally, the difference in annual RNFL thinning rates (1.43 ± 0.81 µm and 1.07 ± 0.32 µm) between the two groups was statistically significant (p = 0.009).
Conclusion
The annual rate of glaucomatous RNFL loss in early-stage PEG patients (1.23 µm) was higher than in POAG patients (0.87 µm). However, despite these loss rates, scotoma was not detected in the visual field tests of these patients. Therefore, using CAS in the follow-up of early-stage glaucoma patients is a useful alternative for monitoring glaucomatous progression. Furthermore, this method can be utilized in future research for the diagnosis and follow-up of glaucoma in special populations (e.g., those with pathological myopia or high hyperopia) that are not included in normative databases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glaucoma is a chronic, progressive, neurodegenerative optic neuropathy characterized by rapid visual field (VF) loss, reduced peripapillary retinal nerve fiber layer (RNFL) thickness, and loss of retinal ganglion cells (RGCs) [1]. Early diagnosis and monitoring of glaucoma and accurate assessment of its progression are crucial in clinical practice [2]. Therefore, functional and structural tests are used for early recognition and tracking of glaucomatous damage [3]. Standard automated perimetry (SAP), a functional test, has been the gold standard test for assessing the clinical progression of glaucomatous damage for decades. However, Quigley et al. [4] reported that 40% to 50% of the RNFL is lost even when visual field defects are first detected by SAP. In addition, some studies demonstrated that 25% or more of RGCs are lost before abnormalities are detected by automated perimetry [5, 6]. Thus, structural changes in glaucoma commence before the development of optic disc cupping and visual field loss [7]. Therefore, in patients with early-stage glaucoma, VF testing may not reveal any findings, and SAP may be inadequate to diagnose glaucoma at an early stage and monitor its progression. On the other hand, in patients with advanced or late-stage glaucoma, SAP is more successful in monitoring disease progression. In conclusion, the ability to diagnose glaucoma and monitor its progression with perimetry is significantly affected by the stage of the disease [8].
Structural testing has become indispensable in clinical practice with the invention of optical coherence tomography (OCT), particularly with the transition from time-domain OCT to spectral-domain optical coherence tomography (SDOCT) [9, 10]. In particular, at the early stages of the disease, when SAP was unable to detect any VF defects, the SDOCT is of paramount importance for the diagnosis of glaucoma and the monitoring of disease progression. For instance, Gardiner and colleagues demonstrated that the longitudinal signal-to-noise ratio of RNFL measurements was superior to that of mean deviation (MD) from SAP [11]. Another study suggested that RNFL from SDOCT may provide a better measure of change than SAP MD in the early stage of the disease [12]. Findings from the studies above, OCT can detect small and true changes before VF testing in the mild stage of glaucoma. OCT can also measure many parameters, such as macular ganglion cell complex (GCC) thickness, RNFL thickness, and optic nerve head (ONH). Additionally, many studies evaluated the role of RNFL and GCC measurements in assessing glaucoma progression using SDOCT [13,14,15,16,17,18]. Although both the RNFL and GCC are measured in micrometers, it is inappropriate to directly compare rates of change between parameters because the measurements differ in magnitude and range. To overcome this problem, Hammel et al. calculated the loss rates using a dynamic-range-based normalized coefficient to compare loss rates between GCC and RNFL. They also found that normalized RNFL thickness decreased by 1.7% per year compared to a 1.3% per year decrease in GCC thickness. These results suggested that this 1.3-fold faster rate of RNFL thinning than GCC indicates that RNFL may be a more sensitive index of glaucomatous progression in early and moderate-stage glaucoma [19].
Many commercially available OCT devices have software developed to analyze glaucoma progression. Two types of software are used in OCTs, based on trend and event analysis methods [20]. In event analysis, progression is defined when the difference of a parameter of interest between the baseline and the follow-up visits is greater than the test–retest variability (or the reproducibility coefficient). In trend analysis, progression is defined when a significant negative slope is detected between the parameter of interest and time using linear regression analysis. Furthermore, trend analysis is very useful in clinical practice to determine both progression and rate of progression [21]. On the other hand, many studies in the literature using different OCT devices have found the mean rate of change of RNFL with age to be between − 0.14 and − 0.91 µm/year. These data are essential because the normal age-related loss of RNFL must be considered when monitoring glaucoma progression. Otherwise, glaucomatous progression will be found as falsely higher than its actual value [15,16,17,18, 22, 23].
Currently, when SAP is insufficient for monitoring glaucomatous progression in mild-stage glaucoma, SDOCT becomes inevitable to monitor glaucoma progression. While numerous OCT parameters are available for this purpose, RNFL is the most appropriate one. Because the macula holds around 50% of the RGCs in the retina, therefore, the health status of all RGCs can only be monitored with the RNFL [24]. Moreover, RNFL is a more sensitive index than other parameters for monitoring glaucoma progression in the early and moderate stages of the disease [19]. Therefore, in the present study, we aimed to characterize the progression of glaucoma in early-stage patients with RNFL using change analysis software (CAS).
Methods
This longitudinal, retrospective cohort study was conducted at the Diskapi Yildirim Beyazit Training and Research Hospital, Ophthalmology Clinic. The University of Health Sciences ethics committee approved the medical and health research ethics study under the Declaration of Helsinki. All subjects were recruited over 6 years between July 2017 and October 2023 from the Diskapi glaucoma clinic registry. This study enrolled 102 patients diagnosed with early-stage glaucoma. To ensure homogeneity in the follow-up period, we utilized data collected within the first 5 years of the patients' follow-up. Additionally, glaucoma was diagnosed according to the guidelines of the European Glaucoma Society (EGS) [25], and the severity of glaucoma was also determined according to the International Classification of Diseases (ICD-9) [26] staging criteria, as described below;
Stage 1: Mild or early-stage glaucoma, defined as optic nerve abnormalities consistent with glaucoma but no visual field abnormalities on any visual field test.
Stage 2: Moderate-stage glaucoma, characterized by optic nerve abnormalities consistent with glaucoma and glaucomatous visual field abnormalities in 1 hemifield, not within 5 degrees of fixation.
Stage 3: Severe-stage glaucoma, described as optic nerve abnormalities consistent with glaucoma and glaucomatous visual field abnormalities in both hemifields or loss within 5 degrees of fixation in at least one hemifield.
All patients were Caucasian and underwent a comprehensive ophthalmic examination including visual acuity, slit-lamp biomicroscopy, intraocular pressure (IOP) measurement by Goldmann applanation tonometry (GAT), iridocorneal angle measurement with Goldmann three-mirror lens, and dilated fundoscopy. Furthermore, automated perimetry measurement was performed using Humphrey Field Analyzer (Carl Zeiss Meditec Inc.). In addition, RNFL and central corneal thickness (CCT) measurements using Fourier-domain OCT (RTVue-XR 100 Avanti, software v. 18.1.0.33, Optovue, Inc. Fremont, CA, USA) were performed for each patient. In order to avoid potential impacts on the OCT and visual field (VF) testing results due to the use of proparacaine and fluorescein, GAT measurements were conducted after the OCT and VF testing. Additionally, since the 24–2 test has limited ability to detect or accurately identify central visual field loss, patients underwent both the 24–2 Swedish Interactive Threshold Algorithm (SITA)-Fast VF test and the 10–2 VF test annually [27, 28]. Furthermore, VFs with more than 20% fixation loss or more than 33% false-negative or false-positive errors were automatically excluded, and normal VFs were defined as those with a mean deviation (MD) and pattern standard deviation (PSD) within the 95% confidence limits and a glaucoma hemifield test (GHT) result within normal limits.
Patients diagnosed with PEG and POAG according to EGS guidelines were included in this study. In all patients diagnosed with PEG and POAG, IOP measured by GAT was higher than 21 mmHg. Dilated fundoscopy revealed cup-to-disc ratios greater than 0.3. Iridocorneal angle measurement was performed using the Goldmann three-mirror lens. The angle width was graded as 3 or 4 according to the Schafer angle grading system, indicating that at least a scleral spur structure was visible on examination in all patients. Moreover, the Sampaolesi line was observed in some of the PEG patients. Additionally, a slit-lamp biomicroscopic examination of patients diagnosed with PEG revealed the accumulation of pseudoexfoliative material on the anterior lens capsule. Furthermore, some PEG patients experienced pigment loss from the pupil margin, resulting in a moth-eaten appearance. Other inclusion criteria were best-corrected visual acuity (BCVA) of 20/40 or better, spherical refraction ≤ 5 diopters, and cylinder correction ≤ 3 diopters. On the other hand, eyes that underwent ocular surgery such as phacoemulsification, trabeculectomy, and vitreoretinal surgery during the study period and eyes that developed any macular pathology and any glaucomatous VF defect during the follow-up period were excluded.
Fourier-domain OCT
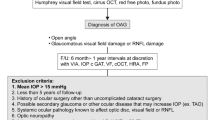
RTVue uses a super luminescent diode wavelength of 840 ± 10 nm to acquire high resolution images. It is also capable of collecting 70,000 A-scans per second with an axial resolution of 5 µm. All patients underwent the ONH protocol with the RTVue device. The ONH protocol consists of 12 radial scans of 3.4 mm in length, and 13 concentric ring scans ranging from 1.3–4.9 mm in diameter, and all rings are centered on the optic disc and used to generate an RNFL thickness map. In addition, the RNFL thickness measurement is sampled relative to the center of the disc, not the center of the 3.45 mm diameter scanning beam, so that small distortions of the center of the disc relative to the scanning beam do not affect the measurement. Furthermore, image quality was carefully checked after each image acquisition. Only images of adequate quality were used in the study. Although, as defined by the RTVue user manual guide [29], a signal strength index (SSI) > 28 was sufficient for image quality, only images with SSI > 40 were used. Finally, the instrument includes software that uses a trend analysis method called change analysis. This software can calculate the annual rate of change in RNFL, 95% confidence interval, and p-value. A minimum of 3 measurements are required for the software to perform this calculation. It can also evaluate up to a maximum of 6 measurements. In the output of change analysis, the data of all measurements are available. In addition, the RNFL thickness results from each measurement are displayed side by side in eight quadrants (Fig. 1). This allows all measurements to be viewed and evaluated together.
Change analysis output sample of Optovue optical coherence tomography device. (All measured RNFL values for the patient are displayed in a side-by-side format at the top of the output page, along with the corresponding measurement dates. A graphical representation of these values in eight quadrants is also demonstrated at the bottom right. The age-RNFL thickness graph and the annual RNFL loss rate calculated by the CAS software are shown at the bottom left of the output)
Statistical analysis
SPSS v.18.0 for Windows (SPSS Inc. IBM Corp. Chicago. IL. USA) was used for statistical analysis of the data. Descriptive statistics are presented as mean ± standard deviations. The Pearson chi-square test was used for categorical data. A multifaceted approach was employed to check the normal distribution of the variables. Graphs and quantitative statistical tests were used to determine the normal distribution of the data. The Histogram and Q-Q plot were used to visually assess whether the data are normally distributed. Skewness and kurtosis values were evaluated afterwards. Lastly, the Shapiro–Wilk test and the Kolmogorov–Smirnov test were applied to assess the normal distribution of data. If the p-value is greater than 0.05, it can be concluded that the data is normally distributed. In this study, we determined whether the data followed a normal distribution or not by analyzing the graphs and statistical test results. The Mann–Whitney U test was used to analyze data that did not follow a normal distribution, while the independent samples t-test was used to assess data that did follow a normal distribution. Finally, statistical significance was set at p < 0.05.
Results
One hundred and two patients were enrolled in this study. The study cohort included 50 cases of pseudoexfoliation glaucoma (PEG) and 52 cases of primary open-angle glaucoma (POAG). During the follow-up period, six PEG patients were excluded from the study for the following reasons: (One patient underwent 5-FU trabeculectomy due to uncontrolled IOP with topical treatment, while three patients underwent phacoemulsification due to nuclear cataract, and two other patients developed arcuate defects on visual field testing). In the POAG patients, one patient underwent 5-FU trabeculectomy, the other two developed nasal step defects in the visual field, and one patient underwent vitreoretinal surgery due to traumatic vitreoretinal hemorrhage (Table 1). For these reasons, four patients were excluded from the study. Finally, a total of 44 PEG and 48 POAG patients' right eye measurements were analyzed in this study.
All data from the two groups are demonstrated in Table 2. The mean age was 68.5 ± 8.9 years in the PEG group and 64.2 ± 10.3 years in the POAG group. There were 20 females and 24 males in the PEG group and 26 females and 22 males in the POAG group. There were no statistically significant differences in age and gender between the groups (p = 0.064 and 0.078, respectively). In addition, the difference between the two groups in the number of visits per year (1.88 ± 0.76 and 1.6 ± 0.42) was not statistically significant (p > 0.05). However, the difference between the mean RNFL thickness at baseline (91.39 ± 10.71 and 96.9 ± 8.6 µm) and at the last visit (85.2 ± 15.76 µm and 91.56 ± 9.58 µm) was statistically significant between the two groups (p = 0.043, p = 0.039, respectively). Furthermore, the difference in annual RNFL thinning rates (1.43 ± 0.81 µm and 1.07 ± 0.32 µm) between the two groups was statistically significant (p = 0.009). In addition, the mean CCT was 518.52 ± 34.16 µm in the PEG patients and 540.27 ± 32.13 µm in the POAG patients. POAG group had significantly thicker CCT (p = 0.002). Finally, the mean IOP in five years (the arithmetic mean of each patient's IOP measurements at each visit over five years) was 15.12 ± 2.12 mm Hg in the PEG group and 17.37 ± 2.2 mm Hg in the POAG group. There was a statistically significant difference in mean IOP between the two groups (p < 0.001). Finally, the initial cup/disc ratio was 0.46 ± 0.08 in the PEG group and 0.45 ± 0.1 in the POAG group. There was no statistically significant difference between the two groups (p = 0.217).
Discussion
In the study, we analyzed the glaucomatous progression in early-stage PEG and POAG patients by calculating the annual rate of RNFL thinning using the CAS of RTVue SDOCT. The CAS establishes the initial two RNFL measurements as baseline data and compares subsequent measurements to this baseline data to determine the annual rate of RNFL change [29]. Notably, the results in the CAS are not linked to data obtained from the normative database. This approach prevents any errors caused by anatomical variations, refractive errors, race, or age-related differences, ensuring that the results are specific to the patient being examined. However, to this very useful advantage for clinical use, the CAS also has some disadvantages because it uses simple regression analysis. For example, an eye with an RNFL thickness of 90 microns and a real annual glaucomatous thinning rate of − 1 µm/year, if monitored annually for five years, the RNFL thickness is mathematically expected to decrease by 1 micron per measurement, from 90 to 85 microns, in the form of 90 µm—89 µm—88 µm—87 µm—86 µm—85 µm. However, in real clinical conditions, the annual change in RNFL thickness in patients does not exactly follow this mathematical expectation and may be observed as 90 µm—91 µm—89 µm—87 µm—86 µm—85 µm—86 µm [30]. This was taken into account in our study.
In the literature, there were only three studies investigating glaucoma progression with the Optovue SDOCT. First, Iverson et al. [16] found a mean RNFL thinning of 1.15 µm/year in a total of 74 patients with suspected glaucoma and preperimetric glaucoma who were followed up for an average of 43 months and a mean age-related RNFL thinning of 0.91 µm/year in 23 healthy participants. In this study, these results were obtained by comparing outside normal limits using a method similar to event analysis. Second, Naghizadeh et al. [17] revealed a mean RNFL thinning of 0.33 µm/year and 0.24 µm/year in 51 perimetric glaucoma patients and 17 healthy subjects followed up for 1.5–3 years, respectively. However, if we carefully analyzed these two studies, we realized that the groups are very asymmetric and that the patient group is almost three times larger than the healthy group. In addition, the RTVue SDOCT devices used in the two studies described above do not include an eye tracking system, so even small saccadic eye movements may have affected the RNFL measurement outcomes. On the other hand, Holló et al. [18] found a mean RNFL loss of 0.33, 0.44, and 0.69 µm/year in 17 healthy subjects, 17 patients with treated ocular hypertension, and 67 patients with POAG, respectively, with a mean follow-up of 5 years. However, it is unclear that trend analysis software was used to calculate the annual loss rate, although it was available on the OCT device used in this study. The study method states that the new software (version 6.12) of the Avanti RTVue-XR OCT device was used to calculate the annual loss rate. In this study, as in the previous two studies, the groups were very asymmetrical in number, which affected the statistical calculations. In addition, the group of glaucoma patients was not divided according to the severity of the disease. It is possible that early, moderate, and advanced-stage patients were all evaluated in the same group. Therefore, while the mean RNFL loss rate in the POAG group was 0.69 µm/year, there were patients with a high thinning rate of 4.35 µm/year. In contrast to the three studies discussed above, our study used the CAS to calculate the annual RNFL loss rate. In addition, the RTVue-XR 100 Avanti software v. 18.1.0.33 SDOCT device we used in our study has an eye tracking system, and the age-related loss rate, which was found to be different in many studies [15,16,17,18, 22, 23], is available in the CAS as 0.2 µm/year [29]. Therefore, a control group of healthy subjects was not included in the present study to calculate the rate of age-related loss. Moreover, all our patients were at the same glaucoma stage and were evaluated according to their clinical glaucoma type. The present study is the first in the literature to demonstrate that the annual rate of glaucomatous RNFL thinning is higher in early-stage PEG patients than in POAG patients and that the clinical type of glaucoma affects the annual rate of RNFL thinning. These are the strengths of our study compared to the three studies mentioned above.
In the existing literature, apart from the Optovue SDOCT device, studies examining the annual change of RNFL in glaucoma patients were performed with the Cirrus OCT (Carl Zeiss Meditec, Dublin, CA) and Spectralis OCT (Heidelberg Engineering, GmbH, Dossenheim, Germany) devices. The Spectralis OCT does not include any analysis software, while the Cirrus OCT includes both trend and event analysis software. When evaluating the literature studies conducted with Cirrus OCT device, in their study Leung et al. [15] evaluated 150 eyes of 90 glaucoma patients. They found that 41 eyes exhibited glaucomatous progression over an average follow-up period of 45 months. The mean annual RNFL thinning in these eyes was 1.53 µm/year. However, the clinical glaucoma types and stages of the glaucoma patients in the study were not specified. Hammel and colleagues [19] analyzed 97 open-angle glaucoma patients. The mean annual RNFL loss in these patients was 0.98 µm/year. The glaucoma stages of the patients in this study were not specified. Na et al. [31] observed an annual RNFL loss of 0.62 µm/year in 87 eyes with pre-perimetric glaucoma. In 40 patients with perimetric glaucoma, the annual RNFL loss was 0.69 µm/year. The clinical glaucoma types of the patients in this study were not specified. In all three studies described above, the annual RNFL loss rates were calculated using statistical linear mixed-effect modeling, rather than the trend analysis software of the Cirrus OCT device. Finally, Yu and colleagues [32] prospectively followed 240 eyes of 139 POAG patients for 5 years and determined annual RNFL thinning using trend analysis software. In the study, glaucomatous progression was identified in 117 of the 240 eyes in the study. The annual RNFL thinning in these progressing eyes was 0.72 µm/year. It should be noted that the glaucoma stages of the patients were not specified in this study. Conversely, when examining the literature studies conducted with the Spectralis OCT device, Wessel et al. [23] examined 38 eyes with POAG. Glaucomatous progression was observed in 13 of the 38 eyes, with an annual RNFL loss of 2.12 µm/year. In the 25 eyes without glaucomatous progression, this rate was 1.18 µm/year. In the study by Miki and colleagues [33] 454 eyes of 294 OHT patients were examined. The annual RNFL thinning of 40 eyes that developed VF defects was found to be 2.02 µm/year. In the 414 eyes without glaucomatous progression, this rate was 0.82 µm/year. In these two studies with Spectralis OCT, annual RNFL loss rates were calculated using statistical linear mixed-effect modeling. This is because Spectralis OCT does not include analytical software for trend or event analysis. Consequently, a direct comparison between the results of the six studies discussed in this paragraph and the results of our study is not possible. This is due to the fact that the clinical glaucoma types, glaucoma stages, refraction values, and races of the patients in the studies were not homogeneous. Furthermore, trend analysis software was not used in five of the studies. Finally, the normative database utilized to obtain RNFL thickness values differs between these studies.
The current investigation offers novel findings on the rate of annual RNFL thinning in early-stage PEG and POAG patients. To our knowledge, this is the first study utilizing the CAS. Our results indicate that the average annual RNFL thinning was 1.43 ± 0.81 µm/year in PEG patients and 1.07 ± 0.32 µm/year in POAG patients after the five-year follow-up period. Although IOP was under control in both groups, it is an expected finding that annual RNFL thinning is faster in PEG patients than in POAG patients, and the reasons are as follows: First, diurnal IOP fluctuations are higher in PEG than in POAG [34]. Second, dysregulated expression of the lysyl oxidase-like 1 gene decreases tissue resistance in the lamina cribrosa, leading to glaucomatous optic atrophy even when IOP is in the normal range [35]. Third, dysfunction in intracellular autophagy processes and mitochondrial abnormalities have been demonstrated in Tenon's capsule-derived fibroblasts from patients with PEG. As in age-related macular degeneration, this autophagy disorder and decreased lysosomal activity lead to the accumulation of intracellular waste products, that affect the functions of retinal ganglion cells and cause neurodegeneration [36]. For the reasons described above, we propose three recommendations for the treatment and follow-up of early-stage PEG patients. First, the EGS guideline recommends an IOP level of 18 to 20 mmHg with at least a 20% reduction in IOP as the target IOP for early-stage glaucoma patients. However, in our study, although the mean IOP of PEG patients was 15.12 mmHg, the annual thinning of the RNFL was higher than in POAG patients. Therefore, it can be concluded that maintaining a target IOP level below the IOP level recommended in the EGS guideline during the follow-up of early-stage PEG patients will be beneficial in slowing RNFL thinning. Our second recommendation, although the level of evidence is low, is that neuroprotective agents such as brimonidine and coenzyme Q10 can be added to topical treatment [37, 38]. Our third recommendation is that early-stage PEG patients should be followed more closely, with more visits than POAG patients.
The most commonly utilized test pattern for the detection of glaucomatous damage in SAP is 24–2. This pattern is frequently selected for its capacity to reduce the test duration and eliminate frame artifacts. However, with this test, only four points in the central 8-degree retinal region are evaluated. Additionally, this test scans 54 points in a central retinal area of 27 degrees nasally and 21 degrees temporally at 6-degree intervals. The 10–2 test pattern, which scans the central 10 degrees at 2 degree intervals, tests 68 points in this region and is more effective at detecting central scotomas than the 24–2 test pattern [28]. However, if glaucomatous damage has occurred in the RGCs between these scanned points, SAP will not be able to detect it. There is also considerable redundancy in the visual system. A stimulus projected to a particular retinal location affects many RGCs at that location. Therefore, even if some RGCs at that location are dead, other RGCs serving the same area can still perceive the stimulus [27]. For the reasons described above, SAP can only detect glaucomatous damage in early stage glaucoma patients with 50% RNFL loss and 25% RGC loss [5,6,7]. For clinical practice, SDOCT is essential for diagnosis and follow-up of early glaucoma when SAP was insufficient. Finally, based on the results of our study, we recommend that clinicians utilize new software such as CAS, especially for monitoring the progression of early-stage glaucoma.
CCT is considered an important variable in glaucoma. Despite its effect on IOP measurement, literature has highlighted its impact on glaucoma progression. Patients with advanced damage are more likely to have a thin CCT [39]. In addition, ocular hypertension (OHT) patients with thin corneas had thinner RNFL measurements compared with ocular hypertensives with thick corneas [40]. Moreover, the widely accepted results are from the multicentre Ocular Hypertension Study (OHTS) which revealed that the risk for the development of POAG from OHT is greater in eyes with thinner CCT and lower in eyes with thicker CCT [41]. Some literature studies have found a significant correlation between CCT and RNFL in POAG patients [42, 43], while other studies have not found a significant correlation between these two variables in POAG patients [44, 45]. PEG patients have been reported to have thinner CCT compared with normal controls [39, 46, 47]. In accordance with the existing literature, our study found that patients with PEG had a thinner CCT than those with POAG. OHTS also highlighted that a thin CCT is a risc factor for glaucoma development, independent of IOP. Therefore, the thinner CCT value observed in PEG patients may have contributed to their higher glaucomatous progression rate compared to POAG patients.
Nonetheless, our study has several limitations. First and most importantly, the CAS uses only simple regression. Second, this study is limited by its retrospective design. Retrospective studies use data that were collected in the past for another objective, which means that investigators lack control over the collection of data. Additionally, it is difficult to measure and control the outcome, predictor, and confounding variables in retrospective studies. Third, we cannot draw conclusions for other races because the study included only Caucasian patients. Finally, since we included patients between − 5 and + 5 D, the data we found cannot be used in advanced myopic and hyperopic patients. Due to the aforementioned limitations of the study, in order to compare and generalize the annual RNFL loss data obtained in the present study with that obtained in other studies, it is necessary that the groups in the studies to be compared be homogeneous in many aspects (age, race, gender, refractive error, clinical glaucoma type and stage). Otherwise, the data obtained can only be generalized for the studied patient group.
In conclusion, to the best of our knowledge, the present study reported the annual rate of glaucomatous RNFL loss in early-stage PEG and POAG patients using CAS for the first time in the literature. This rate was found to be 1.23 ± 0.81 µm/year and 0.87 ± 0.32 µm/year in PEG and POAG patients, respectively, when age-related loss of 0.2 µm/year was subtracted from the annual RNFL thinning rate of patients. However, despite this level of glaucomatous damage, scotoma was not detected in the visual field tests of these patients for five years. Ultimately, we believe that this approach will be valuable in monitoring early-stage glaucoma patients and we recommend its use. Furthermore, the data obtained with CAS are independent of the normative database of the OCT device. Consequently, this method can be employed in future research for the diagnosis and follow-up of glaucoma in special populations (pathologic myopia, high hyperopia, etc.) that are not included in normative databases.
References
Dielemans I, Vingerling JR, Wolfs RC et al (1994) The prevalence of primary open-angle glaucoma in a population-based study in The Netherlands. Rotterdam Study Ophthalmol 101:1851–1855. https://doi.org/10.1016/s0161-6420(94)31090-6
Quigley HA, Miller NR, George T (1980) Clinical evaluation of nerve fiber layer atrophy as an indicator of glaucomatous optic nerve damage. Arch Ophthalmol 98:1564–1571. https://doi.org/10.1001/archopht.1980.01020040416003
Keltner JL, Johnson CA, Anderson DR et al (2006) The association between glaucomatous visual fields and optic nerve head features in the ocular hypertension treatment study. Ophthalmology 113:1603–1612. https://doi.org/10.1016/j.ophtha.2006.05.061
Quigley HA, Addicks EM, Green WR (1982) Optic nerve damage in human glaucoma III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema and toxic neuropathy. Arch Ophthalmol 100:135–146. https://doi.org/10.1001/archopht.1982.01030030137016
Quigley HA, Dunkelberger GR, Green WR (1989) Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol 107:453–464. https://doi.org/10.1016/0002-9394(89)90488-1
Kerrigan-Baumrind LA, Quigley HA, Pease ME et al (2000) Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci 41:741–748
Cvenkel B, Kontestabile AS (2011) Correlation between nerve fibre layer thickness measured with spectral domain OCT and visual field in patients with different stages of glaucoma. Graefes Arch Clin Exp Ophthalmol 249:575–584. https://doi.org/10.1007/s00417-010-1538-z
Abe RY, Diniz-Filho A, Zangwill LM et al (2016) The relative odds of progressing by structural and functional tests in glaucoma. Invest Ophthalmol Vis Sci 57:421–428. https://doi.org/10.1167/iovs.15-18940
Miki A, Medeiros FA, Weinreb RN et al (2014) Rates of retinal nerve fiber layer thinning in glaucoma suspect eyes. Ophthalmology 1212:1350–1358. https://doi.org/10.1016/j.ophtha.2014.01.017
Yu M, Lin C, Weinreb RN et al (2016) Risk of visual field progression in glaucoma patients with progressive retinal nerve fiber layer thinning a 5-year prospective study. Ophthalmology 123:1201–1210. https://doi.org/10.1016/j.ophtha.2016.02.017
Gardiner SK, Fortune B, Demirel S (2013) Signal-to-noise ratios for structural and functional tests in glaucoma. Transl Vis Sci Technol 2:3. https://doi.org/10.1167/tvst.2.6.3
Medeiros FA, Zangwill LM, Bowd C et al (2012) The structure and function relationship in glaucoma: implications for detection of progression and measurement of rates of change. Invest Ophthalmol Vis Sci 53:6939–6946. https://doi.org/10.1167/iovs.12-10345
Sung KR, Na JH, Lee Y (2012) Glaucoma diagnostic capabilities of optic nerve head parameters as determined by Cirrus HD optical coherence tomography. J Glaucoma 21:498–504. https://doi.org/10.1097/ijg.0b013e318220dbb7
Na JH, Sung KR, Lee JR et al (2013) Detection of glaucomatous progression by spectral-domain optical coherence tomography. Ophthalmology 120:1388–1395. https://doi.org/10.1016/j.ophtha.2012.12.014
Leung CK, Ye C, Weinreb RN et al (2013) Impact of age-related change of retinal nerve fiber layer and macular thicknesses on evaluation of glaucoma progression. Ophthalmology 120:2485–2492. https://doi.org/10.1016/j.ophtha.2013.07.021
Iverson SM, Feuer WJ, Shi W et al (2014) Frequency of abnormal retinal nerve fibre layer and ganglion cell layer SDOCT scans in healthy eyes and glaucoma suspects in a prospective longitudinal study. Br J Ophthalmol 98:920–925. https://doi.org/10.1136/bjophthalmol-2013-303877
Naghizadeh F, Garas A, Vargha P et al (2014) Detection of early glaucomatous progression with different parameters of the RTVue optical coherence tomograph. J Glaucoma 23:195–198. https://doi.org/10.1097/ijg.0b013e31826a9707
Holló G, Zhou Q (2016) Evaluation of retinal nerve fiber layer thickness and ganglion cell complex progression rates in healthy, ocular hypertensive, and glaucoma eyes with the avanti RTVue-XR optical coherence tomograph based on 5-year follow-up. J Glaucoma 25:e905–e909. https://doi.org/10.1097/ijg.0000000000000410
Hammel N, Belghith A, Weinreb RN et al (2017) Comparing the rates of retinal nerve fiber layer and ganglion cell-inner plexiform layer loss in healthy eyes and in glaucoma eyes. Am J Ophthalmol 178:38–50. https://doi.org/10.1016/j.ajo.2017.03.008
Leung CK (2014) Diagnosing glaucoma progression with optical coherence tomography. Curr Opin Ophthalmol 25:104–111. https://doi.org/10.1097/icu.0000000000000024
Yu M, Weinreb RN, Yiu C et al (2011) Computer simulation of progressive retinal nerve fiber layer loss in glaucoma: performance of event and trend analyses. Invest Ophthalmol Vis Sci 52:9674–9683. https://doi.org/10.1167/iovs.11-8052
Zhang X, Francis BA, Dastiridou A et al (2016) Longitudinal and cross-sectional analyses of age effects on retinal nerve fiber layer and ganglion cell complex thickness by fourier-domain OCT. Transl Vis Sci Technol 5:1. https://doi.org/10.1167/tvst.5.2.1
Wessel JM, Horn FK, Tornow RP et al (2013) Longitudinal analysis of progression in glaucoma using spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 54:3613–3620. https://doi.org/10.1167/iovs.12-9786
Curcio CA, Allen KA (1990) Topography of ganglion cells in human retina. J Comp Neurol 300:5–25. https://doi.org/10.1002/cne.903000103
BMJ Publishing Group Ltd BMA House, Square T, London, 9jr W. (2017) European Glaucoma Society Terminology and Guidelines for Glaucoma, 4th Edition - Chapter 2: classification and terminology. Br J Ophthalmol 101:73–127. https://doi.org/10.1136/bjophthalmol-2016-egsguideline.002
Parekh AS, Tafreshi A, Dorairaj SK et al (2014) Clinical applicability of the international classification of disease and related health problems (ICD-9) glaucoma staging codes to predict disease severity in patients with open-angle glaucoma. J Glaucoma 23:18–22. https://doi.org/10.1097/ijg.0000000000000033
Grillo LM, Wang DL, Ramachandran R et al (2016) The 24–2 Visual field test misses central macular damage confirmed by the 10–2 visual field test and optical coherence tomography. Transl Vis Sci Technol 5:15. https://doi.org/10.1167/tvst.5.2.15
De Moraes CG, Hood DC, Thenappan A et al (2017) 24–2 Visual fields miss central defects shown on 10–2 tests in glaucoma suspects, ocular hypertensives, and early glaucoma. Ophthalmology 124:1449–1456. https://doi.org/10.1016/j.ophtha.2017.04.021
Optovue, RTVue-XR 100 Avanti software User Manual Guide (2015) 113–117.
Wu Z, Saunders LJ, Zangwill LM et al (2017) Impact of normal aging and progression definitions on the specificity of detecting retinal nerve fiber layer thinning. Am J Ophthalmol 181:106–113. https://doi.org/10.1016/j.ajo.2017.06.017
Na JH, Sung KR, Baek SH et al (2015) Rates and patterns of macular and circumpapillary retinal nerve fiber layer thinning in preperimetric and perimetric glaucomatous eyes. J Glaucoma 24:278–285. https://doi.org/10.1097/ijg.0000000000000046
Yu M, Lin C, Weinreb RN et al (2016) Risk of visual field progression in glaucoma patients with progressive retinal nerve fiber layer thinning: a 5-year prospective study. Ophthalmology 123:1201–1210. https://doi.org/10.1016/j.ophtha.2016.02.017
Miki A, Medeiros FA, Weinreb RN et al (2014) Rates of retinal nerve fiber layer thinning in glaucoma suspect eyes. Ophthalmology 121:1350–1358. https://doi.org/10.1016/j.ophtha.2014.01.017
Tarkkanen AH, Kivela TT (2015) Comparision of primary open-angle glaucoma and exfoliation glaucoma at diagnosis. Eur J Ophthalmol 25:137–139. https://doi.org/10.5301/ejo.5000516
Netland PA, Ye H, Streeten BW et al (1995) Elastosis of the lamina cribrosa in pseudoexfoliation syndrome with glaucoma. Ophthalmology 102:878–886. https://doi.org/10.1016/s0161-6420(95)30939-6
Want A, Gillespie SR, Wang Z et al (2016) Autophagy and mitochondrial dysfunction in tenon fibroblasts from exfoliation glaucoma patients. PLoS ONE 11:e0157404. https://doi.org/10.1371/journal.pone.0157404
Saylor M, McLoon LK, Harrison AR et al (2009) Experimental and clinical evidence for brimonidine as an optic nerve and retinal neuroprotective agent: an evidence-based review. Arch Ophthalmol 127:402–406. https://doi.org/10.1001/archophthalmol.2009.9
Martucci A, Mancino R, Cesareo M et al (2022) Combined use of coenzyme Q10 and citicoline: a new possibility for patients with glaucoma. Front Med (Lausanne) 15(9):1020993. https://doi.org/10.3389/fmed.2022.1020993
Kniestedt C, Lin S, Choe J et al (2006) Correlation between intraocular pressure, central corneal thickness, stage of glaucoma, and demographic patient data: prospective analysis of biophysical parameters in tertiary glaucoma practice populations. J Glaucoma 15:91–97. https://doi.org/10.1097/00061198-200604000-00003
Kaushik S, Gyatsho J, Jain R et al (2006) Correlation between retinal nerve fiber layer thickness and central corneal thickness in patients with ocular hypertension: an optical coherence tomography study. Am J Ophthalmol 141:884–890. https://doi.org/10.1016/j.ajo.2005.12.026
Gordon MO, Beiser JA, Brandt JD et al (2002) The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 120:714–720. https://doi.org/10.1001/archopht.120.6.714
Mohamed EY, Basiony AI, Ibrahim A (2019) Correlation between central corneal thickness and retinal nerve fiber layer thickness in open-angle glaucoma. Delta J Ophthalmol 20:55–62. https://doi.org/10.4103/DJO.DJO_69_18
Wangsupadilok B, Orapiriyakul L (2014) Correlation between central corneal thickness and visual field defect, cup to disc ratio and retinal nerve fiber layer thickness in primary open-angle glaucoma patients. J Med Assoc Thai 97(7):1. https://doi.org/10.12669/pjms.331.11623
Sarfraz MH, Mehboob MA, Ul Haq RI et al (2017) Correlation between central corneal thickness and visual field defects, cup to disc ratio and retinal nerve fiber layer thickness in primary open angle glaucoma patients. Pak J Med Sci 33:132–136. https://doi.org/10.12669/pjms.331.11623
Day AC, Machin D, Aung T, Gazzard G, Husain R, Chew PT, Khaw PT, Seah SK, Foster PJ (2011) Central corneal thickness and glaucoma in East Asian people. Invest Ophthalmol Vis Sci 52(11):8407–8412. https://doi.org/10.1167/iovs.11-7927
Aghaian E, Choe JC, Lin S et al (2004) Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology 111:2211–2219. https://doi.org/10.1016/j.ophtha.2004.06.013
Ozcura F, Aydin S, Dayanir V (2011) Central corneal thickness and corneal curvature in pseudoexfoliation syndrome with and without glaucoma. J Glaucoma 20:410–413. https://doi.org/10.1097/ijg.0b013e3181f7afb8
Funding
The authors declare no financial support.
Author information
Authors and Affiliations
Contributions
NE and OC took part in all steps of the manuscript together.
Corresponding author
Ethics declarations
Conflict of interest
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no financial support or financial conflicts of interest. The authors have reported no financial relationship with any company and no external funding.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration of 1964 and its subsequent amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eraslan, N., Celikay, O. Rates of retinal nerve fiber layer loss in early-stage pseudoexfoliation and primary open-angle glaucoma patients using optical coherence tomography. Int Ophthalmol 44, 250 (2024). https://doi.org/10.1007/s10792-024-03214-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03214-6